Abstract
Background/Objectives: The COVID-19 pandemic has impacted the lifestyles of children and adolescents because of the restrictions imposed to contain the infection. This systematic review examined the possible reduction in children’s and adolescents’ physical activity and changes in their BMI and weight status. Methods: A systematic review (PROSPERO: CRD42024589208) of English-language studies published up to 1 October 2024 in individuals with a mean age between 6 and 18 years that investigated physical activity data before and during or after the pandemic and focused on their BMI and weight status according to age, sex, and country making use of PubMed, Web of Science, and Scopus, identified 1040 possible articles. Results: Following the PRISMA statement, 26 articles with a whole set of 138,737 children and adolescents were enclosed in the review. The majority of included articles were of moderate quality, as determined by the Newcastle–Ottawa Scale adapted for observational studies. The studies found a decrease in PA, an increase in sedentary activities during/after the lockdown, and an increase in BMI and prevalence of overweight and obesity, especially in males and 8–11-year-olds. Conclusions: The interruption or restriction of outdoor physical activities and sports during the COVID-19 pandemic resulted in a more sedentary lifestyle among children and adolescents, contributing to an overall increase in BMI and obesity, with alarming implications for related health risks and other noncommunicable diseases. Therefore, the adverse effects of restrictive measures should be assessed when implementing public health strategies during pandemics.
1. Introduction
In the aftermath of the COVID-19 outbreak, most nations worldwide placed stringent restrictions on thwarting the spread of the infection. On 11 March 2020, the World Health Organization (WHO) proclaimed coronavirus 2019 (COVID-19) as an epidemic due to its fast diffusion worldwide.
Movement restrictions or lockdowns affected more than a third of the world’s population at the beginning of April 2020 [1]; China was the first nation to activate the lockdown in Wuhan as of 23 January 2020. Among the first European countries, Italy imposed a nationwide lockout starting 9 March 2020, where residents were ordered to stay at home; schools, sports facilities, restaurants, and stores (except grocery stores and pharmacies) were closed; there were travel restrictions; and isolation. Similar initiatives since followed elsewhere: over 100 nations implemented stringent measures to limit the transmission of the epidemic, awaiting the availability of vaccines and efficacious drugs [2].
As a result of the restrictions imposed during the epidemic [3], the daily routines of children and adolescents were disrupted, leading to changes in eating behaviors and sedentary lifestyles [4,5]. On the one hand, physical activity (PA) decreased due to the closure of schools, sports centers, and outdoor activities while sedentary and screen time increased [6]. Consequently, the WHO guidance for individuals aged 5–17 years to perform an average of 60 daily minutes spent in moderate to vigorous PA was disregarded during periods of isolation [7]. On the other hand, increased food intake including unhealthy food characterized this period, generally leading to increased body weight and health risks, as shown by studies conducted on adults, children, and adolescents [8,9,10].
Similarities between some of the referred changes (increased inactivity, school absence, etc.) and those that occur during the holiday season when there is a tendency for increased weight and adiposity can be pointed out [2,11,12]. However, there is no doubt that there were substantial differences between these periods from a psychological perspective: anxiety, depression, misbehavior, poor attention span, and impulsivity were observed in children, and especially adolescents during the epidemic, with a rising trend of mental health impact as the duration of isolation increased [13,14]. Conversely, summer vacations generally provide a chance for increased family interaction and beneficial recreational activities. However, this can also be a stressful time for low-income families, during which loneliness can hurt young people’s mental well-being [15]. Briefly, the extent of the restrictions applied during the epidemic and the rapidity of their application accentuated the critical situations already highlighted during the summer holidays, leading to a rapid weight gain that is difficult to shed [16,17].
Following the global health emergency brought about by the pandemic outbreak, there has been a collective effort to try to understand the biological, psychological, and sociological determinants of weight gain [18,19] because of the serious health risks caused by overweight/obesity. The obesity prevalence in childhood and adolescence has been increasing globally, reaching a plateau in most high-income countries around 2000 [20,21]. Recently, the COVID-19 pandemic has reportedly resulted in a weight gain in children and adolescents compared with the pre-pandemic rate as a result of lifestyle changes. Obesity during childhood tends to persist into adulthood. This condition is commonly combined with both psychosocial and cardio-metabolic comorbidities as well as early death [22,23].
Various determinants could have caused a gain of weight in children and adolescents over the course of the pandemic, and among them has emerged, in particular, the large reduction in PA. Sedentariness, measured as time spent on screen, is correlated with obesity risk factors in adolescents, and conversely, low sedentary and high PA levels are crucial for good health including weight status [24]. A recent review comparing the efficacy of several interventions on lifestyle for body composition in children showed that PA engagement is the most efficient tool in reducing the BMI, and the second most efficient in reducing the BMI z-score and body fat percentage [25]. In Europe, the decline in all kinds of PA recorded during the pandemic was greatest during periods when schools were closed [26]. The COVID-19 pandemic, with school closures, isolation, and the subsequent physical inactivity of children and adolescents, represents an unprecedented health crisis whose extent has yet to be fully understood.
Although a general increase in weight and obesity during the pandemic was detected in children and adolescents, further research is needed to fully understand the effect of lifestyle changes. Notably, the contribution of this review differs from that of several previous studies [27,28,29] in that it intends to systematically explore the literature focusing on a precise factor (PA) instead of generic unhealthy behaviors or eating habits [6,8,29]. Although the epidemic and subsequent restrictions affected almost all populations, some reviews only focused on specific geographic areas [26,30]. In addition, we selected the articles to be included regardless of the type of study design, unlike others (e.g., Anderson et al. [10] who only included longitudinal studies) focusing on changes in BMI and weight status, while most studies mainly considered weight gain [2,16,17], although only the ratio of weight to height (BMI) allows individuals to be categorized into different weight categories. The application of this anthropometric index is important, especially in growing subjects, because of the significant changes in stature with age. Finally, early reviews published on the topic [2,27,28], although essential in highlighting the early trends observed at the beginning of the pandemic, do not allow for an assessment of the possible evolution of the phenomenon throughout the pandemic period.
Taking the above into account as well as some inconsistent findings from the literature related to the COVID-19 outbreak [2,29,31,32], the main purpose of this review was to respond and provide up-to-date evidence to the following questions: What is known about the PA decline during the lockdown in response to the outbreak of COVID-19? What is known about changes in the BMI and weight status of children and adolescents? What is known about the possible trends of these traits with age, sex, and geographic area? Understanding these features is critical for targeting future interventions under similar isolation conditions in growing individuals.
2. Materials and Methods
Our systematic review was conducted following the PRISMA recommendations [33]. In the Supplementary Materials, we include Table S1 with the PRISMA 2020 checklist for abstracts and Table S2 with the PRISMA 2020 checklist. The review was registered in PROSPERO with the protocol CRD42024589208.
2.1. Search Strategy and Selection Process
We conducted a systematic search for articles in the PubMed, Web of Science, and Scopus electronic databases from 1 January 2020 to 1 October 2024 using the following string: (quarantine OR confinement OR lockdown OR lock-down OR isolation OR social-distancing) AND (“physical activity” OR “physical inactivity” OR exercise OR sedentar*) AND (covid* OR sars-cov-2 OR coronavirus OR pandemic) AND (child* OR schoolchildren OR adolescen* OR boys OR girls OR students) AND (“body mass index” OR BMI OR “weight status” OR underweight OR “normal weight” OR overweight OR obes*). We restricted the search outputs using publication date filters for the three databases and the age filters “child: 6–12 years” and “adolescent: 13–18 years” on PubMed.
A manual and independent review of potential articles for eligibility was performed by both authors (L.Z.; E.G.-R.) in two steps, on the basis of: (1) the title and abstract; (2) the full text. Specifically, after eliminating duplicates, the two authors, in line with the PRISMA guidelines, proceeded to independently examine the consistency of the articles with the inclusion and exclusion criteria reported below: the titles and abstracts of articles were screened for relevance and eligibility. The full text of the articles that passed this screening was examined, recording any reasons for exclusion. Any doubts or disagreements about the eligibility of the selected articles were cleared up by additional examination and discussion between the co-authors. At the end of the selection process, the bibliographies of the included articles were examined to check for any other articles not in the electronic databases considered.
2.2. Inclusion and Exclusion Criteria
Eligibility criteria were selected according to the PECO framework [34] considering the population, exposure, comparator, and outcomes. In this research, the population consisted of individuals aged 6 to 18 who suffered from being socially isolated during the COVID-19 outbreak with the resulting restrictions on sports and PA with no geographical limitation. The COVID-19 pandemic constituted the exposure. Comparisons were, firstly, trends between the pre-COVID and during/post-lockdown, and secondly, trends with age, sex, and geographical area. Primary outcomes concerned the effects of PA practice on body characteristics (BMI and/or weight status) over the periods considered. Secondary outcomes concerned the influences of age, sex, and population factors. In addition, only peer-reviewed, English-language articles, whose full text was available, were included.
The following exclusion criteria were applied: (i) mean sample age below 6 years or above 18 years; and (ii) lack of pre- and during/post-lockdown comparison data for PA (or sedentary activities) and BMI or weight status. We excluded studies that included the same sample or a sub-sample that had already been reported in another article. We also excluded qualitative studies, studies of clinical populations (including obese patients), non-English articles, literature reviews, editorials and commentaries, letters, abstracts, reports, case studies, books (or book chapters), protocol studies, and conference proceedings. The entire selection process and exclusion reasons are specified in the Results section using a PRISMA flowchart.
From each selected study, the two authors independently extracted the following information if available: the name of the first author and year of publication, study design, sampling period and country, study sample (size, sex, age), sample characteristics (changes in PA, BMI and/or weight status), and the main outcomes. We reported a qualitative summary of the data in the tables and listed the studies in alphabetical order.
2.3. Quality and Risk of Bias Assessment
Consistent with the PRISMA guidelines for systematic reviews [33], the two authors conducted an independent evaluation of all included investigations with the adapted Newcastle–Ottawa Scale (NOS) for observational studies [35,36].
This tool includes four main assessment criteria (study clearness; sample selection; comparability; outcome). Concerning the sample selection criteria, we assessed “Exposure assessment” regarding PA, while for “Assessment of the outcome”, we focused on the tools used in the body weight evaluation. Further adaptations of the NOS involved the “Clearness of the aim”, in which we decided to assign a score of 2 to the accuracy and relevance of the question in light of the available literature when the number of citations was ≥10, and 1 when it was <10. We also maintained a score equal to 0 on the NOS-adapted scale for the third item in sample selection relative to the non-respondents category when “One or none of three” of the possible conditions were fulfilled, as already undertaken in previous reviews [37,38]. Finally, regarding the “Comparability of individuals from different groups based on study design or analysis”, we assigned a score of 1 when the sex composition of the sample was the same, or in any case, did not differ more than 10%.
We calculated each study’s overall score (range: 0–16) by summing the ratings of each component. We rated studies with scores of 13–16 points as high quality and low bias risk (scores > 75%), studies with 9–12 point scores as of moderate quality and risk (scores > 50%), and studies with ≤8 point score (scores ≤ 50%) low quality and high risk [36]. To ensure transparency, no study was dropped from this review due to the results of this assessment. Again, any discordant ratings between the two authors were addressed through discussion.
3. Results
3.1. Study Selection
The search across the three databases (Web of Science, Scopus, and PubMed) identified 1040 records. After removing 433 duplicates, we screened the titles and abstracts of the remaining 607 articles and excluded 420 non-relevant articles. We then screened the full text of the 187 articles and excluded 165, identifying 22 articles that met the inclusion criteria. The screening of the quotations from the 22 selected articles led to the inclusion of four additional articles, so in this systematic review we considered 26 articles. Figure 1 displays the flow diagram of the whole selection process of the study.
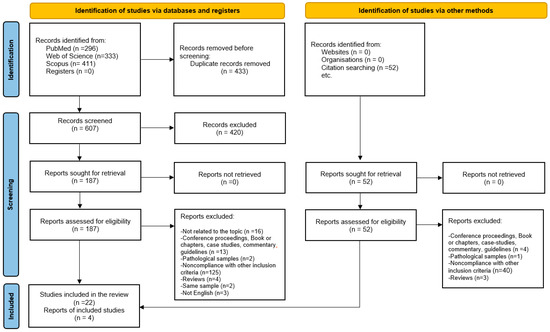
Figure 1.
Flowchart of the study selection process (PRISMA 2020 flow diagram).
3.2. Study Characteristics
Table 1 and Table 2 synthesize the characteristics of the enclosed papers about PA change and BMI/weight status change caused by lockdown in children and adolescents.

Table 1.
Characteristics of the included studies (in alphabetical order).

Table 2.
Outcomes of the included studies.
Half of the articles were published in 2022, seven in 2021, four in 2024, and one each in 2020 and 2023. These studies were performed in nineteen different nations: thirteen studies were performed in Europe (including four in Italy, two in Germany, and one each in England, Croatia, Spain, the Netherlands, Ukraine, the Czech Republic, and Poland), Eleven studies in Asia (including four in China and one each in Jordan, Saudi Arabia, Qatar, Iran, South Korea, Singapore, and India), one in South America (Argentina), and one in North Africa (Algeria).
Seven studies (27%) used a longitudinal design [43,45,47,51,54,60,63], two studies (8%) used both a longitudinal and a cross-sectional design [42,59], and the majority (the remaining seventeen studies equal to 65%) used a cross-sectional design. When the sample was observed more than once, the first time was before the COVID-19 emergence, usually in the period October 2019–March 2020, [42,43,45,47,51,54], and the second time was during the pandemic one year later [42,43,45,51] or before, in June–July 2020 [47,54]. Azrak et al. [42] and Palmieri et al. [51] carried out a third data collection another year later in September–November 2021.
The participants in these studies were healthy children and/or adolescents of both sexes, mostly primary, secondary, or high school students. The smallest sample size was 50 Spanish students from a primary school in Cantabria (Spain) [54], and the largest was 112,251 Korean students from 800 secondary and high schools [52]. Specifically, regarding the number of subjects studied, four studies (15%) had a sample size of less than 100, twelve studies (46%) had a sample size between 101 and 1000, nine studies (34.6%) had a sample size between 1001 and 10,000, and only one study (4%) had more than 10,000 subjects. Regarding the age of the subjects, six studies (23.1%) considered children under the age of 10, twelve studies (46.2%) included the age range 10–15, two studies included adolescents over the age of 15, and six studies (23.1%) included subjects in the full age range of 6–18.
3.3. Analysis of Physical Activity
PA was measured objectively in only a few studies, using an activity monitor (accelerometer Actigraph wGT3X-BT delivered to the doorstep or delivered to the school) [56,59] or through personal devices (smartwatch or smartphones) reporting the daily number of steps [57]. In most studies, the amount of PA of the children and adolescents during the lockdown was assessed subjectively, self-reported, or reported by parents using validated questionnaires (GPAQ [64], PAQ-C [55,57], Baecke [59], or IPAQ long form [62]) or by answering simple questions (like “Did you do any PA before lockdown? and “Did you do any PA during lockdown?”) [51], the mean time spent in sports clubs [43], the proportion of subjects that never engaged in PA during weekdays [41], the proportion of subjects practicing PA on a determined number of days per week [39], MVPA ≥ 60 min per day on all 7 days, and the number of days in the last week with MVPA ≥ 60 min [50]). PA was assessed both objectively using an Actigraph accelerometer and subjectively using the PAQ-C questionnaire in two studies [45,60]. Regardless of the method used to assess PA, all studies found a decrease in PA in children and adolescents during or after the lockdown, and when considered, an increase in sedentary time and a lower proportion of subjects meeting the WHO recommended minimum of 60 min per day of moderate-to-vigorous physical activity (MVPA) in the students under lockdown or studying at a distance [64].
Specifically, Abed Alah et al. [39] found a significant 20% decrease in the proportion of Qatari children and adolescents who engaged in regular sports before and during COVID-19, and that 35% fewer students engaged in PA 2–4 days per week and 37% more engaged in PA once or less per week. Al-Agha et al. [41] found a 20% increase in males and a 16% increase in females in the percentage of Saudi subjects who never engaged in PA activities during COVID-19 compared with before. In He et al. [47], Chinese children decreased their daily PA by 7.3 min (equivalent to 8%) and increased their screen time by 15 min (equivalent to 17.6%). In Europe, Croatian students [48] with low PA levels increased by 57%; Spanish students who did not engage in any PA increased by 28% [54]; 75% of German students reduced their participation in sports and 55.8% increased their sedentary behavior [55]; 44% of another German sample [61] reduced their PA (especially the min 10–12 age group by 57%); 62% of Dutch students reduced their PA during lockdown; almost 15% of English children stopped participating in a sports club [43]; in Italian students [45], the MVPA decreased by 19.5 min per day in boys and 8.3 min per day in girls: as a result, the prevalence of boys not meeting the recommended levels of PA increased by 41% and that of the girls by 14%.
3.4. Analysis of BMI/Weight Status
The methods used to assess the BMI were the direct measurement of weight and stature by expert personnel [43,47,48,51,54,55,58,59,60,63] or the retrieval of data from electronic health record systems (especially for the pre-COVID-19 data) [39,41,42] or from school records [49] or online questionnaires with self-reported data on weight and stature from which the BMI was calculated [40,44,52,53,57,62,64]. The BMI values were either expressed in raw kg/m2 or transformed into BMI-for-age Z-score and then used to establish the weight status by classifying subjects as underweight, normal weight, overweight, or obese on the basis of age- and sex-specific BMI thresholds. In some studies, weight status was asked and then self-reported by the parents or the subjects themselves [46,61]. Regardless of the method of BMI/weight status assessment, all studies observed increased BMI values and the prevalence of overweight/obese subjects. In particular, the zBMI change ranged from 0.07 in Chinese children [56] to 0.9 in Iranian adolescents [49], while the BMI change ranged from 0.1 kg/m2 in the Chinese sample [47] to 1.5 kg/m2 in English children [43] and Singaporean children [58]. When the change was considered according to sex and age, it was usually greater in males and the 8–11 year age group or in the youngest age group considered [39,47,49,52]. Unlike the general trend, Łuszczki et al. [50] found a lower (−0.32 kg/m2), although not significant, BMI (with a halving of the percentage of obese subjects from 11.5% to 6.4% and an increase in underweight subjects (+3.3%)), despite lower PA during the pandemic than before: anthropometric data before the pandemic were directly measured but during the pandemic were self-declared by the parents or themselves. Similarly, Štveráková et al. [57] found a decrease in BMI (−0.57 kg/m2) despite reduced PA (−0.38 in PAQ-C score): even in this study, the anthropometric data were directly measured before COVID and self-reported during the COVID pandemic.
The perception of the weight status of their child by Italian parents in the study by Farello et al. [46] was also in agreement with what has already been established about directly collected data: they observed a higher number of reports post-lockdown of overweight (+5.7% in the 5–11 age group and +0.8% in the 12–18 age group) and obesity (+0.6% in the 5–11 age group and +0.7% in the 12–18 age group) as well as a lower number of reports of normal weight or underweight after the closure.
To look for possible predictors of changes in the BMI or BAZ scores over the period of COVID-19-related school closures, the authors of some of the papers included in this review performed different statistical analyses (univariate linear regression, multivariate linear regression, or logistic regression) using different independent and dependent variables. The linear regression performed by Abed Alah et al. [39] showed that the PA reduction while schools were closed was a significant predictor of the increase in BAZ scores in different sexes and age groups. In the study of Kenđel Jovanović et al. [48], the odds of overweight and obesity before lockdown were significantly lower for the ones with moderate PA than for the ones with low PA (OR = 0.71; p = 0.016). Those who played organized sports between two and three times per week were less likely to be overweight and obese than those who committed to less than two times a week (OR = 0.59; p = 0.001). During the lockdown, the odds for overweight and obesity increased almost twofold (OR = 0.23, OR = 0.36; both p < 0.001) for those engaged in organized sports more than two days a week than those who played sports less than two days a week. Generalized estimating equation analysis performed by Yang et al. [63] reported that the teen students involved in MVPA for at least 60 min per day for all seven days were less likely to have obesity. In addition, boys with ≥2 h of computer time per day and girls with ≥2 h of mobile screen time per day or ≥2 h of TV time per day were more likely to have obesity. Similar results were found by He et al. [47] in their generalized model showing that less daily PA and more screen time were positively related to obesity.
3.5. Risk of Bias
The range of NOS scores of the included articles was from 6 to 14 points: the lowest score was 6 in the longitudinal study on Spanish students [54], and the highest score of 14 was obtained by two longitudinal studies, one on Indian students [60] and one on Chinese students in Shanghai [63]. Most studies (65.4%) were of moderate quality, 23.1% were of low quality, and 11.5% were of high quality. The highest scores were obtained in the items: clarity of the stated aim, assessment of the outcome, and statistical tests (no study obtained a score of 0); the lowest scores were obtained in the items “non-respondents” (20 studies obtained a score of 0) and “control of confounding factors” (Table 3).

Table 3.
Quality assessment of the included studies by the Newcastle–Ottawa scale (NOS) with a relative range for each item. Higher scores indicate better quality research.
4. Discussion
In this review, we examined the impact of the restrictions imposed during the COVID-19 pandemic, such as the lockdown, which disrupted daily routines by suspending school attendance and physical activities including outdoor activities and sports, increased screen time, and home confinement [5,65]. The same sleep–wake rhythm and eating habits, with large use of comfort food, also changed during this period [6,66]. As a result of the restrictive measures implemented by most countries around the world, on 7 April 2020, 3.9 billion people, over one-half of the population of the world, were in lockdown [67].
Our results suggest that the COVID-19 pandemic, characterized by drastic measures of social estrangement and confinement, significantly affected the practice of PA and the weight status and BMI of children and adolescents.
In particular, through this systematic review, we reported data regarding a total of 138,737 individuals with an average age between 6 and 18 years, distributed across 19 countries from 4 continents worldwide (Algeria, Argentina, China, Croatia, Czech Republic, England, Germany, India, Iran, Italy, Jordan, Qatar, Poland, Saudi Arabia, Singapore, South Korea, Spain, the Netherlands, Ukraine).
The practice of PA is essential for children and adolescents to develop social relationships and reduce the risk of psychological, social, and physical issues [18,68]. In this period of growth, characterized by physical and mental fragility, the abrupt interruption of social contacts and life habits imposed during the epidemic period by the lockdown, with the suspension of PA among other things, seems to have affected physical and mental health. According to this review, the highest percentage decrease in PA was observed in children from Europe (Italy and Spain), the highest overweight/obesity prevalence in Qatar and Argentina, and the highest increase in BMI according to z-BMI in the Middle East (Jordan, Qatar, Iran), in addition to England and Singapore (BMI values). Notably, some Eastern European countries (Ukraine and Poland) showed no change or increase in BMI after the pandemic. These trends may depend on the sample composition examined (changes were greater in children/pre-adolescents than in adolescents and males than in females) and on the spread and severity of the infection with consequent differences in the restrictions imposed by governments. Thus, China was the first to impose a strict lockdown on 60 million people in Hubei Province starting in January 2020, followed in March 2020 by Italy with 67 days of lockdown [69]; the longest lockdown period in 2020 with 234 days was implemented in Argentina [70], unlike some countries where this strategy was never implemented (e.g., Sweden among European countries). Specifically, in Sweden, where mild restrictions were implemented, Helgadóttir et al. found, in an accelerometer-based study on a large sample of Swedish adolescents, that the MVPA remained generally stable (even increased significantly by 4 min during weekdays) while the light PA and sedentary time changed unfavorably, especially in girls and overweight/obese subjects [71].
4.1. Physical Activity During the Lockdown
Although it is generally believed that PA is practiced inadequately compared with general indications [7], a further negative trend in PA practice was observed from childhood to adolescence during the epidemic. Therefore, this decrease in PA is worrisome for child and adolescent health: the reduction in the practice of PA, already deemed inadequate according to the WHO recommendations for 5- to 17-year-old children/adolescents, can lead to repercussions on the short-term, medium-term, and long-term physical and cognitive development, with a tendency to weight gain, cardio-metabolic, and psychological problems [72]. This review showed that the decrease in PA during lockdown was larger in children/pre-adolescents and the male sex. Adolescents are generally more prone to sedentariness than children because of different age-typical interests, which in the lockdown period manifested in more screen time devoted to the Internet and gaming [73]. As for sex, it is well-known that girls usually engage for fewer hours than boys in PA during the week and on weekends [72,74,75]. Therefore, the further decrease due to the pandemic in the amount of time devoted to PA practice by girls is worrying. The female sex is less physically active than the male sex throughout their life span, through childhood, adolescence, and adulthood [76]. Girls face greater barriers than boys in participating in sports: their cultural background, dissatisfaction with their physical appearance, and athletic ability are some of the possible causes [77]. During the lockdown, screen time increased, contravening the WHO recommendation of a maximum of 2 h per day for children and adolescents [7,72]. Intensive Internet use on cell phones and video games is linked to increased BMI values and overweight in adolescents [78], and Internet addiction is more pronounced in females than in males [73]. The concept that practicing PA increases health benefits and decreases the risk of problematic Internet use [79] is particularly valid in the case of confinement as during the recent pandemic [80]. In general, Internet use is positively linked to an increased probability of overweight and obesity [81].
4.2. BMI/Weight Status During the Lockdown
The increase in the BMI mean values and overweight/obese prevalence was mainly achieved in children/pre-adolescents and the male sex, as reported above. The increase in BMI and weight status is generally justified in the literature by the restrictions imposed during the outbreak of COVID-19 (among others: [10,82,83]). Schools were shut down during the COVID-19 pandemic, and most scholastic and extracurricular physical activities and sports were suspended. While a regular practice of PA, in an indoor or outdoor space sufficient, may help to reduce depression and anxiety development due to epidemic stress [18,84]), it would have been crucial in controlling weight gain caused by a sedentary lifestyle and jungle food use during the confinement period, especially at the ages considered. According to a previous review [66], the greater influence of lockdown on weight gain in pediatric age compared with adulthood must be highlighted. Regarding weight status, a particular rise in overweight prevalence was observed, while obesity tended to remain stable. This trend is probably related to the greater sedentary behavior of the obese even before the lockdown, which therefore did not particularly affect them from this point of view. The weight gains observed during the epidemic period are believed to be similar to those resulting from physical inactivity during summer vacation [2,12]. However, some apparent differences should be pointed out: the stay-at-home period during the epidemic was coercively imposed on the entire population and has resulted in mental health effects (anxiety, depression) related to both losses of individual freedom of movement and socialization, and concern about getting sick that affected the behavior from sedentary to emotional eating (snacks and sweets are considered the most common forms of psychological compensation) [85]. Future studies may help verify whether the bad habits acquired during the confinement period, where, unlike holiday-related effects, the lockdown period could have long-lasting physical and mental health effects: recent European studies seem to indicate maintenance in the post-COVID period of negative effects on the BMI and weight status despite the resumption of the practice of PA [55,83,86].
4.3. Strengths and Limitations
The main strengths of this review are as follows: adherence to the PRISMA statement; an accurate literature search through a specific string aimed at identifying as many relevant articles as possible, complemented by the final search on the bibliographies of the selected articles; an independent evaluation of the eligibility, selection process, and data extraction for the study by the two authors; and a quality evaluation of all studies involved. Assessment of the appropriateness of the inclusion/exclusion of studies in the review was also carried out through direct contact with the authors to avoid overlapping sampling.
This review had some weaknesses. We first limited ourselves to examining the increase in BMI and weight status during lockdown, assuming that it depended on decreased PA. However, numerous factors may have played a role in this trend, but the analysis of other factors was beyond the scope of the study. Furthermore, our review showed that studies on PA and BMI conducted in different populations obtained concordant results.
The studies were performed at different epidemic and pre-epidemic times. The extent of restrictions applied in various nations worldwide, such as the length of the lockdown, was not necessarily the same, depending on the policies adopted and the severity of the epidemic. In addition, a further limitation came from the studies’ heterogeneity not only in the size of the sample, gender, and ethnic group but also in the variables analyzed (from the frequency in PA practice to the measurement of precise parameters with the accelerometer) and methods (direct measurements vs. interviews; direct participant analysis vs. parental interview). Enhancing the heterogeneity, most studies used a cross-sectional design, but nine included studies were conducted with longitudinal or mixed designs, resulting in possible different levels of reliability of the results obtained. However, the trend of the examined characters was the same regardless of the study design employed. In addition, other methodological differences consisted of using reliable medical databases in retrospective studies, while others employed self-reported data, resulting in an increased risk of bias. Even BMI, sometimes based on direct measures of weight and height, and others on participant- or parent-reported data, is referred to as kg/m2 values or z-scores. Moreover, the resulting weight status was categorized according to thresholds in the WHO growth curve for children or Cole cut-off values. Concerning the percentiles, the reference for underweight was, according to different studies, a BMI ≤ 2, ≤5, or ≤10 percentile, for overweight ≥85 or ≥90 percentile, and for obesity ≥95 or ≥97 percentile. Comparisons between the resulting frequencies must therefore be made with extreme caution. Finally, the statistical parameters related to the association between PA and BMI, even when present among the same variables, differed, ranging from the Pearson’s r coefficient to odds ratios up to multiple linear regression between an independent variable (generally BMI or z-BMI) and two or more dependent variables. The generality of the selected articles did not consider potential confounders in their analyses. Further limitations of this study can stem from the limitations of the studies reviewed. Precisely because of the heterogeneity of the examined studies, we could not undertake a meta-analysis and merely reported the results with a narrative synthesis. Finally, only articles in English were included in our review excluding articles published in other languages.
5. Conclusions
Our study showed that a reduction in PA and an increasing BMI and weight status consistently characterized children and adolescents undergoing lockdown in different countries. Although a growing trend of overweight/obesity is evident in the world, the COVID-19 epidemic seems to have worsened the situation with particular reference to children. In the case of an epidemic, policymakers, educators, and health professionals should carefully evaluate the negative impact of restrictions and social isolation on children and adolescents, developing effective strategies to promote healthy development and growth.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/children12020178/s1, Table S1: PRISMA 2020 for abstract checklist; Table S2: PRISMA 2020 checklist. References [87] is cited in the supplementary materials
Author Contributions
Conceptualization, E.G.-R. and L.Z.; Methodology, E.G.-R. and L.Z.; Formal analysis, L.Z.; Investigation, E.G.-R. and L.Z.; Data curation, E.G.-R. and L.Z.; Writing—original draft preparation, E.G.-R. and L.Z.; Writing—review and editing, E.G.-R. and L.Z.; Supervision, E.G.-R.; Project administration, E.G.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Koh, D. COVID-19 lockdowns throughout the world. Occup. Med. 2020, 70, 322. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Chourdakis, M. Impact of the first COVID-19 lockdown on body weight: A combined systematic review and a meta-analysis. Clin. Nutr. 2022, 41, 3046–3054. [Google Scholar] [CrossRef] [PubMed]
- Girum, T.; Lentiro, K.; Geremew, M.; Migora, B.; Shewamare, S.; Shimbre, M.S. Optimal strategies for COVID-19 prevention from global evidence achieved through social distancing, stay at home, travel restriction and lockdown: A systematic review. Arch. Public Health 2021, 79, 150. [Google Scholar] [CrossRef] [PubMed]
- An, R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: A microsimulation model. J. Sport Health Sci. 2020, 9, 302–312. [Google Scholar] [CrossRef]
- Zaccagni, L.; De Luca, F.; Rinaldo, N.; Mazzoni, G.; Mandini, S.; Gualdi-Russo, E. The COVID-19 Experience in Adolescents: Emotional and Behavioral Recall at the End of the Pandemic. Diseases 2024, 12, 116. [Google Scholar] [CrossRef]
- Bates, L.C.; Zieff, G.; Stanford, K.; Moore, J.B.; Kerr, Z.Y.; Hanson, E.D.; Gibbs, B.B.; Kline, C.E.; Stoner, L. COVID-19 Impact on Behaviors across the 24-Hour Day in Children and Adolescents: Physical Activity, Sedentary Behavior, and Sleep. Children 2020, 7, 138. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Cinelli, G.; Bigioni, G.; Soldati, L.; Attinà, A.; Bianco, F.F.; Caparello, G.; Camodeca, V.; Carrano, E.; et al. Psychological Aspects and Eating Habits during COVID-19 Home Confinement: Results of EHLC-COVID-19 Italian Online Survey. Nutrients 2020, 12, 2152. [Google Scholar] [CrossRef] [PubMed]
- Zaccagni, L.; Rinaldo, N.; Mazzoni, G.; Mandini, S.; Masotti, S.; Toselli, S.; De Luca, F.; Gualdi-Russo, E. Assessing the Impact of COVID-19 Prevention Measures on Adolescent Growth in Italy. Healthcare 2023, 11, 2101. [Google Scholar] [CrossRef]
- Anderson, L.N.; Yoshida-Montezuma, Y.; Dewart, N.; Jalil, E.; Khattar, J.; De Rubeis, V.; Carsley, S.; Griffith, L.E.; Mbuagbaw, L. Obesity and weight change during the COVID-19 pandemic in children and adults: A systematic review and meta-analysis. Obes. Rev. 2023, 24, e13550. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Zavala, R.G.; Castro-Cantú, M.F.; Valencia, M.E.; Álvarez-Hernández, G.; Haby, M.M.; Esparza-Romero, J. Effect of the Holiday Season on Weight Gain: A Narrative Review. J. Obes. 2017, 2017, 2085136. [Google Scholar] [CrossRef]
- Eglitis, E.; Miatke, A.; Virgara, R.; Machell, A.; Olds, T.; Richardson, M.; Maher, C. Children’s Health, Wellbeing and Academic Outcomes over the Summer Holidays: A Scoping Review. Children 2024, 11, 287. [Google Scholar] [CrossRef] [PubMed]
- Meade, J. Mental Health Effects of the COVID-19 Pandemic on Children and Adolescents: A Review of the Current Research. Pediatr. Clin. N. Am. 2021, 6, 945–959. [Google Scholar] [CrossRef] [PubMed]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef]
- Morgan, K.; Melendez-Torres, G.J.; Bond, A.; Hawkins, J.; Hewitt, G.; Murphy, S.; Moore, G. Socio-Economic Inequalities in Adolescent Summer Holiday Experiences, and Mental Wellbeing on Return to School: Analysis of the School Health Research Network/Health Behaviour in School-Aged Children Survey in Wales. Int. J. Environ. Res. Public Health 2019, 16, 1107. [Google Scholar] [CrossRef] [PubMed]
- Rundle, A.G.; Park, Y.; Herbstman, J.B.; Kinsey, E.W.; Wang, Y.C. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity 2020, 28, 1008–1009. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Menon, P.; Govender, R.; Abu Samra, A.M.; Allaham, K.K.; Nauman, J.; Östlundh, L.; Mustafa, H.; Smith, J.E.M.; AlKaabi, J.M. Systematic review of the effects of pandemic confinements on body weight and their determinants. Br. J. Nutr. 2022, 127, 298–317. [Google Scholar] [CrossRef]
- Zhong, B.; Sun, H.; Wang, G.; Junwen, S.; Tang, S.; Gao, Y.; Chen, H.; Lu, T.; Yan, J. Physical activity on the mental health of children and adolescents during COVID-19 pandemic-induced school closures—A systematic review. PLoS ONE 2024, 19, e0299158. [Google Scholar] [CrossRef] [PubMed]
- Ramalho, S.; Martins-Mendes, D.; Macedo, J.M.; Barros, C.; Luis, C.; Sá, S.; Gestoso, Á.; Pereira, A.C.; Baylina, P.; Fernandes, R. Unveiling the Path to Resilience: Prioritizing Mental Health, Sleep, and Nutrition in the Post-COVID Era. Healthcare 2023, 11, 2463. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef]
- Horesh, A.; Tsur, A.M.; Bardugo, A.; Twig, G. Adolescent and childhood obesity and excess morbidity and mortality in young adulthood—A systematic review. Curr. Obes. Rep. 2021, 10, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Jebeile, H.; Kelly, A.S.; O’Malley, G.; Baur, L.A. Obesity in children and adolescents: Epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef] [PubMed]
- De Craemer, M.; Cardon, G.; Decraene, M.; Androutsos, O.; Moreno, L.; Iotova, V.; Koletzko, B.; Socha, P.; Manios, Y.; Verbestel, V. Longitudinal changes in preschoolers’ adiposity indicators according to compliance with 24-hour movement behavior guidelines: Results from the ToyBox-study. BMC Public Health 2024, 24, 3115. [Google Scholar] [CrossRef] [PubMed]
- Su, X.; Hassan, M.A.; Kim, H.; Gao, Z. Comparative effectiveness of lifestyle interventions on children’s body composition management: A systematic review and network meta-analysis. J. Sport Health Sci. 2024, 14, 101008. [Google Scholar] [CrossRef] [PubMed]
- Ludwig-Walz, H.; Siemens, W.; Heinisch, S.; Dannheim, I.; Loss, J.; Bujard, M. How the COVID-19 pandemic and related school closures reduce physical activity among children and adolescents in the WHO European Region: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 149. [Google Scholar] [CrossRef]
- Rossi, L.; Behme, N.; Breuer, C. Physical Activity of Children and Adolescents during the COVID-19 Pandemic—A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11440. [Google Scholar] [CrossRef] [PubMed]
- Yomoda, K.; Kurita, S. Influence of social distancing during the COVID-19 pandemic on physical activity in children: A scoping review of the literature. J. Exerc. Sci. Fit. 2021, 19, 195–203. [Google Scholar] [CrossRef]
- Cena, H.; Fiechtner, L.; Vincenti, A.; Magenes, V.C.; De Giuseppe, R.; Manuelli, M.; Zuccotti, G.V.; Calcaterra, V. COVID-19 Pandemic as Risk Factors for Excessive Weight Gain in Pediatrics: The Role of Changes in Nutrition Behavior. A Narrative Review. Nutrients 2021, 13, 4255. [Google Scholar] [CrossRef] [PubMed]
- Shobako, N. Lessons from the health policies for children during the pandemic in Japan. Front. Public Health 2022, 10, 1015955. [Google Scholar] [CrossRef]
- Tai, D.B.G.; Shah, A.; Doubeni, C.A.; Sia, I.G.; Wieland, M.L. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clin. Infect. Dis. 2021, 72, 703–706. [Google Scholar] [CrossRef]
- Faienza, M.F.; Colaianni, V.; Di Ciaula, A.; Bonfrate, L.; Urbano, F.; Chiarito, M.; Brunetti, G.; Giordano, P.; Corbo, F.; D’Amato, G.; et al. Different Variation of Intra-familial Body Mass Index subjected to COVID-19 Lockdown. J. Gastrointest. Liver Dis. 2022, 31, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Morgan, R.L.; Whaley, P.; Thayer, K.A.; Schunemann, H.J. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ. Int. 2018, 121, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.; Shea, B.; O’Connell, D.; Robertson, J.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Eur. J. Epidemiol. 2000, 25, 603–605. [Google Scholar]
- Hillen, M.A.; Medendorp, N.M.; Daams, J.G.; Smets, E.M.A. Patient-Driven Second Opinions in Oncology: A Systematic Review. Oncologist 2017, 22, 1197–1211. [Google Scholar] [CrossRef] [PubMed]
- Zaccagni, L.; Gualdi-Russo, E. The Impact of Sports Involvement on Body Image Perception and Ideals: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 5228. [Google Scholar] [CrossRef] [PubMed]
- Gualdi-Russo, E.; Zaccagni, L. COVID-19 Vaccination and Predictive Factors in Immigrants to Europe: A Systematic Review and Meta-Analysis. Vaccines 2024, 12, 350. [Google Scholar] [CrossRef] [PubMed]
- Abed Alah, M.; Abdeen, S.; Bougmiza, I.; Selim, N. COVID-19 lockdowns weigh heavily on youth: An analysis of the impact on BMI for Age Z scores in children and adolescents. J. Public Health 2024, 46, 209–222. [Google Scholar] [CrossRef] [PubMed]
- Al Hourani, H.; Alkhatib, B.; Abdullah, M. Impact of COVID-19 Lockdown on Body Weight, Eating Habits, and Physical Activity of Jordanian Children and Adolescents. Disaster Med. Public Health Prep. 2022, 16, 1855–1863. [Google Scholar] [CrossRef]
- Al-Agha, A.; Alsalmi, R.; Alahmadi, B.; Aljilani, T.; Alasbli, S.; Alsharef, F.; Baothman, G.; Maddah, J. Impact of Virtual Education Versus Traditional Learning Modalities on the Body Mass Index of Students During the COVID-19 Pandemic in Western Saudi Arabia: A Cross-Sectional Study. Cureus 2022, 14, e22596. [Google Scholar] [CrossRef] [PubMed]
- Azrak, M.Á.; Fasano, M.V.; Avico, A.J.; Sala, M.; Casado, C.; Padula, M.; Kruger, A.L.; Malpeli, A.; Andreoli, M.F. Prolonged body weight gain, lifestyle changes and health-related quality of life in children during the COVID-19 pandemic lockdown: A follow-up study. Eur. J. Clin. Nutr. 2023, 77, 460–467. [Google Scholar] [CrossRef]
- Basterfield, L.; Burn, N.L.; Galna, B.; Batten, H.; Goffe, L.; Karoblyte, G.; Lawn, M.; Weston, K.L. Changes in children’s physical fitness, BMI and health-related quality of life after the first 2020 COVID-19 lockdown in England: A longitudinal study. J. Sports Sci. 2022, 40, 1088–1096. [Google Scholar] [CrossRef]
- Benmerzoug, M.; Djoudi, B.; Debbache, A.; Harbouche, A.; Dehmani, I.D.; Djekkoun, N.; Abdelkader, R.; Vitiello, D.; Leila, R. Impact of COVID-19 Lockdown on Children’s Health in North Africa. Matern. Child Health J. 2022, 26, 1701–1708. [Google Scholar] [CrossRef]
- Dallolio, L.; Marini, S.; Masini, A.; Toselli, S.; Stagni, R.; Bisi, M.C.; Gori, D.; Tessari, A.; Sansavini, A.; Lanari, M.; et al. The impact of COVID-19 on physical activity behaviour in Italian primary school children: A comparison before and during pandemic considering gender differences. BMC Public Health 2022, 22, 52. [Google Scholar] [CrossRef]
- Farello, G.; D’Andrea, M.; Quarta, A.; Grossi, A.; Pompili, D.; Altobelli, E.; Stagi, S.; Balsano, C. Children and Adolescents Dietary Habits and Lifestyle Changes during COVID-19 Lockdown in Italy. Nutrients 2022, 14, 2135. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Luo, B.; Zhao, L.; Liao, S. Influences of the COVID-19 Pandemic on Obesity and Weight-Related Behaviors among Chinese Children: A Multi-Center Longitudinal Study. Nutrients 2022, 14, 3744. [Google Scholar] [CrossRef] [PubMed]
- Kenđel Jovanović, G.; Dragaš Zubalj, N.; Klobučar Majanović, S.; Rahelić, D.; Rahelić, V.; Vučak Lončar, J.; Pavičić Žeželj, S. The Outcome of COVID-19 Lockdown on Changes in Body Mass Index and Lifestyle among Croatian Schoolchildren: A Cross-Sectional Study. Nutrients 2021, 13, 3788. [Google Scholar] [CrossRef] [PubMed]
- Khamesan, B.; Khatibzade-Nasari, N.; Zare, S.; Rostami-Gooran, N.; Baghestani-Koozehgar, R. Long-term effects of the COVID-19 lockdown on weight status, eating habits, and lifestyle changes related to school-aged children in Bandar Abbas, Iran. BMC Public Health 2024, 24, 1981. [Google Scholar] [CrossRef]
- Łuszczki, E.; Bartosiewicz, A.; Pezdan-Śliż, I.; Kuchciak, M.; Jagielski, P.; Oleksy, Ł.; Stolarczyk, A.; Dereń, K. Children’s Eating Habits, Physical Activity, Sleep, and Media Usage before and during COVID-19 Pandemic in Poland. Nutrients 2021, 13, 2447. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Vecchiato, M.; Pennella, S.; Marasca, A.; Spinelli, A.; De Luca, M.; De Martino, L.; Fernando, F.; Sirico, F.; Biffi, A. The Impact of the COVID-19 Pandemic on Childhood Obesity and Lifestyle—A Report from Italy. Pediatr. Rep. 2022, 14, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Park, H.K.; Lim, J.S. Change of obesity prevalence and lifestyle patterns before and during COVID-19 among Korean adolescents. Ann. Pediatr. Endocrinol. Metab. 2022, 27, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Pujia, R.; Ferro, Y.; Maurotti, S.; Khoory, J.; Gazzaruso, C.; Pujia, A.; Montalcini, T.; Mazza, E. The Effects of COVID-19 on the Eating Habits of Children and Adolescents in Italy: A Pilot Survey Study. Nutrients 2021, 13, 2641. [Google Scholar] [CrossRef]
- Ramos-Álvarez, O.; Arufe-Giráldez, V.; Cantarero-Prieto, D.; Ibáñez-García, A. Impact of SARS-CoV-2 Lockdown on Anthropometric Parameters in Children 11/12 Years Old. Nutrients 2021, 13, 4174. [Google Scholar] [CrossRef] [PubMed]
- Samigullin, A.; Groß, G.; Gählert, J.; Buchenberger, S.; Morcos, M.; Schwertz, R.; Öste, R.; Siegel, E.; Humpert, P. Impact of COVID-19 lockdowns on the anthropometric development in primary school children in the Rhein-Neckar Region, Germany. BMC Nutr. 2024, 10, 78. [Google Scholar] [CrossRef]
- So, H.K.; Chua, G.T.; Yip, K.M.; Tung, K.T.S.; Wong, R.S.; Louie, L.H.T.; Tso, W.W.Y.; Wong, I.C.K.; Yam, J.C.; Kwan, M.Y.W.; et al. Impact of COVID-19 Pandemic on School-Aged Children’s Physical Activity, Screen Time, and Sleep in Hong Kong: A Cross-Sectional Repeated Measures Study. Int. J. Environ. Res. Public Health 2022, 19, 10539. [Google Scholar] [CrossRef] [PubMed]
- Štveráková, T.; Jačisko, J.; Busch, A.; Šafářová, M.; Kolář, P.; Kobesová, A. The impact of COVID-19 on Physical Activity of Czech children. PLoS ONE 2021, 16, e0254244. [Google Scholar] [CrossRef] [PubMed]
- Sum, K.K.; Cai, S.; Law, E.; Cheon, B.; Tan, G.; Loo, E.; Lee, Y.S.; Yap, F.; Chan, J.K.Y.; Daniel, M.; et al. COVID-19-Related Life Experiences, Outdoor Play, and Long-term Adiposity Changes Among Preschool- and School-Aged Children in Singapore 1 Year After Lockdown. JAMA Pediatr. 2022, 176, 280–289. [Google Scholar] [CrossRef]
- Ten Velde, G.; Lubrecht, J.; Arayess, L.; van Loo, C.; Hesselink, M.; Reijnders, D.; Vreugdenhil, A. Physical activity behaviour and screen time in Dutch children during the COVID-19 pandemic: Pre-, during- and post-school closures. Pediatr. Obes. 2021, 16, e12779. [Google Scholar] [CrossRef]
- Thapar, S.; Thakur, J.S.; Schayck, O.C.v.; Willeboordse, M.; Winkens, B.; Vreugdenhil, A. Physical Activity of School-Going Adolescents During the COVID-19 Pandemic: A Natural Experiment Study. Indian Pediatr. 2024, 61, 441–446. [Google Scholar] [CrossRef]
- Weihrauch-Blüher, S.; Huizinga, O.; Joisten, C.; Pflanz, J.; Torbahn, G.; Wiegand, S.; Holzapfel, C.; Hauner, H. Changes in Lifestyle and Body Weight in Children and Adolescents during the COVID-19 Pandemic: A Representative Survey of Parents in Germany. Obes. Facts. 2023, 16, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Guo, B.; Ao, L.; Yang, C.; Zhang, L.; Zhou, J.; Jia, P. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin. Obes. 2020, 10, e12416. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Luo, C.; Feng, X.; Qi, W.; Qu, S.; Zhou, Y.; Sun, L.; Wu, H. Changes in obesity and lifestyle behaviours during the COVID-19 pandemic in Chinese adolescents: A longitudinal analysis from 2019 to 2020. Pediatr. Obes. 2022, 17, e12874. [Google Scholar] [CrossRef] [PubMed]
- Yelizarova, O.; Stankevych, T.; Parats, A.; Polka, N.; Lynchak, O.; Diuba, N.; Hozak, S. The effect of two COVID-19 lockdowns on physical activity of school-age children. Sports Med. Health Sci. 2022, 4, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, G.; Fanos, V.; Cataldi, L.; Cugusi, L.; Crisafulli, A.; Bassareo, P.P. Need for resuming sports and physical activity for children and adolescents following COVID-19 infection. Sport Sci. Health. 2022, 18, 1179–1185. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.H.; Chen, Y.C.; Chen, W.Y.; Chen, C.Y.; Hsu, W.Y.; Chou, Y.; Chang, Y.H. Weight Gain Associated with COVID-19 Lockdown in Children and Adolescents: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 3668. [Google Scholar] [CrossRef] [PubMed]
- Kumari, P.; Toshniwal, D. Impact of lockdown on air quality over major cities across the globe during COVID-19 pandemic. Urban Clim. 2020, 34, 100719. [Google Scholar] [CrossRef]
- Srivastav, P.; Vaishali, K.; Rajwar, E.; Broadbent, S.; Bhat, H.V. Factors associated with physical activity participation among children: A systematic review protocol. Syst. Rev. 2023, 12, 70. [Google Scholar] [CrossRef] [PubMed]
- Treccani. Lockdown: Un Anno Dopo. Available online: https://www.treccani.it/magazine/atlante/societa/Lockdown_un_anno_dopo.html (accessed on 16 December 2024).
- WIKIPEDIA. COVID-19 Lockdowns by Country. Available online: https://en.wikipedia.org/wiki/COVID-19_lockdowns_by_country (accessed on 16 December 2024).
- Helgadóttir, B.; Fröberg, A.; Kjellenberg, K.; Ekblom, Ö.; Nyberg, G. COVID-19 induced changes in physical activity patterns, screen time and sleep among Swedish adolescents—A cohort study. BMC Public Health 2023, 23, 380. [Google Scholar] [CrossRef] [PubMed]
- Coll, I.; Vallejos, D.; López-Safont, N. Differences in Physical Activity Levels, Screen Time, and Body Mass Index and Their Associations with Oral Health in Schoolchildren in Mallorca. Children 2024, 11, 1280. [Google Scholar] [CrossRef] [PubMed]
- Toselli, S.; Grigoletto, A.; Zaccagni, L.; Gualdi-Russo, E.; Rinaldo, N. A Pilot Study on the Association of Internet Use with Sports Practice and Sex in Italian Adolescents. Healthcare 2023, 11, 3075. [Google Scholar] [CrossRef] [PubMed]
- Duarte, L.S.; Palombo, C.N.T.; Solis-Cordero, K.; Kurihayashi, A.Y.; Steen, M.; Borges, A.L.V.; Fujimori, E. The association between body weight dissatisfaction with unhealthy eating behaviors and lack of physical activity in adolescents: A systematic review. J. Child Health Care 2021, 25, 44–68. [Google Scholar] [CrossRef] [PubMed]
- Gualdi-Russo, E.; Rinaldo, N.; Zaccagni, L. Physical Activity and Body Image Perception in Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 13190. [Google Scholar] [CrossRef] [PubMed]
- Djurdjevic, D.; Terzic-Supic, Z.; Todorovic, J.; Bjegovic Mikanovic, V.; Radovanovic Spurnic, A.; Laaser, U. Association between health-enhancing physical activity and the social factors, lifestyle and dietary characteristics. PLoS ONE 2024, 19, e0311974. [Google Scholar] [CrossRef]
- Yang, Y.; Gao, Y.; Yi, X.; Hu, Y.; Zhao, L.; Chen, L.; Sui, W.; Zhang, S.; Ma, S. Does physical activity affect social skills and antisocial behavior? The gender and only child status differences. Front. Public Health 2024, 12, 1502998. [Google Scholar] [CrossRef]
- Shen, C.; Dumontheil, I.; Thomas, M.; Röösli, M.; Elliott, P.; Toledano, M. Digital Technology Use and BMI: Evidence from a Cross-Sectional Analysis of an Adolescent Cohort Study. J. Med. Internet Res. 2021, 23, e26485. [Google Scholar] [CrossRef]
- Luo, R.; Li, Q.; Meng, G.; Zheng, Y.; Hu, K.; Zhang, X.; Dai, B.; Liu, X. The Association between Intolerance of Uncertainty and Internet Addiction during the Second Wave of the Coronavirus Disease 2019 Pandemic: A Multiple Mediation Model Considering Depression and Risk Perception. PsyCh J. 2022, 11, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Király, O.; Potenza, M.N.; Stein, D.J.; King, D.L.; Hodgins, D.C.; Saunders, J.B.; Griffiths, M.D.; Gjoneska, B.; Billieux, J.; Brand, M.; et al. Preventing Problematic Internet Use during the COVID-19 Pandemic: Consensus Guidance. Compr. Psychiatry 2020, 100, 152180. [Google Scholar] [CrossRef] [PubMed]
- Aghasi, M.; Matinfar, A.; Golzarand, M.; Salari-Moghaddam, A.; Ebrahimpour-Koujan, S. Internet Use in Relation to Overweight and Obesity: A Systematic Review and Meta-Analysis of Cross-Sectional Studies. Adv. Nutr. 2020, 11, 349–356. [Google Scholar] [CrossRef]
- Li, H.; Song, Y.; Wang, Y.; Feng, X.; Li, C.; Peng, J.; Yu, H. Impact of the COVID-19 pandemic lockdown on Body Mass Index: A three-year follow up study in 6156 Chinese college students. Front. Endocrinol. 2024, 15, 1387151. [Google Scholar] [CrossRef]
- Gualdi-Russo, E.; Masotti, S.; Rinaldo, N.; De Luca, F.; Toselli, S.; Mazzoni, G.; Mandini, S.; Zaccagni, L. A Longitudinal Study on Body Image Perception and Size among Italian Early Adolescents: Changes over Time and Discrepancies between Genders. Nutrients 2024, 16, 3439. [Google Scholar] [CrossRef] [PubMed]
- Ren, H.; He, X.; Bian, X.; Shang, X.; Liu, J. The Protective Roles of Exercise and Maintenance of Daily Living Routines for Chinese Adolescents During the COVID-19 Quarantine Period. J. Adolesc. Health 2021, 68, 35–42. [Google Scholar] [CrossRef]
- Wang, Y.F.; Wang, K.H. Will Public Health Emergencies Affect Compensatory Consumption Behavior? Evidence from Emotional Eating Perspective. Foods 2024, 13, 3571. [Google Scholar] [CrossRef] [PubMed]
- Artymiak, P.; Żegleń, M.; Kryst, Ł. Changes in BMI and the prevalence of overweight and obesity in children and adolescents (11–15 years) from Kraków (Poland) during COVID-19 pandemic. Anthropol. Anz. 2024. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; Moher, D.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).