Abstract
This study examined the changes in physical function and quality of life (QOL) of postoperative patients with pancreatic cancer for 3 months after surgery and examined the factors affecting the QOL at the 3 months after surgery. Methods: This study comprised 32 pancreatic cancer patients who underwent surgery at our hospital. Among these patients, 20 patients for whom data was measured before surgery to 3 months after surgery were selected for statistical analyses: 8 males and 12 females, 69.8 ± 7.4 years. The preoperative and postoperative rehabilitation was given to patients under the guidance of a physiotherapist. Nutritional status, body composition, physical function, gait assessments, and QOL were investigated. Results: Body weight, body fat mass, body fat percentage, body mass index (BMI), and muscle mass significantly decreased 3 months after surgery compared with their respective preoperative values. The mean grip strength at the time of 3 months after the surgery had decreased significantly from 27.3 kg to 24.5 kg. The mean skeletal muscle mass index (SMI) had decreased significantly from 6.3 kg before surgery to 5.9 kg after the surgery. The QOL scores for global health status, physical, and role showed significant decreases 2 weeks after surgery compared with the respective preoperative scores. Significant improvements in these scores were observed 3 months after surgery compared with the respective scores 2 weeks after surgery. Physical function assessments after surgery were associated with QOL 3 months after surgery. Conclusion: Recovery of patients after pancreatic cancer surgery in body weight, BMI, body fat percentage, body fat percentage, muscle mass, SMI, and grip strength was not sufficient at the time of 3 months after surgery. It has been observed that physical function of patients has affected the improvement of QOL.
1. Introduction
Pancreatic cancer is an aggressive malignancy and one of the leading causes of cancer-related death [1,2]. Although surgical resection is an effective treatment for pancreatic cancer, many patients experience recurrence after surgery [1,2].
Pancreatic cancer patients have experienced reduced physical function, such as loss of endurance and muscle strength [3]. Body weight loss and sarcopenia may also occur and are poor prognostic factors for postoperative patients with gastrointestinal cancer [4,5]. Pancreatic cancer survivors have been reported to experience reduced quality of life (QOL), including diminished physical and psychological well-being, compared with the survivors of other malignancies and individuals without cancer [6]. Treatment to maintain physical function and improve QOL is very important due to the poor prognosis of patients with pancreatic cancer [7].
In patients with esophagogastric cancer, physical function can also be significantly impaired during recovery, both pre-discharge [8] and 3 months post-surgery [9]. Few reports have examined changes in the physical functions of patients after pancreatic cancer surgery over time and the effects of physical function on QOL. Examining how physical function affects QOL in postoperative patients with pancreatic cancer can be useful for determining the need for interventions to improve QOL.
This study examined the changes in physical function and QOL of postoperative patients with pancreatic cancer for 3 months after surgery and examined the factors affecting the QOL at the 3 months after surgery.
2. Methods
2.1. Patients and Methods
This study comprised 32 pancreatic surgery patients who underwent surgery at our hospital between April 2018 and March 2020. Among these patients, 20 patients for whom data was measured before surgery to 3 months after surgery were selected for statistical analyses.
Patients fulfilling the following criteria were excluded: (1) Barthel index < 100 scores, (2) Revised Hasegawa Dementia Scale (HDS-R) ≤ 20 scores, (3) patients who were not available for evaluation before, 2 weeks, 1 month, and 3 months after surgery.
Nutritional status (albumin), body weight, body mass index (BMI), body fat mass, body fat percentage, muscle mass, skeletal muscle mass index (SMI), grip strength, muscle strength of the lower limb, one-leg standing time, gait, and QOL were investigated. Measurements were performed before the surgery and 2 weeks, 1 month, and 3 months after surgery.
2.2. Rehabilitation Program
The preoperative program consisted of muscle-strengthening exercises—squatting and calf raise exercises—and walking. The preoperative program was performed for 2 days before surgery. On postoperative day (POD) 1, sitting, standing, and walking still were started. On POD 4, muscle-strengthening exercises were started. On POD 7, aerobic exercise, stair climbing/descending and outdoor walking were performed, and physical activities were increased depending on the patient’s physical condition. In food textures, POD 4, controlled diet (rice gruel in three degree) was started. Starting POD 7 after the operation, the subjects of this study were allowed to consume a normal diet. The timing of mobilization changed according to the physical status of the patient for a few days.
Squatting and calf raise exercises were performed 20 times each using the patient’s own body weight. The preoperative and postoperative rehabilitation were 20 min per day. Exercise intensity for preoperative and postoperative rehabilitation were set at 3–5 points on the Borg’s Category-Ratio scale (Borg CR-10). The preoperative and postoperative were performed under the guidance of a physiotherapist.
At discharge, the physiotherapist instructed patients to perform the same rehabilitation performed during hospitalization at home. For meals as well, patients were instructed on the contents of meals after discharge, how to eat, and how to drink water.
2.3. Body Composition
BMI, body fat mass, body fat percentage, muscle mass, and SMI were measured by bioimpedance analysis using In Body S720 (In Body Japan Inc., Tokyo, Japan) [10]. The measurement was performed after 1 h or more after eating. SMI was evaluated by dividing the limb skeletal muscle mass (kg) by the square of the height (m2).
2.4. Physical Function
Handgrip strength was measured using a digital dynamometer (TTM, Inc., Tokyo, Japan), with the participant standing upright [11]. The patients had shoulder adducted and neutrally rotated, elbows fully extended, forearms and wrists in neutral position, and legs open to shoulder width. The patients needed to keep the dynamometer away from any part of the body.
To measure the muscle strength of the lower limb, the quadriceps muscle strength was measured using a hand-held dynamometer (ANIMA, μ-Tas F-01) [12]. Measurements were made with the patients sitting upright on a treatment bed, without back support, and with both upper extremities crossed in front of the trunk. Patients sat with the knee joint at 90-degree flexion. The sensor pad of the hand-held dynamometer was attached to the front of the distal crus. The sensor was fastened using Velcro placed just above the malleolus and the sensor pad was affixed to a belt connected to a pillar of the treatment bed. The patients were then asked to make a maximum isometric contraction of the quadriceps for 5 s. The recorded value (kgf) was divided by the patient’s body weight, and this value (kgf/kgf) was defined as the muscle strength of the lower limb.
For the one-leg standing time, the patients were asked to stand on one leg at a time, with their eyes open and both hands on their hips [13]. The measurement ended when the patients were no longer able to maintain balance and the suspended leg touched the floor, or the position of the supporting lower limb shifted. The one-leg standing time was measured using a stopwatch. The maximum achievable one-leg standing time was 60 s.
Grip strength, muscle strength of the lower limb, and one-leg standing time were measured twice on each side, and the maximum values were used.
2.5. Gait Assessments
For gait assessments, 5 m fast gait speed was measured [14]. The time required to walk the middle 5 m of a 7 m, indoor, flat surface was recorded. The patients were asked to walk as quickly and safely as possible without running. Patients performed the test twice, and the lowest time registered on stopwatch was considered for the study.
2.6. Quality of Life
The EORTC-QLQ-C30 is a questionnaire for QOL measure, designed for use in cancer patients. The QLQ-C30 includes a global health status item, five functional scales (physical, role, emotional, cognitive, and social), three symptom scales (fatigue, nausea or vomiting, and pain), and six single-item symptom measures (dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial difficulties) [15]. In this study, among the items offered in the QLQ-C30, the global health status item and the five functional scales (physical, role, emotional, cognitive, and social) were used.
2.7. Statistical Analysis
For pre- and postoperative comparisons of nutritional status body composition, physical function, gait assessment, and QOL, repeated-measures analysis of variance was applied to identity the differences among before, 2 weeks, 1 month, and 3 months after surgery, and then differences between periods of evaluation were compared with Tukey’s test. The Friedman test was administered to analyze differences among preoperative, 2 weeks, 1 month, and 3 months after surgery, and then the Wilcoxon signed-rank test with Bonferroni correction was applied. The choice of the repeated-measures analysis of variance or Friedman test was made according to the result of the Shapiro–Wilk normality test.
To assess which factors affect QOL 3 months after surgery, stepwise multiple regression analyses were performed, using the items from the QLQ-C30 (global health status, physical, role, emotional, cognitive, and social) as dependent variables and age, sex, albumin, weight, BMI, body fat mass, body fat percentage, muscle mass, SMI, grip strength, muscle strength of the lower limb, one-leg standing time, and gait assessment data from 3 months after surgery as the independent variables. SPSS software version 22.0 (IBM Corp., Armonk, NY, USA) was used to analyze the collected data. The significance level was set to p < 0.05 for repeated measures analysis of Variance and Friedman’s tests, and the Wilcoxon signed-rank results were used to adjust the p-values for multiple pairwise comparisons (p < 0.05/6 = 0.008, corrected for 6 pairwise comparisons) for the test after the Friedman’s tests.
3. Results
3.1. Socio-Demographic and Clinical Characteristics
Table 1 shows characteristics of the study patients. Operative procedures were pancreaticoduodenectomy in 3 patients, subtotal stomach-preserving pancreatoduodenectomy in 6 patients, pylorus-preserving pancreatoduodenectomy in 1 patient, and distal pancreatectomy with celiac axis resection in 10 patients. The mean volume bleeding during surgery was 803.8 ± 425.6 mL. The mean period of postoperative rehabilitation was 14.7 ± 5.8 days. No patients had exocrine pancreatic insufficiency. After discharge, no specific rehabilitation was given to patients at the hospital.

Table 1.
Characteristics of the study subjects.
3.2. Differences in Nutritional Status, Body Composition, Physical Function, and Gait Assessment before, Two Weeks, One Month, and Three Months after Surgery
The results of albumin, body composition, physical function, and gait assessment before, 2 weeks, 1 month, and 3 months after surgery are shown in Figure 1. Albumin was significantly reduced at 2 weeks and 1 month after surgery compared with preoperative albumin (p < 0.05). The level of albumin 2 weeks after surgery was significantly lower than 1 month and 3 months after surgery (p < 0.05). The level of albumin 3 months after surgery was significantly higher than 1 month after surgery (p < 0.05). Body weight was significantly reduced at 2 weeks, 1 month, and 3 months after surgery compared with preoperative body weight (p < 0.05). BMI also decreased significantly 2 weeks, 1 month, and 3 months after surgery compared with preoperative BMI (p < 0.05). BMI values at 1 month and 3 months after surgery were significantly lower than BMI at 2 weeks after surgery (p < 0.05). No significant difference was observed between BMI values at 1 and 3 months. Body fat mass was significantly reduced at 2 weeks, 1 month, and 3 months after surgery compared with preoperative values. Body fat percentage was significantly reduced at 1 month and 3 months after surgery compared with preoperative values. The level of body fat mass and body fat percentage 3 months after surgery were significantly lower than 2 weeks and 1 month after surgery (p < 0.05). Muscle mass, SMI, and grip strength showed significant decreases at 2 weeks, 1 month, and 3 months after surgery compared with the respective preoperative values (p < 0.05). Gait speed showed a significant deterioration at 2 weeks and 1 month after surgery compared with the value before surgery, and the gait at 3 months after surgery was significantly improved compared with the gait at 2 weeks after surgery (p < 0.05).
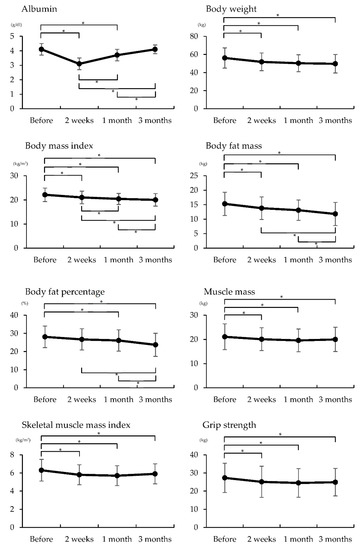
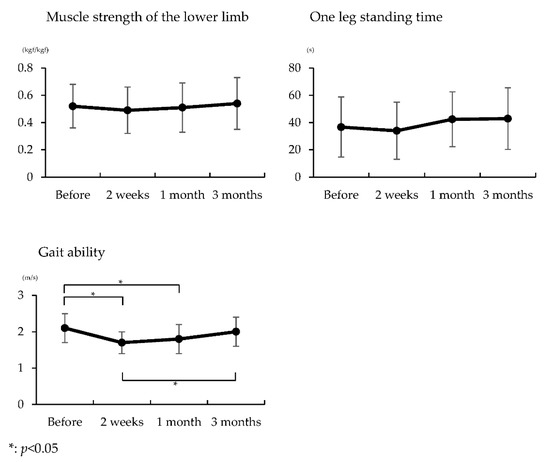
Figure 1.
Comparisons of body composition, physical function, and gait ability at before, two weeks, one month, and three months after surgery.
Three patients were diagnosed with sarcopenia at 3 months after surgery according to parameters by Cruz-Jentoft et al. (2019).
3.3. Differences in Quality of Life Scores before, Two Weeks, One Month, and Three Months after Surgery
The QLQ-C30 results before, 2 weeks, 1 month, and 3 months after surgery are shown in Figure 2. The global health status score showed a significant decrease at 2 weeks and 1 month after surgery compared with the preoperative score. The score at 3 months was significantly improved compared to the score at 2 weeks (p < 0.05). The QOL physical score showed a significant decrease at 2 weeks after surgery compared with the preoperative score. The score at 3 months was significantly improved compared with the value at 2 weeks (p < 0.05). The QOL role score showed a significant decrease at 2 weeks and 1 month after surgery compared with the preoperative score (p < 0.05). The score 3 months after surgery was significantly improved compared with the scores 2 weeks and 1 month after surgery (p < 0.05).
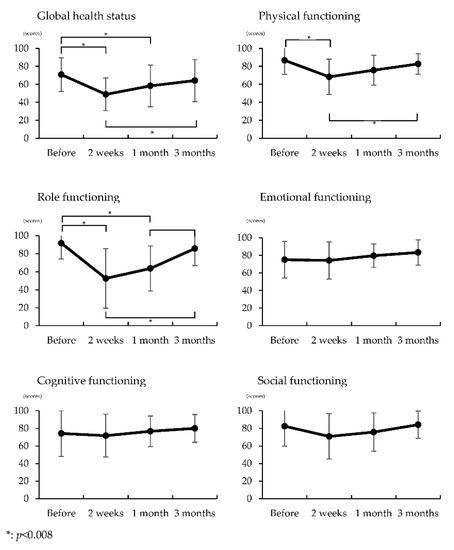
Figure 2.
Comparisons of quality of life at before, two weeks, one month, and three months after surgery.
3.4. Factors Predicting Quality of Life at Three Months after Surgery
Stepwise multiple regression analyses is shown in Table 2. The grip strength 3 months after surgery was associated with global health status score (p < 0.05, R2 = 0.322).

Table 2.
Factors predicting of QOL at three months after surgery.
4. Discussion
This study aimed to clarify the changes in physical function and QOL among postoperative patients with pancreatic cancer and determine the factors that affect QOL. The results showed that body composition and grip strength significantly decreased 3 months after the operation compared with the respective preoperative values. The QOL scores for global health status, physical, and role showed significant decreases 2 weeks after surgery compared with the respective preoperative scores, and significant improvements in these scores were observed 3 months after surgery compared with the respective scores 2 weeks after surgery. Physical function assessment after surgery was associated with QOL 3 months after surgery.
After pancreatic resection, patients showed significantly reduced cardiorespiratory fitness (VO2peak), functional capacity (6-min walking distance), and muscle strength compared with healthy controls [3]. Another study demonstrated that 6 months of progressive resistance training improved muscle strength [16]. A home walking program resulted in significant improvements in resected pancreas and periampullary cancer patients in terms of fatigue levels, physical function, and health-related QOL scores [17]. In this study, we promoted early mobilization after surgery and performed rehabilitation, such as muscle strengthening exercises and ADL exercises for an average of 15 days after surgery, while only the patient’s own self-training was performed after discharge. In this study, SMI and grip strength decreased significantly compared with the preoperative values, even 3 months after surgery. Sarcopenia is diagnosed based on the detection of low muscle mass and low muscle function (muscle strength or physical performance) [18], and sarcopenia has been significantly associated with poorer overall survival [19]. Three patients in this study were diagnosed with sarcopenia, and patients with sarcopenia may increase in the future. Additionally, decreased physical function can result in decreased ADL.
Body weight loss is associated with reduced physical function [19], lower QOL, reduced tolerance to anticancer therapy [4], and overall survival [5,20]. In this study, 4 days after the operation, controlled diet (rice gruel in three degree) was started. Additionally, starting 7 days after the operation, the subjects of this study were allowed to consume a normal diet and did not have any dietary restrictions. At the time of discharge, we provided nutritional guidance at home. In this study, body weight, body fat mass, body fat percentage, and BMI decreased significantly, even 3 months after surgery compared with their respective preoperative values. On the other hand, albumin showed improvement 3 months after the surgery. Reduction of Dietary intake of patients with pancreatic cancer is affected by the effects of surgery, it is considered that the lack of nutritional guidance after discharge have affected the results. Results of this study suggests that patients need continuous nutritional management even after discharge.
After pancreatic cancer surgery, patients have been reported to experience a significant decline in QOL 14 days after resection [21]. QOL 60 days after surgery was reported to be significantly worse than preoperative QOL, although emotional functioning was found to be significantly better after surgery than preoperatively [21]. In contrast, another study showed comparable QOL scores between measurements performed preoperative and measurements performed 3 and 6 months after surgery [22]. In this study, the global health status, physical, and role scores decreased 2 weeks after surgery and improved 3 months after surgery. Grip strength at 3 months after surgery was found to be factors affecting global health status QOL scores. The results of this study showed that patients with pancreatic cancer must actively perform postoperative rehabilitation.
Study Limitations
First, the number of subjects was small. Second, all subjects in this study underwent rehabilitation interventions and were not compared with a non-active control group. Third, the patient’s home exercise time, physical activity, and dietary status could not be evaluated after discharge. Fourth, we could not clarify the factors that affected emotional, cognitive, and social QOL scores. Further consideration of these factors remains necessary in the future.
5. Conclusions
This study aimed to clarify the changes in physical function and QOL among postoperative patients with pancreatic cancer and determine the factors that affect QOL.
Recovery of patients after pancreatic cancer surgery in body weight, body mass index, body fat percentage, body fat percentage, muscle mass, SMI, and grip strength was not sufficient at the time of 3 months after surgery. In conclusion, patients submitted to pancreatic cancer surgery observed after 3 months of recovery had no improvements in physical function or QOL. It was observed that that the physical function conditions contributed negatively to QOL
Author Contributions
Conceptualization, H.K. and Y.A.; Data curation, Y.A.; Formal analysis, H.K. and Y.A.; Investigation, H.K., R.T., M.O., M.K., M.H., Y.M., K.O. and S.S.; Methodology, H.K. and Y.A.; Project administration, H.K. and Y.A.; Supervision, Y.A., K.O and S.S.; Visualization, H.K.; Writing—original draft, H.K. and Y.A.; Writing—review & editing, Y.A., R.T., M.O., M.K., M.H., Y.M., K.O. and S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
All procedures performed in studies involving human participants were performed under an approved protocol and in accordance with the ethical standards of the Shikoku Cancer Center Ethics Committee (Approval No. 2018-93) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to Participant’s personal information.
Conflicts of Interest
The authors declare that they have no competing interests.
References
- Saad, A.M.; Turk, T.; Al-Husseini, M.J.; Abdel-Rahman, O. Trends in pancreatic adenocarcinoma incidence and mortality in the United States in the last four decades; a SEER-based study. BMC Cancer 2018, 18, 688. [Google Scholar] [CrossRef] [PubMed]
- Okumura, S.; Kaido, T.; Hamaguchi, Y.; Fujimoto, Y.; Masui, T.; Mizumoto, M.; Hammad, A.; Mori, A.; Takaori, K.; Uemoto, S. Impact of preoperative quality as well as quantity of skeletal muscle on survival after resection of pancreatic cancer. Surgery 2015, 157, 1088–1098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clauss, D.; Tjaden, C.; Hackert, T.; Schneider, L.; Ulrich, C.M.; Wiskemann, J.; Steindorf, K. Cardiorespiratory fitness and muscle strength in pancreatic cancer patients. Support. Care Cancer 2017, 25, 2797–2807. [Google Scholar] [CrossRef]
- Bachmann, J.; Heiligensetzer, M.; Krakowski-Roosen, H.; Büchler, M.W.; Friess, H.; Martignoni, M.E. Cachexia worsens prognosis in patients with resectable pancreatic cancer. J. Gastrointest. Surg. 2008, 12, 1193–1201. [Google Scholar] [CrossRef]
- Dewys, W.D.; Begg, C.; Lavin, P.T.; Band, P.R.; Bennett, J.M.; Bertino, J.R.; Cohen, M.H.; Douglass, H.O., Jr.; Engstrom, P.F.; Ezdinli, E.Z.; et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Am. J. Med. 1980, 69, 491–497. [Google Scholar] [CrossRef]
- Sun, V.; Ruel, N.; Chung, V.; Singh, G.; Leong, L.; Fakih, M.; Fong, Y.; Ferrell, B. Pilot study of an interdisciplinary supportive care planning intervention in pancreatic cancer. Support. Care Cancer 2016, 24, 3417–3424. [Google Scholar] [CrossRef] [Green Version]
- Cormie, P.; Spry, N.; Jasas, K.; Johansson, M.; Yusoff, I.F.; Newton, R.U.; Galvão, D.A. Exercise as medicine in the management of pancreatic cancer: A case study. Med. Sci. Sports Exerc. 2014, 46, 664–670. [Google Scholar] [CrossRef]
- Tatematsu, N.; Hasegawa, S.; Tanaka, E.; Sakai, Y.; Tsuboyama, T. Impact of oesophagectomy on physical fitness and health-related quality of life in patients with oesophageal cancer. Eur. J. Cancer Care 2013, 22, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, S.; Osugi, H.; Higashino, M.; Tokuhara, T.; Takada, N.; Takemura, M.; Lee, S.; Kinoshita, H. Comparison of three-field esophagectomy for esophageal cancer incorporating open or thoracoscopic thoracotomy. Surg. Endosc. 2003, 17, 1445–1450. [Google Scholar] [CrossRef]
- Sullivan, P.A.; Still, C.D.; Jamieson, S.T.; Dixon, C.B.; Irving, B.A.; Andreacci, J.L. Evaluation of multi-frequency bioelectrical impedance analysis for the assessment of body composition in individuals with obesity. Obes. Sci. Pract. 2018, 5, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Owashi, K.; Kanauchi, Y.; Mura, N.; Takahara, M.; Ogino, T. The short-term reliability of grip strength measurement and the effects of posture and grip span. J. Hand Surg. Am. 2005, 30, 603–609. [Google Scholar] [CrossRef]
- Hirano, M.; Katoh, M.; Gomi, M.; Arai, S. Validity and reliability of isometric knee extension muscle strength measurements using a belt-stabilized hand-held dynamometer: A comparison with the measurement using an isokinetic dynamometer in a sitting posture. J. Phys. Ther. Sci. 2020, 32, 120–124. [Google Scholar] [CrossRef] [Green Version]
- Kita, K.; Hujino, K.; Nasu, T.; Kawahara, K.; Sunami, Y. A simple protocol for preventing falls and fractures in elderly individuals with musculoskeletal disease. Osteoporos. Int. 2007, 18, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Van de Port, I.G.; Kwakkel, G.; Lindeman, E. Community ambulation in patients with chronic stroke: How is it related to gait speed? J. Rehabil. Med. 2008, 40, 23–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Wiskemann, J.; Clauss, D.; Tjaden, C.; Hackert, T.; Schneider, L.; Ulrich, C.M.; Steindorf, K. Progressive resistance training to impact physical fitness and body weight in pancreatic cancer patients: A randomized controlled trial. Pancreas 2019, 48, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Yeo, T.P.; Burrell, S.A.; Sauter, P.K.; Kennedy, E.P.; Lavu, H.; Leiby, B.E.; Yeo, C.J. A progressive postresection walking program significantly improves fatigue and health-related quality of life in pancreas and periampullary cancer patients. J. Am. Coll. Surg. 2012, 214, 463–475. [Google Scholar] [CrossRef] [Green Version]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moses, A.W.G.; Slater, C.; Preston, T.; Barber, M.D.; Fearon, K.C.H. Reduced total energy expenditure and physical activity in cachectic patients with pancreatic cancer can be modulated by an energy and protein dense oral supplement enriched with n-3 fatty acids. Br. J. Cancer 2004, 90, 996–1002. [Google Scholar] [CrossRef]
- Hendifar, A.E.; Chang, J.I.; Huang, B.Z.; Tuli, R.; Wu, B.U. Cachexia, and not obesity, prior to pancreatic cancer diagnosis worsens survival and is negated by chemotherapy. J. Gastrointest. Oncol. 2018, 9, 17–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eaton, A.A.; Gonen, M.; Karanicolas, P.; Jarnagin, W.R.; D’Angelica, M.I.; DeMatteo, R.; Kingham, T.P.; Allen, P.J. Health-Related Quality of Life After Pancreatectomy: Results from a Randomized Controlled Trial. Ann. Surg. Oncol. 2016, 23, 2137–2145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schniewind, B.; Bestmann, B.; Henne-Bruns, D.; Faendrich, F.; Kremer, B.; Kuechler, T. Quality of life after pancreaticoduodenectomy for ductal adenocarcinoma of the pancreatic head. Br. J. Surg. 2006, 93, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).