Ageism and the Pandemic: Risk and Protective Factors of Well-Being in Older People
Abstract
1. Introduction
The Current Research
2. Materials and Methods
2.1. Procedure of Recruitment and Participants
2.2. Instruments
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics and Correlation Analysis
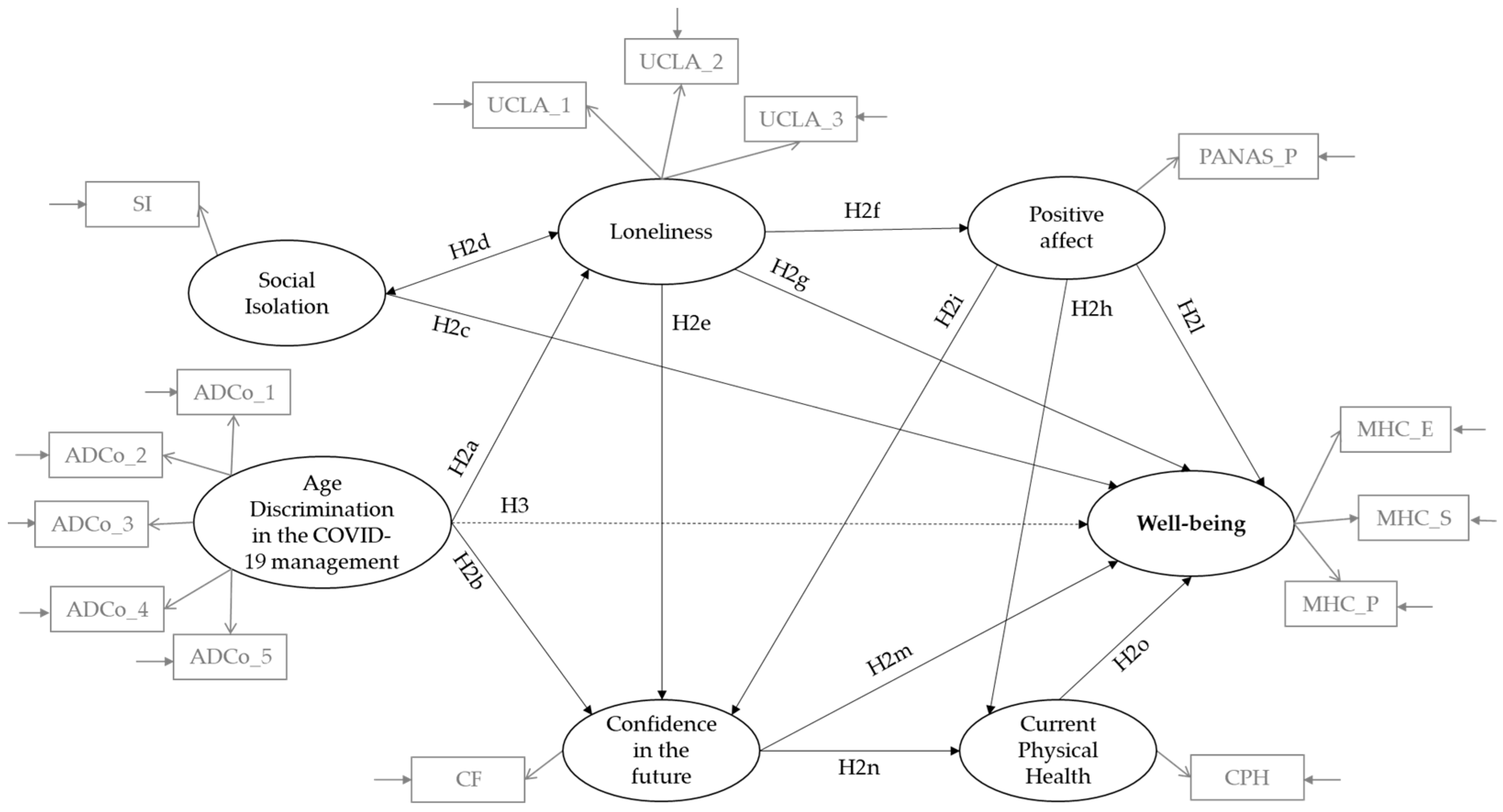
3.2. Testing of the Hypothesised Conceptual Model
4. Discussion
4.1. Limitations
4.2. Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Italian Ministry of Health. Section Dedicated to COVID-19. Available online: http://www.salute.gov.it/portale/home.html (accessed on 22 June 2020).
- Livingston, E.; Bucher, K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA 2020, 323, 1335. [Google Scholar] [CrossRef]
- Bavishi, C.; Maddox, T.M.; Messerli, F.H. Coronavirus disease 2019 (COVID-19) infection and renin angiotensin system blockers. JAMA Cardiol. 2020, 5, 745–747. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Decree of the President of the Council of Ministers. Available online: https://www.esteri.it/mae/resource/doc/2020/03/decreto_del_presidente_del_consiglio_dei_ministri_8_marzo_2020_en_rev_1.pdf (accessed on 22 June 2020).
- Roma, P.; Monaro, M.; Colasanti, M.; Ricci, E.; Biondi, S.; Di Domenico, A.; Verrocchio, M.C.; Napoli, C.; Ferracuti, S.; Mazza, C. A 2-Month Follow-Up Study of Psychological Distress among Italian People during the COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2020, 17, 8180. [Google Scholar] [CrossRef] [PubMed]
- Garfin, D.R.; Silver, R.C.; Holman, E.A. The Novel Coronavirus (COVID-2019) Outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020, 39, 355–357. [Google Scholar] [CrossRef]
- Cornwell, B.; Laumann, E.O. The health benefits of network growth: New evidence from a national survey of older adults. Soc. Sci. Med. 2015, 125, 94–106. [Google Scholar] [CrossRef]
- Santini, Z.I.; Jose, P.E.; York Cornwell, E.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef]
- Donizzetti, A.R.; Lagacé, M. COVID-19 and the Elderly’s Mental Illness: The Role of Risk Perception, Social Isolation, Loneliness and Ageism. Int. J. Environ. Res. Public Health 2022, 19, 4513. [Google Scholar] [CrossRef]
- Nicholson, N.R. A Review of Social Isolation: An Important but Underassessed Condition in Older Adults. J. Prim. Prev. 2012, 33, 137–152. [Google Scholar] [CrossRef]
- Valtorta, N.K.; Kanaan, M.; Gilbody, S.; Hanratty, B. Loneliness, social isolation and social relationships: What are we measuring? A novel framework for classifying and comparing tools. BMJ Open 2016, 6, e010799. [Google Scholar] [CrossRef]
- Beller, J.; Wagner, A. Loneliness, social isolation, their synergistic interaction, and mortality. Health Psychol. 2018, 37, 808–813. [Google Scholar] [CrossRef] [PubMed]
- McHugh, P.J.E.; Steptoe, A.; Kee, F.; Lawlor, B. Loneliness and social engagement in older adults: A bivariate dual change score analysis. Psychol. Aging 2019, 34, 152–162. [Google Scholar] [CrossRef] [PubMed]
- De Jong Gierveld, J.; van Tilburg, T.G.; Dykstra, P.A. Loneliness and social isolation. In The Cambridge Handbook of Personal Relationships Cambridge; Perlman, D., Vangelisti, A., Eds.; Cambridge University Press: Cambridge, UK, 2006; pp. 485–500. [Google Scholar]
- Dykstra, P.A. Older adult loneliness: Myths and realities. Eur. J. Ageing 2009, 6, 91–100. [Google Scholar] [CrossRef]
- De Jong Gierveld, J. A review of loneliness: Concept and definitions, determinants and consequences. Rev. Clin. Gerontol. 1998, 8, 73–80. [Google Scholar] [CrossRef]
- Peplau, L.A.; Perlman, D. Loneliness: A Sourcebook of Current Theory, Research, and Therapy; Wiley: New York, NY, USA, 1982. [Google Scholar]
- Shiovitz-Ezra, S.; Shemesh, J.; McDonnell/Naughton, M. Pathways from Ageism to Loneliness. In Contemporary Perspectives on Ageism. International Perspectives on Aging; Ayalon, L., Tesch-Römer, C., Eds.; Springer: Cham, Switzerland; Berlin/Heidelberg, Germany, 2018; Volume 19, pp. 131–147. [Google Scholar] [CrossRef]
- Steptoe, A.; Owen, N.; Kunz-Ebrecht, S.R.; Brydon, L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology 2004, 29, 593–611. [Google Scholar] [CrossRef]
- Russell, D.; Peplau, L.A.; Cutrona, C.E. The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. J. Pers. Soc. Psychol. 1980, 39, 472–480. [Google Scholar] [CrossRef]
- Russell, D.; Peplau, L.A.; Ferguson, M.L. Developing a measure of loneliness. J. Pers. Assess 1978, 42, 290–294. [Google Scholar] [CrossRef]
- Dahlberg, L.; McKee, K.J.; Frank, A.; Naseer, M. A systematic review of longitudinal risk factors for loneliness in older adults. Aging Ment. Health 2021, 10, 225–249. [Google Scholar] [CrossRef]
- COVID-19, le Misure di Contenimento per l’Italia Nel Nuovo DPCM [COVID-19, the Containment Measures for Italy in the New DPCM]. Available online: https://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4155 (accessed on 11 December 2021).
- Fraser, S.; Lagacé, M.; Bongué, B.; Ndeye, N.; Guyot, J.; Bechard, L.; Garcia, L.; Taler, V.; CCNA Social Inclusion and Stigma Working Group; Adam, S.; et al. Ageism and COVID-19: What does our society’s response say about us? Age Ageing 2020, 49, 692–695. [Google Scholar] [CrossRef]
- Manso, M.E.G.; Kim, B.M.J.; de Silva, W.F.; Baticini, B. Ageism and COVID-19: An integrative review. Res. Soc. Dev. 2021, 10, e274101119233. [Google Scholar] [CrossRef]
- Iversen, T.N.; Larsen, L.; Solem, P.E. A conceptual analysis of ageism. Nord. Psychol. 2009, 61, 4–22. [Google Scholar] [CrossRef]
- Donizzetti, A.R. Misurare il pregiudizio verso gli anziani: Validazione italiana della Fraboni Scale of Ageism e analisi delle differenze per genere ed età [Measuring prejudice towards the elderly: Italian validation of the Fraboni Scale of Ageism and analysis of differences by gender and age]. G. Psicol. 2010, 4, 258–269. [Google Scholar]
- Donizzetti, A.R. Ageism in an Aging Society: The Role of Knowledge, Anxiety about Aging, and Stereotypes in Young People and Adults. Int. J. Environ. Res. Public Health 2019, 16, 1329. [Google Scholar] [CrossRef] [PubMed]
- Ayalon, L. Perceived age, gender, and racial/ethnic discrimination in Europe: Results from the European social survey. Educ. Gerontol. 2014, 40, 499–517. [Google Scholar] [CrossRef]
- Voss, P.; Wolff, J.K.; Rothermund, K. Relations between views on ageing and perceived age discrimination: A domain-specific perspective. Eur. J. Ageing 2017, 14, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Levy, B. Stereotype embodiment: A psychosocial approach to aging. Curr. Dir. Psychol. Sci. 2009, 18, 332–336. [Google Scholar] [CrossRef]
- Shiovitz-Ezra, S.; Ayalon, L. Situational versus chronic loneliness as risk factors for all-cause mortality. Int. Psychogeriatr. 2010, 22, 455–462. [Google Scholar] [CrossRef]
- Levy, B.R.; Slade, M.D.; Kunkel, S.R.; Kasl, S.V. Longevity increased by positive self-perceptions of aging. J. Pers. Soc. Psychol. 2002, 83, 261–270. [Google Scholar] [CrossRef]
- Keyes, C.L.M. Comprehensive mental health: An agenda for the 21st century. In Flourishing: Positive Psychology and the Well-Lived; Keyes, C.L.M., Haidt, J., Eds.; American Psychological Association: Washington, DC, USA, 2003; pp. 293–312. [Google Scholar] [CrossRef]
- Ryan, R.M.; Huta, V.; Deci, E.L. Living well: A self-determination theory perspective on eudaimonia. J. Happiness Stud. 2008, 9, 139–170. [Google Scholar] [CrossRef]
- Keyes, C.L. Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. Am. Psychol. 2007, 62, 95–108. [Google Scholar] [CrossRef]
- Cowen, E.L. In pursuit of wellness. Am. Psychol. 1991, 46, 404–408. [Google Scholar] [CrossRef]
- Pressman, S.D.; Cross, M.P. Moving beyond a one-size-fits-all view of positive affect in health research. Curr. Dir. Psychol. Sci. 2018, 27, 339–344. [Google Scholar] [CrossRef]
- Watson, D.; Wiese, D.; Vaidya, J.; Tellegen, A. The two general activation systems of affect: Structural findings, evolutionary considerations, and psychobiological evidence. J. Pers. Soc. Psychol. 1999, 76, 820–838. [Google Scholar] [CrossRef]
- Steptoe, A.; Wardle, J.; Marmot, M. Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proc. Natl. Acad. Sci. USA 2005, 102, 6508–6512. [Google Scholar] [CrossRef] [PubMed]
- Sin, N.L.; Moskowitz, J.T.; Whooley, M.A. Positive affect and health behaviors across 5 years in patients with coronary heart disease: The Heart and Soul Study. Psychosom. Med. 2015, 77, 1058–1066. [Google Scholar] [CrossRef]
- Lyubomirsky, S.; King, L.; Diener, E. The benefits of frequent positive affect: Does happiness lead to success? Psychol. Bull. 2005, 131, 803–855. [Google Scholar] [CrossRef]
- Pressman, S.D.; Cohen, S. Does positive affect influence health? Psychol. Bull. 2005, 131, 925–971. [Google Scholar] [CrossRef]
- Fredrickson, B.L. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. Am. Psychol. 2001, 56, 218–226. [Google Scholar] [CrossRef]
- Greenglass, E.R.; Fiksenbaum, L. Proactive coping, positive affect and well-being: Testing for mediation using path analysis. Eur. Psychol. 2009, 14, 29–39. [Google Scholar] [CrossRef]
- Sirgy, M.J. Positive balance: A hierarchical perspective of positive mental health. Qual Life Res 2019, 28, 1921–1930. [Google Scholar] [CrossRef]
- Fredrickson, B.L. Cultivating positive emotions to optimize health and well-being. Prev. Treat. 2000, 3, 0001a. [Google Scholar] [CrossRef]
- Stankov, L.; Kleitman, S. Processes on the borderline between cognitive abilities and personality: Confidence and its realism. In The SAGE Handbook of Personality Theory and Assessment; Boyle, G.J., Matthews, G., Saklofske, D.H., Eds.; Sage Publications, Inc.: Newbury Park, CA, USA, 2008; Volume 1, pp. 545–559. [Google Scholar]
- Keyes, C.L.M. The mental health continuum: From languishing to flourishing in life. Am. J. Health Behav. 2002, 43, 207–222. [Google Scholar] [CrossRef]
- Petrillo, G.; Capone, V.; Caso, D.; Keyes, C.L. The mental health continuum–short form (MHC–SF) as a measure of well-being in the Italian context. Soc. Indic. Res. 2015, 121, 291–312. [Google Scholar] [CrossRef]
- Garstka, T.A.; Schmitt, M.T.; Branscombe, N.R.; Hummert, M.L. How Young and Older Adults Differ in Their Responses to Perceived Age Discrimination. Psychol. Aging 2004, 19, 326–335. [Google Scholar] [CrossRef]
- Russell, D.W. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J. Pers. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef]
- Boffo, M.; Mannarini, S.; Munari, C. Exploratory Structure Equation Modeling of the UCLA Loneliness Scale: A contribution to the Italian adaptation. TPM Test Psychom. Methodol. Appl. Psychol. 2012, 19, 345–363. [Google Scholar] [CrossRef]
- Wister, A.; Cosco, T.; Mitchell, B.; Menec, V.; Fyffe, I. Development and Concurrent Validity of a Composite Social Isolation Index for Older Adults Using the CLSA. Can. J. Aging 2019, 38, 180–192. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Terracciano, A.; McCrae, R.R.; Costa, P.T., Jr. Factorial and construct validity of the Italian positive and negative affect schedule (PANAS). Eur. J. Psychol. 2003, 19, 131–141. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Fava, G.A. Assessing depressive symptoms across cultures: Italian validation of the CES-D self-rating scale. J. Clin. Psychol. 1983, 39, 249–251. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.C.; Bernstein, I.J. Psychometric Theory; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- MacCallum, R.C.; Austin, J.T. Applications of structural equation modeling in psychological research. Annu. Rev. Psychol. 2000, 51, 201–226. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cuto criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- McNeish, D.; An, J.; Hancock, G.R. The Thorny Relation between Measurement Quality and Fit Index Cutoffs in Latent Variable Models. J. Pers. Assess. 2018, 100, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Ullman, J.B. Structural equation modeling. In Using Multivariate Statistics; Tabachnick, B.G., Fidell, L.S., Eds.; Allyn & Bacon: Needham Heights, MA, USA, 2001; pp. 653–771. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Perspective; The Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Holt-Lunstad, J.; Smith, T.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef]
- Kraav, S.L.; Lehto, S.M.; Junttila, N.; Ruusunen, A.; Kauhanen, J.; Hantunen, S.; Tolmunen, T. Depression and loneliness may have a direct connection without mediating factors. Nord. J. Psychiatry 2021, 75, 553–557. [Google Scholar] [CrossRef]
- Hoppmann, C.A.; Infurna, F.J.; Ram, N.; Gerstorf, D. Associations between individual perceptions of future time, individual resources, and subjective well-being in old age. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017, 72, 388–399. [Google Scholar] [CrossRef]
- Desmyter, F.; De Raedt, R. The relationship between time perspective and subjective well-being of older adults. Psychol. Belg. 2012, 52, 19–38. [Google Scholar] [CrossRef]
- Abrams, D.; Swift, H.J.; Lamont, R.A.; Drury, L. The Barriers to and Enablers of Positive Attitudes to Ageing and Older People, at the Societal and Individual Level; Government Office for Science: London, UK, 2015; pp. 1–35. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/454735/gs-15-15-future-ageing-attitudes-barriers-enablers-er06.pdf (accessed on 18 February 2022).
- Nelson, T.D. Ageism: Prejudice against our feared future self. J. Soc. Issues 2005, 61, 207–221. [Google Scholar] [CrossRef]
- Nelson, T.D. Promoting healthy aging by confronting ageism. Am. Psychol. 2016, 71, 276–282. [Google Scholar] [CrossRef]
- Jang, Y.; Chiriboga, D.A.; Small, B.J. Perceived discrimination and psychological well-being: The mediating and moderating role of sense of control. Int. J. Aging Hum. Dev. 2008, 66, 213–227. [Google Scholar] [CrossRef] [PubMed]
- Vogt Yuan, A.S. Perceived age discrimination and mental health. Soc. Forces 2007, 86, 291–311. [Google Scholar] [CrossRef]
- Previtali, F.; Allen, L.D.; Varlamova, M. Not Only Virus Spread: The Diffusion of Ageism during the Outbreak of COVID-19. J. Aging Soc. Policy 2020, 32, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Kasomo, D. Loneliness and Depression among University Students in Kenya? Glob. J. Hum. Soc. Sci. 2013, 13, 11–18. [Google Scholar]
- Soto-Perez-de-Celis, E. Social media, ageism, and older adults during the COVID-19 pandemic. E Clin. Med. 2020, 29, 100634. [Google Scholar] [CrossRef] [PubMed]

| Means (SD) | Range | Skew | Kurt | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Well-being (MHC-SF) | 2.64 (1.00) | 0–5 | −0.04 | −0.47 | 1 | ||||||
| 2. Age Discrimination in the Context of the COVID-19 Pandemic (ADCo) | 2.75 (0.96) | 1–5 | 0.28 | −0.50 | −0.16 ** | 1 | |||||
| 3. Loneliness (UCLA) | 2.10 (0.47) | 1–4 | 0.24 | −0.19 | −0.56 ** | 0.24 ** | 1 | ||||
| 4. Social Isolation (SII) | 2.92 (0.64) | 0–5 | 0.04 | −0.32 | −0.42 ** | 0.03 | 0.32 ** | 1 | |||
| 5. Positive Affect (PA) | 2.57 (0.91) | 1–5 | 0.24 | −0.43 | 0.67 ** | −0.13 ** | −0.42 ** | −0.36 ** | 1 | ||
| 6. Confidence in the Future (CF) | 2.84 (0.88) | 1–4 | −0.26 | −0.73 | 0.45 ** | −0.15 ** | −0.35 ** | −0.22 ** | 0.41 ** | 1 | |
| 7. Current Physical Health (CPH) | 3.24 (0.83) | 1–5 | −0.37 | 0.20 | 0.35 ** | −0.12 ** | −0.28 ** | −0.20 ** | 0.32 ** | 0.23 ** | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donizzetti, A.R.; Capone, V. Ageism and the Pandemic: Risk and Protective Factors of Well-Being in Older People. Geriatrics 2023, 8, 14. https://doi.org/10.3390/geriatrics8010014
Donizzetti AR, Capone V. Ageism and the Pandemic: Risk and Protective Factors of Well-Being in Older People. Geriatrics. 2023; 8(1):14. https://doi.org/10.3390/geriatrics8010014
Chicago/Turabian StyleDonizzetti, Anna Rosa, and Vincenza Capone. 2023. "Ageism and the Pandemic: Risk and Protective Factors of Well-Being in Older People" Geriatrics 8, no. 1: 14. https://doi.org/10.3390/geriatrics8010014
APA StyleDonizzetti, A. R., & Capone, V. (2023). Ageism and the Pandemic: Risk and Protective Factors of Well-Being in Older People. Geriatrics, 8(1), 14. https://doi.org/10.3390/geriatrics8010014







