Abstract
On behalf of Society ÖGSF and the Swiss Stroke Society SHG, we are pleased to present the Abstracts of the Annual Meeting that was held from 14–15 June 2022 in Innsbruck/Austria. Twenty (20) abstracts were selected for presentation as oral presentations and sixteen (16) abstracts were selected as poster presentations. We congratulate all the presenters on their research work and contribution.
- All abstracts and information are published as submitted by the authors and are not the responsibility of the CTN journal (Clinical and Translational Neuroscience) or the meeting organizer.
- O01–O20 Oral Presentations
- P01–P17 Poster Presentations
- O01
- Implementation of a Guideline for Prevention, Recognition and Treatment of Delirium in a Stroke Unit
1
Stroke Unit, Inselspital, University Hospital Bern, Switzerland
2
Berner Fachhochschule Departement Gesundheit, Bern, Switzerland
- Background: In March 2020, our institution published an “evidence-based treatment-guiding document” (ETD) for delirium. Such documents have to be adapted by nursing experts to specific departments and units. This adaptation is presented to the hospital management, and then implemented in the various units. Our goal was to integrate the collaborators in the decision process, in the guideline adaptation and in the implementation in the stroke unit from the onset of the ETD implementation.
- Methods: We created and mandated a project group with interested stroke team members to review the delirium management in our stroke unit. This group had to select tools for delirium screening, for delirium prevention, and for methods of implementation. After selecting specific methods, we disseminated them through bedside teaching, and later evaluated the guideline with a qualitative and quantitative questionnaire.
- Results: The project group was able to adapt the content of the institutional ETD to the stroke unit’s needs, and to teach it to the collaborators. The questionnaires indicated a visible and positive effect on patients since the introduction of this tool. The collaborators were capable to integrate the selected tools in their daily routine.
- Conclusions: The members of this project group successfully implemented an institutional delirium guideline in the stroke unit. They became the main promoters for its propagation and will guarantee the continuity of its use. Limited time resources and availability of the nursing personnel made bedside teaching difficult, however.
- O02
- Elaboration of a Laxative Protocol for a Stroke Center in Switzerland
1
Stroke Center and Department of Nursing Development, Cantonal Hospital St. Gallen, Switzerland.
2
Institute of Nursing Science and Practic, Paracelsus Medical University, Salzburg, Austria
- Background: Bed rest, immobilisation, dysphagia and dehydration after stroke increase the risk of constipation. There are multiple potential therapeutic products with variable indications and ways of application. Furthermore, treatment team (nurses, doctors) and patients have variable preferences regarding pharmacological and non-pharmacological interventions for the treatment of constipation.
- Goals: Our goal was to establish a unified laxative protocol for the Stroke Center (SC) at Kantonsspital St.Gallen (KSSG), in order to increase the autonomy of the nurses regarding treatment adapted to the individual patient. First-line laxatives should have a favourable side effect profile, few contraindications, and a particular suitability for stroke patients.
- Methods: We performed a literature search of English and German publications on existing and/or scientifically investigated laxative protocols and treatments. In addition, we contacted other Stroke Units (SU) and SC from the Swiss Stroke Nursing Network in order to obtain their protocols and recommendations.
- Results: There were few articles in English or German regarding bowel movement or management of constipation after stroke. The existing literature focused mainly on acupuncture and moxa-therapy. We were able to obtain some guidance from laxative protocols of other Swiss SU and SC.
- Implementation: We tested our newly established laxative protocol in the neurovascular intensive care unit at KSSG during three months. We found a high acceptance rate by the treatment team. As a result, we extended the protocol use to the entire SC.
- Conclusion: The new laxative protocol is now used in our SC on a routine basis and allows for a constipation therapy tailored to the patient’s needs. Nurses tend to obtain a bowel transit and defecation history more often. Interventions were found to focus more on laxatives than on non-pharmacological treatments.
- O03
- Serum S-100B Adds Incremental Value for the Prediction of Symptomatic Intracranial Hemorrhage and Brain Edema After Acute Ischemic Stroke: Data from the Multicentre BIOSIGNAL-Cohort Study
1
Department of Neurology, University Hospital Zurich, Switzerland
2
Department of Neurology Inselspital University of Berne, Switzerland
3
Department of Neurology and Stroke Center University Hospital Basel, Switzerland
4
Department of Neurology, Kantonsspital Aarau, Switzerland
5
Stroke Center, Neurocenter of Southern Switzerland (NSI), Ospedale Regionale di Lugano, Switzerland
6
Department of Neurology, Kantonsspital St. Gallen, Switzerland
7
Neurovascular Research Laboratory, Vall d’Hebron Institute of Research (VHIR) Barcelona; Institute de Bio medicine of Seville, IBiS/Hospital Universitario Virgen del Rocío/CSIC/University of Seville & Department of Neurology, Hospital Universitario Virgen Macarena, Seville, Spain
8
Stroke Unit, Hospital Universitari Germans Trias i Pujol, Badalona, Barcelona, Spain
9
Neurovascular Research Laboratory, Vall d’Hebron Institute of Research (VHIR)-Universitat Autònoma de Barcelona, Barcelona, Spain
10
Department of Internal Medicine, University of Thessaly Larissa, Greece
11
Department of Neurology, Goethe University Frankfurt, Germany
12
Institute of Clinical Chemistry, University Hospital Zurich, Switzerland
†
Equally contributing authors.
- Background and Purpose: Early identification of patients developing symptomatic intracranial hemorrhage (sICH) and symptomatic brain edema (sBE) after acute ischemic stroke (AIS) is essential for clinical decision-making. Astroglial protein S-100B is a marker of blood-brain barrier (BBB) disruption, which plays a role in the formation of sICH and sBE. In this study, we assessed the prognostic value of serum S-100B for the development of sICH and sBE.
- Methods: Serum S-100B levels were measured on admission (within 24 h from symptom onset) in 1749 consecutive AIS patients from the multicenter BIOSIGNAL cohort study (mean age 72.0 years, 58.3% male). To determine sICH or sBE, follow-up neuroimaging was routinely performed in all patients receiving re-canalisation therapy or experiencing significant clinical worsening defined as an NIHSS increase of ≥4 during hospital stay.
- Results: Of the 1749 consecutively enrolled patients, 46 (2.6%) developed sICH and 90 (5.2%) developed sBE. After adjustment for established risk-factors, S-100B levels remained independently associated with both sICH (OR 3.41, 95%CI 1.7–6.9, p = 0.001) and sBE (OR 4.08, 95%CI 2.3–7.1, p < 0.001) in multivariable logistic regression models. Adding S-100B to the best clinical prediction model led to an improvement of AUC from 0.72 (95%CI 0.65–0.78) to 0.75 (95%CI 0.68–0.82) (p = 0.001) for sICH and from 0.78 (95%CI 0.73–0.83) to 0.81 (95%CI 0.76–0.86) (p < 0.0001) for sBE (Figure 1).
- Conclusion: Serum S-100B levels are independently associated with the development of sICH and sBE adding incremental prognostic value in AIS patients. Thus, S-100B may be clinically useful for early risk-stratification regarding acute stroke complications.
- O04
- Occurrence of No-Harm Incidents and Adverse Events in Hospitalized Patients with Ischemic Stroke or TIA: A Cohort Study Using Trigger Tool Methodology
Departementsfachleitung Pflege, Departement Kopforgane, Wirbelsäulen- und Neuromedizin, Universitätsspital Basel, Switzerland
- Background:Adverse events (AEs) -healthcare caused events leading to patient harm or even death- are common in healthcare. Systematic knowledge on this phenomenon in stroke patients is limited.
- Aim: To determine cumulative incidence of no-harm incidents and AEs, including their severity and preventability.
- Method: A cohort study using trigger tool methodology for retrospective record review was designed and carried out in a German speaking stroke center. Electronic records from 150 randomly selected patient admissions for TIA or ischemic stroke, with or without acute recanalization therapy, were used.
- Results: Totally, 170 events (108 AEs and 62 no-harm incidents) were identified, affecting 83 patients (55.3%; 95% CI 47 to 63.4), corresponding to an event rate of 113 events/100 admissions or 142 events/1000 patient days. The three most frequent AEs were ischemic strokes (n = 12, 7.1%), urinary tract infections (n = 11, 6.5%) and phlebitis (n = 10, 5.9%). The most frequent no-harm incidents were medication events (n = 37, 21.8%). Preventability ranged from 12.5% for allergic reactions to 100% for medication events and pressure ulcers. Most of the events found (142; 83.5%; 95% CI 76.9 to 88.6) occurred throughout the whole stroke care.
- Conclusions: Trigger tool methodology allows detection of AEs and no-harm incidents, showing a frequent occurrence of both event types during stroke care. Further investigations into events’ relationships with organizational systems and processes will be needed, first to achieve a better understanding of these events’ underlying mechanisms and risk factors, then to determine efforts needed to improve patient safety.
- O05
- Stroke in the Stroke Unit: Recognition, Treatment and Outcomes in a Single-Center Cohort
1
Neurology Service, Hospital de Egas Moniz, Centro Hospitalar Lisboa Ocidental, Lisbon, Portugal
2
Stroke Center, Neurology Service, Lausanne University Hospital and University of Lausanne, Switzerland
- Background and Purpose: In-hospital strokes (IHS) are associated with longer diagnosis times, treatment delays, and poorer outcomes. Strokes occurring in the stroke unit have seldom been studied. Our aim is to assess the quality of management of in-stroke unit ischemic stroke (ISUS) in our institution.
- Methods: Consecutive patients from the Acute Stroke Registry and Analysis of Lausanne registry, from January 2003 to June 2019, were classified as ISUS, other-IHS or community-onset stroke (COS). Baseline and stroke characteristics of patients, time-to-imaging and -to treatment, missed treatment opportunities, treatment rates and outcomes were compared using multivariate analysis.
- Results: Among the 3456 patients analyzed, 138 (4.0%) were ISUS, 214 (6.2%) other-IHS and 3104 (89.8%) COS. In multivariate analysis, patients with ISUS more frequently had known stroke onset-time than other-IHS (adjusted odds ratio [aOR] 2.44; 95% confidence interval [CI] 1.39–4.35) or COS (aOR 2.56; 95% CI 1.59–4.17), had less missed treatment opportunities than other-IHS (aOR 0.22; 95% CI 0.06–0.86) and higher endovascular treatment rates than COS (aOR 3.03; 95% CI 1.54–5.88). ISUS were associated with a favorable shift in the modified Rankin Scale at 3 months in comparison with other-IHS (aOR 1.73; 95% CI, 1.11–2.69) or COS (aOR 1.46; 95% CI, 1.00–2.12).
- Conclusions: ISUS more frequently had known stroke onset-time than other-IHS or COS, less missed treatment opportunities than other-IHS and a higher endovascular treatment rate than COS. This readiness to identify and treat patients in the stroke unit may explain the better longterm outcome of ISUS.
- O06
- Mental Imagery in Gait Rehabilitation After Stroke—A Pilot Study
Department of Neurology, St. John’s Hospital, Vienna, Austria
- Background: Many patients show motor deficits in the early phase after a stroke. They are dependent in their daily living (ADL’s) and restricted in their walking abilities. Mental imagery is a method where patients can work independently on their walking skills.
- Objective: The aim of this pilot study is to verify the feasibility of mental imagery in the early phase after stroke. Additionally, the effects of mental imagery on the motor functions of the lower extremities and in particular on the recovery of the ability to walk shall be tested.
- Methods: This single-center randomized pilot study included eight study participants. Mental imagery training was applied to the intervention group (n = 4) for 15 min five times a week for four weeks additionally to the standard physiotherapy (30 min). The control group (n = 4) had 45 min of regular physiotherapy five times a week. The primary outcome variable was the Functional Ambulation Category (FAC) to assess the functional walking ability. To measure the postural control and the ability of mental imagery, the Berg Balance Scale (BBS) and the Kinesthetic and Visual Imagery Questionnaire (KVIQ-10) were applied as secondary outcome measures.
- Results: The feasibility of mental imagery training for a larger randomized controlled trial is confirmed. It has a positive effect on the recovery of the walking abilities, but due to the small study population, no statistically significant statement can be made.
- Conclusions: Mental imagery training is a low-cost, fast, and easy method to integrate in the everyday practice. It requires further investigation in order to make statistically relevant statements.
- O07
- Aphasia Profiles and Trajectories in Acute Ischemic Stroke: An Observational Study
1
Stroke Center, Neurology Service, Department of Clinical Neurosciences, Lausanne University Hospital, Bugnon 46, 1011 Lausanne, Switzerland
2
Neuropsychology and Neurorehabilitation Service, Department of Clinical Neurosciences, Lausanne University Hospital, Bugnon 46, 1011 Lausanne, Switzerland
- Background: In acute ischemic stroke (AIS), long term impact comes also from neurpsychological impairments such as aphasia, insufficiently considered in research. We studied pure aphasic AIS patients, their short-term aphasiological course, predictors of persisting aphasia, and poor long-term outcome.
- Methods: In ASTRAL Registry, all AIS patients from 2003–2019 were included. We assessed pure aphasic AIS in acute phase, and reviewed neuropsychological examination in subacute phase at 3–10 days. We identified factors associated with persistent significant aphasia in the subacute phase, and predictors of unfavourable functional outcome at 3 months (mRS ≥ 2), using multivariate analyses (MVA).
- Results: Among 4513 consecutive AIS, 131 (2.9%) had pure aphasia at admission. 81 had a good quality neuropsychological examination and were analysed (median age 76.3; 44.4% females; 6.2% left-handed; 24.7% treated with intravenous thrombolysis; 2.5% with endovascular treatment. 28.4% still had significant aphasia in the subacute phase. In MVA, persistent aphasia patients had more cardioembolic (OR 15.6; 95%CI 1.9–123.8) and atheromatous (OR 17.5; 95%CI 1.7–181.1) strokes. At 3months, unfavourable outcome was predicted by female sex (OR 4.6; 95%CI 0.9–21.7) and significant aphasia in the subacute phase (OR 8.8; 95%CI 1.6–47.8).
- Conclusions: Pure aphasia is present in 2.9% of AIS, and resolves in 2/3 at 3–10 days. Persistent aphasia is associated with embolic mechanisms, and poor outcome with female sex and persistent aphasia. These data may help with prognostication, rehabilitation planning and studying the effects of more aggressive revascularisation treatment in purely aphasic stroke patients.
- O08
- Providing Neurorehabilitation at Home During COVID-19 Pandemic Using Telehealth Mediated Dtx Solution: A Pilot Feasibility Study
1
MindMaze SA, Lausanne, Switzerland
2
Department of Clinical Neurosciences, Lausanne University Hospital, Switzerland
- Introduction: During the COVID-19 pandemic, most of outpatient services were suspended, disturbing the continuum of care in the rehabilitation process for neurological patients. Tech-enhanced neurorehabilitation can provide a suitable and feasible solution for clinicians to increase patient rehabilitation time on task and provide appropriate monitoring.
- Methods: MindMotion™ GO is a versatile medical device that accounts 26 activities designed for motor neurorehabilitation of upper limb, lower limb, trunk and hand. Devices uses Kinect camera and Leap Motion system to quantify the patients motion. 3 patients (2 stroke, 1 multiple sclerosis) were given the device to continue performing rehabilitation at home over a 4-week period during the COVID-19 pandemic. Therapists used an online platform to prescribe rehabilitation programs and monitor the patient progress. Patient and Ttherapist usage, and structured feedback was assessed.
- Results: The three patients used the device on average (mean) 14h07 during the 4 weeks, and 32 min per day, applying 4 activities per session. The average (mean) adherence was 72%. The structured feedback questionnaire showed that all three patients found the device easy to install and use. The three therapists also perceived a clinical value in adding remote therapy in the practice.
- Conclusions: This study demonstrated the feasibility and ease of the usage of the MindMotion™ GO system for remote therapy both for patients and for therapists. The tool gave the possibility to administer high dosage and high adherence rehabilitation services during the COVID-19 pandemic. Further study of this model of care is ongoing.
- O09
- Once Versus Twice Daily Direct Oral Anticoagulants in Patients with Recent Stroke and Atrial Fibrillation
1
Department of Neurology and Stroke Center, University Hospital Basel and University of Basel, Basel, Switzerland
2
Neurology and Neurorehabilitation, University Department of Geriatric Medicine Felix Platter, University of Basel, Basel, Switzerland
3
Department of Intensive Care Medicine, University Hospital Basel and University of Basel, Basel, Switzerland
4
Department of Neurology, Inselspital University Hospital and University of Bern, Switzerland
5
Medical Faculty, University of Basel, Basel, Switzerland
6
Stroke Center, Klinik Hirslanden Zurich, Zurich, Switzerland
†
Shared senior authorship.
- Background: Data on the safety and effectiveness of once-daily (QD) versus twice-daily (BID) direct oral anticoagulants (DOAC) in comparison to vitamin K antagonists (VKA) and to one another in patients with atrial fibrillation (AF) and recent stroke are scarce.
- Patients and Methods: Based on prospectively obtained data from the observational registry Novel-Oral-Anticoagulants-in-Ischemic-Stroke-Patients(NOACISP)-LONGTERM (NCT03826927) from Basel, Switzerland, we compared the occurrence of the primary outcome—the composite of recurrent ischemic stroke, major bleeding and all-cause death—among consecutive AF patients treated with either VKA, QD DOAC or BID DOAC following a recent stroke using Cox proportional hazards regression including adjustment for potential confounders.
- Results: We analyzed 956 patients (median age 80 years, 46% female), of whom 128 received VKA (13.4%), 264 QD DOAC (27.6%) and 564 BID DOAC (59%). Over a total follow-up of 1596 patient-years, both QD DOAC and BID DOAC showed a lower hazard for the composite outcome compared to VKA (adjusted HR [95%-CI] 0.71 [0.49,1.04] and 0.69 [0.49,0.95], respectively). Upon direct comparison, the hazard for the composite outcome did not differ between patients treated with QD versus BID DOAC (adjusted HR [95%-CI] 0.95 [0.71,1.29]). Secondary analyses focusing on the individual components of the composite outcome revealed no clear differences in the risk-benefit profile of QD versus BID DOAC.
- Discussion and Conclusions: The overall benefit of DOAC over VKA seems to apply to both QD and BID DOAC in AF patients with a recent stroke, without evidence that one DOAC dosing regimen is more advantageous than the other.
- O10
- Mechanical Thrombectomy in Acute Stroke Patients with Moderate to Severe Pre-Stroke Disability
1
Department of Neurology, St. John’s Hospital, Vienna, Austria
2
Medical Faculty, Sigmund Freud University Vienna, Vienna, Austria
3
Stroke Center, Neurology Service, Department of Clinical Neurosciences, Lausanne University Hospital and University of Lausanne, Switzerland
4
Gesundheit Österreich GmbH/BIQG, Vienna, Austria
5
Research Unit of Computational Statistics, University of Technology, Vienna, Austria
6
Department of Neurology, Medical University of Graz, Austria
7
Division of Neuroradiology, Vascular and Interventional Radiology, Department of Radiology, Medical University of Graz, Austria
8
Department of Neuroradiology, Medical University of Innsbruck, Innsbruck, Austria
9
Neuroimaging Research Core Facility, Medical University of Innsbruck, Innsbruck, Austria
10
Department of Radiology, St. John’s Hospital, Vienna, Austria
- Background and Purpose: There are limited data on mechanical thrombectomy (MT) in acute ischemic stroke (AIS) patients with preexisting disability. We aimed to compare functional and safety outcomes of AIS patients with pre-stroke disability treated with MT compared to those receiving best medical treatment.
- Methods: From the Austrian Stroke Unit registry and the ASTRAL registry, we included all consecutive acute ischemic stroke patients with pre-stroke disability, defined as modified Rankin Score (mRS) ≥3, and acute intracranial large vessel occlusion (LVO). Patients undergoing MT were compared to those receiving best medical treatment (BMT) by means of univariate and multivariate logistic regression analysis.
- Results: We included in the study 462 AIS patients with pre-stroke mRS ≥3 and LVO. Among them, 175 underwent MT and 287 received BMT. Patients with MT were younger, had more severe strokes and lower pre-stroke mRS, but similar proportion of treatment with intravenous thrombolysis. On multivariate analysis, MT was associated with a higher probability of returning to baseline mRS at 3 months (aOR 2.5, CI 1.4–4.5) and early neurological improvement ≥8 NIHSS points (aOR 2.6, CI 1.4–4.9), as well as to a lower probability of 3-month poor outcome (aOR 0.4, CI 0.2–0.7) and mortality (aOR 0.3, CI 0.2–0.5).
- Conclusions: Patients with pre-stroke mRS ≥3 treated with mechanical thrombectomy had better short-term and 3-month outcomes. This suggests that pre-stroke disability alone should not be a reason to withhold MT, but that individual case-by-case decisions may be more appropriate.
- O11
- Incomplete Recanalization and Complications Related to Early Vs. Late Endovascular Treatment in Ischemic Stroke: Frequency, Predictors and Clinical Implications
1
Stroke Center, Neurology Service, Department of Clinical Neurosciences, Lausanne University Hospital and University of Lausanne, Switzerland
2
Interventional Neuroradiological Unit, Service of Diagnostic and Interventional Radiology, Lausanne University Hospital and University of Lausanne, Switzerland
3
Department of Statistical Science, University College London, United Kingdom
- Introduction: Endovascular treatment (EVT) in acute ischemic stroke (AIS) is now performed more frequently in the late window in radiologically selected patients. Little is known whether incomplete recanalization, cerebrovascular and technical (procedural) complications differ in the early vs. late window in the real world, on their predictors and clinical impact.
- Methods: We retrospectively reviewed all patients with AIS receiving EVT <24 h from 2015–2019 from the Acute STroke Registry and Analysis of Lausanne (ASTRAL). We compared all the EVT complications in the early (<6 h) vs. late (6–24 h) windows, identified their predictors and correlated them with short and long-term clinical outcome.
- Results: Among 682 AIS patients receiving EVT, 144 (21.1%) had at least one complication. Frequency of incomplete recanalization was similar in early and late EVT (7.5% vs 9.3%, padj = 0.26), as was the frequency of technical (procedural) complications (16.2% vs. 16.3%, padj = 0.90) and cerebrovascular complications (16.9% vs 20.5%, padj = 0.36). We identified groin puncture during the night shift (OR = 2.24), treatment of two arterial sites (OR = 2.71) and active smoking (OR = 1.93) as the most powerful predictors of procedural complications. Although complications lead to worse short-term outcome in late EVT (delta-NIHSS-24h = -2.5 vs 2, Padj = 0.01), 3-months mRS-values were similar (3 vs 3, p = 0.69).
- Conclusions: The frequency of incomplete recanalization and EVT complications seems similar in early and well-selected late EVT patients. Late EVT seemed to have worse 24 h outcome, but the long-term outcome did not differ. Our results confirm the safety of well-selected late EVT on AIS patients.
- O12
- Intravenous Thrombolysis Versus Early Dual Antiplatelet Therapy in Patients with Mild Ischemic Stroke
1
Department of Neurology, St. John’s Hospital, Vienna, Austria
2
Medical Faculty, Sigmund Freud University Vienna, Vienna, Austria
- Background and purpose: It is unclear whether intravenous thrombolysis (IVT) outperforms early dual antiplatelet therapy (DAPT) in the setting of mild ischemic stroke. The aim of this study was to compare early safety and efficacy of IVT as compared to DAPT.
- Methods: Data of mild non-cardioembolic stroke patients with admission NIHSS ≤3 who received IVT or early DAPT in the period 2018–2021 were extracted from a nationwide, prospective stroke unit registry. Study endpoints included symptomatic intracerebral haemorrhage (sICH) according to ECASS3 criteria, early neurological deterioration ≥4 NIHSS points (END) and 3-months functional outcome by modified Rankin Score (mRS).
- Results: 1195 stroke patients treated with IVT and 2625 treated with DAPT were included. IVT patients were younger (68.1 vs 70.8 years), had less hypertension (72.8% versus 83.5%), diabetes (19% versus 28.8%) and history of myocardial infarction (7.6% versus 9.2%) and slightly higher admission NIHSS scores (median 2 versus median 1) as compared to DAPT patients. After propensity score matching, IVT was associated with sICH (4 (1.2%) vs 0), END (aOR 2.8, CI 1.1–7.5), and mRS 0–1 at 3 months (aOR 1.3, CI 0.7–2.6).
- Conclusions: This large non-randomized comparison may indicate that IVT is not superior to DAPT in the setting of mild non-cardioembolic stroke and may eventually be associated with harm. Further research focusing acute therapy of mild stroke seems to be highly warranted.
- O13
- Safety and Effectiveness of IV Thrombolysis in Retinal Artery Occlusion
1
Department of Neurology, University Hospital Zurich and University of Zurich, Switzerland
2
Stroke Center and Department of Neurology, University Hospital Basel and University of Basel, Switzerland
3
Neurology and Neurorehabilitation, University Department of Geriatric Medicine Felix Platter, University of Basel, Switzerland
4
Department of Neurology, Kantonsspital St. Gallen, Switzerland
5
Stroke Center, Neurology Service, Lausanne University Hospital, Lausanne, Switzerland
6
Department of Neurology, Amsterdam UMC, University of Amsterdam, Amsterdam, the Netherlands
7
Charité-Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, Berlin Institute of Health, Germany and Center for Stroke Research Berlin (CSB), Charité-Universitätsmedizin Berlin, Germany
8
Department of Neurology, Inselspital, Bern University Hospital and University of Bern, Switzerland
9
Univ. Lille, Inserm, CHU Lille, U1172 - LilNCog - Lille Neuroscience & Cognition, Lille, France
10
Department of Neurology, University Hospital Heidelberg, Germany
11
Epidemiology, Biostatistics & Prevention Institute, University of Zurich, Switzerland
12
Institute for Data Analysis and Process Design, Zurich University of Applied Sciences, Winterthur, Switzerland
- Background and Aims: Acute retinal artery occlusion (RAO) may lead to irreversible blindness if not treated rapidly. Intravenous thrombolysis (IVT) is used in clinical practice; however, data about its effectiveness and safety is limited. We retrospectively analyzed the outcome of CRAO patients treated with IVT from nine European stroke centers.
- Methods: From the multicenter IVT database ThRombolysis for Ischemic Stroke Patients (TRISP), we compared assessed Visual acuity (VA) at baseline and within 3 months. Outcomes were any visual improvement, favorable VA (>0.2 in decimal) and safety (symptomatic intracranial hemorrhage (sICH) according to ECASS II criteria, asymptomatic intracranial hemorrhage (ICH) and major extracranial bleeding).
- Results: We identified 56 IVT and 141 non-IVT patients with CRAO. We excluded 106 patients with missing information about VA. Median IVT symptom-to-needle time was 235 min (25th/75th percentile: 216, 306). At baseline, IVT patients had more severely impaired VA. At follow up, VA improved in 27/48 (56%) IVT patients and in 17/43 (39%) non-IVT patients. Rates of favourable VA recovery were 12/48 (25%) in IVT and 21/43 (48%) in non-IVT patients. We observed no sICH, two asymptomatic ICH (4%) and one major extracranial bleeding (2%) after IVT and none in non-IVT patients.
- Conclusion: Our study provides real-life data from a large European cohort of IVT treated RAO patients. IVT seems safe and may improve VA in RAO patients. However, rates of satisfactory visual outcomes remain low. To facilitate further studies, outcome assessment in RAO patients should be standardised.
- O14
- Prediction Model for Medical Rescue Treatment Strategies in Patients with Incomplete Reperfusion
1
University Institute of Diagnostic and Interventional Neuroradiology, University Hospital Bern, Inselspital, University of Bern, Bern, Switzerland
2
Department of Neurology, University Hospital Bern, Inselspital, University of Bern, Bern, Switzerland
3
University Institute of Diagnostic, Interventional and Pediatric Radiology, University Hospital Bern, Inselspital, University of Bern, Bern, Switzerland
4
Department of Neuroradiology, Heidelberg University Hospital, Heidelberg, Germany
5
Department of Neurology, University Hospital Basel, Basel, Switzerland
- Background: After successful reperfusion is achieved (extended Thrombolysis in Cerebral Infarction (eTICI) ≥ 2b50), decision on pursuing additional treatment strategies in order to achieve complete reperfusion (eTICI = 2c/3), is multifactorial and depends on patient’s clinical and imaging characteristics. We have developed and validated a clinical decision tool to provide individualized predictions on achieving delayed reperfusion based on individual patient data.
- Methods: Single-center registry analysis for all consecutive patients admitted between February 2015–December 2020. Primary variable of interest was perfusion imaging outcome in patients with incomplete reperfusion (eTICI 2a-2c), evaluated on the 24-h follow-up imaging. This variable was dichotomized into delayed reperfusion, in case of non-observable perfusion deficit, and persistent perfusion deficit, in case of perfusion deficit captured on the final angiography imaging. Final model variable selection was performed via bootstrapped (n = 200) stepwise backwards regression. Model was split into a training and testing set (80:20 ratio), with 10-fold cross validation resampling.
- Results: 372 patients (50.8% female, mean age 74) were included, with 228 (61.2%) of them having delayed reperfusion. Final model identified seven variables of importance including: age, sex, atrial fibrillation, Intervention-to-Follow-Up time, maneuver count, eTICI and collateral status. Model’s discriminative ability for predicting delayed reperfusion was adequate (AUC 0.83, 95% CI 0.74–0.92), with an overall adjusted calibration (Brier score 0.17, 95% CI 0.15–0.18).
- Conclusions: Current model presents a tool that may aid clinical decision-making process in selection of patients for pursuing additional treatment strategies after incomplete reperfusion has been achieved. This is an important next step towards personalized treatment of stroke patients undergoing mechanical thrombectomy.
- O15
- Effect of Symptomatic and Asymptomatic COVID-19 on Safety and Outcome of Acute Ischemic Stroke Treatments
1
Stroke Centre, Neurology Service, Department of Neurological Sciences, Lausanne University Hospital, Lausanne, Switzerland
2
Department of Neurology, Hospital de Egas Moniz, Centro Hospitalar Lisboa Ocidental, Lisbon, Portugal
3
Department of Internal Medicine, Faculty of Medicine, School of Health Sciences, University of Thessaly, Larissa, Greece
4
Department of Neurology, Radiology, Boston Medical Centre, Boston University School of Medicine, Boston, MA, USA
5
Department of Neurology, Comprehensive Stroke Centre, Charles University Faculty of Medicine and University Hospital, Hradec Králové, Czech Republic
6
2nd Department of Neurology, Institute of Psychiatry and Neurology, Warsaw, Poland
7
Neurology Department, Leuven University Hospital, Leuven, Belgium
8
Alexandria University Hospitals and Affiliated Stroke Network, Alexandria, Egypt
9
School of Biomedical Engineering and Imaging Sciences, St Thomas Hospital, King’s College London, UK
10
Department of Clinical Therapeutics, National and Kapodistrian University of Athens, Greece
11
Departments of Radiology, Neurology and Neurosurgery, Grady Memorial Hospital, Atlanta, GA, USA
†
Contributed equally.
- Background and aims: COVID-19 related inflammation, endothelial dysfunction and coagulopathy may increase the bleeding risk and lower the efficacy of revascularization treatments in patients with ischemic stroke (IS). The effect of these pathophysiological processes is possibly related to the disease severity. We aimed to evaluate the safety and outcomes of revascularization treatments in patients with IS and asymptomatic or symptomatic COVID-19.
- Methods: Retrospective multicenter cohort study of consecutive IS patients receiving intravenous thrombolysis (IVT) and/or endovascular treatment (EVT) between March-2020 and June-2021, tested for SARS-CoV-2 infection, with or without COVID-19-compatible symptoms. By multivariate logistic regression analysis, we assessed the association of asymptomatic and symptomatic COVID-19 with bleeding complications and clinical outcomes. Study protocol was registered in ClinicalTrials.gov (NCT04895462).
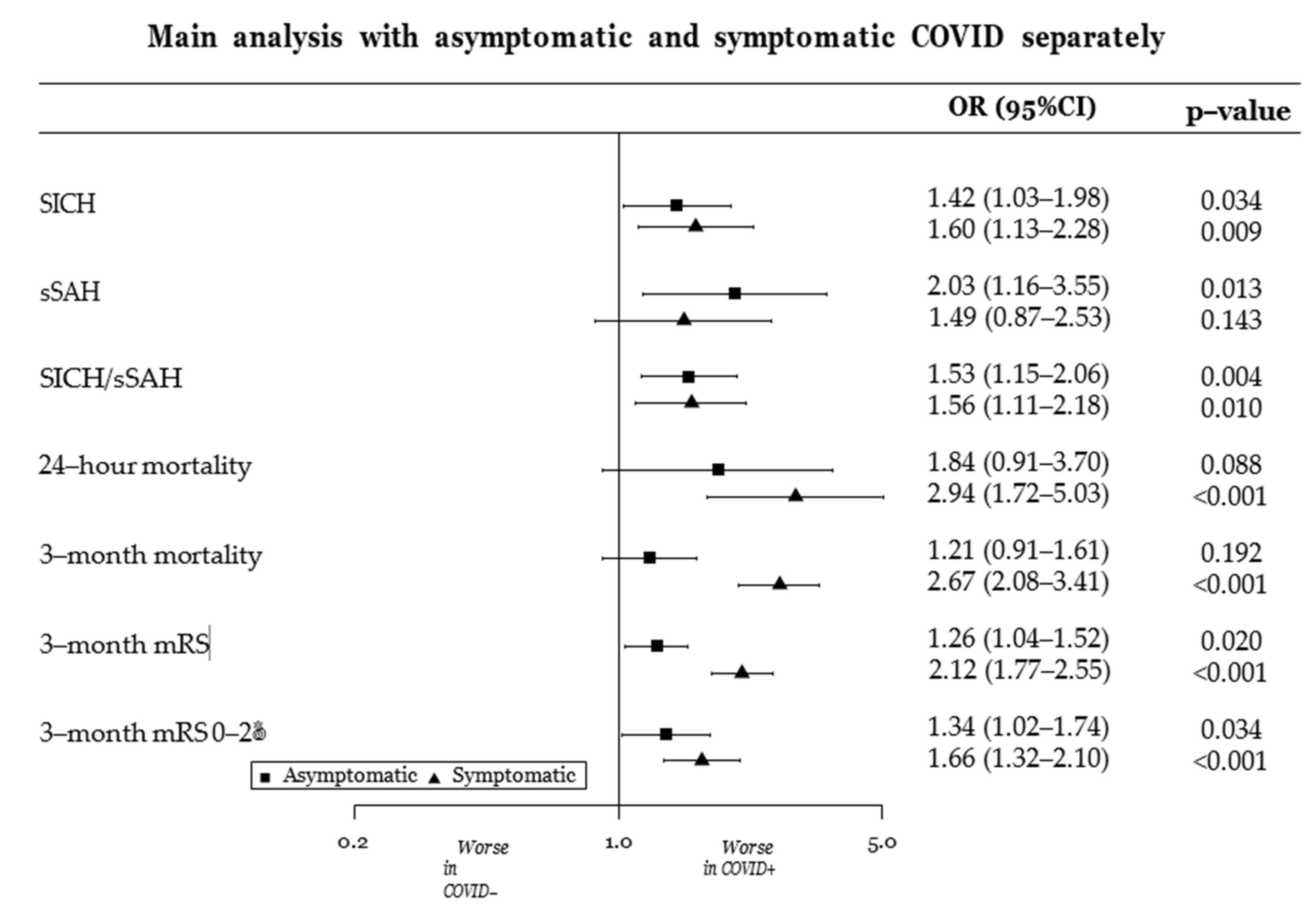
- Results: Among 15128 revascularized patients from 105 centers, 853 (5.6%) were diagnosed with COVID-19, of whom 395 (46%) were asymptomatic and 454 (54%) symptomatic. 5848 (38.7%) patients received IVT only, and 9280 (61.3%) EVT (+/− IVT). As shown in Figure, the hemorrhagic complications similarly increased in both asymptomatic and symptomatic COVID-19 patients, while 24-h and 3-month mortality was significant increased only in symptomatic ones. Compared to COVID-negative controls, 3-month disability was significantly worse in COVID-19 patients regardless the symptoms of the disease, but it was affected to a larger extent in symptomatic patients.
- Conclusions: Ischemic stroke patients with asymptomatic or symptomatic COVID-19 showed higher rates of intracranial bleeding complications and worse clinical outcomes after acute revascularization treatments than contemporaneous non-COVID-19 treated patients.
- O16
- Diagnostic Yield of a Systematic Vascular Health Screening Approach in Adolescents at Schools
1
Department of Neurology, Hochzirl Hospital, Zirl, Austria
2
VASCage, Research Centre on Vascular Ageing and Stroke, Innsbruck, Austria
3
Department of Neurology, Medical University of Innsbruck, Innsbruck, Austria
4
Department of Pediatrics II, Medical University of Innsbruck, Innsbruck, Austria
5
Department of Pediatrics III, Medical University of Innsbruck, Innsbruck, Austria
6
Department of Pediatrics I, Medical University of Innsbruck, Innsbruck, Austria
7
The Central Institute of Clinical Chemistry and Laboratory Medicine (ZIMCL), Medical University of Innsbruck, Innsbruck, Austria
- Purpose: A significant proportion of non-communicable diseases in adults has its roots in adolescence and this is particularly true for cardiovascular disease and stroke. Detection of vascular and metabolic risk factors at young ages may aid disease prevention.
- Methods: In 2088 adolescents sampled from the general population of Tyrol, Austria and South Tyrol, Italy, we systematically assessed the frequency of yet unknown vascular and metabolic risk conditions that require further diagnostic work-up or intervention (life-style counselling or pharmacotherapy). The health screening included medical history taking, fasting blood analysis, and blood pressure and body measurements, and was performed at schools. To recruit a representative sample of adolescents, equal proportions (about 67%) of schools were invited per school type and region.
- Results: Adolescents were on average 16.4 (SD 1.1) years old and 56.4 percent were female. A proportion of 22.8 (95%CI, 19.6–26.3) percent had previous or current physician-confirmed diseases. The health screening newly detected relevant medical conditions in 45.4 [95%CI, 41.5–49.4] percent (55.8 [95%CI, 52.7–58.7] percent in boys and 37.4 [95%CI, 35.0–39.8] percent in girls, p < 0.001). The most prevalent were elevated blood pressure and hypertension, metabolic syndrome, hypercholesterolemia, hypertriglyceridemia, hyperuricemia, and subclinical hypothyroidism. Detection of risk conditions did not depend on socioeconomic status but increased with age and body-mass index.
- Conclusions: Vascular health screening in adolescence at schools has a high diagnostic yield and may aid guideline-recommended prevention in the young. Implementation should carefully consider national differences in health-care systems, resources, and existing programs.
- O17
- Association of Patient and Intracranial Aneurysm Characteristics with the Risk of Subarachnoid Hemorrhage: An International Pooled-Analysis
1
Neurosurgery Division, Department of Clinical Neurosciences, Faculty of Medicine, Geneva University Hospitals, Geneva, Switzerland
2
Department of Pathology and Immunology, Faculty of Medicine, University of Geneva, Geneva, Switzerland
3
Stroke Research Centre, University College London Queen Square Institute of Neurology, London, UK
4
Department of Neurosurgery, Canton Hospital St. Gallen, St. Gallen, Switzerland
5
ZHAW School of Life Sciences and Facility Management, Zurich, Switzerland
6
INSERM, CNRS, UNIV Nantes, CHU Nantes, l’institut du thorax, Nantes, France
7
Department of Neuroradiology, University hospital of Nantes, Nantes, France
8
Department of Neurology, Faculty of Medicine, Jagiellonian University Medical College, Krakow, Poland
9
Stroke Research Centre, University College London, Institute of Neurology, London, UK
10
Neurogenetics Laboratory, The National Hospital of Neurology and Neurosurgery, London, UK
11
Department of Neurology and Neurosurgery, University Medical Center Utrecht Brain Center, Utrecht University, Utrecht, The Netherlands
12
Department of Medical and Molecular Genetics, Indiana University School of Medicine, Indianapolis, IN, USA
13
University of Cincinnati College of Medicine, Cincinnati, OH, USA
14
Departments of Neurology and Public Health Sciences, University of Virginia School of Medicine, Charlottesville, VA, USA
15
Department of Neuroradiology, Pitié-Salpêtrière Hospital, Paris, France
16
CHU de Nantes, INSERM CIC 1413, Pôle Hospitalo-Universitaire 11: Santé Publique, Clinique des données, Nantes, France
17
Department of Neuroradiology, Dupuytren university hospital, Limoges, France
18
Department of Neurosurgery, Helsinki University Hospital, University of Helsinki, Finland
19
Clinical Neurosciences, University of Helsinki, Helsinki, Finland
20
Neurosurgery Research Group, Biomedicum, Helsinki, Finland
21
Department of Vascular Surgery, Helsinki University Hospital, University of Helsinki, Finland
22
Department of Computer Science, University of Applied Science and Arts, Dortmund, Germany
23
Institute for Medical Informatics, Biometry and Epidemiology (IMIBE), University Hospital Essen, Germany
24
SIB Swiss Institute of Bioinformatics, Lausanne, Switzerland
25
Diagnostic and Interventional, Department of Diagnostics, Faculty of Medicine, Geneva University Hospitals, Geneva, Switzerland
26
Division of Neurosurgery, Department of Surgery, St Michael’s Hospital and University of Toronto, Canada
27
Swiss Neuroradiology Institute, Zurich, Switzerland
28
Lucerne School of Business, Lucerne University of Applied Sciences, Lucerne, Switzerland
29
Neurosurgery NeuroCenter Kuopio, University Hospital Kuopio, Finland
30
Institute of Clinical Medicine, Faculty of Health Sciences, University of Eastern Finland, Kuopio, Finland
31
Institut Hospital del Mar d’Investigacions Biomèdiques (IMIM) and Hospital del Mar, Barcelona, Spain
32
Clinical Trial Service Unit and Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK
33
MRC Population Health Research Unit, University of Oxford, Oxford UK
34
A list of members and affiliations appears in the Appendix 2
35
Department of Anesthesia and Perioperative Care, Center for Cerebrovascular Research, University of California, San Francisco, California, USA
36
Department of Epidemiology and Biostatistics, University of California, San Francisco, California, USA Institute for Human Genetics, University of California, San Francisco, California, USA
37
Department of Neurology, University of California, San Francisco, California, USA
38
Montreal Neurological Institute and Hospital, McGill University, Montréal, QC, Canada
39
Department of Clinical Radiology, Kuopio University Hospital, Kuopio, Finland
- Objective: Intracranial aneurysms (IAs) are usually asymptomatic with a low risk of rupture, but consequences of aneurysmal subarachnoid hemorrhage (aSAH) are severe. Identifying IAs at risk of rupture has important clinical and socio-economic consequences. The goal of this study was to identify patient- and IA-characteristics associated with IA rupture.
- Methods: Patients with saccular IA were recruited at 21 international centers in the context of genetic studies on IA. Patient-characteristics included basis of recruitment, sex, positive family history of IA/aSAH, hypertension, smoking, age at time of IA rupture and IA multiplicity. IA-characteristics were rupture status, maximum diameter at rupture, and location. We performed a cross-sectional analysis of patient- and IA-characteristics associated with IA rupture using multivariate analyses.
- Results: 8560 patients were included. In the final cohort of 7992 participants, 31% had ruptured IAs. Multivariate analysis demonstrated that: (1) IA rupture was associated with IA location, awareness of hypertension, and former smoking; (2) IA size and age at rupture were associated with IA location; (3) IA in smokers ruptured at larger sizes and younger age; (4) Former smokers had a lower risk of rupture than current smokers; (5) IAs in female ruptured at smaller sizes and older age; (6) IA size at rupture correlated with patient age at rupture.
- Conclusions: We extend the current IA disease model showing that IA location and size are the strongest factors associated with rupture, followed by active smoking and hypertension awareness. Female sex and IA multiplicity are not associated with rupture.
- O18
- Correlation Between Transcranial Duplex Sonography and Perfusion MRI to Identify Cerebral Hyperperfusion After Stroke Thrombectomy
1
Department of Neurology, Medical University of Graz, Graz, Austria
2
Division of Neuroradiology, Vascular and Interventional Radiology, Department of Radiology, Medical University of Graz, Graz, Austria
- Background: Increased middle cerebral artery (MCA) flow velocities on transcranial duplex sonography (TCD) were observed in individual patients after stroke thrombectomy and associated with intracranial hemorrhage and poor outcome. However, the retrospective study design did not allow elucidation of the underlying pathomechanism, and the relationship between TCD and parenchymal perfusion abnormalities remains to be determined.
- Methods: Successfully recanalized anterior circulation stroke thrombectomy patients were prospectively investigated with TCD and MRI including contrast-enhanced perfusion sequences within 48 h post-intervention. Increased MCA flow on TCD was defined as >30% mean blood flow velocity in the treated compared to the contralateral MCA. MRI blood flow maps served to assess hyperperfusion rated by neuroradiologists blinded to TCD.
- Results: All included 226 thrombectomy patients underwent postinterventional TCD and 92 patients additionally had perfusion MRI (41%). 85 patients (38%) showed increased postinverventional MCA flow on TCD. Of those, 10 patients (12%) had an underlying focal stenosis or vasospasm. Increased TCD blood flow in the recanalized MCA was associated with intracranial hemorrhage, larger infarct size and poor 90-day outcome (p < 0.001, multivariable adjustment). In the subgroup that had both TCD and perfusion MRI available (n = 92), 29 patients had increased ipsilateral MCA flow velocities on TCD (31%). Of those, 25 patients also showed parenchymal hyperperfusion on MRI (86%, p < 0.001; diagnostic accuracy: 77%). Hyperperfusion severity on MRI correlated with MCA flow velocities on TCD (r = 0.457, p < 0.001)
- Conclusions: TCD is a reliable tool to identify post-reperfusion hyperperfusion, correlates well with perfusion MRI, and indicates bleeding complications and poor outcome after stroke thrombectomy.
- O19Trends of Functional Outcome in Acute Stroke Patients Treated with Intravenous Thrombolysis
1
Medical University of Vienna, Department of Neurology, Vienna, Austria
2
Gesundheit OÖsterreich GmbH, Vienna, Austria
3
Krankenanstalt Rudolfstiftung, Department of Neurology, Vienna, Austria
4
Krankenhaus Barmherzige Bruüder, Department of Neurology, Vienna, Austria
5
Medical University of Innsbruck, Department of Neurology, Innsbruck, Austria
- Background and aims: Frequencies of rtPA-treatment for acute stroke have been increasing over time. We aimed to investigate trends in frequencies of good functional outcome in rtPA- treated patients and to assess the influence of clinical variables on functional outcome.
- Methods: We analyzed patient data in the Austrian Stroke Unit Registry from 2006 to 2019. Frequencies of favorable outcome, defined as modified Rankin Scale (mRS) 0–2, were assessed for the overall population and prespecified subgroups. Logistic regression analysis was performed to evaluate associations of baseline characteristics, including relevant interaction terms, with functional outcome.
- Results: Overall, 4865/9409 rtPA-treated patients (51.7%) achieved favorable outcome at 3 months. Frequencies of favorable outcome increased from 45.9% in 2006 to 56.8% in 2019. In logistic regression analysis, year of treatment (OR 1.08, 95%CI 1.01–1.15) was associated with favorable outcome. Stroke severity (NIHSS, OR 0.86, 95%CI 0.85–0.87), age (61–70 years: OR 0.67, 95%CI 0.55–0.80, 71–80 years: OR 0.42, 95%CI 0.35–0.50, >80 years: OR 0.16, 95%CI 0.13–0.20), female sex (OR 0.53, 95%CI 0.89–0.99), and cardiovascular comorbidities were negatively associated. Including interaction terms into the model we observed an association of favorable outcome with interactions between stroke severity and year of treatment (OR 1.01, 95%CI 1.0–1.02), and stroke severity and endovascular treatment (EVT, OR 1.02, 95%CI 1.01–1.03).
- Conclusions: Frequencies of favorable outcome in rtPA-treated patients have been increasing over time, likely driven by improved outcome in more severely affected patients receiving EVT. However,
- O20
- Head-/Neck Pain Characteristics after Spontaneous Cervical Artery Dissection in The Acute Phase and on aLong-Run
1
Department of Neurology, Medical University Innsbruck, Austria
2
Department of Neuroradiology, Medical University Innsbruck, Austria
3
Department of Dermatology, Medical University Innsbruck, Austria
4
VASCage, Research Center on Vascular Ageing and Stroke, Innsbruck, Austria
- Objective: Head/neck-pain is one of the primary symptoms associated with spontaneous cervical artery dissection (sCeAD). Still, data on pain quality, -intensity, and long-term dynamics are scarce.
- Methods: sCeAD subjects were included if mural hematoma was visualized through T1-fat-saturated MRI at baseline. All available medical records were evaluated and patients were invited to standardized clinical follow-up visits at least one year after the index event.
- Results: In total, 279 subjects were included in the ReSect-study with head/neck-pain being the most frequent symptom of sCeAD (220 of 273, 80.6%). Pain was of pulling nature in 107 of 218 (49.1%), and extended to the neck area in 145 of 218 (66.5%). In those with prior headache history, pain was novel in quality in 75.4% (42 of 55). Median patient-reported pain intensity was 5 of 10 with thunderclap type headache being uncommon (12 of 218, 5.5%). Prior to hospital admission, head/neck-pain rarely responded to self-medication (32 of 218, 14.7%). Characteristics did not differ between subjects with and without cerebral ischemia. Pain resolved completely in all subjects within a median of 13.5 days (IQR 12). Upon follow-up in 42 of 164 (25.6%) novel recurring headache occurred, heterogeneous in quality, localization and intensity.
- Conclusions: We present an in-depth analysis of sCeAD-related head/neck-pain characteristics and its long-term dynamics.
- P01
- Liver Fibrosis is Related to Atrial Fibrillation in Acute Ischemic Stroke
1
Department of Neurology, Medical University of Graz, Austria
2
Division of Gastroenterology and Hepatology, Department of Internal Medicine, Medical University of Graz, Austria
3
Clinical Institute of Medical and Chemical Laboratory Diagnostics, Medical University of Graz, Austria
4
Institute for Medical Informatics, Statistics and Documentation, Medical University of Graz, Austria
5
Division of Neuroradiology, Vascular and Interventional Radiology, Department of Radiology, Medical University of Graz, Austria
- Background: Non-alcoholic fatty liver disease and particularly liver fibrosis may indicate an increased risk for atrial fibrillation, but this association has not yet been systematically investigated in a cohort of ischemic stroke patients. Therefore, we aimed to explore whether clinically inapparent liver fibrosis is related to atrial fibrillation and other stroke etiologies in a cohort of consecutive acute ischemic stroke patients.
- Methods: We analyzed data from a prospective single-center study investigating all ischemic stroke patients admitted to our stroke over a one-year-period. All patients received thorough etiological work-up including extended cardiac rhythm monitoring. For evaluation of liver fibrosis, we calculated the FIB-4 index, a well-established non-invasive liver fibrosis test based on simple clinical and laboratory parameters (cut-off ≥ 2.67). Laboratory results were analyzed from a uniform blood sample, which was taken within 24 h of stroke unit admission.
- Results: Of 418 included patients (mean age 70.3 years, 57.2% male), FIB-4 indicated advanced liver fibrosis in 92 (22.0%). Atrial fibrillation as the underlying stroke mechanism was present in 24.6% (large vessel disease: 25.6%, small vessel disease: 11.2%, cryptogenic: 32.8%). Atrial fibrillation was strongly related to liver fibrosis (Odds Ratio 4.41, 95% confidence interval 2.70–7.19, p < 0.001). This association remained significant after correction for relevant co-morbidities (hypertension, diabetes, dyslipidemia, coronary heart disease) and age (p = 0.001).
- Conclusions: Clinically inapparent liver fibrosis evaluated by a simple noninvasive test is independently associated with atrial fibrillation in acute ischemic stroke patients. Further studies should evaluate whether adding liver fibrosis to atrial fibrillation risk scores will increase their precision.
- P02
- Association of MRI Small Vessel Disease-Phaenotype with 3-Month Functional Outcome and Cerebrovascular Events in Intracerebral Haemorrhage Patients. A Pilot Anal-ysis.
1
Department of Neurology, Inselspital Bern University Hospital and University of Bern, Switzerland
2
Graduate School for Health Sciences, University of Bern, Switzerland
3
University Institute for Diagnostic and Interventional Neuroradiology, Inselspital Bern University Hospital and University of Bern, Switzerland
4
Department of Neurosurgery, Inselspital Bern University Hospital and University of Bern, Switzerland
5
Department of Neurology, University Hospital Basel, Switzerland
- Background: Knowledge about different intracerebral haemorrhage (ICH) subtypes is scarce and there is no accepted classification. We present a new, small vessel disease (SVD) phaenotype-based ICH classification and investigate association of SVD-phaenotypes with outcomes.
- Methods: We assessed non-traumatic ICH patients from the Bernese Stroke Registry with available MRI after the index ICH. ICH aetiology was classified according to a new MRI SVD marker-based classification as cerebral amyloid angiopathy (CAA), deep perforator arteriopathy (DPA), mixed SVD or undetermined SVD. The primary outcome was modified Rankin Scale (mRS) shift after 3 months, secondary outcomes included recurrent ICH or ischaemic strokes within 3 months.
- Results: 376/801 patients (46.9%) with non-traumatic ICH had MRI. In 259 (32.3%) cases, ICH was classified as SVD-related (mean age 68.8 ± 13.7 years; 48.3% female). The most frequent phaenotype was mixed SVD (148 patients, 57.1%), followed by undetermined SVD (45 patients, 17.4%), DPA (42 patients, 15.8%) and CAA (25 patients, 9.7%). Compared to mixed SVD, CAA was associated with better outcome (aOR for mRS shift 0.32, 95%-CI 0.11–0.93), while DPA (aOR 2.18 95%-CI 0.75–6.35) had similar and undetermined SVD (aOR 2.51, 95%-CI 1.04–6.03) poorer outcome. Relative recurrent ICH rates were highest in CAA and mixed SVD (10.5% each), while ischaemic stroke occurred similarly in DPA, mixed SVD (5.9% each) and undetermined SVD (7.4%), but not in CAA (0.0%).
- Conclusions: This classification provides objective criteria for SVD-phaenotypes, including DPA. Functional outcomes and recurrent cerebrovascular event rates within 3 months differ amongst SVD-phaenotypes. Findings may influence future diagnostic work-up and secondary prevention.
- P03
- Acute Ischemic Stroke in Patients with Newly Diagnosed Versus Known Active Cancer: Characteristics, Mechanisms, and Recurrences
1
Stroke Center, Service of Neurology, Lausanne University Hospital and University of Lausanne, Lausanne, Switzerland
2
Services of Neurology and Oncology, Lausanne University Hospital and University of Lausanne, Switzerland
3
1st Department of Internal Medicine, University of Ioannina, Medical School, Ioannina, Greece
4
Feil Brain and Mind Research Institute and Department of Neurology, Weill Cornell Medicine, New York, USA
5
Department of Neurology, Memorial Sloan Kettering Cancer Center, New York, USA
- Background: Acute ischemic stroke (AIS) and cancer are important causes of disability and death among adults. We aimed to estimate the rate of newly-diagnosed cancer (NDC) and active cancer (AC) in AIS patients, and to compare demographic, clinical, and long-term outcome data between groups.
- Methods: We retrospectively analyzed data from ASTRAL (Acute-STroke-Registry-and-Analysis-of-Lausanne) between 1/2003–10/2021, a consecutive single-center registry in Switzerland. We defined NDC as cancer diagnosed <12 months since the index stroke. AC was defined following standard definition (Khorana, J. Thromb. Haemost, 2018). We compared both groups regarding patients’ characteristics, stroke mechanisms, long-term functional outcome, mortality, and recurrences. Univariate analysis is provided; other logistic regression analyses are ongoing and will be presented at the congress.
- Results: Among 6686 AIS patients, 38.9% were women and the median age was 74.3 years (IQR 16.7). Eighty six (1.3%) patients had NDC and 310 (4.6%) had AC. Table 1 indicates no difference in risk factors and stroke mechanisms between NDC and AC patients, except that NDC patients had a lower pre-stroke modified Rankin Scale (mRS). Unadjusted analysis indicates no difference in short- or long-term mortality nor 3-month disability (mRS > 2). The 3-month stroke recurrence rate was 16.2% with NDC vs 9.7% with AC (OR 1.80, 95% CI 0.91–3.58).
- Conclusions: In the year after AIS, 1.3% of patients were newly diagnosed with cancer. Patients with NDC and AC seem to be similar in most aspects, except that NDC patients seem to have less pre-stroke disability and a trend towards more stroke recurrence.
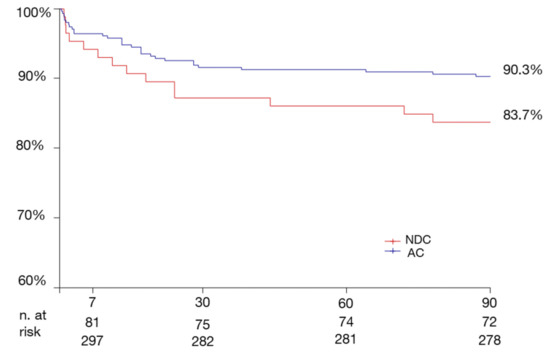
Figure 1.
Months after the index stroke in NDC and AC patients. Log rank test = 2.9, (p > 0.05).

Table 1.
Patient characteristics and results. Continuous and ordinal variables are expressed as medians (with interquartile range, IQR), and categorical variables as absolute counts (with percentage). Results from the univariate analysis in the “NDC” and “AC” groups are reported as odds ratio (OR) and 95% confidence interval (CI). PFO: patent foramen ovale; mRS: modified Rankin Scale.
Table 1.
Patient characteristics and results. Continuous and ordinal variables are expressed as medians (with interquartile range, IQR), and categorical variables as absolute counts (with percentage). Results from the univariate analysis in the “NDC” and “AC” groups are reported as odds ratio (OR) and 95% confidence interval (CI). PFO: patent foramen ovale; mRS: modified Rankin Scale.
| Variable | Study Cohort (N = 396) | Newly Diagnosed Cancer (NDC) (N = 86) | Active Cancer (AC) (N = 310) | OR (95% CI) | p-Value |
|---|---|---|---|---|---|
| Age | 74.3 (16.7) | 74.8 (15.4) | 74.3 (17.2) | 0.87 (0.98–1.02) | 0.87 |
| Female sex | 154/396(38.9%) | 35/86 (40.7%) | 119/310 (38.4%) | 0.91 (0.56–1.48) | 0.7 |
| mRS pre-stroke | 1 (2) | 1(2) | 1(2) | 0.026 | |
| Vascular risk factors | |||||
| Hypertension | 288/396 (72.9%) | 67/86 (77.9%) | 221/309 (71.5%) | 1.4 (0.8–2.47) | 0.24 |
| Atrial fibrillation | 106/396 (27%) | 24/86 (27.9%) | 82/307(26.7%) | 1.06 (0.62–1.81) | 0.83 |
| Diabetes | 80/396 (20.3%) | 14/86 (16.3%) | 66/309 (21.4%) | 0.72 (0.38–1.35) | 0.3 |
| Dyslipidaemia | 274/396 (69.7%) | 63/86 (73.3%) | 211/307 (68.7%) | 1.25 (0.73–2.13) | 0.42 |
| Smoking | 105/396 (27%) | 28/85 (32.9%) | 77/304 (25.3%) | 1.5 (0.86–2.44) | 0.16 |
| Coronary disease | 79/396 (20.2%) | 18/85 (21.2%) | 61/306 (19.9%) | 1.08 (0.6–1.95) | 0.8 |
| Prosthetic valve | 7/396 (1.8%) | 2/86 (2.3%) | 5/308 (1.6%) | 1.44 (0.28–7.57) | 0.66 |
| Eject. fraction <35% | 18/396 (4.5%) | 7/86 (8.1%) | 11/310 (3.5%) | 2.41 (0.9–6.4) | 0.071 |
| Stroke etiologies | |||||
| Atherosclerosis | 49/370 (13.2%) | 11/86 (12.8%) | 38/284 (13.4%) | 0.95 (0.46–1.95) | 0.89 |
| Cardioembolism | 86/370 (23.2%) | 22/86 (25.6%) | 64/284 (22.5%) | 1.48 (0.84–2.61) | 0.117 |
| Lacunar | 26/370 (7%) | 6/86 (7%) | 20/284 (7%) | 1.17(0.45–3.03) | 0.74 |
| Dissection | 3/370 (0.8%) | 1/86 (1.2%) | 2/284 (0.7%) | 1.95 (0.17–21.8) | 0.58 |
| PFO-related | 3/370 (0.8%) | 1/86 (1.2%) | 2/284 (0.7%) | 1.92 (0.17–21.5) | 0.59 |
| Rare and/or cancer- related | 94/370 (25.4%) | 23/86 (26.7%) | 71/284 (25%) | 1.28 (0.74–2.23) | 0.37 |
| Multiple mechanism | 48/370 (13%) | 10/86 (11.6%) | 38/284 (13.38%) | 0.98 (0.47–2.1) | 0.97 |
| Embolic stroke of undet. source | 37/370 (10%) | 10/86 (11.6%) | 27/284 (9.51%) | 1.5 (0.69–3.25) | 0.3 |
| Undetermined, and/or incomplete work-up | 24/370 (6.5%) | 2/86 (2.3%) | 22/284 (7.75%) | 0.33 (0.07–1.45) | 0.13 |
| Recurrence 3 months | 44/394 (11.2%) | 14/86 (16.2%) | 30/308 (9.7%) | 1.8 (0.91–3.58) | 0.089 |
| Mortality 7 days | 42/396 (10.6%) | 6/86 (7.0%) | 36/310 (11.6%) | 0.57 (0.23–1.4) | 0.22 |
| Mortality 3 months | 110/349 (31.5%) | 23/82 (28%) | 87/267 (32.6%) | 0.81 (0.47–1.4) | 0.44 |
| Mortality 12 months | 165/305 (54%) | 41/71 (57.7%) | 124/234 (53.0%) | 1.21 (0.71–2.07) | 0.48 |
| mRS > 2 at 3 months | 194/350 (55.4%) | 42/82 (51.2%) | 152/268 (56.7%) | 0.8 (0.49–1.32) | 0.38 |
| mRS 3 months | 3 (5) | 3(4) | 3 (5) | 0.71 |
- P04
- Gapless ECG-Monitoring in Stroke at High Risk of Atrial Fibrillation—Gems af Preliminary Results
1
Medical University of Vienna, Department of Neurology, Vienna, Austria
2
Medical University of Vienna, Department of Medicine II, Division of Cardiology, Vienna, Austria
3
Clinic Landstrasse (Rudolfstiftung Hospital), Department of Neurology, Vienna, Austria
4
Clinic Landstrasse (Rudolfstiftung Hospital), Department of Cardiology, Vienna, Austria
5
Medical University of Salzburg, Department of Neurology, Salzburg, Austria
- Background: Atrial fibrillation (AF) is a major risk factor for ischemic stroke. Gapless electrocardiogram (ECG) monitoring without any interruption of monitoring time via an implantable loop recorder (ILR) might increase the detection rates of AF after ischemic stroke.
- Methods: Patients with acute ischemic stroke or transient ischemic attack without known AF were included in this prospective multicenter study. Participants received gapless ECG monitoring via telemetry followed by implantation of an ILR during stroke-unit admission, avoiding any interruption in monitoring time. Patients acted as their own controls and also received standard Holter ECG-monitoring. The primary outcome parameter was new-onset AF within six months of follow-up.
- Results: A total of 80 patients were included. Of these, 65 (81.3%) patients had an embolic stroke of unknown source, 6 (9.2%) patients were included with large-artery disease and 9 (11.3%) participants had small-vessel disease. AF was newly detected in 15 (18.8%) patients via ILR monitoring compared to one patient (1.3%) via Holter-ECG monitoring (p = 0.001). The median time to the first AF episode was 19 days [Interquartile range (IQR): 9–43] with a median duration of the detected AF episodes of 3.1 [IQR: 0.25–4.78] hours. Patients with a CHA2DS2-VASc Score ≥ 5 had a significantly higher risk of new onset AF compared to patients with a CHA2DS2-VASc Score < 5 (Figure 1, p = 0.008). Oral anticoagulation was established in all patients with new-onset AF.
- Conclusions: Gapless ECG monitoring with an ILR is a feasible and highly effective approach to significantly increase the detection rates of AF after acute ischemic stroke.
- P05
- The Smoker’s Paradox in Stroke: No Evidence for Smoking-Induced Preconditioning in Large Vessel Occlusion Stroke
1
University Hospital Zurich, Department of Neurology, Zurich, Switzerland
2
Clinical Neuroscience Center, University Hospital Zurich, University of Zurich, Zurich, Switzerland
3
University Hospital Zurich, Department of Neuroradiology, Zurich, Switzerland
4
Epidemiology, Biostatistics and Prevention Institute (EBPI), University of Zurich, Zurich, and Institute of Data Analysis and Process Design (IDP), Winterthur, Switzerland
5
University Hospital Bern, Department of Neurology, Switzerland
- Background: Smoking is a well-known risk factor for stroke. However, several studies have reported a better outcome after stroke for patients who smoke. We aimed to investigate this “Smoker’s Paradox”, which may originate from a preconditioning-like protection due to better collaterals in smokers.
- Methods: In this retrospective study, we analysed data of patients with acute ischemic stroke due to middle cerebral artery M1 segment occlusion treated with mechanical thrombectomy at the University Hospital Zurich between 2014 and 2018. We assessed angiography and CT perfusion imaging along with clinical characteristics. Patients were grouped into current, former and never smokers. We compared the association of smoking to stroke severity on admission (NIHSS), functional disability after 3–6 months (mRS), collateral status, infarct core volume and recanalisation success using unadjusted and adjusted analyses.
- Results: Out of 402 patients with M1 occlusion, we included 320. 19.7% (n = 63) were current, 18.8% (n = 60) were former, and 61.6% (n = 197) never smokers. Admission NIHSS and mRS after 6 months were similar in all groups. Current smokers were younger, more often male and significantly less likely to have atrial fibrillation. Neither current nor former smoker status were associated with good collateral status, smaller infarct cores or better recanalization success.
- Conclusions: We could not confirm the smoking paradox. Neither stroke severity nor imaging parameters were suggestive of a preconditioning effect provided by smoking. On the contrary; smoking causes atherosclerotic stroke at a younger age, highlighting the role of smoking as a an avoidable vascular risk factor.
- P06
- Lipoprotein (A) is a Newly Validated Biomarker for Large-Artery-Atherosclerosis Stroke Aetiology
1
University Hospital Basel, Neurology, Basel, Switzerland
2
Cantonal Hospital Schaffhausen, Internal Medicine, Schaffhausen, Switzerland
3
University Hospital Zürich, Neurology, Zürich, Switzerland
4
University of Basel, Clinical Research, Basel, Switzerland
5
University Department of Geriatric Medicine Felix Platter, Neurology and Neurorehabilitation, Basel, Switzerland
6
Hirslanden Hospital Zurich, Neurology, Zürich, Switzerland
7
Inselspital, University Hospital Bern, Neurology, Bern, Switzerland
8
University Hospital Basel, Laboratory Medicine, Basel, Switzerland
9
University Hospital Basel, Endocrinology, Basel, Switzerland
- Background and aims: Lipoprotein(a) (Lp(a)) serum levels are genetically determined and contribute to atherogenesis. High Lp(a) levels are associated with an increased cardiovascular morbidity. Recently, serum Lp(a) levels have been associated with large artery atherosclerosis stroke (LAAS) aetiology. We aimed to validate this association in an independent cohort.
- Methods: We included acute ischemic stroke patients from a prospective cohort study from the University Hospital Bern (Inselspital), Switzerland. Lp(a) serum levels were measured in serum, drawn within 24 h after symptom onset. We assessed the association of Lp(a) with LAAS in univariate and multivariate analysis, adjusting for traditional LAAS risk factors.
- Results: Overall, 746 patients were included, of which 105 had a LAA stroke (14%). Lp(a) was higher in patients with LAAS compared to patients with non-LAAS (23.0 nmol/l [IQR:9.8–80.0] versus 16.3 nmol/l [IQR:5.8–57.0], p = 0.01). In univariate analysis, patients with LAAS were significantly more often men, suffered more often from Dyslipidaemia, Arterial Hypertension, Diabetes and had a higher BMI than patients with non-LAAS (Table 1). In a multivariable logistic regression model, elevated Log10(Lp(a)) was associated with LAAS with a OR of 1.50 (95%CI 1.02–2.21) (Table 2).
- Conclusions: Among ischemic stroke patients, we could validate the independent association of higher Lp(a) levels with LAAS aetiology, also after adjusting for traditional cardiovascular risk factors. Independent validation of biomarkers, especially with the aim to guide secondary prevention, is essential. These findings are relevant in view of randomised clinical trials investigating the effect of specific Lp(a) lowering agents in reducing major adverse cardiovascular events.

Table 1.
Baseline Characteristics of Patients with an acute ischemic stroke.
Table 1.
Baseline Characteristics of Patients with an acute ischemic stroke.
| Total (n = 746) | LAA Stroke (n = 105) | Non-LAA Stroke (n = 641) | p-Value | |
|---|---|---|---|---|
| Demographic data | ||||
| Age, y, median (IQR) | 71 (61–80) | 72 (63–79) | 71 (60–80) | 0.59 |
| Men, n (%) | 467 (62.6) | 77 (73.3) | 390 (60.8) | 0.02 |
| Medical history, n (%) | ||||
| Dyslipidemia | 427 (58.0) | 71 (67.6) | 356 (56.4) | 0.03 |
| Previous cerebrovascular event | 154 (20.7) | 29 (27.6) | 125 (19.5) | 0.07 |
| Arterial hypertension | 510 (68.4) | 85 (81.0) | 425 (66.3) | 0.002 |
| Current Smoking | 133 (17.8) | 26 (24.8) | 107 (16.7) | 0.05 |
| Ever Smoking | 238 (31.9) | 37 (35.2) | 201 (31.4) | 0.43 |
| Coronary heart disease | 133 (17.8) | 19 (18.1) | 114 (17.8) | 0.89 |
| Diabetes mellitus | 115 (15.4) | 25 (23.8) | 90 (14.1) | 0.01 |
| Positive family history | 112 (19.9) | 12 (16.0) | 100 (20.5) | 0.44 |
| Clinical data, median (IQR) | ||||
| BMI kg/m2 | 25.7 (23.1–28.3) | 26.4 (24.4–29.1) | 25.6 (22.9–28.3) | 0.01 |
| NIHSS on admission | 6 (3–12.5) | 5 (3–12) | 6 (3–13) | 0.64 |
| Medication on admission, n (%) | ||||
| Statins | 195 (26.2) | 35 (33.7) | 160 (25.0) | 0.07 |
| Platelet inhibitors | 280 (37.6) | 52 (49.5) | 228 (35.6) | 0.009 |
| Antihypertensive drugs | 442 (59.5) | 76 (73.1) | 366 (57.3) | 0.002 |
| Laboratory values, median (IQR) | ||||
| Lipoprotein (a), nmol/L | 16.9 (6.1–60.0) | 23 (9.8–80.0) | 16.3 (5.8–57.0) | 0.01 |
| LDL, mmol/L | 2.6 (2.0–3.3) | 2.6 (2.1–3.4) | 2.6 (2.0–3.3) | 0.33 |
| Apolipoprotein B, g/L | 0.95 (0.78–1.13) | 0.94 (0.8–1.13) | 0.95 (0.77–1.13) | 0.74 |
| Cholesterol, mmol/L | 4.7 (4.0–5.5) | 4.6 (4.1 -5.4) | 4.7 (4.0–5.5) | 0.75 |
| Triglycerides, mmol/L | 1.4 (1.0–2.0) | 1.4 (1.1–2.0) | 1.4 (1.0–2.0) | 0.92 |
| Non-HDL, mmol/l | 3.3 (2.7–4.2) | 3.3 (2.9–4.2) | 3.3 (2.7–4.1) | 0.58 |
| HbA1c, % | 5.8 (5.6–6.2) | 6.0 (5.7–6.3) | 5.8 (5.6–6.2) | 0.002 |
| TOAST Classification, n (%) | ||||
| Macroangiopathy | 105 (14.1) | 105 (100) | 0 | n/a |
| Cardioembolism | 288 (38.6) | 0 | 288 (44.9) | n/a |
| Microangiopathy (lacunar) | 43 (5.8) | 0 | 43 (6.7) | n/a |
| Other etiologies | 28 (3.8) | 0 | 28 (4.4) | n/a |
| Undetermined, evaluations complete | 117 (15.7) | 0 | 117 (18.3) | n/a |
| Undetermined, evaluations incomplete | 95 (12.7) | 0 | 95 (14.8) | n/a |
| More than 1 possible aetiology | 70 (9.4) | 0 | 70 (10.9) | n/a |

Table 2.
Multivariable logistic regression model for the association with large artery atherosclerotic stroke and Lipoprotein (a).
Table 2.
Multivariable logistic regression model for the association with large artery atherosclerotic stroke and Lipoprotein (a).
| Variable | aOR | 95%-CI | p |
|---|---|---|---|
| Log10 (Lp (a)) | 1.50 | 1.02–2.21 | 0.04 |
| Arterial Hypertension | 1.98 | 1.07–3.68 | 0.03 |
| Women | 0.59 | 0.34–1.02 | 0.06 |
| Diabetes mellitus | 1.72 | 0.95–3.13 | 0.08 |
| BMI | 1.03 | 0.98–1.09 | 0.18 |
| Dyslipidaemia | 1.34 | 0.79–2.29 | 0.28 |
| Platelet inhibitor on Admission | 1.34 | 0.82–2.21 | 0.24 |
Legend: aOR = adjusted odds ratio, CI = confidence interval, Lp(a) = Lipoprotein A.
- P07
- Deep Learning vs. Stroke Neurologists: Functional Outcome Prediction in Large Vessel Occlusion Stroke Patients Based on Clinical and Imaging Data
1
Epidemiology, Biostatistics and Prevention Institute (EBPI), University of Zurich, Zurich, Switzerland
2
Institute of Data Analysis and Process Design (IDP), Zurich University of Applied Sciences, Zurich, Switzerland
3
Department of Neurology, University Hospital Zurich and University of Zurich, Zurich, Switzerland
4
Clinical Neuroscience Center, University Hospital Zurich, University of Zurich, Zurich, Switzerland
5
Department of Neurology, InselSpital Berne, Berne, Switzerland
6
Diagnostic and Interventional Neuroradiology, University Hospital of Berne, Berne, Switzerland.
7
Department of Diagnostic, Interventional and Pediatric Radiology, University Hospital of Berne, Berne, Switzerland
8
Department of Neurology, University Hospital Basel, Switzerland
- Background: Even with mechanical thrombectomy (MT), functional outcomes vary fundamentally between patients with large vessel occlusion (LVO) stroke. Can we predict functional outcome of individual stroke patients? In a “competition” between experienced stroke neurologists and neural networks, we assessed clinical and imaging data for functional outcome prediction in LVO stroke.
- Methods: We considered data of 222 patients with middle cerebral artery occlusion who received MT at the Inselspital Berne. We developed (deep) neural networks based on clinical features, diffusion weighted MRI (DWI) and a combination thereof to evaluate the relative importance of these data for predicting functional outcome (modified Rankin Scale (mRS)) at 3 months. Model performances were compared to those of four experienced neurologists predicting mRS of 50 patients based on either clinical features, diffusion and perfusion MRI, or a combination of both.
- Results: A favorable outcome (mRS 0–2) was achieved in 54% of patients, 78% of patients were successfully recanalized. The highest predictive performance was obtained with the model combining DWIs with clinical features. Predictive performances of models and neurologists dropped when only clinical, or only imaging data was provided. All models achieved higher predictive performances than neurologists.
- Conclusions: Both, models and neurologists achieved the best prediction performances based on a combination of clinical and imaging data. However, in contrast to the models, most neurologists showed a significant drop in predictive performance when being provided with imaging data only. Currently, we aim at highlight imaging features most important for functional outcome prediction.
- P08
- 10-Year Trends in Cardiovascular Risk Factors in Switzerland: Non-Traditional Risk Factors Are on The Rise in Women More Than in Men
1
Department of Neurology and Clinical Neuroscience Center, University Hospital Zurich and University of Zurich, Switzerland
2
Department of Biostatistics and Epidemiology, Biostatistics and Prevention Institute, University of Zurich, Switzerland
3
Department of Nuclear Medicine, University Hospital Zurich and University of Zurich, Switzerland
- Background and Aims: Effective control of cardiovascular risk factors (cvrf) is the prerequisite to prevent cardiovascular disease (CVD). Recently, non-traditional cardiovascular risk factors (nt-cvrf) have been discovered to significantly add to cardiovascular risk arising from modifiable traditional cardiovascular risk factors (t-cvrf), such as diabetes or hypertension. In order to discover sex-specific changes that may underlie previously reported inclines in the prevalence of CVD in women, we assessed 10-year trends in the prevalence of cvrf in Switzerland.
- Methods: We acquired data from the governmental Swiss Health Survey. Anonymized data from 2007, 2012 and 2017 were analyzed in a cross-sectional approach, including epidemiological parameters, t-cvrf, and nt-cvrf.
- Results: 51% of all participants (22,134) were female. There was a significant increase in women with full-time jobs (2007: 38%, 2012: 39%, 2017: 44%). We found a rise in stress at work (2007: not available, 2012: 59%, 2017: 66%), sleep disorders (2007: 26%, 2012: 24%, 2017: 29%) and reduced feeling of energy and vitality (2007: not available, 2012: 23%, 2017: 29%), more pronounced in women. The prevalence of hypercholesterolemia and obesity increased over time in both sexes, whereas other t-cvrf like diabetes (5%), hypertension (27%) and smoking (9.4cigarettes/day) remained stable.
- Conclusions: Our results highlight that sex-differences in nt-cvrf exist in Switzerland, with an alarming trend towards a particular increase in women. Further activities in prevention are needed to target particularly nt-cvrf, in order to decrease CVD in women and men.
- P09
- Differences Between Anticoagulated Patients Suffering Ischemic Stroke Versus Intracerebral Hemorrhage
1
Department of Neurology and Stroke Center, University Hospital Basel and University of Basel, Switzerland
2
Clinical Trial Unit, University of Basel, Switzerland
3
Department of Intensive Care Medicine, University Hospital Basel, Switzerland
4
Department of Neurology and Stroke Center, University Hospital Bern, Switzerland
5
Neurology and Neurorehabilitation, University Department of Geriatric Medicine Felix Platter, University of Basel, Switzerland
6
Stroke Center, Klinik Hirslanden Zurich, Switzerland
- Introduction: Data on the relative contribution of clinical and neuroimaging risk factors to acute ischemic stroke (AIS) versus intracerebral hemorrhage (ICH) occurring on oral anticoagulant (OAC) treatment are scarce.
- Methods: Cross-sectional study on consecutive OAC-treated patients presenting with AIS, transient ischemic attack (TIA) or ICH from the prospective observational NOACISP (Novel-Oral- Anticoagulants-In-Stroke-Patients)-Acute registry. We compared clinical and neuroimaging characteristics (small vessel disease [SVD] markers and atherosclerosis) in ICH versus AIS/TIA (reference) using logistic regression.
- Results: Among 734 patients presenting with stroke on OAC treatment (404 [55%] direct oral anticoagulants, 330 [45%] vitamin K antagonists), 605 patients (82%) had AIS/TIA and 129 (18%) ICH. Prior AIS/TIA, coronary artery disease, dyslipidemia and worse renal function were associated with AIS/TIA (aOR [95%-CI] 0.51 [0.32–0.82], 0.48 [0.26–0.86], 0.55 [0.34–0.89], 0.82 [0.75–0.90] per 10 mL/min). Prior ICH, older age, higher admission blood pressure and statin treatment were associated with ICH (aOR [95%-CI] 6.33 [2.87–14.04], 1.37 [1.04–1.81] per 10 years, 1.19 [1.10–1.29] per 10 mmHg, 1.81 [1.09–3.03]). Cerebral microbleeds and moderate-to-severe white matter hyperintensities contributed more to ICH (aOR [95%-CI] 2.77 [1.34–6.18], 2.62 [1.28–5.63]). Aortic arch, common and internal carotid artery atherosclerosis and internal carotid artery stenosis ≥50% contributed more to AIS/TIA (aOR [95%-CI] 0.54 [0.31–0.90], 0.29 [0.05–0.97], 0.48 [0.30–0.76], 0.32 [0.13–0.67]).
- Conclusions: In patients presenting with stroke on OAC, AIS/TIA was 5 times more common than ICH. A high atherosclerotic burden (indicated by cardiovascular comorbidities and extracranial atherosclerosis) and prior AIS/TIA contributed more to AIS/TIA, while SVD markers and prior ICH were stronger determinants for ICH.
- Clinical Trial Registration: https://clinicaltrials.gov; NCT02353585.
- P10
- Mechanical Thrombectomy Versus Best Medical Treatment between 6 and 24 Hours in Patients with Large Vessel Occlusion Not Fulfilling the Defuse-3 And Dawn Criteria
1
Department of Neurology, University Hospital Basel and University of Basel, Basel, Switzerland
2
Department of Neuroradiology, University Hospital Basel, Basel, Switzerland
3
Department of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
4
Clinic for Internal Medicine, Cantonal Hospital Schaffhausen, Schaffhausen, Switzerland
5
Department of Neurology and Stroke Center, Hirslanden Hospital Zurich, Zurich, Switzerland
6
Department of Neurology, University Hospital Zurich and University of Zurich, Zurich, Switzerland
7
Neurology and Neurorehabilitation, University Department of Geriatric Medicine Felix Platter, Basel, Switzerland
8
Department of Intensive Care Medicine, University Hospital Basel, Basel, Switzerland
9
Emergency Department University Hospital Basel and University of Basel, Basel, Switzerland
10
Department of Radiology and Nuclear Medicine, Cantonal Hospital of Lucerne, Lucerne, Switzerland
11
Department of Neuroradiology, EOC Neurocenter of Southern Switzerland, Lugano, Switzerland
12
Department of Neurology and Stroke Center, EOC Neurocenter of Southern Switzerland, Lugano, Switzerland
13
Rheinfelden Rehabilitation Clinic, Rheinfelden, Switzerland
†
Shared first co-authorship.
‡
Shared senior co-authorship.
- Keywords: Ischemic stroke; Large vessel occlusion; Late window; Thrombectomy; Endovascular treatment
- Background: To assess the efficacy and safety of mechanical thrombectomy (MT) in adult stroke patients with anterior circulation large vessel occlusion (LVO) presenting in the late time window not fulfilling the DEFUSE-3 and DAWN (DAD) inclusion criteria.
- Methods: Cohort study of adults with LVO admitted between 6–24 h after last seen well at five participating Swiss Stroke Centers between 2014–2021. Mismatch was assessed by CT or MRI perfusion with an automated software. We excluded patients meeting DAD inclusion criteria and compared those who underwent MT with those receiving best medical treatment alone (BMT) by propensity score weighted regression. The primary efficacy endpoint was a favorable functional outcome at 90 days. The primary safety endpoint was symptomatic intracranial hemorrhage (sICH).
- Results: Among 278 patients with LVO presenting in the late time window, 190 (68%) did not meet the DAD inclusion criteria and thus were included in the analyses. Of those, 102 (54%) received MT. Patients in the MT group had higher odds of favorable outcomes compared to the BMT group (mRS 0–2: aOR 1.57 [1.02–2.44], p = 0.04; mRS shift: cOR 0.68 [0.47–0.99], p = 0.045). Rates of sICH did not differ (MT vs BMT: 5% vs 2%, p = 0.63); patients in the MT group had lower odds of all-cause death within 90 days (aOR 0.68 [0.43–1.08], p = 0.10).
- Conclusions: Two out of three patients with LVO presenting in the late window did not meet the DAD inclusion criteria. In these patients, MT was associated with higher odds of favorable functional outcomes without increased rates of sICH.
- P11
- The Role of Competing Stroke Etiologies in Stroke Patients with Atrial Fibrillation
1
Department of Neurology and Stroke Center, University Hospital Basel and University of Basel, Switzerland
2
Clinical Trial Unit, Department of Clinical Research, University Hospital Basel and University of Basel, Switzerland
3
Department of Intensive Care Medicine, University Hospital Basel, Switzerland
4
Department of Neurology, Inselspital, University Hospital and University of Bern, Switzerland
5
Neurology and Neurorehabilitation, University Department of Geriatric Medicine Felix Platter, University of Basel, Switzerland
6
Stroke Center, Klinik Hirslanden, Zürich, Switzerland
- Background: Oral anticoagulation (OAC) is the treatment of choice in secondary prevention in stroke related to Atrial Fibrillation (AF). Nevertheless, stroke recurrence may occur under OAC, indicating potentially different stroke etiologies
- Methods: Observational study based on the prospective “Novel oral anticoagulants in stroke patients” (NOACISP-Longterm)-registry (inclusion period 2013–2020) enrolling stroke patients with AF. Etiology of index and recurrent stroke was classified according to the TOAST criteria. We analyzed the stroke etiologies and association between etiology and incident recurrent ischemic stroke using Cox proportional hazard models (adjusted for confounding demographic and vascular factors).
- Results: Among 959 patients (median age 81 [74,86], 46% female) index stroke etiology was available in 912. In patients without recurrent ischemic stroke, index stroke was more often cardioembolic (78.0% vs. 65.3%) and less often classified as Large-Artery Atherosclerosis (LAA) (1.7 vs 5.6%) or more than one possible etiology (13.1% vs 26.4%). Overall, 72 patients had recurrent stroke (7.9%) during a median follow-up time of 2 years. For the distribution of the index and recurrent stroke etiology see Figure 1. An index stroke due to LAA (aHR 3.42 [1.22, 9.62], p = 0.038) or more than one possible etiology (aHR 2.21 [1.26, 3.86], p = 0.007) was associated with recurrent stroke.
- Conclusions: In patients treated with OAC for AF-stroke, index stroke due to LAA or more than one possible etiology was associated with recurrent ischemic stroke. Patients should undergo thorough etiological work-up to identify other stroke etiologies.
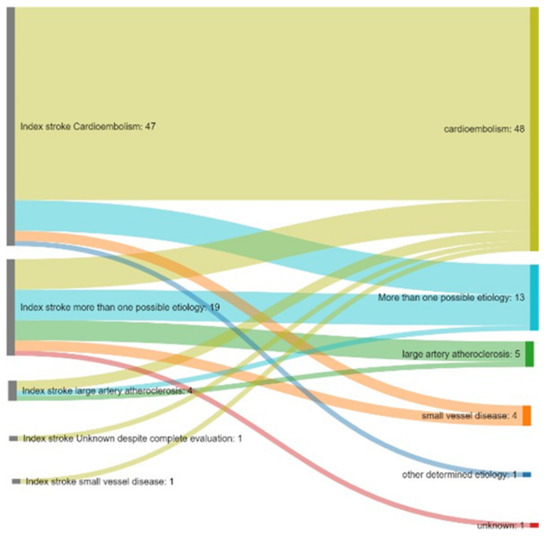
Figure 1.
Detailed Illustration of patients with recurrent ischemic stroke. On the left side, the index stroke etiology is noted, on the right side the etiology of the recurrent stroke based on the TOAST classification. The flows represent the changes between the index and recurrent stroke etiology.
- P12: withdrawn
- P13
- Lack of Susceptibility Vessel Sign in Patients with Malignancy-related Acute Ischemic Stroke
1
Department of Neurology, Inselspital, Bern University Hospital, and University of Bern, Switzerland
2
Institute for Diagnostic and Interventional Neuroradiology, Inselspital, Bern University Hospital, and University of Bern, Switzerland
3
Department of Neuroradiology, University Hospital, Freiburg, Germany
4
Neurology Department, University Hospital of Basel, University of Basel, Basel, Switzerland
5
Department of Oncology, Inselspital, Bern University Hospital, and University of Bern, Switzerland
†
Equal contribution.
- Background and Purpose: Platelet and fibrin-rich composition of retrieved thrombi in patients with acute ischemic stroke (AIS) are associated both with active malignancy and the lack of susceptibility vessel sign (SVS) on MRI. This study analyzed the association between SVS status and the presence of active malignancy in AIS patients that underwent mechanical thrombectomy (MT).
- Methods: Single-centered, retrospective and cross-sectional study including consecutive patients with admission MRI treated for AIS with MT between January 2010 and December 2018. SVS was evaluated on susceptibility weighted imaging (SWI). Patients with active malignancy were identified via the clinical information system. Odds ratio (OR) and adjusted OR (aOR) were calculated to determine the association between SVS negativity and active malignancy. Performance of predictive models with and without SVS status were assessed by calculating the areas under the Receiver Operating Characteristics curve (auROC).
- Results: Of the 577 AIS patients with assessable SVS status, 40 (6.9%) had a documented active malignancy and 72 patients (12.5%) showed no SVS. The lack of SVS was strongly associated with active malignancy (OR 5.07, 95% CI 2.52–10.18, p < 0.001), even after adjusting for other common malignancy-biomarkers (aOR 4,85, 95% CI 1.94–12.11, p = 0.001). The auROC of predictive models including demographics and common malignancy-biomarkers decreased from 0.85 to 0.81 when SVS status was excluded.
- Conclusions: The lack of SVS on baseline MRI is associated with active malignancy in patients with AIS eligible for MT. Considering SVS status may increase the chances of detecting occult malignancy in patients with AIS.
- P14
- Machine Learning Analysis to Develop Outcome Prediction Scores for Posterior Circulation Occlusions: Internal Validation of the Posterior Circulation Clot Burden Score (Pc-CBS)
1
Stroke Center, Neurology Service, Lausanne University Hospital and University of Lausanne, Switzerland
2
Interventional Neuroradiological Unit, Service of Diagnostic and Interventional Radiology, Lausanne University Hospital and University of Lausanne, Switzerland
- Background and Purpose: Early evaluation and prompt treatment are key elements for the correct management of acute ischemic stroke (AIS). The early identification of an accurate prognosis including advanced neuroimaging currently lacks a posterior circulation clot burden score (pc-CBS) able to correlate vascular patency status to long-term functional outcome.
- Methods: We retrospectively reviewed 415 CTA/MRA images of patients from the Acute Stroke Registry and Analysis of Lausanne (ASTRAL) with posterior circulation occlusion to: (1) assess vascular patency of 13 segments of the posterior circulation system (2) calculate the interrater variability for assessment of vascular patency, (3) develop a prediction score of 3-month functional outcome based on standard logistic regression models, and (4) compare logistic regression models to machine learning algorithms in order to increase performance of the model.
- Results: The interrater agreement is substantial for vascular patency of the Circle of Willis and posterior circulation segments. We expect to develop a prediction model with a good performance, which will be able to correlate the pattern of vascular patency to 3-month functional outcome, as it is already the case for anterior circulation strokes with the Clot Burden Score. We expect to increase performance of the model by applying xgboost and neural network machine learning algorithms.
- Conclusions: Such score has the impact to support the neurologist in the definition of outcome since the early phases of AIS. External validation is planned in order to confirm its effectiveness on larger cohorts. Furthermore, it may aid develop more accurate prediction models when associated to other clinical and neuroimaging variables.
- P15
- The Triad of Cavernous Sinus Thrombosis, Internal Carotid Artery Vasculitis and Acute Ischemic Stroke as A Complication of Acute Bacterial Sphenoid Sinusitis
1
Stroke Center, Neurology Service, Lausanne University Hospital and University of Lausanne, Switzerland
2
Ear-Nose-Throat Service, Lausanne University Hospital and University of Lausanne, Switzerland
3
Diagnostic Neuroradiological Unit, Service of Diagnostic and Interventional Radiology, Lausanne University Hospital and University of Lausanne, Switzerland
- Background and Purpose: Acute bacterial sinusitis is a common affection of the upper airways that rarely complicates with dissemination to the nervous system. We describe a first case series and suggest the pathophysiological mechanism of complicated acute bacterial sphenoid sinusitis (cABSS) presenting with the triad, cerebral venous thrombosis (CVT) of the cavernous sinus, internal carotid artery (ICA) vasculitis and acute ischemic stroke (AIS).
- Methods: We conducted a retrospective analysis of patients admitted to Lausanne University Hospital between 2005 and 2020 with cABSS complicated by CVT and concomitant AIS from ICA vasculitis (N = 3) and reviewed literature.
- Results: Median age was 38 years and the pathogens responsible for cABSS were S. aureus (n = 2) or undetermined (n = 1). All patients had a CVT of the cavernous sinus, evidence of carotid vasculitis and middle cerebral artery stroke. They were all treated with endoscopic surgical drainage by sphenoidotomy, broad-spectrum antibiotics and antithrombotics. At 3 months, 66% of patients had a good functional outcome, and one died.
- Discussion: Simultaneous CVT and ICA vasculitis with AIS is a rare complication of acute bacterial sphenoid sinusitis. It can have a good outcome when correctly treated by endoscopic surgical drainage by sphenoidotomy, broad-spectrum antibiotics and antithrombotics.
- P16
- Multispectral Optoacoustic Imaging (MSOT) of Cerebrovascular Disease
1
Department of Neurology, Clinical Neuroscience Center, University Hospital Zurich and University of Zurich, Zurich, Switzerland
2
Institute for Biomedical Engineering and Institute of Pharmacology and Toxicology, University of Zurich, Zurich, Switzerland
3
Institute for Biomedical Engineering, Department of Information Technology and Electrical Engineering, ETH Zurich, Zurich, Switzerland
4
Department of Ophthalmology, University Hospital Zurich, University of Zurich, Zurich, Switzerland.
5
Department of Neurology, Clinical Neuroscience Center, University Hospital Zurich, Zurich, Switzerland and Cereneo Center for Neurology and Rehabilitation, Vitznau, Switzerland
6
Institute of Diagnostic and Interventional Radiology, University Hospital Zurich, Zurich, Switzerland
†
Contributed equally.
- Stenosis of the internal carotid artery is a common cause of ischemic stroke. Current treatment recommendations focus on stenosis degree and include medical treatment, endovascular stenting as well as surgical carotid endarterectomy. Ultrasound is the method of choice to establish stenosis degree, but it is limited with respect to characterization of the plaque or vessel wall morphology. However, there is increasing evidence that plaque composition critically determines risk of rupture.
- Multi-spectral optoacoustic tomography (MSOT) is an emerging non-invasive approach based on acoustic echoes emitted by biological tissues when illuminated with short pulses of light. MSOT has the unique potential to acquire disease-specific molecular biomarkers in addition to morphological/flow assessment by conventional ultrasound methods. For carotid imaging, assessment of lipid content and oxygenation state are of particular interest, as lipid accumulation and plaque vascularization are key indicators of plaque formation, progression towards instability and stroke risk.
- We aimed at establishing a link between the lipid- and oxy/deoxyhemoglobin signals of the carotid artery/plaque and the superficial temporal artery (STA) and the type (atherosclerosis versus inflammation) and severity of cardiovascular disease. To this end, the in vivo data was acquired from carotid arteries of eight patients with cerebrovascular disease and from temporal arteries in three patients with suspicion of giant cell arteritis (GCA), a large vessel vasculitis. Data were co- registered to ultrasound findings. Lipid signal was detected mainly on the vessel wall in patients with cerebrovascular disease. More patients will be included and data presented at the conference.
- P17
- Stenting in Internal Carotid Artery Dissection—A single center Cohort Analysis
1
Department of Neurology, University Clinic Tulln, Karl Landsteiner University of Health Sciences, Austria
2
Department of Radiology, University Clinic Tulln, Karl Landsteiner University of Health Sciences, Austria
- Introduction: Carotid artery dissection is the leading cause of ischemic stroke in the young population. In up to 25% it is the origin of embolic stroke in this age group. In 90% the extracranial portion of the internal carotid artery (ICA) is affected. The goal of treatment is to prevent (recurrent) strokes and to avoid complications.
- Methods and Materials: 15 patients with spontaneous extradural ICA dissection and acute ischemic stroke symptoms at onset were included in our retrospective analysis. 8 patients were treated with endovascular stenting, 7 patients with medical therapy strategy.
- Results: In stenting group 75% were presented with ICA occlusion, 25% with >50% ICA stenosis. The stenting group was clinical more severely affected with mean NIHSS 10 ± 6 versus 3 ± 6 at stroke onset, whereas after 3 months in each group a good clinical outcome was reached (mRS1 ± 1), mean NIHSS 3 ± 3 versus 2 ± 4. Complete recanalization rate was 88% (stent) versus 57% (medical) after 6 months. Acute phase complications with new ischemic lesions on brain imaging was seen in 38% (stent) versus 29% (medical). Symptomatic intracranial hemorrhage occurred in 12% (stent) versus 14% (medical).
- Discussion: In our analysis we could show, that acute stenting in ICA dissection, especially in neurological severely affected patients at stroke onset, is save and feasible.
- Conclusions: We present the preliminary results of a retrospective cohort analysis from our clinic.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).