Abstract
Potentially inappropriate medications (PIMs) identified by the American Geriatrics Society should generally be avoided by older adults because of ineffectiveness or excess risk of adverse effects. Few studies have examined the effects of PIMs on driving safety measured by prospectively and objectively collected driving data. Data for this study came from the Longitudinal Research on Aging Drivers study, a multisite naturalistic driving study of older adults. Multivariable negative binominal modeling was used to estimate incidence rate ratios and 95% confidence intervals of hard braking events (proxies for unsafe driving behavior defined as events with a deceleration rate ≥0.4 g) associated with PIM use among older drivers. The study sample consisted of 2932 drivers aged 65–79 years at baseline, including 542 (18.5%) who used at least one PIM. These drivers were followed through an in-vehicle recording device for up to 44 months. The overall incidence of hard braking events was 1.16 per 1000 miles. Use of PIMs was associated with a 10% increased risk of hard braking events. Compared to drivers who were not using PIMs, the risk of hard braking events increased 6% for those using one PIM, and 24% for those using two or more PIMs. Use of PIMs by older adult drivers is associated in a dose-response fashion with elevated risks of hard braking events. Reducing PIM use in older adults might help improve driving safety as well as health outcomes.
1. Introduction
Drugs that may impair driving safety include illicit substances, such as cocaine and amphetamines, and prescription medications, such as opioids, benzodiazepines, and antidepressants [1]. Older drivers are particularly at heightened risk of crash involvement due in part to use of prescription medications for chronic medical conditions [2,3,4]. In addition, age-related decline in psychomotor skills and cognitive functioning may compromise driving ability among older adults [5].
The American Geriatrics Society (AGS) Beers Criteria [6] has identified three categories of potentially inappropriate medications (PIMs): (1) medications that should be generally avoided by older adults aged 65 years or older; (2) medications that are potentially inappropriate in older adults with certain disease conditions; and (3) medications that should be used with caution. Research on PIMs has focused on the first category of medications because these medications are deemed ineffective or harmful due to unfavorable risk-benefit ratios. PIMs most commonly used by older drivers are psychoactive medications, such as benzodiazepines, tricyclic antidepressants, first-generation antihistamines, and opioids [7]. Side effects of these medications include drowsiness, slowed reaction time, impaired attention, dizziness, confusion, and delirium [1,8,9,10]. A number of psychoactive medications have been individually linked to increased risks of crash involvement and crash culpability [1]. For instance, meta-analyses indicate that use of antidepressants is associated with a 40% increased risk of crash involvement [11] and that use of prescription opioids is associated with a 129% increased risk of crash involvement and a 47% increased risk of crash culpability [12].
Previous research on medication use and driving safety was conducted largely in middle age adults although the prevalence of medication use, particularly polypharmacy use, is much higher in older adults [13,14]. Moreover, few studies have assessed the relationship between medication use and driving safety based on objectively and prospectively collected driving data. Driving safety can be measured in different ways according to data availability, data quality, study objective, and other considerations. While commonly used safety outcome measures, such as crashes, injuries, fatalities, and violations, are readily available through administrative and surveillance systems, they are infrequent events and may not be sensitive enough to detect an adverse effect in a defined study sample within a reasonable timeframe. Moreover, accurate and detailed driving exposure data, such as driving patterns and driving space, are essential for rigorously measuring driving safety but are often lacking [15]. In recent years, the naturalistic driving design has been increasingly used in road safety research as it incorporates technologies, such as sensors, small cameras, and other recording devices, to capture detailed data on vehicle maneuvers (e.g., left turns and right turns, speed, and deceleration), driving patterns, performance, and behaviors [16]. Objectively measured data from naturalistic driving studies allow researchers to examine the effects of risk-taking behaviors, such as distracted driving, on real-world safety performance using surrogate indicators, such as hard braking events (i.e., near-crashes) [17]. The present study aims to examine the association between PIM use and the risk of hard braking events in a large cohort of older drivers with prospectively collected naturalistic driving data.
2. Materials and Methods
2.1. Study Sample
Data for this study came from the Longitudinal Research on Aging Drivers (LongROAD) project, an ongoing prospective cohort study of older drivers conducted in five sites (Ann Arbor, MI; Baltimore, MD; Cooperstown, NY; Denver, CO; and San Diego, CA) and sponsored by the AAA Foundation for Traffic Safety (Washington, DC). The LongROAD research team recruited 2990 older drivers from primary care clinics and health care systems. At the time of enrollment, study participants met the following inclusion criteria: (1) being 65–79 years of age; (2) holding a valid driver’s license; (3) being fluent in English; (4) driving at least once a week on average; (5) residing in the catchment area of any one of the five study sites for at least 10 months per calendar year; (6) having no plans to move outside of the catchment area within the next 5 years; (7) having access to a motor vehicle of model year 1996 or newer with an accessible on-board diagnostics II port; and (8) driving the primary vehicle ≥80% of the time if access to more than one vehicle. Those with significant cognitive impairment or degenerative medical conditions that may severely affect driving safety, such as Alzheimer’s disease and related dementias, were not eligible for enrollment. The study design and methods were described in detail elsewhere [18]; all participants completed informed consent and the study was approved by each site’s Institutional Review Board. Of the 2990 participants in the LongROAD study, 58 (1.9%) were excluded from this analysis due to missing baseline medication data (n = 41) or unavailable driving data (n = 17).
2.2. PIM Use
The exposure measure of primary interest in this analysis was PIM use, which was determined based on medication data collected at baseline through the “brown-bag review” method [18]. For the baseline in-person assessment, participants were asked to bring all currently used prescription and over-the-counter medications and supplements with them for review. Trained research staff completed a standard data form for each medication and supplement. Data on up to 50 medications and supplements were collected for each participant and then classified based on the pharmacologic therapeutic classification system established by the American Society of Health-System Pharmacists in the American Hospital Formulary Service (AHFS) Clinical Drug Information [19,20]. PIMs were identified according to the American Geriatrics Society 2015 Beers Criteria [6,7]. PIM use was first analyzed as a binary variable (yes/no) and then as a 3-level ordinal variable based on the number of PIMs identified (0, 1, or 2 and more).
2.3. Hard Braking Event
The outcome measure in this analysis was hard braking event, defined as a braking event with a deceleration rate ≥0.4 g. Data on these events and other driving behaviors were captured during the follow-up through the OBDII DataLogger (Danlaw, Inc., Novi, MI, USA), a recording device installed in the study participant’s primary vehicle at the time of enrollment. As a surrogate measure for aggressive or unsafe driving behavior, hard braking events are widely used in naturalistic driving studies [17,21,22,23,24].
2.4. Statistical Analysis
Incidence rates of hard braking events per 1000 miles driven were computed according to demographic characteristics, urbanicity, and PIM use. Urbanicity was based on the Rural Urban Commuting Area values for zip codes of study participants and was defined as urban (core region of a metropolitan statistical area), suburban (noncore region of a metropolitan statistical area) or rural (nonmetropolitan area) [25]. Because of over-dispersion in hard braking events, multivariable negative binominal modeling was used to estimate incidence rate ratios (IRRs) and 95% confidence intervals (CIs) of hard braking events associated with PIM use with adjustment for confounding variables. Data analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
3. Results
Of the 2932 drivers included in this analysis, 1374 (46.9%) were male, 1203 (41.0%) had graduate degrees, and 2134 (72.8%) lived in urban areas; average age at baseline was 71.08 ± 4.06 years. Use of at least one PIM was reported by 542 (18.5%) drivers (15.3% used only one PIM and 3.2% used two or more PIMs). Benzodiazepines were the most commonly used PIM, accounting for 16.6% of the PIMs identified. Other frequently used PIMs were non-benzodiazepine hypnotics (16.4% of the PIMs identified), antidepressants (15.2%), and first-generation antihistamines (10.5%).
After enrollment, the study participants were followed through the DataLogger for up to 44 months. The follow-up accumulated a total of 65,870,870 miles and 76,414 hard braking events, yielding an incidence rate of 1.16 hard braking events per 1000 miles. The incidence rate of hard braking events varied by demographic characteristics (Table 1). Specifically, drivers who were 70 years and older, female, nonwhite, or not married had elevated incidence rates of hard braking events whereas those who had an annual household income ≥$50,000 or resided in suburban and rural areas had decreased rates of hard braking events (Table 1). The incidence rate of hard braking events for drivers using PIMs at baseline was significantly higher than for those not using PIMs (1.30 vs. 1.13, p < 0.01; Table 1).

Table 1.
Incidence rates of hard braking events per 1000 miles by demographic characteristics, the Longitudinal Research on Aging Drivers (LongROAD) Study.
The final multivariable negative binominal model included only those variables statistically significantly associated with the risk of hard braking events on the multivariate level (Table 2). With adjustment for race, marital status, and urbanicity, PIM use was associated with a 10% increased risk of hard braking events (adjusted IRR 1.10, 95% CI 1.01–1.20). When PIM use was categorized into three groups based on the number of PIMs used, the estimated IRRs of hard braking events showed a dose-response relationship, increasing from 1.06 (95% CI 0.97–1.17) for those using one PIM to 1.24 (95% CI 1.02–1.51) for those using two or more PIMs compared to drivers not using PIMs (Figure 1). When the analysis was stratified based on gender, the dose-response relationship between PIM use and the risk of hard braking events existed in both male and female drivers. In addition to PIM use, drivers who were nonwhite, not married or residing in urban areas were at significantly increased risk of hard braking events (Table 2).

Table 2.
Estimated incidence rate ratios and 95% confidence intervals of hard braking events from the multivariable negative binomial model according to potentially inappropriate medication (PIM) Use, race/ethnicity, marital status and urbanicity, the Longitudinal Research on Aging Drivers (LongROAD) Study.
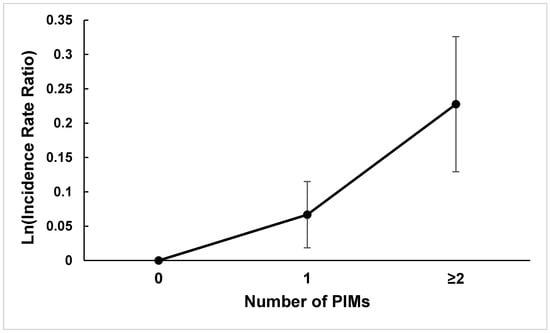
Figure 1.
Adjusted incidence rate ratios of hard braking events and 95% confidence intervals according to the number of potentially inappropriate medications (PIMs) used by older drivers, the Longitudinal Research on Aging Drivers (LongROAD) Study.
4. Discussion
PIM use in older adults has been linked to adverse drug reactions, excess healthcare costs, and increased morbidity and mortality [26,27,28,29]. This study is among the first attempts to assess the potential effect of PIM use on driving safety in older drivers. Results of this study indicate that PIM use is associated with a modest but statistically significant increase in the risk of hard braking events among older drivers. With adjustment for race /ethnicity, marital status and urbanicity, PIM use is associated with a 10% increased risk of hard braking events. Moreover, there exists a dose-response gradient in the relationship between PIM use and the risk of hard braking events.
Based on objectively and prospectively collected driving data, these findings add valuable evidence to the existent literature regarding the health and safety consequences of PIM use in older adults. Specifically, this study suggests that reducing PIM use through innovative intervention programs, such as computerized prescribing decision support tools [30], may help improve both health outcomes and driving safety among older adults. For older adults, driving is an important determinant of autonomy, independence and health [18,31]. Nevertheless, multiple chronic medical conditions (e.g., arthritis and cardiovascular disease) and polypharmacy use are prevalent in older drivers. Over 90% of the LongROAD study participants at baseline had two or more chronic medical conditions (with a median of 5 chronic medical conditions) and were on two or more medications (with a median of 7 medications) [20,32]. Of the medications used by older drivers, PIMs are of particular concern because the majority (about 58%) of them are psychoactive drugs, such as benzodiazepines, opioids, antidepressants, and first-generation antihistamines [7], which are known to be associated with increased risks of crash involvement and culpability [1,11,12,33,34,35,36]. Results of the present study provide empirical evidence that use of PIMs by older drivers, in particular use of multiple PIMs, could impair their safety performance.
Although many studies have examined the association of chronic medical conditions with crash risk, it remains a challenge to tease out the effect of specific medications from the effect of specific medical conditions. Given that the prevalence of multiple chronic medical conditions and polypharmacy use in the older driver population is over 90% [20,32], it is sensible to prioritize research using composite measures of comorbidities and medications, such as the Charlson Comorbidity Index score [37], PIMs [6], and Drug Burden Index [38], over studies of individual disease and medication in relation to driving safety in older adults.
In spite of notable strengths, such as the large sample size, comprehensive medication data and objectively and prospectively collected driving data, this study is limited by the observational study design and the proxy measure of driving safety. The prospective cohort design allows us to rigorously assess the association between PIM use and the risk of hard braking events, but makes it difficult, if not impossible, to infer causality. Moreover, the outcome measure in our study, hard braking event, is a proxy measure of driving safety. As a surrogate measure of driving safety, the incidence of hard braking events has been correlated to many contributing factors for crashes and is known to increase the reliability of risk estimation [21]. However, it should not be viewed as a substitute for crash risk before its validity for measuring crash risk is adequately established. Data on police-reported crashes are included in the LongROAD project. Because of the low incidence rate of motor vehicle crashes, it will take several more years of follow-up to accumulate enough crash records for adequately powered statistical analysis. Finally, the study sample is not nationally representative and thus the findings of this study may not be generalizable to the general older driver population in the United States. Compared to the general older driver population, participants of the LongROAD project are overrepresented by non-Hispanic white drivers and socioeconomically advantaged drivers as indicated by education attainment and annual household income [18].
5. Conclusions
Our study indicates that PIM use is associated with a significantly increased risk of hard braking events in a dose-response fashion in older drivers. In light of the well-documented adverse health consequences associated with PIM use in older adults, results of this study provide further impetus to implement effective intervention programs to reduce the prescription and use of PIMs in older adults.
Author Contributions
Conceptualization, G.L., L.L.H., Y.X., and D.W.E.; methodology, G.L., Y.X., S.C., D.W.E., T.J.M., H.F.A., L.J.M., M.E.B., and C.D.; validation, Y.X., S.C., H.F.A., and G.L.; formal analysis, Y.X., S.C., and G.L.; investigation, G.L., D.W.E., L.J.M., M.E.B., C.D., T.J.M., D.S., V.J., H.F.A., and L.L.H.; resources, B.H.L., T.K.-B., G.L., and H.F.A.; writing-original draft preparation, Y.X. and G.L.; writing-review and editing, G.L., B.H.L., Y.X., S.C., H.F.A., M.E.B., C.D., D.W.E., L.L.H., V.J., T.J.M., L.J.M., D.S., and T.K.-B.; visualization, Y.X. and G.L.; supervision, G.L.; project administration, T.K.-B., B.H.L., G.L., and D.W.E.; funding acquisition, G.L., D.W.E., L.J.M., T.J.M., D.S., C.D., M.E.B., V.J., L.L.H., and H.F.A.; All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the AAA Foundation for Traffic Safety and the APC was funded by the Department of Anesthesiology, Columbia University Vagelos College of Physicians and Surgeons. The contents of this work are the authors’ sole responsibility and do not necessarily represent official views of the AAA Foundation for Traffic Safety or the Department of Veterans Affairs.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Boards at Columbia University and each of the five study sites [Columbia University (New York, NY): protocol #AAAN9950 approved 18 September 2014; The Mary Imogene Bassett Hospital (Cooperstown, NY): protocol #1092 approved 7 July 2015; University of Colorado Anschutz Medical Campus (COMIRB, Aurora, CO): protocol # 14-0528 approved 25 November 2014; Johns Hopkins Bloomberg School of Public Health (Baltimore, MD): protocol #00006200 approved 8 April 2015; University of California, San Diego: protocol #141800 approved 8 January 2015; University of Michigan (Ann Arbor, MI): protocol # HUM00094031 approved 5 July 2015].
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Restrictions apply to the availability of these data. Data are available from the author with permission from the AAA Foundation for Traffic Safety and upon execution of a data use agreement.
Conflicts of Interest
Kelley-Baker is the Guest Editor of the Special Issue, “Driving, Aging, Safety, and Health”, she was not involved in the handling or review of this manuscript. The authors declare no other conflict of interest. The funding agencies had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Rudisill, T.M.; Zhu, M.; Kelley, G.A.; Pilkerton, C.; Rudisill, B.R. Medication use and the risk of motor vehicle collisions among licensed drivers: A systematic review. Accid. Anal. Prev. 2016, 96, 255–270. [Google Scholar] [CrossRef] [PubMed]
- Gibson, J.E.; Hubbard, R.B.; Smith, C.J.P.; Tata, L.J.; Britton, J.R.; Fogarty, A.W. Use of self-controlled analytical techniques to assess the association between use of prescription medications and the risk of motor vehicle crashes. Am. J. Epidemiol. 2009, 169, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Lococo, K.H.; Staplin, L. Literature Review of Polypharmacy and Older Drivers: Identifying Strategies to Collect Drug Usage and Driving Functioning among Older Drivers; National Highway Traffic Safety Administration: Washington, DC, USA, 2006. [Google Scholar]
- Guthrie, B.; Makubate, B.; Hernandez-Santiago, V.; Dreischulte, T. The rising tide of polypharmacy and drug-drug interactions: Population database analysis 1995–2010. BMC Med. 2015, 13, 74. [Google Scholar] [CrossRef] [PubMed]
- Griffin, C.E.; Kaye, A.M.; Bueno, F.R.; Kaye, A.D. Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner. J. 2013, 13, 214–223. [Google Scholar] [PubMed]
- American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr Soc. 2015, 63, 2227–2246. [Google Scholar] [CrossRef]
- Li, G.; Andrews, H.F.; Chihuri, S.; Lang, B.H.; Leu, C.S.; Merle, D.P.; Gordon, A.; Mielenz, T.J.; Strogatz, D.; Eby, D.W.; et al. Prevalence of Potentially Inappropriate Medication use in older drivers. BMC Geriatr. 2019, 19, 260. [Google Scholar] [CrossRef]
- Hetland, A.; Carr, D.B. Medications and impaired driving. Ann. Pharm. 2014, 48, 494–506. [Google Scholar] [CrossRef]
- Chang, C.-M.; Liu, P.-Y.Y.; Yang, Y.-H.K.; Yang, Y.-C.; Wu, C.-F.; Lu, F.-H. Use of the Beers criteria to predict adverse drug reactions among first-visit elderly outpatients. Pharmacotherapy 2005, 25, 831–838. [Google Scholar] [CrossRef]
- McGwin, G.; Sims, R.V.; Pulley, L.; Roseman, J.M. Relations among chronic medical conditions, medications, and automobile crashes in the elderly: A population-based case-control study. Am. J. Epidemiol 2000, 152, 424–431. [Google Scholar] [CrossRef]
- Hill, L.L.; Lauzon, V.L.; Winbrock, E.L.; Li, G.; Chihuri, S.; Lee, K.C. Depression, antidepressants and driving safety. Inj. Epidemiol. 2017, 4, 10. [Google Scholar] [CrossRef]
- Chihuri, S.; Li, G. Use of prescription opioids and motor vehicle crashes: A meta analysis. Accid. Anal. Prev. 2017, 109, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Charlesworth, C.J.; Smit, E.; Lee, D.S.H.; Alramadhan, F.; Odden, M.C. Polypharmacy among Adults Aged 65 Years and Older in the United States: 1988–2010. J. Gerontol. A Biol. Sci. Med. Sci. 2015, 70, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.B.; Hales, C.M.; Gu, Q.; Ogden, C.L. Prescription Drug Use in the United States, 2015–2016. NCHS Data Brief 2019, 1–8. [Google Scholar]
- Molnar, L.J.; Eby, D.W.; Bogard, S.E.; LeBlanc, D.J.; Zakrajsek, J.S. Using naturalistic driving data to better understand the driving exposure and patterns of older drivers. Traffic Inj. Prev. 2018, 19, S83–S88. [Google Scholar] [CrossRef]
- van Schagen, I.; Sagberg, F. The Potential Benefits of Naturalistic Driving for Road Safety Research: Theoretical and Empirical Considerations and Challenges for the Future. Procedia. Soc. Behav. Sci. 2012, 48, 692–701. [Google Scholar] [CrossRef]
- Guo, F.; Klauer, S.G.; Hankey, J.M.; Dingus, T.A. Near Crashes as Crash Surrogate for Naturalistic Driving Studies. Transp. Res. Rec. 2010. [Google Scholar] [CrossRef]
- Li, G.; Eby, D.W.; Santos, R.; Mielenz, T.J.; Molnar, L.J.; Strogatz, D.; Betz, M.E.; DiGuiseppi, C.; Ryan, L.H.; Jones, V.; et al. Longitudinal Research on Aging Drivers (LongROAD): Study design and methods. Inj. Epidemiol. 2017, 4, 22. [Google Scholar] [CrossRef]
- American Society of Health-System Pharmacists. AHFS Clinical Drug Information: AHFS Pharmacologic-Therapeutic Classification; American Society of Health-System Pharmacists: Bethesda, MD, USA, 2017. [Google Scholar]
- Hill, L.L.; Andrews, H.; Li, G.; DiGuiseppi, C.G.; Betz, M.E.; Strogatz, D.; Pepa, P.; Eby, D.W.; Merle, D.; Kelley-Baker, T.; et al. Medication use and driving patterns in older drivers: Preliminary findings from the LongROAD study. Inj. Epidemiol. 2020, 7, 38. [Google Scholar] [CrossRef]
- Keay, L.; Munoz, B.; Duncan, D.D.; Hahn, D.; Baldwin, K.; Turano, K.A.; Munro, C.A.; Bandeen-Roche, K.; West, S.K. Older drivers and rapid deceleration events: Salisbury Eye Evaluation Driving Study. Accid. Anal. Prev. 2013, 58, 279–285. [Google Scholar] [CrossRef]
- Klauer, S.G.; Guo, F.; Simons-Morton, B.G.; Ouimet, M.C.; Lee, S.E.; Dingus, T.A. Distracted driving and risk of road crashes among novice and experienced drivers. N. Engl. J. Med. 2014, 370, 54–59. [Google Scholar] [CrossRef]
- Wang, B.; Hallmark, S.; Savolainen, P.; Dong, J. Crashes and near-crashes on horizontal curves along rural two-lane highways: Analysis of naturalistic driving data. J. Safety Res. 2017, 63, 163–169. [Google Scholar] [CrossRef]
- Seacrist, T.; Douglas, E.C.; Huang, E.; Megariotis, J.; Prabahar, A.; Kashem, A.; Elzarka, A.; Haber, L.; MacKinney, T.; Loeb, H. Analysis of near crashes among teen, young adult, and experienced adult drivers using the SHRP2 naturalistic driving study. Traffic Inj. Prev. 2018, 19, S89–S96. [Google Scholar] [CrossRef]
- Strogatz, D.; Mielenz, T.J.; Johnson, A.K.; Baker, I.R.; Robinson, M.; Mebust, S.P.; Andrews, H.F.; Betz, M.E.; Eby, D.W.; Johnson, R.M.; et al. Importance of Driving and Potential Impact of Driving Cessation for Rural and Urban Older Adults. J. Rural. Health 2020, 36, 88–93. [Google Scholar] [CrossRef]
- Passarelli, M.C.G.; Jacob-Filho, W.; Figueras, A. Adverse drug reactions in an elderly hospitalised population: Inappropriate prescription is a leading cause. Drugs Aging 2005, 22, 767–777. [Google Scholar] [CrossRef]
- Jano, E.; Aparasu, R.R. Healthcare outcomes associated with beers’ criteria: A systematic review. Ann. Pharm. 2007, 41, 438–447. [Google Scholar] [CrossRef]
- Fu, A.Z.; Jiang, J.Z.; Reeves, J.H.; Fincham, J.E.; Liu, G.G.; Perri, M. Potentially inappropriate medication use and healthcare expenditures in the US community-dwelling elderly. Med. Care 2007, 45, 472–476. [Google Scholar] [CrossRef]
- Fick, D.M.; Mion, L.C.; Beers, M.H.; L Waller, J. Health outcomes associated with potentially inappropriate medication use in older adults. Res. Nurs. Health 2008, 31, 42–51. [Google Scholar] [CrossRef]
- Monteiro, L.; Maricoto, T.; Solha, I.; Ribeiro-Vaz, I.; Martins, C.; Monteiro-Soares, M. Reducing Potentially Inappropriate Prescriptions for Older Patients Using Computerized Decision Support Tools: Systematic Review. J. Med. Internet Res. 2019, 21, e15385. [Google Scholar] [CrossRef]
- Chihuri, S.; Mielenz, T.J.; DiMaggio, C.J.; Betz, M.E.; DiGuiseppi, C.; Jones, V.C.; Li, G. Driving Cessation and Health Outcomes in Older Adults. J. Am. Geriatr. Soc. 2016, 64, 332–341. [Google Scholar] [CrossRef]
- Kandasamy, D.; Betz, M.E.; DiGuiseppi, C.; Mielenz, T.J.; Eby, D.W.; Molnar, L.J.; Hill, L.; Strogatz, D.; Li, G. Self-reported health conditions and related driving reduction in older drivers. Occup. Ther. Health Care 2018, 32, 363–379. [Google Scholar] [CrossRef]
- Barbone, F.; McMahon, A.D.; Davey, P.G.; Morris, A.D.; Reid, I.C.; McDevitt, D.G.; MacDonald, T.M. Association of road-traffic accidents with benzodiazepine use. Lancet 1998, 352, 1331–1336. [Google Scholar] [CrossRef]
- Li, G.; Chihuri, S. Prescription opioids, alcohol and fatal motor vehicle crashes: A population-based case-control study. Inj. Epidemiol. 2019, 6, 11. [Google Scholar] [CrossRef]
- Chihuri, S.; Li, G. Use of Prescription Opioids and Initiation of Fatal 2-Vehicle Crashes. JAMA Netw. Open 2019, 2, e188081. [Google Scholar] [CrossRef] [PubMed]
- Bramness, J.G.; Skurtveit, S.; Neutel, C.I.; Mørland, J.; Engeland, A. Minor increase in risk of road traffic accidents after prescriptions of antidepressants: A study of population registry data in Norway. J. Clin. Psychiatry 2008, 69, 1099–1103. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Hilmer, S.N. Calculating and using the drug burden index score in research and practice. Expert Rev. Clin. Pharmacol. 2018, 11, 1053–1055. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).