Abstract
Huntington’s disease is an autosomal dominant neurodegenerative disease caused by the repetition of cytosine, adenine, and guanine trinucleotides on the short arm of chromosome 4p16.3 within the Huntingtin gene. In this study, we aim to examine and map the existing evidence on the use of innovations in the rehabilitation of Huntington’s disease. A scoping review was conducted on innovative rehabilitative treatments performed on patients with Huntington’s disease. A search was performed on PubMed, Embase, Web of Science, and Cochrane databases to screen references of included studies and review articles for additional citations. Of an initial 1117 articles, only 20 met the search criteria. These findings showed that available evidence is still limited and that studies generally had small sample sizes and a high risk of bias. Regarding cognitive rehabilitation, it has emerged that VR- and PC-based methods as well as NIBS techniques are feasible and may have promising effects in individuals with Huntington’s disease. On the other hand, scarce evidence was found for cognitive and motor training that might have a slight impact on overall cognitive function in individuals with Huntington’s disease. Data show that further investigation is needed to explore the effects of innovative rehabilitation tools on cognition, especially considering that cognitive and psychiatric symptoms can precede the onset of motor symptoms by many years.
1. Introduction
Huntington’s disease (HD), an autosomal dominant neurodegenerative disease, is caused by the repetition of cytosine, adenine, and guanine trinucleotides on the short arm of chromosome 4p16.3 within the Huntingtin gene [1,2]. This disease generally affects individuals between the age of 30 and 50, but it can also manifest before the age of 20 as juvenile HD, which is characterized by learning difficulties and behavioral disorders at school [3]. HD diagnosis is mainly clinical, based on the observation of motor and/or cognitive and behavioral disorders in individuals with a family history of the disease, and is confirmed through DNA testing [4]. Unfortunately, there is currently no cure for the disease, and treatment focuses on managing symptoms and complications (such as pneumonia and suicide attempts) and improving the quality of life [5,6]. The latter, in fact, resulted to be strongly impacted by motor, cognitive, and psychiatric disorders related to HD. Involuntary choreic movements along with cognitive and behavioral disturbances constitute pathognomonic symptoms of pathology [7,8,9,10]. Specifically, the most common motor disorders involve involuntary movements that begin in the distal extremities, including the facial muscles, and then gradually progress to the more proximal and axial muscles, increasing in amplitude [7,8]. Over time, motor symptoms progressively worsen and may include hypokinesia with bradykinesia, dystonia, rigidity, and extremity contractures. Additionally, dysarthria and dysphagia, dystonia, tics, and cerebellar signs, such as ataxia, may occur. As for behavioral and psychiatric symptoms, they often precede motor symptoms and resemble frontal lobe dysfunction, with poor attention, impulsiveness, and irritability [10,11]. Other possible symptoms include apathy, loss of intuition and creativity, psychosis, lack of awareness, and depression, often associated with suicide attempts [11,12]. Cognitive difficulties are frequently present in HD, affecting executive functions related to organization, multitasking, and planning [13], sometimes resembling subcortical dementia with memory loss [13].
Given the considerable impact the disease has on the patient’s personal, relational, and psychophysical sphere, rehabilitation approaches are an excellent option to treat these patients. The term rehabilitation refers to a multidisciplinary approach aimed at restoring or enhancing an individual’s ability to live independently and participate fully in society following an injury, illness, or disability [14]. It encompasses various traditional approaches, including physical therapy, occupational therapy, speech therapy, and neuropsychology. However, the use of new rehabilitation technologies, such as virtual reality (VR), Pc-Based training, or innovative techniques, such as non-invasive brain stimulation (NIBS), could make a significant contribution to improving functional outcomes, as seen in other conditions [15,16,17,18].
Therefore, the aim of this scoping review is to map the existing evidence on the use of innovations in the rehabilitation of HD.
2. Methods
We conducted this scoping review to explore existing evidence on innovative rehabilitation in HD for improving motor and cognitive outcomes in patients. This review was registered with a DOI (https://doi.org/10.17605/OSF.IO/H46KJ) on the Open Science Framework (OSF).
2.1. Search Strategy
This review aimed to map existing evidence on the use of innovations in Huntington’s disease rehabilitation by selecting full-length articles. A review of currently published studies was performed in the following databases: Pubmed, Embase, Cochrane Database, and Web of Science. The search terms used included ((Huntington’s disease) AND (cognitive rehabilitation); (Huntington’s disease) AND (computer); (Huntington’s disease) AND (NIBS); (Huntington’s disease) AND (physical therapy); (Huntington’s disease) AND (robotic); (Huntington’s disease) AND (virtual reality)). All articles were initially reviewed based on titles and abstracts by three investigators (M.G.M., D.C., L.B.), who independently collected data to minimize the risk of bias (e.g., publication bias, delay bias, language bias). Full-text articles deemed suitable for the study were then read by these researchers, and in case of disagreements regarding inclusion or exclusion criteria, a final decision was made by a fourth researcher (R.S.C.).
2.2. Inclusion Criteria
A study was included if it described or investigated patients with Huntington’s disease treated with innovative approaches of cognitive or motor rehabilitation. Only articles written in English and published in a peer-reviewed journal were included in the review.
2.3. Exclusion Criteria
A study was excluded if it described theoretical models, methodological approaches, algorithms, and basic technical descriptions as well as: (i) animal studies; (ii) conference proceedings or reviews; and (iii) studies involving other neurological patients.
3. Results
The list of articles was refined for relevance, reviewed, and summarized, with key themes identified based on inclusion/exclusion criteria.
Data extraction was conducted on 1117 articles. Data considered for extraction included information on authors, year and type of publication (e.g., clinical studies, pilot studies), participant characteristics, and study purposes. After a thorough review, only 20 articles met the inclusion criteria (Figure 1).
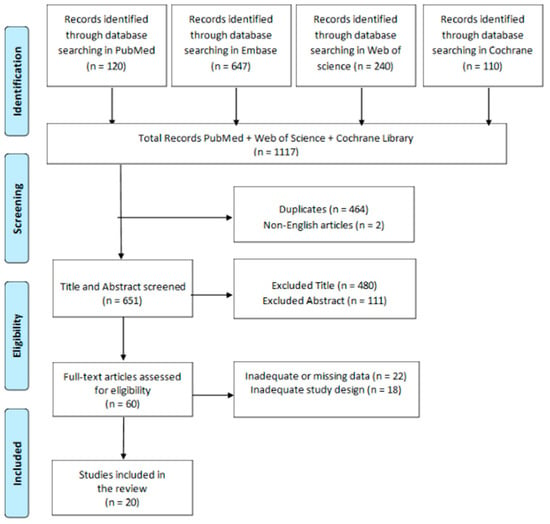
Figure 1.
PRISMA flow chart for the current review.
3.1. Innovative Rehabilitation Devices
3.1.1. Virtual Reality
Virtual Reality (VR) is a multisensory and interactive simulation of ecological scenarios. These scenarios are typically three-dimensional, replicating objects and events to provide the users with the illusion of active interaction with the screen [19]. Additionally, VR provides audiovisual feedback in response to the subject’s movements. Due to its characteristics, VR has the potential to enhance motor and cognitive functions as well as improve well-being and treatment compliance [20]. VR experiences allow for patients to be at the center of the implemented programs, thanks to the high level of training customization [21]. Furthermore, two key concepts related to VR are immersion and presence. Immersion represents the objective sense of sensory absorption/immersion in the computer-generated, three-dimensional environment. This process is connected to the concept of presence, with a subjective psychological state in which the user is consciously engaged in the virtual context. From this perspective, VR could be highly beneficial in the treatment of cognitive, emotional, and motor disorders in HD patients.
The VR devices used in the reviewed studies differ significantly. Some devices promote daily life skills, as seen in RCT conducted by Begeti et al. [22]. The authors utilized a VR tool where patients swim in a pool using a joystick, with the task of reaching a submerged platform guided by external cues. Similarly, Julio et al. used a VR device, namely “EcoKitchen”, which enhances the executive functions necessary for simple daily tasks, such as making toast or a cup of coffee with milk, or simple actions, such as removing a kettle from heat. This highlights the potential role of VR in increasing task execution awareness [23]. Two other studies by the same authors emphasized that the “EcoKitchen” can detect executive deficits in patients with early and premanifest HD and is feasible [24,25]. Lastly, Cellini et al., in a single case study, evaluated the effectiveness of the Computer Assisted Rehabilitation Environment (CAREN), an immersive VR tool, in the rehabilitation of an HD patient, observing the potential role of VR devices in improving motor outcomes [26].
3.1.2. PC-Based Rehabilitation
PC-based methods involve the use of software to implement intensive, targeted, and repeated interventions for specific cognitive and motor functions. These interventions typically include the execution of tasks or games, often referred to as ‘serious games’, that involve various domains [26]. The primary goal of this method is to enhance performance by utilizing positive reinforcement, which includes providing sensory and motivational feedback [27]. Additionally, these exercises offer therapists the flexibility to adjust the duration and difficulty of the tasks to match the individual’s characteristics and needs [27,28]. In our analysis of the literature, we identified 378 articles related to PC-based methods for interventions in HD patients.
We have selected eight studies that meet the inclusion criteria, including three RCTs.
Kempnich et al., in an RCT using a computerized program known as the MicroExpression Training Tool, found that emotion recognition training has proven promising in maintaining participant engagement [29]. Another RCT by Kloos et al. demonstrates the feasibility and effectiveness of a PC game called “Dance Dance Revolution” in patients with HD for enhancing motor skills [30]. In this context, Yhnell et al. observed that the Cogmed computer program, designed for cognitive and motor improvement, is well-received and feasible for individuals with HD [31]. The same tool has been used by Sadeghi et al. to enhance working memory with positive results [32]. On the other hand, Coulson et al. conducted a study on the messages exchanged by patients in online chats, noting that social support provided through online IT platforms plays a crucial role in patients with HD [33]. Moreover, some researchers have also emphasized the importance of multidisciplinary treatments, in which PC-based methods were included. Bartlett et al. showed that subjecting individuals with HD to a multidisciplinary intervention, including computerized training, leads to significant improvements in verbal learning, memory, attention, cognitive flexibility, and processing speed compared to conventional treatment [34]. Indeed, another study by the same authors showed that multidisciplinary rehabilitation, including PC-based approaches, can mitigate hypothalamic volume loss and sustain peripheral BDNF levels in preclinical HD individuals, improving cognitive functions [35]. Finally, Metzler-Baddeley et al. conducted a web-based survey, demonstrating that tablet-based touch screens were recognized as feasible and accessible solutions for rehabilitation with a PC app [36].
A description of the main features of the studies concerning VR and PC-based interventions can be found in Table 1.

Table 1.
The main studies regarding innovative interventions for Huntington’s disease.
3.2. Other Therapy (Cognitive and Motor Rehabilitation)
Most studies in the literature encourage the use of physical rehabilitation, either performed individually or as part of a multidisciplinary approach, to promote improvements in the physical and cognitive outcomes of HD patients [37,38,39,40,41]. Among various interventions, we have selected some articles that presented motor and cognitive therapies implemented with innovative technology (Table 2). In this context, Khalil et al. have focused on improving home-based rehabilitation with physical exercises using an exercise DVD [42]. The authors found that structured, short-term home exercise programs are practical, beneficial, and safe for individuals in the early and middle stages of HD [42].
Furthermore, Shih et al. employed a four-month coaching program in which participants utilized Fitbit devices and received support through a behavioral intervention aimed at promoting the physical activity, showing the effectiveness of this device [43].
Finally, another type of intervention with promising results is dance therapy. A study by Trinkel et al. on HD patients showed promising results in terms of spatial and bodily representations, helping to enhance motor function in individuals with HD [44].

Table 2.
The main studies regarding other interventions in Huntington’s disease.
Table 2.
The main studies regarding other interventions in Huntington’s disease.
| Studies | Study Design | Sample Size | Intervention | Device Type Tools Domains | Outcome Measures | Major Findings |
|---|---|---|---|---|---|---|
| Khalil et al. (2013) [42] | RCT | 21 EG:11 CG:10 | EG: Exercises at home three times a week for eight weeks using an exercise DVD. GC received their usual care. | DVD Motor functions | GAITRite system BBS SAM SF36 | Structured, short-term home exercise programs are practical, beneficial, and safe for individuals in the early and middle stages of Huntington’s disease. |
| Shih et al. (2023) [43] | Clinical study | early-PD: 13 HD: 14 | 4-month coaching program, wore a Fitbit, and were guided through a behavioural intervention to facilitate PA uptake | Coaching Program with FitBit Motor functions | BBS | Incorporating wearables into a coaching intervention was achievable and offered valuable insights into physical activity behavior |
| Trinkler et al. (2019) [44] | Pilot study | 19 | Contemporary dance, a lyrical dance form, practiced for two hours per week over five months | Dance therapy Motor functions | UHDRS MDRS TMT LARS PBA QLI | Dance therapy has promising results in terms of spatial and bodily representations, helping to enhance motor function in individuals with HD |
Legend: Berg Balance Scale (BBS), Control group (CG), Experimental Goup (EG), Unified Huntington’s Disease Rating Scale (UHDRS), Lille Apathy Rating Scale (LARS), Mattis Dementia Rating Scale (MDRS), Short Form 36 (SF36), Problem Behaviors Assessment (PBA), Quality of Life Index (QLI), Step Watch Step Activity Monitor (SAM), Trail Making Test (TMT).
3.3. Non-Invasive Brain Stimulation (NIBS)
Recent studies explored alterations in interhemispheric connectivity in HD and its temporal association with clinical manifestations. The prevailing understanding of motor symptoms in HD attributes them to a disorganized sensory–motor network and disrupted neurotransmission between the motor cortex and basal ganglia [45,46,47].
The use of neuromodulation techniques for managing HD-related symptoms has been FDA-approved, although their application remains primarily in the research contexts. However, growing interest surrounds non-invasive neuromodulation methods, including transcranial magnetic stimulation (TMS), transcranial electric stimulation (tES), and particularly transcranial direct current stimulation (tDCS), as potential therapies for neurodegenerative diseases, such as HD [48]. A recent systematic review highlights abnormal brain connectivity in various networks in HD, including sensory, motor, visual, and executive/attentional networks [49]. Non-invasive neuromodulation methods are believed to work by reorganizing brain networks, potentially rectifying the aberrant connectivity observed in HD, thereby positively influencing associated symptoms. While the initial studies suggest the effectiveness of these methods with minimal side effects, the evidence remains limited [50].
We evaluated two studies regarding tDCS [51,52], five studies assessing TMS [53,54,55,56,57], and two studies about tACS [58,59].
3.4. tDCS
The utility of transcranial electric stimulation (tES) in movement disorders has proven promising, but its mainstream application remains limited, primarily due to the diversity of patient populations and protocols [51,52]. Transcranial direct current stimulation (tDCS), combined with cognitive tasks, has shown the potential to enhance cognitive functioning, which is particularly relevant in HD, given its progressive cognitive impairment [51,52]. Two double-blinded crossover trials with tDCS have demonstrated improvements in cognitive and motor symptoms in HD, although further research is needed to understand the full extent of these effects [51,52].
3.5. TMS
Repetitive transcranial magnetic stimulation (rTMS) has been employed to alleviate choreiform movements in HD patients. Five studies have utilized TMS for HD [53,54,55,56,57]. These studies used different TMS modalities and coil types, targeting various brain regions. The studies reported symptom improvements, with some variations in the results likely due to different factors, including target accuracy, coil size, and pulse parameters. However, the duration of improvement, in some cases, was temporary.
3.6. tACS
Transcranial alternating current stimulation (tACS) is a versatile non-invasive brain stimulation (NIBS) technique that can target specific neural oscillatory frequencies, showing minimal and transient adverse effects [57,58]. Recent research has indicated that alpha frequency tACS, targeting bilateral mPFC (medial prefrontal cortex), has the potential to influence brain activity in HD patients. In summary, neuromodulation techniques, such as TMS, tDCS, and tACS, show promise in ameliorating the symptoms and connectivity issues associated with HD, but further research is necessary to better understand their efficacy and potential applications [59].
A summary of the main characteristics of studies regarding NIBS in HD patients can be found in Table 3.

Table 3.
The main studies regarding NIBS in Huntington’s disease.
4. Discussion
To the best of our knowledge, this is the first review that evaluated the state of the art of cognitive and motor rehabilitation using innovative methods in HD. Our review showed that the available evidence is limited, and the studies generally had small sample sizes and a high risk of bias. However, this was expected because of the low prevalence of HD, and this is why we decided to carry out a scoping review on this topic.
Regarding cognitive rehabilitation, it has emerged that VR- and PC-based methods as well as NIBS techniques are feasible and may have a promising effect in individuals with HD. This is in line with previous studies that highlighted the beneficial role in cognitive training of healthy elderly individuals, patients with mild cognitive impairment, and various neurological and dementia-related conditions [60,61,62,63], including Parkinson’s disease [64] and multiple sclerosis [65,66]. Indeed, cognitive training has been shown to improve cognitive function by promoting neuroplasticity through structural and functional changes in the brain [67]. Notably, studies on cognitive training have mostly included mixed groups of individuals with pre-manifest and manifest HD, also incorporating other conditions, such as PD, making it difficult to draw conclusions about the effects based on the disease stage. However, the results from various studies suggested that the disease stage has been identified as a barrier to participation or in the benefits obtained from rehabilitation [68,69].
Nevertheless, there was low-quality evidence suggesting that cognitive training might have a slight impact on overall cognitive function in individuals with HD. Therefore, further investigation is needed to explore the effects of innovative rehabilitation tools on cognition, especially considering that cognitive and psychiatric symptoms can precede the onset of motor symptoms by many years. In fact, although the diagnosis of HD is primarily based on motor symptoms, cognitive deficits are prevalent. During the pre-manifest phase of HD, which occurs before clinical diagnosis, approximately 40% of individuals experience mild cognitive impairment [70]. This percentage escalates up to 80% at the onset of the disease [71,72]. Furthermore, cognitive symptoms have a more substantial impact on the quality of life compared to motor and psychiatric symptoms. In this perspective, given the lack of available pharmaceutical treatments to improve or preserve cognitive function in individuals with HD, it is valuable to enhance treatment possibilities with innovative methods [73]. An interesting aspect is that combined interventions, which include both physical and cognitive exercises, lead to greater results compared to interventions focused on each treatment alone. In fact, interventions based solely on physical exercises could have reduced effects on cognition. This agrees with previous reviews that emphasized the diminished effects of solely physical interventions on cognition in both HD [74,75] and dementia [76]. This aspect should not be due to the stage of HD, as our review also includes studies involving pre-manifest participants, not just manifest patients with severe symptoms [24,25,26,27,28]. Therefore, cognitive training can boost cognitive domains, also influencing motor outcomes. In fact, a previous meta-analysis demonstrated in the elderly that a combined cognitive–motor treatment is more effective than treatments implemented individually [77]. Another interesting aspect is that innovative rehabilitation has better effects on cognitive and motor domains, compared to non-specific treatments, such as activities such as puzzles or independent exercises, as observed in the control groups of some studies [23,24,25,26,30].
Regarding the studies carried out on the motor component, the studies are limited but have encouraging results. Specifically, studies were conducted both at a preventive level and following the appearance of motor symptoms. In the latter case, these are mainly studies conducted with NIBS methods, with good effects on the improvement of choreic symptoms [52,53,54]. The heterogeneity of patients, including a mixed sample of individuals with manifest/pre-manifest Huntington’s disease and other neurodegenerative disorders, along with small sample sizes, variations in protocols used, a lack of follow-up, and the diversity of standardized tests used to assess functional outcomes, are the main limitations of the study. These hinder the definition of the role of innovative rehabilitative interventions in HD. However, general considerations can be made based on the analyses conducted. First, given the scarcity of available treatments, investing in innovative rehabilitation methods could be a viable alternative. This is especially relevant since these methods show encouraging results and can also enhance patient motivation towards treatment, as observed in other neurodegenerative populations. In addition, randomized trials on larger samples to explore the possible interaction and complementarity of these innovative approaches are needed.
In conclusion, this scoping review has highlighted the feasibility and potential efficacy of innovative rehabilitation tools in the rehabilitation of cognitive and behavioral dysfunction in patients with HD. Few data are still available on the motor outcomes. Considering the negative impact of cognitive–motor dysfunction on patients’ outcomes and the poor effect of pharmacological treatments, research on innovation technology to deal with these concerns is fundamental in order to improve the quality of life of both patients and their caregivers.
Funding
This study was supported by Current Research Funds 2023, Ministry of Health, Italy.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| HD | Huntington’s Disease |
| RCT | Randomized Clinical Trials |
| VR | Virtual Reality |
| PC | Personal Computer |
| NIBS | Non-Invasive Brain Stimulation |
| mPFC | Medial Prefrontal Cortex |
| TMS | Transcranial Magnetic Stimulation |
| tES | Transcranial Electric Stimulation |
| tDCS | Transcranial Direct Current Stimulation |
| tACS | Transcranial Alternating Current Stimulation |
References
- Ajitkumar, A.; De Jesus, O. Huntington Disease. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Liang, S.; Zhou, J.; Yu, X.; Lu, S.; Liu, R. Neuronal conversion from glia to replenish the lost neurons. Neural Regen. Res. 2024, 19, 1446–1453. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.Y.; Gough, S.; Niyibizi, A.; Sheikh, M. Juvenile Huntington’s Disease: A Case Report and a Review of Diagnostic Challenges. Cureus 2023, 15, e40637. [Google Scholar] [CrossRef] [PubMed]
- Meem, T.M.; Khan, U.; Mredul, M.B.R.; Awal, M.A.; Rahman, M.H.; Khan, M.S. A Comprehensive Bioinformatics Approach to Identify Molecular Signatures and Key Pathways for the Huntington Disease. Bioinform. Biol. Insights 2023, 17, 11779322231210098. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Song, M.K. Update of Rehabilitation in Huntington’s Disease: Narrative Review. Brain Neurorehabil. 2023, 16, e28. [Google Scholar] [CrossRef] [PubMed]
- Roos, R.A. Huntington’s disease: A clinical review. Orphanet J. Rare Dis. 2010, 5, 40. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Huang, Y.; Orth, M.; Gillis, T.; Siciliano, J.; Hong, E.; Mysore, J.S.; Lucente, D.; Wheeler, V.C.; Seong, I.S.; et al. Genetic modifiers of Huntington disease differentially influence motor and cognitive domains. Am. J. Hum. Genet. 2022, 109, 885–899. [Google Scholar] [CrossRef]
- Koch, E.T.; Sepers, M.D.; Cheng, J.; Raymond, L.A. Early Changes in Striatal Activity and Motor Kinematics in a Huntington’s Disease Mouse Model. Mov. Disord. 2022, 37, 2021–2032. [Google Scholar] [CrossRef]
- Ruiz-Idiago, J.; Pomarol-Clotet, E.; Salvador, R. Longitudinal analysis of neuropsychiatric symptoms in a large cohort of early-moderate manifest Huntington’s disease patients. Park. Relat. Disord. 2023, 106, 105228. [Google Scholar] [CrossRef]
- Olvera, C.; Stebbins, G.T.; Romero, V.P.; Hall, D.A. Criminality in Huntington Disease. Neurol. Clin. Pract. 2022, 12, 397–405. [Google Scholar] [CrossRef]
- Bilal, H.; Harding, I.H.; Stout, J.C. The relationship between disease-specific psychosocial stressors and depressive symptoms in Huntington’s disease. J. Neurol. 2023. [Google Scholar] [CrossRef]
- Eddy, C.M.; Rickards, H. Social cognition and quality of life in Huntington’s disease. Front. Psychiatry 2022, 13, 963457. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; Mridha, D. Unraveling Huntington’s Disease: A Report on Genetic Testing, Clinical Presentation, and Disease Progression. Cureus 2023, 15, e43377. [Google Scholar] [CrossRef] [PubMed]
- Kreitzer, N.; Rath, K.; Kurowski, B.G.; Bakas, T.; Hart, K.; Lindsell, C.J.; Adeoye, O. Rehabilitation Practices in Patients with Moderate and Severe Traumatic Brain Injury. J. Head. Trauma. Rehabil. 2019, 34, E66–E72. [Google Scholar] [CrossRef] [PubMed]
- Pfalzer, A.C.; Watson, K.H.; E Ciriegio, A.; Hale, L.; Diehl, S.; E McDonell, K.; Vnencak-Jones, C.; Huitz, E.; Snow, A.; Roth, M.C.; et al. Impairments to executive function in emerging adults with Huntington disease. J. Neurol. Neurosurg. Psychiatry 2023, 94, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, S.; Maggio, M.G.; Russo, M.; Bramanti, A.; Arcadi, F.A.; Naro, A.; Calabrò, R.S.; De Luca, R. Cognitive recovery in people with relapsing/remitting multiple sclerosis: A randomized clinical trial on virtual reality-based neurorehabilitation. Clin. Neurol. Neurosurg. 2021, 208, 106828. [Google Scholar] [CrossRef] [PubMed]
- Manuli, A.; Maggio, M.G.; Stagnitti, M.C.; Aliberti, R.; Cannavò, A.; Casella, C.; Milardi, D.; Bruschetta, A.; Naro, A.; Calabrò, R.S. Is intensive gait training feasible and effective at old age? A retrospective case-control study on the use of Lokomat Free-D in patients with chronic stroke. J. Clin. Neurosci. 2021, 92, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Naro, A.; Billeri, L.; Balletta, T.; Lauria, P.; Onesta, M.P.; Calabrò, R.S. Finding the Way to Improve Motor Recovery of Patients with Spinal Cord Lesions: A Case-Control Pilot Study on a Novel Neuromodulation Approach. Brain Sci. 2022, 12, 119. [Google Scholar] [CrossRef] [PubMed]
- Maggio, M.G.; Cezar, R.P.; Milardi, D.; Borzelli, D.; DEMarchis, C.; D’Avella, A.; Quartarone, A.; Calabrò, R.S. Do patients with neurological disorders benefit from immersive virtual reality? A scoping review on the emerging use of the computer-assisted rehabilitation environment. Eur. J. Phys. Rehabil. Med. 2023; Epub ahead of print. [Google Scholar] [CrossRef]
- Bruschetta, R.; Maggio, M.G.; Naro, A.; Ciancarelli, I.; Morone, G.; Arcuri, F.; Tonin, P.; Tartarisco, G.; Pioggia, G.; Cerasa, A.; et al. Gender Influences Virtual Reality-Based Recovery of Cognitive Functions in Patients with Traumatic Brain Injury: A Secondary Analysis of a Randomized Clinical Trial. Brain Sci. 2022, 12, 491. [Google Scholar] [CrossRef]
- De Giorgi, R.; Fortini, A.; Aghilarre, F.; Gentili, F.; Morone, G.; Antonucci, G.; Vetrano, M.; Tieri, G.; Iosa, M. Virtual Art Therapy: Application of Michelangelo Effect to Neurorehabilitation of Patients with Stroke. J. Clin. Med. 2023, 12, 2590. [Google Scholar] [CrossRef]
- Begeti, F.; Schwab, L.C.; Mason, S.L.; Barker, R.A. Hippocampal dysfunction defines disease onset in Huntington’s disease. J. Neurol. Neurosurg. Psychiatry 2016, 87, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Júlio, F.; Ribeiro, M.J.; Morgadinho, A.; Sousa, M.; van Asselen, M.; Simões, M.R.; Castelo-Branco, M.; Januário, C. Cognition, function and awareness of disease impact in early Parkinson’s and Huntington’s disease. Disabil. Rehabil. 2022, 44, 921–939. [Google Scholar] [CrossRef] [PubMed]
- Júlio, F.; Caetano, G.; Januário, C.; Castelo-Branco, M. The effect of impulsivity and inhibitory control deficits in the saccadic behavior of premanifest Huntington’s disease individuals. Orphanet J. Rare Dis. 2019, 14, 246. [Google Scholar] [CrossRef] [PubMed]
- Júlio, F.; Ribeiro, M.J.; Patrício, M.; Malhão, A.; Pedrosa, F.; Gonçalves, H.; Simões, M.; Van Asselen, M.; Simões, M.R.; Castelo-Branco, M.; et al. A Novel Ecological Approach Reveals Early Executive Function Impairments in Huntington’s Disease. Front. Psychol. 2019, 10, 585. [Google Scholar] [CrossRef] [PubMed]
- Cellini, R.; Paladina, G.; Mascaro, G.; Lembo, M.A.; Lombardo Facciale, A.; Ferrera, M.C.; Fonti, B.; Pergolizzi, L.; Buonasera, P.; Bramanti, P.; et al. Effect of Immersive Virtual Reality by a Computer Assisted Rehabilitation Environment (CAREN) in Juvenile Huntington’s Disease: A Case Report. Medicina 2022, 58, 919. [Google Scholar] [CrossRef]
- De Luca, R.; Russo, M.; Gasparini, S.; Leonardi, S.; Cuzzola, M.F.; Sciarrone, F.; Zichittella, C.; Sessa, E.; Maggio, M.G.; De Cola, M.C.; et al. Do people with multiple sclerosis benefit from PC-based neurorehabilitation? A pilot study. Appl. Neuropsychol. Adult 2021, 28, 427–435. [Google Scholar] [CrossRef]
- De Luca, R.; Leonardi, S.; Spadaro, L.; Russo, M.; Aragona, B.; Torrisi, M.; Maggio, M.G.; BioEng, A.B.; Naro, A.; De Cola Mstat, M.C.; et al. Improving Cognitive Function in Patients with Stroke: Can Computerized Training Be the Future? J. Stroke Cerebrovasc. Dis. 2018, 27, 1055–1060. [Google Scholar] [CrossRef]
- Kempnich, C.L.; Wong, D.; Georgiou-Karistianis, N.; Stout, J.C. Feasibility and Efficacy of Brief Computerized Training to Improve Emotion Recognition in Premanifest and Early-Symptomatic Huntington’s Disease. J. Int. Neuropsychol. Soc. 2017, 23, 314–321. [Google Scholar] [CrossRef]
- Kloos, A.D.; Fritz, N.E.; Kostyk, S.K.; Young, G.S.; Kegelmeyer, D.A. Video game play (Dance Dance Revolution) as a potential exercise therapy in Huntington’s disease: A controlled clinical trial. Clin. Rehabil. 2013, 27, 972–982. [Google Scholar] [CrossRef]
- Yhnell, E.; Furby, H.; Lowe, R.S.; Brookes-Howell, L.C.; Drew, C.J.; Playle, R.; Watson, G.; Metzler-Baddeley, C.; Rosser, A.E.; Busse, M.E. A randomised feasibility study of computerised cognitive training as a therapeutic intervention for people with Huntington’s disease (CogTrainHD). Pilot. Feasibility Stud. 2020, 6, 88. [Google Scholar] [CrossRef]
- Sadeghi, M.; Barlow-Krelina, E.; Gibbons, C.; Shaikh, K.T.; Fung, W.L.A.; Meschino, W.S.; Till, C. Feasibility of computerized working memory training in individuals with Huntington disease. PLoS ONE 2017, 12, e0176429. [Google Scholar] [CrossRef] [PubMed]
- Won, E.J.; Johnson, P.W.; Punnett, L.; Dennerlein, J.T. Upper extremity biomechanics in computer tasks differ by gender. J. Electromyogr. Kinesiol. 2009, 19, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.M.; Govus, A.; Rankin, T.; Lampit, A.; Feindel, K.; Poudel, G.; Teo, W.-P.; Lo, J.; Georgiou-Karistianis, N.; Ziman, M.R.; et al. The effects of multidisciplinary rehabilitation on neuroimaging, biological, cognitive and motor outcomes in individuals with premanifest Huntington’s disease. J. Neurol. Sci. 2020, 416, 117022. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.M.; Lazar, A.S.; Kordsachia, C.C.; Rankin, T.J.; Lo, J.; Govus, A.D.; Power, B.D.; Lampit, A.; Eastwood, P.R.; Ziman, M.R.; et al. Multidisciplinary rehabilitation reduces hypothalamic grey matter volume loss in individuals with preclinical Huntington’s disease: A nine-month pilot study. J. Neurol. Sci. 2020, 408, 116522. [Google Scholar] [CrossRef] [PubMed]
- Metzler-Baddeley, C.; Busse, M.; Drew, C.; Pallmann, P.; Cantera, J.; Ioakeimidis, V.; Rosser, A. HD-DRUM, a Tablet-Based Drumming Training App Intervention for People with Huntington Disease: App Development Study. JMIR Form. Res. 2023, 7, e48395. [Google Scholar] [CrossRef] [PubMed]
- Quinn, L.; Playle, R.; Drew, C.J.; Taiyari, K.; Williams-Thomas, R.; Muratori, L.M.; Hamana, K.; Griffin, B.A.; Kelson, M.; Schubert, R.; et al. Physical activity and exercise outcomes in Huntington’s disease (PACE-HD): Results of a 12-month trial-within-cohort feasibility study of a physical activity intervention in people with Huntington’s disease. Park. Relat. Disord. 2022, 101, 75–89. [Google Scholar] [CrossRef] [PubMed]
- van Walsem, M.R.; Piira, A.; Mikalsen, G.; Fossmo, H.L.; Howe, E.I.; Knutsen, S.F.; Frich, J.C. Cognitive Performance After a One-Year Multidisciplinary Intensive Rehabilitation Program for Huntington’s Disease: An Observational Study. J. Huntingtons Dis. 2018, 7, 379–389. [Google Scholar] [CrossRef]
- Atkins, K.J.; Friel, C.P.; Andrews, S.C.; Chong, T.T.; Stout, J.C.; Quinn, L. A qualitative examination of apathy and physical activity in Huntington’s and Parkinson’s disease. Neurodegener. Dis. Manag. 2022, 12, 129–139. [Google Scholar] [CrossRef]
- Cruickshank, T.M.; Reyes, A.P.; Penailillo, L.E.; Pulverenti, T.; Bartlett, D.M.; Zaenker, P.; Blazevich, A.J.; Newton, R.U.; Thompson, J.A.; Lo, J.; et al. Effects of multidisciplinary therapy on physical function in Huntington’s disease. Acta Neurol. Scand. 2018, 138, 500–507. [Google Scholar] [CrossRef]
- Zinzi, P.; Salmaso, D.; De Grandis, R.; Graziani, G.; Maceroni, S.; Bentivoglio, A.; Zappata, P.; Frontali, M.; Jacopini, G. Effects of an intensive rehabilitation programme on patients with Huntington’s disease: A pilot study. Clin. Rehabil. 2007, 21, 603–613. [Google Scholar] [CrossRef]
- Khalil, H.; Quinn, L.; van Deursen, R.; Dawes, H.; Playle, R.; Rosser, A.; Busse, M. What effect does a structured home-based exercise programme have on people with Huntington’s disease? A randomized, controlled pilot study. Clin. Rehabil. 2013, 27, 646–658. [Google Scholar] [CrossRef] [PubMed]
- Shih, H.S.; Quinn, L.; Morgan-Jones, P.; Long, K.; Schreier, A.R.; Friel, C.P. Wearable activity monitors to support physical activity interventions in neurodegenerative disease: A feasibility study. Neurodegener. Dis. Manag. 2023, 13, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.; Lalonde, K.; Truesdell, A.; Gomes Welter, P.; Brocardo, P.S.; Rosenstock, T.R.; Gil-Mohapel, J. New Avenues for the Treatment of Huntington’s Disease. Int. J. Mol. Sci. 2021, 22, 8363. [Google Scholar] [CrossRef] [PubMed]
- Wolf, R.C.; Sambataro, F.; Vasic, N.; Depping, M.S.; Thomann, P.A.; Landwehrmeyer, G.B.; Süssmuth, S.D.; Orth, M. Abnormal resting-state connectivity of motor and cognitive networks in early manifest Huntington’s disease. Psychol. Med. 2014, 44, 3341–3356. [Google Scholar] [CrossRef]
- Werner, C.J.; Dogan, I.; Saß, C.; Mirzazade, S.; Schiefer, J.; Shah, N.J.; Schulz, J.B.; Reetz, K. Altered resting-state connectivity in Huntington’s disease. Hum. Brain Mapp. 2014, 35, 2582–2593. [Google Scholar] [CrossRef]
- Ganguly, J.; Murgai, A.; Sharma, S.; Aur, D.; Jog, M. Non-invasive Transcranial Electrical Stimulation in Movement Disorders. Front. Neurosci. 2020, 14, 522. [Google Scholar] [CrossRef]
- Pini, L.; Jacquemot, C.; Cagnin, A.; Meneghello, F.; Semenza, C.; Mantini, D.; Vallesi, A. Aberrant brain network connectivity in presymptomatic and manifest Huntington’s disease: A systematic review. Hum. Brain Mapp. 2020, 41, 256–269. [Google Scholar] [CrossRef]
- Chase, H.W.; Boudewyn, M.A.; Carter, C.S.; Phillips, M.L. Transcranial direct current stimulation: A roadmap for research, from mechanism of action to clinical implementation. Mol. Psychiatry 2020, 25, 397–407. [Google Scholar] [CrossRef]
- Eddy, C.M.; Shapiro, K.; Clouter, A.; Hansen, P.C.; Rickards, H.E. Transcranial direct current stimulation can enhance working memory in Huntington’s disease. Prog. Neuropsychopharmacol. Biol. Psychiatry 2017, 77, 75–82. [Google Scholar] [CrossRef]
- Bocci, T.; Baloscio, D.; Ferrucci, R.; Sartucci, F.; Priori, A. Cerebellar Direct Current Stimulation (ctDCS) in the Treatment of Huntington’s Disease: A Pilot Study and a Short Review of the Literature. Front. Neurol. 2020, 11, 614717. [Google Scholar] [CrossRef]
- Brusa, L.; Versace, V.; Koch, G.; Bernardi, G.; Iani, C.; Stanzione, P.; Centonze, D. Improvement of choreic movements by 1 Hz repetitive transcranial magnetic stimulation in Huntington’s disease patients. Ann. Neurol. 2005, 58, 655–656. [Google Scholar] [CrossRef] [PubMed]
- Shukla, A.; Jayarajan, R.N.; Muralidharan, K.; Jain, S. Repetitive transcranial magnetic stimulation not beneficial in severe choreiform movements of Huntington disease. J. ECT 2013, 29, e16–e17. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.; Phillips, A.; Tendler, A.; Oberdeck, A. Deep rTMS for Neuropsychiatric Symptoms of Huntington’s Disease: Case Report. Brain Stimul. 2016, 9, 960–961. [Google Scholar] [CrossRef] [PubMed]
- Bocci, T.; Hensghens, M.J.; Di Rollo, A.; Parenti, L.; Barloscio, D.; Rossi, S.; Sartucci, F. Impaired interhemispheric processing in early Huntington’s Disease: A transcranial magnetic stimulation study. Clin. Neurophysiol. 2016, 127, 1750–1752. [Google Scholar] [CrossRef] [PubMed]
- Groiss, S.; Netz, J.; Lange, H.; Buetefisch, C. Frequency dependent effects of rTMS on motor and cognitive functions in Huntington’s disease. Basal Ganglia 2012, 2, 41–48. [Google Scholar] [CrossRef]
- Booth, S.J.; Taylor, J.R.; Brown, L.J.E.; Pobric, G. The effects of transcranial alternating current stimulation on memory performance in healthy adults: A systematic review. Cortex. 2022, 147, 112–139. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.-C.; Hill, A.T.; Fitzgerald, P.B.; Bailey, N.W.; Sullivan, C.; Stout, J.C.; Hoy, K.E. Medial prefrontal transcranial alternating current stimulation for apathy in Huntington’s disease. Prog. Neuropsychopharmacol. Biol. Psychiatry 2023, 126, 110776. [Google Scholar] [CrossRef] [PubMed]
- Tavakoli, A.V.; Yun, K. Transcranial Alternating Current Stimulation (tACS) Mechanisms and Protocols. Front. Cell. Neurosci. 2017, 11, 214. [Google Scholar] [CrossRef]
- Billeri, L.; Naro, A. A narrative review on non-invasive stimulation of the cerebellum in neurological diseases. Neurol. Sci. 2021, 42, 2191–2209. [Google Scholar] [CrossRef]
- Davis, M.C.; Fitzgerald, P.B.; Bailey, N.W.; Sullivan, C.; Stout, J.C.; Hill, A.T.; Hoy, K.E. Effects of medial prefrontal transcranial alternating current stimulation on neural activity and connectivity in people with Huntington’s disease and neurotypical controls. Brain Res. 2023, 1811, 148379. [Google Scholar] [CrossRef]
- Gavelin, H.M.; Lampit, A.; Hallock, H.; Sabatés, J.; Bahar-Fuchs, A. Cognition-oriented treatments for older adults: A systematic overview of systematic reviews. Neuropsychol. Rev. 2020, 30, 167–193. [Google Scholar] [CrossRef]
- Al Qasem, W.; Abubaker, M.; Kvašňák, E. Working Memory and Transcranial-Alternating Current Stimulation-State of the Art: Findings, Missing, and Challenges. Front. Psychol. 2022, 13, 822545. [Google Scholar] [CrossRef]
- Maggio, M.G.; De Bartolo, D.; Calabrò, R.S.; Ciancarelli, I.; Cerasa, A.; Tonin, P.; Di Iulio, F.; Paolucci, S.; Antonucci, G.; Morone, G.; et al. Computer-assisted cognitive rehabilitation in neurological patients: State-of-art and future perspectives. Front. Neurol. 2023, 14, 1255319. [Google Scholar] [CrossRef]
- Maggio, M.G.; Bonanno, M.; Manuli, A.; Onesta, M.P.; De Luca, R.; Quartarone, A.; Calabrò, R.S. Do Individuals with Spinal Cord Injury Benefit from Semi-Immersive Virtual Reality Cognitive Training? Preliminary Results from an Exploratory Study on an Underestimated Problem. Brain Sci. 2023, 13, 945. [Google Scholar] [CrossRef]
- Maggio, M.G.; Luca, A.; D’Agate, C.; Italia, M.; Calabrò, R.S.; Nicoletti, A. Feasibility and usability of a non-immersive virtual reality tele-cognitive app in cognitive rehabilitation of patients affected by Parkinson’s disease. Psychogeriatrics 2022, 22, 775–779. [Google Scholar] [CrossRef]
- Uygur-Kucukseymen, E.; Pacheco-Barrios, K.; Yuksel, B.; Gonzalez-Mego, P.; Soysal, A.; Fregni, F. Non-invasive brain stimulation on clinical symptoms in multiple sclerosis patients: A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2023, 78, 104927. [Google Scholar] [CrossRef]
- Maggio, M.G.; Stagnitti, M.C.; Calatozzo, P.; Formica, S.; Latella, D.; Manuli, A.; Avena, G.; Oddo, V.; Calabrò, R.S. Cognitive rehabilitation outcomes in patients with Multiple sclerosis: Preliminary data about the potential role of personality traits. Mult. Scler. Relat. Disord. 2022, 58, 103533. [Google Scholar] [CrossRef]
- Baykara, E.; Könen, T.; Unger, K.; Karbach, J. MRI predictors of cognitive training outcomes. J. Cogn. Enhanc. 2020, 5, 245–258. [Google Scholar] [CrossRef]
- Yhnell, E.; Furby, H.; Breen, R.S.; Brookes-Howell, L.C.; Drew, C.J.G.; Playle, R.; Watson, G.; Metzler-Baddeley, C.; Rosser, A.E.; Busse, M.E. Exploring computerised cognitive training as a therapeutic intervention for people with Huntington’s disease (CogTrainHD): Protocol for a randomised feasibility study. Pilot. Feasibility Stud. 2018, 4, 45. [Google Scholar] [CrossRef]
- Metzler-Baddeley, C.; Cantera, J.; Coulthard, E.; Rosser, A.; Jones, D.K.; Baddeley, R.J. Improved executive function and callosal white matter microstructure after rhythm exercise in Huntington’s disease. J. Huntingtons Dis. 2014, 3, 273–283. [Google Scholar] [CrossRef]
- Duff, K.; Paulsen, J.; Mills, J.; Beglinger, L.J.; Moser, D.J.; Smith, M.M.; Langbehn, D.; Stout, J.; Queller, S.; Harrington, D.L. Mild cognitive impairment in prediagnosed Huntington disease. Neurology 2010, 75, 500. [Google Scholar] [CrossRef] [PubMed]
- Julayanont, P.; McFarland, N.R.; Heilman, K.M. Mild cognitive impairment and dementia in motor manifest Huntington’s disease: Classification and prevalence. J. Neurol. Sci. 2020, 408, 116523. [Google Scholar] [CrossRef] [PubMed]
- Huynh, K.; Nategh, L.; Jamadar, S.; Stout, J.; Georgiou-Karistianis, N.; Lampit, A. Cognition-oriented treatments and physical exercise on cognitive function in Huntington’s disease: A systematic review. J. Neurol. 2023, 270, 1857–1879. [Google Scholar] [CrossRef] [PubMed]
- Simpson, J.A.; Lovecky, D.; Kogan, J.; Vetter, L.A.; Yohrling, G.J. Survey of the Huntington’s disease patient and caregiver community reveals most impactful symptoms and treatment needs. J. Huntingtons Dis. 2016, 15, 395–403. [Google Scholar] [CrossRef]
- Mueller, S.M.; Petersen, J.A.; Jung, H.H. Exercise in Huntington’s Disease: Current State and Clinical Significance. Tremor Other Hyperkinet. Mov. 2019, 9, 601. [Google Scholar] [CrossRef]
- Li, X.; Guo, R.; Wei, Z.; Jia, J.; Wei, C. Effectiveness of exercise programs on patients with dementia: A systematic review and meta-analysis of randomized controlled trials. BioMed Res. Int. 2019, 2019, 2308475. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).