Abstract
Intra-abdominal and gastrointestinal mucormycosis are less frequent than rhino-orbito-cerebral and pulmonary mucormycosis, but highly lethal. Their diagnosis remains challenging due to the non-specific clinical presentation. We collected English-language cases of intra-abdominal and gastrointestinal mucormycosis in non-haematological and non-neonatal patients published up to October 2024. This review analysed the epidemiological, clinical, and therapeutic charts of 290 cases. A proportion of 53.4% were reported from India and the USA. The main predisposing conditions were diabetes, solid organ transplant, ICU, and corticosteroid treatment. The most common site was the stomach (53.8%). Gastrointestinal perforation, skin breakdown, and abdominal wall infection were sources of intra-abdominal localisation. The most common symptoms were abdominal pain, vomiting, and gastrointestinal bleeding. The diagnosis relied on histology (93.8%), mycology with microscopy and culture (38.8%), and molecular methods (9.9%). Mortality (52.9%) was lower when treatment was intravenous amphotericin B, combined or not with surgery. Prompt treatment, essential for a favourable outcome, relies on early suspicion and diagnosis. Gastrointestinal and intra-abdominal mucormycosis should also be suspected in patients admitted in ICU with ventilation/nasogastric tube and corticosteroids and those with abdominal trauma or surgery, presenting abdominal distension, pain, and GI bleeding. Mycological diagnosis including direct examination, culture and Mucorales qPCR on tissue should assist with rapid diagnosis and thus treatment.
1. Introduction
Mucormycoses are life-threatening invasive infections caused by fungi of the order Mucorales, which until the last decade were known as Zygomycetes. Based on molecular phylogenetic analysis, taxonomy has evolved, the phylum Zygomycota has been abandoned, and these opportunistic human pathogens have been placed in the order Mucorales within the families Cunninghamellaceae, Lichtheimiaceae, Mucoraceae, Saksenaceae, and Syncephalastraceae [1,2]. Of more than 30 pathogenic species, those belonging to the genera Rhizopus, Mucor, and Lichtheimia (formerly Absidia) are reported to be responsible for most human mucormycoses [2,3]. Their identification has often been based on phenotypic characteristics, which are currently considered to be less accurate than molecular identification.
The worldwide increase in the number of cases during the last decades and the outbreak of mucormycosis in the context of the COVID-19 pandemic led the WHO to designate Mucorales as priority pathogens [4,5,6,7,8,9,10]. Infection usually occurs in debilitated patients such as those with haematological malignancies and bone marrow transplantation, solid organ transplantation (SOT), iron overload, diabetes mellitus, and the use of corticosteroids [3]. However, there have been reports of mucormycosis in immunocompetent hosts with trauma or burns over the last three decades [11,12,13,14,15,16].
Pulmonary, rhinocerebral, sinonasal, sino-orbital, and cutaneous localisations are the most common, accounting for more than 70% of cases. Gastrointestinal (GI) localisation is the least common, estimated at 5–13% of mucormycosis cases, and other intra-abdominal (IA) localisations are even rarer [3,17,18,19]. Their diagnosis remains a challenge due to the non-specific clinical presentation, especially when they occur outside the usual contexts such as those with haematological malignancies, neutropenia, SOT, and neonates [20,21].
We report here a comprehensive review of human mucormycoses with GI and IA localisations in patients without haematological malignancies and outside the neonatal context.
2. Patients and Methods
2.1. Search
We reviewed IA and GI mucormycoses cases from PubMed according to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines for systematic reviews [22].
Each of the following key words were used: human, mucormycosis, zygomycosis, phycomycosis, abdominal, gastric, intestinal, colic, peritoneal, splenic, hepatic, disseminated, Rhizopus, Mucor, Lichtheimia, Absidia, Rhizomucor, Apophysomyces, Saksenaea, Syncephalastrum, Cunninghamella, and Mucorales. Renal and urinary tract infections (UTIs) without abdominal or peritoneal cavities involvement were not included in this review. Lists of articles in CSV (comma-separated values) format were generated and saved from PubMed, and then converted to Excel format.
The search was completed by reviewing the reference sections of original articles, of reviews, case series including those with pooled analysis and case reports and adding those that were not present in the PubMed CSV and summary files. The same inclusion criteria were used as for the PubMed search.
The inclusion criteria for this review were as follows: (1) articles in the English language; (2) absence of neonatal context and/or haematological disease and/or documented neutropenia; (3) documentation of proven Mucorales infection either histologically or by culture, or by molecular methods according to the European Organisation for Research and Treatment of Cancer (EORTC) and the Mycoses Study Group Education and Research Consortium (MSGERC) criteria for invasive fungal disease [23]; (4) cases with documentation of age and sex of the patient, underlying diseases/predisposing factors, site(s) of infection, methods of diagnosis, treatment, and outcome. Poorly described cases, including those from reviews and pooled cases, were excluded.
Data of sex, age, underling conditions, infection site, fungal agent, concomitant other infections, diagnostic methods (cytopathology, microscopic direct examination, cultures, and molecular methods), and antifungal and surgical treatment and outcome at 3 months after diagnosis were collected in an Excel table.
2.2. Definitions
GI and IA mucormycoses were defined as proven infections according to the EORTC and MSGERC criteria for invasive fungal diseases [23], the sites of infection being oesophagus, stomach, and small and large bowel and, respectively, abdominal wall, peritoneum, omentum, mesenteron, liver, spleen, and adrenal gland.
2.3. Statistics
A descriptive analysis of data and maps was performed using Microsoft Excel®. Categorical variables were expressed as the number of cases and as a percentage of the total (%). Comparisons between groups were made using Fisher’s exact test for continuous variables. p values < 0.05 were considered statistically significant.
3. Results
Our literature search of PubMed yielded a total of 363 articles. After excluding duplicate, non-English, and irrelevant articles, a total of 142 studies reported individual patient data. Together with the studies retrieved from the additional search of reference sections, 116 cases from 108 articles for a total of 290 cases were included (Supplementary Tables S1 and S2). A flowchart of the sorting process is shown in Figure 1.
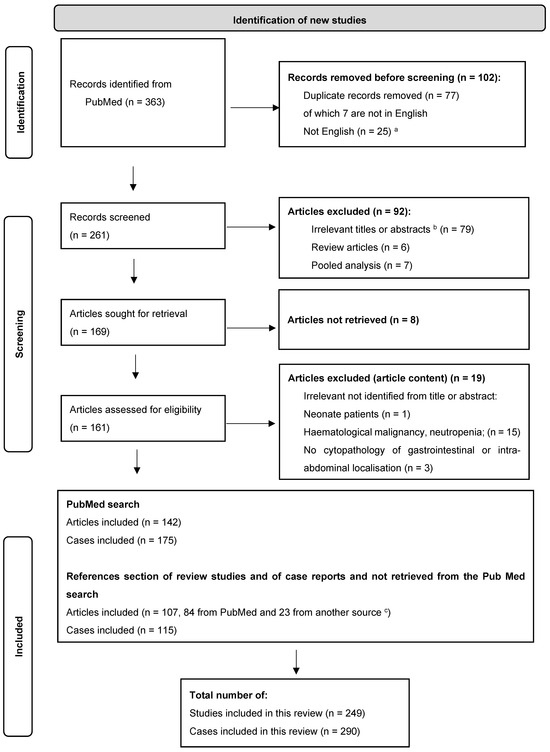
Figure 1.
PRISMA 2020 flow diagram [22]. a. Of these, 9 articles reported cases which met the other inclusion criteria of gastrointestinal and intra-abdominal mucormycosis: Spanish language (n = 2: 1 gastric, 1 intestinal), French (n = 2: 1 hepatic, 1 disseminated with hepatic, splenic, and gastric involvement), German (1 gastro-duodenal), Italian (1 peritoneal), Czech (1 gastric), Norwegian (1 gastric), Chinese (1 gastric). b. Irrelevant title or abstract: not mucormycosis (e.g., blastomycosis); neonatal or haematological, including neutropenia, contexts; no intra-abdominal or digestive proven localisation. c. Other sources: ScienceDirect.com, Elsevier, journal site (e.g., The American Journal of Gastroenterology—ACG).
The first documented case was published in 1960. The chronological increase in the number of cases since the 2000s is illustrated in Figure 2.
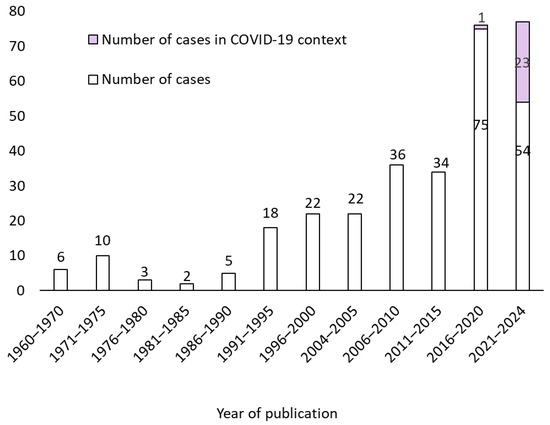
Figure 2.
Number of published cases per year from 1960 to October 2024.
Among the included studies, the countries reporting the highest number of GI/IA mucormycosis were India (93/290, 32.06%), USA (62/290, 21.37%), South Africa (19/290, 6.55%), Spain (14/290, 4.83%), and China (13/290, 4.48%) (Figure 3, Supplementary Table S1).
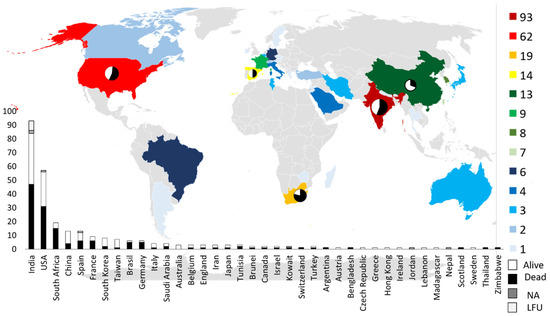
Figure 3.
Geographical distribution of cases. NA, not available; LFU, lost to follow-up.
3.1. Demographic Data and Underling Conditions
Age information was available for 288 cases. The median age of included GI/IA mucormycosis patients was 45 years [1.5 month–86 years] and the majority of them were men (192/288, 66.67%). Thirty cases were reported in patients under 18 years, and 20 patients have age under 16 years.
Data of underling disease or condition were available for 281 cases. Their frequency varied across the decades and the countries (Table 1 and Supplementary Figures S1 and S2). A majority of cases (220/281, 78.01%) had two or more underling diseases/conditions. Diabetes was the most common comorbidity (70/282, 24.82%), with no significant difference between men (39/70, 55.71%) and women (31/70, 44.29%). Of the patients with diabetes, 14.8% presented with ketoacidosis (KA).

Table 1.
Underlying disease or condition. The sum of underlying diseases/conditions is greater than 291 (100%) because in most cases there was more than one. Percentage calculated only for number ≥ 5. CAPD, Continuous ambulatory peritoneal dialysis; HIV, human immunodeficiency virus; AIDS, acquired immune deficiency syndrome; ARDS, acute respiratory distress syndrome; ECMO, extra corporeal membrane oxygenation; ICU, intensive care unit. a. Metabolic acidosis does not include diabetic keto-acidosis. b. Other: (i) GI/IA, pelvic condition (n = 25): gastritis (n = 3), gastric erosion, adenocarcinoma, portal gastropathy, gastroparesis, peptic ulcer history, gastro-enteritis, Salmonella enteritis, C. difficile colitis, pan-colitis, digestive adenocarcinoma, diarrhoea, pancreatitis, peritoneal infection/peritonitis history (n = 6), breach in CAPD sterile technique, percutaneous drainage of renal collection, postpartum haemorrhage, testicular cancer + chemotherapy, sider bite (n = 1); (ii) thoracic/pulmonary condition (n = 18): ARDS (9), COPD (n = 3), respiratory failure, emphysema, H1N1 pneumonia, pulmonary tuberculosis, pleural infection, chest stab, thoracic surgery (n = 1); (iii) infection history (n = 4): typhoid fever (2), rhino-facial mucormycosis, P. falciparum malaria (n = 1); iron overload/transfusions (n = 5); (iiii) miscellaneous (n = 12): tobacco use (n = 5), burn (n = 2), back trauma, pesticide ingestion, cytopenia, haemolytic uremic syndrome, motor hemiplegia (n = 1).
SOT (46/282, 16.31%) with kidney and liver transplant was the most frequent (20/282, 7.09% and 15/282, 5.31%, respectively), and renal failure (36/282, 12.76%) were the most frequent comorbidities after diabetes. Abdominal surgery was reported in 42/282 cases (14.89%), with 37.5% (18/48) being performed for with GI perforation or peritonitis.
Cases associated with COVID-19 accounted for 8.51% of all cases and for 18.46% (24/130) of cases since 2020. Of the 24 cases, 14 (58.33%) occurred in India.
Intensive care unit (ICU) stay (67/282, 23.75%) and corticosteroid treatment (45/282, 15.96%) other than that prescribed in the context of SOT were common conditions in GI/AI mucormycosis cases.
Underlying conditions varied according to the GI and IA localisation (Figure 4). GI localisations had varied underling conditions. On the contrary, IA abscesses and abdominal wall infection abdominal injury and surgery were the main, whereas ICU stay was not reported.
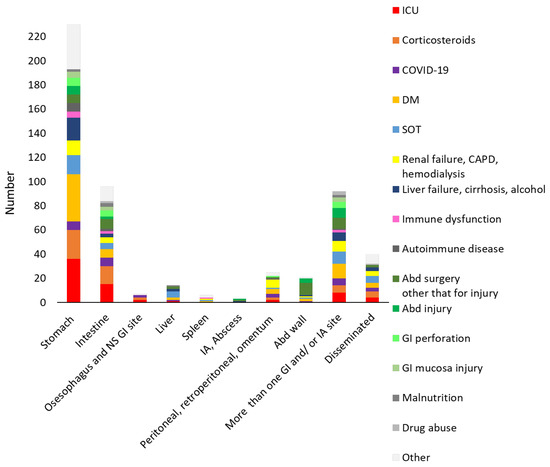
Figure 4.
Underlying diseases and conditions distribution according to the gastrointestinal (GI) and intra-abdominal (IA) localisations. For each localisation, the sum of underlying diseases/conditions is greater than the number of each localisation because in most cases there was more than one. ICU, intensive care unit; DM, diabetes mellitus; SOT, solid organ transplant; CAPD, continuous ambulatory peritoneal dialysis; NS, not specified. “Other” includes the “other” category as summarised in Table 1.
3.2. Clinical and Paraclinical Presentation
The clinical and paraclinical characteristics of the cases (adult and paediatric) are shown in Supplementary Table S1. Of the 290 cases, 4 had no more precise information on the site than “GI” or “digestive”. In 59 cases, more than one GI and/or IA site was reported, and in 24 cases, the mucormycosis was disseminated.
Overall, stomach (156/290, 53.79%) was the most common site, followed by intestine (78/290, 26.89%), abdominal wall (26/290, 8.93%), and peritoneum/retroperitoneum (24/290, 8.24%) (Figure 5). The distribution according to patient age was different in patients younger than 16 years, with the intestine (11/20, 55%) being the most common site, followed by the stomach (5/20, 25%), liver (3/20, 15%), and peritoneum (2/20, 10%).
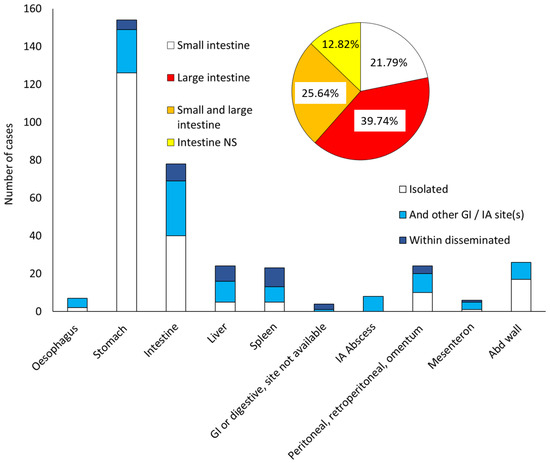
Figure 5.
Gastrointestinal (GI) and intra-abdominal (IA) mucormycosis sites. Abd, abdominal; NS, not specified. Within disseminated: disseminated cases of mucormycosis with a GI and/or IA localisation.
The large intestine (cecum, colon, rectum, anal canal) was most commonly involved (31/78, 39.74%), followed by the small intestine (duodenum, ileum, jejunum) (17/78, 21.79%) or both.
According to publication date, the distribution of sites differs after 2000, with fewer cases of disseminated mucormycosis and more cases of stomach, intestine, and GI/IA with more than one site (Figure 6).
Figure 6.
Site distribution (%) according to the publication period. Abd, abdominal.
3.3. Clinical Presentation
Symptoms were specified for 249 cases. They were non-specific with abdominal pain or discomfort (100/249, 40.16%) being the most common, followed by vomiting/nausea (51/249, 20.48%), GI bleeding (47/249, 18.87%), and fever (45/249, 18.07%) (Figure 7). All symptoms are summarised in Table 2.
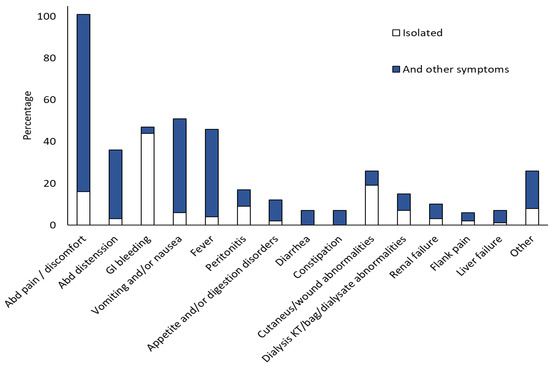
Figure 7.
Symptoms rate (percentage). GI, gastrointestinal. Abd, abdominal. Dialysis catheter or bag or dialysate abnormalities (clogged Tenckhoff catheter, cloudy dialysis bag, or dialysate fluid). Other symptoms: acute abdomen, bowel movements, mass in epigastrium, hepato-splenomegaly, splenomegaly (HSM), paralytic ileus, pneumoperitoneum, rectum mucosal sloughing, anaemia, multi-organ failure (MOF), sepsis, and symptoms linked to other site in disseminated cases (cardiac tamponade, chest pain, dyspnoea, mental confusion).

Table 2.
Symptoms distribution for the 249 cases with available information. IA, intra-abdominal: peritoneal (n = 14), peritoneal + intra-abdominal abscess (n = 4) infection, intra-abdominal abscess. Abd. Wall, abdominal wall. GI, gastrointestinal. a. Dialysis catheter or bag or dialysate abnormalities (clogged Tenckhoff catheter, cloudy dialysis bag or dialysate fluid). b. Other symptoms: acute abdomen, bowel movements, mass in epigastrium, HSM, hepatosplenomegaly (n = 2), paralytic ileus, pneumoperitoneum (n = 2), rectum mucosal sloughing, anaemia, multi-organ failure (MOF), sepsis, and symptoms linked to other site in disseminated cases (cardiac tamponade, chest pain, dyspnoea, mental confusion). c. Other sites: spleen (n = 5), liver (n = 3), oesophagus (n = 1), mesenteron (n = 1).
Endoscopy was reported in 127/291 cases of mucormycosis: 93 were gastric, 4 were gastric with another intra-abdominal site other than the intestine, 6 were gastric and intestinal, 16 were intestinal, and 6 were disseminated with gastric or intestinal localisation.
Ulcer or erosion (96, 75.6%) and necrosis (44, 34.64%) were the main endoscopic features in both gastric and intestinal lesions. These were followed by the presence of exudate, mainly green or greyish (21, 16.53%), bleeding (20, 15.74%), infiltration or proliferative lesion (19, 14.96%), and mucosal inflammation or gastritis (13, 10.23%). Necrosis was reported more frequently in gastric localisation (34.64%), whereas mucosal inflammation or congestion was reported more frequently in intestinal localisation (Figure 8).
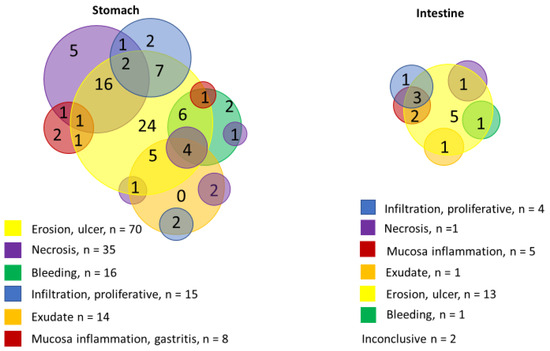
Figure 8.
Endoscopic features distribution according to the gastric versus the intestinal localisation.
CT scan findings were reported in 114 cases and were not specific. Their characteristics are summarised in Supplementary Table S1.
3.4. Diagnostic
Diagnostic methods and results are summarised in Supplementary Table S2. In 272/290 patients, cytopathology was performed on biopsy, on tissue specimen obtained during surgery and on the contents of IA collection or abscess, showing large, irregular, non-septate hyphae. In 87 cases, cytopathology was performed only on biopsy, in 112 cases only on tissue sample and in one case only on abscess content. The diagnosis was made ante-mortem in one case and post-mortem in 45 (16.36%) cases, of which 38 were autopsies and 7 post-mortem biopsies.
A basic mycological diagnosis which included microscopy and/or fungal culture was reported in 104/271 (38.37%) cases: 30 with direct examination (DE) and culture, 73 with culture only, and one with DE only. In total, 30 cases were positive by DE and 90 by culture. Of these, 77 were GI or IA specimens, 6 were GI or IA and other sites, and 7 were other sites (2 peritoneal catheter tips, 1 peritoneal dialysis bag, 1 blood culture, 1 lung specimen, 1 sputum, and 1 skin). Of the 82 cases with a positive culture from a GI and/or IA specimen, 25 were from the stomach, 22 from the abdominal wall, and 16 from the peritoneum. In 84 cases, both cytopathology and mycology were performed. In 17 cases, the diagnosis was based on mycology because the cytopathology was negative, and in 14 cases, the diagnosis was based on cytopathology because the mycology was negative.
Molecular diagnosis, based on PCR and sequencing of rDNA regions, was performed in 27 cases: 15 on tissue samples, mostly on formalin-fixed and paraffin-embedded tissue (FFPET), and 12 on fungal culture for accurate identification.
Genus and species identification were available for 94/290 (32.41%) cases: 39 cases with genus identification and 53 cases with species identification, one case where cytopathology with immunochemistry could not differentiate between Rhizomucor sp. and Rhizopus sp. and one case where the molecular method on FFPET could not differentiate between R. oryzae and R. sexualis (Table 3).

Table 3.
Genus and species identification for the 95 cases for which it was reported.
Rhizopus, Mucor, Apophysomyces, and Lichtheimia were the most commonly isolated genera, with differences depending on the site of infection (Figure 9). Saksanea vasiformis and Apophysomyces were more frequently isolated from abdominal wall infections.
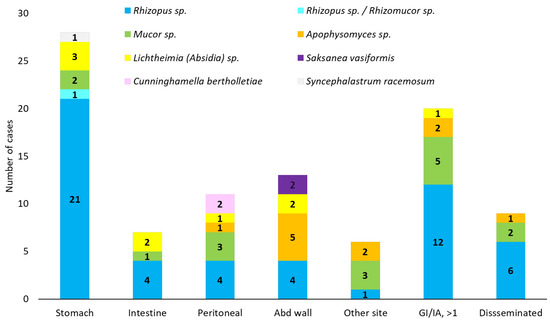
Figure 9.
Mucorales genus distribution according to the gastrointestinal (GI) and intra-abdominal (IA) localisation. Abd, abdominal. GI/IA, >1, GI/IA localisation with more than 1 site: Mucor sp. (3 with stomach infection, 2 with peritoneal infection). Disseminated: Rhizopus sp., all cases were from USA and Europe.
Bacterial (Acinetobacter sp., Bacteroides fragilis, Clostridium difficile, Enterobacter spp., Enterococcus spp., Escerichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Stenotrophomonas maltophila, Serratia marcescens, Satphylococcus spp., Streptococcus viridians, Legionella pneumophila, Mycobacterium tuberculosis complex), viral (SARS-CoV2, HIV, H1N1 influaenzae, CMV, HVA, HVB, HVC), fungal (Candida spp., Aspergillus spp., Pneumocistis jirovecii) or parasitic (Strongyloides stercoralis, Schistosoma sp., Taenia solium cysticercosis, Plasmodium falciparum, Toxoplasma gondii) co-infections were reported in 75/290 (25.6%) of the patients. They are summarised in Supplementary Table S2.
3.5. Management and Outcome
The management was documented in 285 out of 290 cases (Supplementary Table S2). In 40 out of 286 cases (29 diagnosed post-mortem), no treatment was recorded. The treatment modalities included antifungal therapy (AFT) (69/246, 28.16%), surgical interventions (41/246, 16.67%), and a combination of surgery and AFT (127/246, 51.62%). In eight cases, the intervention was limited to the removal of the peritoneal catheter and in two cases, to suturing the gastric ulcer.
Of the 203/290 (70%) cases for which AFT was reported, 3 did not specify the molecule. Amphotericin B (Amp B) intravenous derivatives were utilised as a first-line therapy, with Amp B deoxycholate (86/200, 43%), followed by the lipid formulations liposomal Amp B (79/200, 39.5%) and Amp B lipid complex (6/200, 3%). High-dose (≥5 mg/kg/d) administration of an Amp B lipid formulation was utilised in 34 cases. AmpB administered either as a monotherapy or in combination with other antifungal agents. In one case (abdominal wall fasciitis), Amp B deoxycholate was employed as a topical agent. Azoles, such as pozaconazole (PSZ) and isavuconazole (ISV), were predominantly utilised as maintenance therapy. PSZ was used as a first-line therapy (4/201, 2%), in combination (2/201, 1%), in combination and maintenance (3/201, 1.47%), and maintenance (28/201, 13.93%) therapy. Similarly, ISV was used as first line (2/201, 1%), in combination (2/201, 1%), and maintenance (3/201, 1.47%) therapy. Itraconazole (ITZ) was utilised as maintenance therapy in 3/201 (1.47%) cases, while fluconazole (FCZ) and ketoconazole (KTZ) were employed as a first-line therapy in 3 and 1 cases, respectively. Micafungin and caspofungin were used in combination in 7/201 (2.48%) and 2/201 (1.47%) cases, respectively. In conjunction with the administration of AFT and/or surgical intervention, a reduction in immunosuppression was reported in 16/39 (41.02%) patients with SOT for whom treatment was specified.
Outcome information at 90 days was available for 272 cases, and the 90-day mortality rate was 52.94% (see Supplementary Table S2). This mortality rate differed significantly (p < 0.01) according to the treatment regimen, with the highest mortality rate (83.78%) being observed in patients treated only with surgery, in comparison to all other main regimens (see Figure 10).
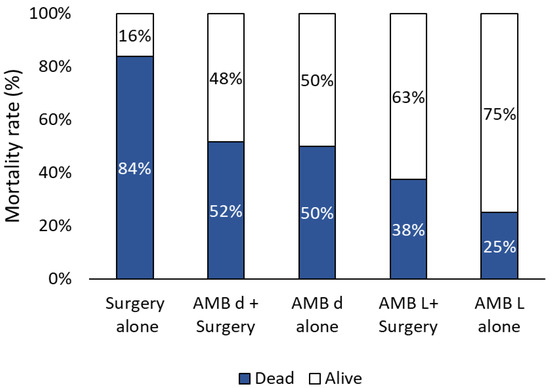
Figure 10.
Outcome (%) according to the main treatment regimens. AMB d, amphotericin B deoxycholate. AMB L, amphotericin B lipid formulations.
No significant differences were observed among the other treatment regimens, despite the lower mortality rate observed in subjects treated with Amb lipid formulations.
The mortality rate exhibited variation across different countries (Figure 3) and according to the infection sites (Figure 11). No significant differences were observed based on age, with a median age of 45 years for both survivors (0.5 y–82 y) and non-survivors (0.13 y–86 y) and between adults (52.89%) and children (53.33%).
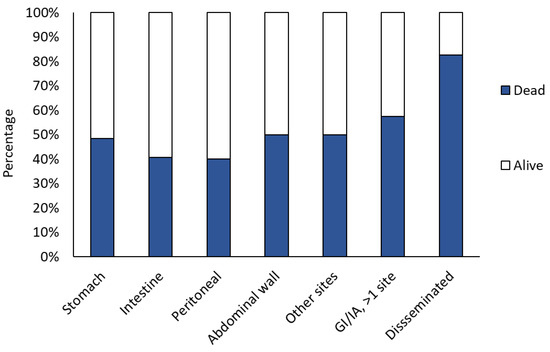
Figure 11.
Outcome percentage according to the infection site. GI, gastrointestinal; IA, Intra-abdominal.
4. Discussion
This comprehensive review of GI and/or IA mucormycosis in non-neonatal and non-haematological contexts collected data on the epidemiology, diagnosis, management, and outcome of 290 cases between 1960 and 2024.
It is not possible to estimate the incidence or prevalence of GI and IA mucormycosis, but in the present study, the number of reported confirmed cases increased after 2010. This may reflect either a true increase in GI and/or IA mucormycosis due to increased awareness and improved diagnostic methods, or more reports of this fungal infection. For example, the outbreak of mucormycosis associated with the COVID-19 pandemic, particularly in India, led to the WHO issuing a warning on this infection. The overall prevalence of mucormycosis in India was estimated to be almost 70 times higher than that in the global data [9]. However, in this study, the prevalence of GI and IA mucormycosis in children and adults, without haematological disease and outside the neonatal context, in India was less than twice that of the USA, which ranked second in case numbers. This may be due to a lower number of cases of GI/IA infections in this population compared to India, as GI cases were reported mainly in premature neonates prior to 1990 [21], but also to the overall similar underlying diseases and conditions.
Diabetes mellitus, SOT, especially renal, and renal failure were the most common underlying diseases of GI and IA mucormycosis, with frequencies that may vary between countries (Supplementary Figure S2). Among countries with more than 10 reported cases, the percentage of cases with diabetes and renal failure (5%) was lower in South Africa, where abdominal trauma predominated (26%), and that of SOT was higher in the USA (21%) and China (23%). Cases with HIV were most commonly reported in the USA (10%) and Spain (14%) and those with COVID-19 (15%) in India and China. The percentage of cases admitted to intensive care and treated with corticosteroids was higher in Spain (64% and 71%, respectively) and lower in South Africa (5% for both). Gastric and intestinal mucosa and abdominal wall injuries, either disease-related or iatrogenic, were potential portals of entry for Mucorales. As for the other clinical forms, ICU admission, abdominal surgery and corticosteroid treatment were common underlying conditions, suggesting that they may be healthcare-associated risk factors for GI and IA mucormycosis [24].
The source of GI and IA mucormycosis remains unclear, but the ingestion or introduction of Mucorales spores with contaminated food, drink, or medical devices is strongly suspected as a route of entry through the digestive tract. On the other hand, in cases with abdominal wall involvement, the main route of entry appears to be through the skin from environmental sources.
As in other studies, the stomach was the most commonly affected GI site, followed by the colon and ileum, with an inverse distribution in children under 16 years of age [21], and then liver, spleen, and IA cavity following.
As neither clinical nor CTS or USG features are specific, the diagnosis of GI mucormycosis remains a challenge with 17% of cases diagnosed post or perimortem, particularly before 2000. Abdominal distension and pain and GI bleeding as haematemesis, haematochezia or melena were the common features for GI forms or swelling, fasciitis, necrosis for IA forms with abdominal wall as the primary site. Ulceration or erosion was the most common but non-specific endoscopic GI feature. However, necrosis, reported in more than 30% of cases and reflecting vascular invasion, should be an alerting feature.
Improving the diagnostic delay is therefore important in GI ulcerations, IA abscesses and abdominal wall fasciitis, even if the patient is immunocompetent, the differential diagnosis should include mucormycosis. Microscopic examination of wet mounts with KOH or fluorescent brighteners such as calcofluor white (Sigma Aldrich, St. Louis, MO, USA) or blankophor (Tanatax Chemicals, Ede, The Netherlands) is one of the cornerstones in the diagnosis of mucormycosis [25] and strongly recommended since it provides rapid at least presumptive diagnosis [26]. However, in this study, it was only performed in 11.76% of the cases. Direct examination needs to be confirmed by histopathology for evidence of tissue invasion of non-sterile sites and by culture and/or molecular or in situ identification techniques when such assays are available [26]. Overall, fungal cultures are positive in 50% to 71% of cases of mucormycosis [17,25]. In this study, culture was only performed in 38% of cases and was positive in 74.04% of cases and similar to that reported by Didehdar et al. (14/19, 73.68%) for 87 cases reported between 2015 and 2021 [27]. This high rate may be due to publication bias.
The identification of the fungal agent was mainly based on phenotypic characteristics. Molecular methods, mainly based on PCR and the sequencing of the ITS1 and ITS2 regions of the rDNA, have been performed in 27 cases since 2003, of which 24 allowed the identification of Mucorales. Gastroenterologists and surgeons should be encouraged to send samples for mycological examination to determine the exact aetiological agent.
Worldwide, more than 90% of mucormycoses are caused by Rhizopus spp., Mucor spp. and Lichtheimia (formerly Absidia) spp. In contrast, Cunninghamella spp., Apophysomyces spp., Saksenaea spp., Rhizomucor spp., Cokeromyces spp., and Syncephalastrum each account for fewer than 5% of cases. However, there are geographical variations, with Mucor spp. and Lichtheimia spp. as secondary causes in the Americas and Europe, and Apophysomyces spp. as secondary causes in India [3]. The genera Rhizopus, Mucor, Apophysomyces, and Lichtheimia were identified with varying frequencies according to the site of infection (Figure 9). The genus Apophysomyces, with a particular emphasis on A. elegans, was the third most isolated genus. This is likely attributable to the inclusion of IA mucormycosis with abdominal wall start, predominantly from India, for which this genus was identified in 9/13 cases. However, it is important to note that the identification of these genera relied predominantly on phenotypic characteristics (70/94, 74.46%), which are currently considered less accurate than molecular identification. Consequently, the interpretation of genera and species epidemiology should be approached with a degree of caution.
The guidelines for the treatment of mucormycosis recommend a combination of surgical debridement and AFT with a high dose of Amp B lipid preparations of as a first-line therapy [26]. However, in settings where resources are limited, Amp B deoxycholate may be the only option. In the present review, 51.41% of the treated patients received the combined therapy with surgery and Amp B lipid preparations (39.80%) or with Amp B deoxycholate (42.78%). High-dose (≥5 mg/kg/d) of Amp B lipid formulations was used in 39.53% of cases. Since 2010, there have been reports of the utilisation of PSZ or ISZ, primarily in the context of maintenance or combination therapy.
In the present review, crude mortality at three months was 52.94%, which is comparable with that of cases with only one GI or IA localisation (40% to 50%) and lower than that of cases with more than one localisation (57%) or with disseminated infection (82%). This is consistent with previous publications, which reported a mortality between 40 and 85%, with lower mortality reported after 2010 [17,21,27,28,29]. The mortality rates of adults (52.89%) and children (53.33%) were comparable. This can be attributed to the exclusion of the neonatal population, in which the mortality rate of GI mucormycosis is significantly higher, ranging from 70% to 85% [27,29]. Abdominal wall mucormycosis has been documented in various case reports and reviews, predominantly concerning cutaneous localisations, with an overall mortality rate of 35% [30]. Abdominal wall mucormycosis has been documented in various case reports and reviews, predominantly concerning cutaneous localisations, with an overall mortality rate of 35%. Thus, specific mortality of abdominal wall mucormycosis with deep subcutaneous involvement (beyond the subcutaneous plane) was not reported. This review found that the mortality rate for cases involving the abdominal wall was higher (59.09%), with 53.33% of cases occurring as the sole site of infection and 71.43% of cases involving other sites.
The mortality rate exhibited a significant variation according to the treatment regimen, with the highest mortality rate (83.78%) observed in patients treated exclusively with surgery, in comparison to all other main regimens and a lower mortality rate found in subjects treated with Amb lipid formulations with or without surgery. The low mortality (25%) observed in patients treated with only Amb lipid formulations is intriguing. It is noteworthy that 12/15 (80%) of cases exhibited solely gastric involvement, and vascular invasion was documented in only 3 of these cases, suggesting a low degree of invasion as a potential contributing factor to the favourable outcomes observed. Furthermore, half of the survivors received prolonged AFT (2 to 6 months) with liposomal Amb or liposomal Amb followed by PSZ. This experience is limited, but it suggests that when surgery is not possible, prolonged AFT may be an option.
The present review is subject to certain limitations. Firstly, it was retrospective in nature and primarily consists of case reports and case series, thus being limited by the absence of prospective and controlled trials. Even if it has been systematic, some cases may have been overlooked. Secondly, publication bias must be noted, since cases considered unusual are more likely to be reported or published. However, the analysed data relied on stringent inclusion criteria.
5. Conclusions
GI and IA mucormycosis are a deadly fungal infection, the diagnosis of which is complicated by its rarity and non-specific clinical presentation. Consequently, these infections are under-suspected. It is therefore vital that suspicion of mucormycosis is raised at the earliest opportunity, and that treatment is commenced promptly, in order to ensure a favourable outcome [26]. In light of this, we propose to suspect GI and IA mucormycosis in patients at risk, as well as those admitted to the ICU with ventilation/nasogastric tube and corticosteroids, exhibiting symptoms such as abdominal distension and pain, and fever, particularly when associated with GI bleeding. The diagnosis of mucormycosis can be expedited through the utilisation of mycological diagnostic methods, encompassing direct examination and culture on invasive samples (endoscopic biopsy, surgical sample), and Mucorales qPCR performed on tissue and blood samples in select circumstances. These approaches facilitate a swift diagnosis of mucormycosis prior to histological examination. The treatment regimen should encompass AFT, predicated on Amp B derivatives, and surgical intervention when feasible.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jof11040298/s1, Figure S1: Distribution (%) of the underling diseased and conditions according to the decade of publication; Figure S2: Distribution (%) of main underlying diseases and conditions according to the country for the five countries with more than 10 reported cases; Table S1: Summary of epidemiological and clinical data reported in the 290 cases of gastrointestinal (GI) and intra-abdominal (IA) mucormycosis that were included in the study; Table S2. Summary of diagnostic, treatment and outcome reported in the 290 cases of gastrointestinal (GI) and intra-abdominal (IA) mucormycosis that were included in the study. Refs [31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227,228,229,230,231,232,233,234,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250,251,252,253,254,255,256,257,258,259,260,261,262,263,264,265,266,267,268,269,270,271,272,273,274,275,276] are cited in the Supplementary Materials.
Author Contributions
All the authors contributed to the writing. A.A. original draft preparation and supervision, B.H., A.L.U. and S.J. review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All analysed data are included in this paper.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Vitale, R.G.; de Hoog, G.S.; Schwarz, P.; Dannaoui, E.; Deng, S.; Machouart, M.; Voigt, K.; Wendy, W.; van de Sande, W.W.; Dolatabadi, S.; et al. Antifungal susceptibility and phylogeny of opportunistic members of the order mucorales. J. Clin. Microbiol. 2012, 50, 66–75. [Google Scholar] [CrossRef]
- Walther, G.; Wagner, L.; Kurzai, O. Updates on the Taxonomy of Mucorales with an Emphasis on Clinically Important Taxa. J. Fungi 2019, 5, 106. [Google Scholar] [CrossRef] [PubMed]
- Alqarihi, A.; Kontoyiannis, D.P.; Ibrahim, A.S. Mucormycosis in 2023: An update on pathogenesis and management. Front. Cell Infect. Microbiol. 2023, 13, 1254919. [Google Scholar] [CrossRef] [PubMed]
- Kontoyiannis, D.P.; Wessel, V.C.; Bodey, G.P.; Rolston, K.V. Zygomycosis in the 1990s in a tertiary-care cancer center. Clin. Infect. Dis. 2000, 30, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Marr, K.A.; Carter, R.A.; Crippa, F.; Wald, A.; Corey, L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin. Infect. Dis. 2002, 34, 909–917. [Google Scholar] [CrossRef]
- Ambrosioni, J.; Bouchuiguir-Wafa, K.; Garbino, J. Emerging invasive zygomycosis in a tertiary care center: Epidemiology and associated risk factors. Int. J. Infect. Dis. 2010, 14 (Suppl. S3), e100–e103. [Google Scholar] [CrossRef]
- Bitar, D.; Lortholary, O.; Le Strat, Y.; Nicolau, J.; Coignard, B.; Tattevin, P.; Che, D.; Dromer, F. Population-based analysis of invasive fungal infections, France, 2001–2010. Emerg. Infect. Dis. 2014, 20, 1149–1155. [Google Scholar] [CrossRef]
- Dolatabadi, S.; Ahmadi, B.; Rezaei-Matehkolaei, A.; Zarrinfar, H.; Skiada, A.; Mirhendi, H.; Nashibi, R.; Niknejad, F.; Nazeri, M.; Rafiei, A.; et al. Mucormycosis in Iran: A six-year retrospective experience. J. Mycol. Med. 2018, 28, 269–273. [Google Scholar] [CrossRef]
- Prakash, H.; Chakrabarti, A. Epidemiology of Mucormycosis in India. Microorganisms 2021, 9, 523. [Google Scholar] [CrossRef]
- Danion, F.; Letscher-Bru, V.; Guitard, J.; Sitbon, K.; Delliere, S.; Angoulvant, A.; Desoubeaux, G.; Botterel, F.; Bellanger, A.P.; Gargala, G.; et al. Coronavirus Disease 2019-Associated Mucormycosis in France: A Rare but Deadly Complication. Open Forum Infect Dis. 2022, 9, ofab566. [Google Scholar] [CrossRef]
- Spellberg, B.; Edwards, J., Jr.; Ibrahim, A. Novel perspectives on mucormycosis: Pathophysiology, presentation, and management. Clin. Microbiol. Rev. 2005, 18, 556–569. [Google Scholar] [PubMed]
- Tribble, D.R.; Warkentien, T.; Rodriguez, C.; Trauma Infectious Diseases Outcomes Study Group of the Infectious Disease Clinical Research Program. Mucormycosis after a tornado in Joplin, Missouri. N. Engl. J. Med. 2013, 368, 1067. [Google Scholar]
- Warkentien, T.E.; Shaikh, F.; Weintrob, A.C.; Rodriguez, C.J.; Murray, C.K.; Lloyd, B.A.; Ganesan, A.; Aggarwal, D.; Carson, M.L.; Tribble, D.R. Impact of Mucorales and Other Invasive Molds on Clinical Outcomes of Polymicrobial Traumatic Wound Infections. J. Clin. Microbiol. 2015, 53, 2262–2270. [Google Scholar]
- Legrand, M.; Gits-Muselli, M.; Boutin, L.; Garcia-Hermoso, D.; Maurel, V.; Soussi, S.; Benyamina, M.; Ferry, A.; Chaussard, M.; Hamane, S.; et al. Detection of Circulating Mucorales DNA in Critically Ill Burn Patients: Preliminary Report of a Screening Strategy for Early Diagnosis and Treatment. Clin. Infect. Dis. 2016, 63, 1312–1317. [Google Scholar]
- Dang, J.; Goel, P.; Choi, K.J.; Massenzio, E.; Landau, M.J.; Pham, C.H.; Huang, S.; Yenikomshian, H.A.; Spellberg, B.; Gillenwater, T.J. Mucormycosis following burn injuries: A systematic review. Burns 2023, 49, 15–25. [Google Scholar]
- Drogari-Apiranthitou, M.; Skiada, A.; Panayiotides, I.; Vyzantiadis, T.A.; Poulopoulou, A.; Christofidou, M.; Antoniadou, A.; Roilides, E.; Iosifidis, E.; Mamali, V.; et al. Epidemiology of Mucormycosis in Greece; Results from a Nationwide Prospective Survey and Published Case Reports. J. Fungi 2023, 9, 425. [Google Scholar] [CrossRef]
- Roden, M.M.; Zaoutis, T.E.; Buchanan, W.L.; Knudsen, T.A.; Sarkisova, T.A.; Schaufele, R.L.; Sein, M.; Sein, T.; Chiou, C.C.; Chu, J.H. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin. Infect. Dis. 2005, 41, 634–653. [Google Scholar]
- Petrikkos, G.; Skiada, A.; Lortholary, O.; Roilides, E.; Walsh, T.J.; Kontoyiannis, D.P. Epidemiology and clinical manifestations of mucormycosis. Clin. Infect. Dis. 2012, 54 (Suppl. S1), S23–S34. [Google Scholar]
- Serris, A.; Danion, F.; Lanternier, F. Disease Entities in Mucormycosis. J. Fungi 2019, 5, 23. [Google Scholar] [CrossRef]
- Dioverti, M.V.; Cawcutt, K.A.; Abidi, M.; Sohail, M.R.; Walker, R.C.; Osmon, D.R. Gastrointestinal mucormycosis in immunocompromised hosts. Mycoses 2015, 58, 714–718. [Google Scholar]
- Kaur, H.; Ghosh, A.; Rudramurthy, S.M.; Chakrabarti, A. Gastrointestinal mucormycosis in apparently immunocompetent hosts-A review. Mycoses 2018, 61, 898–908. [Google Scholar] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar]
- Donnelly, J.P.; Chen, S.C.; Kauffman, C.A.; Steinbach, W.J.; Baddley, J.W.; Verweij, P.E.; Clancy, C.J.; Wingard, J.R.; Lockhart, S.R.; Groll, A.H.; et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin. Infect. Dis. 2020, 71, 1367–1376. [Google Scholar]
- Rammaert, B.; Lanternier, F.; Zahar, J.R.; Dannaoui, E.; Bougnoux, M.E.; Lecuit, M.; Lortholary, O. Healthcare-associated mucormycosis. Clin. Infect. Dis. 2012, 54 (Suppl. S1), S44–S54. [Google Scholar]
- Skiada, A.; Lass-Floerl, C.; Klimko, N.; Ibrahim, A.; Roilides, E.; Petrikkos, G. Challenges in the diagnosis and treatment of mucormycosis. Med. Mycol. 2018, 56 (Suppl. S1), 93–101. [Google Scholar]
- Cornely, O.A.; Alastruey-Izquierdo, A.; Arenz, D.; Chen, S.C.A.; Dannaoui, E.; Hochhegger, B.; Hoenigl, M.; Jensen, H.E.; Lagrou, K.; Lewis, R.E.; et al. Global guideline for the diagnosis and management of mucormycosis: An initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect. Dis. 2019, 19, e405–e421. [Google Scholar]
- Didehdar, M.; Chegini, Z.; Moradabadi, A.; Anoushirvani, A.A.; Tabaeian, S.P.; Yousefimashouf, M.; Shariati, A. Gastrointestinal mucormycosis: A periodic systematic review of case reports from 2015 to 2021. Microb. Pathog. 2022, 163, 105388. [Google Scholar]
- Song, Y.; Qiao, J.; Giovanni, G.; Liu, G.; Yang, H.; Wu, J.; Chen, J. Mucormycosis in renal transplant recipients: Review of 174 reported cases. BMC Infect. Dis. 2017, 17, 283. [Google Scholar]
- Mustafa, A.; Mahmood, Y.; Hasan, A.; Asaad, H.; Gharib, D.; Hama Hussein, K.; Hasan, K.M.; Ismaeil, D.A.; Hiwa, D.S.; Ali, R.M.; et al. Gastric Mucormycosis: A Systematic Review with Metadata. Barw. Med. J. 2024, 2, 65–84. [Google Scholar]
- Sutherland, J.C.; Jones, T.H. Gastric mucormycosis: Report of case in a Swazi. S. Afr. Med. J. 1960, 34, 161. [Google Scholar]
- Kahn, L.B. Gastric Mucormycosis: Report of a Case with a Review of the Literature. S. Afr. Med. J. 1963, 37, 1265–1269. [Google Scholar] [PubMed]
- Abramowitz, I. Fatal Perforations of the Stomach Due to Mucormycosis of the Gastro-Intestinal Tract. S. Afr. Med. J. 1964, 38, 93–94. [Google Scholar] [PubMed]
- Dannheimer, I.P.; Fouche, W.; Nel, C. Gastric mucormycosis in a diabetic patient. S. Afr. Med. J. 1974, 48, 838–839. [Google Scholar] [PubMed]
- Lawson, H.H.; Schmaman, A. Gastric phycomycosis. Br. J. Surg. 1974, 61, 743–746. [Google Scholar]
- Schulman, A.; Bornman, P.; Kaplan, C.; Morton, P.; Rose, A. Gastrointestinal mucormycosis. Gastrointest. Radiol. 1979, 4, 385–388. [Google Scholar]
- Brullet, E.; Andreu, X.; Elias, J.; Roig, J.; Cervantes, M. Gastric mucormycosis in a patient with acquired immunodeficiency syndrome. Gastrointest. Endosc. 1993, 39, 106–107. [Google Scholar]
- Winkler, S.; Susani, S.; Willinger, B.; Apsner, R.; Rosenkranz, A.R.; Potzi, R.; Berlakovich, G.A.; Pohanka, E. Gastric mucormycosis due to Rhizopus oryzae in a renal transplant recipient. J. Clin. Microbiol. 1996, 34, 2585–2587. [Google Scholar]
- Uchida, T.; Okamoto, M.; Fujikawa, K.; Yoshikawa, D.; Mizokami, A.; Mihara, T.; Kondo, A.; Ohba, K.; Kurohama, K.; Nakashima, M.; et al. Gastric mucormycosis complicated by a gastropleural fistula: A case report and review of the literature. Medicine 2019, 98, e18142. [Google Scholar]
- Corley, D.A.; Lindeman, N.; Ostroff, J.W. Survival with early diagnosis of invasive gastric mucormycosis in a heart transplant patient. Gastrointest. Endosc. 1997, 46, 452–454. [Google Scholar]
- Knoop, C.; Antoine, M.; Vachiery, J.L.; Depre, G.; Alonso-Vega, C.; Struelens, M.; Van Laethem, J.L.; Lingier, P.; Nagy, N.; Jacobs, F.; et al. Gastric perforation due to mucormycosis after heart-lung and heart transplantation. Transplantation 1998, 66, 932–935. [Google Scholar]
- Sharma, M.C.; Gill, S.S.; Kashyap, S.; Kataria, R.; Gupta, D.K.; Sahni, P.; Acharya, S.K. Gastrointestinal mucormycosis--an uncommon isolated mucormycosis. Indian J. Gastroenterol. 1998, 17, 131–133. [Google Scholar] [PubMed]
- Sheu, B.S.; Lee, P.C.; Yang, H.B. A giant gastric ulcer caused by mucormycosis infection in a patient with renal transplantation. Endoscopy 1998, 30, S60–S61. [Google Scholar] [PubMed]
- Barroso, F.; Forcelledo, J.L.; Mayorga, M.; Pena, F.; Marques, F.F.; de la Pena, J. A fatal case of gastric mucormyosis in a heart transplant recipient. Endoscopy 1999, 31, S2. [Google Scholar]
- Cherney, C.L.; Chutuape, A.; Fikrig, M.K. Fatal invasive gastric mucormycosis occurring with emphysematous gastritis: Case report and literature review. Am. J. Gastroenterol. 1999, 94, 252–256. [Google Scholar]
- Al-Rikabi, A.C.; Al-Dohayan, A.D.; Al-Boukai, A.A. Invasive mucormycosis in benign gastric ulcer. Saudi Med. J. 2000, 21, 287–290. [Google Scholar]
- Pickeral, J.J., 3rd; Silverman, J.F.; Sturgis, C.D. Gastric zygomycosis diagnosed by brushing cytology. Diagn. Cytopathol. 2000, 23, 51–54. [Google Scholar]
- Geramizadeh Bita, A.S. Invasive gastric mucormycosis: Report of a case and review of the litterature. Med. J. Islam. Republic Iran 2001, 14, 397–398. [Google Scholar]
- Tinmouth, J.; Baker, J.; Gardiner, G. Gastrointestinal mucormycosis in a renal transplant patient. Can. J. Gastroenterol. 2001, 15, 269–271. [Google Scholar]
- Paulo De Oliveira, J.E.; Milech, A. A fatal case of gastric mucormycosis and diabetic ketoacidosis. Endocr. Pract. 2002, 8, 44–46. [Google Scholar]
- Park, Y.S.; Lee, J.D.; Kim, T.H.; Joo, Y.H.; Lee, J.H.; Lee, T.S.; Kim, E.K. Gastric mucormycosis. Gastrointest. Endosc. 2002, 56, 904–905. [Google Scholar]
- Shahapure, A.G.; Patankar, R.V.; Bhatkhande, R. Gastric mucormycosis. Indian J. Gastroenterol. 2002, 21, 231–232. [Google Scholar] [PubMed]
- Vera, A.; Hubscher, S.G.; McMaster, P.; Buckels, J.A. Invasive gastrointestinal zygomycosis in a liver transplant recipient: Case report. Transplantation 2002, 73, 145–147. [Google Scholar] [PubMed]
- Maravi-Poma, E.; Rodriguez-Tudela, J.L.; de Jalon, J.G.; Manrique-Larralde, A.; Torroba, L.; Urtasun, J.; Salvador, B.; Montes, M.; Mellado, E.; Rodríguez-Albarrán, F.; et al. Outbreak of gastric mucormycosis associated with the use of wooden tongue depressors in critically ill patients. Intensive Care Med. 2004, 30, 724–728. [Google Scholar] [PubMed]
- Stamm, B. Mucormycosis of the stomach in a patient with multiple trauma. Histopathology 2005, 47, 222–223. [Google Scholar]
- Prasad, N.; Ram, R.; Satti Reddy, V.; Dakshinamurty, K.V. Non-fatal gastric mucormycosis in a renal transplant patient and review of the literature. Transpl. Infect. Dis. 2006, 8, 237–241. [Google Scholar]
- Devlin, S.M.; Hu, B.; Ippoliti, A. Mucormycosis presenting as recurrent gastric perforation in a patient with Crohn’s disease on glucocorticoid, 6-mercaptopurine, and infliximab therapy. Dig. Dis. Sci. 2007, 52, 2078–2081. [Google Scholar]
- Ho, Y.H.; Wu, B.G.; Chen, Y.Z.; Wang, L.S. Gastric Mucormycosis in an Alcoholic with Review of the Literature. Tzu Chi Med. J. 2007, 19, 169–172. [Google Scholar]
- Vaiphei, K.; Suri, V.; Bhalla, A. Fever, jaundice, altered sensorium, with multiple systemic manifestations. Indian J. Gastroenterol. 2007, 26, 82–86. [Google Scholar]
- Chung, C.S.; Wang, W.L.; Liu, K.L.; Lin, J.T.; Wang, H.P. Green ulcer in the stomach: Unusual mucormycosis infection. Gastrointest. Endosc. 2008, 68, 566–567. [Google Scholar]
- Shiva Prasad, B.N.; Shenoy, A.; Nataraj, K.S. Primary gastrointestinal mucormycosis in an immunocompetent person. J. Postgrad. Med. 2008, 54, 211–213. [Google Scholar]
- Azhar, A.; Calubiran, O.V.; Kilaru, R.M.; Lincoln, J.A.; Moshenyat, I.; Basti, K.; Visconti, E. Patient With Abdominal Pain-Concealing Gastrointestinal Mucormycosis. Gastroenterol. Hepatol. 2009, 5, 657–661. [Google Scholar]
- Nandu, V.; Nagral, A.; Khubchandani, S.; Agrawal, C. A rare cause of upper GI bleeding. Gut 2009, 58, 1039. [Google Scholar] [CrossRef] [PubMed]
- Small, M.; Gill, J.; Reed, J.; Poetter, D.; Goldsmith, S. Isolated gastric mucormycosis—A rare cause of a large gastric ulceration in an immunocompetent host. Am. J. Gastroenterol. 2010, 105, S172. [Google Scholar] [CrossRef]
- Feng, W.; Tseng, C.; Lin, C.; Tseng, K. Nonfatal gastric mucormycosis associated with emphysematous gastritis. Tzu Chi Med. J. 2010, 22, 146–148. [Google Scholar] [CrossRef]
- Johnson, C.B.; Ahmeti, M.; Tyroch, A.H.; Zuckerman, M.J.; Hakim, M.N. Gastric mucormycosis as a cause of life-threatening upper gastrointestinal bleeding in a trauma patient. Am. Surg. 2010, 76, E76–E77. [Google Scholar] [CrossRef]
- Paydar, S.; Baezzat, S.; Fazelzadeh, A.; Geramizadeh, B. A case of gastric zygomycosis in a diabetic patient successfully treated with total gastrectomy. Middle East. J. Dig. Dis. 2010, 2, 46–48. [Google Scholar]
- Pruthvi, B.C.R.C.; Rupashree, S.; Deepak, S.; Vikram, S.; Jayaprakash, B.R.N.; Rao, L. Gastric mucormycosis masquerading asmalignancy in an immunocompetent host. Arab. J. Gastroenterol. 2010, 11, 227–229. [Google Scholar] [CrossRef]
- Shenoi, S.; Emery, H.M. Successful treatment of invasive gastric mucormycosis in a child with systemic lupus erythematosus. Lupus 2010, 19, 646–649. [Google Scholar] [CrossRef]
- Woo, P.C.; Lau, S.K.; Ngan, A.H.; Tung, E.T.; Leung, S.Y.; To, K.K.; Cheng, V.C.; Yuen, K.Y. Lichtheimia hongkongensis sp. nov., a novel Lichtheimia spp. associated with rhinocerebral, gastrointestinal, and cutaneous mucormycosis. Diagn. Microbiol. Infect. Dis. 2010, 66, 274–284. [Google Scholar] [CrossRef]
- Chhaya, V.; Gupta, S.; Arnaout, A. Mucormycosis causing giant gastric ulcers. Endoscopy 2011, 43 (Suppl. S2), E289–E290. [Google Scholar] [CrossRef]
- Chang, C.F.; Huang, T.Y.; Lin, T.Y. Unusual giant gastric cardia ulcer. Intern. Emerg. Med. 2018, 13, 795–796. [Google Scholar] [CrossRef] [PubMed]
- Dutta, A.; Roy, M.; Singh, T.; Singh, T. Gastric mucormycosis in an immunocompetent patient. J. Med. Soc. 2012, 26, 192–194. [Google Scholar]
- Naqvi, H.A.; Nadeem Yousaf, M.; Chaudhary, F.S.; Mills, L. Gastric Mucormycosis: An Infection of Fungal Invasion into the Gastric Mucosa in Immunocompromised Patients. Case Rep. Gastrointest. Med. 2020, 2020, 8876125. [Google Scholar]
- Muthuswamy, M. Giant necrotic ulcer: Invasive gastric mucormycosis. Am. J. Gastroenterol. 2012, 107, S300. [Google Scholar] [CrossRef]
- Ryan, O.; Frohlich, S.; Crotty, T.B.; Ryan, D. Rhizopus microsporus infection in an immunocompetent host: A case of immunoparalysis? Anaesth. Intensive Care. 2012, 40, 367–368. [Google Scholar]
- Corey, K.E.; Gupta, N.K.; Agarwal, S.; Xiao, H.D. Case records of the Massachusetts General Hospital. Case 32-2013. A 55-year-old woman with autoimmune hepatitis, cirrhosis, anorexia, and abdominal pain. N. Engl. J. Med. 2013, 369, 1545–1553. [Google Scholar] [CrossRef]
- Irtan, S.; Lamerain, M.; Lesage, F.; Verkarre, V.; Bougnoux, M.E.; Lanternier, F.; Zahar, J.R.; Salvi, N.; Talbotec, C.; Lortholary, O.; et al. Mucormycosis as a rare cause of severe gastrointestinal bleeding after multivisceral transplantation. Transpl. Infect. Dis. 2013, 15, E235–E238. [Google Scholar] [CrossRef]
- Katta, J.G.S.; Narach, T.; Poetter, D.; Kulkarni, P.; Reed, J.; Goldsmith, S.F. Gastric mucormycosis managed with combination antifungal therapy and no surgical debridement. Infect. Dis. Clin. Pract. 2013, 21, 265–268. [Google Scholar] [CrossRef]
- Machicado, J.Y.M.; Wolf, D. Gastric mucormycosis presenting as gastrotrointestinal bleeding in a trauma patient. Am. J. Gastroenterol. 2013, 108, S228–S229. [Google Scholar] [CrossRef]
- Bini, R.; Addeo, A.; Maganuco, L.; Fontana, D.; Viora, T.; Leli, R. The role of surgery in a case of diffuse mucormycosis with haematemesis and gastric necrosis. Ann. R. Coll. Surg. Engl. 2014, 96, e31–e33. [Google Scholar] [CrossRef]
- Kaiser, P.; Maggio, E.M.; Pfammatter, T.; Misselwitz, B.; Flury, S.; Schneider, P.M.; Dutkowski, P.; Breitenstein, S.; Müllhaupt, B.; Clavien, P.A.; et al. Histopathological evidence of invasive gastric mucormycosis after transarterial chemoembolization and liver transplantation. Infection 2014, 42, 779–783. [Google Scholar] [PubMed]
- Lee, S.H.; Son, Y.G.; Sohn, S.S.; Ryu, S.W. Successful treatment of invasive gastric mucormycosis in a patient with alcoholic liver cirrhosis: A case report. Exp. Ther. Med. 2014, 8, 401–404. [Google Scholar] [PubMed]
- Kulkarni, R.V.; Thakur, S.S. Invasive Gastric Mucormycosis—A Case Report. Indian J. Surg. 2015, 77 (Suppl. S1), 87–89. [Google Scholar] [PubMed]
- Nandwani, A.; Jha, P.K.; Duggal, R.; Kher, V. Invasive gastric mucormycosis and cytomegalovirus infection in an ABO incompatible renal transplant recipient. Indian J. Nephrol. 2015, 25, 373–376. [Google Scholar]
- Nasta, A.M.B.K.; Ranjan, S. An unusual case of gastric gangrene, diaphragmatic gangrene and autosplenectomy due to mucormycosis in a diabetic patient. Int. J. Case Rep. Images 2015, 5, 95–98. [Google Scholar]
- Raviraj, K.S.; Miglani, P.; Garg, A.; Agarwal, P.K. Gastric Mucormycosis with Hemolytic Uremic Syndrome. J. Assoc. Physicians India 2015, 63, 75–76. [Google Scholar]
- Lin, P.Y.; Tang, J.H.; Chang, C.C. A rare cause of GI bleeding in a 56-year-old man. Gut 2017, 66, 1074. [Google Scholar]
- Mittal, T.; Pulle, M.V.; Dey, A.; Malik, V.K. Gastric Mucormycosis Presenting as Gastrocolic Fistula: A Rare Entity. Indian J. Surg. 2016, 78, 511–512. [Google Scholar]
- Ravi, D.; Naqvi, A.; Odashiro, A.; Alowami, S. Gastrointestinal mucormycosis in a patient with COPD and diabetes mellitus. Can. J. Pathol. 2016, 8, 13. [Google Scholar]
- Tathe, S.P.; Dani, A.A.; Chawhan, S.M.; Meshram, S.A.; Randale, A.A.; Raut, W.K. Gastric mucormycosis: Diagnosis by imprint cytology. Diagn. Cytopathol. 2016, 44, 820–822. [Google Scholar]
- Chow, K.L.; McElmeel, D.P.; Brown, H.G.; Tabriz, M.S.; Omi, E.C. Invasive gastric mucormycosis: A case report of a deadly complication in an immunocompromised patient after penetrating trauma. Int. J. Surg. Case Rep. 2017, 40, 90–93. [Google Scholar] [PubMed]
- Chugh, P.; Sasken, H.; Azeez, S.; Kassab, M. Gastric Mucormycosis as a Cause of Upper Gastrointestinal Bleeding in an Immunocompetent Patient. Am. J. Gastroenterol. 2017, 112, S1059–S1060. [Google Scholar]
- Galvan Fernandez, J.; Jimenez Cuenca, M.I.; Molpeceres Martinez, I.; Alvarez-Quinones, M.L. A rare cause of emphysematous infectious gastritis. Rev. Esp. Enferm. Dig. 2017, 109, 368. [Google Scholar]
- Grimaldi, D.; Pradier, O.; Hotchkiss, R.S.; Vincent, J.L. Nivolumab plus interferon-gamma in the treatment of intractable mucormycosis. Lancet Infect. Dis. 2017, 17, 18. [Google Scholar]
- Metussin, D.; Telisinghe, P.U.; Chong, P.L.; Chong, V.H. Gastrointestinal: Gastric mucormycosis. J. Gastroenterol. Hepatol. 2017, 32, 1537. [Google Scholar]
- Nasa, M.; Sharma, Z.; Lipi, L.; Sud, R. Gastric Angioinvasive Mucormycosis in Immunocompetent Adult, A Rare Occurrence. J. Assoc. Physicians India 2017, 65, 103–104. [Google Scholar]
- Sanchez Velazquez, P.; Pera, M.; Gimeno, J.; Zapatero, A.; Nolla, J.; Pera, M. Mucormycosis: An unusual cause of gastric perforation and severe bleeding in immunocompetent patients. Rev. Esp. Enferm. Dig. 2017, 109, 223–225. [Google Scholar]
- Suhaildeen, K.; Majhi, U.; Seshadri, R.A.; Murhekar, K. Gastric Mucormycosis Masquerading as Gastric Malignancy. Indian J. Surg. Oncol. 2017, 8, 407–410. [Google Scholar]
- Abreu, B.; Duarte, M.L.; Santos, L.R.D.; Sementilli, A.; Figueiras, F.N. A rare case of gastric mucormycosis in an immunocompetent patient. Rev. Soc. Bras. Med. Trop. 2018, 51, 401–402. [Google Scholar]
- Alfano, G.; Fontana, F.; Francesca, D.; Assirati, G.; Magistri, P.; Tarantino, G.; Ballarin, R.; Rossi, G.; Franceschini, E.; Codeluppi, M.; et al. Gastric Mucormycosis in a Liver and Kidney Transplant Recipient: Case Report and Concise Review of Literature. Transplant. Proc. 2018, 50, 905–909. [Google Scholar]
- Kim, H.N.; Han, S.A.; Park, H.Y.; Kim, H.W.; Hong, R.; Choi, N.G.; Shin, M.H.; Yoon, N.R.; Kim, H.L.; Chung, J.H.; et al. Successful treatment of invasive gastric mucormycosis in a kidney transplant recipient. J. Korean Soc. Transplant. 2018, 32, 104–107. [Google Scholar] [CrossRef]
- Termos, S.; Othman, F.; Alali, M.; Al Bader, B.M.S.; Alkhadher, T.; Hassanaiah, W.F.; Taqi, A.; Sapkal, A. Total Gastric Necrosis Due to Mucormycosis: A Rare Case of Gastric Perforation. Am. J. Case Rep. 2018, 19, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, S.; Gautam, A.R.; Paudyal, B.; Sigdel, K.R.; Basnyat, B. Case Report: Gastric Mucormycosis—A rare but important differential diagnosis of upper gastrointestinal bleeding in an area of Helicobacter pylori endemicity. Wellcome Open Res. 2019, 4, 5. [Google Scholar] [CrossRef]
- Gani, I.; Doroodchi, A.; Falkenstrom, K.; Berry, H.; Lee, W.; Mulloy, L.; Saeed, M.; Kapoor, R. Gastric Mucormycosis in a Renal Transplant Patient Treated with Isavuconazole Monotherapy. Case Rep. Transplant. 2019, 2019, 9839780. [Google Scholar] [CrossRef]
- Guzman Rojas, P.; Robalino Gonzaga, E.; Catania, J.; Moqete, M. An unexpected cause of gastric ulcer. Am. J. Gastroenterol. 2019, 114, S1506–S1507. [Google Scholar] [CrossRef]
- Lankarani, D.; Maka, R.R.; Aziz, H.; Maklad, M.; Jayaraj, M.; Ohning, G. Medical management of gastric mucormycosis in an immunocompetent patient. 2746. Am. J. Gastroenterol. 2019, 114, S1517–S1518. [Google Scholar] [CrossRef]
- Malek, A.; De la Hoz, A.; Arduino, R.; Aisenberg, G.M. Disseminated tuberculosis and gastric mucormycosis coinfection. IDCases 2019, 18, e00595. [Google Scholar] [CrossRef]
- Peng, H.; Xiao, J.; Wan, H.; Shi, J.; Li, J. Severe Gastric Mycormycosis Infection Followed by Cytomegalovirus Pneumonia in a Renal Transplant Recipient: A Case Report and Concise Review of the Literature. Transplant. Proc. 2019, 51, 556–560. [Google Scholar] [CrossRef]
- Sharaan, A.; Alziadat, M.R.; Syed, Z.; Samuel, A.; Yelisetti, R.; Mathew, J.; Ismail, M. Often a deadly fungus; mucor must be among us: A case of angioinvasive gastric mucormycosis with a positive outcome. Am. J. Respir. Crit. Care Med. 2019, 199, A6582. [Google Scholar]
- Monte Junior, E.S.D.; Santos, M.; Ribeiro, I.B.; Luz, G.O.; Baba, E.R.; Hirsch, B.S.; Funari, M.P.; de Moura, E.G.H. Rare and Fatal Gastrointestinal Mucormycosis (Zygomycosis) in a COVID-19 Patient: A Case Report. Clin. Endosc. 2020, 53, 746–749. [Google Scholar] [CrossRef]
- Hameed, T.; Jain, S.K.; Ansari, F.M.; Nizam, A.; Dua, A. Spontaneous Gastric Necrosis: A Rare Presentation of Invasive Mucormycosis in an Immunocompetent Adult. Case Rep. Infect. Dis. 2020, 2020, 7514051. [Google Scholar]
- Jaju, M.; Sagar, R.; Srivastav, S.; Singh, R.; Kumar, V.; Faisal, M. Different types of mucormycosis: Case series. Int. J. Res. Med. Sci. 2000, 8, 2284–2296. [Google Scholar]
- Jung, H.; Kim, G.J.; Oh, T.H. Successful Management of a Rare Gastric Mucormycosis Presenting with Massive Melena in a Polytrauma Patient. Int. Med. Case Rep. J. 2020, 13, 531–535. [Google Scholar]
- Rivas, C.; Gonzalez, M.; Rapoport, G.; Chacon, I. Mucormycosis in an Immunocompromised Patient. Am. J. Gastroenterol. 2020, 115, S1581. [Google Scholar]
- Sharma, D. Successful management of emphysematous gastritis with invasive gastric mucormycosis. BMJ Case Rep. 2020, 13, e231297. [Google Scholar]
- Ghuman, S.S.; Sindhu, P.; Buxi, T.B.S.; Sheth, S.; Yadav, A.; Rawat, K.S.; Sud, S. CT appearance of gastrointestinal tract mucormycosis. Abdom. Radiol. 2021, 46, 1837–1845. [Google Scholar]
- Huang, H.; Xie, L.; Zheng, Z.; Yu, H.; Tu, L.; Cui, C.; Yu, J. Mucormycosis-induced upper gastrointestinal ulcer perforation in immunocompetent patients: A report of two cases. BMC Gastroenterol. 2021, 21, 311. [Google Scholar]
- Rai, A.; Gajula, B.; Kumar, N.; Malik, A. Gastric Perforation Secondary to Fungal Gastritis in an Immuno-Competent Adult. Cureus 2021, 13, e13156. [Google Scholar]
- Yuvaraj, M.; Mathapati, P.M.; Seena, C.R.; Ramaswami, S. Gastric mucormycosis with splenic invasion a rare abdominal complication of COVID-19 pneumonia. J. Clin. Imaging Sci. 2021, 11, 62. [Google Scholar]
- Bhaskar, B.K.; Gutte, S.H.; Gurjar, M.; Saran, S.; Rahul, R.; Sengar, P. A Rare Case Report of Intra-abdominal Mucormycosis Complicating Acute Pancreatitis. Indian J. Crit. Care Med. 2022, 26, 736–738. [Google Scholar]
- Chauhan, N.K.; Agarwal, A.; Dutt, N.; Yadav, T.; Kochar, R. Pulmonary embolism and gastric bleed with disseminated mucormycosis—Treading dangerous waters. Monaldi Arch. Chest Dis. 2022, 93, 2418. [Google Scholar] [CrossRef] [PubMed]
- Ozbek, L.; Topcu, U.; Manay, M.; Esen, B.H.; Bektas, S.N.; Aydin, S.; Özdemir, B.; Khostelidi, S.N.; Klimko, N.; Cornely, O.; et al. COVID-19-associated mucormycosis: A systematic review and meta-analysis of 958 cases. Clin. Microbiol. Infect. 2023, 29, 722–731. [Google Scholar] [CrossRef] [PubMed]
- Khsiba, A.; Moalla, M.; Nechi, S.; Bani, A.; Elloumi, A.; Jemal, S.; Azouz, M.M.; Medhioub, M.; Hamzaoui, L. Fatal invasive gastric mucormycosis: Two case reports. Clin. Case Rep. 2022, 10, e6330. [Google Scholar] [CrossRef] [PubMed]
- Sachan, A.; Choudhury, A.; Sasani, A.; Mandavdhare, H. Two tales of gastric mucormycosis S3683. Am. J. Gastroenterol. 2022, 117, S2310. [Google Scholar] [CrossRef]
- Safwan, M.; Khan, S.; Belthazar, A.; Sasidharan, M. Primary invasive gastric mucormycosis presenting as Meleney’s gangrene: A case report and review of literature. Libyan J. Med. Sci. 2021, 5, 171–173. [Google Scholar] [CrossRef]
- Albtoosh, A.S.; Shaf’ei, M.; Al Hayek, S.; Ramdan, L.I.; Abu Shahin, N.; Alzyoud, M.; Farah, R. A successfully treated gastric mucormycosis in an immunocompetent patient: Case report and literature review. Clin. Case Rep. 2023, 11, e7540. [Google Scholar] [CrossRef]
- Arora, S.; Singh, A.; Prasad, P.; Rahul Singh, R. Case Reports on Black Fungus of the Gastrointestinal Tract: A New Complication in COVID-19 Patients. Korean J. Gastroenterol. 2023, 81, 221–225. [Google Scholar] [CrossRef]
- Bhowmik, S.; Jadav, D.; Aggarwal, D.; Shekhawat, R.S. Gastric mucormycosis. Autops. Case Rep. 2023, 13, e2023421. [Google Scholar] [CrossRef]
- Khanna, D.; Sahu, P. Primary gastric mucormycosis after COVID. Gastrointest. Endosc. 2023, 97, 1159–1160. [Google Scholar] [CrossRef]
- Kim, J.; Wee, D.; Behin, D.; Brandt, L. Gastric mucormycosis in an immunosuppressed patient following dual pancreas-kidney ransplant. Am. J. Gastroenterol. 2023, 118, S2624. [Google Scholar] [CrossRef]
- Malakar, S.; Elhence, A.; Prasad, P.; Ghoshal, U.C.; Pandey, G.; Mohindra, S. Primary gastric mucormycosis presenting with post-Coronavirus disease-19 upper gastrointestinal bleed. Indian J. Gastroenterol. 2023, 42, 736–737. [Google Scholar] [CrossRef] [PubMed]
- Marco, D.N.; Gonzalez-Munoz, B.; Doti, P.I. Gastric mucormycosis presenting as fever of unknown origin in an immunocompetent host after heatstroke. Pol. Arch. Intern. Med. 2023, 133, 16513. [Google Scholar] [CrossRef] [PubMed]
- Chaudhari, V.; Amarapurkar, A.D.; Rane, P. Mucormycosis Masquerading as Gastric Tumor. ACG Case Rep. J. 2024, 11, e01401. [Google Scholar] [CrossRef] [PubMed]
- de Lucena, L.A.; de Oliveira, F.G.; de Andrade, M.M.P.; de Paula, K.C.; Praxedes, M.R.G.; de Oliveira, R.A. Mucormycosis-induced hypercalcemia: A case report. CEN Case Rep. 2024, 13, 66–71. [Google Scholar] [CrossRef]
- He, D.; Wang, Z. Multiple Gastric Ulcers in An Immunosuppressed Patient with COVID-19 Infection caused by Mucormycosis. J. Gastrointestin. Liver Dis. 2024, 33, 16. [Google Scholar] [CrossRef]
- Huang, W.; Li, L.; Gao, J.; Kang, L. Gastric mucormycosis presenting as diffuse thickening of the gastric wall with enhancement. Rev. Esp. Enferm. Dig. 2024, 116, 167–168. [Google Scholar] [CrossRef]
- Ji, R. Mucormycosis mimicking portal hypertensive haemorrhage as a complication of alcoholic liver cirrhosis: A case report. BMC Infect. Dis. 2024, 24, 136. [Google Scholar]
- Lalwani, S.; Govindasamy, M.; Gupta, M.; Siraj, F.; Varma, V.; Mehta, N.; Kumaran, V.; Mohan, N.; Chopra, P.; Arora, A.; et al. Gastrointestinal mucormycosis—Four cases with different risk factors, involving different anatomical sites. Indian J. Gastroenterol. 2012, 31, 139–143. [Google Scholar] [CrossRef]
- Perez Fernandez, A.; Rubio Mateos, J.M.; Sanchez Fernandez, M.J. Gastric ulcer due to mucormycosis in a critical patient. Rev. Esp. Enferm. Dig. 2020, 112, 576–577. [Google Scholar] [CrossRef]
- Raju, B.; Santhanakumar, K.S.; Kesavachandran, U. Gastrointestinal involvement of unusual Mucormycete Syncephalastrum racemosum in a diabetic patient with adenocarcinoma: Rare case presentation with review of literature. Infection 2020, 48, 791–797. [Google Scholar] [CrossRef]
- Taams, M.; Bade, P.G.; Thomson, S.R. Post-traumatic abdominal mucormycosis. Injury 1992, 23, 390–392. [Google Scholar] [PubMed]
- Saltmarsh, G.; Plurad, D.; Bricker, S.; Bongard, F.; Neville, A.; Putnam, B.; Kim, D. Gastric necrosis and recurrent small bowel perforation resulting from gastrointestinal mucormycosis. Am. Surg. 2014, 80, E293–E294. [Google Scholar] [PubMed]
- Ju, J.H.; Park, H.S.; Shin, M.J.; Yang, C.W.; Kim, Y.S.; Choi, Y.J.; Song, H.J.; Kim, S.W.; Chung, I.S.; Bang, B.K. Successful treatment of massive lower gastrointestinal bleeding caused by mixed infection of cytomegalovirus and mucormycosis in a renal transplant recipient. Am. J. Nephrol. 2001, 21, 232–236. [Google Scholar] [PubMed]
- Kaneko, Y.; Oinuma, K.I.; Terachi, T.; Arimura, Y.; Niki, M.; Yamada, K.; Kakeya, H.; Mizutani, T. Successful Treatment of Intestinal Mycosis Caused by a Simultaneous Infection with Lichtheimia ramosa and Aspergillus calidoustus. Intern. Med. 2018, 57, 2421–2424. [Google Scholar]
- Nidhi, M.; Sadia, K.; Khatri, A.; Arnab, G.; Khan, N.A. Gastrointestinal Mucormycosis in a two-year-old child: A clinical and radiological enigma. Med. Mycol. Case Rep. 2019, 26, 5–9. [Google Scholar]
- Hyvernat, H.; Dunais, B.; Burel-Vandenbos, F.; Guidicelli, S.; Bernardin, G.; Gari-Toussaint, M. Fatal peritonitis caused by Rhizopus microsporus. Med. Mycol. 2010, 48, 1096–1098. [Google Scholar]
- Wotiye, A.B.; Ks, P.; Ayele, B.A. Invasive intestinal mucormycosis in a 40-year old immunocompetent patient—A rarely reported clinical phenomenon: A case report. BMC Gastroenterol. 2020, 20, 61. [Google Scholar]
- Liu, Q.; Chen, P.; Xin, L.; Zhang, J.; Jiang, M. A rare intestinal mucormycosis caused by Lichtheimia ramosa in a patient with diabetes: A case report. Front. Med. 2024, 11, 1435239. [Google Scholar]
- Mungazi, S.G.; Zambuko, B.; Muchuweti, D.; Muguti, E.G.; Mlotshwa, S. Fatal haemorrhagic duodenal mucormycosis in a non-immunocompromised host: A case report. Med. Mycol. Case Rep. 2017, 17, 1–3. [Google Scholar]
- Sun, M.; Hou, X.; Wang, X.; Chen, G.; Zhao, Y. Gastrointestinal Mucormycosis of the Jejunum in an Immunocompetent Patient: A Case Report. Medicine 2017, 96, e6360. [Google Scholar]
- Poyuran, R.; Dharan, B.S.; Sandhyamani, S.; Narasimhaiah, D. Mucormycosis-induced ileocecal perforation: A case report and review of literature. J. Postgrad. Med. 2020, 66, 48–50. [Google Scholar] [CrossRef] [PubMed]
- Bhat, V.; Anitha, S.; Thomas, A.; Kanavi, J.V.; Thomas, A. Intestinal Perforation Secondary to Mucormycosis Associated with Puerperal Sepsis. Cureus 2021, 13, e17428. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Jayashree, M.; Chakrabarti, A.; Sodhi, K.S.; Kanojia, R.P.; Mitra, S. Invasive Gastrointestinal Mucormycosis: A Master Masquerader. Pediatr. Infect. Dis. J. 2018, 37, 1067–1070. [Google Scholar] [CrossRef]
- Aruni, A., Sr.; Tandup, C.; Chowdhury, A., Sr.; Roy, A.; Jha, B. Illicit Drug Use a Risk Factor for Ileal Mucormycosis Presenting with Acute Abdomen. Cureus 2020, 12, e12213. [Google Scholar] [CrossRef]
- Himaal Dev, G.J.; Venkategowda, P.M.; Sutar, A.R.; Shankar, V. Intestinal mucormycosis in an adult with H1N1 pneumonia on extracorporeal membrane oxygenation. Ann. Card. Anaesth. 2021, 24, 92–94. [Google Scholar]
- Manda, D.; Sen, I.; Thakral, P.; Das, S.S.; Cb, V.; Malik, D. Invasive Fungal Infection in COVID-19-Recovered Patient Detected on 18F-FDG-Labeled Leukocytes PET/CT Scan. Clin. Nucl. Med. 2022, 47, e177–e179. [Google Scholar] [CrossRef]
- Zulpi, P.K.; Kulkarni, V.K.; Rani, H.; Halgeri, A.; Agnihotri, A. Double Whammy Due to Coronavirus Disease-2019: Invasive Small Bowel Mucormycosis with Recent-Onset Diabetic Ketoacidosis Presenting as Diffuse Fecal Peritonitis in a 12-Year-Old Girl. J. Indian Assoc. Pediatr. Surg. 2023, 28, 59–61. [Google Scholar] [CrossRef]
- Chethan, K.; Prasad, S.; Ramachandra, L. Ileocolic mucormycosis—An unusual cause of a mass in the right iliac fossa. Can. J. Infect. Dis. Med. Microbiol. 2012, 23, e65–e66. [Google Scholar] [CrossRef][Green Version]
- Yadav, S.; Sharma, A.; Kothari, N.; Bhatia, P.K.; Goyal, S.; Goyal, A. Mucormycosis: A Case Series of Patients Admitted in Non-COVID-19 Intensive Care Unit of a Tertiary Care Center during the Second Wave. Indian J. Crit. Care Med. 2021, 25, 1193–1196. [Google Scholar]
- Sarkardeh, M.; Meftah, E.; Mohammadzadeh, N.; Koushki, J.; Sadrzadeh, Z. COVID-19 and Intestinal Ischemia: A Multicenter Case Series. Front. Med. 2022, 9, 879996. [Google Scholar] [CrossRef]
- Martinello, M.; Nelson, A.; Bignold, L.; Shaw, D. “We are what we eat”! Invasive intestinal mucormycosis: A case report and review of the literature. Med. Mycol. Case Rep. 2012, 1, 52–55. [Google Scholar] [PubMed]
- Kumar, C.; Jain, P.; Wadhwa, N.; Diwaker, P.; Nirupma Panikar, K. Nosocomial Jejunal Mucormycosis—An Unusual Cause of Perforation Peritonitis. Iran. J. Pathol. 2017, 12, 295–300. [Google Scholar] [PubMed]
- Budhiraja, R.; Bhargava, S.; Sood, N. Jejunal stricture due to mucormycosis. Trop. Doct. 2019, 49, 318–320. [Google Scholar]
- Bhana, M.; Laher, N.; McGrath, N.G.; Moeng, M.S. Small bowel mucormycosis: An unexpected case in a penetrating trauma survivor. Int. J. Surg. Case Rep. 2023, 113, 109071. [Google Scholar]
- Watson, M.; Fong, R.; Schoemaker, D.; Due, S. Black fungus: Gastrointestinal invasive mucormycosis causing small bowel perforation, gastric and peristomal ulceration. ANZ J. Surg. 2024, 94, 252–253. [Google Scholar]
- Paliwal, P.; Rahar, S.; Sharma, A.; Gupta, D.; Ahuja, A.; Chauhan, D.S. Intestinal mucormycosis in a patient with COVID-19: A case report. Indian J. Pathol. Microbiol. 2022, 65, 475–477. [Google Scholar]
- Sriperumbuduri, S.; Kalidindi, K.; Megha, H.; Guditi, S.; Taduri, G. An unusual case of gastrointestinal mucormycosis in a patient with nephrotic syndrome. Indian J. Nephrol. 2017, 27, 145–147. [Google Scholar]
- Singh, R.P.; Gupta, N.; Kaur, T.; Gupta, A. Rare case of gastrointestinal mucormycosis with colonic perforation in an immunocompetent patient with COVID-19. BMJ Case Rep. 2021, 14, e244096. [Google Scholar]
- Nagy-Agren, S.E.; Chu, P.; Smith, G.J.; Waskin, H.A.; Altice, F.L. Zygomycosis (mucormycosis) and HIV infection: Report of three cases and review. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 1995, 10, 441–449. [Google Scholar]
- Cebisli, E.; Ulgen-Tekerek, N.; Dursun, O.; Koker, A.; Kisaoglu, A.; Artan, R.; Soyucen, E.; Elpek, G.O. Intestinal Mucormycosis in a Child with Maple Syrup Urine Disease After Orthotopic Liver Transplant. Exp. Clin. Transplant. 2023, 21, 375–379. [Google Scholar]
- Saraf, P.; Naresh Bharti, J. Mucormycosis presenting as intestinal perforation: A pathologist perspective. Arab. J. Gastroenterol. 2024, 25, 234–236. [Google Scholar] [PubMed]
- Eiser, A.R.; Slifkin, R.F.; Neff, M.S. Intestinal mucormycosis in hemodialysis patients following deferoxamine. Am. J. Kidney Dis. 1987, 10, 71–73. [Google Scholar] [PubMed]
- Yinadsawaphan, T.; Ngamskulrungroj, P.; Chalermwai, W.; Dhitinanmuang, W.; Angkasekwinai, N. Gastrointestinal mucormycosis due to Rhizopus microsporus following Streptococcus pyogenes toxic shock syndrome in an HIV patient: A case report. BMC Infect. Dis. 2020, 20, 817. [Google Scholar]
- Li, C.; Zhu, H.; Tan, Y.; Liu, D. Gastrointestinal bleeding due to duodenal mucormycosis in an immunocompetent host mimicking malignancy. Rev. Esp. Enferm. Dig. 2019, 111, 961–962. [Google Scholar]
- Evert, K.; Dienemann, T.; Brochhausen, C.; Lunz, D.; Lubnow, M.; Ritzka, M.; Keil, F.; Trummer, M.; Scheiter, A.; Salzberger, B.; et al. Autopsy findings after long-term treatment of COVID-19 patients with microbiological correlation. Virchows Arch. 2021, 479, 97–108. [Google Scholar]
- Marco del Pont, J.; De Cicco, L.; Gallo, G.; Llera, J.; De Santibanez, E.; D’Agostino, D. Hepatic arterial thrombosis due to Mucor species in a child following orthotopic liver transplantation. Transpl. Infect. Dis. 2000, 2, 33–35. [Google Scholar]
- Mekeel, K.L.; Hemming, A.W.; Reed, A.I.; Matsumoto, T.; Fujita, S.; Schain, D.C.; Nelson, D.R.; Dixon, L.R.; Fujikawa, T. Hepatic mucormycosis in a renal transplant recipient. Transplantation 2005, 79, 1636. [Google Scholar]
- Zhan, H.X.; Lv, Y.; Zhang, Y.; Liu, C.; Wang, B.; Jiang, Y.Y.; Liu, X.M. Hepatic and renal artery rupture due to Aspergillus and Mucor mixed infection after combined liver and kidney transplantation: A case report. Transplant. Proc. 2008, 40, 1771–1773. [Google Scholar]
- Abboud, C.S.; Bergamasco, M.D.; Baia, C.E.; Lallee, M.P.; Zan, A.S.; Zamorano, M.M.; Pereira, O.I.; Mies, S. Case report of hepatic mucormycosis after liver transplantation: Successful treatment with liposomal amphotericin B followed by posaconazole sequential therapy. Transplant. Proc. 2012, 44, 2501–2502. [Google Scholar]
- Chaudhary, R.J.; Choudhary, N.S.; Saraf, N.; Gautam, D.; Piplani, T.; Thiagrajan, S.; Bhangui, P.; Saigal, S.; Rastogi, A.; Soin, A.S. Delayed Graft Dysfunction due to Invasive Hepatic Mucormycosis After Living Donor Liver Transplantation. J. Clin. Exp. Hepatol. 2020, 10, 629–632. [Google Scholar]
- Teira, R.; Trinidad, J.M.; Eizaguirre, B.; Ortiz, J.; Santamaria, J.M. Zygomycosis of the spleen in a patient with the acquired immunodeficiency syndrome. Mycoses 1993, 36, 437–439. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Huang, X.; Li, Y.; Wang, J. Isolated splenic mucormycosis secondary to diabetic ketoacidosis: A case report. BMC Infect. Dis. 2022, 22, 596. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, A.; Ghosh, A.; Prasad, G.S.; David, J.K.; Gupta, S.; Das, A.; Sakhuja, V.; Panda, N.K.; Singh, S.K.; Das, S.; et al. Apophysomyces elegans: An emerging zygomycete in India. J. Clin. Microbiol. 2003, 41, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Singh, S.K.; Kakkar, N.; Jain, S.; Kalra, N.; Sakia, U.N. Splenic and renal mucormycosis in a healthy host: Successful management by aggressive treatment. Trop. Gastroenterol. 2010, 31, 57–58. [Google Scholar]
- O’Connor, C.; Farrell, C.; Fabre, A.; Eaton, D.; Redmond, K.; McSharry, D.G.; Conneely, J.B.; Shields, C.J.; Egan, J.J.; Hannan, M.M. Near-fatal mucormycosis post-double lung transplant presenting as uncontrolled upper gastrointestinal haemorrhage. Med. Mycol. Case Rep. 2018, 21, 30–33. [Google Scholar] [CrossRef]
- Jain, M.; Tyagi, R.; Tyagi, R.; Jain, G. Post-COVID-19 Gastrointestinal Invasive Mucormycosis. Indian J. Surg. 2022, 84, 545–547. [Google Scholar] [CrossRef]
- Okhuysen, P.C.; Rex, J.H.; Kapusta, M.; Fife, C. Successful treatment of extensive posttraumatic soft-tissue and renal infections due to Apophysomyces elegans. Clin. Infect. Dis. 1994, 19, 329–331. [Google Scholar] [CrossRef]
- Durila, M.; Pavlicek, P.; Hadacova, I.; Nahlovsky, J.; Janeckova, D. Endogenous Heparinoids May Cause Bleeding in Mucor Infection and can be Detected by Nonactivated Thromboelastometry and Treated by Recombinant Activated Factor VII: A Case Report. Medicine 2016, 95, e2933. [Google Scholar] [CrossRef]
- Sedlacek, M.; Cotter, J.G.; Suriawinata, A.A.; Kaneko, T.M.; Zuckerman, R.A.; Parsonnet, J.; Block, C.A. Mucormycosis peritonitis: More than 2 years of disease-free follow-up after posaconazole salvage therapy after failure of liposomal amphotericin, B. Am. J. Kidney Dis. 2008, 51, 302–306. [Google Scholar] [CrossRef]
- Polo, J.R.; Luno, J.; Menarguez, C.; Gallego, E.; Robles, R.; Hernandez, P. Peritoneal mucormycosis in a patient receiving continuous ambulatory peritoneal dialysis. Am. J. Kidney Dis. 1989, 13, 237–239. [Google Scholar] [CrossRef]
- Fergie, J.E.; Fitzwater, D.S.; Einstein, P.; Leggiadro, R.J. Mucor peritonitis associated with acute peritoneal dialysis. Pediatr. Infect. Dis. J. 1992, 11, 498–500. [Google Scholar] [PubMed]
- Adam, R.D.; Hunter, G.; DiTomasso, J.; Comerci, G., Jr. Mucormycosis: Emerging prominence of cutaneous infections. Clin. Infect. Dis. 1994, 19, 67–76. [Google Scholar] [PubMed]
- Khan, Z.U.; Chugh, T.D. Invasive fungal infections in Kuwait: A retrospective study. Indian J. Chest Dis. Allied Sci. 2000, 42, 279–287. [Google Scholar] [PubMed]
- Monecke, S.; Hochauf, K.; Gottschlich, B.; Ehricht, R. A case of peritonitis caused by Rhizopus microsporus. Mycoses 2006, 49, 139–142. [Google Scholar]
- Pimentel, J.D.; Dreyer, G.; Lum, G.D. Peritonitis due to Cunninghamella bertholletiae in a patient undergoing continuous ambulatory peritoneal dialysis. J. Med. Microbiol. 2006, 55 Pt 1, 115–118. [Google Scholar]
- Nayak, S.; Satish, R.; Gokulnath Savio, J.; Rajalakshmi, T. Peritoneal mucormycosis in a patient on CAPD. Perit. Dial. Int. 2007, 27, 216–217. [Google Scholar]
- Bhutada, K.; Borkar, S.S.; Mendiratta, D.K.; Shende, V.R. Successful treatment of peritonitis by C. bertholletiae in a chronic kidney failure patient on continuous ambulatory peritoneal dialysis after kidney rejection. Singap. Med. J. 2012, 53, e106–e109. [Google Scholar]
- Pamidimukkala, U.; Sudhaharan, S.; Kancharla, A.; Vemu, L.; Challa, S.; Karanam, S.D.; Chavali, P.; Prakash, H.; Ghosh, A.K.; Gupta, S.; et al. Mucormycosis due to Apophysomyces species complex- 25 years’ experience at a tertiary care hospital in southern India. Med. Mycol. 2020, 58, 425–433. [Google Scholar]
- Dalgic, B.; Bukulmez, A.; Sari, S. Pyogenic liver abscess and peritonitis due to Rhizopus oryzae in a child with Papillon-Lefevre syndrome. Eur. J. Pediatr. 2011, 170, 803–805. [Google Scholar]
- Verma, G.R.; Lobo, D.R.; Walker, R.; Bose, S.M.; Gupta, K.L. Disseminated mucormycosis in healthy adults. J. Postgrad. Med. 1995, 41, 40–42. [Google Scholar]
- Kaushik, R. Primary cutaneous zygomycosis in India. Indian J. Surg. 2012, 74, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, A.; Kumar, P.; Padhye, A.A.; Chatha, L.; Singh, S.K.; Das, A.; Wig, J.D.; Kataria, R.N. Primary cutaneous zygomycosis due to Saksenaea vasiformis and Apophysomyces elegans. Clin. Infect. Dis. 1997, 24, 580–583. [Google Scholar] [CrossRef] [PubMed]
- Mathews, M.S.; Raman, A.; Nair, A. Nosocomial zygomycotic post-surgical necrotizing fasciitis in a healthy adult caused by Apophysomyces elegans in south India. J. Med. Vet. Mycol. 1997, 35, 61–63. [Google Scholar] [CrossRef][Green Version]
- Kumar, A.; Khilnani, G.C.; Aggarwal, S.; Kumar, S.; Banerjee, U.; Xess, I. Primary cutaneous mucormycosis in an immunocompetent host: Report of a case. Surg. Today 2003, 33, 319–322. [Google Scholar] [CrossRef]
- Thami, G.P.; Kaur, S.; Bawa, A.S.; Chander, J.; Mohan, H.; Bedi, M.S. Post-surgical zygomycotic necrotizing subcutaneous infection caused by Absidia corymbifera. Clin. Exp. Dermatol. 2003, 28, 251–253. [Google Scholar] [CrossRef]
- Kerbaul, F.; Guidon, C.; Collart, F.; Lepidi, H.; Cayatte, B.; Bonnet, M.; Bellezza, M.; Métras, D.; Gouin, F. Abdominal wall mucormycosis after heart transplantation. J. Cardiothorac. Vasc. Anesth. 2004, 18, 822–823. [Google Scholar] [CrossRef]
- Padmaja, I.J.; Ramani, T.V.; Kalyani, S. Cutaneous zygomycosis: Necrotising fascitis due to Saksenaea vasiformis. Indian J. Med. Microbiol. 2006, 24, 58–60. [Google Scholar] [CrossRef]
- Belfiori, R.; Terenzi, A.; Marchesini, L.; Repetto, A. Absidia Corymbifera in an immune competent accident victim with multiple abdominal injuries: Case report. BMC Infect. Dis. 2007, 7, 46. [Google Scholar] [CrossRef]
- Tilak, R.; Raina, P.; Gupta, S.K.; Tilak, V.; Prakash, P.; Gulati, A.K. Cutaneous zygomycosis: A possible postoperative complication in immunocompetent individuals. Indian J. Dermatol. Venereol. Leprol. 2009, 75, 596–599. [Google Scholar] [CrossRef]
- Tapish, S.; Taha, M.; Naresh, G.; Neeraj, D.; Malik Vinod, K. Primary mucormycosis of abdominal wall: A rare fungal infection in a immunocompetent patient. Indian J. Surg. 2010, 72 (Suppl. S1), 306–308. [Google Scholar] [CrossRef]
- Alharbi, M.; Jhinger, R.K.; Wuerz, T.; Walkty, A. Marked peripheral eosinophilia due to prolonged administration of posaconazole. JMM Case Rep. 2017, 4, e005100. [Google Scholar]
- Ram, R.; Swarnalatha, G.; Prasad, N.; Dakshinamurty, K.V. Exit site infection due to Zygomycosis resulting in abdominal wall necrosis in a continuous ambulatory peritoneal dialysis patient. Nephrol. Dial. Transplant. 2007, 22, 266–267. [Google Scholar]
- Patel, A.K.; Vora, H.J.; Patel, K.K.; Patel, B. Elderly diabetic patient with surgical site mucormycosis extending to bowel. J. Glob. Infect. Dis. 2010, 2, 186–188. [Google Scholar]
- Zhao, L.; Wang, C.X.; Zhang, L.; Tu, X.A.; Wang, W.; Chen, Y.; Liu, L.S. Mucormycosis extending from the surgical wound to the transplanted kidney: Case report and literature review. Exp. Clin. Transplant. 2012, 10, 403–405. [Google Scholar]
- Paonam, S.; Bag, S.; Mavuduru, R.S.; Agarwal, M.M.; Mandal, A.K. Isolated bilateral renal mucormycosis masquerading as renal abscess in an immunocompetent individual: A lesson learnt. Case Rep. Urol. 2014, 2014, 304380. [Google Scholar]
- Narayanaswamy, S.; Goradia, R.; Bellurkar, A.; Patwardhan, S. Isolated renal mucormycosis masquerading as emphysematous pyelonephritis. BMJ Case Rep. 2023, 16, e254501. [Google Scholar]
- Stein, A.; Schmaman, A. Rupture of the stomach due to mucormycosis. S Afr. J. Surg. 1965, 3, 123–129. [Google Scholar]
- Deal, W.B.; Johnson, J.E., 3rd. Gastric phycomycosis. Report of a case and review of the literature. Gastroenterology 1969, 57, 579–586. [Google Scholar]
- Branton, M.H.; Johnson, S.C.; Brooke, J.D.; Hasbargen, J.A. Peritonitis due to Rhizopus in a patient undergoing continuous ambulatory peritoneal dialysis. Rev. Infect. Dis. 1991, 13, 19–21. [Google Scholar]
- Norden, G.; Bjorck, S.; Persson, H.; Svalander, C.; Li, X.G.; Edebo, L. Cure of zygomycosis caused by a lipase-producing Rhizopus rhizopodiformis strain in a renal transplant patient. Scand. J. Infect. Dis. 1991, 23, 377–382. [Google Scholar]
- Vadeboncoeur, C.; Walton, J.M.; Raisen, J.; Soucy, P.; Lau, H.; Rubin, S. Gastrointestinal mucormycosis causing an acute abdomen in the immunocompromised pediatric patient—Three cases. J. Pediatr. Surg. 1994, 29, 1248–1249. [Google Scholar] [PubMed]
- Hosseini, M.; Lee, J. Gastrointestinal mucormycosis mimicking ischemic colitis in a patient with systemic lupus erythematosus. Am. J. Gastroenterol. 1998, 93, 1360–1362. [Google Scholar] [PubMed]
- Guardia, J.A.; Bourgoignie, J.; Diego, J. Renal mucormycosis in the HIV patient. Am. J. Kidney Dis. 2000, 35, E24. [Google Scholar]
- Herbrecht, R.; Letscher-Bru, V.; Bowden, R.A.; Kusne, S.; Anaissie, E.J.; Graybill, J.R.; Noskin, G.A.; Oppenheim, B.A.; Andrès, E.; Pietrelli, L.A. Treatment of 21 cases of invasive mucormycosis with amphotericin B colloidal dispersion. Eur. J. Clin. Microbiol. Infect. Dis. 2001, 20, 460–466. [Google Scholar]
- Nannini, E.C.; Paphitou, N.I.; Ostrosky-Zeichner, L. Peritonitis due to Aspergillus and zygomycetes in patients undergoing peritoneal dialysis: Report of 2 cases and review of the literature. Diagn. Microbiol. Infect. Dis. 2003, 46, 49–54. [Google Scholar]
- Serna, J.H.; Wanger, A.; Dosekun, A.K. Successful treatment of mucormycosis peritonitis with liposomal amphotericin B in a patient on long-term peritoneal dialysis. Am. J. Kidney Dis. 2003, 42, E14–E17. [Google Scholar]
- Alkhunaizi, A.M.; Amir, A.A.; Al-Tawfiq, J.A. Invasive fungal infections in living unrelated renal transplantation. Transplant. Proc. 2005, 37, 3034–3037. [Google Scholar]
- Sethi, J.; Ramachandran, R.; Kohli, H.S.; Gupta, K.L. Isolated renal mucormycosis in a patient with Idiopathic CD4 lymphocytopenia. BMJ Case Rep. 2018, 2018, bcr201825234. [Google Scholar]
- Deja, M.; Wolf, S.; Weber-Carstens, S.; Lehmann, T.N.; Adler, A.; Ruhnke, M.; Tintelnot, K. Gastrointestinal zygomycosis caused by Mucor indicus in a patient with acute traumatic brain injury. Med. Mycol. 2006, 44, 683–687. [Google Scholar]
- Taj-Aldeen, S.J.; Almaslamani, M.; Theelen, B.; Boekhout, T. Phylogenetic analysis reveals two genotypes of the emerging fungus Mucor indicus, an opportunistic human pathogen in immunocompromised patients. Emerg. Microbes Infect. 2017, 6, e63. [Google Scholar]
- Manchikalapati, P.; Canon, C.L.; Jhala, N.; Eloubeidi, M.A. Gastrointestinal zygomycosis complicating heart and lung transplantation in a patient with Eisenmenger’s syndrome. Dig. Dis. Sci. 2005, 50, 1181–1183. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.H.; Choi, H.J.; Yoo, J.; Kang, S.J.; Lee, K.Y. Emphysematous gastritis associated with invasive gastric mucormycosis: A case report. J. Korean Med. Sci. 2007, 22, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Berne, J.D.; Villarreal, D.H.; McGovern, T.M.; Rowe, S.A.; Moore, F.O.; Norwood, S.H. A fatal case of posttraumatic gastric mucormycosis. J. Trauma 2009, 66, 933–935. [Google Scholar] [CrossRef] [PubMed]
- Islam, J.; Thomson, S.R.; Tudor, G.; Khan, Z.; Mjoli, M. Ileosigmoid knot complicated by gastric and splenic mucormycosis: A lethal combination. BMJ Case Rep. 2009, 2009, bcr10.2008.1049. [Google Scholar] [CrossRef]
- Mezhir, J.J.; Mullane, K.M.; Zarling, J.; Satoskar, R.; Pai, R.K.; Roggin, K.K. Successful nonoperative management of gastrointestinal mucormycosis: Novel therapy for invasive disease. Surg. Infect. 2009, 10, 447–451. [Google Scholar] [CrossRef]
- Van Sickels, N.; Hoffman, J.; Stuke, L.; Kempe, K. Survival of a patient with trauma-induced mucormycosis using an aggressive surgical and medical approach. J. Trauma. 2011, 70, 507–509. [Google Scholar] [CrossRef]
- Rudler, M.; Barret, M.; Poynard, T.; Thabut, D. Gastric mucormycosis: A rare cause of gastrointestinal bleeding in cirrhosis. Clin. Res. Hepatol. Gastroenterol. 2012, 36, e32–e33. [Google Scholar] [CrossRef]
- Tan, J.; Manickam, R.; Pisharam, J.; Telisinghe, P.; Chong, V.H. Mucormycosis—A possible trigger pathogen for encapsulating peritoneal sclerosis. Perit. Dial. Int. 2012, 32, 479–481. [Google Scholar] [CrossRef]
- Enani, M.A.; Alharthi, B.N.; Dewanjee, N.; Bhat, N.A.; Fagih, M. Spontaneous gastric ulcer perforation and acute spleen infarction caused by invasive gastric and splenic mucormycosis. J. Glob. Infect. Dis. 2014, 6, 122–124. [Google Scholar] [CrossRef]
- Gaut, D.; Cone, B.D.; Gregson, A.L.; Agopian, V.G. Gastrointestinal Mucormycosis After Orthotopic Liver Transplantation Presenting as Femoral Nerve Palsy: A Case Report and Review of the Literature. Transplant. Proc. 2017, 49, 1608–1614. [Google Scholar] [CrossRef]
- Izaguirre-Anariba, D.E.; Chee, F.; Thet, Z.; Lanza, J. An Interesting Case of a 57-Year-Old Male with an Upper Gastrointestinal Bleeding and Obstructive Uropathy with Bilateral Hydronephrosis Diagnosed with Systemic Mucormycosis. Case Rep. Infect. Dis. 2018, 2018, 6283701. [Google Scholar]
- Aggarwal, P.; Patel, H.; Gonzalez, L.; Brown, L.; Agarwal, A.; Speeg, K. Invasive Colonic Mucormycosis in an Immunocompromised Postliver Transplant Patient. ACG Case Rep. J. 2020, 7, e00450. [Google Scholar]
- Reis, F.P.D.; Campos, S.V.; Aiello, V.D.; Duarte, M.I.S.; Samano, M.N.; Pego-Fernandes, P.M. Gastrointestinal mucormycosis post lung transplantation. Braz. J. Infect. Dis. 2019, 23, 368–370. [Google Scholar] [PubMed]
- Rotundo, L. A fatal case of disseminated gastric mucormycosis with emphysematous gastritis. Am. J. Gastroenterol. 2019, 114, S1505–S1506. [Google Scholar]
- Sehmbey, G.; Malik, R.; Kosa, D.; Srinivasan, I.; Chuang, K.Y.; Bellapravalu, S. Gastric Ulcer and Perforation due to Mucormycosis in an Immunocompetent Patient. ACG Case Rep. J. 2019, 6, e00154. [Google Scholar]
- Shankaralingappa, S. Unsuspected invasive gastrointestinal mucormycosis masquerading as inflammatory bowel disease: A pathologist’s perspective. Indian J. Pathol. Microbiol. 2019, 62, 332–334. [Google Scholar]
- Petrochko, J.M.; Abrahamian, G.; Cigarroa, F.; Thomas, E. Colonic mucormycosis in solid organ transplantation: Case report and review of the literature (colonic mucormycosis after DDLT). Transpl. Infect. Dis. 2020, 22, e13362. [Google Scholar]
- Shah, C.; Zimmerman, S.; McKinney, J.; Ebers, A. Colonic mucormycosis in an immunocompetent patient with endocarditis. IDCases 2020, 20, e00773. [Google Scholar]
- Chiang, T.H.; Lee, Y.W.; Tan, J.H.; Kao, C.C.; Chang, C.C.; Fang, K.C. Mucormycosis causing massive lower gastrointestinal bleeding: A case report. BMC Gastroenterol. 2021, 21, 272. [Google Scholar]
- Hammami, F.; Koubaa, M.; Chakroun, A.; Smaoui, F.; Marrakchi, C.; Hentati, N.; Mzali, R.; Rekik, K.; Jemaa, M.B. Survival of an immuno-competent patient from splenic and gastric mucormycosis-case report and review of the literature. J. Mycol. Med. 2021, 31, 101174. [Google Scholar]
- Martin-Blais, R.; Pathak, S.; Fitzwater, S.; Dawson, D.W.; Sisk, A.E.; Farmer, D.G.; Venick, R.; Yeganeh, N. Intestinal mucormycosis initially identified by next-generation sequencing of cell-free, D.N.A. Transpl. Infect. Dis. 2021, 23, e13656. [Google Scholar]
- Varshney, V.K.; Swami, A.; Thirunavukkarasu, B.; Agarwal, A.; Baid, G. Synchronous Small Bowel Gangrene with Pyelonephritis Secondary to Mucormycosis: A Disastrous Complication of COVID-19 Pandemic. Cureus 2021, 13, e15911. [Google Scholar]
- Kyuno, D.; Kubo, T.; Tsujiwaki, M.; Sugita, S.; Hosaka, M.; Ito, H.; Harada, K.; Takasawa, A.; Kubota, Y.; Takasawa, K.; et al. COVID-19-associated disseminated mucormycosis: An autopsy case report. World J. Clin. Cases. 2022, 10, 10358–10365. [Google Scholar] [PubMed]
- Ito, H.; Kakizaki, R.; Harada, K.; Kyuno, D.; Kubo, T.; Bunya, N.; Kasai, T.; Uemura, S.; Narimatsu, E. Disseminated mucormycosis in a patient with severe COVID-19 on venovenous extracorporeal membrane oxygenation: A case report. IDCases 2022, 29, e01578. [Google Scholar]
- Meshram, H.S.; Kumar, D.; Kute, V.B. Rare and Unusual Follow-up Sequelae of Coronavirus Disease 2019: Splenic Mucormycosis in a Renal Transplant Recipient. Transplant Proc. 2022, 54, 1554–1556. [Google Scholar]
- Ralaizanaka, B.M.; Razafindrazoto, C.I.; Bolot, E.; Bors, G.; Housson-Wetzel, S.; Razafimahefa, S.H.; Ramanampamonjy, R.M.; Claude, P. Gastrointestinal Mucormycosis-Induced Massive Lower Gastrointestinal Bleeding, Rectal Perforation, and Pulmonary Embolism: A Long Diagnostic Pathway in a Case Report. Clin. Exp. Gastroenterol. 2022, 15, 145–151. [Google Scholar]
- Banerjee, N.; Lodha, M.; Kompally, P.; Chawla, S. Post-COVID-19 Intestinal and Mesenteric Mucormycosis. Am. Surg. 2023, 89, 2770–2773. [Google Scholar]
- Rathi, C.; Shinde, R.K.; Dighe, S.P.; Lamture, Y.; Mahawar, R. Gastric Necrosis: A Rare Complication of Gastric Mucormycosis. Cureus 2023, 15, e35810. [Google Scholar]
- Li, K.W.; Wen, T.F.; Li, G.D. Hepatic mucormycosis mimicking hilar cholangiocarcinoma: A case report and literature review. World J. Gastroenterol. 2010, 16, 1039–1042. [Google Scholar]
- Rabin, E.R.; Lundberg, G.D.; Mitchell, E.T. Mucormycosis in severely burned patients. Report of two cases with extensive destruction of the face and nasal cavity. N. Engl. J. Med. 1961, 264, 1286–1289. [Google Scholar]
- Virmani, R.; Connor, D.H.; McAllister, H.A. Cardiac mucormycosis. A report of five patients and review of 14 previously reported cases. Am. J. Clin. Pathol. 1982, 78, 42–47. [Google Scholar] [PubMed]
- Straatsma, B.R.; Zimmerman, L.E.; Gass, J.D. Phycomycosis. A clinicopathologic study of fifty-one cases. Lab. Investig. 1962, 11, 963–985. [Google Scholar] [PubMed]
- Agger, W.A.; Maki, D.G. Mucormycosis. A complication of critical care. Arch. Intern. Med. 1978, 138, 925–927. [Google Scholar]
- Gupta, K.L.; Joshi, K.; Pereira, B.J.; Singh, K. Disseminated mucormycosis presenting with acute renal failure. Postgrad. Med. J. 1987, 63, 297–299. [Google Scholar]
- Nakamura, M.; Weil, W.B., Jr.; Kaufman, D.B. Fatal fungal peritonitis in an adolescent on continuous ambulatory peritoneal dialysis: Association with deferoxamine. Pediatr. Nephrol. 1989, 3, 80–82. [Google Scholar]
- Singh, N.; Gayowski, T.; Singh, J.; Yu, V.L. Invasive gastrointestinal zygomycosis in a liver transplant recipient: Case report and review of zygomycosis in solid-organ transplant recipients. Clin. Infect. Dis. 1995, 20, 617–620. [Google Scholar]
- Stoebner, P.E.; Gaspard, C.; Mourad, G.; Beraud, J.J.; Meynadier, J.; Meunier, L. Fulminant mucormycosis in a renal transplant recipient. Acta Derm. Venereol. 2000, 80, 305. [Google Scholar]
- Tsaousis, G.; Koutsouri, A.; Gatsiou, C.; Paniara, O.; Peppas, C.; Chalevelakis, G. Liver and brain mucormycosis in a diabetic patient type II successfully treated with liposomial amphotericin B. Scand. J. Infect. Dis. 2000, 32, 335–337. [Google Scholar]
- Sehgal, A.; Raghavendran, M.; Kumar, D.; Srivastava, A.; Dubey, D.; Kumar, A. Rhinocerebral mucormycosis causing basilar artery aneurysm with concomitant fungal colonic perforation in renal allograft recipient: A case report. Transplantation 2004, 78, 949–950. [Google Scholar]
- Gimeno-García, A.; Parra-Blanco, A.; Nicolás-Pérez, D.; Manzano-Sanz, C.; Méndez-Medina, R.; Quintero, E. Mucormycosis with gastric involvement in a patient with severe atheromatous vascular disease. Dig. Endosc. 2006, 18, 144–146. [Google Scholar]
- Alexander, B.D.; Schell, W.A.; Siston, A.M.; Rao, C.Y.; Bower, W.A.; Balajee, S.A.; Howell, D.N.; Moore, Z.S.; Noble-Wang, J.; Rhyne, J.A.; et al. Fatal Apophysomyces elegans infection transmitted by deceased donor renal allografts. Am. J. Transplant. 2010, 10, 2161–2167. [Google Scholar] [PubMed]
- Arena, V.; De-Giorgio, F.; Pennacchia, I.; Manna, R.; Vetrugno, G.; Stigliano, E.; Milic, N.; Gasbarrini, G.; Abenavoli, L. Haemophagocytic syndrome associated with mucormycosis infection. Int. J. Immunopathol. Pharmacol. 2012, 25, 751–755. [Google Scholar] [PubMed]
- Gurevich, M.; Levi, I.; Steinberg, R.; Shonfeld, T.; Shapiro, R.; Israeli, M.; Sprecher, H.; Shalit, I.; Mor, E. Mucormycosis in a liver allograft: Salvage re-transplantation and targeted immunosuppressive management. Transpl. Infect. Dis. 2012, 14, E97–E101. [Google Scholar]
- Nam, Y.; Jung, J.; Park, S.S.; Kim, S.J.; Shin, S.J.; Choi, J.H.; Kim, M.; Yoon, H.E. Disseminated mucormycosis with myocardial involvement in a renal transplant recipient. Transpl. Infect. Dis. 2015, 17, 890–896. [Google Scholar]
- Alqhamdi, S.; Idress, B.; Alharbi, A.; Aljurais, N. Case report: Disseminated pulmonary mucormycosis involving spleen in diabetic patient with aggressive surgical approach. Int. J. Surg. Case Rep. 2019, 54, 42–46. [Google Scholar]
- Sami, C.A.; Rashed, H.M.; Khan, A.H.; Barai, L.; Arafat, S.M. Disseminated mucormycosis: An unusual case of ascites with bone marrow invasion. IDCases 2022, 29, e01553. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).