Personality Assessment Inventory in Fibromyalgia: Links to Functional, Physical–Somatic, and Emotional Impact
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Participants
2.3. Study Design and Procedure
2.4. Instruments
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Impact Domain (FIQ) | Cluster | PAI Psychological Characteristics | Most Prevalent Diagnosis by PAI |
|---|---|---|---|
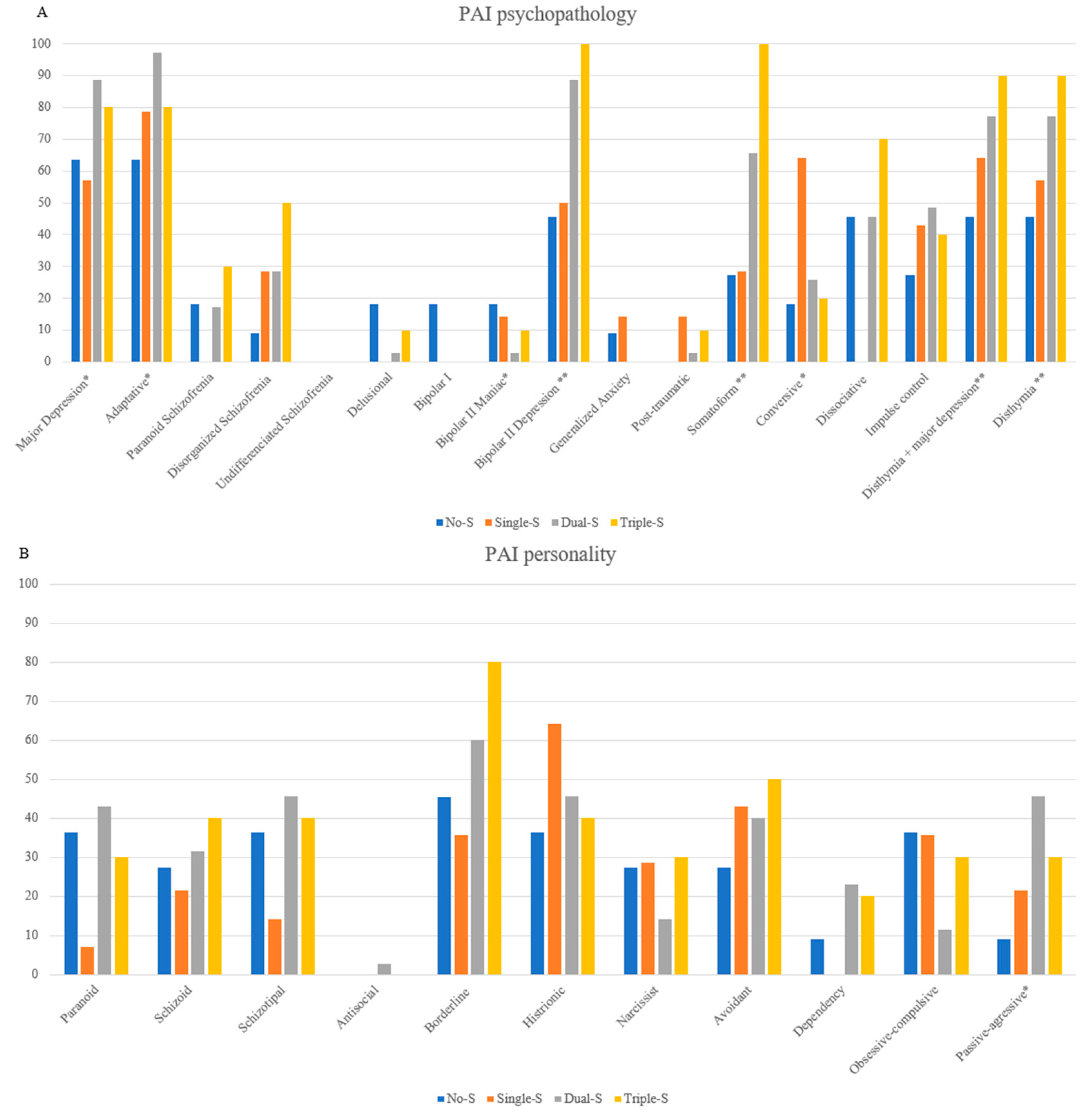
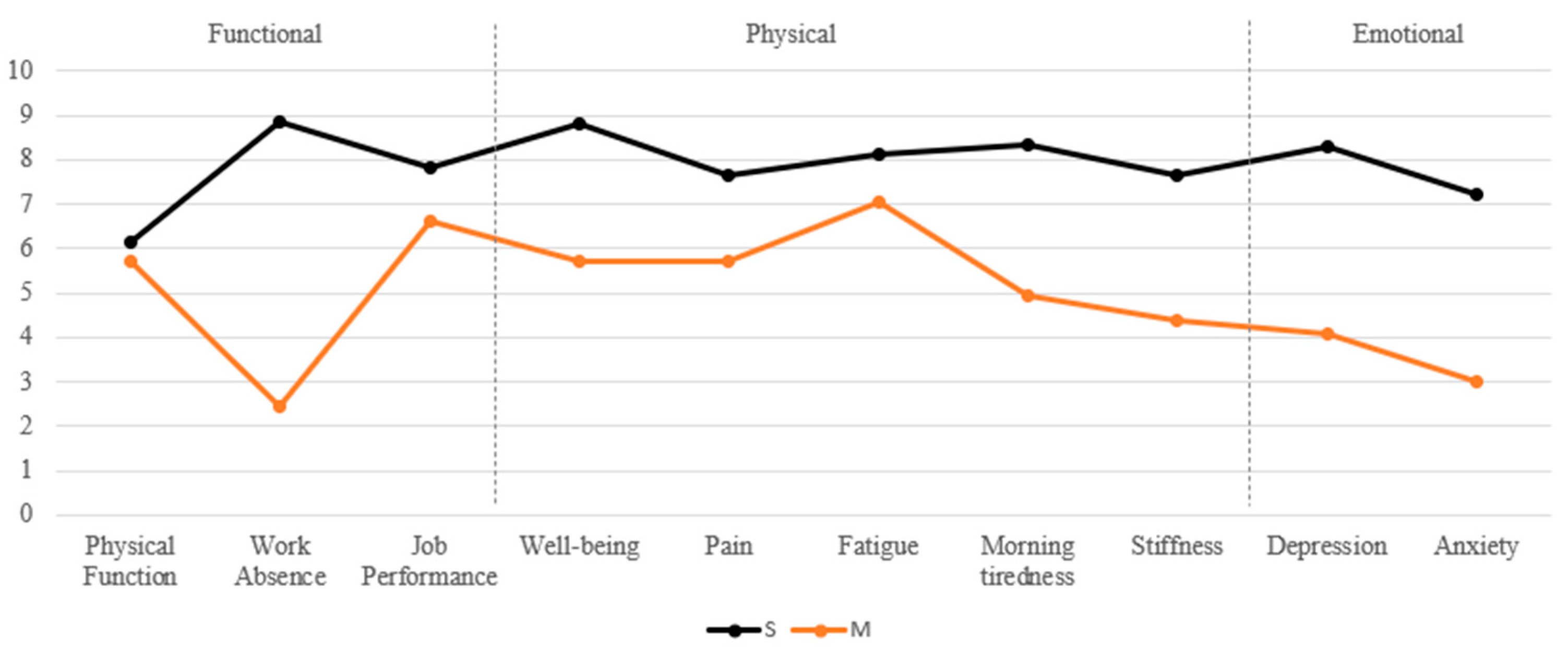
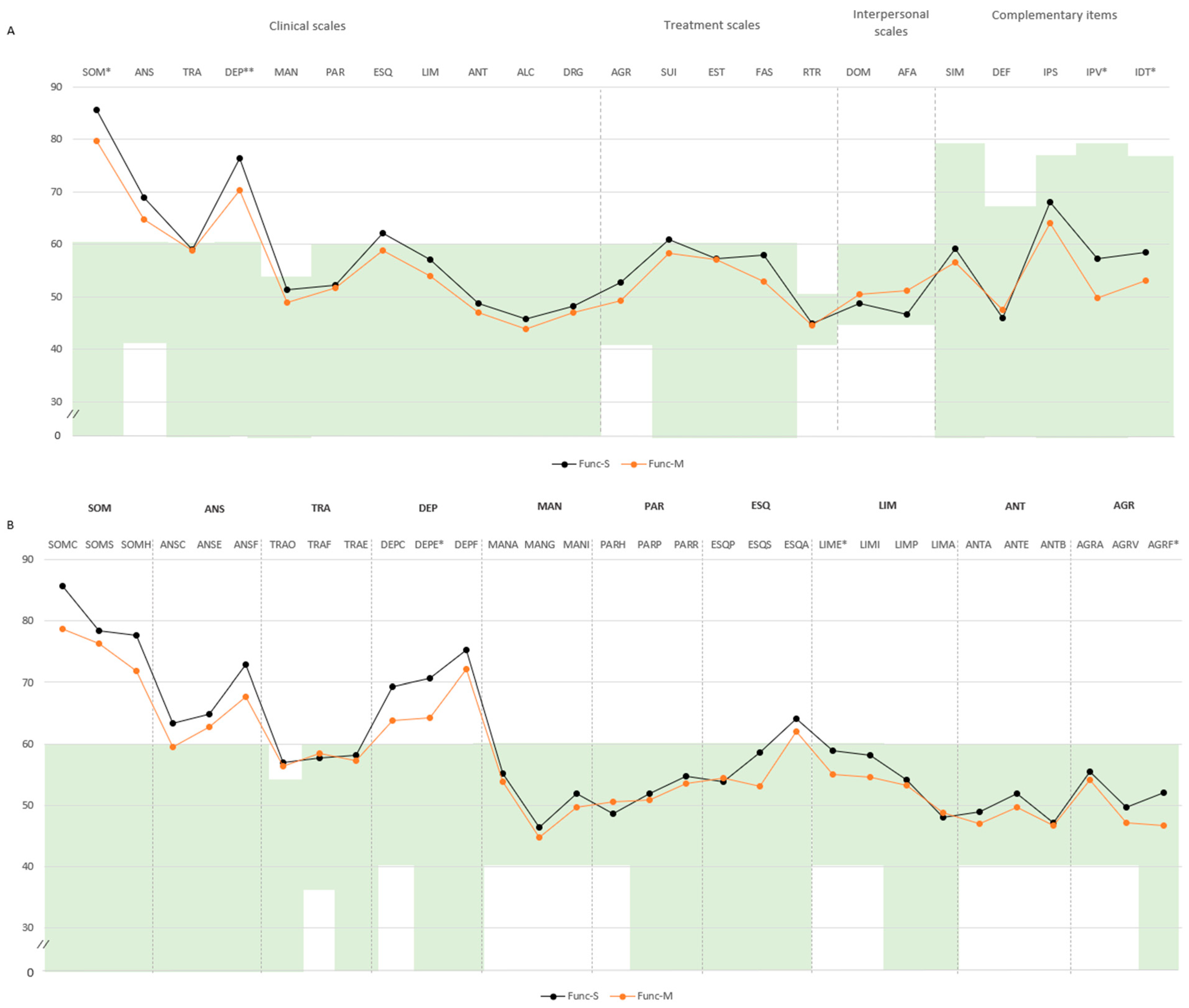
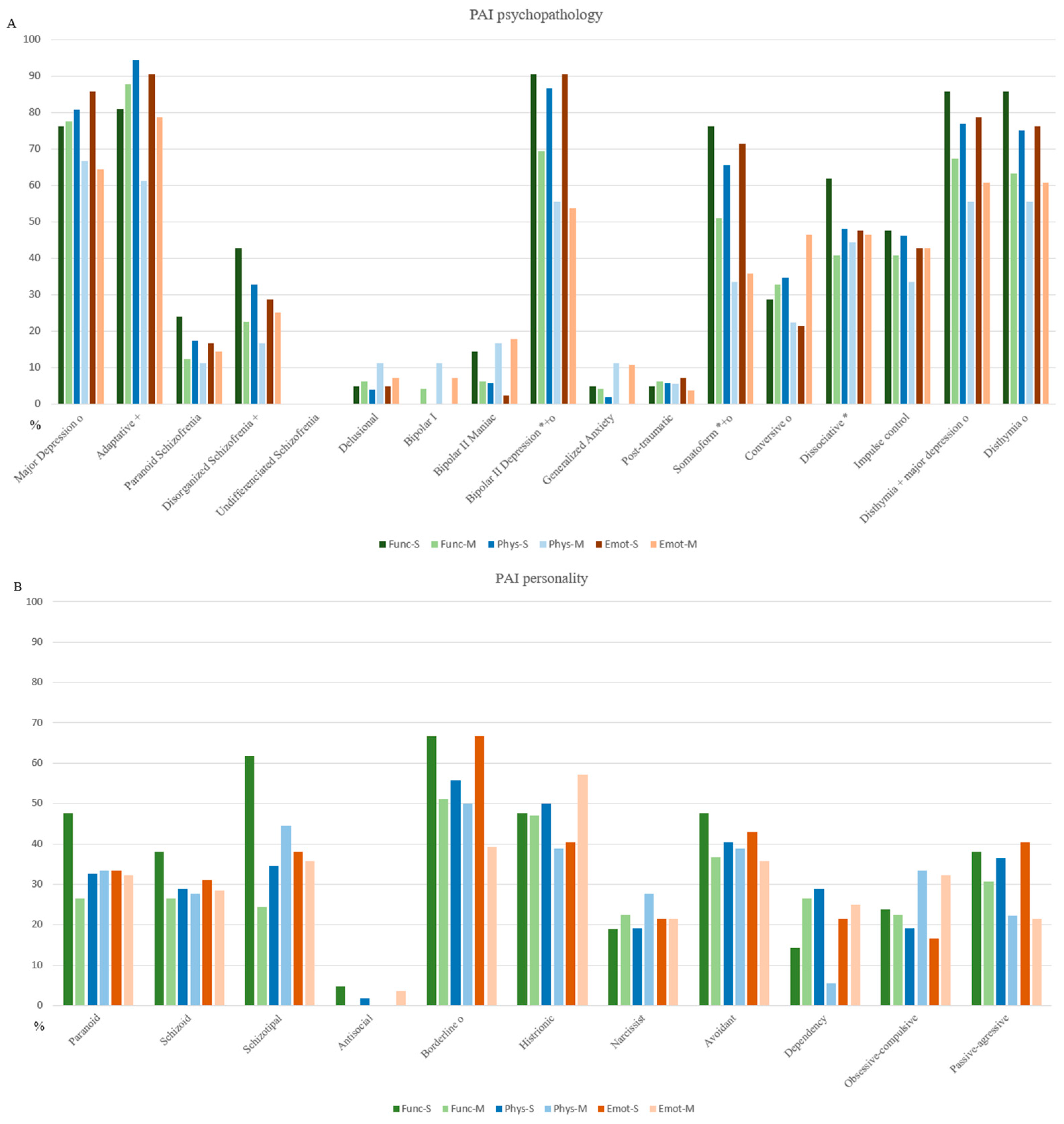
| Functional | Func-M | Milder emotional distress and fewer physical symptom concerns | Major depression (77.55%) and adaptative disorder (87.75%). Borderline personality disorder (51%). |
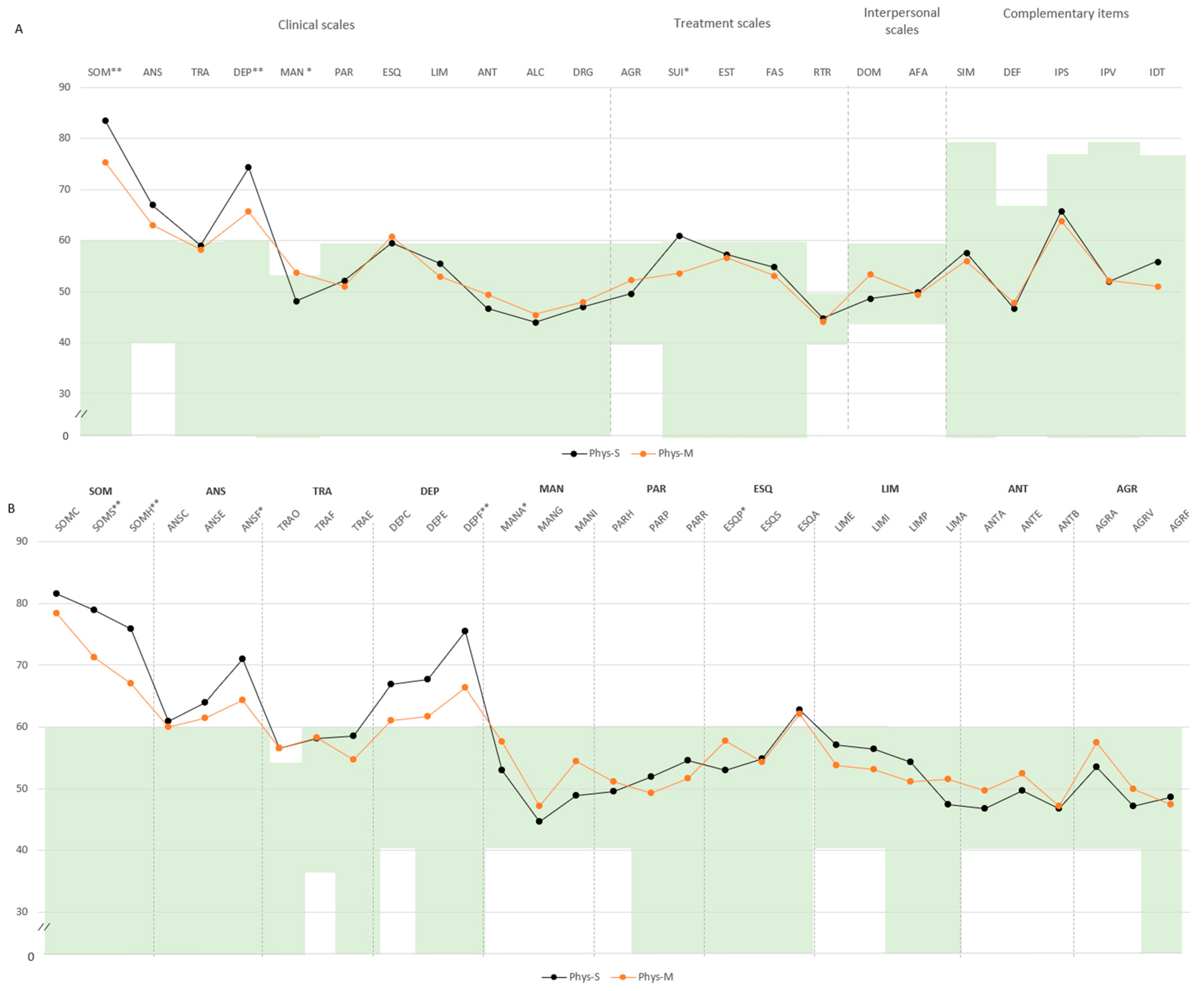
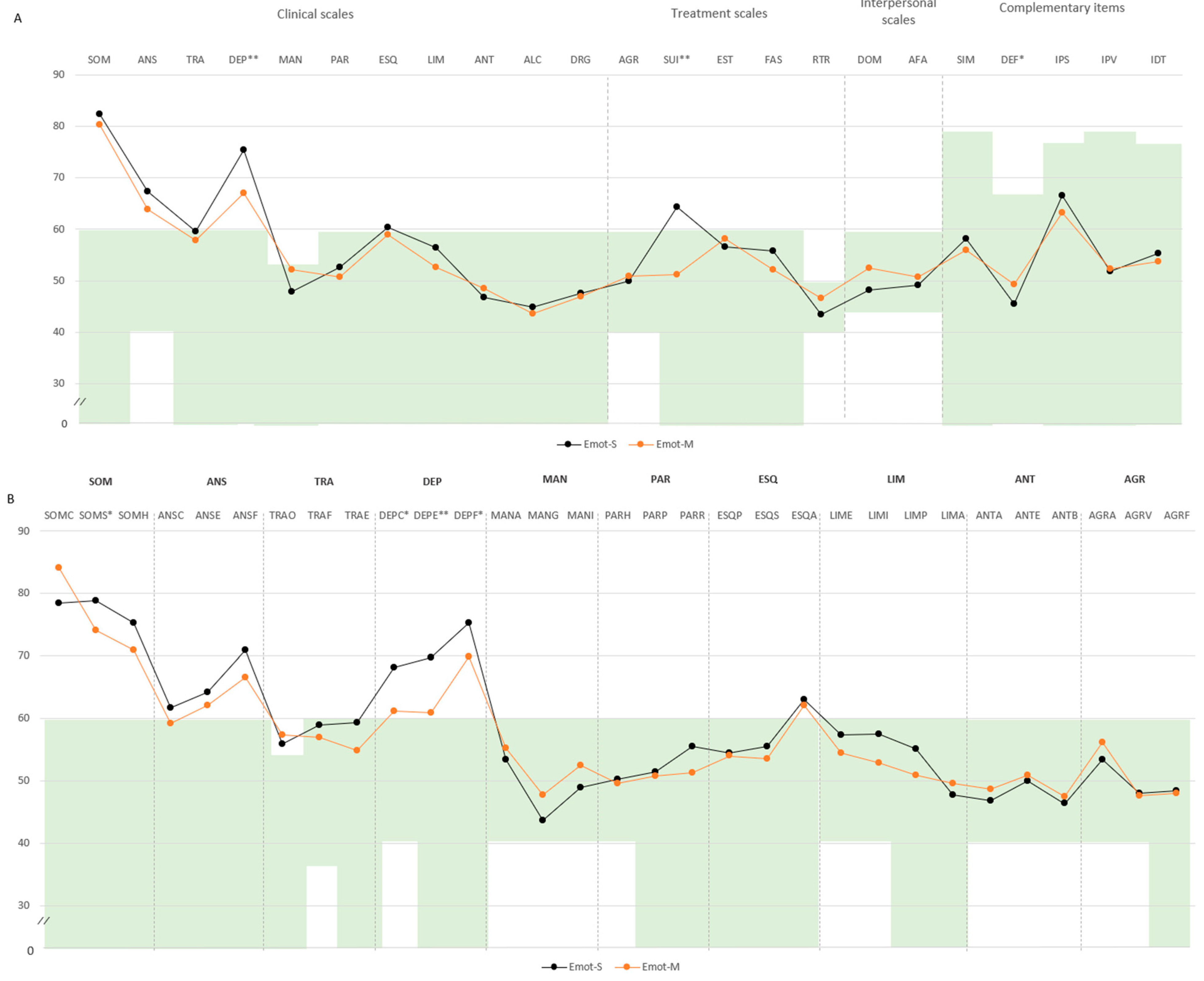
| Func-S | Increased sensitivity to symptoms, mood variability, and treatment engagement difficulties | Bipolar II depression (90.47%), Somatoform disorder (76.19%), dissociative disorder (61.90%), dysthymia (85.71%), and dysthymia with Major Depression (85.71%). Schizotypal (61.90%) and borderline (66.66%) personality disorder. | |
| Physical–somatic | Phys-M | Higher energy levels with relatively stable mood and fewer emotional symptoms (depressive and anxiety features) | Bipolar II depressive (55.55%), borderline (50%), narcissist (27.77%), and avoidant (38.88%) personality disorder. |
| Phys-S | Heightened sensitivity to bodily symptoms and mood-related challenges with suicidal ideation | Major depression (80.76%), adaptative (94.23%), bipolar II depression (86%). Somatoform (65.38%), dysthymia (75%), and dysthymia with major depression (76.92%). | |
| Emotional | Emot-M | Functional physical responses to stress, dominance or directive interpersonal style with limited emotional distress and low suicidal ideation | Conversive disorder (46.42%) and histrionic personality disorder (57.14%). |
| Emot-S | Pronounced emotional (depression and anxiety) and physical distress (somatization), with reduced emotional resilience or lowered coping barriers | Major depression (85.71%), adaptative disorder (90.47%), bipolar II depression (90.47%), dysthymia (76.19%), and dysthymia with major depression (78.57%). | |
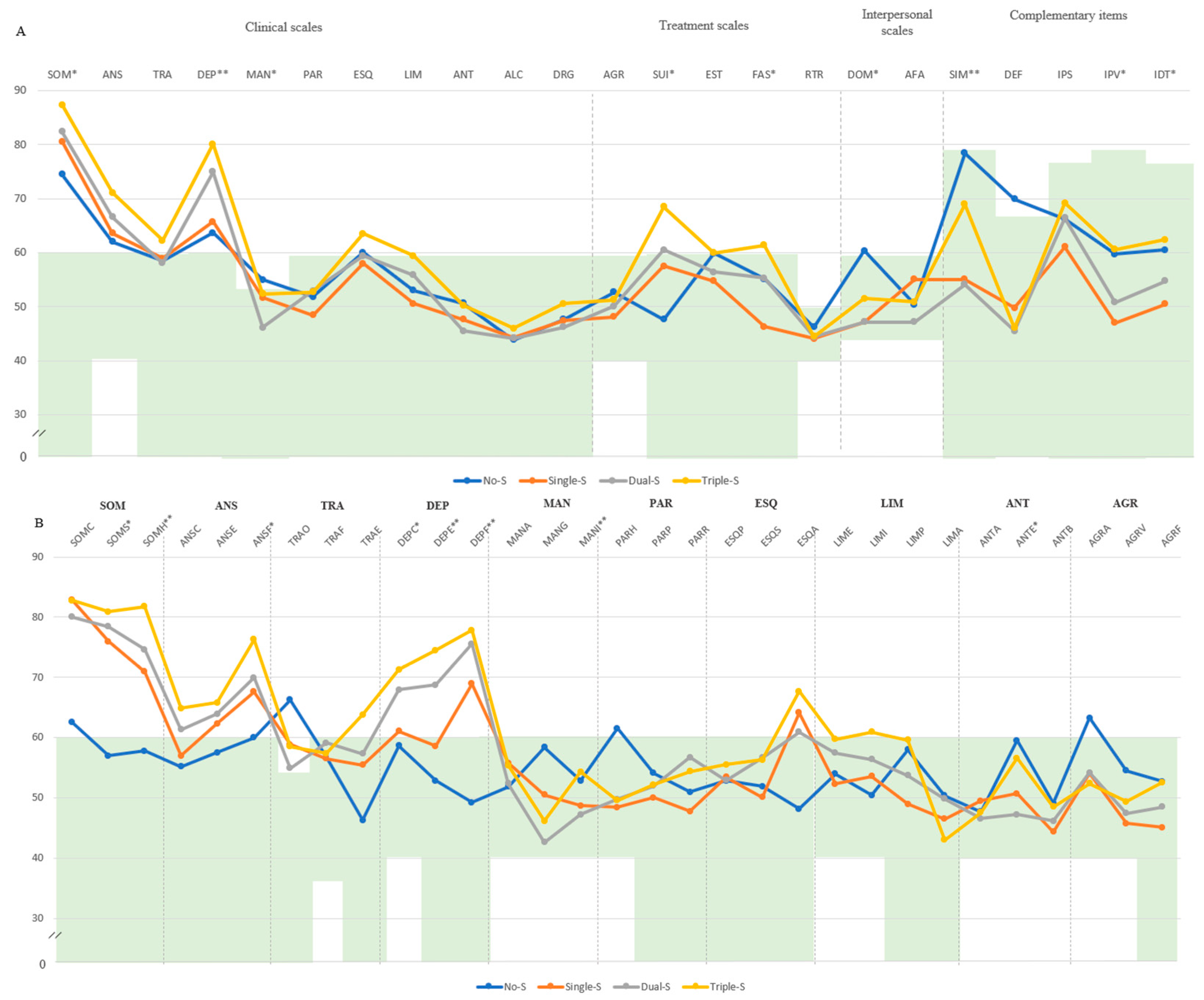
| Cumulative | No-S | Cautious self-presentation or defensive coping style and oppositional attitudes under stress | Obsessive–compulsive personality disorder (36.36%). |
| Single-S | Stable interpersonal functioning with adequate support and few treatment challenges, as well as a supportive psychosocial environment | Psychogenic disorder (64.29%) and obsessive–compulsive personality disorder (35.71%). | |
| Dual-S | Stable activity levels and mood regulation, with no signs of elevated impulsivity or energy dysregulation | Major depression (88.57%) and adaptative disorder (97.14%). Paranoid (42.86%), schizotypal (45.71%), and passive-aggressive personality disorder (45.71%). | |
| Triple-S | Severe multidimensional distress marked by intense symptom preoccupation, emotional suffering with suicidal ideation, as well as heightened physical and psychological sensitivity | Bipolar II depressive (100%), somatoform (100%), dysthymia (90%), and dysthymia with major depression (90%). Borderline (80%) and avoidant personality disorder (50%). |
References
- Adawi, M., Chen, W., Bragazzi, N. L., Watad, A., McGonagle, D., Yavne, Y., Kidron, A., Hodadov, H., Amital, D., & Amital, H. (2021). Suicidal behavior in fibromyalgia patients: Rates and determinants of suicide ideation, risk, suicide, and suicidal attempts—A systematic review of the literature and meta-analysis of over 390,000 fibromyalgia patients. Frontiers in Psychiatry, 12, 629417. [Google Scholar] [CrossRef]
- Aghbelaghi, D. T., Jalali, M., Tayim, N., & Kiyani, R. (2024). A network analysis of depression and cognitive impairments in fibromyalgia: A secondary analysis study. Psychiatric Quarterly, 96(1), 39–57. [Google Scholar] [CrossRef]
- Almulla, A. F., Al-Hakeim, H. K., Abed, M. S., Carvalho, A. F., & Maes, M. (2020). Chronic fatigue and fibromyalgia symptoms are key components of deficit schizophrenia and are strongly associated with activated immune-inflammatory pathways. Schizophrenia Research, 222, 342–353. [Google Scholar] [CrossRef] [PubMed]
- Al Sharie, S., Varga, S. J., Al-Husinat, L., Sarzi-Puttini, P., Araydah, M., Bal’awi, B. R., & Varrassi, G. (2024). Unraveling the complex web of fibromyalgia: A narrative review. Medicina, 60(2), 272. [Google Scholar] [CrossRef] [PubMed]
- Alsiri, N., Alhadhoud, M., Alkatefi, T., & Palmer, S. (2022). The concomitant diagnosis of fibromyalgia and connective tissue disorders: A systematic review. Seminars in Arthritis and Rheumatism, 58, 152127. [Google Scholar] [CrossRef] [PubMed]
- Ansari, A. H., Pal, A., Ramamurthy, A., Kabat, M., Jain, S., & Kumar, S. (2021). Fibromyalgia pain and depression: An update on the role of repetitive transcranial magnetic stimulation. ACS Chemical Neuroscience, 12(2), 256–270. [Google Scholar] [CrossRef]
- Araújo, F. M., & DeSantana, J. M. (2019). Physical therapy modalities for treating fibromyalgia. F1000Research, 8, 2030. [Google Scholar] [CrossRef]
- Arslan, D., & Ünal Çevik, I. (2022). Interactions between the painful disorders and the autonomic nervous system. Ağrı—The Journal of The Turkish Society of Algology, 34(3), 155–165. [Google Scholar] [CrossRef]
- Attademo, L., & Bernardini, F. (2018). Prevalence of personality disorders in patients with fibromyalgia: A brief review. Primary Health Care Research & Development, 19(5), 523–528. [Google Scholar] [CrossRef]
- Bair, M. J., & Krebs, E. E. (2020). Fibromyalgia. Annals of Internal Medicine, 172(5), ITC33–ITC48. [Google Scholar] [CrossRef]
- Berk, E. (2020). The relationship between disease severity and defense mechanisms in fibromyalgia syndrome. Turkish Journal of Physical Medicine and Rehabilitation, 66(1), 47–53. [Google Scholar] [CrossRef] [PubMed]
- Berwick, R., Barker, C., Goebel, A., & on behalf of the guideline development group. (2022). The diagnosis of fibromyalgia syndrome. Clinical Medicine, 22(6), 570–574. [Google Scholar] [CrossRef]
- Bhargava, J., & Goldin, J. (2025). Fibromyalgia. In StatPearls [Internet]. StatPearls Publishing. [Google Scholar]
- Bortolato, B., Berk, M., Maes, M., McIntyre, R. M. R., & Carvalho, A. (2016). Fibromyalgia and bipolar disorder: Emerging epidemiological associations and shared pathophysiology. Current Molecular Medicine, 16(2), 119–136. [Google Scholar] [CrossRef] [PubMed]
- Bravo, C., Skjaerven, L. H., Sein-Echaluce, L. G., & Catalan-Matamoros, D. (2019). Effectiveness of movement and body awareness therapies in patients with fibromyalgia: A systematic review and meta-analysis. European Journal of Physical and Rehabilitation Medicine, 55(5), 646–657. [Google Scholar] [CrossRef]
- Brown, T., Hammond, A., Ching, A., & Parker, J. (2023). Work limitations and associated factors in rheumatoid arthritis, axial spondyloarthritis, osteoarthritis and fibromyalgia. Musculoskeletal Care, 21(3), 827–844. [Google Scholar] [CrossRef] [PubMed]
- Bucourt, E., Martaillé, V., Goupille, P., Joncker-Vannier, I., Huttenberger, B., Réveillère, C., Mulleman, D., & Courtois, R. (2019). A comparative study of fibromyalgia, rheumatoid arthritis, spondyloarthritis, and sjögren’s syndrome; impact of the disease on quality of life, psychological adjustment, and use of coping strategies. Pain Medicine, 22(2), 372–381. [Google Scholar] [CrossRef] [PubMed]
- Bulu, A., Onalan, E., Korkmaz, S., Yakar, B., Karatas, T. K., Guven, T., Karatas, A., Koca, S. S., Atli, H., & Donder, E. (2023). Attitude towards seeking psychological help regarding psychiatric symptoms and stigma in patients with fibromyalgia. European Review for Medical and Pharmacological Sciences, 27(21), 10661–10668. [Google Scholar] [CrossRef]
- Burckhardt, C. S., Clark, S. R., & Bennett, R. M. (1991). The fibromyalgia impact questionnaire: Development and validation. The Journal of Rheumatology, 18(5), 728–733. [Google Scholar]
- Burneo-Garcés, C., Fernández-Alcántara, M., Aguayo-Estremera, R., & Pérez-García, M. (2020). Psychometric properties of the spanish adaptation of the personality assessment inventory in correctional settings: An ESEM study. Journal of Personality Assessment, 102(1), 75–87. [Google Scholar] [CrossRef]
- Cagliyan Turk, A., Erden, E., Eker Buyuksireci, D., Umaroglu, M., & Borman, P. (2024). Prevalence of fibromyalgia syndrome in women with lipedema and its effect on anxiety, depression, and quality of life. Lymphatic Research and Biology, 22(1), 2–7. [Google Scholar] [CrossRef] [PubMed]
- Campos, R. P., Vázquez, I., & Vilhena, E. (2021). Clinical, psychological and quality of life differences in fibromyalgia patients from secondary and tertiary healthcare. European Journal of Pain, 25(3), 558–572. [Google Scholar] [CrossRef]
- Castel, A., Cascón-Pereira, R., & Boada, S. (2021). Memory complaints and cognitive performance in fibromyalgia and chronic pain: The key role of depression. Scandinavian Journal of Psychology, 62(3), 328–338. [Google Scholar] [CrossRef]
- Chang, E. C., Lucas, A. G., Chang, O. D., Angoff, H. D., Li, M., Duong, A. H., Huang, J., Perera, M. J., Sirois, F. M., & Hirsch, J. K. (2019). Relationship between future orientation and pain severity in fibromyalgia patients: Self-compassion as a coping mechanism. Social Work, 64(3), 253–258. [Google Scholar] [CrossRef]
- Ciuffini, R., Cofini, V., Muselli, M., Necozione, S., Piroli, A., & Marrelli, A. (2023). Emotional arousal and valence in patients with fibromyalgia: A pilot study. Frontiers in Pain Research, 4, 1075722. [Google Scholar] [CrossRef]
- Conversano, C., Carmassi, C., Bertelloni, C. A., Marchi, L., Micheloni, T., Carbone, M. G., Pagni, G., Tagliarini, C., Massimetti, G., Bazzichi, L. M., & Dell’osso, L. (2019). Potentially traumatic events, post-traumatic stress disorder and post-traumatic stress spectrum in patients with fibromyalgia. Clinical and Experimental Rheumatology, 37(1), 39–43. [Google Scholar]
- Creed, F. (2022). The risk factors for self-reported fibromyalgia with and without multiple somatic symptoms: The Lifelines cohort study. Journal of Psychosomatic Research, 155, 110745. [Google Scholar] [CrossRef] [PubMed]
- Dell’Osso, L., Bazzichi, L., Consoli, G., Carmassi, C., Carlini, M., Massimetti, E., Giacomelli, C., Bombardieri, S., & Ciapparelli, A. (2009). Manic spectrum symptoms are correlated to the severity of pain and the health-related quality of life in patients with fibromyalgia. Clinical and Experimental Rheumatology, 27(5), S57–S61. [Google Scholar] [PubMed]
- de Souza, J. B., Goffaux, P., Julien, N., Potvin, S., Charest, J., & Marchand, S. (2009). Fibromyalgia subgroups: Profiling distinct subgroups using the Fibromyalgia Impact Questionnaire. A preliminary study. Rheumatology International, 29(5), 509–515. [Google Scholar] [CrossRef] [PubMed]
- Dizner-Golab, A., Lisowska, B., & Kosson, D. (2023). Fibromyalgia—Etiology, diagnosis and treatment including perioperative management in patients with fibromyalgia. Rheumatology, 61(2), 137–148. [Google Scholar] [CrossRef]
- Doreste, A., Pujol, J., Penelo, E., Pérez, V., Blanco-Hinojo, L., Martínez-Vilavella, G., Pardina-Torner, H., Ojeda, F., Monfort, J., & Deus, J. (2024). Exploring the psychopathological profile of fibromyalgia: Insights from the personality assessment inventory and its association with disease impact. Frontiers in Psychology, 15, 1418644. [Google Scholar] [CrossRef]
- Doreste, A., Pujol, J., Penelo, E., Pérez, V., Blanco-Hinojo, L., Martínez-Vilavella, G., Pardina-Torner, H., Ojeda, F., Monfort, J., & Deus, J. (2025). Outlining the psychological profile of persistent depression in fibromyalgia patients through Personality Assessment Inventory (PAI). European Journal of Investigation in Health, Psychology and Education, 15(1), 2. [Google Scholar] [CrossRef]
- Estévez-López, F., Rodriguez-Ayllon, M., Soriano-Maldonado, A., Acosta-Manzano, P., Segura-Jiménez, V., Álvarez-Gallardo, I. C., Pulido-Martos, M., Herrador-Colmenero, M., Geenen, R., Carbonell-Baeza, A., & Delgado-Fernández, M. (2019). Lower fatigue in fit and positive women with fibromyalgia: The al-ándalus project. Pain Medicine, 20(12), 2506–2515. [Google Scholar] [CrossRef]
- Fischer-Jbali, L., Montoro, C., Montoya, P., Halder, W., & Duschek, S. (2021). Central nervous activity during implicit processing of emotional face expressions in fibromyalgia syndrome. Brain Research, 1758, 147333. [Google Scholar] [CrossRef]
- Fischer-Jbali, L., Montoro, C., Montoya, P., Halder, W., & Duschek, S. (2022). Central nervous activity during an emotional Stroop task in fibromyalgia syndrome. International Journal of Psychophysiology, 177, 133–144. [Google Scholar] [CrossRef]
- Font Gayà, T., Bordoy Ferrer, C., Juan Mas, A., Seoane-Mato, D., Álvarez Reyes, F., Delgado Sánchez, M., Martínez Dubois, C., Sánchez-Fernández, S. A., Marena Rojas Vargas, L., García Morales, P. V., Olivé, A., Rubio Muñoz, P., Larrosa, M., Navarro Ricós, N., Sánchez-Piedra, C., Díaz-González, F., Bustabad-Reyes, S., & Working Group Proyecto EPISER. (2016). Prevalence of fibromyalgia and associated factors in Spain. Clinical and Experimental Rheumatology, 38(Suppl. S123), 47–52. [Google Scholar]
- Galvez-Sánchez, C. M., & del Paso, G. A. R. (2020). Diagnostic criteria for fibromyalgia: Critical review and future perspectives. Journal of Clinical Medicine, 9(4), 1219. [Google Scholar] [CrossRef]
- Galvez-Sánchez, C. M., Duschek, S., & del Paso, G. A. R. (2019). Psychological impact of fibromyalgia: Current perspectives. Psychology Research and Behavior Management, 12, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Fontanals, A., Portell, M., García-Blanco, S., Poca-Dias, V., García-Fructuoso, F., López-Ruiz, M., Gutiérrez-Rosado, T., Gomà-I-Freixanet, M., & Deus, J. (2017). Vulnerability to Psychopathology and dimensions of personality in patients with fibromyalgia. The Clinical Journal of Pain, 33(11), 991–997. [Google Scholar] [CrossRef] [PubMed]
- García-Domínguez, M. (2025). Fibromyalgia and inflammation: Unrevealing the connection. Cells, 14(4), 271. [Google Scholar] [CrossRef]
- Garip, Y., Güler, T., Tuncer, Ö. B., & Önen, S. (2019). Type D personality is associated with disease severity and poor quality of life in turkish patients with fibromyalgia syndrome: A cross-sectional study. Archives of Rheumatology, 35(1), 13–19. [Google Scholar] [CrossRef] [PubMed]
- Gelonch, O., Garolera, M., Valls, J., Castellà, G., Varela, O., Rosselló, L., Pifarre, J., & Gualtieri, C. (2018). The effect of depressive symptoms on cognition in patients with fibromyalgia. PLoS ONE, 13(7), e0200057. [Google Scholar] [CrossRef]
- Gil-Ugidos, A., Rodríguez-Salgado, D., Pidal-Miranda, M., Samartin-Veiga, N., Fernández-Prieto, M., & Carrillo-De-La-Peña, M. T. (2021). Working memory performance, pain and associated clinical variables in women with fibromyalgia. Frontiers in Psychology, 12, 747533. [Google Scholar] [CrossRef]
- Goldway, N., Petro, N. M., Ablin, J., Keil, A., Ben Simon, E., Zamir, Y., Weizman, L., Greental, A., Hendler, T., & Sharon, H. (2022). Abnormal visual evoked responses to emotional cues correspond to diagnosis and disease severity in fibromyalgia. Frontiers in Behavioral Neuroscience, 16, 852133. [Google Scholar] [CrossRef]
- Gonzalez, B., Novo, R., & Ferreira, A. S. (2020). Fibromyalgia: Heterogeneity in personality and psychopathology and its implications. Psychology, Health & Medicine, 25(6), 703–709. [Google Scholar] [CrossRef]
- Gota, C. E., Kaouk, S., & Wilke, W. S. (2017). The impact of depressive and bipolar symptoms on socioeconomic status, core symptoms, function and severity of fibromyalgia. International Journal of Rheumatic Diseases, 20(3), 326–339. [Google Scholar] [CrossRef] [PubMed]
- Hadlandsmyth, K., Dailey, D. L., Rakel, B. A., Zimmerman, M. B., Vance, C. G., Merriwether, E. N., Chimenti, R. L., Geasland, K. M., Crofford, L. J., & A Sluka, K. (2020). Somatic symptom presentations in women with fibromyalgia are differentially associated with elevated depression and anxiety. Journal of Health Psychology, 25(6), 819–829. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, J. K., Altier, H. R., Offenbächer, M., Toussaint, L., Kohls, N., & Sirois, F. M. (2021). Positive psychological factors and impairment in rheumatic and musculoskeletal disease: Do psychopathology and sleep quality explain the linkage? Arthritis Care & Research, 73(1), 55–64. [Google Scholar] [CrossRef]
- Islam, Z., D’sIlva, A., Raman, M., & Nasser, Y. (2022). The role of mind body interventions in the treatment of irritable bowel syndrome and fibromyalgia. Frontiers in Psychiatry, 13, 1076763. [Google Scholar] [CrossRef]
- Izquierdo-Alventosa, R., Inglés, M., Cortés-Amador, S., Gimeno-Mallench, L., Chirivella-Garrido, J., Kropotov, J., & Serra-Añó, P. (2020). Low-intensity physical exercise improves pain catastrophizing and other psychological and physical aspects in women with fibromyalgia: A randomized controlled trial. International Journal of Environmental Research and Public Health, 17(10), 3634. [Google Scholar] [CrossRef]
- İnal, Ö., Aras, B., & Salar, S. (2020). Investigation of the relationship between kinesiophobia and sensory processing in fibromyalgia patients. Somatosensory & Motor Research, 37(2), 92–96. [Google Scholar] [CrossRef]
- Jacobsen, H. B., Brun, A., Stubhaug, A., & Reme, S. E. (2023). Stress specifically deteriorates working memory in peripheral neuropathic pain and fibromyalgia. Brain Communications, 5(4), fcad194. [Google Scholar] [CrossRef]
- Jurado-Priego, L. N., Cueto-Ureña, C., Ramírez-Expósito, M. J., & Martínez-Martos, J. M. (2024). Fibromyalgia: A review of the pathophysiological mechanisms and multidisciplinary treatment strategies. Biomedicines, 12(7), 1543. [Google Scholar] [CrossRef]
- Karlin, B. E., Creech, S. K., Grimes, J. S., Clark, T. S., Meagher, M. W., & Morey, L. C. (2005). The Personality Assessment Inventory with chronic pain patients: Psychometric properties and clinical utility. Journal of Clinical Psychology, 61(12), 1571–1585. [Google Scholar] [CrossRef]
- Keller, D., de Gracia, M., & Cladellas, R. (2011). Subtipos de pacientes con fibromialgia, características psicopatológicas y calidad de vida [Subtypes of patients with fibromyalgia, psychopathological characteristics and quality of life]. Actas Españolas de Psiquiatría, 39(5), 273–279. (In Spanish). [Google Scholar]
- Kim, S., Dowgwillo, E. A., & Kratz, A. L. (2023). Emotional dynamics in fibromyalgia: Pain, fatigue, and stress moderate momentary associations between positive and negative emotions. The Journal of Pain, 24(9), 1594–1603. [Google Scholar] [CrossRef]
- Kocyigit, B. F., & Akyol, A. (2022). Fibromyalgia syndrome: Epidemiology, diagnosis and treatment. Rheumatology, 60(6), 413–421. [Google Scholar] [CrossRef] [PubMed]
- Kudlow, P., Rosenblat, J., Weissman, C., Cha, D., Kakar, R., McIntyre, R., & Sharma, V. (2015). Prevalence of fibromyalgia and co-morbid bipolar disorder: A systematic review and meta-analysis. Journal of Affective Disorders, 188, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Lahat-Birka, N. M., Boussi-Gross, R. M., Ben Ari, A., Efrati, S., & Ben-David, S. (2024). Retrospective analysis of fibromyalgia: Exploring the interplay between various triggers and fibromyalgia’s severity. The Clinical Journal of Pain, 40(10), 578–587. [Google Scholar] [CrossRef] [PubMed]
- Levine, D., & Horesh, D. (2020). Suicidality in fibromyalgia: A systematic review of the literature. Frontiers in Psychiatry, 11, 535368. [Google Scholar] [CrossRef]
- López-Ruiz, M., Losilla, J. M., Monfort, J., Portell, M., Gutiérrez, T., Poca, V., Garcia-Fructuoso, F., Llorente, J., Garcia-Fontanals, A., Deus, J., & Doering, S. (2019). Central sensitization in knee osteoarthritis and fibromyalgia: Beyond depression and anxiety. PLoS ONE, 14(12), e0225836. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Luciano, J. V., Forero, C. G., Cerdà-Lafont, M., Peñarrubia-María, M. T., Fernández-Vergel, R., Cuesta-Vargas, A. I., Ruíz, J. M., Rozadilla-Sacanell, A., Sirvent-Alierta, E., Santo-Panero, P., García-Campayo, J., Serrano-Blanco, A., Pérez-Aranda, A., & Rubio-Valera, M. (2016). Functional status, quality of life, and costs associated with fibromyalgia subgroups: A latent profile analysis. The Clinical Journal of Pain, 32(10), 829–840. [Google Scholar] [CrossRef]
- Martínez, M., Sánchez, A., Cáliz, R., & Miró, E. (2021). Psychopathology as a moderator of the relationship between physical symptoms and impairment in fibromyalgia patients. Psicothema, 2(33), 214–221. [Google Scholar] [CrossRef]
- Maurel, S., Giménez-Llort, L., Alegre-Martin, J., & Castro-Marrero, J. (2023). Hierarchical cluster analysis based on clinical and neuropsychological symptoms reveals distinct subgroups in fibromyalgia: A population-based cohort study. Biomedicines, 11(10), 2867. [Google Scholar] [CrossRef]
- Meade, E., & Garvey, M. (2022). The role of neuro-immune interaction in chronic pain conditions; functional somatic syndrome, neurogenic inflammation, and peripheral neuropathy. International Journal of Molecular Sciences, 23(15), 8574. [Google Scholar] [CrossRef] [PubMed]
- Monterde, S., Salvat, I., Montull, S., & Fernández-Ballart, J. (2004). Validation of the spanish version of the fibromyalgia impact questionnaire. Revista Española de Reumatología, 31(9), 507–513. [Google Scholar]
- Morey, L. C. (1991). Personality assessment inventory–Professional manual. Psychological Assessment Resources. [Google Scholar]
- Morey, L. C., & Alarcón, M. O. T. (2013). PAI: Inventario de evaluación de la personalidad. Manual de corrección, aplicación e interpretación. TEA Ediciones. [Google Scholar]
- Munipalli, B., Chauhan, M., Morris, A. M., Ahmad, R., Fatima, M., Allman, M. E., Niazi, S. K., & Bruce, B. K. (2024). Recognizing and treating major depression in fibromyalgia: A narrative primer for the non-psychiatrist. Journal of Primary Care & Community Health, 15, 21501319241281221. [Google Scholar] [CrossRef]
- Nadal-Nicolás, Y., Rubio-Arias, J. Á., Martínez-Olcina, M., Reche-García, C., Hernández-García, M., & Martínez-Rodríguez, A. (2020). Effects of manual therapy on fatigue, pain, and psychological aspects in women with fibromyalgia. International Journal of Environmental Research and Public Health, 17(12), 4611. [Google Scholar] [CrossRef]
- Olfa, S., Bouden, S., Sahli, M., Tekaya, A. B., Rouached, L., Rawdha, T., Mahmoud, I., & Abdelmoula, L. (2023). Fibromyalgia in spondyloarthritis: Prevalence and effect on disease activity and treatment. Current Rheumatology Reviews, 19(2), 214–221. [Google Scholar] [CrossRef]
- Ortiz-Tallo, M., Cardenal, V., Ferragut, M., & Cerezo, M. V. (2011). Personalidad y síndromes clínicos: Un estudio con el MCMI-III basado en una muestra española. Revista de Psicopatología y Psicología Clínica, 16(1), 49. [Google Scholar] [CrossRef]
- Pacheco-Barrios, K., Teixeira, P. E. P., Martinez-Magallanes, D., Neto, M. S., Pichardo, E. A., Camargo, L., Lima, D., Cardenas-Rojas, A., & Fregni, F. (2024). Brain compensatory mechanisms in depression and memory complaints in fibromyalgia: The role of theta oscillatory activity. Pain Medicine, 25(8), 514–522. [Google Scholar] [CrossRef] [PubMed]
- Pallanti, S., Porta, F., & Salerno, L. (2021). Adult attention deficit hyperactivity disorder in patients with fibromyalgia syndrome: Assessment and disabilities. Journal of Psychiatric Research, 136, 537–542. [Google Scholar] [CrossRef]
- Pujol, J., Blanco-Hinojo, L., Doreste, A., Ojeda, F., Martínez-Vilavella, G., Pérez-Sola, V., Deus, J., & Monfort, J. (2022). Distinctive alterations in the functional anatomy of the cerebral cortex in pain-sensitized osteoarthritis and fibromyalgia patients. Arthritis Research & Therapy, 24(1), 252. [Google Scholar] [CrossRef]
- Pujol, J., Macià, D., Garcia-Fontanals, A., Blanco-Hinojo, L., López-Solà, M., Garcia-Blanco, S., Poca-Dias, V., Harrison, B. J., Contreras-Rodríguez, O., Monfort, J., Garcia-Fructuoso, F., & Deus, J. (2014). The contribution of sensory system functional connectivity reduction to clinical pain in fibromyalgia. Pain, 155(8), 1492–1503. [Google Scholar] [CrossRef] [PubMed]
- Puşuroğlu, M., Topaloğlu, M. S., Hocaoğlum, Ç., & Yıldırım, M. (2023). Expressing emotions, rejection sensitivity, and attachment in patients with fibromyalgia. Turkish Journal of Physical Medicine and Rehabilitation, 69(3), 303–308. [Google Scholar] [CrossRef]
- Rivera, J., & González, T. (2004). The Fibromyalgia Impact Questionnaire: A validated Spanish version to assess the health status in women with fibromyalgia. Clinical and Experimental Rheumatology, 22, 554–560. [Google Scholar] [PubMed]
- Rizzi, M., Radovanovic, D., Santus, P., Airoldi, A., Frassanito, F., Vanni, S., Cristiano, A., Masala, I. F., & Sarzi-Puttini, P. (2017). Influence of autonomic nervous system dysfunction in the genesis of sleep disorders in fibromyalgia patients. Clinical and Experimental Rheumatology, 35(3), 74–80. [Google Scholar] [CrossRef]
- Robbins, J. M., Kirmayer, L. J., & Kapusta, M. A. (1990). Illness worry and disability in fibromyalgia syndrome. The International Journal of Psychiatry in Medicine, 20(1), 49–63. [Google Scholar] [CrossRef]
- Romanov, D. V., Nasonova, T. I., Isaikin, A. I., Filileeva, O. V., Sheyanov, A. M., Iuzbashian, P. G., Voronova, E. I., & Parfenov, V. A. (2023). Personality disorders and traits of ABC clusters in fibromyalgia in a neurological setting. Biomedicines, 11(12), 3162. [Google Scholar] [CrossRef] [PubMed]
- Romeo, A., Benfante, A., Geminiani, G. C., & Castelli, L. (2022a). Personality, defense mechanisms and psychological distress in women with fibromyalgia. Behavioral Sciences, 12(1), 10. [Google Scholar] [CrossRef]
- Romeo, A., Tesio, V., Ghiggia, A., Di Tella, M., Geminiani, G. C., Farina, B., & Castelli, L. (2022b). Traumatic experiences and somatoform dissociation in women with fibromyalgia. Psychological Trauma: Theory, Research, Practice, and Policy, 14(1), 116–123. [Google Scholar] [CrossRef]
- Sarzi-Puttini, P., Giorgi, V., Atzeni, F., Gorla, R., Kosek, E., Choy, E. H., Bazzichi, L., Häuser, W., Ablin, J. N., Aloush, V., Buskila, D., Amital, H., Da Silva, J. A. P., Perrot, S., Morlion, B., Polati, E., Schweiger, V., Coaccioli, S., Varrassi, G., … Batticciotto, A. (2021). Diagnostic and therapeutic care pathway for fibromyalgia. Clinical and Experimental Rheumatology, 39(Suppl. 130(3)), 120–127. [Google Scholar] [CrossRef] [PubMed]
- Sarzi-Puttini, P., Giorgi, V., Marotto, D., & Atzeni, F. (2020). Fibromyalgia: An update on clinical characteristics, aetiopathogenesis and treatment. Nature Reviews Rheumatology, 16(11), 645–660. [Google Scholar] [CrossRef]
- Sedda, S., Cadoni, M. P. L., Medici, S., Aiello, E., Erre, G. L., Nivoli, A. M., Carru, C., & Coradduzza, D. (2025). Fibromyalgia, depression, and autoimmune disorders: An interconnected web of inflammation. Biomedicines, 13(2), 503. [Google Scholar] [CrossRef]
- Serrat, M., Sanabria-Mazo, J. P., Almirall, M., Musté, M., Feliu-Soler, A., Méndez-Ulrich, J. L., Sanz, A., & Luciano, J. V. (2021). Effectiveness of a multicomponent treatment based on pain neuroscience education, therapeutic exercise, cognitive behavioral therapy, and mindfulness in patients with fibromyalgia (FIBROWALK study): A randomized controlled trial. PTJ: Physical Therapy & Rehabilitation Journal, 101(12), pzab200. [Google Scholar] [CrossRef]
- Siracusa, R., Di Paola, R., Cuzzocrea, S., & Impellizzeri, D. (2021). Fibromyalgia: Pathogenesis, mechanisms, diagnosis and treatment options update. International Journal of Molecular Sciences, 22(8), 3891. [Google Scholar] [CrossRef]
- Taylor, S., Noor, N., Urits, I., Paladini, A., Sadhu, M. S., Gibb, C., Carlson, T., Myrcik, D., Varrassi, G., & Viswanath, O. (2021). Complex regional pain syndrome: A comprehensive review. Pain and Therapy, 10(2), 875–892, (Erratum in “Complex regional pain syndrome: A comprehensive review”, 2021, Pain and Therapy, 10(2), 893–894. https://doi.org/10.1007/s40122-021-00291-8). [Google Scholar] [CrossRef]
- Toussaint, L., Vincent, A., McAllister, S. J., & Whipple, M. (2015). Intra- and inter-patient symptom variability in fibromyalgia: Results of a 90-day assessment. Musculoskeletal Care, 13(2), 93–100. [Google Scholar] [CrossRef] [PubMed]
- Trucharte, A., Leon, L., Castillo-Parra, G., Magán, I., Freites, D., & Redondo, M. (2020). Emotional regulation processes: Influence on pain and disability in fibromyalgia patients. Clinical and Experimental Rheumatology, 38(1), 40–46. [Google Scholar]
- Van Alboom, M. M., De Ruddere, L., Kindt, S., Loeys, T., Van Ryckeghem, D., Bracke, P., Mittinty, M. M., & Goubert, L. (2021). Well-being and perceived stigma in individuals with rheumatoid arthritis and fibromyalgia: A daily diary study. The Clinical Journal of Pain, 37(5), 349–358. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A., Hoskin, T. L., Whipple, M. O., Clauw, D. J., Barton, D. L., Benzo, R. P., & A Williams, D. (2014). OMERACT-based fibromyalgia symptom subgroups: An exploratory cluster analysis. Arthritis Research & Therapy, 16(5), 463. [Google Scholar] [CrossRef]
- Vittersø, A. D., Halicka, M., Buckingham, G., Proulx, M. J., & Bultitude, J. H. (2022). The sensorimotor theory of pathological pain revisited. Neuroscience & Biobehavioral Reviews, 139, 104735. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F. (1999). Determinants of WOMAC function, pain and stiffness scores: Evidence for the role of low back pain, symptom counts, fatigue and depression in osteoarthritis, rheumatoid arthritis and fibromyalgia. Rheumatology, 38(4), 355–361. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F., & Rasker, J. J. (2021). The evolution of fibromyalgia, its concepts, and criteria. Cureus, 13(11), e20010. [Google Scholar] [CrossRef]
- Yuan, S. L. K., Matsutani, L. A., & Marques, A. P. (2015). Effectiveness of different styles of massage therapy in fibromyalgia: A systematic review and meta-analysis. Manual Therapy, 20(2), 257–264. [Google Scholar] [CrossRef] [PubMed]
- Zetterman, T., Markkula, R., Partanen, J. V., Miettinen, T., Estlander, A., & Kalso, E. (2021). Muscle activity and acute stress in fibromyalgia. BMC Musculoskeletal Disorders, 22(1), 183. [Google Scholar] [CrossRef]
- Zinchuk, M., Kustov, G., Tumurov, D., Zhuravlev, D., Bryzgalova, Y., Spryshkova, M., Yakovlev, A., & Guekht, A. (2025). Fibromyalgia in patients with non-psychotic mental disorders: Prevalence, associated factors and validation of a brief screening instrument. European Journal of Pain, 29(2), e4730. [Google Scholar] [CrossRef] [PubMed]
| Descriptive Data M (SD) | |
|---|---|
| Age (years) | 48.86 (8.32) |
| Fibromyalgia tender points (0–18) | 17.21 (1.39) |
| Diagnosis Time in Years | 6.70 (6.71) |
| Symptom Onset Time (Years) | 14.94 (11.22) |
| Educational attainment (%) | |
| Primary Studies | 10.0 |
| Secondary Studies | 11.4 |
| Bachelor | 17.1 |
| Professional Studies | 32.8 |
| University | 28.5 |
| Stable medication regime (%) | |
| Analgesic (NSAIDs and/or Opioids) | 68.6 |
| Anti-inflammatory | 58.2 |
| Antidepressant | 73.1 |
| Type of antidepressant (%) | |
| ISRS | 31.3 |
| Dual | 17.9 |
| Tricyclic | 25.3 |
| Benzodiazepine | 37.3 |
| Type of benzodiazepine (%) | |
| Short-acting | 14.9 |
| Intermediate-acting | 4.4 |
| Long-acting | 17.9 |
| FM symptoms (FIQ 1) | |
| FIQ global score (0–100) M (SD) | 66.82 (13.67) |
| Physical Functioning Dimension | |
| Physical function (0–10) M (SD) | 5.85 (2.25) |
| Global Impact Dimension | |
| Well-being (0–10) M (SD) | 8.04 (2.61) |
| Work absence (0–10) M (SD) | 4.33 (3.59) |
| Symptoms Dimension | |
| Job performance (0–10) M (SD) | 6.99 (1.95) |
| Pain (0–10) M (SD) | 7.14 (1.64) |
| Fatigue (0–10) M (SD) | 7.84 (1.37) |
| Morning tiredness (0–10) M (SD) | 7.46 (2.08) |
| Stiffness (0–10) M (SD) | 6.80 (2.46) |
| Anxiety (0–10) M (SD) | 6.60 (2.65) |
| Depression (0–10) M (SD) | 5.54 (2.90) |
| Subgroup | Wilk’s Lambda | Chi-Square | Canonical Correlation | Eigenvalue | M-Box | p-Value (M-Box) |
|---|---|---|---|---|---|---|
| Functional | 0.248 | 92.756 | 0.867 | 3.034 | 9.265 | 0.192 |
| Physical–somatic | 0.277 | 84.053 | 0.850 | 2.608 | 52.919 | <0.001 |
| Emotional | 0.294 | 82.129 | 0.841 | 2.407 | 42.126 | <0.001 |
| Variable | Wilk’s Lambda | F-Value | p-Value | Standard Coefficient | Structure Coefficient |
|---|---|---|---|---|---|
| Functional domain | |||||
| Physical Function | 0.992 | 0.57 | 0.454 | −0.364 | 0.052 |
| Work Absence | 0.277 | 177.26 | <0.001 | 1.129 | 0.927 |
| Job Performance | 0.923 | 5.71 | 0.020 | −0.165 | 0.166 |
| Physical–somatic domain | |||||
| Well-being | 0.713 | 27.35 | <0.001 | 0.831 | 0.393 |
| Pain | 0.738 | 24.16 | <0.001 | 0.664 | 0.369 |
| Fatigue | 0.884 | 8.94 | 0.004 | −0.378 | 0.224 |
| Morning tiredness | 0.489 | 71.07 | <0.001 | 0.564 | 0.633 |
| Stiffness | 0.664 | 34.42 | <0.001 | 0.354 | 0.440 |
| Emotional domain | |||||
| Depression | 0.479 | 73.91 | <0.001 | 0.583 | 0.672 |
| Anxiety | 0.385 | 108.83 | <0.001 | 0.746 | 0.815 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doreste, A.; Pujol, J.; Penelo, E.; Pérez, V.; Blanco-Hinojo, L.; Martínez-Vilavella, G.; Ojeda, F.; Monfort, J.; Deus, J. Personality Assessment Inventory in Fibromyalgia: Links to Functional, Physical–Somatic, and Emotional Impact. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 149. https://doi.org/10.3390/ejihpe15080149
Doreste A, Pujol J, Penelo E, Pérez V, Blanco-Hinojo L, Martínez-Vilavella G, Ojeda F, Monfort J, Deus J. Personality Assessment Inventory in Fibromyalgia: Links to Functional, Physical–Somatic, and Emotional Impact. European Journal of Investigation in Health, Psychology and Education. 2025; 15(8):149. https://doi.org/10.3390/ejihpe15080149
Chicago/Turabian StyleDoreste, Andrea, Jesus Pujol, Eva Penelo, Víctor Pérez, Laura Blanco-Hinojo, Gerard Martínez-Vilavella, Fabiola Ojeda, Jordi Monfort, and Joan Deus. 2025. "Personality Assessment Inventory in Fibromyalgia: Links to Functional, Physical–Somatic, and Emotional Impact" European Journal of Investigation in Health, Psychology and Education 15, no. 8: 149. https://doi.org/10.3390/ejihpe15080149
APA StyleDoreste, A., Pujol, J., Penelo, E., Pérez, V., Blanco-Hinojo, L., Martínez-Vilavella, G., Ojeda, F., Monfort, J., & Deus, J. (2025). Personality Assessment Inventory in Fibromyalgia: Links to Functional, Physical–Somatic, and Emotional Impact. European Journal of Investigation in Health, Psychology and Education, 15(8), 149. https://doi.org/10.3390/ejihpe15080149








