Abstract
Balance is an important component of daily function and impairments can lead to injury and quality-of-life limitations. Balance is not well studied in the burn population. This study examines the frequency of long-term balance impairments and associated factors after a burn injury. The Burn Model System National Database was analyzed. Trouble with balance was self-reported at discharge, 6, 12, 24, and 60 months after injury. Regression analyses examined the associations between demographic and clinical characteristics and balance impairments at 12 months. Of 572 participants, balance impairments were most reported at discharge (40.3%), continuing over 60 months (26.8–36.0%). Those reporting balance impairments (n = 153) were more likely to be older, unemployed, have Medicaid or Medicare, receive inpatient rehabilitation, receive outpatient physical or occupational therapy, have vision problems, have leg or feet burns and swelling, and have foot numbness compared to those without (p ≤ 0.001). Regression analysis demonstrated a 4% increased odds of balance impairment for every increase in year of age (p < 0.001), 71% lower odds if employed at time of injury (p < 0.001), and 140% higher odds if receiving outpatient physical or occupational therapy at 12 months (p = 0.008). Common reports of balance impairments highlight the need for routine screenings to identify burn survivors that may benefit from targeted interventions.
1. Introduction
The word “balance” in English comes from the Latin word (libra) bilanx that means two (bi-) scale pans (-lanx) [1], connecting to the idea of a scale or balance. Balance is a key part of our health, longevity, and performance in activities of daily living [2,3]. Balance involves many intrinsic and extrinsic factors and is affected by various systems in the body including visual, vestibular, proprioception, somatosensory, and auditory [4,5]. Declines in balance occur with aging-related changes, leading to potential falls and injury [2,3]. In addition, there are many factors that can make an individual susceptible to falls such as other chronic conditions, polypharmacy, socioeconomic status, environmental risks (poor footwear, tripping hazards, lack of handrails, poor lighting within or outside their home, living alone), and poor safety and accessibility [6,7,8,9,10]. Among older adults, falls are often responsible for injuries and are a marker of disease severity [11].
Over the last 30 years, burn injury survival rates have continued to improve due to advancements in the standards of care [12]. However, individuals living with a burn injury continue to face a myriad of physical and psychosocial challenges years after injury [13]. Of these challenges, trouble with balance was reported two years after injury in approximately one-quarter of participants in a longitudinal study of burn outcomes [14]. Various burn injury sequelae may contribute to impaired balance, including altered sensory perception [15], debilitation, contractures, nutritional deficiencies, pain, and neuropathies [16]. Preexisting factors may also contribute to balance impairment and fall risk such as vestibular problems, joint or muscle problems, low vision or vision impairment, muscle mass loss, low blood pressure, and other comorbidities (such as diabetes, heart disease, stroke, Parkinson’s, thyroid problems, and other neurological conditions) [17,18,19,20,21].
While previous literature has examined interventions for balance performance and control [22,23] the prevalence of balance impairment and associated risk factors in the burn population is underexplored in the literature [16]. Therefore, the purpose of this study is to describe the frequency in which burn survivors report balance impairments long term and determine the associated risk factors.
2. Materials and Methods
2.1. Burn Model System National Database
This study used data from the Burn Model System (BMS) National Database, funded by the National Institute on Disability, Independent Living, and Rehabilitation Research. This study was approved by the Mass General Brigham Institutional Review Board (#2011P001264) as part of the overarching BMS program. The BMS Database was established in 1994 as a means of exploring the long-term sociodemographic, clinical, and patient reported outcomes of data of burn survivors. Written informed consent was obtained from all participants and the Institutional Review Board at each BMS site oversaw data collection [24]. Data were requested from the BMS National Data and Statistical Center through their standard operating procedure: (https://burndata.washington.edu/sites/burndata/files/files/602BMS_InternalNotificationSOP_2024-2-28.pdf) (accessed on 1 December 2022). Participants who had a burn injury between 1 August 2015 and 30 January 2023, who speak and understand English and/or Spanish, and were consented and alive at discharge were included in this study. During the study period, the following four sites were included: Boston-Harvard Burn Injury Model System (BH-BIMS), Boston, MA, USA; North Texas Burn Rehabilitation Model System, Dallas, TX, USA; Northwest Regional Burn Model System, Seattle, WA, USA; and the Pediatric Burn Injury Rehabilitation Model System, Galveston, TX, USA. Database eligibility included adults with a burn injury that required autografting or amputation surgery for wound closure and met one of the following criteria: (1) 18–64 years of age with a burn injury ≥ 20% total body surface area (TBSA); (2) ≥65 years of age with a burn injury ≥ 10% TBSA; (3) any age with a burn injury to their critical areas including face/neck, hands, or feet; and (4) any age with a high-voltage electrical burn injury. BMS Database enrollment criteria have been modified over time and the data sets generated during and/or analyzed during the current study are publicly available upon request from the BMS National Data and Statistical Center’s website: https://burndata.washington.edu (accessed on 30 January 2023) [24].
2.2. Demographic and Clinical Characteristics
Demographic and clinical variables were obtained through self-report or medical record abstraction. The following demographic variables were examined: age, sex, highest level of education, ethnicity, race, employment status, and insurance type. Clinical variables collected were BMS site (intentionally deidentified), burn etiology, lower extremity amputation (Y/N), alcohol and drug misuse (both variables from the Cut down, Annoyed, Guilty, and Eye-opener (CAGE) Scale; the CAGE Scale is considered positive if the score is greater than or equal to 2; preinjury recall collected at discharge) [25], documented range of motion deficits (Y/N), inpatient rehabilitation stay (Y/N), multiple trips to the operating room (≥2; Y/N), burn location (feet/legs; head/neck/face), vision problems (Y/N), numbness in feet (Y/N), swollen feet or legs (Y/N), comorbidities (diabetes, stroke, Parkinson’s disease, spinal cord injury, and traumatic brain injury; Y/N), burn size (percent TBSA), body mass index (BMI), prescription pain medication use (Y/N), and outpatient physical or occupational therapy received (Y/N). All the demographic and clinical variables were collected at discharge, except for outpatient therapy and prescription pain medication use, which were both collected at the 12-month follow-up.
2.3. Primary Outcomes
The primary outcome was the item, “Trouble with your balance?” (yes/no) in the Adult Review of Systems section of the BMS follow-up questionnaire at the 12-month timepoint. This item is also collected at discharge and at 6, 24, and 60 months after a burn injury. The 12-month timepoint was chosen a priori by the authors because long-term balance outcomes are more visible. Additionally, this timepoint ensured a more robust sample size given documented higher participant attrition rates at more distal timepoints [26].
2.4. Data Analysis
For purposes of analysis, the study population was divided into the following two groups: those with and those without self-reported balance impairments at 12 months. Differences in demographic and clinical variables between groups were tested using nonparametric tests (Wilcoxon–Mann–Whitney) due to the nonnormality of the data for continuous variables and chi-square tests for Fisher’s exact for categorical variables. A p-value less than 0.002 was considered significant, using the Bonferroni method to adjust for multiple comparisons.
The number of participants who reported balance impairments at discharge and all follow-up timepoints were analyzed. Additionally, the frequency of balance impairments at discharge and follow-up (6, 12, 24, and 60 months) among those with repeated measures was examined. For these repeated measures analyses, pairwise deletion was used for those with missing data on any timepoint. Balance impairments were also assessed by age category (18–30, 31–40, 41–50, etc.). Statistically significant differences in the frequency of balance impairments by age categories were assessed using an omnibus chi-square statistical test.
Logistic regressions were used to examine the association between demographic and clinical characteristics and self-reported balance impairments (1 = yes, 0 = no) at 12 months postinjury. The dependent variables included age, sex, BMS site, BMI, lower limb amputation, employment at the time of injury, inpatient rehabilitation stay, multiple trips to the operating room, education (greater than high school vs. high school and less), alcohol and drug misuse, and therapy services. Additional considered variables were not included in the models due to missing data (detailed in the Results Section). All included variables were collected at discharge with the exception of therapy services (12 months). A p-value less than 0.05 was considered significant. Robust standard errors accounted for heteroskedasticity; interactions were examined, and model fit was checked. Additionally, an exploratory regression analysis examined demographic and clinical variables associated with improvement in self-reported balance from discharge to 12 months. Stata 15.1 was used for all analyses [27].
3. Results
3.1. Descriptive Analysis
A total of 572 BMS Database participants met the inclusion criteria for this study, with 153 reporting trouble with balance and 419 reporting no trouble with balance at 12 months after injury (Table 1).

Table 1.
Comparison of populations with and without balance impairments at 12 months (n = 572).
Compared to those without balance impairments, the balance impairment group was older (median 53.3 (interquartile range: 42.1, 63.4) vs. 44.7 (31.1, 57.0), p < 0.001), less likely to be employed at the time of injury (49.0% vs. 74.2%, p < 0.001), and more likely to have Medicaid/Medicare insurance (22.7%/31.3% versus 12.7%/15.1%, p < 0.001), an inpatient rehabilitation stay (34.7% vs. 21.3%, p = 0.001), outpatient physical or occupational therapy (41.7% vs. 23.7%, p < 0.001), vision problems (26.2% vs. 7.0%; p < 0.001), leg or feet burns (79.8% vs. 62.1%; p < 0.001), numbness in their feet (55.7% vs. 16.8%, p < 0.001), and swollen feet or legs (46.3% vs. 14.9%, p < 0.001).
The variables not statistically different between groups were sex, education, ethnicity, race, BMS site, burn etiology, lower extremity amputation, alcohol misuse, drug misuse, range of motion deficit, multiple trips to the operating room, head/neck/face burn, TBSA, and BMI.
The following variables had significant missing data (61–89%) and, therefore, were not included in the analysis: prescription pain medication use at 12 months and comorbidities at discharge (diabetes, stroke, Parkinson’s, spinal cord injury, traumatic brain injury). These variables were missing data due to the timeframe of data collection (i.e., item collection began after 2015) or missing data in the medical record at follow-up timepoints.
3.2. Primary Outcomes over Time
Balance impairments were most frequently reported at discharge (40.3%) and ranged from 26.8% to 36.0% over the five-year follow-up period after injury (Table 2). It is important to note that this data in Table 2 is cross-sectional leading to different sample sizes at each timepoint and excludes participants whose windows for data collection were not yet open (e.g., the five-year datapoint excludes participants with a burn injury after 2019).

Table 2.
Frequency of balance impairments at up to five years after a burn injury.
The frequency of trouble with balance for participants with repeated measures was examined at discharge and all follow-up timepoints (Table 3). In all groups with repeated balance measures, a similar percentage of participants reported impairments of balance at discharge (40.0–51.8%) and at least one timepoint for follow-up (26.3–35.2%).

Table 3.
Frequency of balance impairments at discharge and each follow-up timepoint for participants with repeated measures.
3.3. Association between Age and Self-Reported Balance Impairments
An examination of the relationship between self-reported balance impairments and age demonstrated that trouble with balance was increasingly common with older age (p < 0.001; Figure 1).
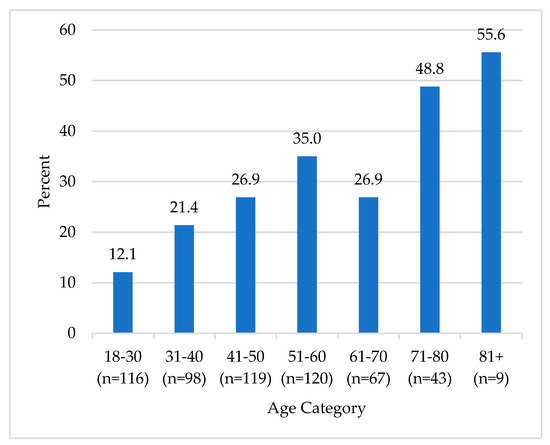
Figure 1.
Histogram of the association between age and self–reported balance impairments. Differences were examined using the omnibus (chi-square) test, p < 0.001.
3.4. Regression Analysis
Logistic regression analysis examined the association between self-reported trouble with balance at 12 months and demographic and clinical factors (Table 4).

Table 4.
Logistic regression analysis examining the association between demographic and clinical characteristics and self-reported balance impairments at 12 months.
For every increase in one year of age, there is a 4% increased odds of a balance impairment (p < 0.001). Participants who were employed at the time of injury had a 71% lower odds of reporting a balance impairment (p < 0.001). Trouble with balance was 140% higher for participants who received outpatient physical or occupational therapy at 12 months (p = 0.008). Interaction between inpatient rehabilitation and outpatient physical or occupational therapy services was not significant.
An exploratory regression analysis examined the associations with improvement in balance and demonstrated that employment prior to a burn injury is associated with a 617% higher odds of improved balance from discharge to 12 months (p = 0.001) compared to those not employed prior to injury. Participants who received outpatient physical or occupational therapy services at 12 months exhibited a 72% lower odds of reporting balance improvement from discharge to 12 months (p = 0.017).
4. Discussion
The frequency of balance impairments and its association with clinical and demo-graphic variables has been underexplored in the burn population; thus, this study helps inform an important gap in the existing literature. This study found that balance impairments are commonly reported at discharge (40.3%) and can persist for up to five years after injury (26.8–36.0%). Those with balance impairments were more likely to be older, unemployed, have Medicaid or Medicare, receive inpatient rehabilitation, receive outpatient physical or occupational therapy, have vision problems, have leg or feet burns and swelling, and have foot numbness compared to those without balance impairments. The regression analysis demonstrated that balance impairments are more likely in people living with a burn injury who are older, were unemployed at the time of injury, and received outpatient physical or occupational therapy.
Consistent with the general balance literature, balance impairments in people living with a burn injury are more common with older age. A prior study demonstrated a significant association between age and balance disorders with the prevalence of balance impairments increasing with age [28]. Trouble with balance is common in the US elderly population, with 34% of elderly individuals reporting a decline in balance and 23% reporting a fall in the prior 12 months [29]. Using an epidemiologic study of self-reported balance disorders in US adults as a comparison, this study found higher percentages of burn survivors reporting balance impairments across all similar age categories [30]. Due to the elderly being the fastest growing portion of the global population [31] and burn survivors living longer due to advancements in care [32], age is a key factor to consider when planning prevention measures for elderly individuals living with a burn injury. Additionally, various environmental factors, which are not contained in the BMS database, may influence elderly individuals’ fall risk, including availability of supportive and accessible living facilities, adaptive equipment, and social support resources. Many of these environmental supports come at a financial cost to the individual, highlighting societal inequities to environmental supports [33].
There is some evidence from this study that unemployment prior to injury could be associated with balance impairments after a burn. This is crucial because employment is identified as a social determinant of health and unemployment is historically tied to poorer health outcomes [34,35]. Full-time employment has predicted significantly slower declines in perceived health and physical functioning, compared to unemployment [36]. Specifically in women, employment is associated with a reduced likelihood of physical function impairments [37]; those who work part time or are unemployed are more likely to experience a physical impairment [37]. Also, there is an association between time spent not working and a likelihood of experiencing a severe physical functional impairment [37]. Additionally, employment confers a protective effect on hospitalization in older adults over their lifetime; in contrast, having an illness or disability is a predictor of hospitalization later in life [38]. In burns, return to work is an important milestone for survivors. The relationship between preburn and postburn employment and postburn balance is complex and the directional relationship over time is hard to interpret. With that in mind, some studies have found that being employed preinjury is highly associated with being employed postinjury [39,40] and that unemployment has been tied to poorer health outcomes [41]. It is worth noting that not-working retired individuals are more likely to be older and therefore also have worse balance due to their age.
In this study, receiving outpatient physical or occupational therapy is associated with balance impairments after a burn injury. Both physical and occupational therapies have been found to be beneficial in improving balance functionality [42]. This is important because individuals who received therapy services for trouble with balance are likely to require these services to help manage their functional deficits. In a study with elderly individuals with fall risk, those who received a combination of rehabilitation services at home (such as physical, occupational, speech therapies, or nursing interventions) were found to have an overall positive change in gait and balance, compared to just physical therapy alone [43]. In another study of elderly over 75 years of age with trouble with balance, individuals who received a physical therapy intervention had a greater improvement in balance at one month compared to a control group; however, the effect was not detected at one-year follow-up [44]. These prior works suggest that individuals living with chronic conditions that affect balance may benefit from long-term outpatient therapy services.
Limitations
There were several limitations to this study. Some clinical factors that may contribute to balance impairments are not collected as part of the BMS database, including escharotomy, fasciotomy, reasons for ongoing physical and occupational therapy, and environmental factors (e.g., delays in provision of adaptive aids, equipment, or home modifications delays). The database includes PROMIS Pain Intensity and Interference and collects pain medication use (a lot of missing data) but does not include the cause of ongoing pain or peripheral neuropathies. In addition, prescription pain medication uses at 12 months and comorbidities at discharge (diabetes, stroke, Parkinson’s, spinal cord injury, traumatic brain injury) were not included in the regression analysis due to a substantial amount of missing data. There is increasing missing data at more distal follow-up timepoints. A potential sample bias is that the BMS Database includes participants with more severe burn injuries [45]. Additionally, there is a selection (did not enroll) and survey response bias (failed to respond, unable to locate, preferred to not respond to item). Prior examination of the BMS Database found that participants who were unemployed, did not have private health insurance or workers’ compensation insurance, and had a history of drug abuse exhibited an increased risk of loss to follow-up across two or more timepoints [26]. Also, participants are less likely to respond at their next follow-up timepoint if they missed the previous follow-up [45]. Although the BMS has been found to be limited in its representation of diverse populations [46], nevertheless, the database has been found to be representative of the general US population [45].
5. Conclusions
This study found that balance impairments are common (40.3% at discharge) and can persist for up to five years after injury (36.0% at 60 months). Furthermore, this study examined data up to the five-year follow-up timepoint since this is the specified interval of data collection in the database; however, future studies are needed to examine the presence of balance impairments beyond five years and the contribution of factors not collected in the database such as environmental factors. Additionally, factors such as age, employment status prior to injury, and outpatient therapy services were associated with balance impairments in the burn population. Although not previously well reported in the literature, data from this study found that balance impairments in the burn population are prevalent and this study may inform future use of balance assessments and intervention in follow-up care. Future clinical recommendations should include (1) screening for fall risk during clinical encounters including acute hospitalization, inpatient rehabilitation, and at follow-up burn and primary care appointments; (2) targeted balance therapy for inpatients; and (3) outpatient therapy referrals for individuals with an elevated fall risk. Further research is needed to examine the effectiveness of balance assessment and potential interventions in the burn population.
Author Contributions
Conceptualization, E.S., K.L.C., L.J.S., K.A.M., M.D.S., M.v.d.R., K.J.K., C.M.R. and J.C.S.; Methodology, E.S., K.L.C., L.J.S., K.A.M., M.D.S., M.v.d.R., K.J.K., C.M.R. and J.C.S.; Software, K.A.M.; Formal analysis, K.A.M.; Investigation, E.S., M.D.S., C.M.R. and J.C.S.; Data curation, K.A.M.; Writing—original draft, E.S.; Writing—review & editing, E.S., K.L.C., L.J.S., K.A.M., M.D.S., M.v.d.R., K.J.K., C.M.R. and J.C.S.; Visualization, M.D.S., C.M.R. and J.C.S.; Supervision, C.M.R. and J.C.S.; Project administration C.M.R. and J.C.S.; funding acquisition, C.M.R. and J.C.S. All authors have read and agreed to the published version of the manuscript.
Funding
The contents of this article were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant numbers 90DPBU0008 and 90DPGE0004). The NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this article do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government. Partial support was obtained from Shriners Hospitals for Children (Grant #79136-BOS-23 and 79138-BOS-23).
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Mass General Brigham (protocol code 2011P001264 and 15 June 2015).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The Burn Injury Model System National Database is a prospective, longitudinal, multicenter research data repository that contains measures of functional and psychosocial outcomes following burns. The data are free and publicly available at https://burndata.washington.edu/ (30 January 2023).
Conflicts of Interest
Ryan received financial support from MediWound for contracted research. This funding did not directly or indirectly impact this work. The remaining authors have no relevant financial or nonfinancial interests to disclose.
References
- Oxford Languages. Oxford Dictionaries. Published 2023. Available online: https://languages.oup.com/ (accessed on 1 December 2023).
- Dunsky, A. The Effect of Balance and Coordination Exercises on Quality of Life in Older Adults: A Mini-Review. Front. Aging Neurosci. 2019, 11, 318. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, E.O.; Afilalo, J.; Ensrud, K.E.; Kowal, P.; Onder, G.; Fried, L.P. Frailty: Implications for clinical practice and public health. Lancet 2019, 394, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Peterka, R.J.; Murchison, C.F.; Parrington, L.; Fino, P.C.; King, L.A. Implementation of a Central Sensorimotor Integration Test for Characterization of Human Balance Control During Stance. Front. Neurol. 2018, 9, 1045. [Google Scholar] [CrossRef] [PubMed]
- Rasman, B.G.; Forbes, P.A.; Tisserand, R.; Blouin, J.S. Sensorimotor Manipulations of the Balance Control Loop-Beyond Imposed External Perturbations. Front. Neurol. 2018, 9, 899. [Google Scholar] [CrossRef] [PubMed]
- Ie, K.; Chou, E.; Boyce, R.D.; Albert, S.M. Fall Risk-Increasing Drugs, Polypharmacy, and Falls Among Low-Income Community-Dwelling Older Adults. Innov. Aging 2021, 5, igab001. [Google Scholar] [CrossRef]
- Lee, H.; Lim, J.H. Living Alone, Environmental Hazards, and Falls Among U.S. Older Adults. Innov. Aging 2023, 7, igad055. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Procter-Gray, E.; Lipsitz, L.A.; Leveille, S.G.; Hackman, H.; Biondolillo, M.; Hannan, M.T. Utilitarian walking, neighborhood environment, and risk of outdoor falls among older adults. Am. J. Public Health 2014, 104, e30–e37. [Google Scholar] [CrossRef]
- Jiang, Y.; Xia, Q.; Wang, J.; Zhou, P.; Jiang, S.; Diwan, V.K.; Xv, B. Environmental risk factors associated with falls among older people living in long-term aged care facilities: A prospective study. Lancet 2019, 394, S23. [Google Scholar] [CrossRef]
- World Health Organization; Ageing Life Course Unit. WHO Global Report on Falls Prevention in Older Age; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Cuevas-Trisan, R. Balance Problems and Fall Risks in the Elderly. Phys. Med. Rehabil. Clin. N. Am. 2017, 28, 727–737. [Google Scholar] [CrossRef] [PubMed]
- Capek, K.D.; Sousse, L.E.; Hundeshagen, G.; Voigt, C.D.; Suman, O.E.; Finnerty, C.C.; Jennings, K.; Herndon, D.N. Contemporary Burn Survival. J. Am. Coll. Surg. 2018, 226, 453–463. [Google Scholar] [CrossRef]
- Abouzeid, C.A.; Wolfe, A.E.; Ni, P.; Carrougher, G.J.; Gibran, N.S.; Hammond, F.M.; Holavanahalli, R.; McMullen, K.A.; Roaten, K.; Suman, O.; et al. Are burns a chronic condition? Examining patient reported outcomes up to 20 years after burn injury-A Burn Model System National Database investigation. J. Trauma Acute Care Surg. 2022, 92, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- Kelter, B.M.; Holavanahalli, R.; Suman, O.E.; Ryan, C.M.; Schneider, J.C. Recognizing the long-term sequelae of burns as a chronic medical condition. Burns 2020, 46, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Nedelec, B.; Hou, Q.; Sohbi, I.; Choinière, M.; Beauregard, G.; Dykes, R.W. Sensory perception and neuroanatomical structures in normal and grafted skin of burn survivors. Burns 2005, 31, 817–830. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.C.; Qu, H.D.; Lowry, J.; Walker, J.; Vitale, E.; Zona, M. Efficacy of inpatient burn rehabilitation: A prospective pilot study examining range of motion, hand function and balance. Burn 2012, 38, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Mayo Clinic Staff. Balance Problems—Symptoms and Causes. Mayo Clinic. Published 2018. Available online: https://www.mayoclinic.org/diseases-conditions/balance-problems/symptoms-causes/syc-20350474 (accessed on 1 June 2024).
- National Institute on Aging. Older Adults and Balance Problems. Published 12 September 2022. Available online: https://www.nia.nih.gov/health/falls-and-falls-prevention/older-adults-and-balance-problems#causes (accessed on 1 June 2024).
- National Institute on Deafness Other Communication Disorders Balance Disorders (NIDCD). Published 12 March 2018. Available online: https://www.nidcd.nih.gov/health/balance-disorders (accessed on 1 June 2024).
- American Speech-Language-Hearing Association (n.d.). Balance System Disorders (Practice Portal). Available online: www.asha.org/Practice-Portal/Clinical-Topics/Balance-System-Disorders/ (accessed on 1 June 2024).
- Appeadu, M.; Bordoni, B. Falls and Fall Prevention in the Elderly. PubMed. Published 4 June 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560761/ (accessed on 1 June 2024).
- Othman, E.M.; Toson, R.A. Response of bone mineral density and balance performance in post-burn patients with selected Qigong training: A single-blind randomized controlled trial. Burns 2024, 50, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, Z.M.; Ali, O.I.; Moawd, S.A.; Eid, M.M.; Taha, M.M. Low Vibrational Training as an Additional Intervention for Postural Balance, Balance Confidence and Functional Mobility in Type 2 Diabetic Patients with Lower Limb Burn Injury: A Randomized Clinical Trial. Diabetes Metab. Syndr. Obes. 2021, 14, 3617–3626. [Google Scholar] [CrossRef] [PubMed]
- Amtmann, D.; McMullen, K.; Bamer, A.; Fauerbach, J.A.; Gibran, N.S.; Herndon, D.; Schneider, J.C.; Kowalske, K.; Holavanahalli, R.; Miller, A.C. National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Review of Program and Database. Arch. Phys. Med. Rehabil. 2020, 101, S5–S15. [Google Scholar] [CrossRef] [PubMed]
- Ewing, J.A. Detecting Alcoholism: The CAGE Questionnaire. JAMA 1984, 252, 1905–1907. [Google Scholar] [CrossRef] [PubMed]
- Bamer, A.M.; McMullen, K.; Gibran, N.; Holavanahalli, R.; Schneider, J.C.; Carrougher, G.J.; Wiechman, S.; Wolfe, A.; Amtmann, D. Factors Associated with Attrition of Adult Participants in a Longitudinal Database: A National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System Study. J. Burn Care Res. 2020, 41, 270–279. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 15.1; StataCorp LLC.: College Station, TX, USA, 2017. [Google Scholar]
- Değer, T.B.; Saraç, Z.F.; Savaş, E.S.; Akçiçek, S.F. The Relationship of Balance Disorders with Falling, the Effect of Health Problems, and Social Life on Postural Balance in the Elderly Living in a District in Turkey. Geriatrics 2019, 4, 37. [Google Scholar] [CrossRef]
- Jia, H.; Lubetkin, E.I.; DeMichele, K.; Stark, D.S.; Zack, M.M.; Thompson, W.W. Prevalence, risk factors, and burden of disease for falls and balance or walking problems among older adults in the U.S. Prev. Med. 2019, 126, 105737. [Google Scholar] [CrossRef]
- Mitchell, M.B.; Bhattacharyya, N. Balance Disorder Trends in US Adults 2008–2016: Epidemiology and Functional Impact. OTO Open 2023, 7, e58. [Google Scholar] [CrossRef]
- WHO Ageing and Health; World Health Organization. Published 1 October 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 1 June 2024).
- Tompkins, R.G. Survival from burns in the new millennium: 70 years’ experience from a single institution. Ann. Surg. 2015, 261, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Bolt, G.; Hooimeijer, P. The impact of residential environment on older people’s capabilities to live independently: A survey in Beijing. BMC Public Health 2024, 24, 843. [Google Scholar] [CrossRef]
- Office of Disease Prevention and Health Promotion. Social Determinants of Health. Healthy People 2030. Published 2023. Available online: https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed on 1 June 2024).
- Hergenrather, K.C.; Zeglin, R.J.; McGuire-Kuletz, M.; Rhodes, S.D. Employment as a Social Determinant of Health: A Systematic Review of Longitudinal Studies Exploring the Relationship Between Employment Status and Physical Health. Rehabil. Res. Policy Educ. 2015, 29, 2–26. [Google Scholar] [CrossRef]
- Ross, C.E.; Mirowsky, J. Does employment affect health? J. Health Soc. Behav. 1995, 36, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Appelhans, B.M.; Gabriel, K.P.; Lange-Maia, B.S.; Karavolos, K.; Ylitalo, K.R.; Karvonen-Gutierrez, C.A.; Kravitz, H.M.; Janssen, I. Longitudinal associations of mid-life employment status with impaired physical function in the Study of Women’s Health Across the Nation. Ann. Epidemiol. 2022, 74, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, P.Y.; Ryu, E.; Jenkins, G.D.; Yost, K.J.; Kirt, C.R.; Larson, N.L.; Gupta, R.; Cerhan, J.R.; Olson, J.E. Employment Characteristics and Risk of Hospitalization Among Older Adults Participating in the Mayo Clinic Biobank. Mayo. Clin. Proc. Innov. Qual. Outcomes 2022, 6, 552–563. [Google Scholar] [CrossRef] [PubMed]
- Carrougher, G.J.; Bamer, A.M.; Mandell, S.P.; Brych, S.; Schneider, J.C.; Ryan, C.M.; Kowalske, K.; Esselman, P.C.; Gibran, N.S. Factors Affecting Employment After Burn Injury in the United States: A Burn Model System National Database Investigation. Arch. Phys. Med. Rehabil. 2020, 101, S71–S85. [Google Scholar] [CrossRef] [PubMed]
- Hutter, M.F.; Smolle, C.; Kamolz, L.P. Life after Burn, Part I: Health-Related Quality of Life, Employment and Life Satisfaction. Medicina 2022, 58, 599. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dyster-Aas, J.; Kildal, M.; Willebrand, M. Return to work and health-related quality of life after burn injury. J. Rehabil. Med. 2007, 39, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Lampiasi, N.; Jacobs, M. The role of physical and occupational therapies in fall prevention and management in the home setting. Care Manag. J. 2010, 11, 122–127. [Google Scholar] [CrossRef]
- Whitney, S.L.; Marchetti, G.F.; Ellis, J.L.; Otis, L. Improvements in balance in older adults engaged in a specialized home care falls prevention program. J. Geriatr. Phys. Ther. 2013, 36, 3–12. [Google Scholar] [CrossRef]
- Wolf, B.; Feys, H.; De Weerdt van der Meer, J.; Noom, M.; Aufdemkampe, G.; Noom, M. Effect of a physical therapeutic intervention for balance problems in the elderly: A single-blind, randomized, controlled multicentre trial. Clin. Rehabil. 2001, 15, 624–636. [Google Scholar] [CrossRef]
- Lezotte, D.C.; Hills, R.A.; Heltshe, S.L.; Holavanahalli, R.K.; Fauerbach, J.A.; Blakeney, P.; Klein, M.B.; Engrav, L.H. Assets and liabilities of the Burn Model System data model: A comparison with the National Burn Registry. Arch. Phys. Med. Rehabil. 2007, 88 (Suppl. S2), S7–S17. [Google Scholar] [CrossRef]
- Wolfe, A.E.; Stockly, O.R.; Abouzeid, C.; Rodríguez-Mercedes, S.L.; Flores, L.E.; Carrougher, G.J.; Gibran, N.S.; Holavanahalli, R.; McMullen, K.; Trinh, N.H.; et al. Burn model system national longitudinal database representativeness by race, ethnicity, gender, and age. PM R 2022, 14, 452–461. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).