Abstract
Specialization training for physiotherapists, occupational therapists, and sports therapists involved in pediatric pain is scarce and curricula are rarely published. The objectives of this study are twofold: firstly, to perform a scoping review to derive important contents for a pediatric pain education curriculum for specialized pain therapists. Secondly, to conduct a survey on specific contents in curricula currently used by pain experts and to obtain their evaluation regarding the importance of such contents for a specialized curriculum. The review substantiated the importance of a specific curriculum in pediatric pain education, but provided little information on adequate contents. In the survey, 45 experts in pediatric pain education confirmed that specific curricula and specialized contents for pediatric pain education are missing. Their answers give a well-defined picture of the specifics needed in the interaction with a pediatric population. The most important items they classified were e.g., the biopsychosocial framework and the impact of pediatric pain on daily life. Those expert ratings were in line with the recommendations of pediatric pain management guidelines. Further curriculum work in an interdisciplinary, international network is highly recommended.
Keywords:
pediatrics; pain; curriculum; education; occupational therapists; physical therapists; review; survey 1. Introduction
All children in different age groups experience pain at some stage [1]. Infants are often exposed to procedural pain [2], and older children or adolescents often suffer some form of chronic pain. A systematic review reported prevalence rates for headache between 8–83%, abdominal pain between 4–53%, back pain between 14–24%, and musculoskeletal pain between 4–40% [3]. Without adequate pain prevention or pain treatment, early pain experiences can have livelong consequences, with impact on quality of life, specifically interfering with school and sport performances, appetite, mood or sleep [4] and can lead to increased pain sensitivity later in life [5].
Current evidence that physical activity/exercise training may be effective for reducing or preventing pain is often based on data extrapolated from studies on adult populations [6,7]. Although there is still need for more high-quality studies in pediatric populations [1,8], there is growing evidence suggesting that exercise/physical activity interventions are also effective for reducing pain and improve physical functioning in this vulnerable group [9,10].
In the rehabilitation of pediatric chronic pain, exercise and physical activity promotion are key elements, hence physiotherapists (PTs) and/or occupational therapist (OTs) form an integral part of the management team in existing pain programs [11,12,13]. There is increased support to involve PTs beneath pediatricians and clinical child psychologists regarding coordinated interventions in intensive interdisciplinary pain treatment programs [13]. A review focusing on specialized pediatric rehabilitation programs with severe disabling chronic pain depicted PT interventions in all of the analyzed programs and OT Interventions in seven of the nine analyzed programs [12].
However, the quantity and quality of the therapists’ training are not standardized with regard to pediatric pain management, and it is unknown how much of the required knowledge and skills are already integrated in existing basic education programs. Unfortunately, basic pain education for health care professionals who regularly work with children is still inadequate despite a large body of literature [14], and deficits regarding basic pain topics in physiotherapy and occupational therapy curricula have been noted [15,16,17]. The phenomenon of insufficient practice transfer is a well-known challenge that also needs to be addressed at an early stage of training [14].
Yet an overview of quantity and contents of pediatric pain education integrated in basic educational curricula for physiotherapists (PTs), occupational therapists (OTs), and sports therapists (STs) still needs to be established.
The general objectives of this study are twofold: firstly, to perform a scoping review to derive important contents for a pediatric pain education curriculum for specialized pain movement therapists. Secondly, to survey the presence of such specific contents in the curricula currently used by pain experts and to get their evaluation regarding the importance of such contents for a specialized curriculum.
2. Materials and Methods
2.1. Theoretical Framework of the Study
Due to the scarcity of specialized pediatric pain management training among therapists, curricular adjustments in educational programs are recommended [1,14]. Differentiated knowledge and understanding of pediatric pain are essential in order to make the correct decision regarding a child centred pain management.
Curricula should implement contents with high relevance regarding this educational topic. Therefore, a decision was made to focus this study on the derivation of appropriate topics for a pediatric pain curriculum using a scoping review, guideline recommendations and an expert survey. This developmental study was performed, following the principles of the educational design research [18]. The different steps of the study are depicted in Figure 1 and described in depth in this section. Step 4 presents possible actions for the future.
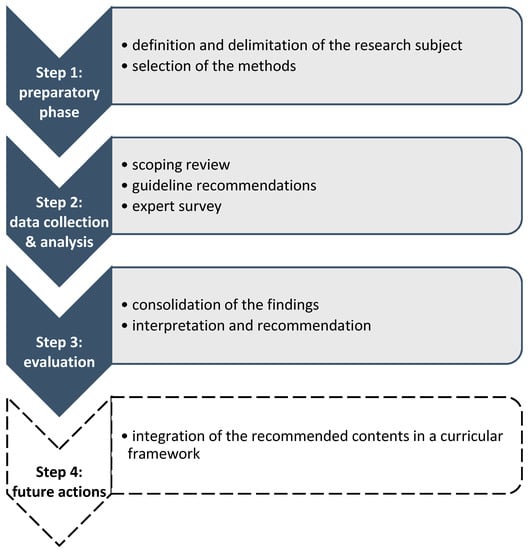
Figure 1.
Theoretical framework of the study. The grey parts of this figure have been finished and are reported in this article. The white part remains to be done in the future.
2.2. Scoping Review
This scoping review was undertaken to get an overview how pediatric pain is addressed in PT/OT/ST curricula/education and to derive essential contents for a specialized pediatric pain curriculum for therapists involved in pediatric pain. The review was carried out based on the recommendations of “PRISMA Extension for Scoping Reviews“ [19,20].
2.2.1. Search Strategy
From 6–10 December 2020, three independent authors (ML, KK and AS) performed the search in five databases (Medline [PubMed], Cochrane, CINAHL, PEDro, OTSeeker). Different combinations of the following terms were used: pain; curriculum; physiotherapy; occupational therapy; sports therapy; exercise therapy; sports medicine. The literature search strategy of Medline (via Pubmed) is exemplarily provided in Box 1:
Box 1. Literature search strategy Medline via Pubmed (search 6/12/2020).
(“Pain”[Mesh]
OR “pain“[tiab]) AND (“Curriculum”[Mesh] OR “curricul*”[tiab]) AND ((((((((“Physical
Therapy Specialty”[Mesh]) OR “Occupational Therapy”[Mesh]) OR “Exercise”[Mesh])
OR “Exercise Therapy”[Mesh])) OR “Sports”[Mesh]) OR “Sports Medicine”[Mesh])
OR (“Physiotherap*” OR “Physical therap*” OR “Occupational therap*” OR “sports
therap*”))
The authors assumed that there are hardly any specific curricula for pediatric pain management, therefore a broader search strategy was chosen. Wildcards and Boolean operators were used and all types of studies were included, without any date restriction. The search strategy for PubMed as depicted above was adapted for the other databases. Also, reference lists of the selected articles were reviewed to identify further important papers (backward citation tracking).
2.2.2. Selection Criteria
After de-duplication, the abstracts and eligible full texts were assessed by two authors (ML, KK) independently according to predefined criteria. Inclusion: articles written in English, German, French or Dutch; studies that refer to pain education curricula for movement therapists (physiotherapists, occupational therapists, sports therapists); studies reporting curriculum and/or education training contents regarding pain management for those professions; mention of pediatric/adolescent/child pain, or pain in vulnerable people, or pain across the lifespan. The exclusion criteria represented editorials or congress abstracts, or when no full text was available.
2.2.3. Data Extraction and Critical Appraisal
Data were extracted from the texts, tables, figures and supplement documents of the selected publications. Two investigators independently reviewed the articles and disagreements were discussed until a consensus was reached (ML, KK). The flowchart for the selection and screening method is provided in Figure 2.
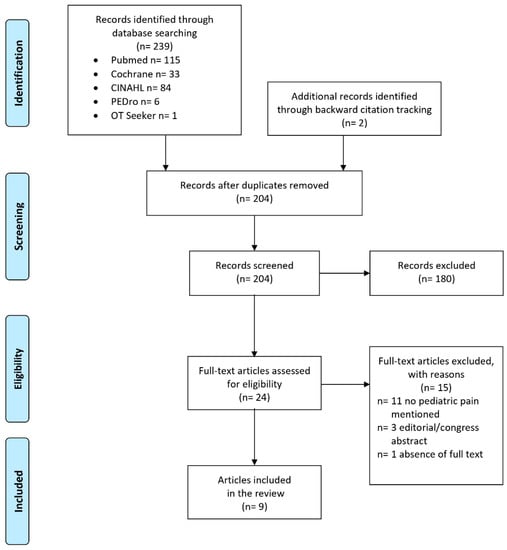
Figure 2.
Flowchart of the study selection process.
Data charting was done in a calibrated form that was developed and tested by two authors (ML, KK) before their use. Important contents of the included studies were selected and entered into this predefined table.
Since existing questionnaires for the critical appraisal of surveys did not exactly reflect criteria suitable for the evaluation, a special checklist for the quality grading was developed.
2.3. Survey
Since the literature review did not provide enough information of meaningful curricular contents, a survey among pediatric pain experts and/or pain educators was conducted using a self-constructed questionnaire for an online-survey.
2.3.1. Development of the Survey Instrument
In line with the analyzed studies in our review, our questionnaire was constructed based on the general pain curricula developed by experts from the International Association for the Study of Pain (IASP), the Interprofessional [21], the Physical Therapy [22], and the Occupational Therapy Pain Curriculum [23], and also the European Pain Federation (EFIC) Core PT Curriculum [24]. However as these curricula are not focused specifically on pediatric pain education, proposed contents for a specific PT/OT curriculum for pediatric pain education were mainly derived from guidelines and two best evidence reports regarding pediatric pain, which included at least parts for physical and/or occupational therapy (n = 7) [11,25,26,27,28,29,30]. The largest part of the derived items is depicted later in the results section.
The online questionnaire included a cover sheet with information regarding the background and the aim of the survey, and guarantee of anonymity and data protection. The first part of the survey included six questions to collect information about characteristics of the responders (country, profession, educational level/qualification, work setting, involvement in curriculum development). Further eight questions asked for information about possibly existing PT/OT courses in pediatric and/or general pain management in the national IASP chapters. Two free text questions asked which learning objectives and main core competencies should be acquired by PTs and OTs in a specialized pediatric pain course.
The second part of the questionnaire was structured analogous to the IASP Curricula in four areas: (1) Multidimensional nature of pediatric pain (13 items); (2) Assessment and measurement of pediatric pain (26 items); (3) Management of pediatric pain (27 items); (4) Specific clinical conditions in pediatric pain populations (two items). The proposed contents regarding the examples of specific pediatric assessment tools and special treatment considerations were compiled from two authors (ML, KK) in consultation and appraisal with the two others authors (AS, ME). Regarding each proposed content for the four curricular areas, we asked if it was covered in the responder’s possibly used curricula (is covered in our curriculum; is not covered in our curriculum; no specific curriculum available). Further it was investigated how important they considered each content (this item is very important; this item is important; this item is less important; this item is not important at all).
In an extra box the participants were invited to list any additional contents for each area they considered important. Another extra box was added for possible further comments. The online survey was constructed and conducted by means of the software SoSci Survey (version 3.2.23) [31]. The survey was pre-tested for comprehensibility and adequacy in a group of pain experts (n = 10), who suggested only some minor changes. The final survey was sent on 9 February 2021 to the IASP Organization with the request for assistance in dissemination.
2.3.2. Participating Experts
Addressees for our survey were defined as individuals being considered as experts in pediatric pain treatment and/or in pain education. With support from the IASP, the survey was at first distributed among the members of the Special Interest Groups ‘Pain in Childhood’, ‘Pain, Mind and Movement’ as well as ‘Pain Education’. All initially invited persons were asked to share the invitation and the weblink to other experts of their network. The survey was conducted in the period of 12 February till 12 March 2021.
2.3.3. Analysis
For quantitative data, descriptive statistics (frequencies and percentages) for each category were calculated. All statistical analyses were performed with SPSS software (v 25.0; IBM Corporation, Armonk, NY, USA). A summarizing content analysis according to Mayring [32] was chosen to analyze ‘free text responses’ for participants’ personal opinions about ‘learning objectives’ and ‘main core competencies’ as well as for additional suggestions for the 4 areas regarding curriculum contents. The responses were paraphrased, generalized, and a first coding scheme was built deductively (the defined 4 areas) and augmented by inductively emerging new aspects; quotes are presented as examples. The coding and analysis were led by KK, and checked for validity and reliability by ML. Discussion of findings and interpretations within the research team helped to ensure credibility and trustworthiness. The analysis was assisted by MAXQDA software for qualitative data analysis, version 12 (MAXQDA. © 1989–2016, VERBI Software Consult Sozialforschung GmbH, Berlin, Germany).
3. Results
3.1. Results of the Scoping Review
3.1.1. Study Selection
The literature search delivered 239 records; two additional records were identified through backward citation tracking (Figure 2). After removing duplicates, 204 records were screened from which 180 were excluded because they did not meet the inclusion criteria. After assessing the full texts of the remaining 24 articles, another 15 articles were excluded with reasons (n = 11 no pediatric pain mentioned, n = 3 editorial or congress abstract, n = 1 absence of full text). Finally, nine articles published between 2001 and 2020, fulfilled the inclusion criteria and were taken into account in the analysis [33,34,35,36,37,38,39,40,41]. An update of the literature search on 27 April 2021 in Medline, Cochrane, CINAHL, PEDro and OTSeeker databases delivered no new relevant records.
3.1.2. Study Characteristics and Contents
The included articles (n = 9) contained general information about approximately 278 educational pain programs in six different regions. The results of the included studies are summarized in Table 1.

Table 1.
Characteristics and main findings of included studies.
Most represented were pre-licensure/undergraduate programs from the USA [33,34], USA and Canada [35], North America and Canada [36], Canada [37,38], Australia [39], Spain [40], the Netherlands and international experts [41].
Most of the studies focused on PT programs [33,35,36,38,39], one on an OT program [34]. The remaining three programmes included several disciplines, among others also OT and PT [37,40,41]. Unfortunately, the data base search did not reveal any studies with information about a pain curriculum in sports therapy programs, thus we excluded this group from further investigations.
Different aspects of curricula were analyzed in the studies. Most of them carried out a survey to derive information about the contents and/or extent of pain education in current educational programs [33,34,36,37,38,40].
All the studies based their evaluation on one or more IASP Curricula [21,22,23]: either the interprofessional curriculum [40,41], or the PT Curriculum [33,38,39], or PT Curriculum and OT Curriculum [36], or PT and interprofessional curriculum [35], or all three [34,37]. Nevertheless, the IASP curricula were not universally followed in the educational programs: some of them implemented only a part of the items from the IASP domains cf. [33,36,38,40,41]. Most of the pain contents were embedded in the educational therapists’ programs and a few studies depicted some stand-alone pain courses (e.g., [33,36,37,38]). The total hours of pain contents varied greatly between the programmes, with a range of 4–129 h. Different groups were targeted in the evaluations: faculty directors or faculty members, pain experts, pain educators or students.
3.1.3. Pediatric Pain Contents
Authors criticized that pediatric pain items were given too little consideration in the existing courses, and programs including specific pediatric pain contents were scarce [36,37,38,40]. For example, one study stated that 28.6% of the PT programs addressed assessment and management of pediatric pain in sufficient depth [38].
3.1.4. Critical Appraisal of the Included Studies
Existing questionnaires for the critical appraisal of surveys do not reflect criteria suitable for our evaluation. Therefore, 10 questions from existing questionnaires and reporting guidelines were derived for the evaluation [42,43,44]. Table 2 shows that all the studies almost meet all of the appraisal criteria with the exception of 2 publications that did not exactly apply a survey methodology [35,39].

Table 2.
Critical Appraisal of the studies included in the scoping review.
3.2. Results of the Survey
3.2.1. Sample Characteristics
A total of n = 45 international pain experts from 18 different countries responded to the survey: European countries (n = 18; 40%); Australia (9; 20%); North-America (8; 17.8%); Africa (4; 8.9%); South-America (2; 4.4%); Asia (1; 2.2%); unknown (3; 6.7%). Concerning the professions, the most highly represented were physiotherapy (n = 28; 62.2%) followed by medicine (6; 13.3%), occupational therapy (4; 8.9%), psychology (3; 6.7%), nursing experts (2; 4.4%), and one response from clinical pharmacology (1; 2.2%) and from epidemiology (1; 2.2%), respectively. Regarding academic qualifications most of the respondents had a PhD/doctoral degree (n = 20; 44.5%), followed by a Master’s degree (11; 24.4%), Bachelor’s degree (5; 11.1%), or other (e.g., vocational school level, 5; 11.1%), 4 (8.9%) had a doctoral degree and another 4 were habilitated (8.9%). A high proportion of responders (73.3%) worked in a pain management setting, and 80% worked with children suffering from pain, with more than half of experts working with chronic pain and a negligible minority with acute pain. The responders were to a great extent (n = 29; 64,4%) involved in delivering (developing or teaching) a pain curriculum for health care professionals.
3.2.2. Specialized Pain Management Courses
Only 4 responders (n = 8.9%) confirmed positively that their country chapter provides stand-alone specialization courses for pediatric pain management, 1 for PTs, 1 for OTs, and 2 for both, with a range of 2–17 h. Regarding generalized specialization courses for pain management, 16 (35.6%) of the participants confirmed positively that their country chapter provides such specialization courses, among 6 of such a course comprised >80 h. Overall, a range from 1–100 h was stated. Among 7 of those general courses stated above include a specific pediatric pain module with a range from 1–12 h.
To the open questions regarding main learning objectives and main core competencies for a specialized pediatric pain educational course, divergent answers were supplied, most of them coincided with the items already listed in our proposed contents for the curriculum.
Regarding learning objectives, the biopsychosocial approach appeared in almost all the answers and foundational knowledge of (pediatric) pain neuroscience/neurophysiology, in particular the differences between children’s and adult’s pain presentation, were mentioned. Further several answers refer to the particularly attentive way of dealing with this vulnerable group of pain patients and the importance of involving the environment (parents, school, peers) in the pain management. Some examples:
“Understanding the neuroscience behind chronic pain and learning different ways to speak of it to families and children using metaphors, stories, toys, etc. …”(#150; OT)
“… Difference in pain management in children vs adults”(#180; Medicine)
“… it is important to take into account how the child experiences pain, and whenever possible to ask them and let them “tell” what their day-to-day life is like, of course, without losing sight of the family’s opinion…”(#193; PT)
“…Considerations of language and it’s use, ways to simplify and enhance interventions to be understood by young people… The role of parents, attachment and family system functioning on pediatric pain…”(#352; OT)
Regarding the core competencies, it was also noticeable that emphasis was placed on competencies related to communication and educational skills in handling with these vulnerable patients and their families, e.g.,:
“… empathy and feeling with the problems of acute and chronic pain in children …”(#248; Nursing)
“… Be able … to coach the child and her/his family in adopting valued life goals.”(#267; Psychology)
“… Affinity with this population, determination, enthusiasm and not careful in treating pediatric pain…”(#286; PT)
Furthermore, importance of interdisciplinary work and training was clearly advocated, e.g.,:
“It would be nice if there was specific training, not just for physical and occupational therapists, but for a whole multidisciplinary team...”(#248; Nursing)
“Ability to work in concert with a multi-disciplinary team including understanding how to communicate and maximize collaboration with physicians and psychologists.”(#133; PT)
These comments were also reflected in the answers to the closed questions.
To the question: “Which contents … are covered in your curriculum and/or do you rate as important for a specialization curriculum for pediatric pain management specific for PTs and OTs.?” 18-32/45 experts gave a response (Figure 3, Figure 4, Figure 5 and Figure 6). About half of them stated that they have no specific curriculum and only a part of the responders stated that they covered partially some items in their curriculum.
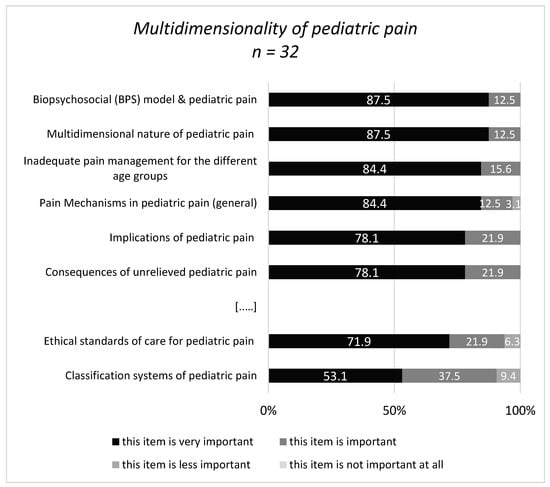
Figure 3.
Response categories with highest/lowest accordance in area 1 (Multidimensionality). […..]: omission of items in the medium range.
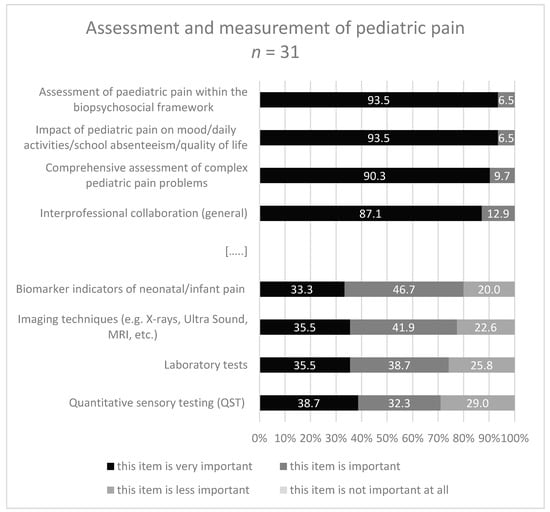
Figure 4.
Response categories with highest/lowest accordance in area 2 (Assessment). […..]: omission of items in the medium range.
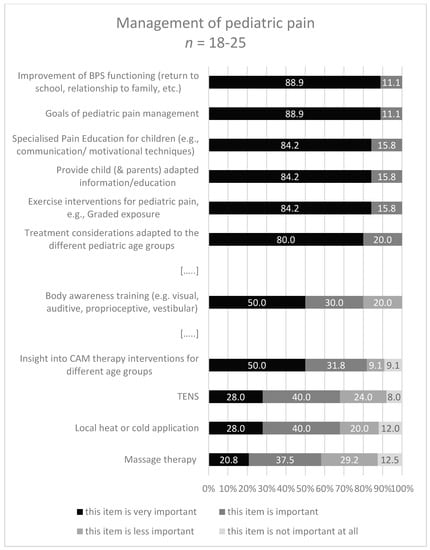
Figure 5.
Response categories with highest/lowest accordance in area 3 (Management). […..]: omission of items. BPS: biopsychosocial; CAM: complement & alternative therapy interventions.
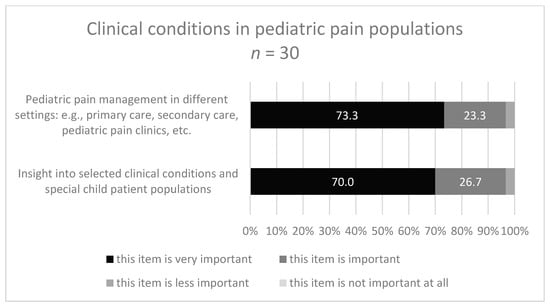
Figure 6.
Response categories with highest/lowest accordance in area 4 (Clinical conditions).
Regarding importance of the contents most of the responders classify the proposed contents in the categories ‘important’ or ‘very important’.
Within the first area ‘Multidimensionality of pediatric pain’ the content definition of pain occurred most frequently (50%) and the content ‘inadequate pediatric pain management for the different age groups’ was the most frequently not covered content (35.7%).
The contents with the highest percentage in the category ‘very important’ were ‘the biopsychosocial model and the multidimensional nature of pediatric pain’ (both 87.5%). Further ratings within the multiple, divergent response categories are illustrated in Figure 2 with regard to the most and least important items, respectively.
The experts were also invited to add suggestions for further contents for this area.
Once again, the biopsychosocial framework was in the foreground and the consideration of childhood development trajectories was mentioned, e.g.,:
“… Attachment and role of developmental trauma on development (including how this impacts threat detection) …”(#352; OT)
“… vulnerable populations (indigenous, remote and rural regions, co-morbid mental health, in justice systems; socially dislocated)”(#225; PT)
“…Yes—general developmental trajectories, underlying neurodevelopmental disorders and their interaction with persistent pain disorders, e.g., Autism …”(#352; OT)
Within the second area ‘Assessment and measurement of pediatric pain’ the content ‘unidimensional tools for pediatric pain intensity’ occurred most frequently (48.3%) in the curricula, and the content ‘biomarker indicators of neonatal/infant pain’ was the most frequently not covered content (35.7%). The contents with the highest rating in the category ‘very important’ were ‘assessment of pediatric pain within biopsychosocial framework’ (93.5%), and ‘impact of pediatric pain on mood, usual activities/function/quality of life/sleep/school absenteeism’ (93.5%). Further ratings with the multiple, divergent response categories are illustrated in Figure 4.
Some suggestions for further contents for this area were inclusion of the child’s environment in the assessment procedure. Furthermore, using a framework like ICF or core outcomes for assessment was recommended, e.g.,:
“I think it’s also important to teach assessment using a conceptual framework like … interpretation of the ICF model…”(#133; PT)
“…Concept of Pain Inventory (COPI) for identifying and addressing specific conceptual ‘gaps’ and misconceptions…”(#347; PT)
“… too often the diagnosis is made too late and there is poor (too little) proper follow-up from the various disciplines...”(#248; Nursing)
In the third area ‘Management of pediatric pain’ the subheading ‘goals of pediatric pain management’ occurred most frequently (44.4%), and the content ‘massage therapy’ was the most frequently not covered content (33.3%).
The contents with the highest rating in the category ‘very important’ were ‘goals of pediatric pain management’ (88.9%) and ‘improvement of bio-, psycho-, social functioning: return to school, relationship to family, etc.’ (88.9%). Further ratings with the multiple, divergent response categories are illustrated in Figure 5.
Suggestions for the third area also placed emphasis on the inclusion of the child’s environment (parents, peers, school, sports, …) in decisions and management. Furthermore, the inclusion of psychological strategies and motivational techniques adapted to children and focusing on activation and self-management were proposed, e.g.,:
“…Use of reward/reinforcement to increase adherence to treatment/exercise program…”(#222; Psychology)
“… Yes, occupational therapists should be able to tailor activity to be both developmentally sensitive and aligned with patient interests…”(#352; OT)
“...teach children to mobilize again and motivate them to move...”(#248; Nursing)
“We focus on self-management strategies and do not teach or promote aquatic therapy (unless the patient is a swimmer), TENS, heat, massage or ice.”(#133; PT)
The two items of the area ‘Specific clinical conditions in pediatric pain populations’ were not frequently covered in the curricula: 25.9% covered ‘insight into selected clinical conditions and special child patient populations’, and 25% covered ‘pediatric pain management in different settings’. Both items were rated as ‘very important’ by 70% and 73.3%, respectively (Figure 6).
Suggestions for the fourth area ‘Specific clinical conditions in pediatric pain populations’ focused on chronic pain and on complex conditions in this vulnerable patient group, e.g.,:
“It is important to understand the complex presentations, particularly those which are associated with high levels of misinformation, distress or stigma in the community.”(#352; OT)
“Managing pain for children and adolescents with complex neurological impairment such as cerebral palsy or autism spectrum disorder.”(#157; OT)
“Setting—school context—how interventions can be delivered in this setting…”(#222; Psychology)
The comparison of experts’ ratings and guidelines that covered this item shows large congruence. Almost all of the highest rated contents by experts (‘very important’) were also found in almost all of the consulted guidelines. Items with a low rating, e.g., “use of laboratory tests/imaging techniques” or ‘insight into the opportunities of CAM (=complement and alternative therapy interventions) for different pediatric age groups’ were also less depicted in the guidelines, see Table 3. This table compares the ratings of the survey responders with the number of guidelines that recommended this content, both shown in percentages.

Table 3.
Comparison of experts’ ratings and guidelines.
4. Discussion
The study provides important information on pediatric pain education issues especially for PTs and OTs. To the best of our knowledge, this is one of the first studies which systematically evaluates contents for a pediatric pain education curriculum for therapists. By combining the different methods: scoping survey, consideration of guideline recommendations and the expert survey a well-founded catalogue of contents was generated.
Our first aim was to extract important contents for a pediatric pain education curriculum for specialized pain therapists from the existing literature. A broad literature search resulted in nine studies with reference to pediatric themes in PT and or OT programs, but none about a pain curriculum in sports therapy programs. Therefore, this profession was excluded from our further investigations, but should all the more be considered in further research and in practice with regard to interprofessional pediatric pain management.
Nevertheless, from the articles included in our review we could derive information about content and extent of pain education in about 278 educational pain programs in six different regions. Especially the studies from the USA and Canada [33,35,37], but also the study from Spain [40], were delivered by teams that included experts who were also task force members of the IASP interprofessional or PT curricula. We could show clearly that most of the programs include very few pediatric topics although all stated the importance of such topics for pain education. However, the results of the studies did not allow to derive in-depth information on adequate contents for a specialized pediatric pain education program.
As a consequence, and as a second step of our project, a survey among pediatric pain experts was conducted. The survey provided information about specific pediatric contents included in the curricula used or developed by the pain experts and depicted their opinion regarding the importance of such contents for a specialized curriculum. The proposed contents for the pediatric pain PT-/OT-curriculum in our questionnaire were mainly derived from recent pediatric pain guidelines, which include PT and OT recommendations. The contents were classified in line with the four domains of the IASP and EFIC curricula [21,22,23,24]. This is a common approach, also propagated by the pain curricular development experts in an IASP Factsheet regarding ‘Pain Curriculum Design Models and Implementation Approaches’ [45].
By inviting the members of three of the IASP Special Interest Groups, we gathered a representative international sample of 45 experts in pediatric pain as well as of educational experience, most of them PTs but also OTs and other professions. We had a majority of PTs compared to OTs in our sample and this is a similar phenomenon in previous curricular studies [16,40,41].
One of the key findings from the survey is that actually there is insufficient specific education for OTs and PTs on the management of pediatric pain. There were hardly any curricula for pediatric pain present and if pediatric pain is covered, then this was limited to a few hours. This is in line with the results of our review, where several studies also reported a low coverage of pediatric themes and inadequate time spent on this topic [33,36,37,38,40]. We also found that little of the contents were included in the curricula mentioned by the experts, if available. It seems that a basic training on general pain management is often prioritized. But given the growing prevalence of pediatric pain at the very least an introduction to this problem should be part of the curricula for standard training to raise awareness among the students for this issue. It is to be expected that only a small number of students are interested to go into depth of this topic, so it seems sensible to build on these introductory hours in subsequent stand-alone specialization courses. The provision of postgraduate specialization courses and eventually online specialized pain education resources could be a solution to cover the deficits on pediatric pain management among OTs and PTs, but there are few specialization courses at present [14]. One interesting online pediatric pain curriculum based on the interprofessional IASP Curriculum [21] is currently available at the homepage of SickKids [46]. Another learning curriculum offers free accessible, downloadable guidance [47]. Both addressed not specific PTs/OTs but all health care providers who are interested in pediatric pain management.
With regard to the survey results we were able to draw on expertise and on evidence-based clinical reasoning of pediatric pain. In each of the four areas, the most important contents were clearly highlighted and the highest rated contents were also the contents that were represented in all the guidelines.
Contents regarding active interventions (e.g., graded exposure) were considered more important in comparison to passive interventions (e.g., massage), which is in line with best evidence recommendations for pediatric pain rehabilitation [11]. Exercise therapy guided by PTs and/or OTs has become an integral part of interdisciplinary pediatric pain programs [48]. In fact, there is little evidence for passive techniques, yet some specific pediatric populations may benefit from them. Massage therapy may reduce pain and anxiety among children with cancer [49,50]. There is also growing evidence regarding skin-to-skin contact especially to reduce procedural pain in neonates and infants [51,52,53,54].
It was encouraging to see that the biopsychosocial approach is of central relevance for almost all responders. It is state-of-the-art to assess biological, psychological, and sociocultural information to plan an adequate multimodal pediatric management [47]. Even when a physical component such as generalized joint hypermobility has been demonstrated in adolescents, psychosocial factors (e.g., catastrophizing thoughts, pain-related anxiety) appear to have an impact on the development or maintenance of chronic musculoskeletal pain [55]. Furthermore, educational curricula addressing psychosocial aspects and considering the children’s life situation, seem to better prepare therapists for their health-focused practice [56].
Particularly important contents for the pediatric target group were clearly identified, e.g., to assess the “impact of pediatric pain on mood, daily activities, school absenteeism, quality of life”. Or in the area “pain management” some pediatric specific goals were considered very important, e.g., improvement of functioning: return to school, relationship to family and peers, etc. These are all recommended contents in pediatric pain rehabilitation [57,58].
Especially the answers to the open questions were able to map that the responding experts put a special emphasis on the differences in pain presentation and handling with a pediatric population compared to adults. Pediatric patients should not be treated like small adults, they need a specialized assessment and management [54,58], and an adequate interaction and communication between therapists-child -parents is imperative [59,60].
Children/youth adapted communication style and the use of informative adapted materials suitable for children and parents were often recommended among the experts in our survey, what is also reflected in the current literature [59,60]. For an adapted education about pain neuroscience vivid, child-friendly materials are available in different languages, e.g., an educational video ”Understanding pain—and what’s to be done about it in 10 min!” [61], a cartoon book ”A Journey to Learn about Pain” [62,63,64], or a pain neuroscience education program for children “PNE4Kids” [65,66].
When interpreting the results, it should be noted that this study is not exempt from limitations. First, as the survey was distributed anonymous via the IASP special interest groups and individual private networks, we could not calculate an exact response rate, because it is not known how many from those invited responded to the questionnaire. Further, it should be considered that data based on self-reporting can give a risk of bias; however, the survey was completely anonymous. The quality of an expert panel’s judgement is highly dependent on the composition of the sample [18]. Based on characteristics and quality of open comments on the questionnaire of this current expert sample, a high level of expertise on pediatric pain education and pediatric pain management could be assumed.
Second, it was not compulsory to answer all the questions, the respondents (n = 45) could skip some questions of the survey. This resulted in varying numbers of responders on the questions regarding covering of items in the curricula or importance of our proposed contents. Although our results focused mainly on chronic pediatric pain, the prevention of pain and timely interventions for acute pain in children should certainly not be ignored. Pain experiences in childhood can make children vulnerable to chronic pain in adulthood [5]. Non-pharmacological interventions are effective in the prevention of pediatric pain and exercise/physical activity (PT and OT) find their rightful place in the treatment of acute pain [67,68].
Furthermore, we could not derive the ideal amount of hours needed for a specialization PT-/OT-program for pediatric pain, as the literature depicted very heterogeneous numbers. The number of hours indicated by the experts between 7 and 12 h seem low for such a complex subject. Based on many years of experience in the teaching of pain management, the authors would recommend a minimum of 20 to 30 h, provided the participant PTs/OTs have previously completed a general basic pain course of at least 80 h.
But overall, both results, those from the review and those from the survey, illustrate a severe underrepresentation of pediatric pain topics in the existing curricula. Fortunately, the results of the survey depicted also clearly that the respondents highly agree to the necessity for a pediatric pain education curriculum for PTs and OTs. Specialized training is essential for improving pediatric pain management programs. In the meantime the integration of pain specialized PTs and OTs in the interdisciplinary multimodal pain teams is demanded to meet the quality standards for adults’ patients pain programs [69]. Also, in the pediatric pain teams the expertise of PT s and OTs becomes more and more relevant [70].
Regarding future lines it should be considered that this study involves only a first step in the direction of a specialized curriculum development. The evaluated contents could be integrated in a curricular model. Currently different models and perspectives for curricular development exist, e.g., a theoretical framework especially for health care providers education as proposed in the publication of Steketee et al. [71]. They described a curriculum with 4 dimensions with the following recommendations: identify the practice needs, define the capabilities, consider the teaching modus and the institutional structure.
5. Conclusions
This study was an important project to evaluate adequate contents for a specialized pediatric pain curriculum for PTs and OTs. The three components (review of the literature; guideline recommendations; experts’ survey) of this study provide a consistent picture that indicates an urgent need for action. The review and the survey reveal the almost non-existent opportunities for pediatric pain specialization for PTs and OTs and, if present in the curricula, then only with very small hourly amounts. The recommendations from the guidelines and those of the experts in the survey provide homogenous, concrete recommendations for required contents, which now need to be systematically transferred into a curriculum.
Furthermore, the project reflects a clear recognition about the specialized needs in the management of pediatric patients and their environment. Especially in the survey, the experts emphasized the importance of involving the parents, school teachers, and peers in the pain management decisions. Further competencies related to communication and educational skills in handling with these vulnerable patients were recommended.
It would be highly recommended to integrate general pain management themes with a short introduction about pediatric pain already in the undergrade educational level for PTs and OTs. An in-depth specialized pediatric pain education should be delivered as a stand-alone course (for experienced professionals), requiring basic knowledge and skills about pain in general. Our survey shows a clear need to build up such a specific curriculum according to the four IASP domains, focused to and enriched by specific pediatric pain issues, e.g., (1) multidimensionality of pediatric pain; (2) specific assessment of pediatric pain; (3) management of pediatric pain (4) clinical conditions in pediatric pain populations. Considering there may not be a very large population of PTs and OTs interested in a pediatric pain specialization course, an online course could also be taken into consideration. Further research and curriculum work is highly recommended, and interdisciplinary as well as international networking could lead to efficient use of knowledge, experiences, and resources.
Author Contributions
Conceptualization, M.L. and K.K.; methodology, M.L., A.S., M.E.M., and K.K.; investigation, M.L. and K.K.; formal analysis, M.L. and K.K.; software, K.K.; data curation, K.K.; writing—original draft preparation, M.L. and K.K.; writing—review and editing, A.S. and M.E.M.; visualization, K.K.; project administration, K.K and M.L. All authors have read and agreed to the published version of the manuscript.
Funding
Funding support for the Open Access publication was given by the Department of General Practice/Family Medicine of the Philipps-University Marburg.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable for the literature review. Experts consented by voluntarily participating in the strictly anonymous online survey. We did not obtain any personal or institutional information by which persons could be identified. As analyses based on anonymized questionnaires regarding experts’ opinions does not fall within the scope of the Medical Research Involving Human Subjects Act there is no requirement for ethical approval.
Data Availability Statement
Materials of the expert survey are available from the corresponding author on reasonable request.
Acknowledgments
We would like to express our gratitude to the experts participating and giving detailed comments in the expert survey. Furthermore, the authors would like to thank the experts who provided constructive feedback to the pre-test of the online survey.
Conflicts of Interest
M.L., M.E.M. and K.K. developed and teach a postgraduate specialized pain physiotherapy training (based on the IASP Curriculum), which contains a 4-h pediatric pain module, through the German Pain Society. All authors declare no conflict of interest.
References
- Eccleston, C.; Fisher, E.; Howard, R.F.; Slater, R.; Forgeron, P.; Palermo, T.M.; Birnie, K.A.; Anderson, B.J.; Chambers, C.T.; Crombez, G.; et al. Delivering transformative action in paediatric pain: A Lancet Child & Adolescent Health Commission. Lancet Child Adolesc. Health 2021, 5, 47–87. [Google Scholar] [PubMed]
- Stevens, B.J.; Abbott, L.K.; Yamada, J.; Harrison, D.; Stinson, J.; Taddio, A.; Barwick, M.; Latimer, M.; Scott, S.D.; Rashotte, J.; et al. Epidemiology and management of painful procedures in children in Canadian hospitals. CMAJ Can. Med. Assoc. J. 2011, 183, E403–E410. [Google Scholar] [CrossRef]
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Mathews, L. Pain in children: Neglected, unaddressed and mismanaged. Indian J. Palliat. Care 2011, 17, S70–S73. [Google Scholar] [CrossRef]
- Fitzgerald, M.; Walker, S.M. Infant pain management: A developmental neurobiological approach. Nat. Clin. Pract. Neurol. 2009, 5, 35–50. [Google Scholar] [CrossRef]
- Belavy, D.L.; van Oosterwijck, J.; Clarkson, M.; Dhondt, E.; Mundell, N.L.; Miller, C.T.; Owen, P.J. Pain sensitivity is reduced by exercise training: Evidence from a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 120, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, A.; Laekeman, M.; Egan Moog, M.; Dieterich, A.V. “On the move”—Prevention of chronic pain with physical activity and movement: [„On the Move“—Prävention chronischer Schmerzen durch körperliche Aktivität und Bewegung]. Schmerz 2021, 35, 14–20. [Google Scholar] [CrossRef]
- Caes, L.; Fisher, E.; Clinch, J.; Eccleston, C. Current Evidence-Based Interdisciplinary Treatment Options for Pediatric Musculoskeletal Pain. Curr. Treat. Options Rheumatol. 2018, 4, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Kichline, T.; Cushing, C.C. A systematic review and quantitative analysis on the impact of aerobic exercise on pain intensity in children with chronic pain. Child. Health Care 2019, 48, 244–261. [Google Scholar] [CrossRef]
- Nijhof, L.N.; Nap-van der Vlist, M.M.; van de Putte, E.M.; van Royen-Kerkhof, A.; Nijhof, S.L. Non-pharmacological options for managing chronic musculoskeletal pain in children with pediatric rheumatic disease: A systematic review. Rheumatol. Int. 2018, 38, 2015–2025. [Google Scholar] [CrossRef]
- Harrison, L.E.; Pate, J.W.; Richardson, P.A.; Ickmans, K.; Wicksell, R.K.; Simons, L.E. Best-Evidence for the Rehabilitation of Chronic Pain Part 1: Pediatric Pain. J. Clin. Med. 2019, 8, 1267. [Google Scholar] [CrossRef] [PubMed]
- Stahlschmidt, L.; Zernikow, B.; Wager, J. Specialized Rehabilitation Programs for Children and Adolescents with Severe Disabling Chronic Pain: Indications, Treatment and Outcomes. Children 2016, 3, 33. [Google Scholar] [CrossRef] [PubMed]
- Hechler, T.; Kanstrup, M.; Holley, A.L.; Simons, L.E.; Wicksell, R.; Hirschfeld, G.; Zernikow, B. Systematic Review on Intensive Interdisciplinary Pain Treatment of Children With Chronic Pain. Pediatrics 2015, 136, 115–127. [Google Scholar] [CrossRef]
- Hurley-Wallace, A.; Wood, C.; Franck, L.S.; Howard, R.F.; Liossi, C. Paediatric pain education for health care professionals. Pain Rep. 2019, 4, e701. [Google Scholar] [CrossRef]
- Briggs, E.V.; Carr, E.C.J.; Whittaker, M.S. Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom. Eur. J. Pain 2011, 15, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Leegaard, M.; Valeberg, B.T.; Haugstad, G.K.; Utne, I. Survey of Pain Curricula for Healthcare Professionals in Norway. Nord. J. Nurs. Res. 2014, 34, 42–45. [Google Scholar] [CrossRef]
- Reyes, A.N.; Brown, C.A. Occupational therapists’ pain knowledge: A national survey. Disabil. Rehabil. 2016, 38, 1309–1317. [Google Scholar] [CrossRef] [PubMed]
- Plomp, T. Educational Design Research: An Introduction. In Educational Design Research: Part A: An Introduction; Plomp, T., Nieveen, N., Eds.; The Netherlands Institute for Curriculum Development (SLO): Enschede, The Netherlands, 2013; pp. 10–51. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Equator Network. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. The EQUATOR Network (equator-network.org). Available online: https://www.equator-network.org/reporting-guidelines/prisma-scr/ (accessed on 11 December 2020).
- IASP. IASP Interprofessional Pain Curriculum Outline. Available online: https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=2057 (accessed on 8 January 2021).
- IASP. IASP Curriculum Outline on Pain for Physical Therapy. Available online: https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=2055 (accessed on 7 January 2021).
- IASP. IASP Curriculum Outline on Pain for Occupational Therapy. Available online: https://www.iasp-pain.org/Education/CurriculumDetail.aspx?ItemNumber=7069 (accessed on 7 January 2021).
- EFIC. European Pain Federation—Core Curriculum for the European Diplom in Pain Physiotherapy. Available online: https://europeanpainfederation.org/wp-content/uploads/2018/10/EFIC-Pain-Physiotherapy-Curriculum1.pdf (accessed on 7 January 2021).
- NVK; Nederlandse Vereniging voor Kindergeneeskunde. Somatisch Onvoldoende Verklaarde Lichamelijke Klachten (SOLK) Bij kinderen (Somatically Unexplained Physical Complaints): Richtlijn. Available online: https://www.nvk.nl/themas/kwaliteit/richtlijnen/richtlijn?componentid=6488085&tagtitles=Maag-Darm-Leverziekten%2B(MDL),Neonatologie,Sociale%2Ben%2BPsychosociale%2Bkindergeneeskunde (accessed on 7 January 2021).
- The Scottish Government. Management of Chronic Pain in Children and Young People: A National Clinical Guideline; The Scottish Government: Edinburgh, UK, 2018. [Google Scholar]
- Draheim, N.; Ebinger, F.; Schnöbel-Müller, E.; Wolf, B.; Häuser, W. Definition, diagnostics and therapy of chronic widespread pain and the (so-called) fibromyalgia syndrome in children and adolescents [Definition, Diagnostik und Therapie von chronischen Schmerzen in mehreren Körperregionen und des (sog.) Fibromyalgiesyndroms bei Kindern und Jugendlichen: Aktualisierte Leitlinie 2017]. Schmerz 2017, 31, 296–307. [Google Scholar] [PubMed]
- Williams, G.; Howard, R.F.; Liossi, C. Persistent postsurgical pain in children and young people: Prediction, prevention, and management. Pain Rep. 2017, 2, e616. [Google Scholar] [CrossRef]
- González-María, E.; Fuentelsaz-Gallego, C.; Moreno-Casbas, T.; Gil-Rubio, P.; Herreros-López, P.; on behalf of the work group of the Clinical Practice Guideline for Pain Management in Children With Cancer. Clinical Practice Guideline for Pain Management in Children with Cancer. Available online: http://www.criscancer.org (accessed on 8 January 2021).
- World Health Organization. Guidelines on the Management of Chronic Pain in Children; World Health Organization: Geneva, Switzerland; Available online: https://apps.who.int/iris/handle/10665/337999 (accessed on 7 January 2021).
- Leiner, D.J. SoSci Survey. Available online: https://www.soscisurvey.de (accessed on 15 March 2021).
- Mayring, P. Qualitative Inhaltsanalyse: Grundlagen und Techniken, 12th ed.; Beltz: Weinheim, Germany, 2015. [Google Scholar]
- Hoeger Bement, M.K.; Sluka, K.A. The current state of physical therapy pain curricula in the United States: A faculty survey. J. Pain 2015, 16, 144–152. [Google Scholar] [CrossRef]
- Rochman, D.L.; Sheehan, M.J.; Kulich, R.J. Evaluation of a pain curriculum for occupational therapists: Experiences from a master’s-level graduate program over six years. Disabil. Rehabil. 2013, 35, 1933–1940. [Google Scholar] [CrossRef]
- Hoeger Bement, M.K.; St Marie, B.J.; Nordstrom, T.M.; Christensen, N.; Mongoven, J.M.; Koebner, I.J.; Fishman, S.M.; Sluka, K.A. An interprofessional consensus of core competencies for prelicensure education in pain management: Curriculum application for physical therapy. Phys. Ther. 2014, 94, 451–465. [Google Scholar] [CrossRef] [PubMed]
- Scudds, R.J.; Scudds, R.A.; Simmonds, M.J. Pain in the physical therapy (pt) curriculum: A faculty survey. Physiother. Theory Pract. 2001, 17, 239–256. [Google Scholar] [CrossRef]
- Hunter, J.; Watt-Watson, J.; McGillion, M.; Raman-Wilms, L.; Cockburn, L.; Lax, L.; Stinson, J.; Cameron, A.; Dao, T.; Pennefather, P.; et al. An interfaculty pain curriculum: Lessons learned from six years experience. Pain 2008, 140, 74–86. [Google Scholar] [CrossRef] [PubMed]
- Wideman, T.H.; Miller, J.; Bostick, G.; Thomas, A.; Bussières, A.; Wickens, R.H. The current state of pain education within Canadian physiotherapy programs: A national survey of pain educators. Disabil. Rehabil. 2020, 42, 1332–1338. [Google Scholar] [CrossRef] [PubMed]
- Hush, J.M.; Nicholas, M.; Dean, C.M. Embedding the IASP pain curriculum into a 3-year pre-licensure physical therapy program: Redesigning pain education for future clinicians. Pain Rep. 2018, 3, e645. [Google Scholar] [CrossRef] [PubMed]
- Miró, J.; Castarlenas, E.; Solé, E.; Martí, L.; Salvat, I.; Reinoso-Barbero, F. Pain curricula across healthcare professions undergraduate degrees: A cross-sectional study in Catalonia, Spain. BMC Med. Educ. 2019, 19, 307. [Google Scholar] [CrossRef]
- van Lankveld, W.; Afram, B.; Staal, J.B.; van der Sande, R. The IASP pain curriculum for undergraduate allied health professionals: Educators defining competence level using Dublin descriptors. BMC Med. Educ. 2020, 20, 60. [Google Scholar] [CrossRef]
- Center for Evidence-Based Management (CEBMa). What Is Critical Appraisal?—Center for Evidence Based Management. Available online: https://cebma.org/resources-and-tools/what-is-critical-appraisal/ (accessed on 28 April 2021).
- Artino, A.R.; Durning, S.J.; Sklar, D.P. Guidelines for Reporting Survey-Based Research Submitted to Academic Medicine. Acad. Med. J. Assoc. Am. Med. Coll. 2018, 93, 337–340. [Google Scholar] [CrossRef]
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef]
- Watt-Watson, J.; Hogans, B.; Carr, E.; Gordon, D. IASP FACT SHEET No. 3 Pain Curriculum Design Models and Implementation Approaches. Available online: https://sbed.org.br/wp-content/uploads/2019/02/factsheet3paincurriculumdesignmodelsenglish2.pdf (accessed on 22 March 2021).
- SickKids. Online Paediatric Pain Curriculum. Available online: https://www.sickkids.ca/en/care-services/centres/pain-centre/#oppc (accessed on 28 March 2021).
- ChildKind. Pediatric Pain (PRN) Curriculum. Available online: https://childkindinternational.org/resources/pediatric-pain-prn-curriculum/ (accessed on 28 March 2021).
- Odell, S.; Logan, D.E. Pediatric pain management: The multidisciplinary approach. J. Pain Res. 2013, 6, 785–790. [Google Scholar] [CrossRef]
- Genik, L.M.; McMurtry, C.M.; Marshall, S.; Rapoport, A.; Stinson, J. Massage therapy for symptom reduction and improved quality of life in children with cancer in palliative care: A pilot study. Complement. Ther. Med. 2020, 48, 102263. [Google Scholar] [CrossRef]
- Radossi, A.L.; Taromina, K.; Marjerrison, S.; Diorio, C.J.; Similio, R.; Njuguna, F.; Afungchwi, G.M.; Ladas, E.J. A systematic review of integrative clinical trials for supportive care in pediatric oncology: A report from the International Society of Pediatric Oncology, T&CM collaborative. Support. Care Cancer 2018, 26, 375–391. [Google Scholar] [PubMed]
- Johnston, C.; Campbell-Yeo, M.; Disher, T.; Benoit, B.; Fernandes, A.; Streiner, D.; Inglis, D.; Zee, R. Skin-to-skin care for procedural pain in neonates. Cochrane Database Syst. Rev. 2017, 2, CD008435. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; McGrath, T.; Drendel, A.L. An Evidence-Based Approach to Minimizing Acute Procedural Pain in the Emergency Department and Beyond. Pediatr. Emerg. Care 2016, 32, 36–42. [Google Scholar] [CrossRef]
- Thrane, S.E.; Wanless, S.; Cohen, S.M.; Danford, C.A. The Assessment and Non-Pharmacologic Treatment of Procedural Pain From Infancy to School Age Through a Developmental Lens: A Synthesis of Evidence With Recommendations. J. Pediatr. Nurs. 2016, 31, e23–e32. [Google Scholar] [CrossRef]
- Krauss, B.S.; Calligaris, L.; Green, S.M.; Barbi, E. Current concepts in management of pain in children in the emergency department. Lancet 2016, 387, 83–92. [Google Scholar] [CrossRef]
- van Meulenbroek, T.; Huijnen, I.P.J.; Simons, L.E.; Conijn, A.E.A.; Engelbert, R.H.H.; Verbunt, J.A. Exploring the underlying mechanism of pain-related disability in hypermobile adolescents with chronic musculoskeletal pain. Scand. J. Pain 2021, 21, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Elvén, M.; Dean, E.; Söderlund, A. Augmented behavioral medicine competencies in physical therapy students’ clinical reasoning with a targeted curriculum: A final-semester cohort-comparison study. Physiother. Theory Pract. 2021, 1–12. [Google Scholar] [CrossRef]
- Hurtubise, K.; Brousselle, A.; Noel, M.; Camden, C. What really matters in pediatric chronic pain rehabilitation? Results of a multi-stakeholder nominal group technique study. Disabil. Rehabil. 2020, 42, 1675–1686. [Google Scholar] [CrossRef] [PubMed]
- Finley, G.A.; MacLaren Chorney, J.; Campbell, L. Not small adults: The emerging role of pediatric pain services. Can. J. Anaesth. J. Can. D’Anesthesie 2014, 61, 180–187. [Google Scholar] [CrossRef]
- Koechlin, H.; Locher, C.; Prchal, A. Talking to Children and Families about Chronic Pain: The Importance of Pain Education-An Introduction for Pediatricians and Other Health Care Providers. Children 2020, 7, 179. [Google Scholar] [CrossRef]
- Emerson, N.D.; Bursch, B. Communicating with Youth about Pain: Developmental Considerations. Children 2020, 7, 184. [Google Scholar] [CrossRef] [PubMed]
- Deutsches Kinderschmerzzentrum (DKSZ). Understanding Pain—And What’s To Be Done About It in 10 Minutes: Den Schmerz Verstehen—Und Was zu Tun Ist in 10 Minuten! Available online: https://www.deutsches-kinderschmerzzentrum.de/ueber-uns/videos/den-schmerz-verstehen/ (accessed on 17 March 2021).
- Pain in Motion. A Journey to Learn about Pain. (English). Available online: www.paininmotion.be/storage/app/media/materials/oct-18/A%20JOURNEY%20TO%20LEARN%20ABOUT%20PAIN_FINAL.pdf (accessed on 17 March 2021).
- Pesquisa em Dor Kids. Uma Jornada para Entender a Dor. (Portugues/Luso-Brasileiro). Available online: http://pesquisaemdor.com.br/?page_id=84 (accessed on 27 March 2021).
- Deutsche Schmerzgesellschaft e.V. Eine Geschichte Über Den Schmerz: (German). Available online: https://www.schmerzgesellschaft.de/topnavi/die-gesellschaft/arbeitskreise/schmerz-und-bewegung/ziele-1 (accessed on 27 March 2021).
- PNE4KIDS Program (English; Dutch; Danish). Available online: http://www.paininmotion.be/pne4kids (accessed on 8 May 2021).
- Pas, R.; Meeus, M.; Malfliet, A.; Baert, I.; van Oosterwijck, S.; Leysen, L.; Nijs, J.; Ickmans, K. Development and feasibility testing of a Pain Neuroscience Education program for children with chronic pain: Treatment protocol. Braz. J. Phys. Ther. 2018, 22, 248–253. [Google Scholar] [CrossRef]
- Friedrichsdorf, S.J.; Goubert, L. Pediatric pain treatment and prevention for hospitalized children. Pain Rep. 2020, 5, e804. [Google Scholar] [CrossRef]
- Gai, N.; Naser, B.; Hanley, J.; Peliowski, A.; Hayes, J.; Aoyama, K. A practical guide to acute pain management in children. J. Anesth. 2020, 34, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Pfingsten, M.; Arnold, B.; Böger, A.; Brinkschmidt, T.; Casser, H.-R.; Irnich, D.; Kaiser, U.; Klimczyk, K.; Lutz, J.; Schiltenwolf, M.; et al. Recommendations on structural and process parameters of the ad hoc commission “Interdisciplinary Multimodal Pain Therapy” of the German Pain Society (Deutsche Schmerzgesellschaft e. V.): [Sektorenübergreifende interdisziplinäre multimodale Schmerztherapie: Empfehlungen zu Struktur-und Prozessparametern der Ad-hoc-Kommission „Interdisziplinäre Multimodale Schmerztherapie“ der Deutschen Schmerzgesellschaft e. V.]. Schmerz 2019, 33, 191–203. [Google Scholar]
- Höfel, L.; Draheim, N.; Haas, J.-P.; Ebinger, F. Medical pain care for children and adolescents with chronic pain in Germany: An inventory: [Schmerzmedizinische Versorgung chronisch schmerzkranker Kinder und Jugendlicher in Deutschland: Eine Bestandsaufnahme]. Schmerz 2021, 35, 94–102. [Google Scholar] [CrossRef]
- Steketee, C.; Lee, A.; Moran, M.; Rogers, G. Towards a theoretical framework for curriculum development in health professional education. Focus Health Prof. Educ. 2013, 14, 64–77. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).