Obesity Report: Distribution and Pattern by Age and Sex in Heart Failure Cohort over 10 Years in Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Source of Data
2.2. Population and Study Design
2.3. Definition of Obesity
2.4. Statistical Analysis
3. Results
3.1. BMI and Sex Distribution in Heart Failure
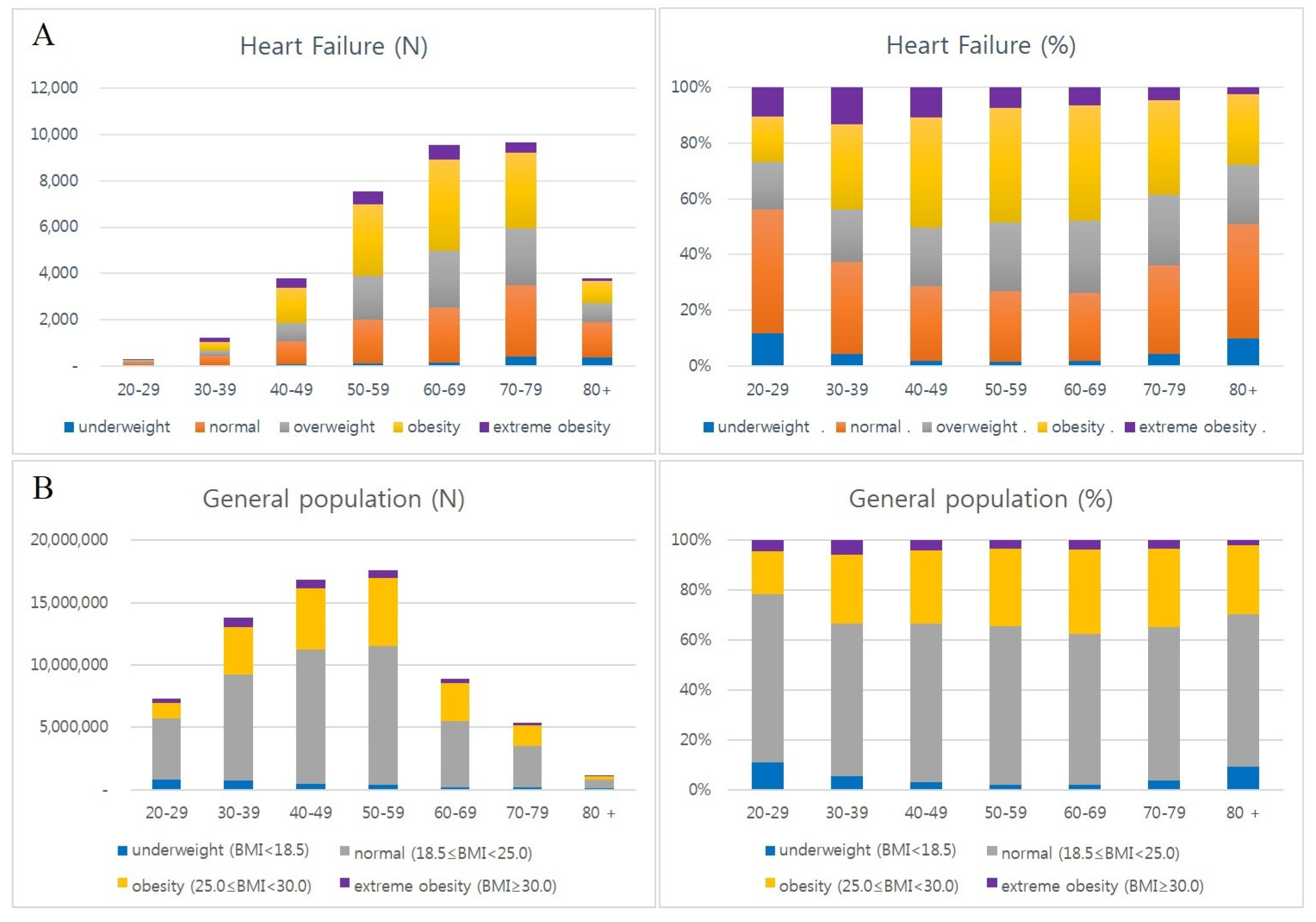
3.2. Distribution of BMI Subgroups by Age in Heart Failure
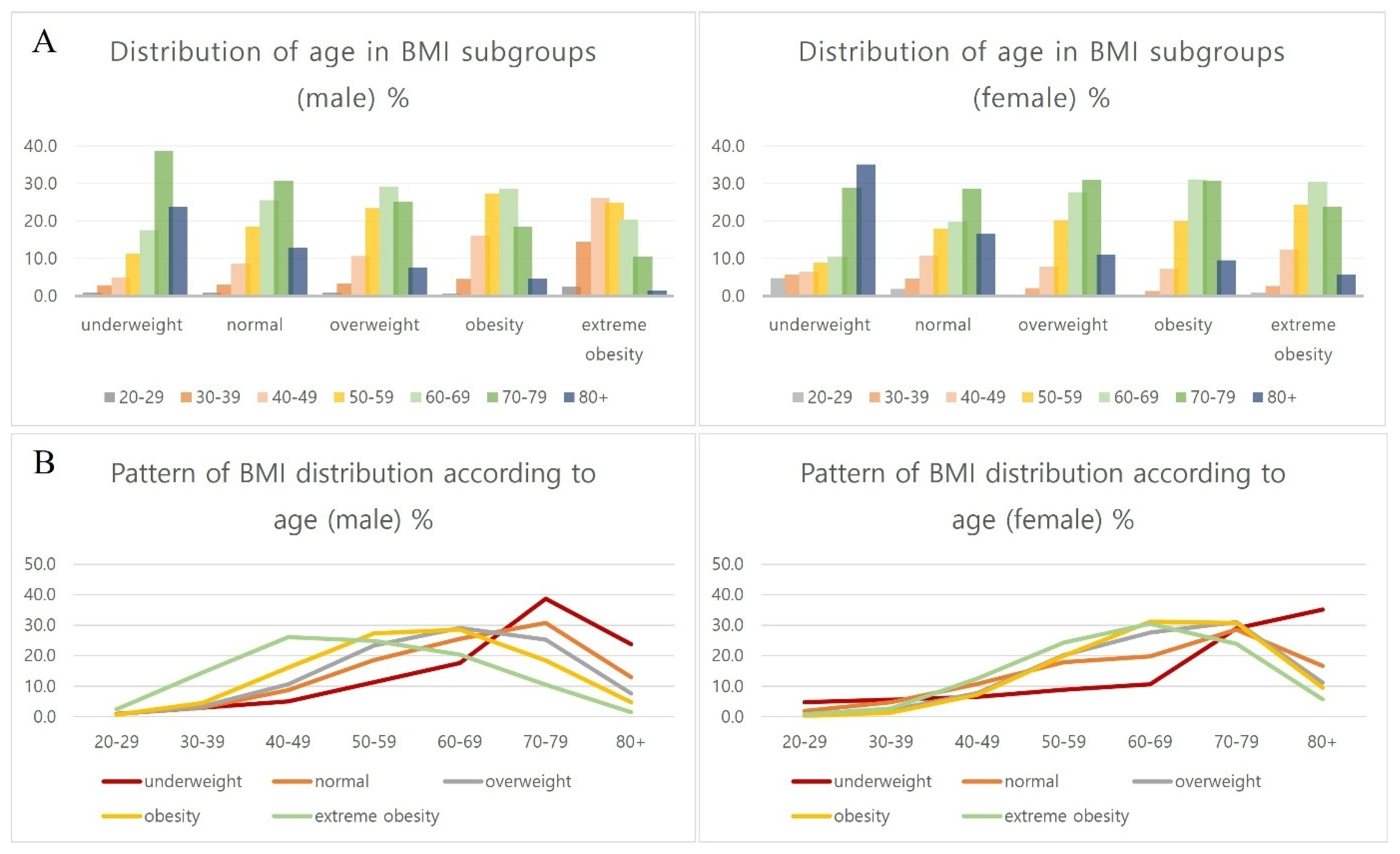
3.3. Distribution of BMI Subgroups by Age and Sex in Heart Failure
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The global syndemic of obesity, undernutrition, and climate change: The Lancet Commission report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Kim, S.E.; Lee, C.J. The paradox in defining obesity in patients with heart failure. Int. J. Heart Fail. 2022, 4, 91–94. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief 2020, 360, 1–8. [Google Scholar]
- World Obesity Federation. World Obesity Atlas 2022; WOF: London, UK, 2022; Available online: https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2022 (accessed on 7 June 2022).
- Nam, G.E.; Kim, Y.H.; Han, K.; Jung, J.H.; Rhee, E.J.; Lee, S.S.; Kim, D.J.; Lee, K.W.; Lee, W.Y.; Korean Society for the Study of Obesity. Obesity Fact Sheet in Korea, 2019: Prevalence of Obesity and Abdominal Obesity from 2009 to 2018 and Social Factors. J. Obes. Metab. Syndr. 2020, 29, 124–132. [Google Scholar] [CrossRef]
- Rhee, E.J. Prevalence and Current Management of Cardiovascular Risk Factors in Korean Adults Based on Fact Sheets. Endocrinol. Metab. 2020, 35, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.S.; Han, B.D.; Han, K.; Jung, J.H.; Son, J.W.; Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity Fact Sheet in Korea, 2021: Trends in Obesity Prevalence and Obesity-Related Comorbidity Incidence Stratified by Age from 2009. J. Obes. Metab. Syndr. 2022, 31, 169–177. [Google Scholar] [CrossRef]
- Seo, M.H.; Kim, Y.H.; Han, K.; Jung, J.H.; Park, Y.G.; Lee, S.S.; Kwon, H.S.; Lee, W.Y.; Yoo, S.J. Prevalence of Obesity and Incidence of Obesity-Related Comorbidities in Koreans Based on National Health Insurance Service Health Checkup Data 2006–2015. J. Obes. Metab. Syndr. 2018, 27, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Stenholm, S.; Head, J.; Aalto, V.; Kivimäki, M.; Kawachi, I.; Zins, M.; Goldberg, M.; Platts, L.G.; Zaninotto, P.; Magnusson Hanson, L.L.; et al. Body Mass Index as a Predictor of Healthy and Disease-Free Life Expectancy between Ages 50 and 75: A Multicohort Study. Int. J. Obes. 2017, 41, 769–775. [Google Scholar] [CrossRef]
- Dai, H.; Alsalhe, T.A.; Chalghaf, N.; Ricco, M.; Bragazzi, N.L.; Wu, J. The Global Burden of Disease Attributable to High Body Mass Index in 195 Countries and Territories, 1990–2017: An Analysis of the Global Burden of Disease Study. PLoS Med. 2020, 17, e1003198. [Google Scholar] [CrossRef]
- Hu, G.; Tuomilehto, J.; Silventoinen, K.; Sarti, C.; Mannisto, S.; Jousilahti, P. Body Mass Index, Waist Circumference, and Waist–Hip Ratio on the Risk of Total and Type-Specific Stroke. Arch. Intern. Med. 2007, 167, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Ye, W.; Adami, H.O.; Weiderpass, E. Prospective Study of Body Size and Risk for Stroke Amongst Women Below Age 60. J. Intern. Med. 2006, 260, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Heart Failure Society of America. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J. Card. Fail. 2010, 16, e1–e194. [Google Scholar] [CrossRef]
- Aune, D.; Sen, A.; Norat, T.; Janszky, I.; Romundstad, P.; Tonstad, S.; Vatten, L.J. Body Mass Index, Abdominal Fatness, and Heart Failure Incidence and Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Circulation 2016, 133, 639–649. [Google Scholar] [CrossRef]
- Kenchaiah, S.; Evans, J.C.; Levy, D.; Wilson, P.W.; Benjamin, E.J.; Larson, M.G.; Kannel, W.B.; Vasan, R.S. Obesity and the Risk of Heart Failure. N. Engl. J. Med. 2002, 347, 305–313. [Google Scholar] [CrossRef]
- Pandey, A.; LaMonte, M.; Klein, L.; Ayers, C.; Psaty, B.M.; Eaton, C.B.; Allen, N.B.; de Lemos, J.A.; Carnethon, M.; Greenland, P.; et al. Relationship Between Physical Activity, Body Mass Index, and Risk of Heart Failure. J. Am. Coll. Cardiol. 2017, 69, 1129–1142. [Google Scholar] [CrossRef]
- Butt, J.H.; Petrie, M.C.; Jhund, P.S.; Sattar, N.; Desai, A.S.; Køber, L.; Rouleau, J.L.; Swedberg, K.; Zile, M.R.; Solomon, S.D.; et al. Anthropometric Measures and Adverse Outcomes in Heart Failure with Reduced Ejection Fraction: Revisiting the Obesity Paradox. Eur. Heart J. 2023, 44, 1136–1153. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO European Regional Obesity Report 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Després, J.P. Body Fat Distribution and Risk of Cardiovascular Disease: An Update. Circulation 2012, 126, 1301–1313. [Google Scholar] [CrossRef]
- Abel, E.D.; Litwin, S.E.; Sweeney, G. Cardiac Remodeling in Obesity. Physiol. Rev. 2008, 88, 389–419. [Google Scholar] [CrossRef]
- Khan, S.S.; Ning, H.; Wilkins, J.T.; Allen, N.; Carnethon, M.; Berry, J.D.; Sweis, R.N.; Lloyd-Jones, D.M. Association of Body Mass Index with Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018, 3, 280–287. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef]
- Lavie, C.J.; Alpert, M.A.; Arena, R.; Mehra, M.R.; Milani, R.V.; Ventura, H.O. Impact of Obesity and the Obesity Paradox on Prevalence and Prognosis in Heart Failure. JACC Heart Fail. 2013, 1, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.J. The South Korean Health Care System. Jpn. Med. Assoc. J. 2009, 52, 206–209. [Google Scholar]
- Lee, H.; Oh, S.H.; Cho, H.; Cho, H.J.; Kang, H.Y. Prevalence and Socio-Economic Burden of Heart Failure in an Aging Society of South Korea. BMC Cardiovasc. Disord. 2016, 16, 215. [Google Scholar] [CrossRef] [PubMed]
- Song, S.O.; Jung, C.H.; Song, Y.D.; Park, C.Y.; Kwon, H.S.; Cha, B.S.; Park, J.Y.; Lee, K.U.; Ko, K.S.; Lee, B.W. Background and Data Configuration Process of a Nationwide Population-Based Study Using the Korean National Health Insurance System. Diabetes Metab. J. 2014, 38, 395–403. [Google Scholar] [CrossRef]
- Choi, E.K. Cardiovascular Research Using the Korean National Health Information Database. Korean Circ. J. 2020, 50, 754–772. [Google Scholar] [CrossRef]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment: International Association for the Study of Obesity; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- WHO Expert Consultation. Appropriate Body-Mass Index for Asian Populations and Its Implications for Policy and Intervention Strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Korean Society for the Study of Obesity. Guideline for the Management of Obesity 2018; Korean Society for the Study of Obesity: Seoul, Republic of Korea, 2018. [Google Scholar]
- Korean Statistical Information Service. Obesity Prevalence in Korean National Health and Nutrition Examination Survey of Korea Disease Control and Prevention Agency [Internet]; Statistics Korea: Daejeon, Republic of Korea, 2007–2015; Available online: https://kosis.kr/eng/ (accessed on 4 May 2025).
- Korean Statistical Information Service. Distribution of Body Mass by Age in Health Checkup Statistics of National Health Insurance Service [Internet]; Statistics Korea: Daejeon, Republic of Korea, 2010–2021; Available online: https://kosis.kr/eng/ (accessed on 4 May 2025).
- Kim, Y.H.; Han, K.; Son, J.W.; Lee, S.S.; Oh, S.W.; Kwon, H.S.; Shin, S.A.; Kim, Y.Y.; Lee, W.Y.; Yoo, S.J. Data Analytic Process of a Nationwide Population-Based Study on Obesity Using the National Health Information Database Presented by the National Health Insurance Service 2006–2015. J. Obes. Metab. Syndr. 2017, 26, 23–27. [Google Scholar] [CrossRef]
- Heymsfield, S.B.; Peterson, C.M.; Thomas, D.M.; Heo, M.; Schuna, J.M. Why Are There Race/Ethnic Differences in Adult Body Mass Index-Adiposity Relationships? A Quantitative Critical Review. Obes. Rev. 2016, 17, 262–275. [Google Scholar] [CrossRef]
- Okorodudu, D.O.; Jumean, M.F.; Montori, V.M.; Romero-Corral, A.; Somers, V.K.; Erwin, P.J.; Lopez-Jimenez, F. Diagnostic Performance of Body Mass Index to Identify Obesity as Defined by Body Adiposity: A Systematic Review and Meta-Analysis. Int. J. Obes. 2010, 34, 791–799. [Google Scholar] [CrossRef]
- Piché, M.E.; Poirier, P.; Lemieux, I.; Després, J.P. Overview of Epidemiology and Contribution of Obesity and Body Fat Distribution to Cardiovascular Disease: An Update. Prog. Cardiovasc. Dis. 2018, 61, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Rothman, K.J. BMI-Related Errors in the Measurement of Obesity. Int. J. Obes. 2008, 32, S56–S59. [Google Scholar] [CrossRef] [PubMed]
- Sorimachi, H.; Omote, K.; Omar, M.; Popovic, D.; Verbrugge, F.H.; Reddy, Y.N.V.; Lin, G.; Obokata, M.; Miles, J.M.; Jensen, M.D.; et al. Sex and Central Obesity in Heart Failure with Preserved Ejection Fraction. Eur. J. Heart Fail. 2022, 24, 1359–1370. [Google Scholar] [CrossRef] [PubMed]
- Sato, R.; von Haehling, S. Revisiting the Obesity Paradox in Heart Failure: What Is the Best Anthropometric Index to Gauge Obesity? Eur. Heart J. 2023, 44, 1154–1156. [Google Scholar] [CrossRef]
- Opoku, A.A.; Abushama, M.; Konje, J.C. Obesity and menopause. Best Pract. Res. Clin. Obstet. Gynaecol. 2023, 88, 102348. [Google Scholar] [CrossRef]



| Men | Women | Total | ||||
|---|---|---|---|---|---|---|
| N (Row %) | Column % | N (Row %) | Column % | N | Column % | |
| Underweight | 559 (45.0) | 3.3 | 683 (55.0) | 3.6 | 1242 | 3.5 |
| Normal | 4920 (47.1) | 29.2 | 5529 (52.9) | 29.1 | 10449 | 29.1 |
| Overweight | 4258 (49.2) | 25.2 | 4392 (50.8) | 23.1 | 8650 | 24.1 |
| Obesity | 6279 (47.7) | 37.2 | 6892 (52.3) | 36.3 | 13171 | 36.7 |
| Extreme obesity | 860 (36.5) | 5.1 | 1495 (63.5) | 7.9 | 2355 | 6.6 |
| Total | 16,876 (47.0) | 100.0 | 18,991 (53.0) | 100.0 | 35,869 | 100 |
| Total Patients | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Group | |||||||||
| Underweight | |||||||||
| N | 37 | 54 | 72 | 123 | 170 | 413 | 372 | 1241 | |
| Column % | 11.8 | 4.4 | 1.9 | 1.6 | 1.8 | 4.3 | 9.8 | ||
| Row % | 3.0 | 4.4 | 5.8 | 9.9 | 13.7 | 33.3 | 30.0 | 100.0 | |
| Normal | |||||||||
| N | 139 | 405 | 1016 | 1898 | 2346 | 3085 | 1547 | 10,436 | |
| Column % | 44.4 | 33.0 | 26.8 | 25.1 | 24.6 | 32.0 | 40.9 | ||
| Row % | 1.3 | 3.9 | 9.7 | 18.2 | 22.5 | 29.6 | 14.8 | 100.0 | |
| Overweight | |||||||||
| N | 53 | 230 | 791 | 1879 | 2451 | 2433 | 811 | 8648 | |
| Column % | 16.9 | 18.8 | 20.9 | 24.9 | 25.7 | 25.2 | 21.5 | ||
| Row % | 0.6 | 2.7 | 9.1 | 21.7 | 28.3 | 28.1 | 9.4 | 100.0 | |
| Obesity | |||||||||
| N | 51 | 374 | 1503 | 3083 | 3932 | 3273 | 952 | 13,168 | |
| Column % | 16.3 | 30.5 | 39.6 | 40.8 | 41.3 | 33.9 | 25.2 | ||
| Row % | 0.4 | 2.8 | 11.4 | 23.4 | 29.9 | 24.9 | 7.2 | 100.0 | |
| Extreme obesity | |||||||||
| N | 33 | 163 | 410 | 575 | 629 | 446 | 97 | 2353 | |
| Column % | 10.5 | 13.3 | 10.8 | 7.6 | 6.6 | 4.6 | 2.6 | ||
| Row % | 1.4 | 6.9 | 17.4 | 24.4 | 26.7 | 19.0 | 4.1 | 100.0 | |
| Total | 313 | 1226 | 3792 | 7558 | 9528 | 9650 | 3779 | 35,867 | |
| (Row %) | 0.9 | 3.4 | 10.6 | 21.1 | 26.6 | 26.9 | 10.5 | 100 | |
| Men | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Group | |||||||||
| Underweight | |||||||||
| N | 5 | 16 | 28 | 63 | 98 | 216 | 133 | 559 | |
| Column % | 3.5 | 2.3 | 1.3 | 1.6 | 2.2 | 5.3 | 9.5 | ||
| Row % | 0.9 | 2.9 | 5.0 | 11.3 | 17.5 | 38.6 | 23.8 | 100.0 | |
| Normal | |||||||||
| N | 40 | 147 | 425 | 910 | 1254 | 1508 | 632 | 4916 | |
| Column % | 28.4 | 20.7 | 19.9 | 23.4 | 27.5 | 37.3 | 45.3 | ||
| Row % | 0.8 | 3.0 | 8.6 | 18.5 | 25.5 | 30.7 | 12.9 | 100.0 | |
| Overweight | |||||||||
| N | 34 | 140 | 450 | 995 | 1241 | 1074 | 324 | 4258 | |
| Column % | 24.1 | 19.7 | 21.1 | 25.6 | 27.2 | 26.6 | 23.2 | ||
| Row % | 0.8 | 3.3 | 10.6 | 23.4 | 29.1 | 25.2 | 7.6 | 100.0 | |
| Obesity | |||||||||
| N | 41 | 282 | 1006 | 1711 | 1789 | 1154 | 293 | 6276 | |
| Column % | 29.1 | 39.8 | 47.2 | 44.0 | 39.3 | 28.6 | 21.0 | ||
| Row % | 0.7 | 4.5 | 16.0 | 27.3 | 28.5 | 18.4 | 4.7 | 100.0 | |
| Extreme obesity | |||||||||
| N | 21 | 124 | 224 | 213 | 175 | 90 | 12 | 859 | |
| Column % | 14.9 | 17.5 | 10.5 | 5.5 | 3.8 | 2.2 | 0.9 | ||
| Row % | 2.4 | 14.4 | 26.1 | 24.8 | 20.4 | 10.5 | 1.4 | 100.0 | |
| Total | 141 | 709 | 2133 | 3892 | 4557 | 4042 | 1394 | 16,868 | |
| Women | |||||||||
| Age | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| year | |||||||||
| Underweight | |||||||||
| N | 32 | 38 | 44 | 60 | 72 | 197 | 239 | 682 | |
| Column % | 18.6 | 7.4 | 2.7 | 1.6 | 1.4 | 3.5 | 10.0 | ||
| Row % | 4.7 | 5.6 | 6.5 | 8.8 | 10.6 | 28.9 | 35.0 | 100.0 | |
| Normal | |||||||||
| N | 99 | 258 | 591 | 988 | 1092 | 1577 | 915 | 5520 | |
| Column % | 57.6 | 49.9 | 35.6 | 27.0 | 22.0 | 28.1 | 38.4 | ||
| Row % | 1.8 | 4.7 | 10.7 | 17.9 | 19.8 | 28.6 | 16.6 | 100.0 | |
| Overweight | |||||||||
| N | 19 | 90 | 341 | 884 | 1210 | 1359 | 487 | 4390 | |
| Column % | 11.0 | 17.4 | 20.6 | 24.1 | 24.3 | 24.2 | 20.4 | ||
| Row % | 0.4 | 2.1 | 7.8 | 20.1 | 27.6 | 31.0 | 11.1 | 100.0 | |
| Obesity | |||||||||
| N | 10 | 92 | 497 | 1372 | 2143 | 2119 | 659 | 6892 | |
| Column % | 5.8 | 17.8 | 30.0 | 37.4 | 43.1 | 37.8 | 27.6 | ||
| Row % | 0.1 | 1.3 | 7.2 | 19.9 | 31.1 | 30.7 | 9.6 | 100.0 | |
| Extreme obesity | |||||||||
| N | 12 | 39 | 186 | 362 | 454 | 356 | 85 | 1494 | |
| Column % | 7.0 | 7.5 | 11.2 | 9.9 | 9.1 | 6.3 | 3.6 | ||
| Row % | 0.8 | 2.6 | 12.4 | 24.2 | 30.4 | 23.8 | 5.7 | 100.0 | |
| Total | 172 | 517 | 1659 | 3666 | 4971 | 5608 | 2385 | 18,978 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Park, G.; Pak, H.; Kim, H.; Jang, J.-Y.; Lee, H.; Park, J.-K.; Oh, S.-J.; Yoon, S.-J. Obesity Report: Distribution and Pattern by Age and Sex in Heart Failure Cohort over 10 Years in Korea. J. Cardiovasc. Dev. Dis. 2025, 12, 244. https://doi.org/10.3390/jcdd12070244
Kim J, Park G, Pak H, Kim H, Jang J-Y, Lee H, Park J-K, Oh S-J, Yoon S-J. Obesity Report: Distribution and Pattern by Age and Sex in Heart Failure Cohort over 10 Years in Korea. Journal of Cardiovascular Development and Disease. 2025; 12(7):244. https://doi.org/10.3390/jcdd12070244
Chicago/Turabian StyleKim, Joongmin, Geunhee Park, Haeyong Pak, Hyeongsoo Kim, Ji-Yong Jang, Hancheol Lee, Jong-Kwan Park, Seung-Jin Oh, and Se-Jung Yoon. 2025. "Obesity Report: Distribution and Pattern by Age and Sex in Heart Failure Cohort over 10 Years in Korea" Journal of Cardiovascular Development and Disease 12, no. 7: 244. https://doi.org/10.3390/jcdd12070244
APA StyleKim, J., Park, G., Pak, H., Kim, H., Jang, J.-Y., Lee, H., Park, J.-K., Oh, S.-J., & Yoon, S.-J. (2025). Obesity Report: Distribution and Pattern by Age and Sex in Heart Failure Cohort over 10 Years in Korea. Journal of Cardiovascular Development and Disease, 12(7), 244. https://doi.org/10.3390/jcdd12070244






