Adherence of Older Cardiac Patients to a Home-Based Cardiac Rehabilitation Program
Abstract
1. Introduction
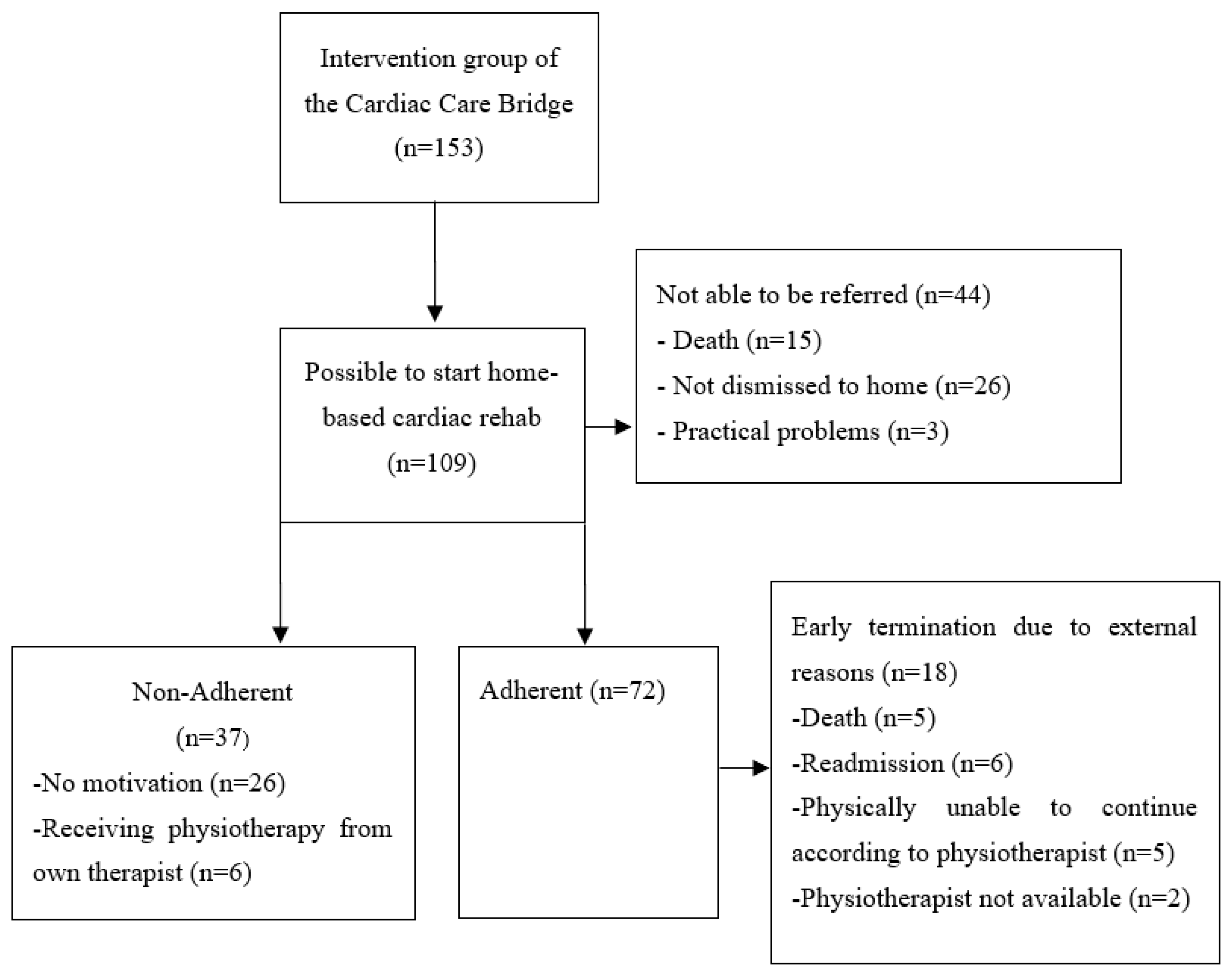
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Intervention and Home-Based Cardiac Rehabilitation
2.4. Measures
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schopfer, D.W.; Forman, D.E. Cardiac Rehabilitation in Older Adults. Can. J. Cardiol. 2016, 32, 1088–1096. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.M.; King-Shier, K.M.; Duncan, A.; Spaling, M.; Stone, J.A.; Jaglal, S.; Angus, J. Factors Influencing Referral to Cardiac Rehabilitation and Secondary Prevention Programs: A Systematic Review. Eur. J. Prev. Cardiol. 2013, 20, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Dibben, G.; Faulkner, J.; Oldridge, N.; Rees, K.; Thompson, D.R.; Zwisler, A.D.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease. Cochrane Database Syst. Rev. 2021, 11, CD001800. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.M.; Hernandez, A.F.; Bittner, V.; Cannon, C.P.; Ellrodt, G.; Liang, L.; Peterson, E.D.; Piña, I.L.; Safford, M.M.; Fonarow, G.C. Predictors of Cardiac Rehabilitation Referral in Coronary Artery Disease Patients. Findings from the American Heart Association’s Get with The Guidelines Program. J. Am. Coll. Cardiol. 2009, 54, 515–521. [Google Scholar] [CrossRef]
- Dalal, H.M. Cardiac Rehabilitation. BMJ 2015, 351, h5000. [Google Scholar] [CrossRef]
- Nusbickel, A.J.; Randall, M.H.; Plasschaert, J.M.; Brown, M.P.; Anderson, R.D.; Arnaoutakis, G.J.; Massoomi, M.R.; Shah, K.B.; Jeng, E.I.; Beaver, T.M.; et al. Cardiac Rehabilitation Referral After Transcatheter Aortic Valve Replacement. Crit. Pathw. Cardiol. 2022, 21, 162–164. [Google Scholar] [CrossRef]
- Anderson, L.; Ga, S.; Rj, N.; Dalal, H.; Sg, D.; Jolly, K.; Cowie, A.; Zawada, A.; Rs, T.; Anderson, L.; et al. Home-Based versus Centre-Based Cardiac Rehabilitation (Review). Cochrane Database Syst. Rev. 2017, 6, CD007130. [Google Scholar] [CrossRef]
- Neubeck, L.; Freedman, S.B.; Clark, A.M.; Briffa, T.; Bauman, A.; Redfern, J. Participating in Cardiac Rehabilitation: A Systematic Review and Meta-Synthesis of Qualitative Data. Eur. J. Prev. Cardiol. 2012, 19, 494–503. [Google Scholar] [CrossRef]
- Kumar, K.R.; Pina, I.L. Cardiac Rehabilitation in Older Adults: New Options. Clin. Cardiol. 2020, 43, 163–170. [Google Scholar] [CrossRef]
- Jepma, P.; Verweij, L.; Buurman, B.M.; Terbraak, M.S.; Daliri, S.; Latour, C.H.M.; ter Riet, G.; Karapinar-Çarkit, F.; Dekker, J.; Klunder, J.L.; et al. The Nurse-Coordinated Cardiac Care Bridge Transitional Care Programme: A Randomised Clinical Trial. Age Ageing 2021, 50, 2105–2115. [Google Scholar] [CrossRef]
- Verweij, L.; Jepma, P.; Buurman, B.M.; Latour, C.H.M.; Engelbert, R.H.H.; ter Riet, G.; Karapinar-Çarkit, F.; Daliri, S.; Peters, R.J.G.; Scholte Op Reimer, W.J.M. The Cardiac Care Bridge Program: Design of a Randomized Trial of Nurse-Coordinated Transitional Care in Older Hospitalized Cardiac Patients at High Risk of Readmission and Mortality. BMC Health Serv. Res. 2018, 18, 508. [Google Scholar] [CrossRef] [PubMed]
- Dutch Society for Cardiology. Multidisciplinary Guideline for Cardiac Rehabilitation; Dutch Society for Cardiology: Utrecht, The Netherlands, 2011. [Google Scholar]
- Kruizenga, H.M.; Seidell, J.C.; de Vet, H.C.W.; Wierdsma, N.J.; van Bokhorst-de van der Schueren, M.A.E. Development and Validation of a Hospital Screening Tool for Malnutrition: The Short Nutritional Assessment Questionnaire (SNAQ©). Clin. Nutr. 2005, 24, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State” a Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic in Longitudinal Studies: Development. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Friedman, B.; Heisel, M.J.; Delavan, R.L. Psychometric Properties of the 15-Item Geriatric Depression Scale in Functionally Impaired, Cognitively Intact, Community-Dwelling Elderly Primary Care Patients. J. Am. Geriatr. Soc. 2005, 53, 1570–1576. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snalth, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association With Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Holman, R.; Weisscher, N.; Glas, C.A.W.; Dijkgraaf, M.G.W.; Vermeulen, M.; de Haan, R.J.; Lindeboom, R. The Academic Medical Center Linear Disability Score (ALDS) Item Bank: Item Response Theory Analysis in a Mixed Patient Population. Health Qual. Life Outcomes 2005, 3, 83. [Google Scholar] [CrossRef]
- Trutschnigg, B.; Kilgour, R.D.; Reinglas, J.; Rosenthall, L.; Hornby, L.; Morais, J.A.; Vigano, A. Precision and Reliability of Strength (Jamar vs. Biodex Handgrip) and Body Composition (Dual-Energy X-ray Absorptiometry vs. Bioimpedance Analysis) Measurements in Advanced Cancer Patients. Appl. Physiol. Nutr. Metab. 2008, 33, 1232–1239. [Google Scholar] [CrossRef]
- Luppa, M.; Luck, T.; Weyerer, S.; König, H.H.; Brähler, E.; Riedel-Heller, S.G. Prediction of Institutionalization in the Elderly. A Systematic Review. Age Ageing 2009, 39, 31–38. [Google Scholar] [CrossRef]
- Hajek, A.; Brettschneider, C.; Lange, C.; Posselt, T.; Wiese, B.; Steinmann, S.; Weyerer, S.; Werle, J.; Pentzek, M.; Fuchs, A.; et al. Longitudinal Predictors of Institutionalization in Old Age. PLoS ONE 2015, 10, e0144203. [Google Scholar] [CrossRef]
- Moreh, E.; Jacobs, J.M.; Stessman, J. Fatigue, Function, and Mortality in Older Adults. J. Gerontol.-Ser. A Biol. Sci. Med. Sci. 2010, 65, 887–895. [Google Scholar] [CrossRef] [PubMed]
- Griffin, B.; Loh, V.; Hesketh, B. A Mental Model of Factors Associated with Subjective Life Expectancy. Soc. Sci. Med. 2013, 82, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Jepma, P.; Snaterse, M.; du Puy, S.; Peters, R.J.G.; op Reimer, W.J.M.S. Older Patients’ Perspectives toward Lifestyle-Related Secondary Cardiovascular Prevention after a Hospital Admission—A Qualitative Study. Age Ageing 2021, 50, 936–943. [Google Scholar] [CrossRef]
- English, K.L.; Paddon-Jones, D. Protecting Muscle Mass and Function in Older Adults during Bed Rest. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 34–39. [Google Scholar] [CrossRef]
- de Liao, C.; Tsauo, J.Y.; Wu, Y.T.; Cheng, C.P.; Chen, H.C.; Huang, Y.C.; Chen, H.C.; Liou, T.H. Effects of Protein Supplementation Combined with Resistance Exercise on Body Composition and Physical Function in Older Adults: A Systematic Review and Meta-Analysis. Nutrients 2018, 10, 1916. [Google Scholar] [CrossRef] [PubMed]
- Deutz, N.E.P.; Bauer, J.M.; Barazzoni, R.; Biolo, G.; Boirie, Y.; Bosy-Westphal, A.; Cederholm, T.; Cruz-Jentoft, A.; Krznariç, Z.; Nair, K.S.; et al. Protein Intake and Exercise for Optimal Muscle Function with Aging: Recommendations from the ESPEN Expert Group. Clin. Nutr. 2014, 33, 929–936. [Google Scholar] [CrossRef]
- Boreskie, K.F.; Hay, J.L.; Kehler, D.S.; Johnston, N.M.; Rose, A.V.; Oldfield, C.J.; Kumar, K.; Toleva, O.; Arora, R.C.; Duhamel, T.A. Prehabilitation: The Right Medicine for Older Frail Adults Anticipating Transcatheter Aortic Valve Replacement, Coronary Artery Bypass Graft, and Other Cardiovascular Care. Clin. Geriatr. Med. 2019, 35, 571–585. [Google Scholar] [CrossRef]
- Bierbauer, W.; Scholz, U.; Bermudez, T.; Debeer, D.; Coch, M.; Fleisch-silvestri, R.; Nacht, C.; Tschanz, H.; Schmid, J. Improvements in Exercise Capacity of Older Adults during Cardiac Rehabilitation. Eur. J. Prev. Cardiol. 2020, 27, 1747–1755. [Google Scholar] [CrossRef]
| Unable to Initiate (n = 44) | Able to Initiate (n = 109) | p | Able to Initiate (n = 109) | ||||
|---|---|---|---|---|---|---|---|
| Non-Adherence (n = 37) | Adherence (n = 72) | p | |||||
| Demographics | |||||||
| Age | Years, Mean (SD) | 83 (6) | 82 (6) | 0.91 | 84 (6) | 82 (6) | 0.05 * |
| Sex | Male | 45 | 46 | >0.99 | 46 | 46 | >0.99 |
| Education | Primary Education | 39 | 45 | 0.52 | 40 | 47 | 0.56 |
| Secondary Education | 41 | 31 | 38 | 28 | |||
| Higher Education | 20 | 24 | 22 | 25 | |||
| Living arrangement | Living together | 41 | 44 | 0.86 | 38 | 47 | 0.46 |
| Socioeconomic status | Low (<1 SD) | 23 | 17 | 0.52 | 14 | 20 | 0.56 |
| Intermediate | 59 | 65 | 67 | 62 | |||
| High (>1 SD) | 18 | 18 | 19 | 18 | |||
| Body mass index | kg/m2, Mean (SD) | 27 (6) | 27 (6) | 0.73 | 27 (6) | 27 (6) | 0.84 |
| Current smoker | 7 | 12 | 0.51 | 11 | 11 | >0.99 | |
| Medical | |||||||
| Hospitalisation | Acute | 98 | 88 | 0.12 | 92 | 86 | 0.57 |
| Diagnosis | Heart failure | 68 | 51 | 0.25 | 46 | 54 | 0.54 |
| Rhythm or conduction disorder | 16 | 18 | 16 | 19 | |||
| Acute coronary syndrome | 9 | 14 | 22 | 10 | |||
| Valve deficit | 7 | 10 | 11 | 10 | |||
| Other | 0 | 6 | 5 | 7 | |||
| Previous Hospital admission | <6 months before index event | 36 | 46 | 0.37 | 43 | 47 | 0.85 |
| Malnutrition | SNAQ | 48 | 30 | 0.06 | 32 | 29 | 0.90 |
| Fall risk | fall < 6 months | 43 | 44 | >0.99 | 35 | 49 | 0.26 |
| Fear of falling | NRS > 4 | 52 | 37 | 0.11 | 35 | 38 | 0.97 |
| Fatigue | NRS, Median (IQR] | 6 (4–7] | 5 (3–6] | 0.03 * | 5 (3–6] | 5 (4–7] | 0.53 |
| Comorbidities | Charlson, Median (IQR] | 3 (1–4] | 2 (1–4] | 0.63 | 2 (1–3] | 3 (1–4] | 0.37 |
| Dyspnoea | Self-reported | 86 | 80 | 0.47 | 70 | 85 | 0.13 |
| Dizziness | Self-reported | 41 | 43 | 0.94 | 32 | 49 | 0.16 |
| Polypharmacy | >5 | 82 | 82 | 0.87 | 83 | 82 | 0.76 |
| Psychosocial | |||||||
| Cognitive impairment | MMSE 15–23 | 6 | 5 | 0.28 | 5 | 5 | 0.33 |
| Depression | GDS, Median (IQR] | 3 (2–6] | 3 (2–4] | 0.03 * | 3 (2–3] | 3 (2–4] | 0.24 |
| Anxiety | HADS-A, Median (IQR] | 4 (2–7] | 3 (1–5] | 0.18 | 2 (1–4] | 3 (2–5] | 0.32 |
| Physical | |||||||
| Physical performance | SPPB, Median (IQR] | 3 (1–5] | 5 (3–7] | 0.01 * | 5 (3–8] | 5 (3–7] | 0.36 |
| ADL-functioning | ALDS-score (0–100) † | 64 (54–78] | 75 (60–86] | <0.01 * | 72 (64–83] | 78 (60–87] | 0.77 |
| Handgrip strength | Male (kg), Mean (SD) | 20 (11) | 27 (10) | 0.02 * | 33 (8) | 25 (11) | 0.01 * |
| Female (kg), Mean (SD) | 16 (5) | 17 (6) | 0.40 | 16 (5) | 18 (6) | 0.11 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Erck, D.; Terbraak, M.; Dolman, C.D.; Weijs, P.J.M.; Henriques, J.P.; Delewi, R.; Verweij, L.; Jepma, P.; Scholte op Reimer, W.J.M.; Schoufour, J.D. Adherence of Older Cardiac Patients to a Home-Based Cardiac Rehabilitation Program. Geriatrics 2023, 8, 53. https://doi.org/10.3390/geriatrics8030053
van Erck D, Terbraak M, Dolman CD, Weijs PJM, Henriques JP, Delewi R, Verweij L, Jepma P, Scholte op Reimer WJM, Schoufour JD. Adherence of Older Cardiac Patients to a Home-Based Cardiac Rehabilitation Program. Geriatrics. 2023; 8(3):53. https://doi.org/10.3390/geriatrics8030053
Chicago/Turabian Stylevan Erck, Dennis, Michel Terbraak, Christine D. Dolman, Peter J. M. Weijs, José P. Henriques, Ronak Delewi, Lotte Verweij, Patricia Jepma, Wilma J. M. Scholte op Reimer, and Josje D. Schoufour. 2023. "Adherence of Older Cardiac Patients to a Home-Based Cardiac Rehabilitation Program" Geriatrics 8, no. 3: 53. https://doi.org/10.3390/geriatrics8030053
APA Stylevan Erck, D., Terbraak, M., Dolman, C. D., Weijs, P. J. M., Henriques, J. P., Delewi, R., Verweij, L., Jepma, P., Scholte op Reimer, W. J. M., & Schoufour, J. D. (2023). Adherence of Older Cardiac Patients to a Home-Based Cardiac Rehabilitation Program. Geriatrics, 8(3), 53. https://doi.org/10.3390/geriatrics8030053







