Abstract
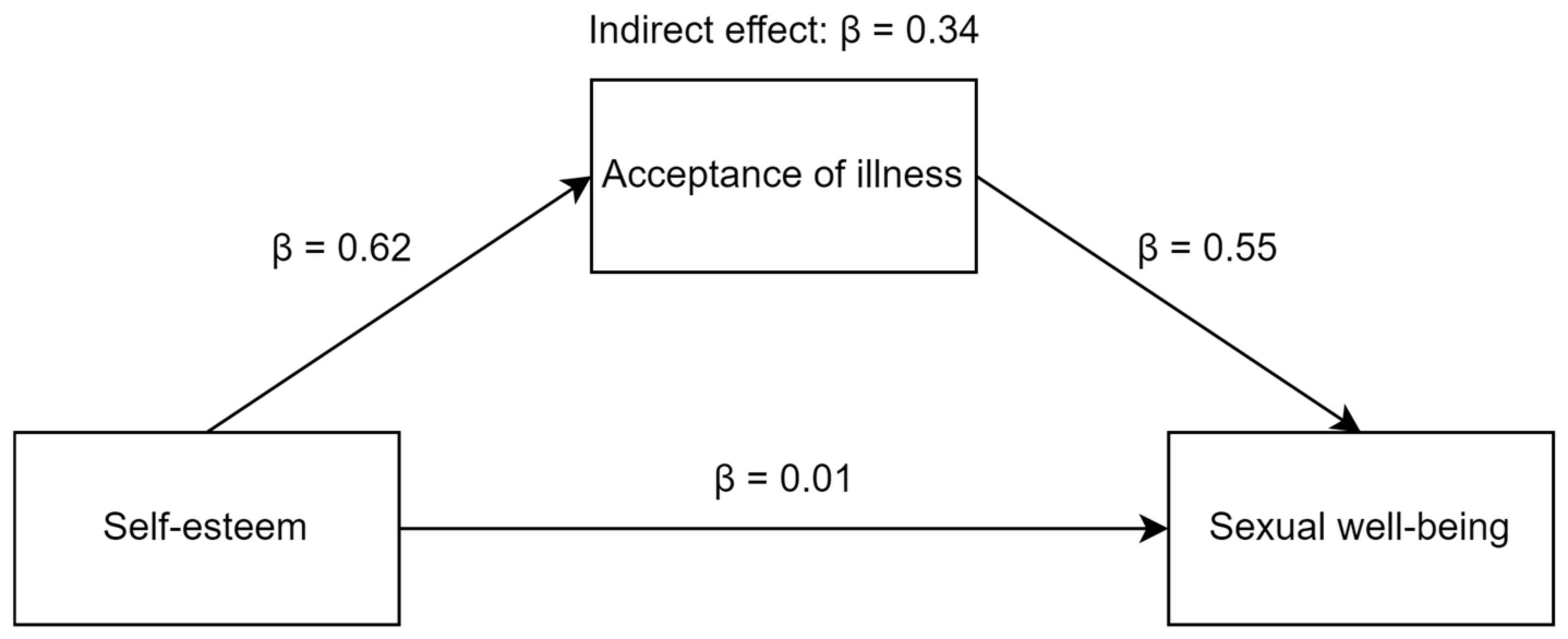
Schizophrenia is one of the most severe chronic mental illnesses. It drastically changes an individual’s life and well-being. Sexual well-being in schizophrenia is often sidelined, even though it is one of the main areas for maintaining quality of life. Based on the conservation of resources theory (COR) and empirical data, we assume that self-esteem and acceptance of illness help in coping with schizophrenia and maintaining sexual well-being. This pilot study aimed to determine the relationship between self-esteem, acceptance of illness, and sexual well-being in Polish individuals with schizophrenia. The results of 60 individuals were included in this study. In the present study, the Self-Esteem Scale (SES), Acceptance of Illness Scale (AIS), and Short Sexual Well-Being Scale (SSWBS) were used. The study showed a significant association between self-esteem, acceptance of illness, and sexual well-being. Self-esteem (β = 0.62) and acceptance of illness (β = 0.55) acted as positive and significant predictors of sexual well-being in individuals with schizophrenia. Acceptance of illness was also found to play a mediating role between self-esteem and sexual well-being in people with schizophrenia (indirect effect: β = 0.34; LLCI = 0.063; ULCI = 0.839). The current pilot study demonstrates the relationship between self-esteem, acceptance of illness, and sexual well-being. Our findings highlight the significant role of acceptance of illness in maintaining sexual well-being among individuals with schizophrenia.
1. Introduction
Schizophrenia is one of the most severe chronic illnesses in mental health. It is characterized by a diverse clinical image. Patients with a diagnosis of schizophrenia struggle with positive, negative and cognitive symptoms [1]. The course of schizophrenia varies and is unpredictable but, for most patients, the illness is associated with experiencing exacerbations and readmissions to hospitals and periods of remission [2]. Schizophrenia can drastically change an individual’s life and well-being. More severe negative symptoms of schizophrenia correlate with lower psychological well-being and many constructs influencing well-being [3,4]. Additionally, negative, positive and cognitive symptoms are negatively related to the quality of life in schizophrenia [5]. An area that is often overlooked in discussions is the sex lives of individuals with schizophrenia, even though sexual dysfunctions in this group are common and can significantly reduce the sexual well-being of patients [6,7]. Barker and Vigod [8] noted in their review that women with a diagnosis of schizophrenia showed lower sexual needs due to an impaired libido. In addition, both positive and negative symptoms of schizophrenia have been shown to intensify sexual dysfunction and decrease sexual satisfaction [8].
McCann and colleagues [9] also point out that, although in clinical practice the quality of services has improved significantly over recent years, there are still problems in supporting patients with their sexual health. In the face of these reports, it is important to help individuals with schizophrenia maintain their sexual well-being by influencing significant predictors of sexual well-being. Based on the fact that personal resources play an important role in the functioning of individuals with schizophrenia [10,11,12], we decided to investigate the associations between sexual well-being, acceptance of illness and self-esteem, which have a significant impact on intimate life and sexuality in individuals with schizophrenia.
1.1. The Relationship between Self-Esteem and Sexual Well-Being in Schizophrenia
Self-esteem is widely discussed in the literature in the context of mental illnesses [13,14], including among individuals with schizophrenia spectrum disorders [15,16]. Self-esteem appears to have a significant impact on sex life [17] and is defined as the subjective attitude towards the self [18,19]. According to Rosenberg [18], people have different attitudes towards different objects, including themselves. Individuals with high self-esteem have a positive attitude towards themselves and the belief that they are a “good enough” and valuable person. In turn, negative attitudes to self are expressed by negative thinking about oneself and dissatisfaction with oneself and one’s accomplishments. Coopersmith [20] states that self-esteem arises from making evaluations about oneself and is often reflected in attitudes and expressed opinions about oneself. Based on this theoretical perspective, attention is directed towards seeing one’s potential and chances for success, self-confidence and self-respect. Despite different theoretical approaches to the concept of self-esteem, subjective positive evaluation of self can positively affect emotional and physical satisfaction with one’s sexuality and sexual relationships.
Empirical studies mainly show associations between self-esteem and sexual satisfaction, also among individuals with somatic and mental illnesses [17,21,22]. However, sexual well-being cannot be equated with sexual satisfaction [23,24]. Stephenson and Meston [25] consider sexual satisfaction as one component of sexual well-being. Sexual well-being is based on emotional, sexual and cognitive satisfaction with one’s sexuality and sexual relationships, whereas sexual satisfaction only relates to the physical component of human sexuality [23,24,26,27]. Self-esteem is related to many constructs influencing our sexual well-being. Robinson and Cameron [28] showed relationships between self-esteem and satisfaction and commitment in relationships. Individuals with higher self-esteem were found to be more engaged in their relationships and to experience greater relationship satisfaction. Other research indicates that a higher level of self-esteem is associated with a greater ability to communicate about satisfying sexual behaviors in intimate relationships [29]. It is also related to greater sexual assertiveness [30]. Sprecher and Hendrick [31] found that self-esteem is associated with self-disclosure in an intimate relationship. On the other hand, self-disclosure is related to greater well-being [32]. A lower level of self-esteem is also associated with indirectly seeking support from a partner, although this strategy often leads to rejection from the partner [33]. Additionally, Tayebi and colleagues [34] showed that lower self-esteem is associated with higher rates of sexual dysfunction. Also, the direct relationship between self-esteem and sexual well-being has been confirmed in previous studies by Gerymski et al. [24].
1.2. The Acceptance of Schizophrenia, Self-Esteem and Sexual Well-Being
The process of adaptation in schizophrenia is extremely difficult for patients, due to the unpredictable course of this illness, its symptoms and pharmacotherapy, which play a significant role during treatment [1]. Acceptance of illness, especially a serious one, is a major challenge for the patient. Because schizophrenia is a chronic illness, it somewhat forces the individual to adapt to a different lifestyle. According to Zauszniewski and colleagues [35], acceptance of illness is defined as an adaptation to other conditions of life, including limitations resulting from the illness. It is also defined as a process during which an individual gradually adapts to a new situation [36,37]. During this process, the person integrates the illness with other characteristics and their lifestyle. According to Rüsch and Corrigan [38], working on acceptance of illness is one element of motivational interviewing, which is a form of help for individuals with schizophrenia.
Empirical studies show that personal resources play a significant role in the process of adaptation to illness. Studies indicate that self-esteem is associated with acceptance of illness [39,40]. The level of acceptance of the illness is visible in the individual’s daily functioning in life. Simmons and colleagues [41] found that acceptance of illness is related to interpersonal relationships. A lower level of acceptance of the illness is associated with greater problems with social relationships. Individuals who accept their illness are open to the world and people, and do not avoid social encounters. Reconciliation with the illness and acceptance of this situation impacts on health-related quality of life [36,37,42]. In addition, Lysaker and colleagues [43] pointed out that insight into one’s illness is associated with a greater quality of life in schizophrenia spectrum disorders. Based on these theoretical and empirical reports, we can assume that a higher level of acceptance of the illness will also be associated with greater well-being in terms of one’s sexuality and sex life.
1.3. The Potential Indirect Effect
No previous research has investigated the relationship between self-esteem, acceptance of illness and sexual well-being in individuals with schizophrenia. To date, we have found only one study related to this subject, which is focused on a different group of patients. Furmańska et al. [17] studied the relationship between acceptance of illness, self-esteem, sexual satisfaction, level of disability, duration of treatment and time of diagnosis in patients with multiple sclerosis. They found that acceptance of illness was not related to self-esteem and sexual satisfaction in the studied group of individuals, but showed that self-esteem was moderately related to sexual satisfaction in multiple sclerosis patients. This is a single piece of evidence for a relationship between the mentioned variables, and therefore, should be further investigated. Moreover, this study does not address self-esteem, acceptance of illness and sexual well-being in individuals with schizophrenia. Many personal resources impact one’s sexuality, sex life and intimate relationships, for instance: personality traits, self-acceptance and self-esteem [17,24,29,44]. All these psychological variables also support the process of adaptation to the situation of illness. Therefore, we can assume that self-esteem does not directly affect sexual well-being, but through the mediation of acceptance of the illness. Acceptance of illness leads to minimizing the impact of the illness on life and favors greater sexual well-being. This hypothesis is also supported by the conservation of resources theory (COR), which states that resources facilitate survival or enable the acquisition of others that help in coping with a critical life situation. In the situation of struggling with schizophrenia, acceptance of the illness increases coping effectiveness, reduces distress, and thus contributes to maintaining well-being in the sphere of sexuality and sex life. Previous studies have also shown that acceptance of illness plays a mediating role between some variables related to self-esteem and sexual well-being. For example, acceptance of illness mediates the relationship between cancer-related complaints and psychological distresses [45]. The mediating role of acceptance of illness is also significant in the relationship between neurological disability and quality of life and its two spheres—the physical sphere and the mental sphere [36].
1.4. The Aim of This Study
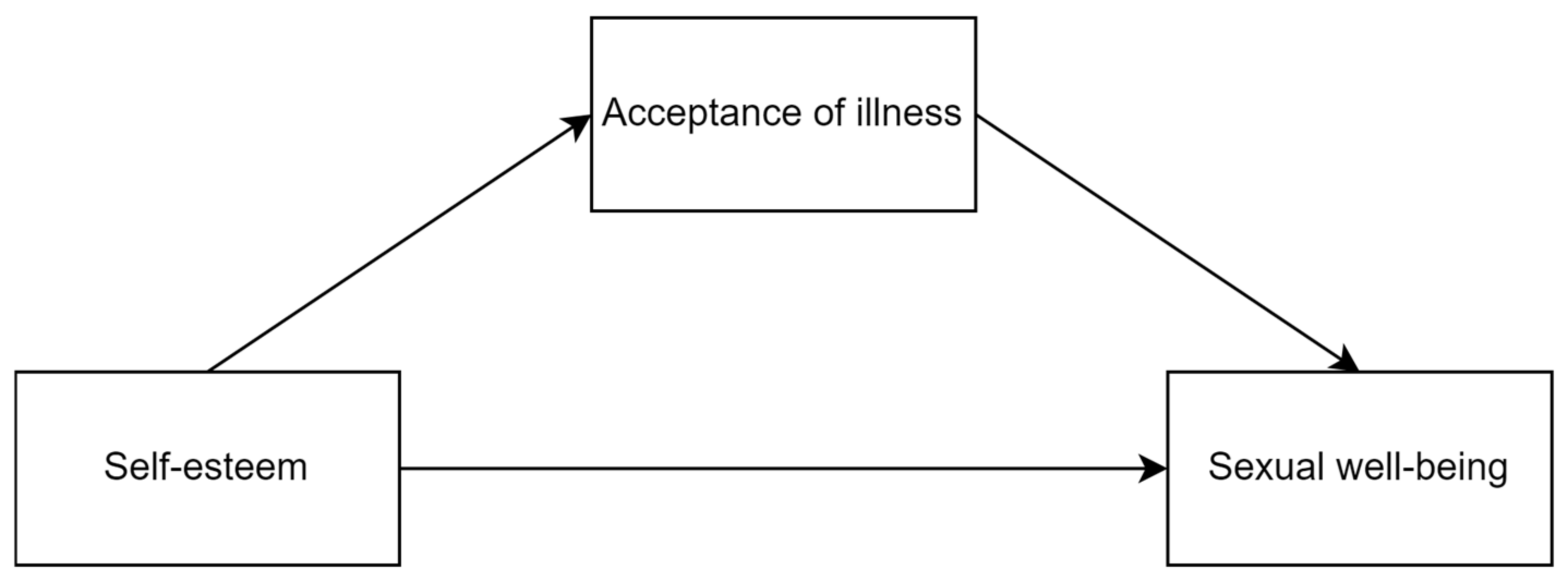
This pilot study aimed to extend previous research on the relationship between self-esteem, acceptance of illness and sexual well-being. It is one of the first studies to verify the relationship between those three variables in individuals with schizophrenia and to assess a new measurement of sexual well-being (the Short Sexual Well-Being Scale) in this group of people. Additionally, it is the first to verify the role of the acceptance of illness in the sexual sphere. Based on prior studies, we formulated the following hypotheses: (1) self-esteem is positively related to acceptance of illness, (2) both self-esteem and acceptance of illness are positively related to sexual well-being and (3) acceptance of illness is a mediator in the relationship between self-esteem and sexual well-being (see Figure 1).
Figure 1.
The visualization of the hypothesized mediation model.
2. Materials and Methods
2.1. Participants and Procedure
The presented pilot study participants were recruited through support groups for people diagnosed with schizophrenia in Poland. All study participants were invited to participate in this study based on an online invitation. Those who were willing to participate, applied to us based on the contact information contained in the invitation. Inclusion criteria were the following: (1) having a diagnosis in the range of F20.0–F20.9 according to the ICD-10 diagnostic manual, (2) being at least 18 years old, (3) being a person whose mother tongue is Polish and (4) having the ability to give informed consent. Exclusion criteria were the following: (1) not attending psychiatrist consultations, (2) being hospitalized in the last 30 days and (3) inability to fill out a questionnaire for any reason. The questionnaires were delivered to the individuals by a trained study assistant. The study participants were informed about the anonymity of the study. They could stop filling out the questionnaires at any time and without giving any reason. All respondents gave verbal and on-paper (by answering the question: Do you consent to participate in the study?) consent to participate in this study.
Initially, 64 individuals were recruited to participate in the study. However, four individuals were excluded based on the inclusion and exclusion criteria. Therefore, 60 Polish individuals with schizophrenia took part in this study, including 31 women and 29 men, aged between 18 and 58 years (M = 31.27; SD = 9.04). More detailed information is available in Table 1.

Table 1.
Characteristics of the studied sample.
2.2. Measures
Three scales were used in the present pilot study. Well-known and broadly available Rosenberg’s Self-Esteem Scale (SES) was used. SES is a 10-item scale on a 4-point answer scale, ranging from 1 (I definitely agree) to 4 (I definitely disagree). It measures self-esteem with items such as: I feel that I have a number of good qualities. The SES measures a global level of self-esteem, without any subscales. In this scale, a higher SES score means higher self-esteem [18]. In the present study, SES was characterized by good reliability (Cronbach’s alpha = 0.89).
Additionally, the Acceptance of Illness Scale (AIS). It is an 8-item scale on a 5-point answer scale (1—I definitely agree; 5—I definitely disagree). It measures one’s attitude towards illness with items such as: I have a hard time adjusting to the limitations of my illness. A higher score on the scale indicates a higher level of illness acceptance. The AIS does not have any subscales [46]. In the present study, AIS was characterized by good reliability (Cronbach’s alpha = 0.85).
Short Sexual Well-Being Scale (SSWBS) contains five items measuring the level of sexual well-being. Two versions of the scale are available: 4-point and 7-point versions. In this study, the 7-point version of the scale was used (where 1—I completely disagree; 7—I completely agree). It measures sexual well-being with items such as: I consider myself sexually fulfilled. A higher score on the scale indicates a higher level of sexual well-being. The SSWBS does not have any subscales [23]. In the present study, SSWBS was characterized by good reliability (Cronbach’s alpha = 0.85).
2.3. Statistical Analysis
Parametric analyzes were chosen to analyze the data for several reasons: (1) the skewness values of the tested variables ranged from 0.36 to 0.43 and the kurtosis values of the tested variables ranged from −1.07 to −0.96 (which indicates the low asymmetry of the studied variables); (2) the tested subgroups were equal; (3) parametric analyzes have more structured recommendations on effect size measures; and (4) parametric tests have high statistical power and resistance to breaking their assumptions (e.g., on distribution and homogeneity of variance). Therefore, the group differences were calculated with the t-test analysis with the Cohen’s d effect size measure. The significance of the relationships was tested with Pearson’s r correlation. Mediation analysis was performed using PROCESS v3.4 [47] with additional R 2 and f 2 effect size measures. All results were analyzed using IBM SPSS Statistics 28 (Predictive Solutions Sp. z o.o., Cracow, Poland). Power analysis was conducted using G*Power 3.1.9.7 [48] and Monte Carlo simulation [49]. A significance level of α = 0.05 was adopted as the threshold value for statistical significance.
3. Results
3.1. Group Differences
Before verifying the mediation hypothesis, we decided to check whether the tested sample of individuals with schizophrenia is a homogeneous group. For this purpose, the t-test analysis was used. We decided to use two variables as the grouping ones: gender and attending psychologist consultations. Other grouping variables were not taken into account due to the small size of most of the available categories (see Table 1 for reference). The analysis showed only one significant difference: men had significantly higher self-esteem than women (moderate effect size). Due to the lack of strong effect sizes and non-significant results in five out of six comparisons, we decided to treat the present group of study participants as homogeneous. More detailed data are shown in Table 2.

Table 2.
Results of the t-test analysis.
3.2. Correlations
In the second step of the statistical analysis, we decided to check whether the tested variables were significantly related. Pearson’s r correlation showed that self-esteem was positively related to acceptance of illness (large effect size) and sexual well-being (moderate effect size). Acceptance of illness was also positively related to life satisfaction (moderate effect size). More detailed data are shown in Table 3.

Table 3.
Results of the Pearson’s r correlation analysis.
3.3. Mediation Analysis
In the next step, we decided to perform a mediation analysis due to the significant relationships found in the Pearson’s r correlation analysis and presented theoretical background. According to Creedon and Hayes [50], the obtained number of respondents (n = 60) allows us to carry out the mediation analysis. Therefore, the bootstrapping mediation using the PROCESS macro was used with the declared number of 5000 samples [51]. The analysis was performed using model number 4 [47].
The PROCESS macro results showed that self-esteem was not a direct predictor of study participants’ sexual well-being. On the other hand, acceptance of illness served as a significant and positive predictor of the sexual well-being of the studied individuals with schizophrenia. Analysis of the confidence intervals of the indirect effect suggested that acceptance of illness served as the mediator in the relationship between self-esteem and sexual well-being in the studied sample. More detailed data are shown in Figure 2 and Table 4.
Figure 2.
Standardized Beta coefficients of the obtained model.

Table 4.
Results of the PROCESS Model 4 analysis.
3.4. Sensitivity Power Analysis
The sensitivity power analysis performed using G*Power 3.1.9.7 [48] suggested that, for the power levels of 1-Beta = 0.80 and a significance of α = 0.05, the obtained sample (n = 60) was sufficient to detect effects larger than rho = 0.31 and f2 = 0.11. In addition, the Monte Carlo simulation [49] with a number of 5000 replications and 20,000 Monte Carlo draws was performed at a confidence level of 95%. The simulation confirmed that the presented indirect effect can be interpreted due to sufficient statistical power. Therefore, it can be concluded that the presented significant results of the pilot study can be discussed.
4. Discussion
The purpose of the present pilot study was to verify the role of acceptance of illness as the mediator of the relationship between self-esteem and sexual well-being. Our research found associations between these variables and revealed that acceptance of illness significantly mediated the relationship between self-esteem and sexual well-being in individuals with schizophrenia.
4.1. Possible Explanations and Clinical Implications of the Presented Results
Firstly, the homogeneity of the examined sample of individuals with schizophrenia was verified. The analysis showed that men with schizophrenia had higher self-esteem than women with schizophrenia. This result may be due to the experience of greater difficulty in coping with the schizophrenia spectrum disorder among women. In a review of studies on gender differences in schizophrenia, Falkenburg and Tracy [52] noted that positive and cognitive symptoms occur more frequently and with greater intensity in women. The unfavorable course of the illness in women may contribute to their lower self-esteem. Additionally, women tend to worry more than men [53]. In turn, greater worry among individuals with schizophrenia spectrum disorders is associated with worse social functioning [54].
Schizophrenia is a severe, chronic illness that affects a person’s level of satisfaction in various areas. Therefore, we investigated the relationship between self-esteem, acceptance of illness and sexual well-being. The correlation results demonstrated that self-esteem was significantly associated with acceptance of illness. Having a positive attitude towards oneself was related to acceptance of the difficulties and limitations associated with schizophrenia. This result confirms the first hypothesis and is in line with previous studies indicating significant relationships between self-esteem and acceptance of illness [17,39]. In addition, self-esteem and acceptance of illness appeared to be associated with sexual well-being, although the strength of this association was moderate. Our research extends previous findings. A particularly interesting result is the relationship between acceptance of illness and sexual well-being. Previous studies have mainly focused on investigating the relationship between acceptance of illness, well-being and quality of life [55,56]. Our study shows that acceptance of one’s illness is also related to physical, emotional and social well-being in terms of a person’s sexuality and satisfaction with the quality of sexual relationships.
In our study, we also hypothesized that the relationship between self-esteem and sexual well-being would be mediated by acceptance of illness. The analysis revealed that acceptance of illness was a significant mediator in the relationship between self-esteem and sexual well-being in individuals with schizophrenia. Self-esteem is positively associated with acceptance of illness which, in turn, favors the fact that the sampled individuals with schizophrenia experienced sexual well-being. The present study thus contributes to previous knowledge by demonstrating that, although there are direct associations between self-esteem and sexual well-being in individuals with schizophrenia, indirect associations, in which illness acceptance was the mediating variable, are stronger. This central result in our study is in line with the researchers’ view that the quality of sexual life depends on many factors that interact with each other [8,23,24,27]. Based on our knowledge, this is the first study in individuals with schizophrenia to show the mediational role of acceptance of illness in the relationship between self-esteem and sexual well-being.
By testing the mediation effects, our study sheds new light on the interplay of personal resources in the sexual well-being of patients with schizophrenia, which also provides practical implications for clinicians. Our results indicate the significant role of acceptance of illness in maintaining satisfaction with one’s sexuality and sexual relationships among individuals with schizophrenia. It is important not to overlook the sex life of individuals with schizophrenia, as it is one of the main areas for maintaining well-being and quality of life [23,25,26]. The authors of this study hope to encourage clinicians in their practice to work with patients with schizophrenia based on the adaptation and acceptance of their new and demanding life situation and the limitations of their illness.
4.2. Limitations
The present study verified the role of self-esteem and acceptance of illness in shaping well-being in individuals with schizophrenia. According to the authors’ knowledge, it is one of the first to discuss the concept of sexual well-being from the perspective of schizophrenia. Unfortunately, like any research project, this one is not free from limitations. Firstly, our results are based on a cross-sectional study. The mediational model does not allow us to draw any causal conclusions regarding the observed relationships. Although the opposite causal direction can occur, our model based on the theoretical background of COR [57] validates the current findings without any definite causal statements. Longitudinal research would be needed to determine the final causality. Secondly, the sample was treated in the analyses as a homogeneous group. This does not mean, however, that all respondents were very similar to each other. Only one aspect of sexuality was assessed, i.e., sexual well-being. The omission of testing for the occurrence of sexual dysfunction caused by a health condition or other sexuality-related variables is a major limitation of the presented research project and should be taken into account in future studies. Thirdly, we did not verify the role of prescribed medication in the sexual well-being of studied individuals with schizophrenia. The study participants took different medications, in different doses and configurations. Despite consulting our results with a team of psychiatrists, we were unable to draw coherent conclusions from these data. Lastly, the presented pilot study shows the results based on 60 individuals with schizophrenia. Despite positive results gathered via various power analyses, the tested relationships should be tested on a larger, representative sample to reinforce the conclusions of this study.
5. Conclusions
The well-being of one’s sexuality, sex life and intimate relationships is a fundamental human right and need. To our knowledge, this is the first study performed among individuals with schizophrenia to indicate the mediating role of acceptance of illness in the relationship between self-esteem and sexual well-being. Self-esteem is positively associated with acceptance of illness which, in turn, favors the fact that the sampled individuals with schizophrenia experienced sexual well-being. Our findings highlight the significant role of acceptance of illness in maintaining satisfying sexual health among patients with schizophrenia and thus encourage clinicians to work with patients based on acceptance of the diagnosis of schizophrenia and the limitations resulting from this illness. Our results are particularly important for Polish practitioners. There are no general clinical interview guidelines in Poland, and the scope of its content varies from institution to institution. The interview questions asked before admission to the hospitals’ wards and psychological centers usually do not include questions about one’s sexual sphere, or are just simply related to one’s sexual activity (assessed based on one sentence: Are you sexually active?). The Mental Health Centers Pilot (in Polish: Pilotaż Centrów Zdrowia Psychicznego) is a Polish Ministry of Health’s program, the aim of which is to ensure free 24 h psychological support, and provide a diagnostic and therapeutic standard [58]. Unfortunately, its Diagnostic and Therapeutic Standards Draft (in Polish: Projekt Standardu Diagnostyczno-Terapeutycznego) does not include questions about one’s sexual sphere. Our study draws attention to the fact that the sexual sphere is significantly related to the acceptance of illness in individuals with schizophrenia, so it should also be taken into account when working with those individuals and assessing their well-being.
Author Contributions
Conceptualization, R.G.; methodology, R.G.; software, R.G.; validation, R.G., formal analysis, R.G.; investigation, M.S.; resources, R.G. and M.S.; data curation, R.G.; writing—original draft preparation, R.G. and M.S.; writing—review and editing, R.G.; supervision, R.G.; project administration, R.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. The manuscript received a full APC waiver from MDPI’s EJIHPE editorial office.
Institutional Review Board Statement
According to the Bioethics Committee at the Institute of Medical Sciences of Opole University in Poland (application number 2/KB/12/2019), due to the cross-sectional and survey nature of the present study, it did not raise any ethical concerns.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data can be made available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- McCutcheon, R.A.; Marques, T.R.; Howes, O.D. Schizophrenia—An Overview. JAMA Psychiatry 2020, 77, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Csernansky, J.G.; Schuchart, E.K. Relapse and Rehospitalisation Rates in Patients with Schizophrenia: Effects of Second Generation Antipsychotics. CNS Drugs 2002, 16, 473–484. [Google Scholar] [CrossRef] [PubMed]
- Krynicki, C.R.; Upthegrove, R.; Deakin, J.F.W.; Barnes, T.R. The Relationship between Negative Symptoms and Depression in Schizophrenia: A Systematic Review. Acta Psychiatr. Scand. 2018, 137, 380–390. [Google Scholar]
- Strauss, G.P.; Sandt, A.R.; Catalano, L.T.; Allen, D.N. Negative Symptoms and Depression Predict Lower Psychological Well-Being in Individuals with Schizophrenia. Compr. Psychiatry 2012, 53, 1137–1144. [Google Scholar] [CrossRef] [PubMed]
- Savilla, K.; Kettler, L.; Galletly, C. Relationships between Cognitive Deficits, Symptoms and Quality of Life in Schizophrenia. Aust. N. Z. J. Psychiatry 2008, 42, 496–504. [Google Scholar] [CrossRef]
- Baggaley, M. Sexual Dysfunction in Schizophrenia: Focus on Recent Evidence. Hum. Psychopharmacol. Clin. Exp. 2008, 23, 201–209. [Google Scholar] [CrossRef]
- Ma, M.-C.; Chao, J.-K.; Hung, J.-Y.; Sung, S.-C.; Chao, I.-H.C. Sexual Activity, Sexual Dysfunction, and Sexual Life Quality among Psychiatric Hospital Inpatients with Schizophrenia. J. Sex. Med. 2018, 15, 324–333. [Google Scholar] [PubMed]
- Barker, L.C.; Vigod, S.N. Sexual Health of Women with Schizophrenia: A Review. Front. Neuroendocrinol. 2020, 57, 100840. [Google Scholar] [CrossRef]
- McCann, E.; Donohue, G.; de Jager, J.; Nugter, A.; Stewart, J.; Eustace-Cook, J. Sexuality and Intimacy among People with Serious Mental Illness: A Qualitative Systematic Review. JBI Evid. Synth. 2019, 17, 74–125. [Google Scholar] [CrossRef]
- Galderisi, S.; Rucci, P.; Kirkpatrick, B.; Mucci, A.; Gibertoni, D.; Rocca, P.; Rossi, A.; Bertolino, A.; Strauss, G.P.; Aguglia, E. Interplay among Psychopathologic Variables, Personal Resources, Context-Related Factors, and Real-Life Functioning in Individuals with Schizophrenia: A Network Analysis. JAMA Psychiatry 2018, 75, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Xu, J.; Mao, Y.; Sun, L.; Sun, Y.; Zhou, Y. Positive Coping and Resilience as Mediators between Negative Symptoms and Disability among Patients with Schizophrenia. Front. Psychiatry 2019, 10, 641. [Google Scholar] [CrossRef] [PubMed]
- Yanos, P.T.; Moos, R.H. Determinants of Functioning and Well-Being among Individuals with Schizophrenia: An Integrated Model. Clin. Psychol. Rev. 2007, 27, 58–77. [Google Scholar] [CrossRef]
- Sowislo, J.F.; Orth, U. Does Low Self-Esteem Predict Depression and Anxiety? A Meta-Analysis of Longitudinal Studies. Psychol. Bull. 2013, 139, 213–240. [Google Scholar] [CrossRef]
- Steiger, A.E.; Allemand, M.; Robins, R.W.; Fend, H.A. Low and Decreasing Self-Esteem during Adolescence Predict Adult Depression Two Decades Later. J. Personal. Soc. Psychol. 2014, 106, 325–338. [Google Scholar] [CrossRef] [PubMed]
- Lysaker, P.H.; Roe, D.; Yanos, P.T. Toward Understanding the Insight Paradox: Internalized Stigma Moderates the Association between Insight and Social Functioning, Hope, and Self-Esteem among People with Schizophrenia Spectrum Disorders. Schizophr. Bull. 2007, 33, 192–199. [Google Scholar] [CrossRef]
- Staring, A.B.P.; Van der Gaag, M.; Van den Berge, M.; Duivenvoorden, H.J.; Mulder, C.L. Stigma Moderates the Associations of Insight with Depressed Mood, Low Self-Esteem, and Low Quality of Life in Patients with Schizophrenia Spectrum Disorders. Schizophr. Res. 2009, 115, 363–369. [Google Scholar] [CrossRef]
- Furmańska, J.; Koziarska, D.; Szcześniak, M.; Rzepa, T.; Nowacki, P. Sexual Satisfaction, Self-Esteem and Acceptance of Illness among Relapse-Remitting Multiple Sclerosis Patients. Adv. Psychiatry Neurol./Postępy Psychiatr. I Neurol. 2017, 26, 236–245. [Google Scholar] [CrossRef]
- Rosenberg, M. Conceiving the Self; Basic Books: New York, NY, USA, 1979. [Google Scholar]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton University Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Coopersmith, S. The Antecedents of Self-Esteem; Princeton University Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Yean, C.; Benau, E.; Dakanalis, A.; Hormes, J.; Perone, J.; Timko, A. The Relationship of Sex and Sexual Orientation to Self-Esteem, Body Shape Satisfaction, and Eating Disorder Symptomatology. Front. Psychol. 2013, 4, 887. [Google Scholar] [CrossRef]
- Gozuyesil, E.; Taylan, S.; Manav, A.I.; Akil, Y. The Evaluation of Self-Esteem and Sexual Satisfaction of Patients with Bowel Stoma in Turkey: Self-Esteem Sexual Satisfaction in Patients with Bowel Stoma. Sex. Disabil. 2017, 35, 157–169. [Google Scholar] [CrossRef]
- Gerymski, R. Short Sexual Well-Being Scale—A Cross-Sectional Validation among Transgender and Cisgender People. Health Psychol. Rep. 2021, 9, 276–287. [Google Scholar] [CrossRef]
- Gerymski, R.; Cisek, A.; Dymecka, J. Seksualny dobrostan a satysfakcja z życia osób z niepełnosprawnością ruchową: Moderacyjna rola samooceny [Sexual well-being and life satisfaction of people with motor disabilities: The moderating role of self-esteem]. J. Sex. Ment. Health 2022, 20, 1–7. [Google Scholar] [CrossRef]
- Stephenson, K.R.; Meston, C.M. Differentiating Components of Sexual Well-Being in Women: Are Sexual Satisfaction and Sexual Distress Independent Constructs? J. Sex. Med. 2010, 7, 2458–2468. [Google Scholar] [CrossRef] [PubMed]
- Davison, S.L.; Bell, R.J.; LaChina, M.; Holden, S.L.; Davis, S.R. The Relationship between Self-Reported Sexual Satisfaction and General Well-Being in Women. J. Sex. Med. 2009, 6, 2690–2697. [Google Scholar] [CrossRef] [PubMed]
- Štulhofer, A.; Jurin, T.; Graham, C.; Enzlin, P.; Træen, B. Sexual Well-Being in Older Men and Women: Construction and Validation of a Multi-Dimensional Measure in Four European Countries. J. Happiness Stud. 2019, 20, 2329–2350. [Google Scholar] [CrossRef]
- Robinson, K.J.; Cameron, J.J. Self-Esteem Is a Shared Relationship Resource: Additive Effects of Dating Partners’ Self-Esteem Levels Predict Relationship Quality. J. Res. Personal. 2012, 46, 227–230. [Google Scholar] [CrossRef]
- Oattes, M.K.; Offman, A. Global Self-Esteem and Sexual Self-Esteem as Predictors of Sexual Communication in Intimate Relationships. Can. J. Human Sex. 2007, 16, 89–100. [Google Scholar]
- Ménard, A.D.; Offman, A. The Interrelationships between Sexual Self-Esteem, Sexual Assertiveness and Sexual Satisfaction. Can. J. Human Sex. 2009, 18, 35–45. [Google Scholar]
- Sprecher, S.; Hendrick, S.S. Self-Disclosure in Intimate Relationships: Associations with Individual and Relationship Characteristics Over Time. J. Soc. Clin. Psychol. 2004, 23, 857–877. [Google Scholar] [CrossRef]
- Jourard, S.M. The Transparent Self; Van Nostrand Reinhold Company: New York, NY, USA, 1971. [Google Scholar]
- Don, B.P.; Girme, Y.U.; Hammond, M.D. Low Self-Esteem Predicts Indirect Support Seeking and Its Relationship Consequences in Intimate Relationships. Personal. Soc. Psychol. Bull. 2019, 45, 1028–1041. [Google Scholar] [CrossRef]
- Tayebi, N.; Beygi, Z.; Zaydanpanahi, Z.; Akbarzadeh, M. The Relationship between Self-Esteem and Sexual Dysfunction in Women at Reproductive Ages: A Cross-Sectional Study. Curr. Women’s Health Rev. 2021, 17, 45–50. [Google Scholar] [CrossRef]
- Zauszniewski, J.A.; McDonald, P.E.; Krafcik, K.; Chung, C.; Dobratz, M.C.; Downe-Wamboldt, B. Acceptance, Cognitions, and Resourcefulness in Women with Diabetes. West. J. Nurs. Res. 2002, 24, 728–750. [Google Scholar] [CrossRef] [PubMed]
- Dymecka, J.; Gerymski, R. Acceptance of Illness as a Mediator of the Relationship between Neurological Disability and Health-Related Quality of Life of People with Multiple Sclerosis. Neuropsychiatr. I Neuropsychol./Neuropsychiatry Neuropsychol. 2020, 15, 13–20. [Google Scholar]
- Dymecka, J.; Gerymski, R.; Tataruch, R.; Bidzan, M. Fatigue, Physical Disability and Self-Efficacy as Predictors of the Acceptance of Illness and Health-Related Quality of Life in Patients with Multiple Sclerosis. Int. J. Environ. Res. Public Health 2021, 18, 13237. [Google Scholar] [CrossRef] [PubMed]
- Rüsch, N.; Corrigan, P.W. Motivational Interviewing to Improve Insight and Treatment Adherence in Schizophrenia. Psychiatr. Rehabil. J. 2002, 26, 23. [Google Scholar] [CrossRef]
- Rode, D.; Rode, M.M. The Relationship between Self-Esteem, Sense of Self-Efficacy and Level of Illness Acceptance, and Healthful Behaviours in Patients with Long-Term Illnesses (Type II Diabetes, Hashimoto’s Disease). Health Psychol. Rep. 2018, 6, 158–170. [Google Scholar] [CrossRef]
- Marthoenis, M.; Syukri, M.; Abdullah, A.; Tandi, T.M.R.; Putra, N.; Laura, H.; Setiawan, A.; Sofyan, H.; Schouler-Ocak, M. Quality of Life, Depression, and Anxiety of Patients Undergoing Hemodialysis: Significant Role of Acceptance of the Illness. Int. J. Psychiatry Med. 2021, 56, 40–50. [Google Scholar]
- Simmons, K.L.; Smith, J.A.; Bobb, K.-A.; Liles, L.L.M. Adjustment to Colostomy: Stoma Acceptance, Stoma Care Self-Efficacy and Interpersonal Relationships. J. Adv. Nurs. 2007, 60, 627–635. [Google Scholar] [CrossRef]
- Karademas, E.C.; Tsagaraki, A.; Lambrou, N. Illness Acceptance, Hospitalization Stress and Subjective Health in a Sample of Chronic Patients Admitted to Hospital. J. Health Psychol. 2009, 14, 1243–1250. [Google Scholar] [CrossRef]
- Lysaker, P.H.; Pattison, M.L.; Leonhardt, B.L.; Phelps, S.; Vohs, J.L. Insight in Schizophrenia Spectrum Disorders: Relationship with Behavior, Mood and Perceived Quality of Life, Underlying Causes and Emerging Treatments. World Psychiatry 2018, 17, 12–23. [Google Scholar] [CrossRef]
- Kurpisz, J.; Mak, M.; Lew-Starowicz, M.; Nowosielski, K.; Bieńkowski, P.; Kowalczyk, R.; Misiak, B.; Frydecka, D.; Samochowiec, J. Personality Traits, Gender Roles and Sexual Behaviours of Young Adult Males. Ann. Gen. Psychiatry 2016, 15, 28. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Ahmad, M.; Ismail, F.B. Illness Acceptance as Mediator for Cancer-Related Complaints and Psychological Distresses among Malaysian Cancer Patients. Future Oncol. 2019, 15, 1759–1770. [Google Scholar] [CrossRef]
- Felton, B.J.; Revenson, T.A.; Hinrichsen, G.A. Stress and Coping in the Explanation of Psychological Adjustment among Chronically Ill Adults. Soc. Sci. Med. 1984, 18, 889–898. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Schoemann, A.M.; Boulton, A.J.; Short, S.D. Determining Power and Sample Size for Simple and Complex Mediation Models. Soc. Psychol. Personal. Sci. 2017, 8, 379–386. [Google Scholar] [CrossRef]
- Creedon, P.S.; Hayes, A.F. Small Sample Mediation Analysis: How Far Can We Push the Bootstrap. In Proceedings of the Annual Conference of the Association for Psychological Science, New York, NY, USA, 21–24 May 2015. [Google Scholar]
- Preacher, K.J.; Hayes, A.F. Asymptotic and Resampling Strategies for Assessing and Comparing Indirect Effects in Multiple Mediator Models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Falkenburg, J.; Tracy, D.K. Sex and Schizophrenia: A Review of Gender Differences. Psychosis 2014, 6, 61–69. [Google Scholar] [CrossRef]
- Mccann, S.J.; Stewin, L.L.; Short, R.H. Sex Differences, Social Desirability, Masculinity, and the Tendency to Worry. J. Genet. Psychol. 1991, 152, 295–301. [Google Scholar] [CrossRef]
- Golędzinowska, M.; Sawicka, M.; Żochowska, A. Worrying in People with Schizophrenia. Adv. Psychiatry Neurol./Postępy Psychiatr. I Neurol. 2018, 27, 3–14. [Google Scholar] [CrossRef]
- Kowalewska, B.; Jankowiak, B.; Niedżwiecka, B.; Krajewska-Ku\lak, E.; Niczyporuk, W.; Khvorik, D.F. Relationships between the Acceptance of Illness, Quality of Life and Satisfaction with Life in Psoriasis. Adv. Dermatol. Allergol./Postępy Dermatol. I Alergol. 2020, 37, 948–955. [Google Scholar] [CrossRef]
- Kocatepe, V.; Arikan, H.C.; Yıldırım, S.; Peker, S.; Unver, V. The Acceptance of Illness and Life Satisfaction of Individuals with Chronic Disease. Int. J. Caring 2020, 13, 1744–1751. [Google Scholar]
- Hobfoll, S.E. Conservation of Resources: A New Attempt at Conceptualizing Stress. Am. Psychol. 1989, 44, 513. [Google Scholar] [CrossRef] [PubMed]
- Pilotaż Centrów Zdrowia Psychicznego [Mental Health Centers Pilot]; Polish Ministry of Health. Projekt Standardu Diagnostyczno-Terapeutycznego w Centrum Zdrowia Psychicznego [Diagnostic and Therapeutic Standard Draft in the Mental Health Center], 2023. Available online: https://czp.org.pl/wp-content/uploads/2023/01/Standarddiagnostycznoterapeutycznywcentrumzdrowiapsychicznego.pdf (accessed on 14 July 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).