Abstract
Introduction: Sickle cell disease (SCD) is a genetic disorder that is widely observed on a global scale and known for its substantial negative impact on health and mortality. The purpose of this research was to explore how SCD influences the outcomes of acute coronary syndrome (ACS) and Percutaneous Coronary Intervention (PCI). Methods: A retrospective observational analysis was conducted using the National Inpatient Sample (NIS) data for the year 2020. Adult patients with concurrent ACS and SCD diagnoses were included in the study. Demographic information, clinical characteristics, in-hospital outcomes, and PCI complications were examined and compared between ACS patients with and without SCD. Results: Among a total of 779,895 ACS patients, 1495 had coexisting SCD. SCD patiets exhibited distinct demographic features, such as younger age (mean age: 59 vs. 66 years), predominantly female (53% vs. 35%), and primarily African American (91% vs. 11%). Comorbid conditions such as hypertension and chronic lung disease were more prevalent in SCD patients. While inpatient mortality odds did not significantly differ, SCD patients demonstrated slightly shorter lengths of stay in cases of STEMI and NSTEMI/UA. Notably, SCD patients faced a statistically significant increased risk of coronary dissection, highlighting a unique complication in this population. Although an increased incidence of atrial fibrillation and acute heart failure was observed in SCD patients, statistical significance was not achieved. Conclusions: This study provides valuable insight into the intricate interplay between SCD and ACS outcomes. SCD patients presented with distinctive demographic and clinical profiles that influenced their experience with ACS. The elevated risk of coronary dissection emphasizes the necessity for tailored interventions and careful management in SCD patients. These findings underscore the need for further research to elucidate underlying mechanisms and optimize treatment strategies for individuals with both SCD and ACS.
1. Introduction
Sickle cell disease (SCD), arising from a single point mutation found on the hemoglobin beta gene, presents a global health concern, affecting over 300,000 infants annually, with projections reaching 400,000 by 2050 [1]. This autosomal recessive genetic disorder holds a higher prevalence among African Americans, with 1 in 500 affected and 1 in 12 carrying the gene [2]. Structurally, hemoglobin S (HbS) or sickle hemoglobin is oriented in a tetramer configuration made up of two β-globin subunits. In such conditions as deoxygenation, the hemoglobin S will precipitate aggregation with other hemoglobin, giving rise to large polymerizations that contribute to an alteration in the overall red cell morphology. At baseline, HbS has a reduced oxygen affinity that exacerbates HbS polymerization and, in turn, further reduces HbS oxygen affinity. This aggregation is a direct result of the hemoglobin S substituting the negatively charged β6 glutamic acid with its hydrophobic counterpart valine [2,3]. SCD’s intricate pathophysiology involves microvascular blockages that disrupt blood flow due to abnormal hemoglobin responses under conditions like hypoxemia, acidosis, dehydration, and stress, leading to painful crises and tissue damage [3]. This cascades into recurrent cycles of ischemia and reperfusion, impacting organ systems, including the heart [4,5]. The expansion of preventative and medical interventions has decreased morbidity and mortality associated with SCD in developed countries. As patients continue to live longer, the long-term impact of vaso-occlusive events leads to the onset of complications within organ systems, especially pronounced in the cardiovascular system. The intriguing link between SCD and acute coronary syndrome (ACS), encompassing events like heart attacks, has emerged from autopsy studies, highlighting a notable proportion of cardiovascular-related deaths in the SCD population, and SCD remains a substantial contributor to premature mortality in the United States [1,6,7,8].
While the existing literature has enriched our understanding of this relationship, a comprehensive grasp of the dynamics and associated risk factors remains limited. This study aims to further explore the impact of SCD on ACS, contributing to a more comprehensive, scientific, holistic understanding of their overarching interplay.
2. Methods
2.1. Study Design
This was a retrospective observational study of adult patients who were admitted for ACS with and without sickle cell disease as a comorbidity within the United States for the year 2020. Among both groups, demographic information, clinical characteristics, and in-hospital outcomes were compared. This study aimed to assess the impact of SCD on ACS patient outcomes as it specifically relates to inpatient mortality, length of stay, hospital charges, and time from admission to percutaneous coronary intervention (PCI). Figure 1 serves as a visual representation of the study methodology including data collection, analysis, interpretation, and outcomes, providing an overview of the analytical framework employed in this investigation.
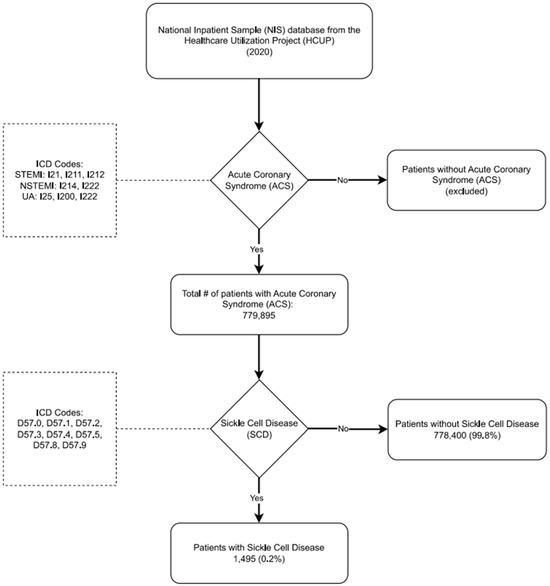
Figure 1.
Flowchart of Population Selection and Analysis for Sickle Cell Disease Patients with Acute Coronary Syndrome (ACS) and Their PCI Outcomes.
2.2. Data Source and Sample
For data analysis, we utilized the National Inpatient Sample (NIS), a comprehensive repository that contains discharge data from a 20% stratified sample of hospitalizations in the United States. It is principled upon a complex sampling design and acquiring national estimates necessitates clustering at hospitals and the stratification of sampled data as well as developments in sampling over time. The NIS uses the tenth revision of the International Classification of Diseases (ICD10-CM) for diagnosis codes. The inclusion criteria for this study were those patients in the NIS2020 database who had an admitting primary diagnosis of ACS (including STEMI, NSTEMI, and UA), during 2020, based on ICD10-CM codes. Patients under 18 years of age were excluded. Furthermore, patients admitted with other primary diagnoses were also excluded from this study. Supplemental Table S1 includes all ICD-10 codes. The NIS database does not allow for further stratification of diagnoses based on severity, procurement of lab values, or imaging of individual patients, nor does it allow for the documentation of causes or etiologies of certain diagnoses. Further limitations of our dataset are outlined in our Section 5.
2.3. Variables of Interest and Study Outcomes
The primary outcomes of our study included in-hospital all-cause mortality, length of stay, total hospital charges, and complications in patients with ACS such as acute heart failure, atrial fibrillation, acute kidney injury, and coronary dissection. We compared these outcomes between two cohorts: patients admitted with ACS and a diagnosis of sickle cell disease (SCD) and patients admitted with ACS without SCD. There was a myriad of potential confounding variables which had to be adjusted for in our study. These confounders encompassed a broad range of factors including patient age, gender, race, socioeconomic status, and medical comorbidities; hospital location and size, and primary expected payer. By adjusting for these confounding variables, we aimed to elucidate the impact of SCD on clinical outcomes and healthcare utilization patterns of patients experiencing ACS. This approach allowed for a nuanced understanding of the interplay between SCD and ACS.
2.4. Statistical Analysis
In adherence to the Healthcare Cost and Utilization Project data use agreement, we refrained from reporting variables with a limited number of observations (≤10) to mitigate potential risks of patient identification or data privacy infringement. Statistical analyses were conducted using STATA version 17.0 software (StataCorp., College Station, TX, USA). Data were represented as percentages for categorical variables and as means ± standard deviations (SDs) for continuous variables. Comparison of continuous variables was performed using Student’s t-test, while categorical variables were compared using the chi-square test, providing insights into both the associations and disparities within our dataset. Univariate regression analysis was employed to compute unadjusted odds ratios for primary and secondary outcomes, providing initial insights into the associations between variables of interest. To adjust for potential confounding factors, multivariable regression analysis was conducted to calculate adjusted odds ratios (aORs). For binary outcomes, a logistic regression model was utilized, whereas linear regression was employed for continuous outcomes, allowing for a comprehensive analysis of both categorical and continuous variables associated with the outcome of interest. Model construction involved the inclusion of variables associated with the outcome of interest in univariable regression analysis, with a significance threshold set at p = 0.02. All p values were two-sided, with statistical significance defined at p < 0.05.
3. Results
3.1. Demographic Data
In this study, we examined a total of 779,895 patients admitted for acute coronary syndrome (ACS). Among them, 520,530 had STEMI (690 in the SCD group) and 259,365 had NSTEMI/unstable angina (805 in the SCD group). Among these ACS patients, 1495 had a confirmed diagnosis of sickle cell disease (SCD). The average age among SCD patients was 59 years, contrasting with the mean age of 66 years in the non-SCD group. Among the SCD patients, 53% were female, while this percentage was 35% among non-SCD patients.
Within the SCD patient subset, 91% self-identified as African Americans, in contrast to the non-SCD group, where the percentages were 74% Caucasian, 11% African American, 9% Hispanic, 3% Asian and/or Pacific Islander, 0.5% Native American, and 3% belonging to other races.
Further investigation into the SCD patient subset revealed the highest localization of hospital region belonging to the south (76% vs. 4%, p < 0.003) compared to that of the northeast, midwest, or west.
Furthermore, patients with SCD had a higher Charlson comorbidity index and a higher likelihood of substance abuse issues (15% vs. 3%, p < 0.001), hypertension (73% vs. 42%, p < 0.001), and chronic lung disease (35% vs. 21%, p < 0.001) compared to non-SCD patients. The comparative demographic data for ACS patients with and without SCD can be observed in Table 1.

Table 1.
Demographic data of patients admitted with acute coronary syndrome (ACS) with and without comorbid sickle cell disease (SCD). p-value ≤ 0.05 indicates significance.
3.2. Inpatient Mortality, Length of Stay, Hospitalization Cost, and Time to PCI for ACS Patients with Concomitant SCD
Our study demonstrated findings regarding inpatient outcomes for SCD patients admitted with ACS. For SCD patients diagnosed with ACS, the odds of inpatient mortality risk were not statistically significant. Length of stay in SCD patients with STEMI or NSTEMI/UA was found to be significant, with an average mean difference of 0.49 days and 0.55 days (p = 0.003), respectively. Neither time from admission to PCI nor hospitalization charges were found to be statistically significant between SCD patients with STEMI and NSTEMI/UA. Table 2 shows inpatient outcomes for patient admitted with STEMI or NSTEMI/UA with comorbid sickle cell disease that were determined through a logistic regression model and adjusted for other predictor variables including age, gender, race, hospital region, and Charlson comorbidity index (CCI).

Table 2.
Logistic regression of inpatient outcomes adjusted for covariates in patients admitted with STEMI, NSTEMI, and UA with comorbid sickle cell disease. p-value ≤ 0.05 indicates significance. Adjusted covariates: age, gender, race, hospital region, and Charlson comorbidity index (CCI).
3.3. PCI Complications in SCD Patients
We tasked the NIS 2020 dataset to ascertain all those patients with ACS undergoing PCI and then further stratified based on the presence or absence of sickle cell disease. The odds of having coronary dissection in SCD patients with ACS were higher compared to non-SCD patients with ACS (aOR: 14.13, CI: 1.73–115.1, p = 0.01). Among SCD patients admitted for ACS who underwent PCI, there was an elevated, yet not significant, risk of atrial fibrillation (aOR 3.07, CI: 0.67–14.1, p = 0.15)) and acute heart failure (aOR 2.05, CI: 0.65–6.48, p = 0.35). Table 3 shows PCI complications among sickle cell patients with adjusted covariates including age, gender, race, hospital, and Charlson comorbidity index (CCI).

Table 3.
Percutaneous coronary intervention (PCI) complications among patients with sickle cell disease. p-value ≤ 0.05 indicates significance. Adjusted covariates: age, gender, race, hospital region, and Charlson comorbidity index (CCI).
4. Discussion
When examining the impacts of sickle cell disease on ACS, our study yielded several significant findings. Firstly, our study reaffirmed the association between the sickle cell population, with higher prevalences of hypertension, drug abuse, and chronic lung diseases. Secondly, among sickle cell patients admitted with ACS, there was a statistically significant decrease in the length of hospital stay, but no significant difference in mortality. Lastly, we found that while sickle cell patients undergoing PCI for STEMI had similar rates of atrial fibrillation, acute heart failure, and acute kidney injury, they had a statistically significant higher rate of coronary artery dissections. For providers caring for this population, these findings provide valuable insight into the clinical characteristics and outcomes of SCD patients with ACS.
The increase in hypertension in SCD patients admitted with ACS is likely due to the acidotic and hyperosmolar environment of renal inner medullary nephrons increasing the risk of polymerization of HbS [9,10,11]. This initiates a cascade of events that leads to microinfarctions in the nephron. Hemolysis and oxidative stress damage further cause chronic tubular damage, leading to tubular dysfunction. This ultimately causes sickle cell nephropathy to activate the renin–angiotensin–aldosterone system (RAAS). The perpetual activation of RAAS likely contributes to a higher prevalence of hypertension and chronic renal disease in these patients [11,12]. In our study, a greater proportion of patients with SCD and ACS had chronic lung disease and pulmonary hypertension. SCD patients are at risk of acute chest syndrome. Repetitive episodes of acute chest syndrome in SCD patients lead to sickle cell chronic lung disease, a form of restrictive lung disease [13]. Additionally, our study identified a noteworthy association between SCD patients admitted with ACS and drug abuse. Clinicians often use opioids to treat chronic complications of vaso-occlusive crises, such as avascular necrosis, which could contribute to the higher prevalence of drug abuse in SCD patients [14]. Previous research has also linked SCD to a higher risk of alcohol use disorder. Furthermore, because of the greater accessibility and accompanying low cost of alcohol compared to opioids, alcohol may be rendered as a more appealing coping strategy for pain than seeking medical treatment [15]. Lower socioeconomic class may be another contributing factor as patients that suffer from sickle cell disease are more likely to be in this demographic. As SCD was initially an evolutionary way of fighting malaria, those with African origins are more likely to have the disease. Moreover, per the US Poverty Statistics, it is estimated that 17.1% of those of African American descent were living in poverty compared to the 11.5% national average. In one article, Lewis et. al. states “Lower SES (socioeconomic status) is associated with increased alcohol, cigarette, and cocaine use among teenagers and showed a higher probability of use disorders in early adulthood”. Low SES has been associated with a worse prognosis as its impact is multifactorial and directly hinders access to nutrition and healthcare [16].
Our findings indicate no difference in the prevalence of atrial fibrillation (AF) or heart failure in SCD patients admitted for ACS. Atrial fibrillation among patients hospitalized with SCD has been previously documented [17]. It has been theorized that cardiac arrhythmias may have a greater incidence in SCD patients due to an affinity to autonomic cardiac dysfunction and myocardial fibrosis, with factors such as aging increasing the risk [17,18]. Additionally, the incidence of heart failure among SCD patients has been documented as chronic anemia from SCD leads to cardiac chamber dilation, an increase in left ventricular mass, and eventual left ventricular diastolic dysfunction [19].
It is also noteworthy to mention that patients diagnosed with sickle cell disease (SCD) experienced a significantly reduced hospitalization period subsequent to an acute coronary syndrome (ACS) episode in contrast to patients without SCD. This disparity in hospital stay duration may primarily stem from the potentially younger age of these individuals.
An interesting finding in our study was the increased risk of coronary artery dissections in those patients with SCD undergoing PCI. It is important to note that the NIS database lists coronary dissection as a procedure diagnosis, rather than a complication of PCI itself and thus it is one of the limitations of this study that we are unable to pinpoint the etiology or type of dissection. Another important thing to note is the fact that being a young female by itself puts patients at risk of developing spontaneous coronary artery dissection [20]. Both of these should be kept in mind as we move forward in the discussion of these results; however, we did in fact adjust for age and gender in our adjusted odds ratios. One proposed theory for why sickle cell patients may be more likely to develop coronary dissection lies in the increasing evidence of arterial ectasias of the coronaries of sickle cell patients. As one review by Danhan states, “coronary artery ectasia is very common in sickle cell disease with an incidence of 17.7%”. The review continues to state that the likely cause for this notable figure is the pro-inflammatory state that is present in sickle cell disease patients [21,22]. SCD patients have chronically elevated pro-inflammatory markers contributing to vascular inflammation. The accelerated hemolysis in SCD leads to an increased circulation of immature red blood cells (RBCs) that have increased expression of adhesion receptors compared to mature RBCs [22]. As per Correia Rodrigues et. al., the vasculopathy associated with sickle cell is likely the result of chronic adhesion and shearing of abnormal hemoglobin, which leads to vascular remodeling, pathologic thickening, and arterial tortuosity [23]. These further contribute to the multifactorial mechanism, causing higher rates of coronary artery dissection in those with sickle cell disease. In reviewing the current medical literature, there have been studies on sickle cell disease and acute coronary syndrome; however, our study answers a curiosity about the impact sickle cell disease has on the lengths of stay, complications, and post-PCI outcomes in those with ACS. The findings of our study show a need for continued research in this field as there is a paucity as of now.
The microvascular nature of vascular disease in sickle cell disease (SCD) patients can lead to worse outcomes in patients undergoing percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS). Chronic hemolytic anemia and recurrent vaso-occlusive crises in SCD result in widespread vasculopathy and multi-organ damage. This can manifest as low cardiac output due to chronic anemia and cardiomyopathy, increased risk of multiple organ failure from microvascular ischemia, higher susceptibility to infections like pneumonia due to functional asplenia, respiratory failure from acute chest syndrome or pulmonary hypertension, and acute kidney injury necessitating hemodialysis. Furthermore, SCD patients often require blood transfusions during acute crises, which can lead to iron overload and associated complications [24].
Iron overload remains a pressing clinical issue for SCD patients. In fact, a post-mortem study conducted by Porter and Garbowski identified the presence of iron overload in one-third of 141 adult SCD patients and in 7% of these cases, iron overload was linked to the cause of death. The pathology of iron overload has been associated with oxidative stress attributed to rises in plasma malondialdehyde and nitrate, both of which can impair the glutathione system [25].
5. Limitation
One possible limitation of this study is related to coding and documentation errors inherent in administrative databases, which could have led to the inadvertent exclusion of patients who should have been included in our data analysis from the utilized database. Another limitation pertains to the incompleteness of patient-specific characteristics, such as individual laboratory results, imaging findings, medications, and social history. Using the NIS database, we are unfortunately unable to stratify patients based on the severity of their diagnosis or laboratory values. Additionally, the dataset available to us only covered the year 2020, limiting our study to short-term outcomes (<1 year). Furthermore, our data were limited in that we could not ascertain the etiologies of certain diagnoses.
Furthermore, the multivariate regression models utilized in this study may have been impacted by multicollinearity or influenced by one of the included covariates, potentially affecting the robustness of our findings.
Despite these limitations, we benefit from a large sample size, which provides our study with good statistical power, allowing for the generalization of our findings to a broader population. However, it is essential to acknowledge that, despite efforts to minimize potential confounders outlined in the Section 2, unaccounted for variables may still impact the findings. Moreover, akin to any observational study, this investigation was susceptible to selection bias and unmeasured biases. Although we endeavored to address allocation bias through multivariable analysis, the possibility of biases cannot be entirely eliminated.
6. Conclusions
In conclusion, our study contributes valuable insight into the clinical characteristics and outcomes of patients admitted for ACS with a diagnosis of SCD. Patients with SCD and ACS were found to have a higher prevalence of coronary dissection, while decreased lengths of stay had no accompanying significant difference in mortality. It reaffirmed known correlations, including those of socioeconomic status, race, and gender, in those with sickle cell disease. Our study also further reinforced the link between the sickle cell population and the increased prevalence of hypertension, drug abuse, and chronic lung diseases. With disease processes as ubiquitous as sickle cell and acute coronary syndrome, further research should be conducted to better understand the impact of this interplay. This is further underscored by the incidence of sickle cell disease continuing to increase. Despite advancements in care aiming to decrease mortality among SCD patients, there has been a notable rise in vaso-occlusive events as patients age, which have a pronounced impact on the cardiovascular system. Additional investigations of this interplay could provide valuable insights into the progression, treatment, and management of SCD.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/hearts5020016/s1, Table S1: Clinical Modification (ICD-10-CM) Coding System Utilized During Data Analysis.
Author Contributions
A.A. (Abdulmajeed Alharbi), C.P., M.M., C.S., M.B., M.C., A.A. (Ahmad Abdulrahman), H.A., E.S.K., M.S. and R.A. conceived and designed the study, drafted the manuscript, and critically revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was deemed exempt by the Institutional Review Board of the University of Toledo as it de-identified patient information.
Informed Consent Statement
Patient consent was waived by the Institutional Review Board of the University of Toledo as this was a database-based study that included de-identified patient information.
Data Availability Statement
The data presented in this study are available in this article (and Supplementary Material).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Piel, F.B.; Steinberg, M.H.; Rees, D.C. Sickle Cell Disease. N. Engl. J. Med. 2017, 376, 1561–1573. Available online: https://www.nejm.org/doi/10.1056/NEJMra1510865 (accessed on 1 February 2024). [CrossRef] [PubMed]
- Sedrak, A.; Kondamudi, N.P. Sickle Cell Disease. In Pediatric Surgery: Diagnosis and Treatment; 2022; pp. 653–663. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482384/ (accessed on 1 February 2024).
- Rivers, A.; Jagadeeswaran, R.; Lavelle, D. Potential role of LSD1 inhibitors in the treatment of sickle cell disease: A review of preclinical animal model data. Am. J. Physiol.—Regul. Integr. Comp. Physiol. 2018, 315, R840–R847. [Google Scholar] [CrossRef] [PubMed]
- Sachdev, V.; Hsieh, M.; Jeffries, N.; Noreuil, A.; Li, W.; Sidenko, S.; Hannoush, H.; Limerick, E.; Wilson, D.; Tisdale, J.; et al. Reversal of a rheologic cardiomyopathy following hematopoietic stem cell transplantation for sickle cell disease. Blood Adv. 2019, 3, 2816–2824. [Google Scholar] [CrossRef] [PubMed]
- Farmakis, D.; Triposkiadis, F.; Lekakis, J.; Parissis, J. Heart failure in haemoglobinopathies: Pathophysiology, clinical phenotypes, and management. Eur. J. Heart Fail. 2017, 19, 479–489. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/ejhf.708 (accessed on 1 February 2024). [CrossRef] [PubMed]
- Ogunbayo, G.O.; Misumida, N.; Olorunfemi, O.; Elbadawi, A.; Saheed, D.; Messerli, A.; Elayi, C.S.; Smyth, S.S. Comparison of Outcomes in Patients Having Acute Myocardial Infarction With Versus Without Sickle-Cell Anemia. Am. J. Cardiol. 2017, 120, 1768–1771. [Google Scholar] [CrossRef] [PubMed]
- Manci, E.A.; Culberson, D.E.; Yang, Y.M.; Gardner, T.M.; Powell, R.; Haynes, J.; Shah, A.K.; Mankad, V.N. Causes of death in sickle cell disease: An autopsy study. Br. J. Haematol. 2003, 123, 359–365. Available online: https://onlinelibrary.wiley.com/doi/full/10.1046/j.1365-2141.2003.04594.x (accessed on 1 February 2024). [CrossRef] [PubMed]
- Payne, A.B.; Mehal, J.M.; Chapman, C.; Haberling, D.L.; Richardson, L.C.; Bean, C.J.; Hooper, W.C. Trends in Sickle Cell Disease-Related Mortality in the United States, 1979 to 2017. Ann. Emerg. Med. 2020, 76, S28–S36. Available online: https://pubmed.ncbi.nlm.nih.gov/32928459/ (accessed on 1 February 2024). [CrossRef]
- Statistical Software for Data Science|Stata. Available online: https://www.stata.com/ (accessed on 1 February 2024).
- Hassell, K.L. Population estimates of sickle cell disease in the U.S. Am. J. Prev. Med. 2010, 38 (Suppl. S4), S512–S521. Available online: https://pubmed.ncbi.nlm.nih.gov/20331952/ (accessed on 1 February 2024). [CrossRef] [PubMed]
- De Jong, P.E.; Van Eps, L.W.S. Sickle cell nephropathy: New insights into its pathophysiology. Kidney Int. 1985, 27, 711–717. [Google Scholar] [CrossRef] [PubMed]
- Ataga, K.I.; Saraf, S.L.; Derebail, V.K. The nephropathy of sickle cell trait and sickle cell disease. Nat. Rev. Nephrol. 2022, 18, 361–377. Available online: https://pubmed.ncbi.nlm.nih.gov/35190716/ (accessed on 1 February 2024). [CrossRef] [PubMed]
- Miller, A.C.; Gladwin, M.T. Pulmonary complications of sickle cell disease. Am. J. Respir. Crit. Care Med. 2012, 185, 1154–1165. Available online: https://pubmed.ncbi.nlm.nih.gov/22447965/ (accessed on 1 February 2024). [CrossRef] [PubMed]
- Kotila, T.R.; Busari, O.E.; Makanjuola, V.; Eyelade, O.R. Addiction or Pseudoaddiction in Sickle Cell Disease Patients: Time to Decide—A Case Series. Ann. Ib. Postgrad. Med. 2015, 13, 44–47. [Google Scholar] [PubMed] [PubMed Central]
- Bruton, S.J.; Nouraie, M.; Scott, D.M.; Gilmore, T.; Taylor, R.E. The Prevalence of Mood and Alcohol Related Disorders within the Adult Sickle Cell Disease Population and Their Impact on Healthcare Utilization. Blood 2015, 126, 2063. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.; Hoffman, L.; Garcia, C.C.; Nixon, S.J. Race and socioeconomic status in substance use progression and treatment entry. J. Ethn. Subst. Abuse 2018, 17, 150–166. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Desai, A.A.; Patel, A.R.; Ahmad, H.; Groth, J.V.; Thiruvoipati, T.; Turner, K.; Yodwut, C.; Czobor, P.; Artz, N.; MacHado, R.F.; et al. Mechanistic insights and characterization of sickle cell disease-associated cardiomyopathy. Circ. Cardiovasc. Imaging 2014, 7, 430–437. Available online: https://pubmed.ncbi.nlm.nih.gov/24676783/ (accessed on 1 February 2024). [CrossRef] [PubMed]
- Indik, J.H.; Nair, V.; Rafikov, R.; Nyotowidjojo, I.S.; Bisla, J.; Kansal, M.; Parikh, D.S.; Robinson, M.; Desai, A.; Oberoi, M.; et al. Associations of Prolonged QTc in Sickle Cell Disease. PLoS ONE 2016, 11, e0164526. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0164526 (accessed on 1 February 2024). [CrossRef] [PubMed]
- Gladwin, M.T. Cardiovascular complications and risk of death in sickle-cell disease. Lancet 2016, 387, 2565–2574. Available online: http://www.thelancet.com/article/S0140673616006474/fulltext (accessed on 1 February 2024). [CrossRef] [PubMed]
- Avula, V.; Karacsonyi, J.; Kostantinis, S.; Simsek, B.; Rangan, B.V.; Gutierrez, A.A.; Burke, M.N.; Garcia, S.; Mooney, M.; Sorajja, P.; et al. Incidence, Treatment, and Outcomes of Coronary Artery Perforation During Percutaneous Coronary Intervention. J. Invasive Cardiol. 2022, 34, E499–E504. [Google Scholar] [PubMed]
- Nicholson, G.T.; Hsu, D.T.; Colan, S.D.; Manwani, D.; Burton, W.B.; Fountain, D.; Lopez, L. Coronary Artery Dilation in Sickle Cell Disease. J. Pediatr. 2011, 159, 789–794.e2. [Google Scholar] [CrossRef]
- Dahhan, A. Coronary artery ectasia in atherosclerotic coronary artery disease, inflammatory disorders, and sickle cell disease. Cardiovasc. Ther. 2015, 33, 79–88. Available online: https://pubmed.ncbi.nlm.nih.gov/25677643/ (accessed on 1 February 2024). [CrossRef] [PubMed]
- Correia Rodrigues, C.; Parreira, S.; Soares, F.; Dias, M.C.; Canhão, P. Cervical dissection in a patient with sickle cell disease. Acta Neurol. Belg. 2024, 124, 287–289. [Google Scholar] [CrossRef] [PubMed]
- Sachdev, V.; Rosing, D.R.; Thein, S.L. Cardiovascular complications of sickle cell disease. Trends Cardiovasc. Med. 2021, 31, 187–193. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Porter, J.; Garbowski, M. Consequences and management of iron overload in sickle cell disease. Hematol. Am. Soc. Hematol. Educ. Program 2013, 2013, 447–456. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).