Xanthogranulomatous Prostatitis: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
- Original articles reporting on patients diagnosed with xanthogranulomatous prostatitis upon histopathological examination.
- Studies providing data on at least one of the following outcomes: patient demographics, clinical presentation, mode of diagnosis, treatment modalities, and patient outcomes.
- Case reports, case series, observational studies (cohort and case–control), and clinical trials were included.
- Reviews, commentaries, editorials, letters, conference abstracts, or expert opinions.
- Studies not providing specific data on outcomes for patients.
- Studies on paediatric or neonatal patients (aged < 18 years).
2.2. Data Extraction and Quality Assessment
2.3. Data Synthesis and Analysis
2.4. Risk of Bias Across Studies
2.5. Ethics Approval and Consent to Participate
2.6. Availability of Data and Material
3. Results
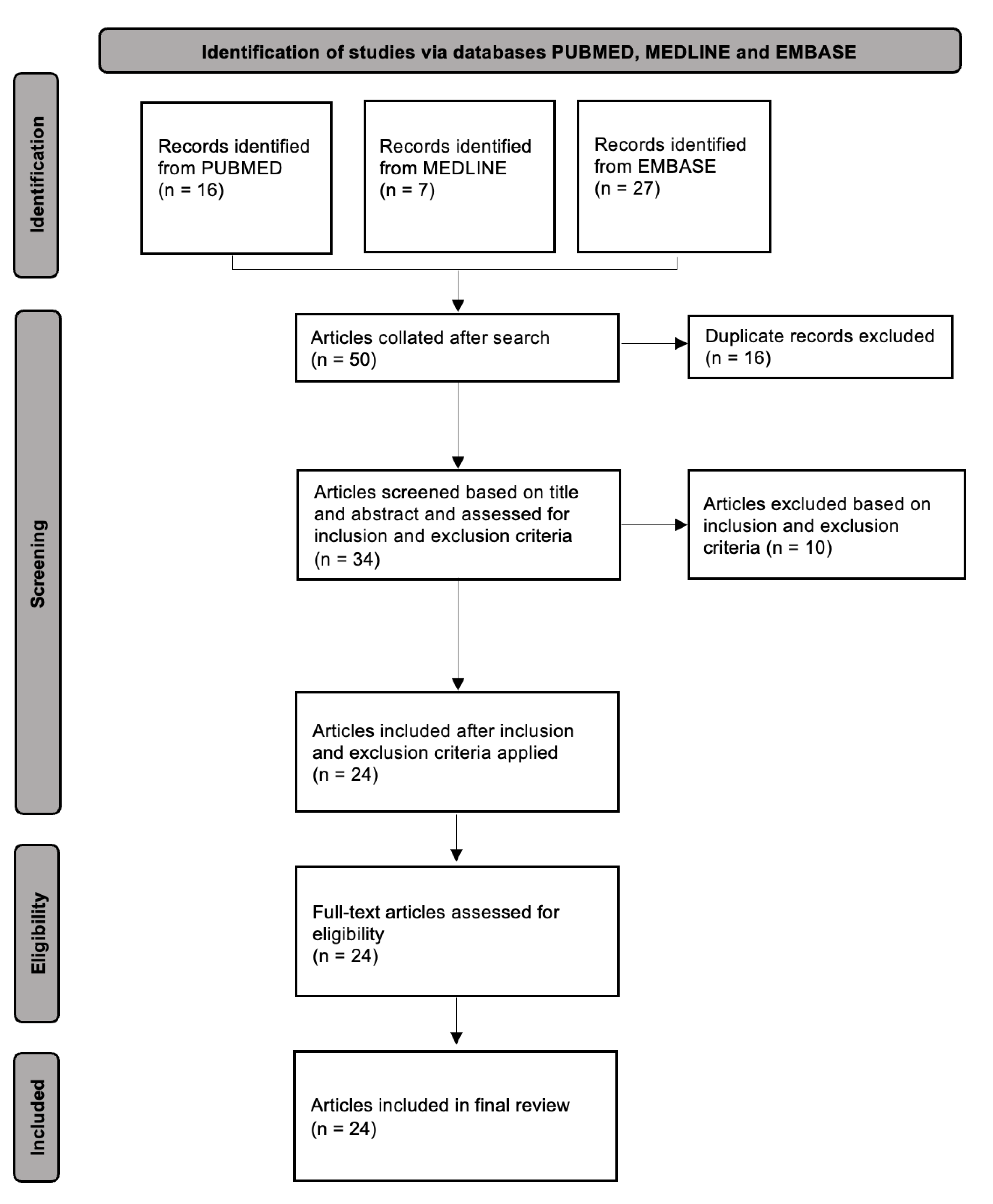
3.1. Study Selection and Characteristics
3.2. Patient Characteristics and Clinical Presentation
3.3. Diagnostic Procedures and Pathologic Findings
3.4. Treatment and Outcomes
3.5. Quality of Included Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Bryan, R.L.; Newman, J.; Campbell, A.; Fitzgerald, G.; Kadow, C.; O’Brien, J.M. Granulomatous prostatitis: A clinicopathological study. Histopathology 1991, 19, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Joseph, C.M.C. Xanthogranulomatous Prostatitis: Novel Presentation of a Rare Condition. Am. J. Case Rep. 2021, 22, e932869. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Sureka, S.K.; Ruidas, S.; Lal, H. Xanthogranulomatous prostatitis mimicking prostatic adenocarcinoma: A diagnostic dilemma. BMJ Case Rep. 2019, 12, e231945. [Google Scholar] [CrossRef]
- Lee, H.Y.; Kuo, Y.T.; Tsai, S.Y.; Li, C.C.; Wu, W.J.; Huang, C.H.; Juan, Y.-S. Xanthogranulomatous prostatitis: A rare entity resembling prostate adenocarcinoma with magnetic resonance image picture. Clin. Imaging 2012, 36, 858–860. [Google Scholar] [CrossRef]
- Mukendi, A.M.; Doherty, S.; Mohanlal, R. Xanthogranulomatous prostatitis: A rare mimicker of prostate adenocarcinoma. Clin. Case Rep. 2020, 8, 203–205. [Google Scholar] [CrossRef]
- Mehta, S.; Kampantais, S.; Wolfe, K.; Liyanage, S.H. Xanthogranulomatous prostatitis: Impressive MRI appearance of a rare entity. Asian J. Urol. 2020, 7, 384–386. [Google Scholar] [CrossRef]
- Tang, Y.; Yang, J.; Zhou, C.; Li, J.; Hu, S. False-positive mpMRI and true-negative 68Ga-PSMA PET/CT xanthogranulomatous prostatitis: A case report. Transl. Androl. Urol. 2022, 11, 561–566. [Google Scholar] [CrossRef]
- Xing, L.; Liu, Z.; Deng, G.; Wang, H.; Zhu, Y.; Shi, P.; Huo, B.; Li, Y. Xanthogranulomatous prostatitis with prostato-rectal fistula: A case report and review of the literature. Res. Rep. Urol. 2016, 8, 165–168. [Google Scholar] [CrossRef]
- Rafique, M.; Yaqoob, N. Xanthogranulomatous prostatitis: A mimic of carcinoma of prostate. World J. Surg. Oncol. 2006, 4, 30. [Google Scholar] [CrossRef]
- Demeter, J.; Deshmukh, A.; Salari, B.; Sindhwani, P.; Khan, O. An improbable trifecta: Occurrence of xanthogranulomatous prostatitis, prostate cancer, and prostatic abscess in a single patient. Urol. Case Rep. 2020, 35, 101526. [Google Scholar] [CrossRef]
- De Silva, S.; De Silva, L.; Sooriyaarchchi, S.; Wijesighe, H.; Ranaweera, G.; De Silva, S.; De Silva, C. Different clinical presentations of xanthogranulomatous prostatitis: A case series and review of the literature. J. Clin. Urol. 2021, 14, 293–299. [Google Scholar]
- Pastore, A.L.; Palleschi, G.; Fuschi, A.; Porta, N.; Cerbelli, B.; Di Cristofano, C.; Petrozza, V.; Carbone, A. Hematospermia and xanthogranulomatous prostatitis: An unusual onset of a rare diagnosis. Can. Urol. Assoc. J. 2013, 7, E820–E822. [Google Scholar]
- Karzoun, M.Z.; Al-Naimi, A.; Abdelfattah, O.; Ibrahim, T. Granulomatous and xanthogranulomatous prostatitis: A case report. Urol. Case Rep. 2022, 40, 101887. [Google Scholar]
- Belga, S.; Chen, W.; Low, G.; Cervera, C. Xanthogranulomatous prostatitis presenting as Pseudomonas aeruginosa prostatic abscesses: An uncommon complication after kidney transplantation. IDCases 2019, 17, e00559. [Google Scholar] [PubMed]
- Miekoś, E.; Włodarczyk, W.; Szram, S. Xanthogranulomatous prostatitis. Int. Urol. Nephrol. 1986, 18, 433–437. [Google Scholar]
- Bostwick, D.G.; Cheng, L. Urologic Surgical Pathology; Elsevier Health Sciences: Gurugram, India, 2008; 1037p. [Google Scholar]
- Cheng, Y.; Zhang, X.; Ji, Q.; Shen, W. Xanthogranulomatous prostatitis: Multiparametric MRI appearances. Clin. Imaging 2014, 38, 755–757. [Google Scholar]
- Grewal, N.; Tuli, A.; Sridhar, F.K.; Mammen, K.J. Xanthogranulomatous Prostatitis with Benign Prostatic Hyperplasia: A Rare Combination. CHRISMED J. Health Res. 2017, 4, 214. [Google Scholar]
- Jabbour, Y.; Lamchahab, H.; Harrison, S.; El Ouazzani, H.; Karmouni, T.; El Khader, K.; Koutani, A.; Andaloussi, A.I.A. Prostatic Abscess on Xanthogranulomatous Prostatitis: Uncommon Complication of an Uncommon Disease. Case Rep. Urol. 2018, 2018, 5417903. [Google Scholar]
- Min, K.S.; Oh, S.Y.; Chun, J.Y.; Um, J.D.; Choi, S.H.; Jung, S.J. A Case of Xanthogranulomatous Prostatitis Concurrent with a Prostatic Abscess. Korean J. Androl. 2011, 29, 174–176. [Google Scholar]
- Noyola, A.; Gil, J.F.; Lujano, H.; Piñon, O.; Muñoz, G.; Michel, J.M.; Garcia, J.; Valdez, J.; Morales, O. Xanthogranulomatous Prostatitis, a Rare Prostatic Entity. Urol. Case Rep. 2016, 10, 4–5. [Google Scholar]
- Patil, N.; Kundargi, V.S.; Patil, S.B.; Biradar, A.K.; Desai, A.S. Xanthogranulomatous Prostatitis: A Rare Case Report. Med. Surg. Urol. 2014, 3, 1. Available online: https://www.omicsonline.org/open-access/xanthogranulomatous-prostatitis-a-rare-case-report-2168-9857.1000131.php?aid=25027 (accessed on 30 September 2024).
- Shukla, P.; Gulwani, H.V.; Kaur, S. Granulomatous prostatitis: Clinical and histomorphologic survey of the disease in a tertiary care hospital. Prostate Int. 2017, 5, 29–34. [Google Scholar] [PubMed]
- Valsangkar, R.S.; Singh, D.P.; Gaur, D.D. Xanthogranulomatous prostatitis: Rare presentation of rare disease. Indian J. Urol. 2012, 28, 204–205. [Google Scholar] [PubMed]
- Wollin, D.A.; Brucker, B.M. Dramatic Enlargement of the Prostate due to Xanthogranulomatous Inflammation. Low. Urin. Tract Symptoms 2015, 7, 166–168. [Google Scholar]
- Zaber, K.; Al-Bareeq, R. Xanthogranulomatous prostatitis causing entero-vesical fistula. Bahrain Med. Bull. 2004, 26, 165–166. [Google Scholar]
| Author and Year | No. of Cases | Age | Presentation | PSA (ng/mL) | Initial Clinical Diagnosis | Indication for Management | Management |
|---|---|---|---|---|---|---|---|
| Miekos 1986 | 2 | 58 | Anuria | NA | BPE | Symptoms. No biopsy. | Simple prostatectomy |
| 46 | Flank pain + LUTS | NA | BPE | Symptoms. Biopsy negative. | TURP | ||
| Zaber 2004 | 1 | 63 | AUR, diarrhoea, faecaluria | 2.2 | Enterovesical fistula | Symptoms. No biopsy. | TURP |
| Rafique 2006 | 1 | 60 | LUTS | 150 | PCa | Symptoms. No biopsy. | TURP |
| Min 2011 | 1 | 82 | Haematuria, LUTS + AUR | 86.8 | BPE | Symptoms. No biopsy. | TURP |
| Lee 2012 | 1 | 74 | LUTS | 11.74 | PCa | Biopsy-proven XGP. | Alpha blocker |
| Valsangkar 2012 | 1 | 52 | AUR + fevers | NA | Prostate abscess | Abscess deroofing. No biopsy. | TURP |
| Pastore 2013 | 5 | Range: 51–62 | Haematospermia, LUTS + fever | 4.8–6.7 | PCa | Symptoms + obstructive uroflowmetry. Biopsy-proven XGP. | TURP |
| Patil 2014 | 1 | 64 | LUTS | 15 | BPE | Symptoms + obstructive uroflowmetry. | TURP |
| Cheng 2014 | 2 | 60 | LUTS | 6.5 | Prostatitis | NA. | NA |
| 71 | LUTS + haematuria | 5.5 | Prostatitis | Biopsy-proven-XGP. | Antibiotics | ||
| Wollin 2015 | 1 | 78 | Recurrent urinary retention | 41.4 | BPE | Ongoing symptoms. Biopsy negative. | Simple prostatectomy |
| Xing 2016 | 1 | 75 | LUTS | 172.5 | PCa | Biopsy-proven XGP. | Alpha blocker |
| Noyola 2016 | 1 | 47 | LUTS | 0.4 | BPE | Symptoms. No biopsy. | Simple prostatectomy |
| Grewal 2017 | 1 | 54 | LUTS | 0.013 | BPE | Symptoms. No biopsy. | TURP |
| Shukla 2017 | 2 | 65 | Dysuria | 8.85 | PCa | NA. | TURP |
| 69 | LUTS | NA | BPE | NA. | TURP | ||
| Jabbour 2018 | 1 | 59 | LUTS | 0.54 | Prostate abscess | Abscess deroofing. | TURP |
| Kumar 2019 | 1 | 57 | LUTS | 11.59 | PCa | Raised PSA, symptoms. Biopsy prostate adenocarcinoma later revised to XGP. | Radical prostatectomy |
| Mukendi 2019 | 1 | 71 | Asymptomatic | 9.5 | PCa | Biopsy-proven XGP. | Alpha blocker |
| Belga 2019 | 1 | 70 | Septic shock | NA | Prostate abscess | Abscess deroofing. | TURP + antibiotics |
| Mehta 2020 | 1 | 60 | Fevers + dysuria | 0.8 | PCa | Biopsy-proven XGP. | Antibiotics |
| Demeter 2020 | 1 | 65 | LUTS | 1.23 | PCa | Abscess drainage. Biopsy-proven XGP. | Abscess aspiration + antibiotics |
| De Silva 2020 | 3 | 68 | LUTS | 5.3 | PCa | Symptoms + obstruction upon uroflowmetry. No biopsy. | TURP |
| 82 | LUTS | 324 | PCa | Symptoms. No biopsy. | TURP | ||
| 69 | LUTS | 1 | BPE | Symptoms. No biopsy. | TURP | ||
| Karzoun 2021 | 1 | 63 | LUTS | 1.7 | BPE | Symptoms + obstruction upon uroflowmetry. | TURP |
| Joseph 2021 | 1 | 65 | Rectal pain | 2.4 | PCa | Biopsy-proven XGP. | Antibiotics |
| Tang 2022 | 1 | 56 | Dysuria | 49.19 | PCa | Biopsy-proven XGP. | Antibiotics |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Société Internationale d’Urologie. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chew, K.K.Y.; Mak, G.C.H.; Wong, E.L.H. Xanthogranulomatous Prostatitis: A Systematic Review. Soc. Int. Urol. J. 2025, 6, 26. https://doi.org/10.3390/siuj6020026
Chew KKY, Mak GCH, Wong ELH. Xanthogranulomatous Prostatitis: A Systematic Review. Société Internationale d’Urologie Journal. 2025; 6(2):26. https://doi.org/10.3390/siuj6020026
Chicago/Turabian StyleChew, Kenneth Keen Yip, Gerald Chin Ho Mak, and Eddy Lee Hao Wong. 2025. "Xanthogranulomatous Prostatitis: A Systematic Review" Société Internationale d’Urologie Journal 6, no. 2: 26. https://doi.org/10.3390/siuj6020026
APA StyleChew, K. K. Y., Mak, G. C. H., & Wong, E. L. H. (2025). Xanthogranulomatous Prostatitis: A Systematic Review. Société Internationale d’Urologie Journal, 6(2), 26. https://doi.org/10.3390/siuj6020026






