Abstract
Background: Physical restraints are frequently used in acute care hospitals. Their application is associated with negative outcomes, while their intended preventive effect is debated. Objectives: To determine the prevalence of physical restraints and associated outcomes on medical wards in a tertiary care hospital. Methods: Retrospective cohort study (January 2018 to December 2021). We included all adult medical in-patients and excluded patients with admission to the intensive care unit, short stays (length of stay (LOS) < 48 h), and patients declining informed consent. Results: Of 11,979 admissions, the prevalence of patients with at least one restraint was 6.4% (n = 772). Sensor mats were used most frequently (73.0%, n = 666), followed by blanket restrictions (14.5%, n = 132), bedrails (8.8%, n = 80) and belts (3.7%, n = 34). On average, restraints were applied 19 h (standard deviation (SD) ± 161) before a fall. Average restraint duration was 42 h (SD ± 57). Patients with a restraint had longer LOS 8 days (IQR 5–14) vs. 5 days (IQR 3–9). Median nurses’ time expenditure was 309 h (IQR 242–402) vs. 182 h (IQR 136–243) for non-restrained patients. Patients with restraints fell more often (22.5% vs. 2.7%) and were more likely to die (13.3% vs. 5.1%). These differences persisted after adjusting a regression model for important clinical confounders. We saw a decline in the duration of restraints over the years, but no variation between wards. Conclusion: Approximately 6% of medical patients, mostly older and severely ill, were affected by restraint use. For the first time, we report data over 4 years up to ward-level granularity.
Keywords:
sensor mats; bedrails; belt; blanket restrictions; physical restraints; patients; confusion; delirious behavior; falls 1. Introduction
Physical restraints are defined as the application of devices (including belts, harnesses, manacles, sheets, and straps) nearby or to a person’s body to restrict their movement and to prevent the person from harming themselves or endangering others, or to ensure that essential treatment can be provided [1]. The efficacy of these methods has widely been discussed especially regarding their ethical, physical, and psychological implications and intended effect [2]. Additionally, their usage differs widely, making comparisons difficult.
While data on restraint use in general wards are scarce, there is some cross-country information on the use of restraints in the intensive care unit (ICU) setting available. The PRICE Study compared prevalence in ICUs across nine European countries with a total of 566 patients and found a large variation with prevalence ranging from 0.0% to 100%. However, these results need to be interpreted with caution because sample sizes differed between 15 and 319 patients [3]. Not surprisingly, Minnick et al. found that restraining rates on regular wards were much lower than in ICUs. Still, major differences were found between different clinics. For example, geriatric units had a much higher rate of restraint use than did medical, cardiac, or oncology units [4].
A cross-sectional study in a German acute care hospital found a prevalence rate of restraints of 11.8% (n = 1276). Then again, restraint use differed greatly ranging from 0 to 31% on general wards [5].
Even scarcer data are available on trends over time on restraint use. A study from Kwok et al. in China looked at 1946 patients admitted to medical wards in 2007 and 2009. With the implementation of a restraint reduction program, their use declined significantly from 13.3% in 2007 to 4.1% in 2009 [6]. Unfortunately, the authors did not provide specific information on the implemented program.
The scope of this study is to determine the prevalence, the types, and duration of physical restraints in association with length of stay, nurse’s time expenditure hours, falls, and in-hospital death on general wards in an acute care hospital. We hypothesized that patients with physical restraints would have longer length of stay, higher nurse’s time expenditure hours, more falls, and a higher rate of in-hospital death compared to patients without restraint use. Furthermore, we describe the usage of restraints on different wards of the same clinic over time.
2. Methods
This retrospective cohort study was conducted at the Cantonal Hospital Aarau, a tertiary, 600-bed hospital in Switzerland. Our Medical University Clinic has roughly 6000 admissions per year of which 80% are emergency admissions. Indications for the use of physical restraint were based on internal standard operating procedures regulated by the Swiss Civil Law [7].
2.1. Inclusion and Exclusion Criteria
All emergency admissions from January 2018 to December 2021 were screened for eligibility. The inclusion criteria were age ≥18 years, and hospitalization on a medical ward.
Exclusion criteria were non-medical leading diagnoses, length of hospital stay (LOS) <48 h and declined general informed consent. We deliberately excluded admission to an ICU, as these patients are very distinct from patients in a regular ward and have a very high rate of restraint use. We specifically looked at physical restraints, such as blanket restriction, bed rails, belts, and sensor mats. We excluded motion sensor alarms, as their use at our institution is experimental. It has to be noted that due to local regulations, regular, pre-installed and low-raised bed rails are not considered a physical restraint. Only additionally inserted high-raise bed rails are considered a physical restraint. Further, we excluded one-to-one supervision, as it is not a form of physical restraint by Swiss Civil Law.
2.2. Outcomes
Primary outcomes were LOS, nurses’ time expenditure per case, fall and in-hospital death. Previous studies have shown that patients with restraints have much longer LOS, putting additional strain on personnel, and are more likely to suffer adverse in-hospital outcomes [6,8,9]. A secondary outcome was the use of restricting measures in patients with delirium due to the high risk of patients suffering a delirium to be restrained [10].
2.3. Data Collection
We used administrative data provided by the coding department as well as data from the electronic patient record, which includes only in-hospital outcomes. We extracted the number and duration of every physical restraint at hospital admission based on the actual restraining, which provides us with an accurate database as Swiss law mandates that every restraining order is registered in a patient’s health record. Further, we manually conducted quality checks on a random subsample of patients. Data on pharmacological treatment and reason for a particular indication of a physical restraint were obtained by hand searching electronic health records for patients with restraints only by two authors (NL and TS) analogous to a previous study [11]. Per internal protocol, nurses screened patients older than 65 years once per shift (i.e., three times per day) for the first three days of admission for the risk of delirium using the Delirium Observational Screening Scale (DOS) [12]. A DOS ≥ 3 would trigger the confusion assessment method short (CAM-short) assessment to ascertain the presence of delirium [13]. Nurses’ time expenditure includes both working time from registered nurses and their assistants. In our EHR, the time expenditure for common tasks performed by nurses on a daily basis is standardized (e.g., insertion of an intravenous line is credited with 15 min). Nurses document these tasks regularly during their day. In the case of more demanding patients, nurses can modify the standardized times. Although the performed tasks might not be documented eventually, our measure provides at least an average and conservative estimate.
2.4. Statistical Analysis
We used descriptive statistics including mean with standard deviation (SD), median with interquartile range (IQR), and frequencies to describe the population, as appropriate. A two-sided p-value < 0.05 was considered significant. To analyze restraint use over time, we first fitted a linear regression with the number of restraints as the dependent variable and the year as the sole independent variable. We then fitted a second model additionally adjusting for defined clinically relevant confounders and effect modifiers, such as age, Elixhauser comorbidity index, gender, main diagnosis, insurance class, and ward. For the continuous outcome LOS and nurse’s time expenditure, we also fitted a linear regression with restraint use as a binary independent variable. Binary outcomes were assessed accordingly by logistic regression. All models were fitted with robust standard errors. Analyses were performed with Stata version 15.2 (Stata Corp., College Station, TX, USA).
3. Results
3.1. Patient Cohort
From January 2018 to December 2021, we reviewed 16,730 admissions of which 4751 met our exclusion criteria (see Figure 1). Out of 11,979 admissions, 772 (1.7%) experienced at least one physical restraint. The mean age was 78 years (±12), and 41.5% were women. The most frequent diagnoses in restrained patients were diseases of the circulatory system (22.0%), followed by diseases of the respiratory system (16.1%), and neoplasms (16.1%) (see Table 1). To further aid the readers’ interpretation, we added tables depicting the amount of missing information in the dataset (see Supplementary Tables S1 and S2), as we performed a complete case analysis only.
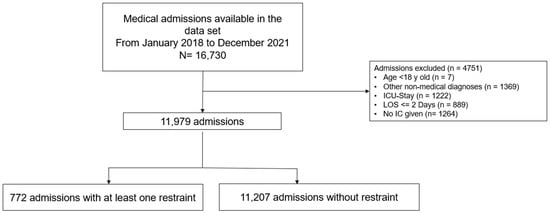
Figure 1.
Flow chart of patient selection process. Abbreviation: LOS, length of stay; IC, informed consent; ICU, intensive care unit.

Table 1.
Baseline.
The most frequently used type of restraint was sensor mats (73.0%, n = 666), followed by blanket restrictions (14.5%, n = 132), bedrails (8.8%, n = 80) and any type of belt (3.7%, n = 34).
The duration of a restraint normalized to the total number of restraints per patient was 42 h (±57). Bedrails had the longest duration with 58 h (±102), followed by sensor mats with 42 h (±51), blanket restrictions with 25 h (±23) and belts with 18 h (±21) (see Table 2).

Table 2.
Falls and outcomes among different types of restraints.
3.2. Association of Physical Restraints and Outcome
LOS was higher among patients with physical restraints with a median of 8 days (IQR 5–14), while patients without restraints had a median LOS of 5 days (IQR 3–9) (see Table 1). Nurses’ time expenditure per patient was performed by registered nurses and nurse assistants. Nurses spent a median of 309 h (IQR 242–402) in patients with restraints and 182 h (IQR 136–243) in patients without restraints. Falls occurred in 22.5% (n = 174) of restrained patients and in 2.7% (n = 300) of non-restrained patients. Only a minority of falls happened after the application of a restraint in 6.0% of patients (n = 46). However, there was a large spread in the timing between the use of restraint and occurrence of a fall (−19 h ± 161) (see Table 2). In-hospital death occurred in 13.3% (n = 103) of patients with physical restraints and 5.1 % (n = 577) of patients without physical restraints. Restraint patients also had a higher DOS (3.3) than those not restrained (0.55).
After controlling for confounders by regression analysis, the utilization of physical restraint still had a significant impact on all the outcomes. For instance, baseline LOS was 4.28 days but was increased by an additional 2.31 days when restraining methods had to be applied to a patient. Additionally, baseline odds for a fall were very low at 0.005 but increased 8.85 times in the case of a restraining measure (see Table 3).

Table 3.
Outcomes multivariable adjusted by important clinical confounders.
3.3. Indication for the Use of Restraint and Medical Therapy
The main reason for the use of restraint was delirium (64.6%, n = 137), followed by fall prevention (26.4 %, n = 56) and preventing aggressive behavior (3.8 %, n = 8). The use of benzodiazepines and antipsychotics tendentially increased during the hospital stay, and usage persisted after the stop of restraints (see Supplementary Table S3).
3.4. Trends over Time
The use of restraints decreased significantly over the years (see Figure 2) while the average duration of restraint adjusted per 1000 patient days also declined (see Figure 3). There were no consistent differences in restraint use between wards in our clinic (see Figure 4).
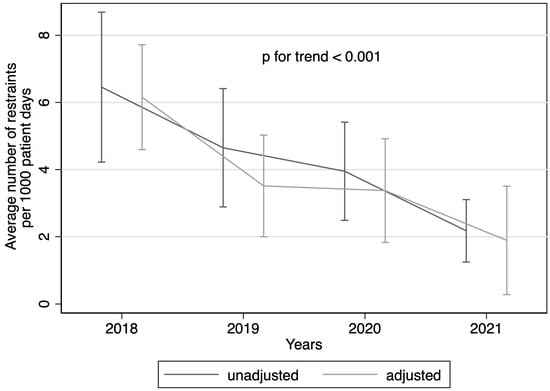
Figure 2.
Use of restraints over the years. Use of restraints over the years fitted by unadjusted linear regression and adjusted by admission year, age, gender, main diagnosis, ward, insurance class, and Elixhauser index. y-axis with average number of restraints per 1000 patient days.
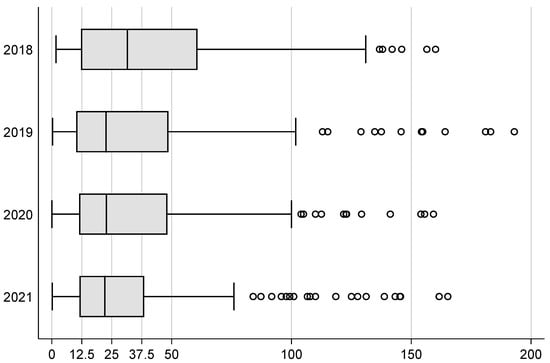
Figure 3.
Boxplot of restraint duration in hours per total number of restraints. Legend: vertical bar in box denotes median, and edges of rectangles the 25th and 75th percentiles, whiskers extend to include all data points within 1.5 times the interquartile range, circles denote outside values. Note: Fourteen outliers between 200 h and 807 h were omitted for better scalability.
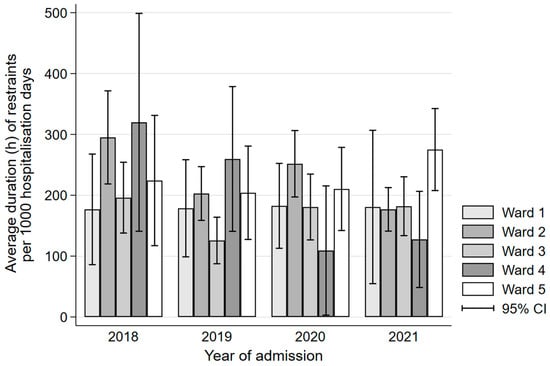
Figure 4.
Bar chart of average duration in hours of restraint per year and ward. Legend: CI, confidence interval.
4. Discussion
In our study, 6.4% out of 11,979 admissions received at least one physical restraint. Restrained patients were more severely ill, were more likely to be male, and older compared to non-restrained patients. The average restrained patient resulted in 309 h in nurses’ time expenditure, compared to 182 h for a non-restrained patient. LOS was 5 days in non-restrained patients, compared to 8 days in restrained patients. 22.5 % of restrained patients experienced a fall compared to 2.7% of non-restrained patients. Also, in-hospital death wase more frequent in restrained patients with 13.3% versus 5.1%. We also saw a decrease in the use of restraints over time, but no differences between wards. We assume that the statistically significant decrease in physical restraints over the time is due to the more liberal use of one-to-one supervision in our institution, however we do not have data to underpin this assumption.
Similar to other studies we have shown that physical restraint use might lead to several negative outcomes including increased risks of falls, aggressive behavior, a decline in physical functioning, and psychiatric comorbidities [2,14,15].
Our study corroborates that the vulnerable group of elderly and severely ill patients is mostly affected by restraint use.
4.1. LOS and Nurses’ Time Expenditure
Patients with physical restraints had a substantially longer LOS compared to non-restrained patients which is consistent with previous studies. Our average LOS for restraint patients was 8 days, which is below the 9 days to 21.1 days reported by others [6,8,9].
Restrained patients generate a large impact on hospital resources; in particular, nurses have to dedicate a lot, leaving them with less time for other tasks. These differences persisted despite adjustment for confounders providing evidence for a high-need patient group.
A detailed evaluation of a restraint’s necessity can help in minimizing both resources of personnel and making a stay for patients safer by preventing adverse events of restraint use, as patients often experience anger, discomfort, resistance, and fear in response to a physical restraint [16]. Providing patients with activities, or directly involving relatives could help minimizing or even avoiding the use of restraints [17]. Multidisciplinary decision making, adequate management of underlying co-precipitant factors such as sleep dysregulation, management of pain, adequate use of pharmacological therapy, and early mobilization alongside strengthening exercises are proven measures to minimize the use of restraints [18].
4.2. Comparing Fall and Type of Restraints
We observed that restraint use was mostly implemented before a fall. Use of physical restraints to prevent fall and ensuring patient’s safety is one of the most widespread indications [11]. Our study showed that 22.5% of restrained patients suffered a fall, which, on average, occurred 19 h before the restraint started. Because of the large heterogeneity in the data, we could not further delineate the associations between restraint use and a consecutive fall in a hierarchical regression model. While many restraints were started after a first fall, restraints do not seem to be effective in preventing a consecutive fall.
This is in line with current evidence implying that restraints do not appear to be effective in reducing falls or injuries among adults in acute care hospitals [19,20]. It is even plausible that physical restraints paradoxically increase the risk of falls, as patients are more agitated, and attempting to escape their restraints may become entangled and fall [21]. In addition, the use of restraint may result in later mobilization another factor known to maintain a delirium [19,22].
While bedrails are the most common type of restraint in North America [23] and Germany [5], sensor mats were the most widely used type in our setting. We attribute this finding to the fact that regular, pre-installed, low raise bed rails are not considered a restraint, but only additionally installed high raise bed rails.
4.3. Differences between Wards of the Same Clinic
A secondary analysis of a cross-sectional study in Germany showed that the prevalence of restraints was 9.3% in a sample of 2827 in-hospital patients and restraints use was more prevalent in women [24]. In contrast to our results, they observed a higher restraint rate on medical wards (12.5%, n = 116), and an even higher rate on the geriatric ward (25.6%, n = 30). However, comparability is difficult, as the patients in wards at our clinic are heterogeneous and polymorbid.
A cross-sectional study in 55 Swiss hospitals found an average prevalence rate of physical restraints of 10.2% in 2021. However, large discrepancies were noted with 40% of all hospitals either using restraints significantly more or less often than the average [25]. The authors concluded that the use of physical restraints should be used as a quality indicator for hospitals. In our view, this call is questionable because of largely varying populations across clinics and hospitals. As a prerequisite, hospitals should be compared to one another clinic wise ensuring comparable patient risk groups and preventing mixing of differing patient populations.
4.4. Strengths and Limitations
As a single centered, retrospective cohort study, our results are not easily generalizable. Furthermore, we provide a descriptive overview and can thus draw no conclusions on causality between restraints and clinical outcomes. Additionally, we have a rather small sample for rare events, and no long-term follow-up outside an admission (e.g., 1 year mortality). In addition, our data warehouse currently only hosts up to five years of data, limiting our conclusions to a rather short time span.
Our study has several strengths. We focused on the admission at medical wards with specific types of restraints and the chronological relation between the use of restraints and fall. In contrast to previous studies, we provide insight at a ward level and trends over the last four years. Further, we described nurses‘ time expenditure hours as a measure of work burden. Additionally, we provided information on the use of pharmacological therapy, and the classification of restraints’ indications.
5. Conclusions
In conclusion, these data suggest that a relatively low rate of approximately 6% of medical patients experienced a restraint with a declining trend over time and no difference between the medical wards.
Our work points out the current challenges in nursing, that is economical pressure to reduce LOS combined with an increased number of elderly and severely ill in-hospital patients at high risk for delirium. In this challenging environment, nurses need to critically evaluate physical restraints as adverse effects from restraints are very common. We assume that patients with delirium are frequently subjected to physical restraints and specifically, we have shown that restraint use does not reduce consecutive falls. Hence, health care professionals should only apply restraints in situations where there is good evidence for a beneficial effect. As such, quality improvement studies should be conducted in various health care settings to find the best solutions for local problems. Additionally, restraints need to be used as shortly as possible, assessed at least once per shift, and be substituted by the least invasive measure such as one-to-one supervision whenever possible. Future studies should critically investigate the crucial relation between unfavorable patient-to-nurse ratios, especially as economical pressure will likely lead to reduced staffing. We need to better understand the optimal management of patients at high risk of a restraint to reduce the overall use of restraints and prevent their harmful complications.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/geriatrics8010015/s1, Table S1: Depiction of missing data in Table 1. Table S2: Depiction of missing data in Table 2. Table S3: Indication for use of restraints and therapy with psychotropic medications.
Author Contributions
T.S. and U.S. designed the study. T.S. and U.S. performed the statistical calculations and wrote the first draft of the manuscript. N.L., T.S. and D.K. were responsible for data extraction. J.S., P.S. and B.M. reviewed and edited the original draft. T.S. and U.S. were responsible for the decision to submit the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported in part by the Swiss National Science Foundation (SNSF, SNSF P400PM_194497/1 to T.S.), and the “Hugo und Elsa Isler Foundation” of the Argovian Department of Health and Social Affairs. The APC was funded by Cantonal Hospital Aarau. The funding sources had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Institutional Review Board Statement
Institutional review board approval, was provided by the Institutional Review Board of Northwestern Switzerland (EKNZ BASEC Req-2022-00977). This study was conducted according to the principles stated in the Declaration of Helsinki and followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines [26].
Informed Consent Statement
The institutional review board waived the requirement of participant informed consent, due to the de-identified data and the retrospective nature of the analysis.
Data Availability Statement
According to Swiss laws, data sharing is restricted to the country.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bleijlevens, M.H.; Wagner, L.M.; Capezuti, E.; Hamers, J.P. International Physical Restraint W: Physical Restraints: Consensus of a Research Definition Using a Modified Delphi Technique. J. Am. Geriatr. Soc. 2016, 64, 2307–2310. [Google Scholar] [CrossRef] [PubMed]
- Gastmans, C.; Milisen, K. Use of physical restraint in nursing homes: Clinical-ethical considerations. J. Med. Ethics 2006, 32, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Benbenbishty, J.; Adam, S.; Endacott, R. Physical restraint use in intensive care units across Europe: The PRICE study. Intensive Crit. Care Nurs. 2010, 26, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Minnick, A.F.; Mion, L.C.; Johnson, M.E.; Catrambone, C.; Leipzig, R. Prevalence and Variation of Physical Restraint Use in Acute Care Settings in the US. J. Nurs. Scholarsh. 2007, 39, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Kruger, C.; Mayer, H.; Haastert, B.; Meyer, G. Use of physical restraints in acute hospitals in Germany: A multi-centre cross-sectional study. Int. J. Nurs. Stud. 2013, 50, 1599–1606. [Google Scholar] [CrossRef]
- Kwok, T.; Bai, X.; Chui, M.Y.; Lai, C.K.; Ho, D.W.; Ho, F.K.; Woo, J. Effect of physical restraint reduction on older patients’ hospital length of stay. J. Am. Med. Dir. Assoc. 2012, 13, 645–650. [Google Scholar] [CrossRef]
- The Federal Assembly of the Swiss Confederation. The Publication Platform for Federal Law. The Civil Code Switzerland; The Federal Assembly of the Swiss Confederation: Bern, Switzerland, 1907. [Google Scholar]
- Raguan, B. Use of Physical Restraints in a General Hospital a cross sectional observational study. IMAJ 2015, 17, 633–638. [Google Scholar]
- Bai, X.; Kwok, T.C.; Ip, I.N.; Woo, J.; Chui, M.Y.; Ho, F.K. Physical restraint use and older patients’ length of hospital stay. Health Psychol. Behav. Med. 2014, 2, 160–170. [Google Scholar] [CrossRef]
- Weinrebe, W.; Johannsdottir, E.; Karaman, M.; Fusgen, I. What does delirium cost? An economic evaluation of hyperactive delirium. Z Gerontol. Geriatr. 2016, 49, 52–58. [Google Scholar] [CrossRef]
- Thomann, S.; Zwakhalen, S.; Richter, D.; Bauer, S.; Hahn, S. Restraint use in the acute-care hospital setting: A cross-sectional multi-centre study. Int. J. Nurs. Stud. 2021, 114, 103807. [Google Scholar] [CrossRef]
- Park, J.; Jeong, E.; Lee, J. The Delirium Observation Screening Scale: A Systematic Review and Meta-Analysis of Diagnostic Test Accuracy. Clin. Nurs. Res. 2021, 30, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.A.; Fearing, M.A.; Sternberg, E.J.; Inouye, S.K. The Confusion Assessment Method: A systematic review of current usage. J. Am. Geriatr. Soc. 2008, 56, 823–830. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Hirdes, J.P.; Smith, T.F.; Finne-Soveri, H.; Chi, I.; Du Pasquier, J.N.; Gilgen, R.; Ikegami, N.; Mor, V. Use of physical restraints and antipsychotic medications in nursing homes: A cross-national study. Int. J. Geriatr. Psychiatry 2009, 24, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Lam, K.; Kwan, J.S.K.; Wai Kwan, C.; Chong, A.M.L.; Lai, C.K.Y.; Lou, V.W.Q.; Leung, A.Y.M.; Liu, J.Y.W.; Bai, X.; Chi, I. Factors Associated With the Trend of Physical and Chemical Restraint Use Among Long-Term Care Facility Residents in Hong Kong: Data From an 11-Year Observational Study. J. Am. Med. Dir. Assoc. 2017, 18, 1043–1048. [Google Scholar] [CrossRef]
- Strumpf, N.E.; Evans, L.K. Physical restraint of the hospitalized elderly: Perceptions of patients and nurses. Nurs. Res. 1988, 37, 132–137. [Google Scholar] [CrossRef]
- Wilson, C.; Rouse, L.; Rae, S.; Kar Ray, M. Mental health inpatients’ and staff members’ suggestions for reducing physical restraint: A qualitative study. J. Psychiatr. Ment. Health Nurs. 2018, 25, 188–200. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhuang, Y.; Lao, Y.; Qiao, L.; Chen, Y.; Guo, F. Development and implementation of a novel decision support tool on physical restraint use in critically ill adult patients. Int. J. Nurs. Pract. 2021, 28, e12961. [Google Scholar] [CrossRef]
- Mott, S.; Poole, J.; Kenrick, M. Physical and chemical restraints in acute care: Their potential impact on the rehabilitation of older people. Int. J. Nurs. Pract. 2005, 11, 95–101. [Google Scholar] [CrossRef]
- Capezuti, E.; Strumpf, N.E.; Evans, L.K.; Grisso, J.A.; Maislin, G. The relationship between physical restraint removal and falls and injuries among nursing home residents. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1998, 53, M47–M52. [Google Scholar] [CrossRef]
- Shorr, R.I.; Guillen, M.K.; Rosenblatt, L.C.; Walker, K.; Caudle, C.E.; Kritchevsky, S.B. Restraint use, restraint orders, and the risk of falls in hospitalized patients. J. Am. Geriatr. Soc. 2002, 50, 526–529. [Google Scholar] [CrossRef]
- Hart, B.D.; Birkas, J.; Lachmann, M.; Saunders, L. Promoting positive outcomes for elderly persons in the hospital: Prevention and risk factor modification. AACN Clin. Issues 2002, 13, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Barton-Gooden, A.; Dawkins, P.E.; Bennett, J. Physical Restraint Usage at a Teaching Hospital: A Pilot Study. Clin. Nurs. Res. 2013, 24, 73–90. [Google Scholar] [CrossRef] [PubMed]
- Heinze, C.; Dassen, T.; Grittner, U. Use of physical restraints in nursing homes and hospitals and related factors: A cross-sectional study. J. Clin. Nurs. 2012, 21, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Thomann, S.; Hahn, S.; Schmitt, K.U.; Barbezat, I.; Siegrist-Dreier, S.; Richter, D. Restraint use as a quality indicator for the hospital setting: A secondary data analysis. Swiss Med. Wkly. 2021, 151, w30043. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).