Abstract
Background: This case report addresses the challenges of integrating orthodontic and prosthodontic treatment, particularly in clear aligner cases. The study introduces a novel milled-provisional crown with attachment (M-PCA) technique designed to enhance treatment efficacy and reduce orthodontic attachment debonding, a common issue in clear aligner therapy. Case Report: This is a case report that presents a 49-year-old female patient seeking orthodontic treatment for Class III malocclusion along with periodontal and prosthodontic challenges. The treatment plan involved a multidisciplinary approach, including using M-PCA for temporization during clear aligner therapy. Conclusions: The M-PCA approach demonstrated promising results, with no reported complications such as orthodontic attachment debonding throughout the treatment period. This innovation offers a significant advantage in managing orthodontic cases requiring provisional crowns, ensuring retention, and facilitating orthodontic treatment.
1. Introduction
Orthodontic treatment conservatively enhances functionality, occlusion, and appearance [1,2]. Clear aligners are a new generation of orthodontic treatment and were designed to treat mild to moderate crowding [3]. Orthodontists claim it has achieved successful outcomes with more complex malocclusions [4]. Nowadays, it is one of the most popular and frequently used treatment options among orthodontists [3]. Compared to conventional orthodontics, clear aligners have shown superior esthetics, lower demineralization, and minimal soft tissue irritation [5,6]. Another advantage of the clear aligner option is digital planning. The software can let patients view the simulated smile and final proposed treatment during treatment planning [7]. It has been shown that clear aligners are more commonly used in adult patients for their esthetic advantage over fixed orthodontic appliances [8]. It was also reported that it is a better option for the gingiva, as clear aligners have fewer periodontal indices measurements compared to other appliances [9]. With the increase in periodontal diseases reaching 50% in several countries [10], clear aligners can be a better choice in some cases.
On the other hand, clear aligners may initially cause speech articulation issues, discomfort, and increased salivation [11]. In some situations, clear aligners may fail to achieve buccal torque of the posterior teeth, significant rotation correction, or significant vertical movement [11]. In addition, the bodily movement of the teeth can be a significant limitation in clear aligner extraction cases [11].
Like conventional orthodontic appliances, clear aligners’ success depends on several factors, such as the duration of treatment. On average, the treatment duration of clear aligners for mild crowding takes 13 months to resolve, moderate crowding takes 15 months, and severe crowding takes around 17 months [12]. Clear aligners incorporate composite attachments during that time to increase their efficacy and predictability [13]. Unfortunately, there are reports of increased loss of these attachments at regular intervals during orthodontic treatment, reaching a prevalence of more than 60% [14]. Orthodontic attachment debonding can be related to several contributing factors, such as the frequency of aligner removal, occlusal forces introduced by mastication, and aligner wearing time [14]. In addition to their efficacy, some of these attachments are commonly used to deliver force to a specific part of the tooth to cause the orthodontic tooth movement necessary and to provide a better-controlled tooth movement depending on the software algorithm [15]. Other attachments are designed to retain the aligners on the teeth [15].
Provisional crowns are encountered in orthodontic cases that involve multidisciplinary approaches [16]. Fixed Partial Dentures (FPDs) and crowns are commonly found in adult patients who seek orthodontic treatment [17]. In some clinical situations, the existing fixed prostheses must be replaced due to biological, mechanical, or esthetic complications. The replacement of the defective prosthesis usually occurs during the first phase of treatment, in which the abutment tooth is temporized by provisional restoration. With clear aligner appliances, bonding attachments to provisional crowns come with challenges [18]. Therefore, this novel approach was developed to combine the attachment and provisional crown as one milled unit to overcome these challenges. This case report aims to present the workflow for the use of a Milled-Provisional Crown with Attachment (M-PCA) and its associated clinical outcomes.
2. Case Report
2.1. Case Presentation
A 49-year-old Saudi female patient came to the orthodontic faculty clinics at Imam Abdulrahman bin Faisal University Dental Hospital with a complaint: “My teeth are crooked, and I would like to correct them”. Her medical history showed no significant findings. Her dental history showed multiple restorations and missing teeth. Upon clinical examination, multiple caries lesions, generalized calculus deposition, generalized gingival recession, a missing tooth (#3), two 3-unit FPDs on teeth #2, X, 4, & 13, X, 15, crowns on teeth #12, 19, 20, and 30, Class I malocclusion, an overjet range from 0 to 1 mm, a shallow overbite of 0–1 mm, a shifted lower midline of 1 mm, 3 mm upper crowding, and 1 mm lower crowding were found. The lateral cephalometric radiograph suggested a normodivergent pattern, with a Class III skeletal relation complicated by the retrognathic maxilla and proclined upper and lower incisors (Figure 1A–E and Figure 2A,B).

Figure 1.
The initial intraoral photographs before restorability assessments: (A) right occlusion; (B) front occlusion; (C) left occlusion; (D) maxillary occlusion; (E) mandibular occlusion.
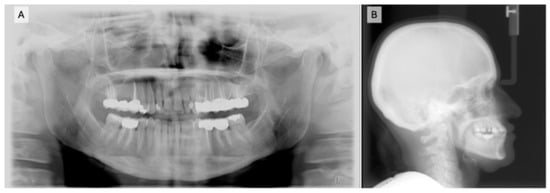
Figure 2.
Radiographs taken before orthodontic treatment: (A) orthopantomography (OPG) taken during the initial visit and (B) a lateral cephalometric radiograph before the start of treatment.
The orthodontic diagnosis was Class III malocclusion due to retrognathic maxilla complicated with mild lower crowding and reverse overjet.
In Phase I, a standard treatment planning protocol was used to fabricate M-PCA prostheses. This was followed by a free gingival graft on the maxillary anterior teeth and orthodontic treatment using a clear aligner (comprehensive Invisalign® treatment).
2.2. M-PCA Design and Technique Description
The patient was referred to the prosthodontics faculty clinics to assess crowns, FPDs, and caries control. After the prosthodontic evaluation, tooth #4 was unrestorable, defective FPDs on #2, X, 4, and #13, X, 15, and several defective crowns needed to be removed. Abutment teeth #2, 13, 14, 15, 18, and 19 were selected for M-PCA units. The technique used for the fabrication of the M-PCA can be summarized as follows:
- Obtain a digital impression of the abutment teeth using an intraoral scanner (Trios 3®, 3Shape, Copenhagen, Denmark) (Figure 3A,B), and then export the impression as standard tessellation language (STL) files.
- Open a new job order in the CAD software program (Exocad DentalCAD Version 3.1, Exocad GmbH, Darmstadt, Germany), and then select the abutment teeth and their antagonist (Figure 3C).
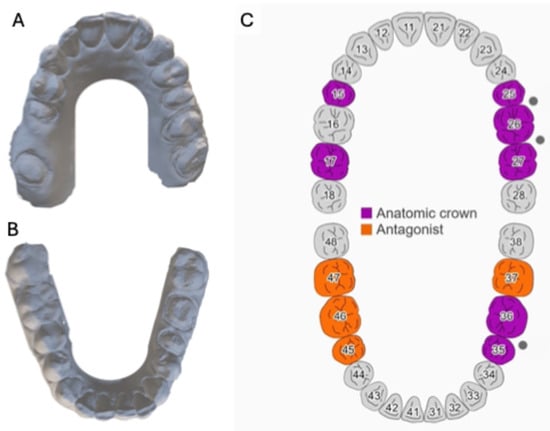 Figure 3. The process for fabricating M-PCA utilizing digital dentistry: (A) maxillary digital model; (B) mandibular digital model; (C) selecting the abutment teeth that will receive M-PCA and their antagonist.
Figure 3. The process for fabricating M-PCA utilizing digital dentistry: (A) maxillary digital model; (B) mandibular digital model; (C) selecting the abutment teeth that will receive M-PCA and their antagonist. - After that, use the anatomical crown option under the crowns and copings for material configuration, select acrylic/PMMA for the material option, and select the other options and parameters, as seen in Figure 4.
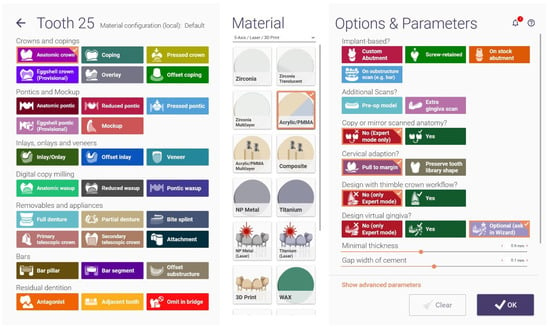 Figure 4. A screenshot of the Exocad software shows the proper options for M-PCA fabrication.
Figure 4. A screenshot of the Exocad software shows the proper options for M-PCA fabrication. - Use the margin line detection feature to detect the margins of all abutment teeth (Figure 5C).
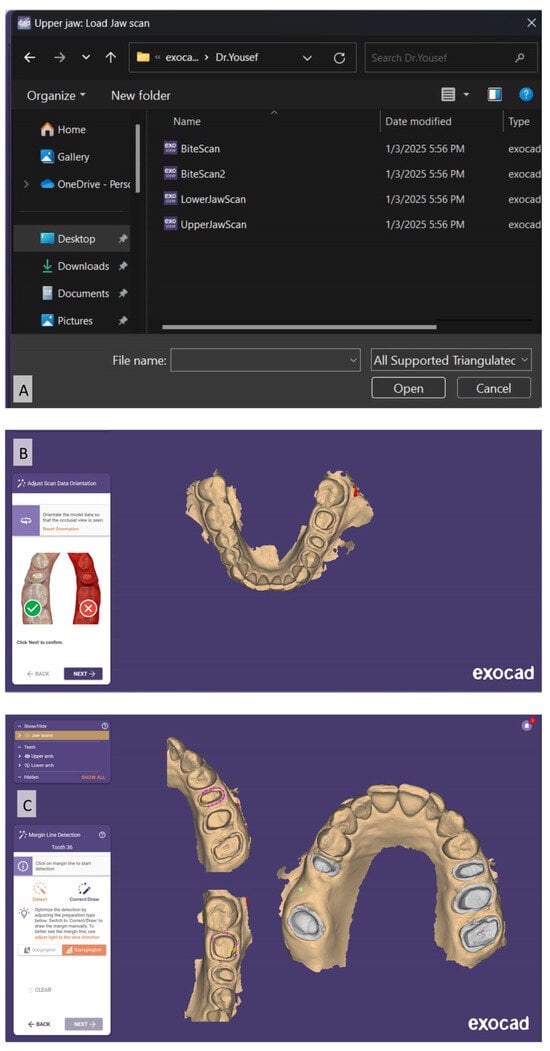 Figure 5. Screenshots of the Exocad software show (A) importing of digital impressions; (B) scan data orientation; and (C) marginal line detection.
Figure 5. Screenshots of the Exocad software show (A) importing of digital impressions; (B) scan data orientation; and (C) marginal line detection. - Modify the cement gap from the crown bottoms menu and set it to “no cement gap” for the marginal area and “0.1 mm” for the remaining structure (Figure 6A).
- From the tooth placement option, perform digital teeth wax-up using a digital library (Figure 6B), and then adjust the axial contour, proximal contact, and occlusion using the free-forming feature (Figure 6C).
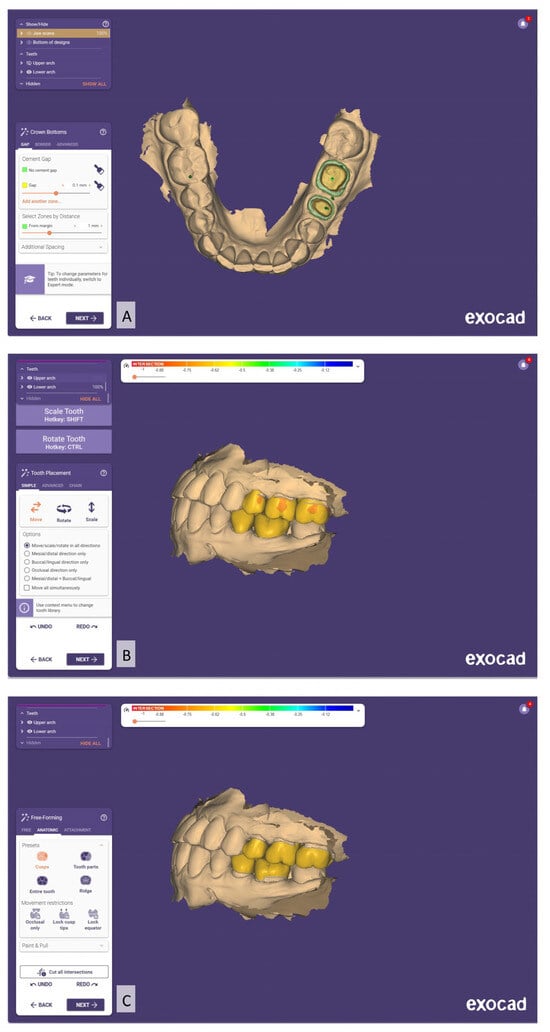 Figure 6. Screenshots of the Exocad software show: (A) cement gap setting; (B) digital teeth wax-up; (C) modification of the teeth wax-up.
Figure 6. Screenshots of the Exocad software show: (A) cement gap setting; (B) digital teeth wax-up; (C) modification of the teeth wax-up. - Rotate the attachment towards the gingival area to mimic the horizontal gingivally beveled attachment (Figure 7B).
- At the end, check the final M-PCA design to ensure that the proper contour, proximal contact, occlusion, and shape and location of the attachment have been achieved (Figure 7C).
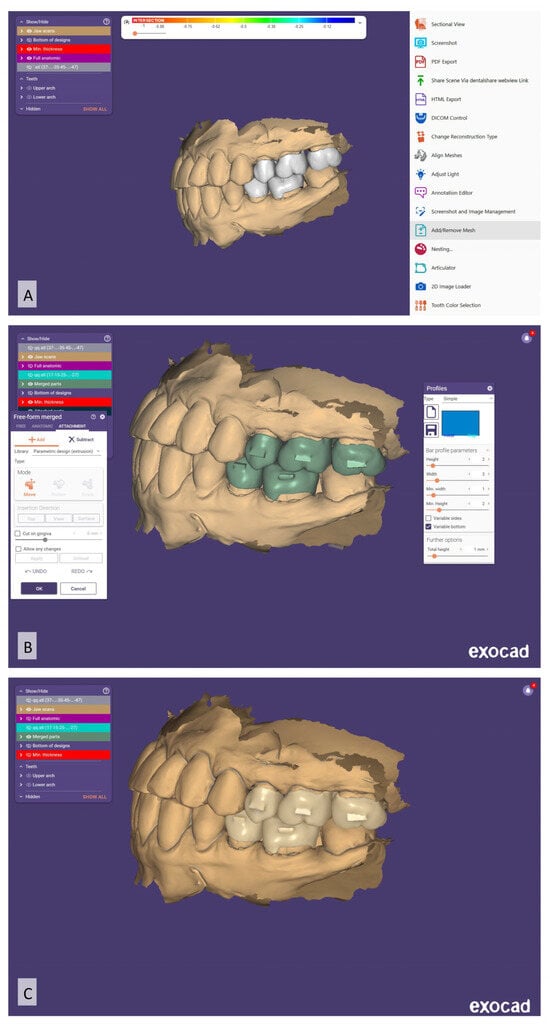 Figure 7. Screenshots of the Exocad software show: (A) option used to add the attachments for the teeth wax-up; (B) parameters and measurements of the attachment; (C) final M-PCA designs.
Figure 7. Screenshots of the Exocad software show: (A) option used to add the attachments for the teeth wax-up; (B) parameters and measurements of the attachment; (C) final M-PCA designs. - Transfer the virtual design to a milling machine (Zenotec T1, Wieland, Germany), and then use a monolayer Poly-(methyl methacrylate) (PMMA) disk to fabricate the M-PCA units.
- After the clinical evaluation of the M-PCA units, perform an air abrasion treatment of the intaglio (inner) surface, and then cement the M-PCA units with an adhesive resin cement (RelyX Unicem, 3M ESPE, St. Paul, MN, USA).
2.3. Periodontic and Orthodontic Treatment Progress
After cementation of the M-PCA units, the patient was referred to the periodontics faculty clinics to evaluate the periodontium, extract tooth #4, and manage the recession with a free gingival graft (Figure 8A–E).

Figure 8.
Intraoral photographs after caries and periodontal clearance with M-PCA cemented to abutment teeth: (A) right occlusion; (B) front occlusion; (C) left occlusion; (D) maxillary occlusion; (E) mandibular occlusion.
Three months later, the patient was scanned for Invisalign® treatment (Align Technology, Santa Clara, CA, USA) (Figure 9A–E).
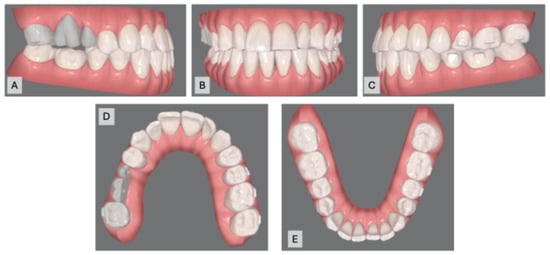
Figure 9.
Intraoral scans for clear aligner: (A) right occlusion; (B) front occlusion; (C) left occlusion; (D) maxillary occlusion; (E) mandibular occlusion.
The patient was seen for visit 1 for transitional aligners 1–3 (3 weeks). At visit 2, an IPR of 0.3 for mandibular anterior teeth was performed, and aligners 4–15 (12 weeks) were provided. In visit 3, aligners 16–27 (12 weeks) were given, followed by 28–39 (12 weeks) at visit 4. The patient was instructed to change aligners weekly. Teeth tracking was satisfactory at each visit, with no emergency incidents or attachment breakage, and aligners adapted well to the M-PCA (Figure 10A–E).

Figure 10.
Intraoral photographs after orthodontic treatment: (A) right occlusion; (B) front occlusion; (C) left occlusion; (D) maxillary occlusion; (E) mandibular occlusion.
3. Discussion
The demand for adult orthodontic treatment utilizing clear aligner therapy is increasing [3]. However, multiple restorations, such as ceramic crowns and FPDs, pose difficulties for orthodontists regarding this age group. Currently, various esthetic restorations and bonding procedures are available [19,20]. Therefore, orthodontists struggle to find the optimal surface conditioning and bonding techniques for ceramics that produce strong attachment bonds without affecting the ceramic’s surface after debonding [21,22]. One of the critical factors for the success of any orthodontic treatment is the retention of the orthodontic appliances on the teeth throughout the treatment. Increased incidence of breakage or detachment of the orthodontic appliance can negatively affect the overall success [23].
In clear aligner therapy, attachments are considered a crucial auxiliary device to deliver forces from the aligner to the tooth crown and root. These attachments are a force transducer that help improve clear aligners’ biomechanics [24]. They are made of direct composite resin attached to the tooth surface [24]. With the aid of a computer program, attachments are automatically positioned in specific locations on teeth. They regulate the force’s application point, direction, and amount applied [25]. Aligner attachments come in different forms that help retain teeth and enable greater control of specific tooth movements [26]. Thus, the primary factors determining the attachment’s effectiveness and aligner fitting are its positioning and configuration [26]. Nevertheless, the material used plays a crucial role, since it should remain in the patient’s mouth throughout orthodontic therapy and must maintain its features over time. Indubitably, these auxiliary components’ mechanical and physical properties are significantly impacted by the material selection [27].
This case report presents a novel dental technique that outlines a method for fabricating M-PCA as a single unit. The attachment design aims to replicate retentive, gingivally beveled attachments as well as vertical and horizontal attachments. The selection of attachments was based on the necessity for tooth movement and to create/manage a force system. In this case report, a horizontal gingivally beveled attachment measuring (2 × 3 mm) was utilized in all M-PCA.
Digital dental workflows are user- and patient-friendly, delivering predictable, accurate, and effective treatment modalities [28,29]. This case report highlighted the opportunity to use Computer-Aided Design and Computer-Aided Manufacturing (CAD-CAM) to fabricate the M-PCA for clear aligner therapy. The results clearly show that the accuracy and adaptation of the M-PCA units used were clinically acceptable. This report provided information that may help the practitioner overcome the difficulties and challenges during bonding attachments on provisional crowns. The bonding time was also reduced, as this step was entirely eliminated during bonding at the attachments visit. Furthermore, the extra flush, discrepancy, and ill-fitting issues were eliminated using this technique.
In clinical settings, several factors contribute to early attachment failure in terms of debonding, shape changes, and loss of aligner fit [14]. Orthodontic attachment debonding can result in significant clinical issues that may increase the likelihood of treatment failure, lengthen treatment times, and require more follow-up visits [30]. Orthodontic attachment debonding can occur due to bond failure or patient negligence, influenced by operator-related, patient-related, and clinical factors [14]. Operator factors involve the bonding materials and protocols, while patient factors include the frequency of aligner removal [14]. Clinical variables encompass the attachment’s location, number, and shape, with molar attachments being the most prone to loss due to increased forces during aligner use [14].
Several investigations evaluated the bond strength of conventional brackets to different restorative materials, such as dental ceramic [31], composite [32], amalgam [33], gold alloy [34], and PMMA [35]. It was reported that the bond strength of conventional stainless steel brackets to provisional crowns can tolerate orthodontic tooth movement using mechanical surface treatment [35]. For that reason, it was recommended to perform surface treatments, such as sandblasting of provisional crowns, to achieve clinically successful bonding and reduce bracket breakage during orthodontic therapy [35].
In clear aligner therapy, efforts have been conducted to improve the bonding of direct composite attachment [21,36]. Alsaud et al. evaluated the effect of different surface treatments of composite attachments bonded to lithium disilicate ceramics [21]. When the dislocation force outweighs the bonding force, the attachment will quickly be lost from the tooth surface. The dislocation force on the attachments will increase each time the patient places or removes the aligner [37].
A recent in vitro study by Shahin et al. [38] evaluated 3D-printed provisional crowns with attachments as one unit to overcome the debonding of orthodontic attachments. In this case report, milled-provisional PMMA crowns were used; with this novel technique, there was no emergency or breakdown of the crown attachment throughout the treatment. Moreover, the aligners were perfectly adapted to the M-PCA.
Since composite attachments are a crucial part of clear aligner therapy, it is vital to meticulously replicate them to preserve their integrity throughout the treatment [24]. The curing process can significantly impact the morphology and resistance of attachments, as in all other polymerization phases [39]. Nevertheless, the polymerization shrinkage factor is eliminated in this case by using M-PCA. After one year of bonding, the attachment deterioration rate was reported to be 14.79% for flowable composite material, while 9.70% was reported for packable composite [40]. In this case, all M-PCA had no damage or change in the shape and size during the “10 months” treatment time.
As reported, clear aligner patients have higher esthetic demands [41]. In addition to orthodontic attachment debonding, attachment discoloration can cause dissatisfaction during orthodontic treatment [42]. Studies have shown that surface roughness influences the staining of resin composites [43,44,45,46]. In this case report, M-PCA use showed good color stability throughout the treatment.
A systematic review confirmed that treatment with clear aligners results in better periodontal health [9]. In this case, the patient’s periodontal health was optimal throughout the orthodontic treatment, and no periodontal breakdown was noticed, especially around the M-PCA abutments.
In summary, this report defined the areas of new methods that can be adopted for many clear aligner providers, especially in adult patients. However, some limitations are associated, such as the use of only one attachment design and dimension and one type of milled provisional restoration. Future in vitro and in vivo studies should be conducted to evaluate this concept using different attachment designs, dimensions, and materials. In addition, these types of attachments’ performance (wear, color change, bacterial accumulation) should be investigated to simulate prolonged clinical usage.
4. Conclusions
This case showed a substantial potential for attachment modality in provisional crowns during orthodontic treatment. M-PCA can be used as a type of provisional crown where clear aligners are to be used. Using this method, the M-PCA was able to overcome most of the challenges encountered during orthodontic treatment. The emergency visit was eliminated, and aligners were found to be tracking exceptionally at each visit. The color stability and attachment durability (shape and size) were well maintained. Moreover, this paper defines and describes new and unique methods that can be adopted by many clear aligner providers, especially in adult patients. However, the M-PCA concept needs to be investigated further.
Author Contributions
Conceptualization, A.A. and Y.A.A.-D.; methodology, A.A. and Y.A.A.-D.; investigation, A.A. and Y.A.A.-D.; resources, A.A. and Y.A.A.-D.; writing—original draft preparation, A.A. and Y.A.A.-D.; writing—review and editing, A.A. and Y.A.A.-D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Imam Abdulrahman Bin Faisal University (IRB: 2023-02-600, 21 December 2023).
Informed Consent Statement
Informed consent was obtained from the subject involved in the study.
Data Availability Statement
Data are available upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Swanson, K.; Hermanides, L. Biomechanics and Function: Altering Paradigms to Treat a Patient’s Esthetic Disability Conservatively. Compend. Contin. Educ. Dent. 2020, 41, 284–289. [Google Scholar]
- Guzman-Perez, G.; Jurado, C.A.; Alshahib, A.; Afrashtehfar, K.I. An Immediate Implant Approach to Replace Failing Maxillary Anterior Dentition Due to Orthodontically Induced Severe Root Resorption. Int. J. Oral Implantol. 2023, 16, 339–348. [Google Scholar]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of Clear Aligners in Controlling Orthodontic Tooth Movement: A Systematic Review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Yassir, Y.A.; Nabbat, S.A.; McIntyre, G.T.; Bearn, D.R. Clinical Effectiveness of Clear Aligner Treatment Compared to Fixed Appliance Treatment: An Overview of Systematic Reviews. Clin. Oral Investig. 2022, 26, 2353–2370. [Google Scholar] [CrossRef]
- Patel, D.; Mehta, F.; Mehta, N. Aesthetic Orthodontics: An Overview. Orthod. J. Nepal 2014, 4, 38–43. [Google Scholar] [CrossRef]
- Alsaeed, S.; Afrashtehfar, K.I.; Alharbi, M.H.; Alfarraj, S.S.; Alluhaydan, S.A.; Abahussain, F.A.; Alotaibi, G.M.; Awawdeh, M.A. Impact of Orthodontic Appliances on Hiring Prospects in Saudi Arabia: A Cross-Sectional Study. Cureus 2023, 15, e40173. [Google Scholar] [CrossRef]
- Weir, T. Clear Aligners in Orthodontic Treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef]
- Phan, X.; Ling, P.H. Clinical Limitations of Invisalign. J. Can. Dent. Assoc. 2007, 73, 263–266. [Google Scholar]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Periodontal Health during Clear Aligners Treatment: A Systematic Review. Eur. J. Orthod. 2014, 37, 539–543. [Google Scholar] [CrossRef]
- Nazir, M.A. Prevalence of Periodontal Disease, Its Association with Systemic Diseases and Prevention. Int. J. Health Sci. 2017, 11, 72–80. [Google Scholar]
- Lemos, C.R.; Fadel, M.A.V.; Polmann, H.; de Oliveira, J.M.D.; Pauletto, P.; Stefani, C.M.; Flores-Mir, C.; Canto, G.D.L. Clear Aligner’s Adverse Effects: A Systematic Review Protocol. PLoS ONE 2024, 19, e0302049. [Google Scholar] [CrossRef]
- Galan-Lopez, L.; Barcia-Gonzalez, J.; Plasencia, E. A Systematic Review of the Accuracy and Efficiency of Dental Movements with Invisalign®. Korean J. Orthod. 2019, 49, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Nucera, R.; Dolci, C.; Bellocchio, A.M.; Costa, S.; Barbera, S.; Rustico, L.; Farronato, M.; Militi, A.; Portelli, M. Effects of Composite Attachments on Orthodontic Clear Aligners Therapy: A Systematic Review. Materials 2022, 15, 533. [Google Scholar] [CrossRef]
- Yaosen, C.; Mohamed, A.; Jinbo, W.; Ziwei, Z.; Al-Balaa, M.; Yan, Y. Risk Factors of Composite Attachment Loss in Orthodontic Patients during Orthodontic Clear Aligner Therapy: A Prospective Study. BioMed Res. Int. 2021, 2021, 6620377. [Google Scholar] [CrossRef]
- El-Bialy, T.; Galante, D.; Daher, S. Orthodontic Biomechanics: Treatment of Complex Cases Using Clear Aligner; Bentham Science Publishers: Sharjah, United Arab Emirates, 2016; Volume 1. [Google Scholar]
- Harrison, J.E.; Bowden, D.E. The Orthodontic/Restorative Interface. Restorative Procedures to Aid Orthodontic Treatment. Br. J. Orthod. 1992, 19, 143–152. [Google Scholar] [CrossRef]
- Andreasen, G.F.; Stieg, M.A. Bonding and Debonding Brackets to Porcelain and Gold. Am. J. Orthod. Dentofac. Orthop. 1988, 93, 341–345. [Google Scholar] [CrossRef]
- Barreda, G.J.; Dzierewianko, E.A.; Muñoz, K.A.; Piccoli, G.I. Surface Wear of Resin Composites Used for Invisalign® Attachments. Acta Odontol. Latinoam. AOL 2017, 30, 90–95. [Google Scholar] [PubMed]
- Makhija, S.K.; Lawson, N.C.; Gilbert, G.H.; Litaker, M.S.; McClelland, J.A.; Louis, D.R.; Gordan, V.V.; Pihlstrom, D.J.; Meyerowitz, C.; Mungia, R.; et al. Dentist Material Selection for Single-Unit Crowns: Findings from the National Dental Practice-Based Research Network. J. Dent. 2016, 55, 40–47. [Google Scholar] [CrossRef]
- Zarone, F.; Ferrari, M.; Mangano, F.G.; Leone, R.; Sorrentino, R. “Digitally Oriented Materials”: Focus on Lithium Disilicate Ceramics. Int. J. Dent. 2016, 2016, 9840594. [Google Scholar] [CrossRef]
- Alsaud, B.A.; Hajjaj, M.S.; Masoud, A.I.; Abou Neel, E.A.; Abuelenain, D.A.; Linjawi, A.I. Bonding of Clear Aligner Composite Attachments to Ceramic Materials: An in Vitro Study. Materials 2022, 15, 4145. [Google Scholar] [CrossRef]
- Bayoumi, R.E.; El-Kabbany, S.M.; Gad, N. Effect of Different Surface Treatment Modalities on Surface Roughness and Shear Bond Strength of Orthodontic Molar Tubes to Lithium Disilicate Ceramics. Egypt. Dent. J. 2019, 65, 641–656. [Google Scholar] [CrossRef][Green Version]
- Borzangy, S. Impact of Surface Treatment Methods on Bond Strength of Orthodontic Brackets to Indirect Composite Provisional Restorations. J. Contemp. Dent. Pract. 2019, 20, 1412–1416. [Google Scholar] [CrossRef] [PubMed]
- Garino, F.; Castroflorio, T.; Daher, S.; Ravera, S.; Rossini, G.; Cugliari, G.; Deregibus, A. Effectiveness of Composite Attachments in Controlling Upper-Molar Movement with Aligners. J. Clin. Orthod. 2016, 50, 341–347. [Google Scholar]
- Abela, S. Interceptive Orthodontics: A Practical Guide to Occlusal Management. Eur. J. Orthod. 2017, 39, 342. [Google Scholar] [CrossRef][Green Version]
- Savignano, R.; Valentino, R.; Razionale, A.; Michelotti, A.; Barone, S.; D’anto, V. Biomechanical Effects of Different Auxiliary-Aligner Designs for the Extrusion of an Upper Central Incisor: A Finite Element Analysis. J. Healthc. Eng. 2019, 2019, 9687127. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, E.; Castroflorio, E.; Rossini, G.; Garino, F.; Cugliari, G.; Deregibus, A.; Castroflorio, T. Scanning Electron Microscopy Analysis of Aligner Fitting on Anchorage Attachments. J. Orofac. Orthop. 2019, 80, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Conejo, J. The Current State of Chairside Digital Dentistry and Materials. Dent. Clin. N. Am. 2019, 63, 175–197. [Google Scholar] [CrossRef] [PubMed]
- Garaicoa, J.; Jurado, C.A.; Afrashtehfar, K.I.; Alhotan, A.; Fischer, N.G. Digital Full-Mouth Reconstruction Assisted by Facial and Intraoral Scanners: A Case Report and Technique Description. Appl. Sci. 2023, 13, 1917. [Google Scholar] [CrossRef]
- Dasy, H.; Dasy, A.; Asatrian, G.; Rózsa, N.; Lee, H.-F.; Kwak, J.H. Effects of Variable Attachment Shapes and Aligner Material on Aligner Retention. Angle Orthod. 2015, 85, 934–940. [Google Scholar] [CrossRef] [PubMed]
- Grewal Bach, G.K.; Torrealba, Y.; Lagravère, M.O. Orthodontic Bonding to Porcelain: A Systematic Review. Angle Orthod. 2013, 84, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Eslamian, L.; Borzabadi-Farahani, A.; Mousavi, N.; Ghasemi, A. The Effects of Various Surface Treatments on the Shear Bond Strengths of Stainless Steel Brackets to Artificially-Aged Composite Restorations. Australas. Orthod. J. 2011, 27, 28–32. [Google Scholar] [CrossRef]
- Zachrisson, B.U.; Büyükyilmaz, T.; Zachrisson, Y. Improving Orthodontic Bonding to Silver Amalgam. Angle Orthod. 1995, 65, 35–42. [Google Scholar] [CrossRef]
- Büyükyilmaz, T.; Zachrisson, Y.Ø.; Zachrisson, B.U. Improving Orthodontic Bonding to Gold Alloy. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 510–518. [Google Scholar] [CrossRef] [PubMed]
- Shahin, S.Y.; Abu Showmi, T.H.; Alzaghran, S.H.; Albaqawi, H.; Alrashoudi, L.; Gad, M.M. Bond Strength of Orthodontic Brackets to Temporary Crowns: In Vitro Effects of Surface Treatment. Int. J. Dent. 2021, 2021, 9999933. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Qian, L.; Qian, Y.; Zhang, Z.; Wen, X. Comparative Study of Three Composite Materials in Bonding Attachments for Clear Aligners. Orthod. Craniofacial Res. 2021, 24, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Skaik, A.; Wei, X.L.; Abusamak, I.; Iddi, I. Effects of Time and Clear Aligner Removal Frequency on the Force Delivered by Different Polyethylene Terephthalate Glycol-Modified Materials Determined with Thin-Film Pressure Sensors. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Shahin, S.Y.; Nassar, E.A.; Gad, M.M. 3D-Printed One-Piece versus Two-Piece Orthodontic Clear Aligner Attachments Bonded with Provisional Crowns: A Proof of Concept. J. Dent. 2024, 151, 105406. [Google Scholar] [CrossRef]
- Gazzani, F.; Bellisario, D.; Quadrini, F.; Parrinello, F.; Pavoni, C.; Cozza, P.; Lione, R. Comparison Between Different Composite Resins Used for Clear Aligner Attachments: An In-Vitro Study. Front. Mater. 2022, 8, 789143. [Google Scholar] [CrossRef]
- Lin, S.; Huang, L.; Li, J.; Wen, J.; Mei, L.; Xu, H.; Zhang, L.; Li, H. Assessment of Preparation Time and 1-Year Invisalign Aligner Attachment Survival Using Flowable and Packable Composites: A Split-Mouth Clinical Study. Angle Orthod. 2021, 91, 583–589. [Google Scholar] [CrossRef]
- Alansari, R.A.; Faydhi, D.A.; Ashour, B.S.; Alsaggaf, D.H.; Shuman, M.T.; Ghoneim, S.H.; Linjawi, A.I.; Marghalani, H.Y.; Dause, R.R. Adult Perceptions of Different Orthodontic Appliances. Patient Prefer. Adherence 2019, 13, 2119–2128. [Google Scholar] [CrossRef]
- Ardu, S.; Duc, O.; Di Bella, E.; Krejci, I. Color Stability of Recent Composite Resins. Odontology 2017, 105, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Roeder, L.B.; Lei, L.; Powers, J.M. Effect of Surface Roughness on Stain Resistance of Dental Resin Composites. J. Esthet. Restor. Dent. 2005, 17, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Ghinea, R.; Ugarte-Alvan, L.; Yebra, A.; Pecho, O.E.; Paravina, R.D.; Perez, M. del M. Influence of Surface Roughness on the Color of Dental-Resin Composites. J. Zhejiang Univ. Sci. B 2011, 12, 552–562. [Google Scholar] [CrossRef] [PubMed]
- Tavangar, M.; Bagheri, R.; Kwon, T.-Y.; Mese, A.; Manton, D.J. Influence of Beverages and Surface Roughness on the Color Change of Resin Composites. J. Investig. Clin. Dent. 2018, 9, e12333. [Google Scholar] [CrossRef] [PubMed]
- Duc, O.; Di Bella, E.; Krejci, I.; Betrisey, E.; Abdelaziz, M.; Ardu, S. Staining Susceptibility of Resin Composite Materials. Am. J. Dent. 2019, 32, 39–42. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).