Balance Impairment in the Burn Population: A Burn Model System National Database Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Burn Model System National Database
2.2. Demographic and Clinical Characteristics
2.3. Primary Outcomes
2.4. Data Analysis
3. Results
3.1. Descriptive Analysis
3.2. Primary Outcomes over Time
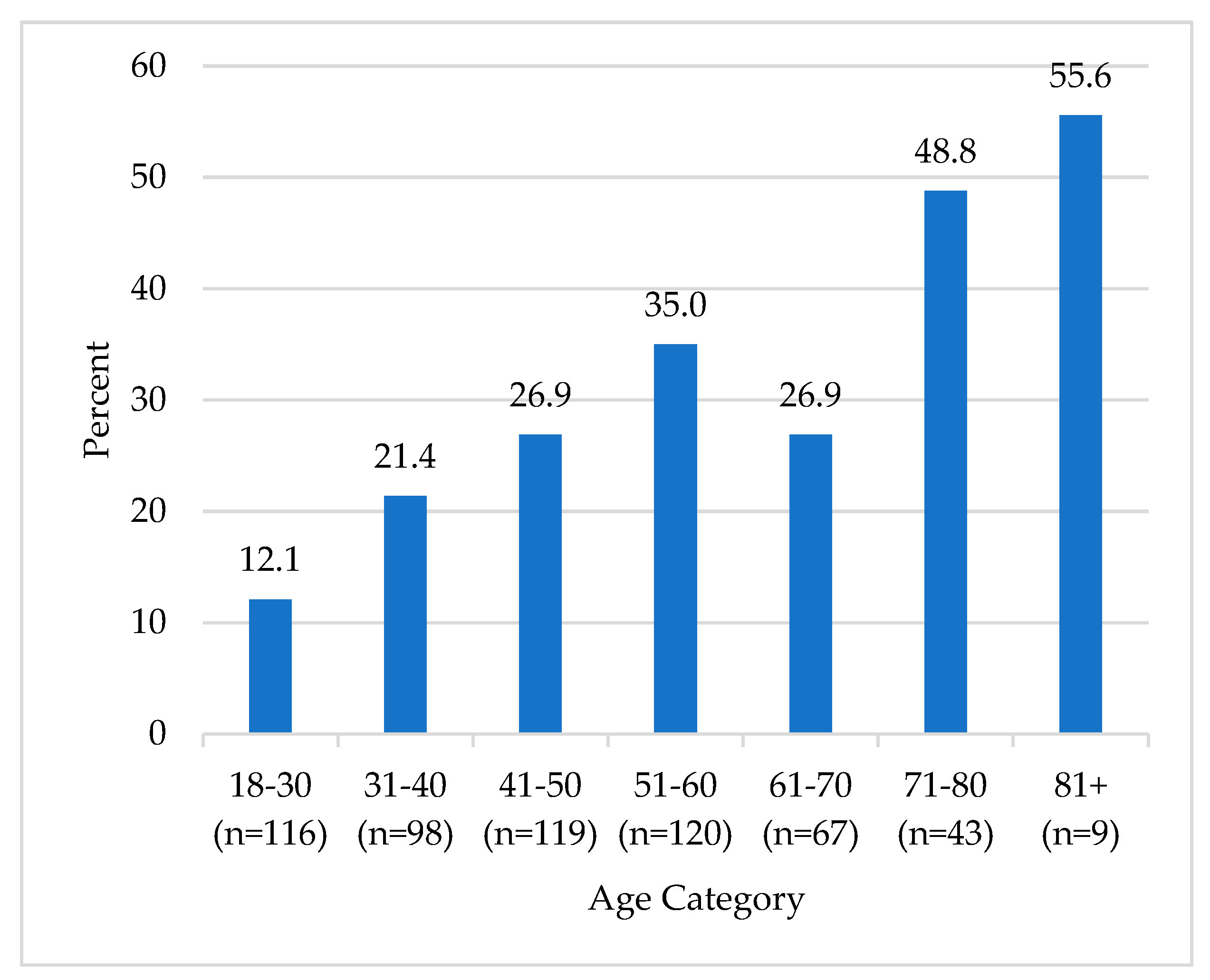
3.3. Association between Age and Self-Reported Balance Impairments
3.4. Regression Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oxford Languages. Oxford Dictionaries. Published 2023. Available online: https://languages.oup.com/ (accessed on 1 December 2023).
- Dunsky, A. The Effect of Balance and Coordination Exercises on Quality of Life in Older Adults: A Mini-Review. Front. Aging Neurosci. 2019, 11, 318. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, E.O.; Afilalo, J.; Ensrud, K.E.; Kowal, P.; Onder, G.; Fried, L.P. Frailty: Implications for clinical practice and public health. Lancet 2019, 394, 1365–1375. [Google Scholar] [CrossRef] [PubMed]
- Peterka, R.J.; Murchison, C.F.; Parrington, L.; Fino, P.C.; King, L.A. Implementation of a Central Sensorimotor Integration Test for Characterization of Human Balance Control During Stance. Front. Neurol. 2018, 9, 1045. [Google Scholar] [CrossRef] [PubMed]
- Rasman, B.G.; Forbes, P.A.; Tisserand, R.; Blouin, J.S. Sensorimotor Manipulations of the Balance Control Loop-Beyond Imposed External Perturbations. Front. Neurol. 2018, 9, 899. [Google Scholar] [CrossRef] [PubMed]
- Ie, K.; Chou, E.; Boyce, R.D.; Albert, S.M. Fall Risk-Increasing Drugs, Polypharmacy, and Falls Among Low-Income Community-Dwelling Older Adults. Innov. Aging 2021, 5, igab001. [Google Scholar] [CrossRef]
- Lee, H.; Lim, J.H. Living Alone, Environmental Hazards, and Falls Among U.S. Older Adults. Innov. Aging 2023, 7, igad055. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Procter-Gray, E.; Lipsitz, L.A.; Leveille, S.G.; Hackman, H.; Biondolillo, M.; Hannan, M.T. Utilitarian walking, neighborhood environment, and risk of outdoor falls among older adults. Am. J. Public Health 2014, 104, e30–e37. [Google Scholar] [CrossRef]
- Jiang, Y.; Xia, Q.; Wang, J.; Zhou, P.; Jiang, S.; Diwan, V.K.; Xv, B. Environmental risk factors associated with falls among older people living in long-term aged care facilities: A prospective study. Lancet 2019, 394, S23. [Google Scholar] [CrossRef]
- World Health Organization; Ageing Life Course Unit. WHO Global Report on Falls Prevention in Older Age; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Cuevas-Trisan, R. Balance Problems and Fall Risks in the Elderly. Phys. Med. Rehabil. Clin. N. Am. 2017, 28, 727–737. [Google Scholar] [CrossRef] [PubMed]
- Capek, K.D.; Sousse, L.E.; Hundeshagen, G.; Voigt, C.D.; Suman, O.E.; Finnerty, C.C.; Jennings, K.; Herndon, D.N. Contemporary Burn Survival. J. Am. Coll. Surg. 2018, 226, 453–463. [Google Scholar] [CrossRef]
- Abouzeid, C.A.; Wolfe, A.E.; Ni, P.; Carrougher, G.J.; Gibran, N.S.; Hammond, F.M.; Holavanahalli, R.; McMullen, K.A.; Roaten, K.; Suman, O.; et al. Are burns a chronic condition? Examining patient reported outcomes up to 20 years after burn injury-A Burn Model System National Database investigation. J. Trauma Acute Care Surg. 2022, 92, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- Kelter, B.M.; Holavanahalli, R.; Suman, O.E.; Ryan, C.M.; Schneider, J.C. Recognizing the long-term sequelae of burns as a chronic medical condition. Burns 2020, 46, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Nedelec, B.; Hou, Q.; Sohbi, I.; Choinière, M.; Beauregard, G.; Dykes, R.W. Sensory perception and neuroanatomical structures in normal and grafted skin of burn survivors. Burns 2005, 31, 817–830. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.C.; Qu, H.D.; Lowry, J.; Walker, J.; Vitale, E.; Zona, M. Efficacy of inpatient burn rehabilitation: A prospective pilot study examining range of motion, hand function and balance. Burn 2012, 38, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Mayo Clinic Staff. Balance Problems—Symptoms and Causes. Mayo Clinic. Published 2018. Available online: https://www.mayoclinic.org/diseases-conditions/balance-problems/symptoms-causes/syc-20350474 (accessed on 1 June 2024).
- National Institute on Aging. Older Adults and Balance Problems. Published 12 September 2022. Available online: https://www.nia.nih.gov/health/falls-and-falls-prevention/older-adults-and-balance-problems#causes (accessed on 1 June 2024).
- National Institute on Deafness Other Communication Disorders Balance Disorders (NIDCD). Published 12 March 2018. Available online: https://www.nidcd.nih.gov/health/balance-disorders (accessed on 1 June 2024).
- American Speech-Language-Hearing Association (n.d.). Balance System Disorders (Practice Portal). Available online: www.asha.org/Practice-Portal/Clinical-Topics/Balance-System-Disorders/ (accessed on 1 June 2024).
- Appeadu, M.; Bordoni, B. Falls and Fall Prevention in the Elderly. PubMed. Published 4 June 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560761/ (accessed on 1 June 2024).
- Othman, E.M.; Toson, R.A. Response of bone mineral density and balance performance in post-burn patients with selected Qigong training: A single-blind randomized controlled trial. Burns 2024, 50, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, Z.M.; Ali, O.I.; Moawd, S.A.; Eid, M.M.; Taha, M.M. Low Vibrational Training as an Additional Intervention for Postural Balance, Balance Confidence and Functional Mobility in Type 2 Diabetic Patients with Lower Limb Burn Injury: A Randomized Clinical Trial. Diabetes Metab. Syndr. Obes. 2021, 14, 3617–3626. [Google Scholar] [CrossRef] [PubMed]
- Amtmann, D.; McMullen, K.; Bamer, A.; Fauerbach, J.A.; Gibran, N.S.; Herndon, D.; Schneider, J.C.; Kowalske, K.; Holavanahalli, R.; Miller, A.C. National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Review of Program and Database. Arch. Phys. Med. Rehabil. 2020, 101, S5–S15. [Google Scholar] [CrossRef] [PubMed]
- Ewing, J.A. Detecting Alcoholism: The CAGE Questionnaire. JAMA 1984, 252, 1905–1907. [Google Scholar] [CrossRef] [PubMed]
- Bamer, A.M.; McMullen, K.; Gibran, N.; Holavanahalli, R.; Schneider, J.C.; Carrougher, G.J.; Wiechman, S.; Wolfe, A.; Amtmann, D. Factors Associated with Attrition of Adult Participants in a Longitudinal Database: A National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System Study. J. Burn Care Res. 2020, 41, 270–279. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 15.1; StataCorp LLC.: College Station, TX, USA, 2017. [Google Scholar]
- Değer, T.B.; Saraç, Z.F.; Savaş, E.S.; Akçiçek, S.F. The Relationship of Balance Disorders with Falling, the Effect of Health Problems, and Social Life on Postural Balance in the Elderly Living in a District in Turkey. Geriatrics 2019, 4, 37. [Google Scholar] [CrossRef]
- Jia, H.; Lubetkin, E.I.; DeMichele, K.; Stark, D.S.; Zack, M.M.; Thompson, W.W. Prevalence, risk factors, and burden of disease for falls and balance or walking problems among older adults in the U.S. Prev. Med. 2019, 126, 105737. [Google Scholar] [CrossRef]
- Mitchell, M.B.; Bhattacharyya, N. Balance Disorder Trends in US Adults 2008–2016: Epidemiology and Functional Impact. OTO Open 2023, 7, e58. [Google Scholar] [CrossRef]
- WHO Ageing and Health; World Health Organization. Published 1 October 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 1 June 2024).
- Tompkins, R.G. Survival from burns in the new millennium: 70 years’ experience from a single institution. Ann. Surg. 2015, 261, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Bolt, G.; Hooimeijer, P. The impact of residential environment on older people’s capabilities to live independently: A survey in Beijing. BMC Public Health 2024, 24, 843. [Google Scholar] [CrossRef]
- Office of Disease Prevention and Health Promotion. Social Determinants of Health. Healthy People 2030. Published 2023. Available online: https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed on 1 June 2024).
- Hergenrather, K.C.; Zeglin, R.J.; McGuire-Kuletz, M.; Rhodes, S.D. Employment as a Social Determinant of Health: A Systematic Review of Longitudinal Studies Exploring the Relationship Between Employment Status and Physical Health. Rehabil. Res. Policy Educ. 2015, 29, 2–26. [Google Scholar] [CrossRef]
- Ross, C.E.; Mirowsky, J. Does employment affect health? J. Health Soc. Behav. 1995, 36, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Appelhans, B.M.; Gabriel, K.P.; Lange-Maia, B.S.; Karavolos, K.; Ylitalo, K.R.; Karvonen-Gutierrez, C.A.; Kravitz, H.M.; Janssen, I. Longitudinal associations of mid-life employment status with impaired physical function in the Study of Women’s Health Across the Nation. Ann. Epidemiol. 2022, 74, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, P.Y.; Ryu, E.; Jenkins, G.D.; Yost, K.J.; Kirt, C.R.; Larson, N.L.; Gupta, R.; Cerhan, J.R.; Olson, J.E. Employment Characteristics and Risk of Hospitalization Among Older Adults Participating in the Mayo Clinic Biobank. Mayo. Clin. Proc. Innov. Qual. Outcomes 2022, 6, 552–563. [Google Scholar] [CrossRef] [PubMed]
- Carrougher, G.J.; Bamer, A.M.; Mandell, S.P.; Brych, S.; Schneider, J.C.; Ryan, C.M.; Kowalske, K.; Esselman, P.C.; Gibran, N.S. Factors Affecting Employment After Burn Injury in the United States: A Burn Model System National Database Investigation. Arch. Phys. Med. Rehabil. 2020, 101, S71–S85. [Google Scholar] [CrossRef] [PubMed]
- Hutter, M.F.; Smolle, C.; Kamolz, L.P. Life after Burn, Part I: Health-Related Quality of Life, Employment and Life Satisfaction. Medicina 2022, 58, 599. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dyster-Aas, J.; Kildal, M.; Willebrand, M. Return to work and health-related quality of life after burn injury. J. Rehabil. Med. 2007, 39, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Lampiasi, N.; Jacobs, M. The role of physical and occupational therapies in fall prevention and management in the home setting. Care Manag. J. 2010, 11, 122–127. [Google Scholar] [CrossRef]
- Whitney, S.L.; Marchetti, G.F.; Ellis, J.L.; Otis, L. Improvements in balance in older adults engaged in a specialized home care falls prevention program. J. Geriatr. Phys. Ther. 2013, 36, 3–12. [Google Scholar] [CrossRef]
- Wolf, B.; Feys, H.; De Weerdt van der Meer, J.; Noom, M.; Aufdemkampe, G.; Noom, M. Effect of a physical therapeutic intervention for balance problems in the elderly: A single-blind, randomized, controlled multicentre trial. Clin. Rehabil. 2001, 15, 624–636. [Google Scholar] [CrossRef]
- Lezotte, D.C.; Hills, R.A.; Heltshe, S.L.; Holavanahalli, R.K.; Fauerbach, J.A.; Blakeney, P.; Klein, M.B.; Engrav, L.H. Assets and liabilities of the Burn Model System data model: A comparison with the National Burn Registry. Arch. Phys. Med. Rehabil. 2007, 88 (Suppl. S2), S7–S17. [Google Scholar] [CrossRef]
- Wolfe, A.E.; Stockly, O.R.; Abouzeid, C.; Rodríguez-Mercedes, S.L.; Flores, L.E.; Carrougher, G.J.; Gibran, N.S.; Holavanahalli, R.; McMullen, K.; Trinh, N.H.; et al. Burn model system national longitudinal database representativeness by race, ethnicity, gender, and age. PM R 2022, 14, 452–461. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Variable | With Balance Impairments (n = 153) | Without Balance Impairments (n = 419) | p-Value |
|---|---|---|---|
| Age, median years (IQR) | 53.3 (42.1, 63.4) | 44.7 (31.1, 57.0) | <0.001 * |
| Male, n (%) | 99 (64.7) | 293 (69.9) | 0.234 |
| Higher than high school education, n (%) | 65 (51.6) | 194 (53.9) | 0.656 |
| Hispanic/Latino ethnicity, n (%) | 22 (14.8) | 91 (22.6) | 0.043 |
| Race, n (%) | |||
| White | 121 (80.7) | 348 (85.9) | 0.007 |
| African American/Black | 22 (14.7) | 25 (6.2) | |
| Other ꝉ | 7 (4.7) | 32 (7.9) | |
| Employed at time of injury, n (%) | 70 (49.0) | 296 (74.2) | <0.001 * |
| Insurance ¥, n (%) | |||
| Medicaid | 34 (22.7) | 53 (12.7) | <0.001 * |
| Medicare | 47 (31.3) | 63 (15.1) | |
| Private | 36 (24.0) | 163 (39.1) | |
| Other ꝉ | 15 (10.0) | 75 (18.0) | |
| No insurance | 18 (12.0) | 63 (15.1) | |
| Burn Model System Site, n (%) | |||
| Site A | 31.4 (48) | 35.3 (148) | 0.419 |
| Site B | 34.6 (53) | 28.2 (118) | |
| Site C | 34.0 (52) | 35.8 (150) | |
| Burn Etiology, n (%) | |||
| Flame | 92 (60.1) | 231 (55.3) | 0.582 |
| Electric | 10 (6.5) | 31 (7.4) | |
| Other ǂ | 51 (33.3) | 156 (37.3) | |
| Lower extremity amputation, n (%) | 5 (3.5) | 3 (0.8) | 0.019 |
| History of alcohol misuse, n (%) | 21 (14.9) | 48 (12.2) | 0.416 |
| History of drug misuse, n (%) | 7 (5.0) | 18 (4.7) | 0.896 |
| Range of motion deficit, n (%) | 99 (66.4) | 231 (56.1) | 0.027 |
| Inpatient rehabilitation, n (%) | 51 (34.7) | 89 (21.3) | 0.001 * |
| Outpatient PT/OT §, n (%) | 58 (41.7) | 93 (23.7) | <0.001 * |
| Multiple trips to the OR ¶, n (%) | 95 (62.1) | 205 (48.9) | 0.005 |
| Head/neck/face burn, n (%) | 79 (51.6) | 199 (47.6) | 0.394 |
| Feet/leg burn, n (%) | 122 (79.8) | 260 (62.1) | <0.001 * |
| Vision problems, n (%) | 39 (26.2) | 29 (7.0) | <0.001 * |
| Numbness in feet, n (%) | 83 (55.7) | 70 (16.8) | <0.001 * |
| Swollen feet or legs, n (%) | 69 (46.3) | 62 (14.9) | <0.001 * |
| Burn size, median TBSA ꝉꝉ percent (IQR) | 14.5 (4.0, 3.0) | 10.0 (3.0, 24.6) | 0.0349 |
| Body Mass Index at admission, median (IQRs) | 28.0 (23.8, 32.4) | 27.1 (24.2, 31.3) | 0.4182 |
| Timepoint ǂǂ | Those with Balance Impairments, n (%) | Total n at Timepoint | Missing Data |
|---|---|---|---|
| Discharge | 365 (40.3) | 906 | 156 |
| 6 months | 194 (28.7) | 675 | 479 |
| 12 months | 153 (26.8) | 572 | 510 |
| 24 months | 144 (28.6) | 503 | 445 |
| 60 months | 58 (36.0) | 161 | 539 |
| Follow-Up Timepoint | Response to Balance Item at Discharge and Follow-Up Timepoint, n | Balance Impairment at Discharge, n (%) | Balance Impairment at Follow-Up Timepoint, n (%) | Follow-Up Timepoint | Response to Balance Item at Discharge and Follow-up Timepoint, n |
|---|---|---|---|---|---|
| 6 Months | 591 | 243 (41.2) | 161 (27.2) | 6 Months | 591 |
| 12 Months | 483 | 193 (40.0) | 127 (26.3) | 12 Months | 483 |
| 24 Months | 343 | 139 (40.5) | 102 (29.7) | 24 Months | 343 |
| 60 Months | 54 | 28 (51.8) | 19 (35.2) | 60 Months | 54 |
| Variable | Odds Ratio | Robust SE | Z | p-Value | 95% Cl |
|---|---|---|---|---|---|
| Age | 1.04 | 0.01 | 3.85 | <0.001 ** | 1.02–1.07 |
| Female | 0.95 | 0.33 | −0.15 | 0.881 | 0.48–1.87 |
| Greater than high school education | 0.67 | 0.21 | −1.28 | 0.201 | 0.36–1.24 |
| Employed at time of injury | 0.29 | 0.10 | −3.50 | <0.001 ** | 0.14–0.58 |
| Burn Model System Site | |||||
| Site A | 0.98 | 0.40 | −0.06 | 0.955 | 0.43–2.19 |
| Site B | 0.89 | 0.36 | −0.29 | 0.768 | 0.40–1.97 |
| Body Mass Index | 0.99 | 0.02 | −0.24 | 0.813 | 0.95–1.04 |
| Alcohol misuse at discharge (preinjury recall) | 1.44 | 0.66 | 0.79 | 0.432 | 0.58–3.55 |
| Drug misuse at discharge (preinjury recall) | 0.62 | 0.48 | −0.62 | 0.536 | 0.14–2.78 |
| Lower limb amputation | 3.20 | 4.71 | 0.79 | 0.430 | 0.18–57.29 |
| Inpatient rehabilitation | 1.94 | 0.77 | 1.68 | 0.094 | 0.89–4.23 |
| Multiple operations §§ | 1.63 | 0.60 | 1.32 | 0.188 | 0.79–3.37 |
| Outpatient PT/OT at 12 months ꝉꝉꝉ | 2.40 | 0.79 | 2.67 | 0.008 ** | 1.26–4.57 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, E.; Chacon, K.L.; Shepler, L.J.; McMullen, K.A.; Slavin, M.D.; van de Rijn, M.; Kowalske, K.J.; Ryan, C.M.; Schneider, J.C. Balance Impairment in the Burn Population: A Burn Model System National Database Study. Eur. Burn J. 2024, 5, 238-248. https://doi.org/10.3390/ebj5030023
Santos E, Chacon KL, Shepler LJ, McMullen KA, Slavin MD, van de Rijn M, Kowalske KJ, Ryan CM, Schneider JC. Balance Impairment in the Burn Population: A Burn Model System National Database Study. European Burn Journal. 2024; 5(3):238-248. https://doi.org/10.3390/ebj5030023
Chicago/Turabian StyleSantos, Edward, Kaitlyn L. Chacon, Lauren J. Shepler, Kara A. McMullen, Mary D. Slavin, Marc van de Rijn, Karen J. Kowalske, Colleen M. Ryan, and Jeffrey C. Schneider. 2024. "Balance Impairment in the Burn Population: A Burn Model System National Database Study" European Burn Journal 5, no. 3: 238-248. https://doi.org/10.3390/ebj5030023
APA StyleSantos, E., Chacon, K. L., Shepler, L. J., McMullen, K. A., Slavin, M. D., van de Rijn, M., Kowalske, K. J., Ryan, C. M., & Schneider, J. C. (2024). Balance Impairment in the Burn Population: A Burn Model System National Database Study. European Burn Journal, 5(3), 238-248. https://doi.org/10.3390/ebj5030023







