Abstract
Polycyclic aromatic hydrocarbons (PAHs) are among the chemicals with proven impact on workers’ health. The use of human biomonitoring (HBM) to assess occupational exposure to PAHs has become more common in recent years, but the data generated need an overall view to make them more usable by regulators and policymakers. This comprehensive review, developed under the Human Biomonitoring for Europe (HBM4EU) Initiative, was based on the literature available from 2008–2022, aiming to present and discuss the information on occupational exposure to PAHs, in order to identify the strengths and limitations of exposure and effect biomarkers and the knowledge needs for regulation in the workplace. The most frequently used exposure biomarker is urinary 1-hydroxypyrene (1-OH-PYR), a metabolite of pyrene. As effect biomarkers, those based on the measurement of oxidative stress (urinary 8-oxo-dG adducts) and genotoxicity (blood DNA strand-breaks) are the most common. Overall, a need to advance new harmonized approaches both in data and sample collection and in the use of appropriate biomarkers in occupational studies to obtain reliable and comparable data on PAH exposure in different industrial sectors, was noted. Moreover, the use of effect biomarkers can assist to identify work environments or activities of high risk, thus enabling preventive risk mitigation and management measures.
1. Introduction
Polycyclic aromatic hydrocarbons (PAHs) are mostly formed during incomplete combustion of organic materials such as coal, coal-derived products, oil, and its by-products, natural gas, and wood [1]. Anthropogenic activities using these organic materials generate environmental air pollution, primarily in big cities where the increasing population requires a growth in the use of hydrocarbon-based fuels for transportation, heating systems, and electric power generation. To a lesser extent, PAHs are also produced by lifestyle habits (e.g., tobacco smoke and consumption of grilled food) and fires (e.g., wildland and structure fires). Although exposure to PAHs in the general population may raise some interest, occupational exposure raises the major concern because workers are frequently exposed to far higher concentrations and for longer periods of their lives [1,2,3].
Occupational exposure to PAHs occurs mainly in industrial sectors such as coking, impregnation processes with tar, creosote, and bitumen, aluminum production and smelting, asphalt industry, mining, metal working, oil refining, and also in non-industrial sectors such as firefighting [3]. PAHs can be absorbed by inhalation, ingestion, and via the skin [4]. Inhalation, followed by dermal contact, are the primary routes of workers exposure [5,6]. Absorption through inhalation is very quick and efficient, and upon exposure to pyrene, a pulmonary retention of 61% has been estimated [7]. High and efficient absorption of PAHs through human skin has been also demonstrated [8,9,10]. Once absorbed, PAHs are rapidly transported via the bloodstream and lymph to every tissue. Because of their lipophilic nature, PAHs can accumulate in adipose tissue, which may act as a depot from which the PAHs are released over time [11,12].
PAHs are metabolized primarily in the liver and kidney, through phase 1 and 2 reactions, such as oxidative, hydroxylation, reductive, and conjugative processes [13,14,15]. The first step of metabolism is always an epoxidation of the aromatic system by cytochrome P450 isoenzymes (CYP) [14]. The major transformation of any epoxide is the epoxide hydrolase catalyzed hydroxylation which results in a di-hydrodiol product. Besides hydroxylation, the epoxide can also undergo phase 2 reactions, e.g., the glutathione-S-transferase controlled addition to glutathione. These reactions result in the corresponding conjugates, which can easily be eliminated via urine ). On the other hand, epoxides can react spontaneously with nucleophilic reaction sites of macromolecules, like proteins and ribonucleic acids [14].
The most prominent PAHs metabolites are the mono-hydroxylated metabolites, which result from isomerization of the epoxides, and are potential target molecules for human biomonitoring (HBM) of PAHs exposure. The formation of these metabolites have been demonstrated for naphthalene (NAP), phenanthrene, fluorene, chrysene, pyrene, and benzo[a]pyrene (BaP) [16,17,18,19]. Also relevant are aldo-keto reductase (AKR) pathways. For example, 1,2-dihydroxynaphthalene, which results from the AKR pathways, is by far the main urinary metabolite of naphthalene [20]. This urinary metabolite has shown a strong correlation with environmental naphthalene exposure, which supports its use as a biomarker for the human biomonitoring of naphthalene exposure as an alternative for more commonly used 1- and 2-naphthol [20]. Pyrene is frequently found in PAH mixtures and its urinary metabolite, 1-hydroxypyrene (1-OH-PYR), has been commonly used as an indicator of exposure to PAHs [21,22]. Overall, many PAHs metabolites with potential for use as exposure biomarkers have been already identified [16,17,18,19], as follows: 1-hydroxynaphthalene (1-OH-NAP), 2-hydroxynaphthalene (2-OH-NAP), 1,2-dihydroxynaphthalene (1,2-OH-NAP), 2-hydroxyfluorene (2-OH-FLU), 3-hydroxyfluorene (3-OH-FLU), 9-hydroxyfluorene (9-OH-FLU), 1-hydroxyphenanthrene (1-OH-PHE), 2-hydroxyphenanthrene (2-OH-PHE), 3-hydroxyphenanthrene (3-OH-PHE), 4-hydroxyphenanthrene (4-OH-PHE), 1,2-dihydroxyphenanthrene (1,2-OH-PHE), 3,4-dihydroxyphenanthrene (3,4-OH-PHE), 9,10-dihydroxyphenanthrene (9,10-OH-PHE), 6-hydroxychrysene (6-OH-CHR), 1-hydroxypyrene (1-OH-PYR), 1,6-dihydroxypyrene (1,6-OH-PYR), 1,8-dihydroxypyrene (1,8-OH-PYR), 3-hydroxybenzo[a]pyrene (3-OH-BaP), 1-hydroxyacenaphtene (1-OH-ACE).
The elimination kinetics after inhalation, oral, and dermal absorption indicates a possible systemic accumulation of PAHs during consecutive exposure, which has been confirmed in several studies [23,24,25,26]. Data available concerning the kinetics of some PAHs metabolites are summarized in Supplementary Table S1.
PAHs are well known to be hazardous to human health. The main effect of PAH exposure is cancer, namely lung and skin cancer [27], and, to a lesser extent, non-cancer effects including cardiovascular [28,29,30] and dermal toxicity (reviewed in [31]).. Many PAHs are classified as probable or possible carcinogens according to the International Agency for Research on Cancer [32]. BaP is classified as carcinogenic (IARC group 1), as well as some PAH mixtures, for example, soot [33], diesel engine exhaust [34], and outdoor air pollution [35]. PAHs can also act as endocrine disruptors [36]. Due to their carcinogenicity, the presence of PAHs in several consumer products is restricted in the European Union. Some PAHs congeners are included in the List of substances of very high concern (SVHC) for possible future Authorization in accordance with Article 59 (10) of the REACH Regulation [37]. Carcinogenic PAH mixtures have been also included in EU directive 2004/37/EC on the protection of workers from the risks related to exposure to carcinogens or mutagens at work, with a skin notation due to the possibility of significant uptake through the skin. However, no binding OEL has been adopted for PAHs or BaP at the EU level.
In order to warrant safe exposure levels, monitoring PAHs is usually performed by means of stationary or personal air-sampling at the workplace, which allows characterizing external exposure and inferring workers’ exposure via inhalation. However, biomarkers of PAHs exposure measured in urine or blood, allow the assessment of the aggregated internal exposure level achieved by inhalation, dermal and gastrointestinal routes. Most of the air monitoring methods available for measuring workplace exposure to PAHs allow the measurement of the 16 priority PAHs (e.g., NIOSH method 5528; https://www.cdc.gov/niosh/nmam/pdf/5528.pdf (accessed on 27 June 2022)). There are no EU-wide biological limit values (BLV) for PAHs. The Scientific Committee on Occupational Exposure Limits (SCOEL) concluded in its opinion published in 2016 that 1-OH-PYR represents the main metabolite of pyrene in mammals and has become accepted as a sensitive and specific marker of PAHs exposure, for which reliable and robust analytical methods are described [28]. However, since PAHs were considered non-threshold carcinogens, no health-based BLV were given, but a biomonitoring guidance value (BGV) of 0.5 µg 1-OH-PYR per g creatinine (determined after conjugate hydrolysis) was proposed to identify occupational exposure from background general population exposure level.
In this work, we describe a systematic review of the literature published between 2008 and 2022 on occupational exposure to PAHs in Europe, developed under the H2020 European Human Biomonitoring Initiative (HBM4EU). An overview of the use of human biomonitoring data is presented, including the HBM parameters applied in occupational studies on PAHs exposure and effects, PAHs metabolites levels reported, and the occupational settings where workers incur in the greatest risk. The knowledge gaps in HBM studies concerning PAHs are identified and the most common and suitable effect biomarkers to assess early biological effects are also discussed.
2. Materials and Methods
2.1. Search Strategy for Papers Concerning HBM of Occupational PAHs Exposure
A systematic literature search on the use of HBM in occupational exposure to PAHs studies was conducted. Papers published between 2008 and March 2022, from different sources, were used: PubMed, Web of Science, and Scopus and were evaluated according to the PRISMA methodology [38]. An outline of the different phases of the search, together with the number of papers identified, can be found in the results section.
At the first stage, broad search terms and filters were defined to identify occupational studies that used human biomonitoring to evaluate exposure to PAHs (Table 1).

Table 1.
Search terms used in the different literature databases.
After the initial removal of duplicates by one member of the team, all retrieved titles and abstracts were independently screened, in parallel by four members of the team, using previously established inclusion/exclusion criteria (Table 2). Articles that did not meet the inclusion criteria were excluded from further analysis.

Table 2.
Inclusion and exclusion criteria for the literature search.
In this search, occupational HBM studies performed in different activity sectors where exposure to PAHs can occur were included. All types of studies were considered (cross-sectional, cohort, and case-control studies), and no minimum limit on the number of individuals included in the study was set. Non-epidemiological studies, e.g., studies on analytical methods and new biomarkers, were excluded.
2.2. Quality Scoring of the Articles Retrieved
The quality of each study in regard to our purpose was assessed using a modification of the LaKind scoring method [39]. Briefly, the scoring method was based on quality criteria for three fundamental areas of epidemiological studies that include biological measurements of short-lived chemicals: (1) biomarker selection and measurement; (2) study design and execution; and (3) general epidemiological study design considerations. In Table 3, the components analyzed within these areas are shown. A value from 1 to 3 was assigned to each parameter, where 1 is the best in the quality criteria score.

Table 3.
Adaptation of LaKind scoring method to HBM studies concerning PAHs.
One of the aims of the H2020 European Human Biomonitoring Initiative (HBM4EU) was the development of the field of effect biomarkers to implement them in a more systematic and harmonized way in large-scale European HBM studies. The implementation of effect biomarkers complements exposure data with mechanistically based biomarkers of early and late adverse effects. Therefore, information about the effect biomarkers used and results obtained was also collected from the articles retrieved, following the literature search conducted according to criteria presented in Table 1 and Table 2.
3. Results
3.1. Literature Search and LaKind Scoring
The search strategy for exposure assessment in HBM studies led to the identification of 369 articles in total, including 227 from PubMed, 53 from Web of Science, and 89 from Scopus. Of these 369 articles, 42 were eligible to be included in this review (Figure 1).
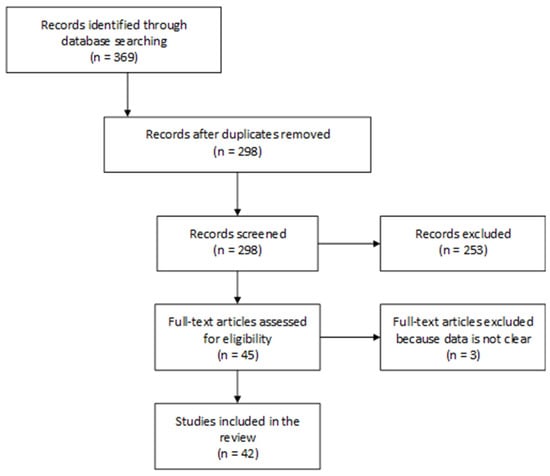
Figure 1.
Diagram showing the different phases in the HBM studies selection in this review.
The results of the LaKind scoring that was applied to the 42 studies selected for review (Supplementary Table S2) showed that the highest score (lowest quality) obtained was 18 [40] and the lowest score (highest quality) was 10 [41]. This scoring system is not a judgment of the scientific quality of the paper, but it is rather an assessment of to which degree it answers the questions raised in this review. Many studies scored poorly on quality assurance parameters; this is not to say that studies were poorly conducted but highlights that still today many studies do not adequately report their use of quality control and quality assurance procedures. Although the poorer scoring papers were older, indicating an improvement in reporting in recent years, there were still high-quality data papers across the date range.
3.2. Exposure Biomarkers and Occupational Exposure (Limit) Values
Among the 42 articles eligible in this study, the main occupational settings focused were firefighting, coke oven, asphalt/bitumen/rode paving, metallurgic and electrode industries, aluminum production, waste incineration, restaurant workers, policemen, drivers, and nurses involved in the topical application of coal tar ointment. Additionally, air force personnel, green spaces workers and roofers, navy workers as well as health care workers were also reported (Table 4).

Table 4.
Summary of exposure biomarkers identified in occupational exposure to PAHs as reported in the studies of interest to the present review.
Table 4 summarizes the biomarkers of exposure to PAHs as reported in the occupational studies included in the present review. PAHs include a mixture of multiple substances and thereby typically one or a few representative PAHs metabolites have been used as urinary markers in biomonitoring studies. The most frequently used biomarkers were: 1-OH-PYR (32 out of 42 studies) followed by 3-hydroxyBaP (3-OH-BaP) (7 out of 42 studies). These two exposure biomarkers were used in the study showing the best score by the Lakind scoring [41]. In addition, other biomarkers have been used, namely, 1-hydroxynaphthalene (i.e., 1-naphthol, 1-OH-NAP); 2-hydroxynaphthalene (2-naphthol, 2-OH-NAP); 2-hydroxyfluorene (2-OH-FLU); 9-hydroxyfluorene (9-OH-FLU); 1-hydroxyphenanthrene (1-OH-PHE); 2-hydroxyphenanthrene (2-OH-PHE); 3-hydroxyphenanthrene (3-OH-PHE); 4-hydroxyphenanthrene (4-OH-PHE); 9-hydroxyphenanthrene (9-OH-PHE) and 6-hydroxychrysene (6-OH-CHR) (Table 4).
Regarding external exposure, the exposure levels of individual PAHs in air vary according to the industry sector. Not all studies eligible for this review analyzed the potential associations between PAHs detected in air and the biomarkers of exposure used. The most detected PAHs in French metallurgic industries were Pyr, BaP, Nap, Flu, and Phe [43,44]. In those studies, 1-OH-PYR correlated with gaseous Pyr and particle Pyr, whereas 3-OH-BaP did not correlate with the measured BaP air levels [43,44]. In another study, the same authors reported a weak correlation of 1-OH-NAP, 2-OH-NAP, 1-OH-PHE and 3-OH-PHE with workplace air levels of parent PAHs and a strong correlation of 2-OH-FLU, 3-OH-FLU, and 2-OH-PHE with air levels of their parents’ PAHs [44]. Using the same air markers, three studies have shown a correlation between PAHs levels in air samples and metabolites in urine [45,47,48]. In fact, Förster et al. [45] also reported correlations between urinary levels of 3-OH-BaP and ∑OH-PHEs and 1-OH-PYR, proving that in metallurgic industries, these three hydroxylated PAHs can be surrogates of each other. Regarding asphalt industries, the majority of studies that measured PAHs in the air and exposure biomarkers were performed in Germany [49,50,53]. All studies measured the 16 US EPA PAHs in air and as biomarkers of exposure, the authors used 1-OH-PYR, ∑OH-PHE and ∑OH-NAP. The authors have not shown a correlation between air concentrations and urinary biomarkers since post-shift urinary PAHs metabolites concentrations did not reflect the different exposure levels. In other industries, such as coke oven [58] and aluminum production [46] the PAHs markers used for air monitoring were ∑PAHs and BaP. Zając et al. reported a correlation between 1-OH-PYR, ∑PAHs, and BaP, showing that 1-OH-PYR might be a surrogate for BaP and PAHs in general [58]. Furthermore, 1-OH-PYR levels in urine showed a wide distribution across different studies (Figure 2) reflecting wide ranges of exposure, either related to air or to other exposure routes, such as dermal exposure.
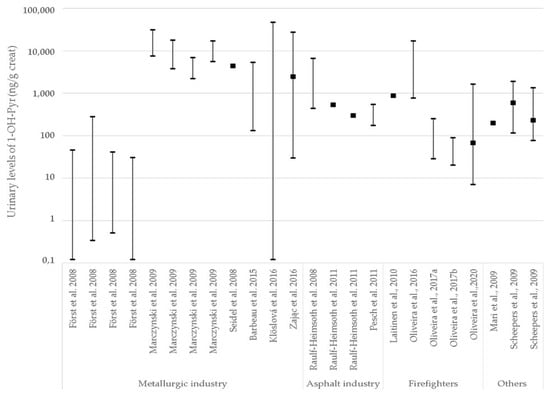
Figure 2.
Urinary levels distribution of 1-OH-PYR across several industries in the literature. Creat: creatinine. Minimum and maximum values are shown together with median/mean (black square) whenever available. The y-axis is depicted in logarithmic scale.
In this sense, in two German studies of workers in different industries with high PAHs exposures, exposure was assessed both by measuring air PAHs concentrations and PAHs metabolites in urine [47,52]. The authors discuss that the observed lack of association between air concentrations of PAHs and the urinary PAHs metabolite levels indicates that other routes of exposure, in addition to inhalation of PAHs, are of importance [47].
The above studies show that PAHs uptake through the dermal route may be significant, thus favoring the use of biomonitoring data for the assessment of occupational PAH exposure in addition to air measurements.
Monohydroxylated PAH metabolites in urine, mostly 1-OH-PYR and also the five hydroxyphenanthrenes (1-, 2-, 3-, 4-, and 9-OH-PHE), have been widely accepted as reliable biomarkers for internal exposure to PAHs [81]. Among the studies reviewed, they were extensively used for the estimation of PAHs exposure in different work sectors, e.g., steel production and coke plants [45,47,48,58], waste incinerators [63,64], asphalt workers [49,53], policemen [73], firefighters [40,65], and dermatology nurses [77].
3.3. Effect Biomarkers
Among the 42 studies selected for the present review, eleven studies reported the use of effect biomarkers in occupational exposure to PAHs [6,47,50,51,52,69,70,73,74,75,76,79]. The reported effect biomarkers primarily included markers of genotoxicity/oxidative stress (nine studies) and cardiovascular effects (six studies). An overview of these studies is presented in Table 5 and Table 6.

Table 5.
Summary of reported effects related to genotoxicity/oxidative stress.

Table 6.
Summary of reported effects related to cardiovascular effects.
Nine of the studies focused on DNA damage: (1) oxidative damage of DNA or RNA, (2) DNA strand breaks, and/or (3) micronuclei (Table 5). The most frequent biomarker of genotoxic/oxidative damage used was DNA strand breaks (five studies), followed by 8-oxodG levels in either blood or urine (3 studies) and formamidopyrimidine DNA glycosylase (Fpg)-sensitive sites in PBMC (2 studies), respectively. In addition, 8-oxoGuo, 8-OHdG, and micronuclei were analyzed in a single study each. A strong correlation between urinary OH-PYR, dermal PAH exposure, and DNA strand breaks in the blood was found in the study of recruits during training as firefighters [6].
The 8-oxodG levels were increased in bus drivers (n = 50) compared to controls (n = 50) in a Czech cross-sectional study. Neither personal nor stationary air concentrations of PAHs, B(a)P or VOC correlated with the 8-oxodG levels. Instead, the 8-oxodG levels correlated with PM2.5 and PM10 concentrations [74]. Increased levels of 8-oxo-dG and DNA strand breaks compared to the control group were observed in coke oven (n = 37), refractory (n = 96), graphite electrode (n = 26), and converter workers (n = 12) as compared to a control group consisting of construction workers (n = 48) in a German cross-sectional study [47]. The highest levels of DNA damage were observed for the graphite-electrode production workers. DNA damage levels were not associated with PAHs exposure measured as air PAHs concentrations or urinary PAHs metabolite levels [47].
Furthermore, increased levels of 8-oxo-dGua adducts and DNA strand breaks were found in bitumen-exposed construction workers (both pre- and post-shift). The level of 8-oxo-Gua was increased post- compared to pre-shift, whereas the level of DNA strand breaks was decreased post- compared to pre-shift. No difference between the levels of (+)-anti-BPDE-DNA adducts in exposed and control samples was observed. No association between exposure to PAHs (measured as urinary metabolites of PAHs or air concentration of PAH) and DNA damage in blood cells was found [52]. Moreover, increased levels of 8-OHdG in second-hand tobacco smoke-exposed workers from Portuguese restaurants were observed compared to non-exposed workers, regardless of smoking status [79]. Proteomics analysis showed nine differentially expressed proteins in plasma of second-hand tobacco smoke-exposed non-smokers. Among these, two acute phase proteins inter-α-trypsin inhibitor heavy chain 4 (ITIH4) and ceruloplasmin (CP) were the most differentially expressed proteins [79]. Genotoxicity effect biomarkers were also used and no clear association between occupational exposure to second-hand smoke and the induction of genotoxicity was observed, although the leukocytes from non-smoking second-hand tobacco smoke-exposed individuals displayed lower DNA damage levels in response to an ex vivo challenge, in comparison to those from non-exposed workers, suggesting a possible adaptive response [82].
The biomarkers of genotoxicity used in the selected studies are on the list of identified effect biomarkers for BaP identified by IARC [33]. In addition to DNA damage (measured by the comet assay) and 8-oxo-deoxyguanosine formation, IARC also lists chromosomal aberrations and sister chromatid exchange as biomarkers of genotoxicity.
Four out of the described studies, indicated increased ROS production and genotoxicity, in workers exposed to PAHs compared to controls, but did not find a correlation between PAHs exposure and genotoxicity [47,52,74,79].
Six studies also included biomarkers of cardiovascular effects (Table 6), three of them analyzing different acute-phase proteins (SAA, CRP, ITIH4, and CP) and/or inflammatory markers (Il-6, IL-8, V-CAM, and I-CAM) without noticing significant increases in the exposed population [6,69,79]. One study found that 1-OH-PYR was negatively associated with systolic and diastolic BP [73], while another study found decreased microvascular function and altered heart rate variability indicating an imbalance in the autonomic activation of the heart [69].
4. Discussion
4.1. Strengths and Limitations of the Strategies Used for HBM of PAHs
Choosing the most appropriate biomarkers to realistically describe the exposure to PAH mixture in each occupational setting is of most importance since health effects depend not only on the PAHs levels but also on the mixture composition. However, this will also require the development of risk assessment models for the interpretation of the impact of varying compositions on the risks of PAH mixtures since the current dose responses for PAH mixtures are based on BaP as an indicator of exposure.
This literature review revealed that most of the selected studies use BaP as a marker for general airborne PAH exposure, justified mainly for practical reasons [28]. However, for some occupational settings, BaP may not be the appropriate indicator of exposure to these compounds. In addition, there are occupational scenarios where airborne PAH exposure is dominated by PAHs of lower ring number, such as naphthalene, anthracene, and phenanthrene [83]. It would therefore be preferable to monitor a broad spectrum of PAH components or at least total PAH exposure, as the relative abundance of other PAHs with adverse effects on human health may vary depending on the occupational setting. When the content of the PAH mixture is unknown, exposure to the 16 priority PAHs should be assessed.
The 1-OH-PYR, the pyrene metabolite, was the most widely used exposure biomarker in the reviewed occupational studies, although it is only an indirect marker of exposure to carcinogenic PAHs, including BaP. Nevertheless, the relative content of pyrene compared to other PAHs is well-studied and fairly constant in air samples from working environments [81]. Moreover, a good correlation between airborne BaP and post-shift urine levels of 1-OH-PYR has been reported (if samples from workers using respiratory protection or with significant dermal exposure were excluded) [84]. The combination of highly sensitive and relatively cheap detection methods (e.g., urinary 1-OH-PYR) and evidence of linear correlation with airborne exposure suggests 1-OH-PYR as a robust biological exposure biomarker [81]. However, the use of PYR and PHE metabolites to assess the carcinogenic risk associated with occupational exposure to PAHs has been questioned [32]. Recently, new biomarkers have been implemented that can provide information on exposure to PAHs of greater toxicological relevance than pyrene, such as 3-OH-BaP, the main urinary metabolite of BaP [85]. Several aspects, however, may negatively affect the routine use of 3-OH-BaP as a reliable biomarker of occupational PAHs exposure. The predominance of the fecal over the urinary excretion pathway for BaP metabolite contributes to very low urinary 3-OH-BaP levels, which requires particularly highly sensitive analytical procedures. Therefore, most studies using 3-OH-BaP are mainly exposure scenarios entailing high occupational exposure, such as those observed among metallurgy workers [41,42] and firefighters [67]. A very recent work analyzed the consistency between air and biological monitoring for PAHs exposure and cancer risk of workers, suggesting an overall agreement between airborne PAH levels and urinary biomarker concentrations [86]. The use of urinary 1-OH-PYR seemed to be more protective than those of urinary 3-OH-BaP and air BaP [86].
The study design of biomonitoring studies may greatly impact the statistical power to detect the effects of exposure. Longitudinal and cross-shift studies, where the volunteers act as their own controls, eliminate the contribution from inter-individual variation as compared to cross-sectional studies. Furthermore, using healthy volunteers or previously unexposed persons may also improve the ability to detect the effects of occupational exposure to PAHs, because occupationally exposed persons (such as firefighters) may have increased pre-shift levels of PAHs due to previous exposures [6]. Needless to say, the number of persons recruited in the studies is an extremely important determinant for the statistical power of a study. Pooled studies across Europe have greatly increased the statistical power as seen in the studies of occupational exposure to hexavalent chrome [87]. In the HBM4EU studies, the study design and detection methods were harmonized to ensure comparability of the biomonitoring data. For PAHs detection, several different methods for quantification were used in the studies reported in this review, and it is not clear whether these are entirely comparable.
The exposure of humans to NAP has also become an environmental and occupational health concern since international agencies classify NAP as a possible human carcinogen [33]. Monohydroxylated metabolites (1- and 2-OH-NAP) have been widely used as biomarkers for the assessment of occupational exposure to NAP at different workplaces [44,53,55,67]. However, the high background levels found in non-occupationally exposed populations and in non-smoker urine samples give rise to doubts about their specificity as occupational biomarkers; 1-OH-NAP is also not specific to naphthalene exposure as it can be formed from carbaryl exposure [88]. Klotz et al., evaluated the suitability of several NAP metabolites, including 1- and 2-OH-NAP, for their application in biomonitoring studies [60]. The dihydroxylated metabolite 1,2-OH-NAP was found to be the most sensitive and 1-naphthylmercapturic acid, the most specific biomarker for biological monitoring of occupational exposure to NAP. However, to date, the latter has not been widely used [60].
The use of effect biomarkers in biomonitoring studies, including occupational studies, is useful for the early identification of subclinical diseases. More importantly, the establishment of relationships between PAHs exposure and biomarkers of effect can be used for risk assessment, as well as for the establishment of exposure limits, both in the occupational and general environment [5]. This review showed that, for genotoxicity, chromosomal aberrations, sister chromatid exchange, DNA damage measured by the comet assay, 8-oxo-deoxyguanosine formation, and micronuclei are established human effect biomarkers in relation to exposure to BaP-containing mixtures, in line with IARC view [32,87]. A review evaluated the effect of PAHs exposure on micronuclei induction in 34 occupational studies showing that the micronucleus assay may be a sensitive biomarker of PAHs exposure in contaminated workplaces [89]. Furthermore, experimental studies with rodents exposed to BaP or anti-BaP-7,8-diol-9,10-oxide support this association [33].
Among the limitations of the search performed, it should be noted that the selected articles included mainly biomarkers of genotoxicity, oxidative stress, and cardiovascular effects, ignoring other effect biomarkers of interest (e.g., proteomic, metabolic, or endocrine disrupting markers), to evaluate the effect of PAHs [90,91,92].
Assessing exposure to PAHs by measuring only airborne concentrations is one of the main limitations found, as other uptake pathways can considerably contribute to internal PAHs exposure to these pollutants [79]. Thus, the importance of the dermal route of PAHs uptake has again been shown in three recent studies of individuals engaged in firefighting [70], where a statistically significant correlation between dermal PAHs exposure and urinary PAHs metabolites was observed [6,71,93]. These studies also showed that firefighting was associated with increased levels of DNA strand breaks in blood cells and increased urinary mutagenicity, compared to controls [6,93]. Moreover, the study by Andersen et al. reported statistically significant correlations between urinary PAHs metabolite levels and DNA damage levels in blood cells, and between dermal exposure to pyrene and ƩPAHs and DNA damage levels [6], suggesting that dermal PAHs exposure contributed to the observed genotoxicity. Genotoxic effects have also been demonstrated following dermal exposure to PAHs in hairless mice [94].
Five of the 11 studies selected with effect biomarkers, focused on biomarkers of cardiovascular disease, specifically the association between PAHs exposure and blood pressure [29,72]. Furthermore, biomarkers of oxidative stress and acute phase response in restaurant workers exposed to second-hand smoke suggested that acute phase proteins, CP and ITIH4, could be candidate biomarkers to monitor second-hand smoke exposure of hospitality workers [79]. In fact, the acute phase response has already been proposed as a possible mechanism of particle-induced cardiovascular disease [95,96,97]. Serum levels of the acute phase proteins C-reactive protein (CRP) and serum amyloid A (SAA) have also been associated with an increased risk of cardiovascular disease in prospective epidemiological studies [98], just as SAA has also been shown to promote atherosclerotic plaque progression, suggesting a causal role in this disease [99].
4.2. HBM Added Value, Gaps and Needs for New Data
A major advantage of HBM data is that it provides an integrated overview of the body burden to selected chemicals and serves as a good estimate of aggregate exposure. In addition, inter-individual variation in uptake, metabolism, and excretion is taken into account. Where respiratory protective equipment (RPE) is worn (e.g., coke ovens), biomonitoring can give an insight into the efficacy of the RPE used and how it is being used. Furthermore, the importance of using biomonitoring tools in occupational exposures to PAHs is justified because these substances are known to be absorbed through the skin and the levels of urinary 1-OH-PYR are particularly high in occupationally exposed populations where dermal exposure is likely [10,100]. However, the dermal exposure route seems to imply a later peak of urinary excretion when compared with the respiratory route with possible continued absorption due to the continuous contact with contaminated clothes and expected penetrating of skin layers and deposit effect [101]. Therefore, and to allow for a correct interpretation of biomonitoring data, a detailed description of the tasks carried out, the duration of tasks, the possible dermal contamination, and the personal protective equipment worn is also needed [100,102].
However, HBM studies should be standardized allowing a more accurate comparison of the PAHs levels across studies and also a more homogeneous publication of the data. This, in turn, requires the use of individual HBM data, accompanied by ancillary information that would shed light on the mechanistic link between exposure dynamics and observed HBM data. This will allow a much better comparison and allow derivation of reference values-based regulations. In fact, at the moment, many studies in Europe use different approaches that in many cases could not be directly comparable.
It seems relevant when developing new occupational studies with harmonized approaches, to apply a set of exposure biomarkers that can be related to the PAHs mixture present in the setting being studied, rather than focusing only on BaP, especially since there is evidence that PAHs exposure is associated not only with cancer risk but also additional health outcomes such as cardiovascular disease. Within HBM4EU, the exposure biomarkers selected for general population studies have been discussed and the most frequently detected monohydroxy-PAHs, 1- and 2-OH-NAP, 1-OH-PYR, 2-, 3-, and 9-OH-FLU and 1-, 2-, 3- 4, and 9-OH-PHE, were selected [103]. A number of European labs underwent a quality assurance process and were qualified for the analysis of these metabolites [103].
Future development of a proposal for a biomonitoring strategy of PAHs to be used in occupational settings, including a specific flowchart considering the exposure scenarios specificity, can be defined based on the information presented here. The approach followed in previous papers for other chemicals of concern [104,105,106] is a good example to consider for PAHs. In addition, effect biomarkers, e.g., indicators of genotoxic and carcinogenic effects or of cardiovascular effects may help early identifying biological alterations and thereby a risk of disease that can be prevented through risk management measures before disease development.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/toxics10080480/s1, Table S1: Kinetic characteristics (tmax: time to maximal value after administration; t1/2: urinary elimination half-life) of urinary PAH metabolite elimination after oral, inhalation and dermal exposure; Table S2: Results of the Lakind scoring (excluding effect biomarkers) of the publications considering the aim of this study. Each category was scored out of 3, the lower scores indicating the better quality.
Author Contributions
Conceptualization, M.J.S.; methodology, B.C.G., H.L., C.V., A.L.I., A.T.S., U.V., K.J.; validation, T.G., A.K., C.M.N., A.O., R.C.D.; investigation, R.C.D., M.F.F., N.O., T.S., S.V., M.J.S.; writing—original draft preparation, B.C.G., H.L., S.V., A.T.S., M.J.S.; writing—review and editing, All authors; supervision, M.J.S. All authors have read and agreed to the published version of the manuscript. Please turn to the CrediT taxonomy for the term explanation. Authorship must be limited to those who have contributed substantially to the work reported.
Funding
This project has received funding from the European Unions’ Horizon 2020 research and innovation Programme under grant agreement No 733032. HBM4EU.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kim, K.-H.; Jahan, S.A.; Kabir, E.; Brown, R.J.C. A review of airborne polycyclic aromatic hydrocarbons (PAHs) and their human health effects. Environ. Int. 2013, 60, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Samburova, V.; Zielinska, B.; Khlystov, A. Do 16 Polycyclic Aromatic Hydrocarbons Represent PAH Air Toxicity? Toxics 2017, 5, 17. [Google Scholar] [CrossRef] [PubMed]
- Kamal, A.; Cincinelli, A.; Martellini, T.; Malik, R.N. A review of PAH exposure from the combustion of biomass fuel and their less surveyed effect on the blood parameters. Environ. Sci. Pollut. Res. 2015, 22, 4076–4098. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, A. Polycyclic aromatic hydrocarbons, carcinogenic (PAH) [MAK Value Documentation, 2012]. In The MAK-Collection for Occupational Health and Safety; Wiley-VCH: Hoboken, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Jongeneelen, F.J. A guidance value of 1-hydroxypyrene in urine in view of acceptable occupational exposure to polycyclic aromatic hydrocarbons. Toxicol. Lett. 2014, 231, 239–248. [Google Scholar] [CrossRef] [PubMed]
- Andersen, M.H.G.; Saber, A.T.; Pedersen, J.E.; Pedersen, P.B.; Clausen, P.A.; Løhr, M.; Kermanizadeh, A.; Loft, S.; Ebbehøj, N.E.; Hansen, M.; et al. Assessment of polycyclic aromatic hydrocarbon exposure, lung function, systemic inflammation, and genotoxicity in peripheral blood mononuclear cells from firefighters before and after a work shift. Environ. Mol. Mutagen. 2018, 59, 539–548. [Google Scholar] [CrossRef]
- Brzeźnicki, S.; Jakubowski, M.; Czerski, B. Elimination of 1-hydroxypyrene after human volunteer exposure to polycyclic aromatic hydrocarbons. Environ. Mol. Mutagen. 1997, 70, 257–260. [Google Scholar] [CrossRef]
- Elovaara, E.; Heikkila, P.; Pyy, L.; Mutanen, P.; Riihimaki, V. Significance of dermal and respiratory uptake in creosote workers: Exposure to polycyclic aromatic hydrocarbons and urinary excretion of 1-hydroxypyrene. Occup. Environ. Med. 1995, 52, 196–203. [Google Scholar] [CrossRef]
- VanRooij, J.G.; Bodelier-Bade, M.M.; Jongeneelen, F.J. Estimation of individual dermal and respiratory uptake of polycyclic aromatic hydrocarbons in 12 coke oven workers. Occup. Environ. Med. 1993, 50, 623–632. [Google Scholar] [CrossRef]
- Van Rooij, J.G.; Van Lieshout, E.M.; Bodelier-Bade, M.M.; Jongeneelen, F.J. Effect of the reduction of skin contamination on the internal dose of creosote workers exposed to polycyclic aromatic hydrocarbons. Scand. J. Work. Environ. Health 1993, 19, 200–207. [Google Scholar] [CrossRef]
- Mitchell, C. Distribution and retention of benzo(a)pyrene in rats after inhalation. Toxicol. Lett. 1982, 11, 35–42. [Google Scholar] [CrossRef]
- Withey, J.R.; Shedden, J.; Law, F.C.P.; Abedini, S. Distribution of benzo[a]pyrene in pregnant rats following inhalation exposure and a comparison with similar data obtained with pyrene. J. Appl. Toxicol. 1993, 13, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Guengerich, F.P. Metabolism of chemical carcinogens. Carcinogenesis 2000, 21, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, B.; Chu, C.; Carlin, D.J. Polycyclic Aromatic Hydrocarbons: From Metabolism to Lung Cancer. Toxicol. Sci. 2015, 145, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Shimada, T. Xenobiotic-Metabolizing Enzymes Involved in Activation and Detoxification of Carcinogenic Polycyclic Aromatic Hydrocarbons. Drug Metab. Pharmacokinet. 2006, 21, 257–276. [Google Scholar] [CrossRef]
- Barbeau, D.; Lutier, S.; Bonneterre, V.; Persoons, R.; Marques, M.; Herve, C.; Maitre, A. Occupational exposure to polycyclic aromatic hydrocarbons: Relations between atmospheric mixtures, urinary metabolites and sampling times. Int. Arch. Occup. Environ. Health 2015, 88, 1119–1129. [Google Scholar] [CrossRef]
- Li, Z.; Sandau, C.D.; Romanoff, L.C.; Caudill, S.P.; Sjodin, A.; Needham, L.L.; Patterson, D.G. Concentration and profile of 22 urinary polycyclic aromatic hydrocarbon metabolites in the US population. Environ. Res. 2008, 107, 320–331. [Google Scholar] [CrossRef]
- Motorykin, O.; Schrlau, J.; Jia, Y.; Harper, B.; Harris, S.; Harding, A.; Stone, D.; Kile, M.; Sudakin, D.; Simonich, S.L.M. Determination of parent and hydroxy PAHs in personal PM2.5 and urine samples collected during Native American fish smoking activities. Sci. Total Environ. 2015, 505, 694–703. [Google Scholar] [CrossRef]
- Urbancova, K.; Lankova, D.; Rossner, P.; Rossnerova, A.; Svecova, V.; Tomaniova, M.; Veleminsky, M.; Sram, R.J.; Hajslova, J.; Pulkrabova, J. Evaluation of 11 polycyclic aromatic hydrocarbon metabolites in urine of Czech mothers and newborns. Sci. Total Environ. 2016, 577, 212–219. [Google Scholar] [CrossRef]
- Klotz, K.; Weiß, T.; Zobel, M.; Bury, D.; Breuer, D.; Werner, S.; Sucker, K.; Zschiesche, W.; Göen, T.; Brüning, T.; et al. Validity of different biomonitoring parameters in human urine for the assessment of occupational exposure to naphthalene. Arch. Toxicol. 2019, 93, 2185–2195. [Google Scholar] [CrossRef]
- Granella, M.; Clonfero, E. Urinary excretion of 1-pyrenol in automotive repair workers. Int. Arch. Occup. Environ. Health 1993, 65, 241–245. [Google Scholar] [CrossRef]
- Santella, R.M.; Hemminki, K.; Tang, D.L.; Paik, M.; Ottman, R.; Young, T.L.; Savela, K.; Vodickova, L.; Dickey, C.; Whyatt, R.; et al. Polycy-clic aromatic hydrocarbon-DNA adducts in white blood cells and urinary 1-hydroxypyrene in foundry workers. Cancer Epidemiol Biomarkers Prev. 1993, 2, 59–62. [Google Scholar] [PubMed]
- Bentsen, R. The effect of dust-protective respirator mask and the relevance of work category on urinary 1-hydroxypyrene concentration in PAH exposed electrode paste plant workers. Ann. Occup. Hyg. 1998, 42, 135–144. [Google Scholar] [CrossRef]
- Jongeneelen, F.J.; Anzion, R.B.M.; Scheepers, P.T.J.; Bos, R.P.; Henderson, P.T.; Nijenhuis, E.H.; Veenstra, S.J.; Brouns, R.M.E.; Winkes, A. 1-hydroxypyrene in urine as a biological indicator of exposure to polycyclic aromatic hydrocarbons in several work environments *. Ann. Occup. Hyg. 1988, 32, 35–43. [Google Scholar] [CrossRef]
- Quinlan, R.; Kowalczyk, G.; Gardiner, K.; Calvert, I.; Hale, K.; Walton, S. Polycyclic aromatic hydrocarbon exposure in coal liquefaction workers: The value of urinary 1-hydroxypyrene excretion in the development of occupational hygiene control strategies. Ann. Occup. Hyg. 1995, 39, 329–346. [Google Scholar] [CrossRef]
- Viau, C. The toxicokinetics of pyrene and its metabolites in rats. Toxicol. Lett. 1999, 108, 201–207. [Google Scholar] [CrossRef]
- Kroese, E.D.; Muller, J.J.A.; Mohn, G.R.; Dortant, P.M.; Wester, P.W. Tumorigenic Effects in Wistar Rats Orally Administered Benzo[a]pyrene for Two Years (Gavage Studies): Implications for Human Cancer Risks Associated with Oral Exposure to Polycyclic Aromatic Hydrocarbons; (658603 010); National Institute for Public Health and the Environment (RIVM): Bilthoven, The Netherlands, 2001; Available online: http://www.rivm.nl/bibliotheek/rapporten/658603010.pdf (accessed on 28 March 2022).
- European Commission; Directorate-General for Employment; Social Affairs and Inclusion; Heederik, D.; Papameletiou, D.; Bolt, H.; Klein, C.L. SCOEL/REC/404 Polycyclic Aromatic Hydrocarbon Mixtures Containing Benzoapyrene (PAH): Recommendation from the from the Scientific Committee on Occupational Exposure Limits; Publications Office of the European Union: Luxembourg, 2016. [Google Scholar] [CrossRef]
- Alhamdow, A.; Lindh, C.; Albin, M.; Gustavsson, P.; Tinnerberg, H.; Broberg, K. Early markers of cardiovascular disease are associated with occupational exposure to polycyclic aromatic hydrocarbons. Sci. Rep. 2017, 7, 9426. [Google Scholar] [CrossRef]
- Alshaarawy, O.; Zhu, M.; Ducatman, A.; Conway, B.; Andrew, M.E. Polycyclic aromatic hydrocarbon biomarkers and serum markers of inflammation. A positive association that is more evident in men. Environ. Res. 2013, 126, 98–104. [Google Scholar] [CrossRef]
- European Commission. Scientific Committee on Food Opinion of the Scientific Committee on Food on the Tolerable Upper Intake Level of Iodine (Brussels). SCF/CS/NUT/GEN/18 Final. 2003. Available online: https://ec.europa.eu/food/system/files/2020-12/sci-com_scf_out171_en.pdf (accessed on 28 March 2022).
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Some traditional herbal medicines, some mycotoxins, naphthalene and styrene. IARC Monogr. Eval. Carcinog. Risks Hum. 2002, 82, 1–556. [Google Scholar]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Chemical agents and related occupations. IARC Monogr. Eval. Carcinog Risks Hum. 2012, 100, 9–562. [Google Scholar]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Some chemicals present in industrial and consumer products, food and drinking water. IARC Monogr. Eval. Carcinog. Risks Hum. 2013, 101, 9–549. [Google Scholar]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans.Outdoor Air Pollution. IARC Monogr. Eval. Carcinog. Risks Hum. 2016, 109, 9–444. [Google Scholar]
- Lee, S.; Hong, S.; Liu, X.; Kim, C.; Jung, D.; Yim, U.H.; Shim, W.J.; Khim, J.S.; Giesy, J.P.; Choi, K. Endocrine disrupting potential of PAHs and their alkylated analogues associated with oil spills. Environ. Sci. Process. Impacts 2017, 19, 1117–1125. [Google Scholar] [CrossRef] [PubMed]
- ECHA Substance Information. Polycyclic-Aromatic Hydrocarbons (PAH). Available online: https://echa.europa.eu/fr/substance-information/-/substanceinfo/100.239.209 (accessed on 5 April 2022).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- LaKind, J.S.; Sobus, J.R.; Goodman, M.; Barr, D.B.; Fürst, P.; Albertini, R.J.; Arbuckle, T.E.; Schoeters, G.; Tan, Y.-M.; Teeguarden, J.; et al. A proposal for assessing study quality: Biomonitoring, Environmental Epidemiology, and Short-lived Chemicals (BEES-C) instrument. Environ. Int. 2014, 73, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Laitinen, J.; Mäkelä, M.; Mikkola, J.; Huttu, I. Fire fighting trainers’ exposure to carcinogenic agents in smoke diving simulators. Toxicol. Lett. 2010, 192, 61–65. [Google Scholar] [CrossRef]
- Lutier, S.; Maître, A.; Bonneterre, V.; Bicout, D.J.; Marques, M.; Persoons, R.; Barbeau, D. Urinary elimination kinetics of 3-hydroxybenzo(a)pyrene and 1-hydroxypyrene of workers in a prebake aluminum electrode production plant: Evaluation of diuresis correction methods for routine biological monitoring. Environ. Res. 2016, 147, 469–479. [Google Scholar] [CrossRef]
- Barbeau, D.; Persoons, R.; Marques, M.; Hervé, C.; Laffitte-Rigaud, G.; Maitre, A. Relevance of urinary 3-hydroxybenzo(a)pyrene and 1-hydroxypyrene to assess exposure to carcinogenic polycyclic aromatic hydrocarbon mixtures in metallurgy workers. Ann. Occup. Hyg. 2014, 58, 579–590. [Google Scholar] [CrossRef]
- Barbeau, D.; Lutier, S.; Choisnard, L.; Marques, M.; Persoons, R.; Maitre, A. Urinary trans-anti-7,8,9,10-tetrahydroxy-7,8,9,10-tetrahydrobenzo(a)pyrene as the most relevant biomarker for assessing carcinogenic polycyclic aromatic hydrocarbons exposure. Environ. Int. 2018, 112, 147–155. [Google Scholar] [CrossRef]
- Barbeau, D.; Lutier, S.; Marques, M.; Persoons, R.; Maitre, A. Comparison of gaseous polycyclic aromatic hydrocarbon metabolites according to their specificity as biomarkers of occupational exposure: Selection of 2-hydroxyfluorene and 2-hydroxyphenanthrene. J. Hazard. Mater. 2017, 332, 185–194. [Google Scholar] [CrossRef]
- Forster, K.; Preuss, R.; Rossbach, B.; Bruning, T.; Angerer, J.; Simon, P. 3-Hydroxybenzo[a]pyrene in the urine of workers with occupational exposure to polycyclic aromatic hydrocarbons in different industries. Occup. Environ. Med. 2008, 65, 224–229. [Google Scholar] [CrossRef]
- Klöslová, Z.; Drímal, M.; Balog, K.; Koppová, K.; Dubajová, J. The Relations between Polycyclic Aromatic Hydrocarbons Exposure and 1-OHP Levels as a Biomarker of the Exposure. Cent. Eur. J. Public Health 2016, 24, 302–307. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Marczynski, B.; Pesch, B.; Wilhelm, M.; Rossbach, B.; Preuss, R.; Hahn, J.-U.; Rabstein, S.; Raulf-Heimsoth, M.; Seidel, A.; Rihs, H.-P.; et al. Occupational exposure to polycyclic aromatic hydrocarbons and DNA damage by industry: A nationwide study in Germany. Arch. Toxicol. 2009, 83, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Seidel, A.; Spickenheuer, A.; Straif, K.; Rihs, H.-P.; Marczynski, B.; Scherenberg, M.; Dettbarn, G.; Angerer, J.; Wilhelm, M.; Brüning, T.; et al. New Biomarkers of Occupational Exposure to Polycyclic Aromatic Hydrocarbons. J. Toxicol. Environ. Health Part A 2008, 71, 734–745. [Google Scholar] [CrossRef] [PubMed]
- Raulf-Heimsoth, M.; Angerer, J.; Pesch, B.; Marczynski, B.; Hahn, J.U.; Spickenheuer, A.; Preuss, R.; Rühl, R.; Rode, P.; Brüning, T. Biological Monitoring as a Useful Tool for the Detection of a Coal-Tar Contamination in Bitumen-Exposed Workers. J. Toxicol. Environ. Health Part A 2008, 71, 746–750. [Google Scholar] [CrossRef]
- Raulf-Heimsoth, M.; Marczynski, B.; Spickenheuer, A.; Pesch, B.; Welge, P.; Rühl, R.; Bramer, R.; Kendzia, B.; Heinze, E.; Angerer, J.; et al. Bitumen workers handling mastic versus rolled asphalt in a tunnel: Assessment of exposure and biomarkers of irritation and genotoxicity. Arch. Toxicol. 2011, 85, 81–87. [Google Scholar] [CrossRef]
- Rihs, H.-P.; Spickenheuer, A.; Heinze, E.; Pesch, B.; Raulf-Heimsoth, M.; Angerer, J.; Brüning, T. Modulation of urinary polycyclic aromatic hydrocarbon metabolites by enzyme polymorphisms in workers of the German Human Bitumen Study. Arch. Toxicol. 2011, 85, 73–79. [Google Scholar] [CrossRef]
- Marczynski, B.; Raulf-Heimsoth, M.; Spickenheuer, A.; Pesch, B.; Kendzia, B.; Mensing, T.; Engelhardt, B.; Lee, E.-H.; Schindler, B.K.; Heinze, E.; et al. DNA adducts and strand breaks in workers exposed to vapours and aerosols of bitumen: Associations between exposure and effect. Arch. Toxicol. 2011, 85, 53–64. [Google Scholar] [CrossRef]
- Pesch, B.; Spickenheuer, A.; Kendzia, B.; Schindler, B.K.; Welge, P.; Marczynski, B.; Rihs, H.-P.; Raulf-Heimsoth, M.; Angerer, J.; Brüning, T. Urinary metabolites of polycyclic aromatic hydrocarbons in workers exposed to vapours and aerosols of bitumen. Arch. Toxicol. 2011, 85, 29–39. [Google Scholar] [CrossRef]
- Lotz, A.; Pesch, B.; Dettbarn, G.; Raulf, M.; Welge, P.; Rihs, H.-P.; Breuer, D.; Gabriel, S.; Hahn, J.-U.; Brüning, T.; et al. Metabolites of the PAH diol epoxide pathway and other urinary biomarkers of phenanthrene and pyrene in workers with and without exposure to bitumen fumes. Int. Arch. Occup. Environ. Health 2016, 89, 1251–1267. [Google Scholar] [CrossRef]
- Fostinelli, J.; Madeo, E.; Toraldo, E.; Sarnico, M.; Luzzana, G.; Tomasi, C.; De Palma, G. Environmental and biological monitoring of occupational exposure to polynuclear aromatic hydrocarbons during highway pavement construction in Italy. Toxicol. Lett. 2018, 298, 134–140. [Google Scholar] [CrossRef]
- Persoons, R.; Roseau, L.; Petit, P.; Hograindleur, C.; Montlevier, S.; Marques, M.; Ottoni, G.; Maitre, A. Towards a recommended biomonitoring strategy for assessing the occupational exposure of roofers to PAHs. Toxicol. Lett. 2020, 324, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Campo, L.; Fustinoni, S.; Consonni, D.; Pavanello, S.; Kapka, L.; Siwinska, E.; Mielzyňska, D.; Bertazzi, P. Urinary carcinogenic 4–6 ring polycyclic aromatic hydrocarbons in coke oven workers and in subjects belonging to the general population: Role of occupational and environmental exposure. Int. J. Hyg. Environ. Health 2014, 217, 231–238. [Google Scholar] [CrossRef]
- Zając, J.; Gomółka, E.; Maziarz, B.; Szot, W. Occupational Exposure to Polycyclic Aromatic Hydrocarbons in Polish Coke Plant Workers. Ann. Occup. Hyg. 2016, 60, 1062–1071. [Google Scholar] [CrossRef] [PubMed]
- Zając, J.; Gomółka, E.; Szot, W. Urinary 1-hydroxypyrene in occupationally-exposed and non-exposed individuals in Silesia, Poland. Ann. Agric. Environ. Med. 2018, 25, 625–629. [Google Scholar] [CrossRef]
- Klotz, K.; Zobel, M.; Schäferhenrich, A.; Hebisch, R.; Drexler, H.; Göen, T. Suitability of several naphthalene metabolites for their application in biomonitoring studies. Toxicol. Lett. 2018, 298, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Hebisch, R.; Karmann, J.; Schäferhenrich, A.; Göen, T.; Berger, M.; Poppek, U.; Roitzsch, M. Inhalation and dermal exposure of workers during timber impregnation with creosote and subsequent processing of impregnated wood. Environ. Res. 2020, 181, 108877. [Google Scholar] [CrossRef]
- Gjesteland, I.; Hollund, B.E.; Kirkeleit, J.; Daling, P.; Bråtveit, M. Biomonitoring of Benzene and Effect of Wearing Respirators during an Oil Spill Field Trial at Sea. Ann. Work Expo. Health 2018, 62, 1033–1039. [Google Scholar] [CrossRef]
- Mari, M.; Schuhmacher, M.; Domingo, J.L. Levels of metals and organic substances in workers at a hazardous waste incinerator: A follow-up study. Int. Arch. Occup. Environ. Health 2009, 82, 519–528. [Google Scholar] [CrossRef]
- Mari, M.; Nadal, M.; Schuhmacher, M.; Domingo, J.L. Body burden monitoring of dioxins and other organic substances in workers at a hazardous waste incinerator. Int. J. Hyg. Environ. Health 2013, 216, 728–734. [Google Scholar] [CrossRef]
- Laitinen, J.; Mäkelä, M.; Mikkola, J.; Huttu, I. Firefighters’ multiple exposure assessments in practice. Toxicol. Lett. 2012, 213, 129–133. [Google Scholar] [CrossRef]
- Oliveira, M.; Slezakova, K.; Alves, M.J.; Fernandes, A.; Teixeira, J.P.; Delerue-Matos, C.; Pereira, M.D.C.; Morais, S. Firefighters’ exposure biomonitoring: Impact of firefighting activities on levels of urinary monohydroxyl metabolites. Int. J. Hyg. Environ. Health 2016, 219, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.; Slezakova, K.; Magalhães, C.P.; Fernandes, A.; Teixeira, J.P.; Delerue-Matos, C.; Pereira, M.D.C.; Morais, S. Individual and cumulative impacts of fire emissions and tobacco consumption on wildland firefighters’ total exposure to polycyclic aromatic hydrocarbons. J. Hazard. Mater. 2017, 334, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.; Slezakova, K.; Alves, M.J.; Fernandes, A.; Teixeira, J.P.; Delerue-Matos, C.; do Carmo Pereira, M.; Morais, S. Polycyclic aromatic hydrocarbons at fire stations: Firefighters’ exposure monitoring and biomonitoring, and assessment of the contribution to total internal dose. J. Hazard. Mater. 2017, 323, 184–194. [Google Scholar] [CrossRef]
- Andersen, M.H.G.; Saber, A.T.; Pedersen, P.B.; Loft, S.; Hansen, M.; Koponen, I.K.; Pedersen, J.E.; Ebbehøj, N.; Nørskov, E.-C.; Clausen, P.A.; et al. Cardiovascular health effects following exposure of human volunteers during fire extinction exercises. Environ. Health 2017, 16, 96. [Google Scholar] [CrossRef] [PubMed]
- Andersen, M.H.G.; Saber, A.T.; Clausen, P.A.; Pedersen, J.E.; Løhr, M.; Kermanizadeh, A.; Loft, S.; Ebbehøj, N.; Hansen, Å.M.; Pedersen, P.B.; et al. Association between polycyclic aromatic hydrocarbon exposure and peripheral blood mononuclear cell DNA damage in human volunteers during fire extinction exercises. Mutagenesis 2018, 33, 105–115. [Google Scholar] [CrossRef]
- Wingfors, H.; Nyholm, J.R.; Magnusson, R.; Wijkmark, C.H. Impact of Fire Suit Ensembles on Firefighter PAH Exposures as Assessed by Skin Deposition and Urinary Biomarkers. Ann. Work. Expo. Health 2018, 62, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Rossbach, B.; Wollschläger, D.; Letzel, S.; Gottschalk, W.; Muttray, A. Internal exposure of firefighting instructors to polycyclic aromatic hydrocarbons (PAH) during live fire training. Toxicol. Lett. 2020, 331, 102–111. [Google Scholar] [CrossRef]
- Sancini, A.; Caciari, T.; Sinibaldi, F. Blood pressure changes and polycyclic aromatic hydrocarbons in outdoor workers. Clin. Ter. 2014, 165, e295–e303. [Google Scholar] [CrossRef]
- Rossner, P.; Svecova, V.; Milcova, A.; Lnenickova, Z.; Solansky, I.; Sram, R.J. Seasonal variability of oxidative stress markers in city bus drivers: Part I. Oxidative damage to DNA. Mutat. Res. Mol. Mech. Mutagen. 2008, 642, 14–20. [Google Scholar] [CrossRef]
- Andersen, M.H.G.; Saber, A.T.; Frederiksen, M.; Clausen, P.A.; Sejbaek, C.S.; Hemmingsen, C.H.; Ebbehøj, N.E.; Catalán, J.; Aimonen, K.; Koivisto, J.; et al. Occupational exposure and markers of genetic damage, systemic inflammation and lung function: A Danish cross-sectional study among air force personnel. Sci. Rep. 2021, 11, 17998. [Google Scholar] [CrossRef]
- Guilbert, A.; De Cremer, K.; Heene, B.; Demoury, C.; Aerts, R.; Declerck, P.; Brasseur, O.; Van Nieuwenhuyse, A. Personal exposure to traffic-related air pollutants and relationships with respiratory symptoms and oxidative stress: A pilot cross-sectional study among urban green space workers. Sci. Total Environ. 2019, 649, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Scheepers, P.T.J.; Van Houtum, J.; Anzion, R.B.; Champmartin, C.; Hertsenberg, S.; Bos, R.P.; Van Der Valk, P. The occupational exposure of dermatology nurses to polycyclic aromatic hydrocarbons—Evaluating the effectiveness of better skin protection. Scand. J. Work. Environ. Health 2009, 35, 212–221. [Google Scholar] [CrossRef]
- Van Gestel, E.A.; Linssen, E.S.; Creta, M.; Poels, K.; Godderis, L.; Weyler, J.J.; De Schryver, A.; Vanoirbeek, J.A. Assessment of the absorbed dose after exposure to surgical smoke in an operating room. Toxicol. Lett. 2020, 328, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, S.A.; Torres, V.M.; Louro, H.; Gomes, F.; Lopes, C.; Marçal, N.S.; Fragoso, E.; Martins, C.; Oliveira, C.L.; Hagenfeldt, M.; et al. Effects of Occupational Exposure to Tobacco Smoke: Is There a Link Between Environmental Exposure and Disease? J. Toxicol. Environ. Health Part A 2013, 76, 311–327. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.; Capelas, S.; Delerue-Matos, C.; Morais, S. Grill Workers Exposure to Polycyclic Aromatic Hydrocarbons: Levels and Excretion Profiles of the Urinary Biomarkers. Int. J. Environ. Res. Public Health 2020, 18, 230. [Google Scholar] [CrossRef]
- Hansen, A.M.; Mathiesen, L.; Pedersen, M.; Knudsen, L.E. Urinary 1-hydroxypyrene (1-HP) in environmental and occupational studies—A review. Int. J. Hyg. Environ. Health 2008, 211, 471–503. [Google Scholar] [CrossRef]
- Vital, N.; Antunes, S.; Louro, H.; Vaz, F.; Simões, T.; Penque, D.; Silva, M.J. Environmental Tobacco Smoke in Occupational Settings: Effect and Susceptibility Biomarkers in Workers from Lisbon Restaurants and Bars. Front. Public Health 2021, 9, 674142. [Google Scholar] [CrossRef]
- Petit, P.; Bicout, D.J.; Persoons, R.; Bonneterre, V.; Barbeau, D.; Maître, A. Constructing a Database of Similar Exposure Groups: The Application of the Exporisq-HAP Database from 1995 to 2015. Ann. Work Expo. Health 2017, 61, 440–456. [Google Scholar] [CrossRef]
- Unwin, J.; Cocker, J.; Scobbie, E.; Chambers, H. An Assessment of Occupational Exposure to Polycyclic Aromatic Hydrocarbons in the UK. Ann. Occup. Hyg. 2006, 50, 395–403. [Google Scholar] [CrossRef]
- Alhamdow, A.; Tinnerberg, H.; Lindh, C.; Albin, M.; Broberg, K. Cancer-related proteins in serum are altered in workers occupationally exposed to polycyclic aromatic hydrocarbons: A cross-sectional study. Carcinogenesis 2019, 40, 771–781. [Google Scholar] [CrossRef]
- Valière, M.; Petit, P.; Persoons, R.; Demeilliers, C.; Maître, A. Consistency between air and biological monitoring for assessing polycyclic aromatic hydrocarbon exposure and cancer risk of workers. Environ. Res. 2022, 207, 112268. [Google Scholar] [CrossRef] [PubMed]
- Vimercati, L.; Bisceglia, L.; Cavone, D.; Caputi, A.; De Maria, L.; Delfino, M.C.; Corrado, V.; Ferri, G.M. Environmental Monitoring of PAHs Exposure, Biomarkers and Vital Status in Coke Oven Workers. Int. J. Environ. Res. Public Health 2020, 17, 2199. [Google Scholar] [CrossRef] [PubMed]
- Sams, C. Urinary Naphthol as a Biomarker of Exposure: Results from an Oral Exposure to Carbaryl and Workers Occupationally Exposed to Naphthalene. Toxics 2017, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Sram, R.J.; Svecova, V.; Rossnerova, A. Systematic review of the use of the lymphocyte cytokinesis-block micronucleus assay to measure DNA damage induced by exposure to polycyclic aromatic hydrocarbons. Mutat. Res. Mutat. Res. 2016, 770, 162–169. [Google Scholar] [CrossRef]
- Alhamdow, A.; Lindh, C.; Albin, M.; Gustavsson, P.; Tinnerberg, H.; Broberg, K. Cardiovascular disease-related serum proteins in workers occupationally exposed to polycyclic aromatic hydrocarbons. Toxicol. Sci. 2019, 171, 235–246. [Google Scholar] [CrossRef]
- Alhamdow, A.; Zettergren, A.; Kull, I.; Hallberg, J.; Andersson, N.; Ekström, S.; Berglund, M.; Wheelock, C.E.; Essig, Y.J.; Krais, A.M.; et al. Low-level exposure to polycyclic aromatic hydrocarbons is associated with reduced lung function among Swedish young adults. Environ. Res. 2021, 197, 111169. [Google Scholar] [CrossRef]
- Gao, P.; da Silva, E.; Hou, L.; Denslow, N.D.; Xiang, P.; Ma, L.Q. Human exposure to polycyclic aromatic hydrocarbons: Metabolomics perspective. Environ. Int. 2018, 119, 466–477. [Google Scholar] [CrossRef]
- Keir, J.L.A.; Akhtar, U.S.; Matschke, D.M.J.; Kirkham, T.; Chan, L.; Ayotte, P.; White, P.A.; Blais, J.M. Elevated Exposures to Polycyclic Aromatic Hydrocarbons and Other Organic Mutagens in Ottawa Firefighters Participating in Emergency, On-Shift Fire Suppression. Environ. Sci. Technol. 2017, 51, 12745–12755. [Google Scholar] [CrossRef]
- Thein, N.; Møller, P.; Amtoft, H.; Vogel, U.; Korsholm, B.; Autrup, H.; Wallin, H. A strong genotoxic effect in mouse skin of a single painting of coal tar in hairless mice and in MutaMouse. Mutat. Res. Mol. Mech. Mutagen. 2000, 468, 117–124. [Google Scholar] [CrossRef]
- Hadrup, N.; Zhernovkov, V.; Jacobsen, N.R.; Voss, C.; Strunz, M.; Ansari, M.; Schiller, H.B.; Halappanavar, S.; Poulsen, S.S.; Kholodenko, B.; et al. Acute Phase Response as a Biological Mechanism-of-Action of (Nano)particle-Induced Cardiovascular Disease. Small 2020, 16, e1907476. [Google Scholar] [CrossRef]
- Saber, A.T.; Jacobsen, N.R.; Jackson, P.; Poulsen, S.S.; Kyjovska, Z.O.; Halappanavar, S.; Yauk, C.L.; Wallin, H.; Vogel, U. Particle-induced pulmonary acute phase response may be the causal link between particle inhalation and cardiovascular disease. WIREs Nanomed. Nanobiotechnology 2014, 6, 517–531. [Google Scholar] [CrossRef] [PubMed]
- Stone, V.; Miller, M.R.; Clift, M.; Elder, A.; Mills, N.L.; Møller, P.; Schins, R.P.; Vogel, U.; Kreyling, W.; Jensen, K.A.; et al. Nanomaterials Versus Ambient Ultrafine Particles: An Opportunity to Exchange Toxicology Knowledge. Environ. Health Perspect. 2017, 125, 106002. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Hennekens, C.H.; Buring, J.E.; Rifai, N. C-Reactive Protein and Other Markers of Inflammation in the Prediction of Cardiovascular Disease in Women. N. Engl. J. Med. 2000, 342, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.C.; Wilson, P.G.; Shridas, P.; Ji, A.; de Beer, M.; de Beer, F.C.; Webb, N.R.; Tannock, L.R. Serum amyloid A3 is pro-atherogenic. Atherosclerosis 2018, 268, 32–35. [Google Scholar] [CrossRef] [PubMed]
- RAC. Note on Reference Dose-Response Relationship for the Carcinogenicity of Pitch, Coal Tar, High Temperature and on PBT and vPvB Properties. 2018. Available online: https://echa.europa.eu/documents/10162/17229/ctpht_rac_note_en.pdf/a184ee42-0642-7454-2d18-63324688e13d?t=1544526560573 (accessed on 12 April 2022).
- Lafontaine, M.; Gendre, C.; Morele, Y.; Laffitte-Rigaud, G. Excretion of Urinary 1-Hydroxypyrene in Relation to the Penetration Routes of Polycyclic Aromatic Hydrocarbons. Polycycl. Aromat. Compd. 2002, 22, 579–588. [Google Scholar] [CrossRef]
- Cherry, N.; Aklilu, Y.-A.; Beach, J.; Britz-McKibbin, P.; Elbourne, R.; Galarneau, J.-M.; Gill, B.; Kinniburgh, D.; Zhang, X. Urinary 1-hydroxypyrene and Skin Contamination in Firefighters Deployed to the Fort McMurray Fire. Ann. Work Expo. Health 2019, 63, 448–458. [Google Scholar] [CrossRef]
- Cequier, E.; Pérez Luzardo, O.; Kasper-Sonnenberg, M.; Koch, H.; Haug, L.S.; Bury, D.; Vorkamp, K.; Knudsen, B.E.; Hajeb, P.; Pardo, O.; et al. Prioritised List of Biomarkers, Matrices and Analytical Methods for the 1st Prioritisation Round of Substances. Deliverable Report D9.WP9—Laboratory Analysis and Quality Assurance. 2017. Available online: https://www.hbm4eu.eu/work-packages/deliverable-9-2-prioritised-list-of-biomarkers-matrices-and-analytical-methods-for-the-1st-prioritisation-round-of-substances/ (accessed on 18 July 2022).
- Santonen, T.; Alimonti, A.; Bocca, B.; Duca, R.C.; Galea, K.S.; Godderis, L.; Göen, T.; Gomes, B.; Hanser, O.; Iavicoli, I.; et al. Setting up a collaborative European human biological monitoring study on occupational exposure to hexavalent chromium. Environ. Res. 2019, 177, 108583. [Google Scholar] [CrossRef]
- Scheepers, P.T.J.; Duca, R.C.; Galea, K.S.; Godderis, L.; Hardy, E.; Knudsen, L.E.; Leese, E.; Louro, H.; Mahiout, S.; Ndaw, S.; et al. HBM4EU Occupational Biomonitoring Study on e-Waste—Study Protocol. Int. J. Environ. Res. Public Health 2021, 18, 12987. [Google Scholar] [CrossRef]
- Jones, K.; Galea, K.S.; Scholten, B.; Loikala, M.; Porras, S.P.; Bousoumah, R.; Ndaw, S.; Leese, E.; Louro, H.; Silva, M.J.; et al. HBM4EU Diisocyanates Study—Research Protocol for a Collaborative European Human Biological Monitoring Study on Occupational Exposure. Int. J. Environ. Res. Public Health 2022, 19, 8811. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).