Introduction
Acute suppurative thyroiditis (AST) is rare, causing 0.1-0.7% of all thyroid diseases [
1]. But this prevalence is based on the retrospective data collected from the surgical specimens. It is estimated that the true epidemiology of this disease is much lower [
2]. The most common cause of AST is a bacterial infection, but other causes also include fungal, mycobacterial, and parasitic infection [
1]. The most common symptoms in AST are anterior neck swelling associated with pain, erythema, and tenderness that may radiate to the jaw, ear, or occiput on the involved side. Many cases appeared after a recent upper respiratory tract infection [
3]. The abscess may cause the compression of the trachea, esophagus, or recurrent laryngeal nerve. During disease progression, most patients develop systemic symptoms, including fever, chills, and malaise.
The rarity of AST may be related to the several mechanisms of the thyroid gland that inhibit suppuration. These include the unique anatomical isolation from other neck structures with separation by fascial planes and encasement by a fibrous capsule, rich supply of blood and lymphatics, high concentration of iodine, and hydrogen peroxide production [
3]. However, in certain situations, the pyriform sinus fistula may lead to abscess information in children, especially in the left lobe [
4]. Other routes of infection include hematogenous or lymphatic spread, a direct extension of abscess, direct inoculation of thyroid or surrounding anatomy, and neck trauma [
4]. However, the route of infection could not be demonstrated in most of the cases. Predisposing factors of AST are anatomically altered thyroid gland (e.g., goiter, adenoma, malignancy) [
5]. and immunocompromised status [
3].
The pathogens most often isolated from AST are
Staphylococcus aureus,
Streptococcus pyogenes,
Staphylococcus epidermidis, and
Streptococcus pneumoniae [
1,
4]. After initial empirical broad-spectrum antibiotic, the correct identification of pathogens may assist in the selection of appropriate antibiotic therapy. Despite the fact that
Streptococcus suis generally causes sepsis and meningitis, this is a unique case report of AST caused by
S. suis in a patient with a preexisting thyroid nodule.
Case report
A 64-year-old Thai female from an iodine-deficient area presented with a five-day history of purulent discharge spontaneously drained from a large mass at the left lobe of the thyroid gland. She had a long-standing left thyroid nodule for 40 years. She was clinically euthyroid but thyroid function tests and fine-needle aspiration (FNA) biopsy had not been investigated before. Two weeks before the hospital visit, she had had a low-grade fever which subsided within two days. One week later, she developed rapid thyroid mass enlargement and inflammation. Two days later, purulent discharge spontaneously drained from the thyroid mass. Then her inflamed goiter slightly improved. She had no complaints of hoarseness, difficulty with breathing, or dysphagia. She did not take any medication except for acetaminophen until the hospital visit.
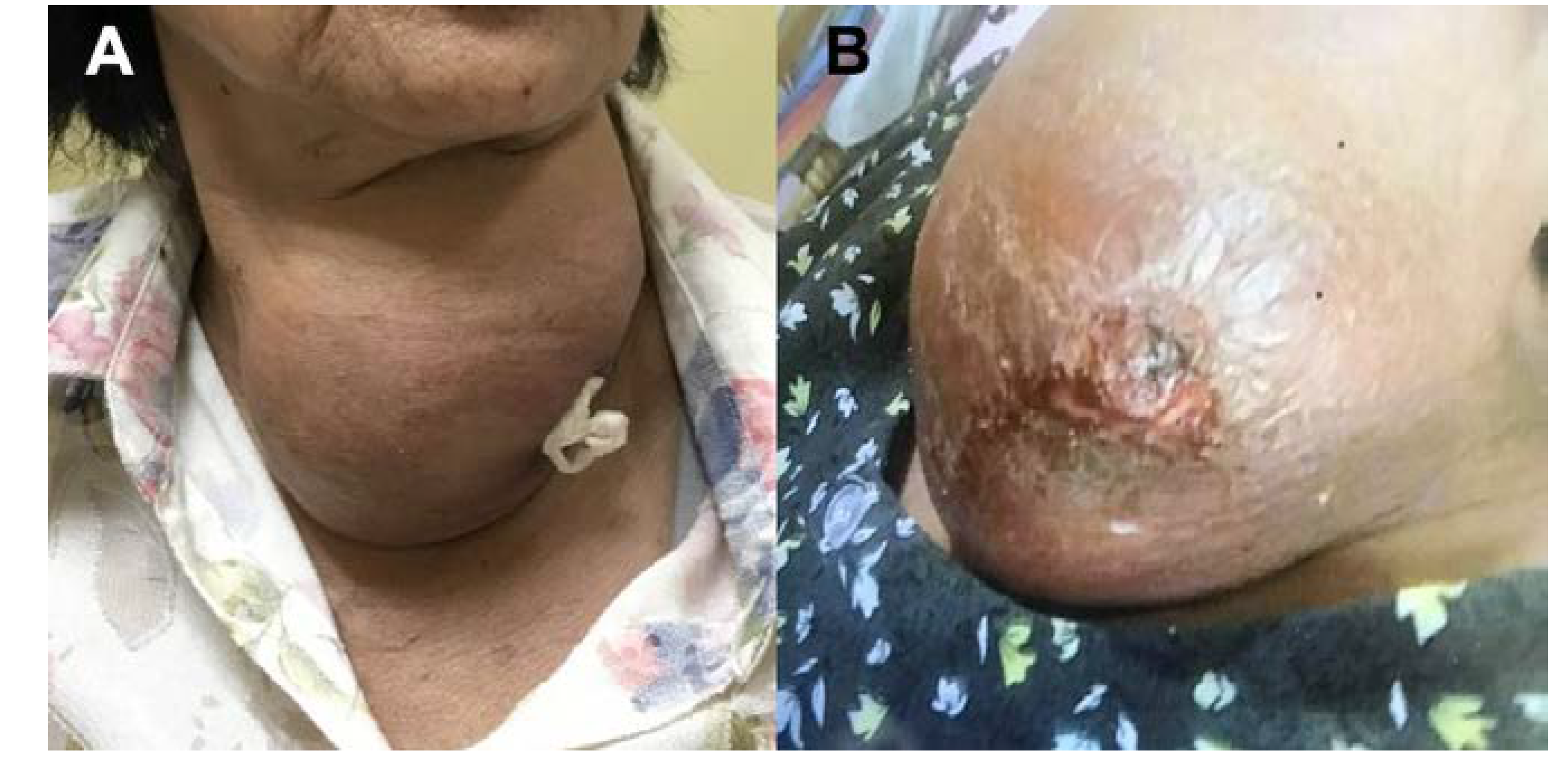
Physical examination revealed a temperature of 37.8 °C, blood pressure of 122/72 mmHg, pulse of 85 beats per minute, and respiratory rate of 18 breaths/minute. On palpation, there was a painful erythematous mass measuring 20 cm with hard consistency on the left thyroid gland (
Figure 1). Yellow purulent discharge was drained from the ulcer on the thyroid mass. Incisional biopsy and drainage were performed at the outpatient ambulatory setting. Gram-stained smear showed abundant neutrophils, but no organism. An empirical antibiotic with oral cephalexin 250 mg QID was initiated at the clinic.
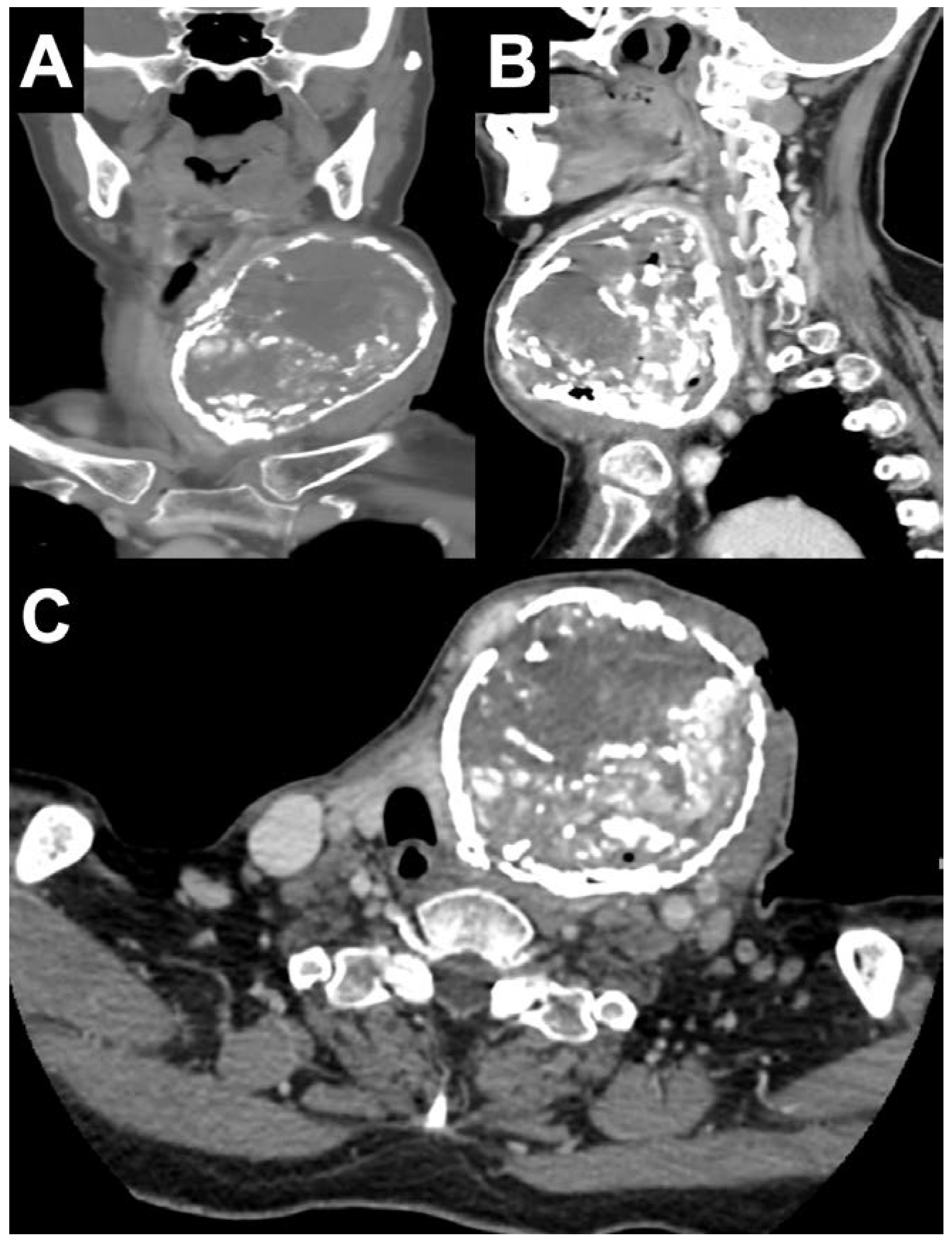
Initial investigations showed a white blood cell count of 7,550 cells/µL with neutrophils at 72%. Thyroid function tests were: free thyroxine (T4) of 0.82 (reference range, 0.70-1.48 ng/dL), free triiodothyronine (T3) of 2.46 (reference range, 1.88-3.18 pg/mL), thyroid-stimulating hormone (TSH) <0.0038 (reference range, 0.35-4.94 IU/mL), compatible with subclinical hyperthyroidism. The TSH receptor antibody was negative. The serologic test for HIV was negative. Her plasma glucose, renal, and liver function tests were within the normal reference ranges, except for low levels of serum albumin. Two blood cultures were negative. Computed tomography (CT) scan of the neck with contrast showed a heterogeneous enhancing mass with internal and rim calcification at the left lobe of the thyroid gland, measuring 8.4×7.2×9.7 cm (
Figure 2). The lesion caused a pressure effect on the trachea and glottic larynx. The thyroid scan showed an uptake in the tilted horseshoe-shaped configuration corresponding to the functioning thyroid tissue in the periphery of the left enlarged thyroid mass and absence of uptake in the suppurative area (
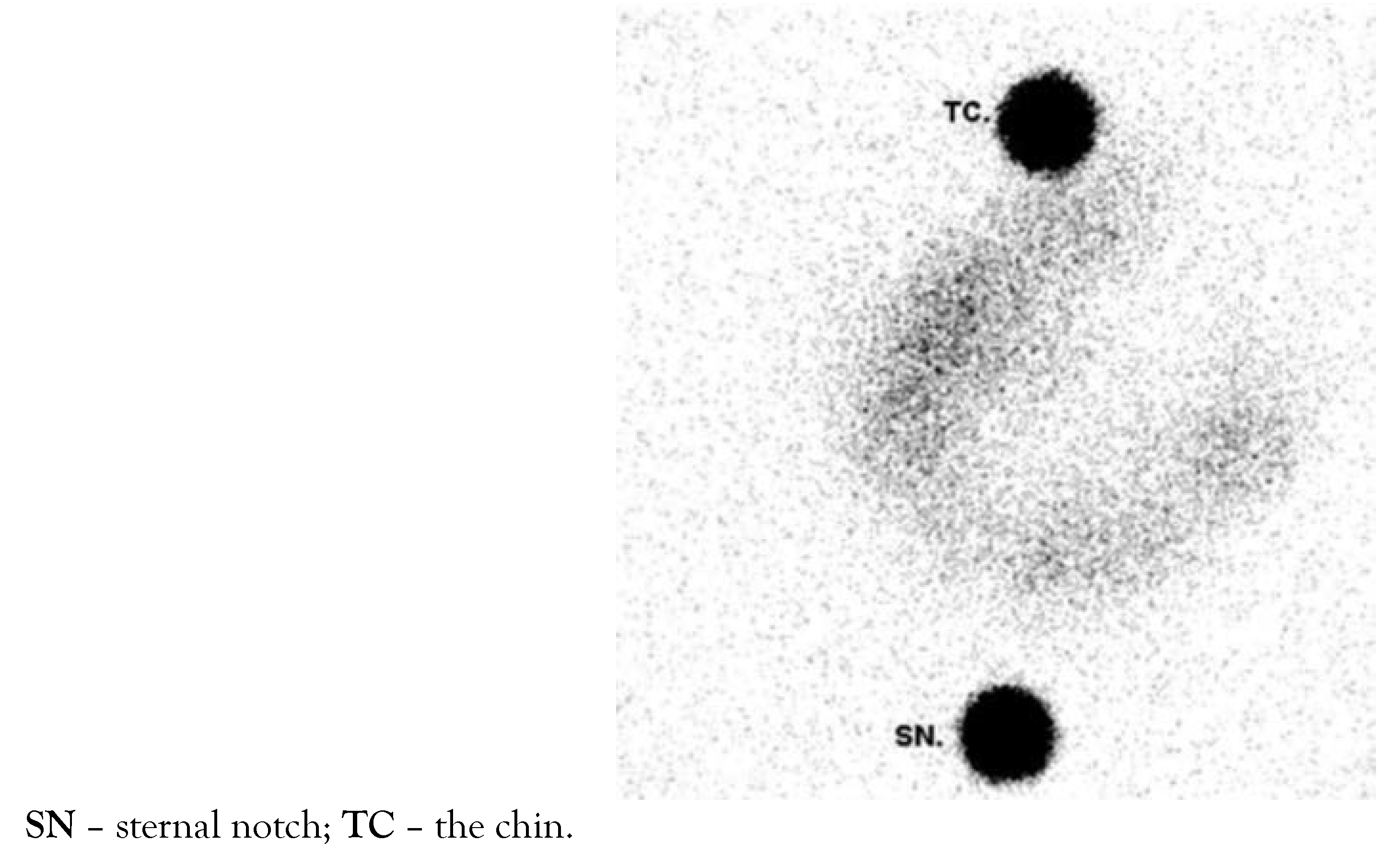
Figure 3).
From the thyroid biopsy sample, the aerobic cultures grew S. suis, sensitive to penicillin, ampicillin, vancomycin, linezolid, levofloxacin; and resistant to clindamycin, erythromycin, tetracycline. Additional information included a history of raw pork product consumption. She had no history of neck trauma and infective endocarditis. At 1 week after the initial visit at the clinic, we changed cephalexin to oral amoxicillin 3 g per day according to the culture report. At one month after the initial presentation, she subsequently underwent a left thyroid lobectomy to exclude malignancy. Pathology was consistent with nodular goiter with central degeneration and acute suppurative inflammation. The presence of xanthogranulomatous inflammation, old calcification at the left lobe of the thyroid gland with pressure effects to the trachea hemorrhage, fibrosis, and the extensive calcified capsule was reported. Amoxicillin was discontinued at 1 week after complete surgery and the duration of amoxicillin therapy was 4 weeks. She recovered well without any complications. Her TSH returned to normal. She is currently in a good health at a 2-year follow-up.
Discussion
To date, this is the first case report of AST due to alpha-hemolytic Gram-positive S. suis in an adult with a hyperfunctioning thyroid nodule. S. suis is a major swine pathogen which can cause serious infections in human. The main route of transmission is from consumption of raw/undercooked pork and close contact with infected pigs or pig meat. Over the past decade, the number of human cases of S. suis reported in the literature has dramatically increased with high prevalence in Southeast Asia, especially in Thailand and Vietnam, where there was a high rate of raw pork consumption [
6]. Meningitis, sepsis, and infective endocarditis are major clinical manifestations of S. suis infection, with a case fatality rate of 13% [
7]. Irreversible hearing loss from labyrinthitis is found as a common sequela of meningitis [
7].
Despite the thyroid being resistant to infection, AST in this case could be due to multiple factors. After consumption of raw pork meats, a highly invasive pathogen
S. suis can penetrate host mucosal barriers and lead to bacteremia and subsequent AST. Patients with preexisting abnormal thyroid structures, such as multinodular goiter, nodule, or malignancy, may be more susceptible to suppuration [
4]. Reduced antioxidant defense system in thyroid tissue samples of multiple nodular goiter and papillary carcinoma has been reported [
5]. and may induce more susceptibility to bacterial infection within the thyroid gland.
FNA biopsy with Gram’s staining and culture is essential to identify the causative organism and differentiate AST from subacute granulomatous thyroiditis. It allows more accurate antibiotic selection. Multiple imaging studies (e.g., ultrasonography, CT) can aid the diagnosis of AST [
4]. Treatment options of AST vary and depend on the severity and response to initial management. In general, conservative treatment with antibiotics is adequate.
S. suis is sensitive to many antibiotics, including penicillin, amoxicillin, ampicillin, and cephalosporins [
8].
If an abscess is present, drainage is necessary in addition to antibiotic. Repeat percutaneous aspiration of pus may be considered a non-operative approach [
9]. In patients who do not respond to percutaneous drainage, surgical drainage is the proper option and may be suitable for a large abscess. Thyroidectomy should be considered in the cases with concomitant extensive necrosis, suspicion of malignancy, hyperthyroidism (Graves’ disease, toxic multinodular goiter), relapsing thyroiditis, or compressive symptoms [
4]. Patients with pyriform sinus fistula as a cause of AST require surgical excision or endoscopic obliteration of the sinus tract to prevent recurrent infection [
4,
10]. Thyroid function tests should be monitored because some patients may develop hypothyroidism and require levothyroxine replacement.
Conclusions
This emphasizes the importance of the correct identification of pathogens for an appropriate antimicrobial agent. Clinicians should consider the possibility of S. suis AST in the patients who live in countries with a high frequency of S. suis diseases. An early diagnosis and proper management can lead to an excellent outcome as demonstrated by this case report.
Author Contributions
VJ wrote the first draft of the manuscript. All authors contributed to data collection, manuscript editing, read, and approved the final version of the manuscript.
Conflicts of interest
All authors – none to declare.
Consent
Written informed consent was obtained from the patient for publication of this case report and images. This case report was approved by the Human Research Ethics Committee of the Faculty of Medicine Ramathibodi Hospital, Mahidol University.
References
- Al-Dajani, N.; Wootton, S.H. Cervical lymphadenitis, suppurative parotitis, thyroiditis, and infected cysts. Infect Dis Clin North Am. 2007, 21, 523-41. [Google Scholar] [CrossRef] [PubMed]
- Lafontaine, N.; Learoyd, D.; Farrell, S.; Wong, R. Suppurative thyroiditis: systematic review and clinical guidance. Clin Endocrinol (Oxf). 2021, 95, 253-64. [Google Scholar] [CrossRef] [PubMed]
- Pearce, E.N.; Farwell, A.P.; Braverman, L.E. Thyroiditis. N Engl J Med. 2003, 348, 2646-55. [Google Scholar] [CrossRef] [PubMed]
- Paes, J.E.; Burman, K.D.; Cohen, J.; et al. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid. 2010, 20, 247-55. [Google Scholar] [CrossRef] [PubMed]
- Erdamar, H.; Cimen, B.; Gülcemal, H.; Saraymen, R.; Yerer, B.; Demirci, H. Increased lipid peroxidation and impaired enzymatic antioxidant defense mechanism in thyroid tissue with multinodular goiter and papillary carcinoma. Clin Biochem. 2010, 43, 650-4. [Google Scholar] [CrossRef] [PubMed]
- Segura, M.; Aragon, V.; Brockmeier, S.L.; et al. Update on Streptococcus suis research and prevention in the era of antimicrobial restriction: 4th international workshop on S. suis. Pathogens. 2020, 9, 374. [Google Scholar] [CrossRef] [PubMed]
- Huong, V.T.; Ha, N.; Huy, N.T.; et al. Epidemiology, clinical manifestations, and outcomes of Streptococcus suis infection in humans. Emerg Infect Dis. 2014, 20, 1105-14. [Google Scholar] [CrossRef] [PubMed]
- Lun, Z.R.; Wang, Q.P.; Chen, X.G.; Li, A.X.; Zhu, X.Q. Streptococcus suis: an emerging zoonotic pathogen. Lancet Infect Dis. 2007, 7, 201-9. [Google Scholar] [CrossRef] [PubMed]
- Ilyin, A.; Zhelonkina, N.; Severskaya, N.; Romanko, S. Nonsurgical management of thyroid abscess with sonographically guided fine needle aspiration. J Clin Ultrasound. 2007, 35, 333-7. [Google Scholar] [CrossRef] [PubMed]
- Lachance, S.; Chadha, N.K. Systematic review of endoscopic obliteration techniques for managing congenital piriform fossa sinus tracts in children. Otolaryngol Head Neck Surg. 2016, 154, 241-6. [Google Scholar] [CrossRef] [PubMed]
© GERMS 2025. Published by MDPI on behalf of the GERMS. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).