Impact of the Presence of Chronic Total Occlusions on the Survival of Patients Treated with Coronary Artery Bypass Grafting
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Population
2.2. Data Collection
2.3. Definition of Parameters
2.4. Definition of Primary and Secondary Outcomes
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Intraoperative Data
3.3. Early Clinical Outcomes
3.4. Follow-Up Data
4. Discussion
- (I)
- The presence of CTO was a predictor of 3-, 5-, and 10-year mortality before and after statistical adjustments. However, this effect was weaker than other investigated factors.
- (II)
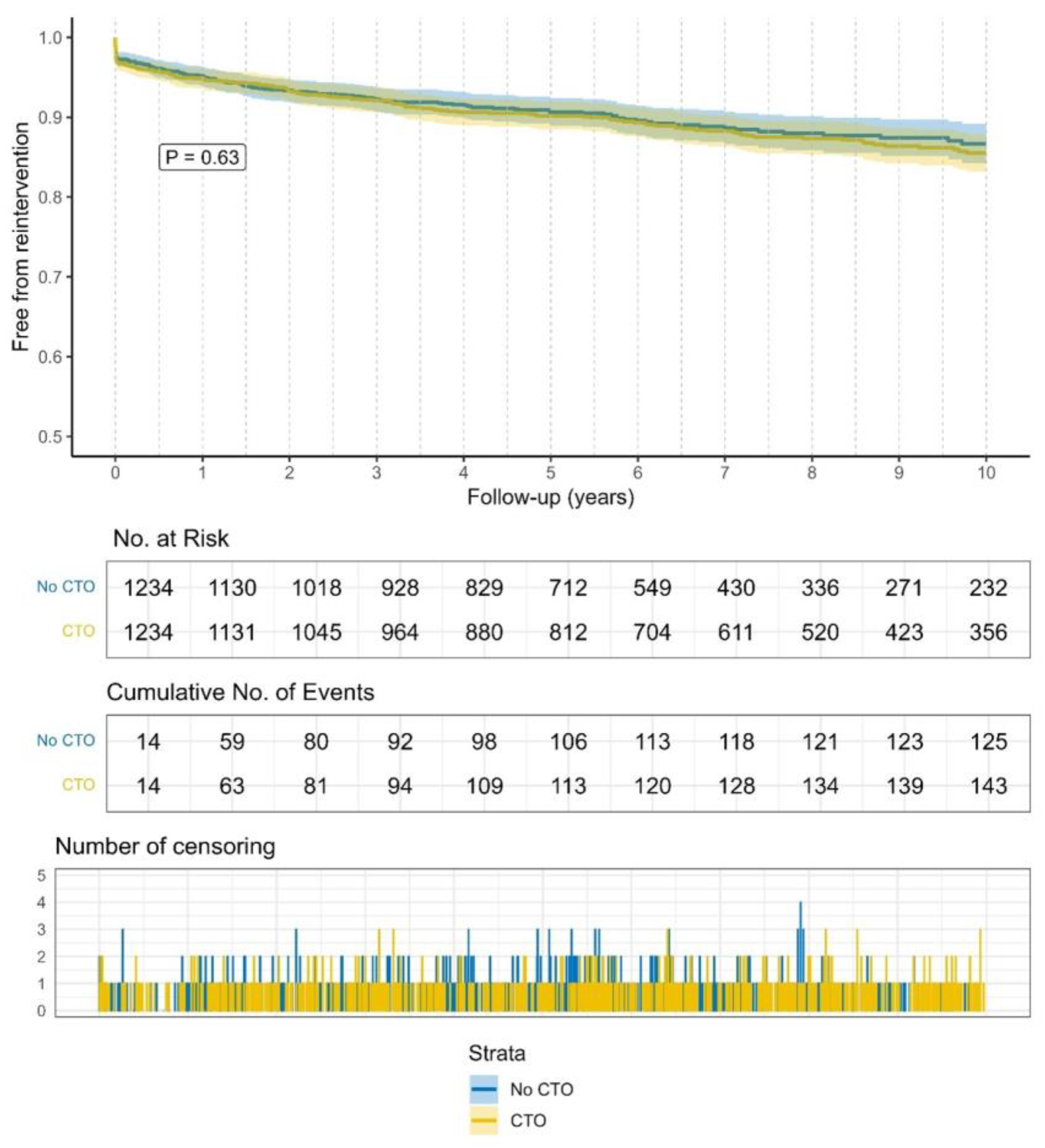
- Coronary reintervention rates remained low, even after 10 years, indicating a durable treatment.
- (III)
- The treatment of CTO with CABG revealed very favorable long-term outcomes.
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Christofferson, R.D.; Lehmann, K.G.; Martin, G.V.; Every, N.; Caldwell, J.H.; Kapadia, S.R. Effect of chronic total coronary occlusion on treatment strategy. Am. J. Cardiol. 2005, 95, 1088–1091. [Google Scholar] [CrossRef] [PubMed]
- Fagu, A.; Berger, T.; Pingpoh, C.; Kondov, S.; Kreibich, M.; Minners, J.; Czerny, M.; Siepe, M. In-Hospital Outcomes Following Surgical Revascularization of Chronic Total Coronary Occlusions. Medicina 2023, 59, 1967. [Google Scholar] [CrossRef] [PubMed]
- Galassi, A.R.; Werner, G.S.; Boukhris, M.; Azzalini, L.; Mashayekhi, K.; Carlino, M.; Avran, A.; Konstantinidis, N.V.; Grancini, L.; Bryniarski, L.; et al. Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO Club. EuroIntervention 2019, 15, 198–208. [Google Scholar] [CrossRef]
- Fefer, P.; Knudtson, M.L.; Cheema, A.N.; Galbraith, P.D.; Osherov, A.B.; Yalonetsky, S.; Gannot, S.; Samuel, M.; Weisbrod, M.; Bierstone, D.; et al. Current perspectives on coronary chronic total occlusions: The Canadian multicenter chronic total occlusions registry. J. Am. Coll. Cardiol. 2012, 59, 991–997. [Google Scholar] [CrossRef] [PubMed]
- Gold, D.A.; Sandesara, P.B.; Jain, V.; Gold, M.E.; Vatsa, N.; Desai, S.R.; Hassan, M.E.; Yuan, C.; Ko, Y.-A.; Ejaz, K.; et al. Long-Term Outcomes in Patients with Chronic Total Occlusion. Am. J. Cardiol. 2024, 214, 59–65. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics-2022 Update: A Report from the American Heart Association. Circulation 2022, 145, E153–E639. [Google Scholar]
- Serruys, P.W.; Morice, M.-C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Ståhle, E.; Feldman, T.E.; Van Den Brand, M.; Bass, E.J.; et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef]
- Irving, J. CTO Pathophysiology: How Does this Affect Management? Curr. Cardiol. Rev. 2014, 10, 99–107. [Google Scholar] [CrossRef]
- Claessen, B.E.; Dangas, G.D.; Weisz, G.; Witzenbichler, B.; Guagliumi, G.; Möckel, M.; Brener, S.J.; Xu, K.; Henriques, J.P.; Mehran, R.; et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur. Heart J. 2012, 33, 768–775. [Google Scholar] [CrossRef]
- Råmunddal, T.; Hoebers, L.P.; Henriques, J.P.; Dworeck, C.; Angerås, O.; Odenstedt, J.; Ioanes, D.; Olivecrona, G.; Harnek, J.; Jensen, U.; et al. Chronic total occlusions in Sweden–A report from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). PLoS ONE 2014, 9, e103850. [Google Scholar] [CrossRef]
- Fefer, P.; Gannot, S.; Kochkina, K.; Maor, E.; Matetzky, S.; Raanani, E.; Guetta, V.; Segev, A. Impact of coronary chronic total occlusions on long-term mortality in patients undergoing coronary artery bypass grafting. Interact. Cardiovasc. Thorac. Surg. 2014, 18, 713–716. [Google Scholar] [CrossRef] [PubMed]
- Roth, C.; Goliasch, G.; Aschauer, S.; Gangl, C.; Ayoub, M.; Distelmaier, K.; Frey, B.; Lang, I.M.; Berger, R.; Mashayekhi, K.; et al. Impact of treatment strategies on long-term outcome of CTO patients. Eur. J. Intern. Med. 2020, 77, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Sianos, G.; Werner, G.S.; Galassi, A.R.; Papafaklis, M.I.; Escaned, J.; Hildick-Smith, D.; Christiansen, E.H.; Gershlick, A.; Carlino, M.; Karlas, A.; et al. Recanalisation of Chronic Total coronary Occlusions: 2012 Consensus document from the EuroCTO club. EuroIntervention 2012, 8, 139–145. [Google Scholar] [CrossRef]
- Gaudino, M.; Alexander, J.H.; Bakaeen, F.G.; Ballman, K.; Barili, F.; Calafiore, A.M.; Davierwala, P.; Goldman, S.; Kappetein, P.; Lorusso, R.; et al. Randomized comparison of the clinical outcome of single versus multiple arterial grafts: The ROMA trial-rationale and study protocol. Eur. J. Cardiothorac. Surg. 2017, 52, 1031–1040. [Google Scholar] [CrossRef]
- Lawton, J.S.; Tamis-Holland, J.E.; Bangalore, S.; Bates, E.R.; Beckie, T.M.; Bischoff, J.M.; Bittl, J.A.; Cohen, M.G.; DiMaio, J.M.; Don, C.W.; et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e4–e17. [Google Scholar] [CrossRef]
- Sousa-Uva, M.; Neumann, F.-J.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. J. Cardio-Thorac. Surg. 2019, 55, 4–90. [Google Scholar] [CrossRef]
- Stone, G.W.; Ali, Z.A.; O’bRien, S.M.; Rhodes, G.; Genereux, P.; Bangalore, S.; Mavromatis, K.; Horst, J.; Dressler, O.; Poh, K.K.; et al. Impact of Complete Revascularization in the ISCHEMIA Trial. J. Am. Coll. Cardiol. 2023, 82, 1175–1188. [Google Scholar] [CrossRef]
- Azzalini, L.; Karmpaliotis, D.; Santiago, R.; Mashayekhi, K.; Di Mario, C.; Rinfret, S.; Nicholson, W.J.; Carlino, M.; Yamane, M.; Tsuchikane, E.; et al. Contemporary Issues in Chronic Total Occlusion Percutaneous Coronary Intervention. Cardiovasc. Interv. 2022, 15, 1–21. [Google Scholar] [CrossRef]
- Lee, S.W.; Lee, P.H.; Ahn, J.M.; Park, D.W.; Yun, S.C.; Han, S.; Kang, H.; Kang, S.J.; Kim, Y.H.; Lee, C.W.; et al. Randomized Trial Evaluating Percutaneous Coronary Intervention for the Treatment of Chronic Total Occlusion: The DECISION-CTO Trial. Circulation 2019, 139, 1674–1683. [Google Scholar] [CrossRef]
- Vadalà, G.; Galassi, A.R.; Werner, G.S.; Sianos, G.; Boudou, N.; Garbo, R.; Maniscalco, L.; Bufe, A.; Avran, A.; Gasparini, G.L.; et al. Contemporary outcomes of chronic total occlusion percutaneous coronary intervention in Europe: The ERCTO registry. EuroIntervention 2024, 20, E185–E197. [Google Scholar] [CrossRef]
- Kletzer, J.; Fagu, A.; Eschenhagen, M.; Micek, L.; Siepe, M.; Czerny, M.; Kreibich, M.; Berger, T. Safety and efficiency of trainees performing bilateral internal thoracic artery coronary bypass grafting using the T-graft technique. Eur. J. Cardio-Thorac. Surg. 2024, 67, ezae419. [Google Scholar] [CrossRef] [PubMed]
- Farooq, V.; Serruys, P.W.; Garcia-Garcia, H.M.; Zhang, Y.; Bourantas, C.V.; Holmes, D.R.; Mack, M.; Feldman, T.; Morice, M.C.; Ståhle, E.; et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: The SYNTAX (Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J. Am. Coll. Cardiol. 2013, 61, 282–294. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Guan, C.; Wu, F.; Xie, L.; Zou, T.; Shi, Y.; Chen, S.; He, L.; Xu, B.; Zheng, Z. Coronary Artery Bypass Grafting and Percutaneous Coronary Intervention in Patients with Chronic Total Occlusion and Multivessel Disease. Circ. Cardiovasc. Interv. 2022, 15, E011312. [Google Scholar] [CrossRef] [PubMed]
- Kirov, H.; Fischer, J.; Caldonazo, T.; Tasoudis, P.; Runkel, A.; Soletti, G.J.; Cancelli, G.; Dell’AQuila, M.; Mukharyamov, M.; Doenst, T. Coronary Artery Bypass Grafting versus Percutaneous Coronary Intervention in Patients with Chronic Total Occlusion. Thorac. Cardiovasc. Surg. 2023. Online ahead of print. [Google Scholar] [CrossRef]

| CTO/No CTO (Matched) | ||||
|---|---|---|---|---|
| Characteristics | Overall, N = 3424 * | CTO, N = 1232 * | No CTO, N = 1232 * | p-Value ** |
| Matched | Matched | |||
| Sex (female) | 532 (15%) | 172 (14%) | 186 (15%) | 0.4 |
| Age (years) | 68.0 (62.0, 74.0) | 69.0 (63.0, 74.0) | 69.0 (63.0, 74.0) | >0.9 |
| BMI (kg/m2) | 27.4 (25.1, 30.1) | 27.7 (25.4, 30.6) | 27.7 (25.4, 30.5) | 0.5 |
| Diabetes | 1082 (32%) | 390 (32%) | 394 (32%) | 0.9 |
| Insulin dependent Diabetes | 386 (10%) | 125 (10%) | 125 (10%) | >0.9 |
| Dyslipidemia | 2728 (80%) | 1027 (83%) | 1027 (83%) | >0.9 |
| Hypertension | 2844 (83%) | 1053 (85%) | 1046 (85%) | 0.7 |
| Arrhythmia | 294 (8.6%) | 103 (8.4%) | 110 (8.9%) | 0.6 |
| Smoking | 1172 (37%) | 469 (38%) | 436 (35%) | 0.2 |
| PAD | 447 (15%) | 167 (14%) | 169 (14%) | >0.9 |
| COPD | 349 (10%) | 122 (9.9%) | 113 (9.2%) | 0.5 |
| History of MI | 1149 (34%) | 397 (32%) | 390 (32%) | 0.8 |
| History of stroke | 209 (6.1%) | 80 (6.5%) | 62 (5.0%) | 0.12 |
| Malignancy | 60 (1.9%) | 22 (1.8%) | 23 (1.9%) | 0.9 |
| NYHA | 0.4 | |||
| 1 | 341 (11%) | 154 (13%) | 164 (13%) | |
| 2 | 1449 (47%) | 595 (48%) | 613 (50%) | |
| 3 | 1213 (39%) | 470 (38%) | 448 (36%) | |
| 4 | 81 (2.6%) | 13 (1.1%) | 7 (0.6%) | |
| Chronic renal failure | 97 (2.9%) | 18 (1.5%) | 14 (1.1%) | 0.5 |
| EuroScore II | 1.3 (0.9, 2.0) | 1.2 (0.9, 1.8) | 1.2 (0.9, 1.8) | 0.2 |
| Preop. LVEF < 30% | 88 (2.8%) | 5 (0.4%) | 5 (0.4%) | >0.9 |
| Significantly stenosed vessels | >0.9 | |||
| 1 | 24 (1%) | 1 (<0.1%) | 1 (<0.1%) | |
| 2 | 283 (8%) | 53 (4%) | 53 (4%) | |
| 3 | 3108 (91%) | 1178 (96%) | 1178 (96%) | |
| CSS Classification | 0.002 | |||
| CCS 0 | 258 (8.4%) | 115 (9.3%) | 90 (7.3%) | |
| CCS 1 | 114 (3.7%) | 51 (4.1%) | 40 (3.3%) | |
| CCS 2 | 816 (27%) | 359 (29%) | 314 (26%) | |
| CCS 3 | 1244 (41%) | 514 (42%) | 531 (43%) | |
| CCS 4 | 638 (21%) | 192 (16%) | 255 (21%) | |
| CTO Distribution | Overall, N = 3424 | CTO, N = 1232 |
|---|---|---|
| Matched | ||
| CTO LAD | 439 (25%) | 285 (23%) |
| CTO RCA | 1174 (67%) | 826 (67%) |
| CTO LCX | 584 (33%) | 403 (33%) |
| Revascularization of CTO LAD | 408 (92%) | 265 (93%) |
| Revascularization of CTO RCA | 1001 (85%) | 702 (85%) |
| Revascularization of CTO LCX | 464 (79%) | 315 (75%) |
| CTO/No CTO (Matched) | ||||
|---|---|---|---|---|
| Characteristic | Overall, N = 3424 * | CTO, N = 1232 * | No CTO, N = 1232 * | p-Value ** |
| 30-day mortality | 59 (1.7%) | 18 (1.5%) | 16 (1.3%) | 0.7 |
| Coronary reintervention after 30 days | 95 (2.8%) | 37 (3.0%) | 35 (2.9%) | 0.8 |
| Re-CABG after 30 days | 4 (0.1%) | 1 (<0.1%) | 1 (<0.1%) | >0.9 |
| PCI after 30 days | 95 (2.8%) | 37 (3.0%) | 36 (2.9%) | >0.9 |
| Hospital stay (days) | 14.0 (11.0, 17.0) | 14.0 (11.0, 17.0) | 13.0 (11.0, 16.0) | <0.001 |
| Length of ICU stay (days) | 1.0 (0.9, 1.9) | 0.9 (0.9, 1.8) | 0.9 (0.8, 1.6) | 0.10 |
| Pacemaker implantation after 30 days | 49 (1.4%) | 18 (1.5%) | 17 (1.4%) | 0.9 |
| Postoperative Dialysis | 113 (3.3%) | 26 (2.1%) | 29 (2.4%) | 0.7 |
| Deep Sternal Infection | 109 (3.3%) | 45 (3.7%) | 31 (2.5%) | 0.10 |
| Postoperative stroke | 73 (2.1%) | 27 (2.2%) | 21 (1.7%) | 0.4 |
| Postoperative AF | 643 (19%) | 252 (20%) | 207 (17%) | 0.020 |
| CTO/No CTO (Matched) | ||||
|---|---|---|---|---|
| Characteristic | Overall, N = 3424 * | CTO, N = 1232 * | No CTO, N = 1232 * | p-Value ** |
| 3-year mortality | 277 (8.1%) | 94 (7.6%) | 67 (5.4%) | 0.028 |
| 5-year mortality | 417 (12%) | 153 (12%) | 100 (8.1%) | <0.001 |
| 10-year mortality | 778 (23%) | 302 (24%) | 187 (15%) | <0.001 |
| Coronary reinterventions after 3 years | 228 (6.7%) | 88 (7.2%) | 86 (7.1%) | >0.9 |
| Coronary reinterventions after 5 years | 274 (8.1%) | 106 (8.7%) | 97 (8.0%) | 0.5 |
| Coronary reinterventions after 10 years | 336 (9.9%) | 143 (12%) | 125 (10%) | 0.2 |
| Re CABG after 3 years | 5 (0.1%) | 2 (0.2%) | 1 (<0.1%) | >0.9 |
| Re CABG after 5 years | 5 (0.1%) | 2 (0.2%) | 1 (<0.1%) | >0.9 |
| Re CABG after 10 years | 5 (0.1%) | 2 (0.2%) | 1 (<0.1%) | >0.9 |
| PCI after 3 years | 228 (6.7%) | 88 (7.1%) | 91 (7.4%) | 0.8 |
| PCI after 5 years | 274 (8.1%) | 107 (8.7%) | 102 (8.3%) | 0.7 |
| PCI after 10 years | 335 (9.9%) | 138 (11%) | 116 (9.4%) | 0.14 |
| Postoperative coronary angiography | 616 (18%) | 253 (21%) | 185 (15%) | <0.001 |
| Multivariable Cox Regression | HR | 95%CI | p-Value |
|---|---|---|---|
| CTO | 1.220 | 1.047–1.420 | 0.010 |
| Age | 1.055 | 1.044–1.066 | <0.001 |
| Hypertension | 1.159 | 0.915–1.468 | 0.218 |
| History of smoking | 1.488 | 1.270–1.743 | <0.001 |
| History of malignancy | 1.647 | 0.998–2.716 | 0.050 |
| NYHA IV | 1.936 | 1.051–3.567 | 0.034 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fagu, A.; Kletzer, J.; Ernst, F.M.; Micek, L.; Kondov, S.; Kreibich, M.; Pingpoh, C.; Siepe, M.; Czerny, M.; Berger, T. Impact of the Presence of Chronic Total Occlusions on the Survival of Patients Treated with Coronary Artery Bypass Grafting. J. Cardiovasc. Dev. Dis. 2025, 12, 243. https://doi.org/10.3390/jcdd12070243
Fagu A, Kletzer J, Ernst FM, Micek L, Kondov S, Kreibich M, Pingpoh C, Siepe M, Czerny M, Berger T. Impact of the Presence of Chronic Total Occlusions on the Survival of Patients Treated with Coronary Artery Bypass Grafting. Journal of Cardiovascular Development and Disease. 2025; 12(7):243. https://doi.org/10.3390/jcdd12070243
Chicago/Turabian StyleFagu, Albi, Joseph Kletzer, Franziska Marie Ernst, Laurin Micek, Stoyan Kondov, Maximilian Kreibich, Clarence Pingpoh, Matthias Siepe, Martin Czerny, and Tim Berger. 2025. "Impact of the Presence of Chronic Total Occlusions on the Survival of Patients Treated with Coronary Artery Bypass Grafting" Journal of Cardiovascular Development and Disease 12, no. 7: 243. https://doi.org/10.3390/jcdd12070243
APA StyleFagu, A., Kletzer, J., Ernst, F. M., Micek, L., Kondov, S., Kreibich, M., Pingpoh, C., Siepe, M., Czerny, M., & Berger, T. (2025). Impact of the Presence of Chronic Total Occlusions on the Survival of Patients Treated with Coronary Artery Bypass Grafting. Journal of Cardiovascular Development and Disease, 12(7), 243. https://doi.org/10.3390/jcdd12070243






