Abstract
The inspection of the urethra in patients with documented or suspected urethral stricture should be carried out with small caliber ureteroscope of 6/7.5Ch. Different from flexible cystoscope (16Ch) or resectoscope (26Ch), small caliber ureteroscope allows a comprehensive evaluation of the stricture, including its length and the status of the mucosa in its proximity, without injuring or overstretching the urethra. With a small caliber ureteroscope it is also possible to cross the stricture, allowing the evaluation of the proximal urethra, the external urethral sphincter, and the bladder. A 6/7.5Ch ureteroscope also allows estimation of the real caliber of the stricture, providing a useful landmark for further treatment decisions.
As members of the reconstructive urology community and experts in the field of urethroplasty, it is our duty not only to discover new surgical techniques[1] but also to provide advice that can change our daily practice to the advantage of our patients. In this regard, we are honored to share our view of the correct management of patients with urethral stricture. We believe the assessment of patients with urethral stricture starts with the appropriate and judicious evaluation of the urethra. In a patient complaining of poor flow, when the urethrogram shows a narrowing along the urethra, the choice of the right endoscopic instrument for inspection is pivotal. Based on our long experience of urethroplasty and urethral disease management, we recommend the use of a small caliber ureteroscope to inspect the urethra. Specifically, a 6/7.5Ch ureteroscope; the first digit refers to the size of the ureteroscope at the tip and the second to the size of the instrument at the base.
The normal caliber of the bulbar urethra is 30Ch[2], which means that the diameter is around 1cm. A resectoscope, which is commonly adopted for transurethral resection of the prostate, is 26Ch, and flexible cystoscopes are approximately 16Ch. According to Smith et al.[3], urethral strictures become symptomatic (ie, require dilatation and antibiotic treatment) when the urine flow is below 7mL/min, which corresponds approximately to a urethral caliber below 16Ch. In other words, when patients come for initial evaluation, the urethral lumen, at the level of the stricture, typically does not allow “common” instruments to go across the stricture (Figure 1).

Figure 1.
The choice of the correct instrument according to the different sizes of urethra. Kulkarni’s flow chart for urethroplasty techniques according to stricture characteristics.
The 6/7.5Ch ureteroscope was introduced into urological practice more than 10 years ago. Since then, it has been employed mainly for stone management [4] and/or pediatric urology [5], and its use has not been popularized among reconstructive urologists. Nonetheless, we believe that small caliber ureteroscope should become the gold standard for the inspection of the urethra in patients referred for stricture management. First and foremost, it decreases the risk of injuring the urethra. Indeed, the 6/7.5Ch ureteroscope allows the surgeon to navigate the urethra away from the urethral walls, preventing accidental injury of the mucosa. It also avoids trauma to the surrounding spongy tissue, preventing over-distension and stretching. Second, a small caliber ureteroscope may allow close-up visualization of the stricture and may enable visualization across the length of the stricture. This second aspect is very important, especially for planning the subsequent treatment. Indeed, retrograde and anterograde urethrograms may underestimate the real complexity of the stricture (Video 1). In particular, retrograde and anterograde urethrograms may not always give a realistic representation of either the extension or the severity of the urethral stricture. Moreover, urethrograms do not provide information on the status of the mucosa across and in proximity to the stricture (Figure 2). Assessing the real length of the stricture and the status of the surrounding mucosa is pivotal in patients with lichen sclerosus or any non-traumatic etiologies, which may involve longer segments of the urethra. Surgical decision- making may change considerably depending on the length of the stricture or the aspect of the forthcoming urethral mucosa. For instance, the choice of end-to-end anastomosis, augmented urethroplasty, or stricturoplasty can be made only with knowledge of the extension of the stricture and the status of the urethra before and after the stricture. This vital information can be acquired only with a full inspection of the urethral lumen. In our experience, the estimation of stricture length is more accurate when it is carried out with the endoscopic view rather than urethrograms. Indeed, the endoscopic findings more frequently match with the surgical view. Only with the use of these small caliber instruments does the surgeon have the advantage of a comprehensive evaluation of the urethra for planning the correct treatment. Third, only small ureteroscope may give access to false passage or fistulae encountered during the inspection of the urethra with minimal risk of extravasation or perforation. The latter is extremely important in patients referred for redo surgery, pelvic fracture urethral injury, or stricture related to infection with concomitant abscess. Fourth, with a small caliber ureteroscope it is possible to cross the stricture reaching the proximal urethra and the bladder. This opportunity is of paramount importance, especially to rule out the presence of stones or neoplasms, which can radically change the management of the patient. The use of small caliber ureteroscope is particularly advantageous in female patients. To rule out the presence of stricture in women, the inspection of the urethra must be carried out with great care and attention because the female urethra is short, poorly distensible, and has great mobility. Larger caliber instruments are inappropriate for this task because they do not allow a comprehensive evaluation of the length and severity of the stricture. Indeed, larger caliber instrument may be unable to enter the meatus when fibrotic or, when the stricture is more proximal, they may overstretch the urethra, hiding the presence of the stenosis and its extension. Last but not least, small caliber instruments provide a useful calibration of the urethral lumen to determine the most appropriate urethroplasty technique. According to our personal flow chart (Figure. 1), a stricture which allows only a 6/7.5Ch ureteroscope can be approached with augmented urethroplasty following the Barbagli[6] or Kulkarni[7] principles. Conversely, an obliterated or semi-obliterated stricture (<3 Ch) can be repaired with anastomotic urethroplasty when secondary to trauma, or with non-transecting approaches (including double face [8], mucosa-to-mucosa [9], augmented non- transecting anastomotic urethroplasty [10]), graft plus flap or two-stage urethroplasty when secondary to non- traumatic etiologies. Finally, we acknowledge that the use of small caliber ureteroscope can be challenging at the beginning because of the difficulties of handling and maneuvering this long and thin instrument, as well as the suboptimal view. However, we believe that the great benefit derived from its use justifies the effort needed for the learning curve.
VIDEO 1.
Patient with distal anastomotic stenosis after dorsal onlay BMG urethroplasty. The 6/7.5Ch ureteroscope was able to cross the stricture and to allow the inspection of the proximal urethra.
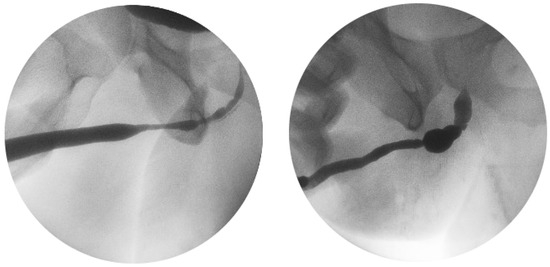
Figure 2.
Examples of retrograde urethrograms where length and characteristics of the strictures cannot be assessed without endoscopic inspection.
In summary, we suggest that all reconstructive urologists dealing with urethroplasty consider discontinuing the use of flexible or rigid cystoscopes with caliber above 16Ch. Instead, we recommend they embrace a small caliber ureteroscope (6/7.5Ch) for the evaluation of the urethra in patients, male or female, with a confirmed or suspected diagnosis of urethral stricture, before surgery.
Conflicts of Interest
None declared.
References
- Barbagli, G.; Bandini, M.; Balò, S.; Sansalone, S.; Butnaru, D.; Lazzeri, M. Surgical treatment of bulbar urethral strictures: tips and tricks. Int Braz J Urol. 2020, 46, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Brandes, S.B.; Morey, A.F. (Eds.) . Advanced Male Urethral and Genital Reconstructive Surgery; SpringerLink: Berlin/Heidelberg, Germany, 2004. [Google Scholar]
- Smith, J.C. The measurement and significance of the urinary flow rate. Br J. Urol. 1966, 38, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Francesca, F.; Scattoni, V.; Nava, L.; Pompa, P.; Grasso, M.; Rigatti, P. Failures and complications of transurethral ureteroscopy in 297 cases: conventional rigid instruments vs. small caliber semirigid ureteroscopes. Eur Urol. 1995, 28, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Phillips, T.M.; Mathews, R.I. Operative management of pediatric urolithiasis. Indian J. Urol. 2010, 26, 536–543. [Google Scholar] [PubMed]
- Barbagli, G.; Montorsi, F.; Guazzoni, G.; Larcher, A.; Fossati, N.; Sansalone, S.; et al. Ventral oral mucosal onlay graft urethroplasty in nontraumatic bulbar urethral strictures: surgical technique and multivariable analysis of results in 214 patients. Eur Urol. 2013, 64, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.; Barbagli, G.; Sansalone, S.; Lazzeri, M. One-sided anterior urethroplasty: a new dorsal onlay graft technique. BJU Int. 2009, 104, 1150–1155. [Google Scholar] [CrossRef] [PubMed]
- Palminteri, E.; Manzoni, G.; Berdondini, E.; Di Fiore, F.; Testa, G.; Poluzzi, M.; et al. Combined dorsal plus ventral double buccal mucosa graft in bulbar urethral reconstruction. Eur Urol. 2008, 53, 81–89 https:// doiorg/101016/jeururo200705033. [Google Scholar] [CrossRef] [PubMed]
- Andrich, D.E.; Mundy, A.R. Non-transecting anastomotic bulbar urethroplasty: A preliminary report. BJU Int. 2012, 109, 1090–1094. [Google Scholar] [CrossRef] [PubMed]
- Welk, B.K.; Kodama, R.T. The augmented nontransected anastomotic urethroplasty for the treatment of bulbar urethral strictures. Urology 2012, 79, 917–921. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2021 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.