Abstract
Background: Low back pain (LBP) is a widespread and disabling condition affecting many older adults. Methods: This study aimed to establish correlations between LBP, physical activity, body composition, and posture in 114 women (mean age: 67.6 ± 5.68 years). Using a cross-sectional study design, LBP was assessed using the Oswestry Disability Index (ODI). Physical activity (PA) was measured using a pedometer to count the steps taken. Spinal curvatures in the sagittal plane were examined with a Rippstein Plurimeter. Results: Significant correlations were found between ODI and waist circumference (WC) (F(1, 113) = 7.574, p = 0.007), body mass index (BMI) (F(1, 113) = 11.660, p = 0.001), total fat (TF) (F(1, 113) = 8.806, p = 0.004, R2 = 0.072), and total steps (F(1, 113) = 4.446, p = 0.037). No associations were found between ODI and hip circumference (HC) (F(1, 113) = 6.257, p = 0.014, R2 = 0.52), waist-to-hip ratio (WHR) (F(1, 113) = 6.342, p = 0.013, R2 = 0.053), thoracic kyphosis (THK) (F(1, 113) = 0.290, p = 0.591, R2 = 0.003), or lumbar lordosis angle (LLA) (F(1, 113) = 0.290, p = 0.591, R2 = 0.003). Conclusion: These results of the study findings reveal the multifactorial nature of LBP syndrome and highlight the connection between LBP and ODI, BMI, WC, and TF in older women. Additionally, we emphasize the importance of implementing further prevention and intervention strategies to manage the clinical manifestation of LBP in the geriatric population. Healthcare providers can better support this population’s well-being by focusing on targeted interventions.
1. Introduction
The aging process is a complex phenomenon that occurs in humans, frequently associated with physiological, psychological, and biomechanical changes that impact quality of life [1].
Low back pain (LBP) is a widespread and disabling condition, with 60–70% of the population suffering at least one episode of LBP during their lifetime worldwide [2,3]. Clinically, it is characterized by mild to severe pain, primarily in the lower back. During acute episodes, LBP disrupts daily life activities and leads to prolonged absences from work [4], creating socio-economic challenges [5]. LBP affects more women than men and is generally defined as a non-specific self-limiting process [6]. Older women are particularly vulnerable to chronic LBP due to postmenopausal hormone changes, which also contribute to decreased bone mineral density [7] and consequently may contribute to functional limitation and musculoskeletal conditions [8].
The causes of LBP are complex and multifaceted, varying from minor muscle strain to a complex systemic issue. Primarily, this condition could arise from a biomechanical limitation, produced by trauma, muscle imbalances, or posture, which leads to intervertebral disk and articular facet overloading [9].
This situation is often amplified by increasing weight, age, and body composition (increase in body fat or sarcopenia). Consequently, this might lead to changes in the spine’s physiological sagittal curvatures, which further intensify LBP [10,11].
With aging, the vertebral column undergoes structural changes, including shortening (due to intervertebral disk dehydration), increased rigidity, and backward curvatures. These changes can lead to impaired function of internal organs, reduced physical activity, increased pain perception, and a decline in overall mood. Furthermore, many elderly individuals with chronic LBP may develop kinesiophobia [12]. Characterized by a fear–avoidant response to movement in an attempt to prevent pain, this behavior can significantly reduce physical activity and negatively impact body composition in patients with lower back pain (LBP) [13,14].
A lower level of physical activity in the elderly population also contributes to increasing adiposity [15]. Body composition is assessed with body mass index (BMI), which is widely used as a great indicator of nutritional status and health risk [16].
The World Health Organization (WHO, 2020) recommends that individuals aged 65 and older should engage in moderate-intensity aerobic activity for at least 150–300 min two or more days per week. All indications of the WHO are based on the central definition of physical activity, which is defined as any movement of the body in general or part of it, produced by the skeletal muscle, with energy expenditure required [17].
Previous research has suggested that physical activity and body composition may play important roles in developing and progressing lower back pain [13,18]. The factors that might lead to increased back pain include sedentary lifestyles. Low physical activity levels accelerate involution changes related to human aging and problems with the motor organs. Muscle strength decreases while body composition and posture change, resulting in disturbed balance in the spinal column, pelvis, and lower limbs, which can hurt locomotion and cause back pain [19]. Studies have also emphasized improper sitting position as an important risk factor of low back pain syndrome [20,21]. While alterations of thoracic and lumbar vertebrae have been linked to back pain in younger populations, the evidence in older adults is limited and inconsistent [22,23].
We initiate our study with the central question, “What are the relationships between low back pain intensity, body composition, physical activity, and spinal posture in older women?” This study aimed to establish the correlations between low back pain and physical activity in relation to specific body composition and posture in women aged 60 years and older. By highlighting these connections, this study underscores the need for effective intervention strategies in geriatric healthcare that could enhance their quality of life.
2. Materials and Methods
2.1. Participants
This study utilized a cross-sectional study design to examine 114 retired women, aged 60 to 80 years (67.6 ± 5.68 years). They were participants in the Third Age University programs and were living in an urban area with over 100,000 people. Data were collected at a single point in time. The purposive sampling method was used to recruit study participants while applying the following inclusion criteria: age over 60 years, written consent to participate in this study, and successful completion of the test using pedometers. The exclusion criteria were comorbidities and functional limitation conditions. Informed consent was obtained from all subjects involved in this study.
The research protocol was approved by the Bioethics Committee at the Jerzy Kukuczka Academy of Physical Education in Katowice, Poland (No. 9 with addendum 29.10.2020) and met the ethical standards of the Declaration of Helsinki, 2013 [24].
2.2. Subjects’ Assessment
The examinations were performed using direct participant observation and a face-to-face diagnostic survey.
The Oswestry Disability Index (ODI) was used to assess low back pain. The questionnaire consisted of ten topics, with the maximum score being 50. The scale was used to quantify disability, and 0–4 indicated no disability, 5–14 indicated minimal disability, 15–24 indicated moderate disability, 25–34 indicated severe disability, and, finally, >35 indicated total disability [25].
Physical activity was evaluated using the objective device to count the number of steps (pedometer, Yamax Inc., Tokyo, Japan). Daily step count was consecutively recorded for 7 days (standards as presented by Tudor-Locke [26]).
Sagittal spinal curvatures were examined using the Rippstein plurimeter to measure the angles of the thoracic (THK) and lumbar (Ll) spine [27]. The Rippstein plurimeter is a tool used to evaluate the ranges of sagittal spine mobility. The result was represented by the two values of angular inclination, which were directly read from the device. Thoracic kyphosis angle (THK) was measured between TH1 (1st thoracic vertebra) and TH12 (12th thoracic vertebra), whereas lumbar lordosis angle (LLA) was measured between L5 (5th lumbar vertebra) and TH12 [28].
The anthropometric parameters were obtained by measuring body height (BH), waist circumference (WC), and hip circumference (HC). BH was measured with a portable stadiometer (Seca 213, Germany) following the procedure proposed by the National Health and Nutrition Examination Survey (NHANES) Anthropometry Procedures Manual [29], while WC and HC data were collected after applying the WHO STEP protocol [30]. A low-frequency bioelectrical impedance method (Tanita TBF-300M) was utilized to evaluate body mass (BM) and body fat percentage (FAT%). Body mass index (BMI in kg/m2) and waist-to-hip ratio (WHR) were calculated [31] (Table 1).

Table 1.
Characteristics of the physical status of the study participants.
2.3. Statistical Analysis
This study utilized a cross-sectional study design to examine 114 women aged 60 to 80 (67.6 ± 5.68 years) who were retired and participants of the Third Age University programs living in an urban agglomeration with over 100,000 people. Data were collected at a single point in time.
The data were analyzed using IBS SPSS Statistics, V.25.
The minimum sample size of 89 participants was determined based on an a priori analysis using G*Power software (version 3.1.9.4, from the University of Dusseldorf, Germany). The analysis was conducted with the following parameters (effect size: 0.15, α = 0.05, β = 0.95, number of predictors = 1).
The normality assumption of the data was checked using the Kolmogorov–Smirnov test, and it was observed that the data did not meet the normality assumption. After the analysis, we decided to use linear regression for data analysis, since it does not require variables to be normally distributed. The results of the analysis are presented in Table 2.

Table 2.
The Oswestry Disability Index and outcome variables.
3. Results
A linear regression analysis demonstrated a significant relationship between ODI and WC (F(1, 113) = 7.574, p = 0.007). However, the R2 value of 0.063 indicates that ODI explains only 6.3% of the variability in WC.
The ODI did not significantly correlate with HC (F(1, 113) = 6.257, p = 0.014, R2 = 0.52) or WHR (F(1, 113) = 6.342, p = 0.013, R2 = 0.053). A significant relationship was observed between ODI and BMI (F(1, 113) = 11.660, p = 0.001). The R2 value of 0.094 indicates a medium effect size of ODI on BMI (Figure 1).
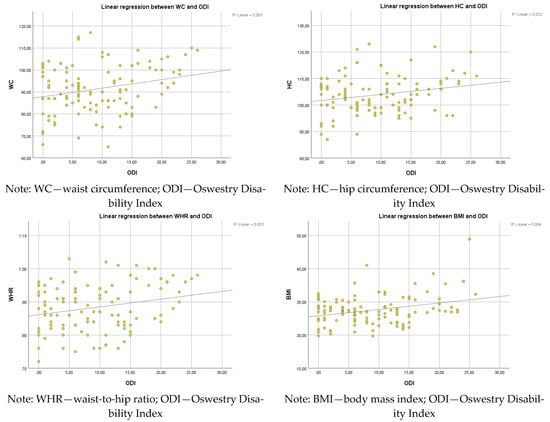
Figure 1.
Linear regression between ODI and WC, HC, WHR, and BMI.
A significant regression was found between ODI and FAT (F(1, 113) = 8.806, p = 0.004, R2 = 0.072), indicating that ODI explained approximately 7.2% of the variance in FAT.
A significant regression was found between ODI and total steps (F(1, 113) = 4.446, p = 0.037). The R2 was 0.038, indicating that ODI explained approximately 3.8% of the variance in total steps.
Further analysis indicated no significant relationship between ODI and thoracic kyphosis (F(1, 113) = 0.290, p = 0.591, R2 = 0.003) or lumbar lordosis (F(1, 113) = 0.290, p = 0.591, R2 = 0.003). The very low R2 values indicate that ODI has no meaningful explanatory power for these spinal curvature parameters in the studied population (Figure 2).
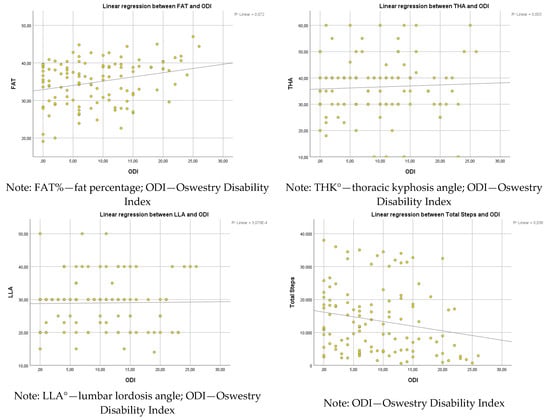
Figure 2.
Linear regression between ODI and FAT, THK, LLA, and total steps.
4. Discussion
LBP syndrome is considered an important factor in limiting people’s everyday activity, and its incidence is permanently increasing [32], especially in the geriatric population, where we can see changes in body posture and body composition [33].
While our regression analysis indicates that the ODI did not significantly affect the subjects’ THK (F(1, 113) = 0.290, p = 0.591, R2 = 0.003) or LLA (F(1, 113) = 0.290, p = 0.591, R2 = 0.003), previous studies found that postural changes occur in the elderly population. Anwajler demonstrated that THK depth gradually increased with age in the 6th, 7th, and 8th decades of life since the aging process leads to the modification of the body posture due to changes in active body-stabilizing muscles’ activity [34]. With aging, muscle strength is reduced, leading to changes in body posture. As a natural consequence, this imbalance is compensated for by an anterior shift of the center of gravity and an increase in the spine curvatures. Singh also found a significant increase in THK in older women, but no significant changes were made in the case of lumbar lordosis [35,36]. Some authors found that an increased THK affected disability, a more significant number of falls due to the shifted center of gravity [37,38,39,40], and deteriorated quality of life [41]. This adverse increase in THK observed with age more often affected female patients [42]. Changes in body posture may increase LBP, causing functional difficulties and affecting quality of life [43]. The relationship between lumbar lordotic curvature and LBP remains controversial. Even though the traditional perspective is associated with increased lordosis, current research found that a decreased LLA has a potential role as a contributing factor of LBP [44].
Age-related vertebral changes are well documented and form the basis of both clinical understanding and biomechanical models of postural adaptation. Chronic low back pain affects the somatosensory integration of the inputs received from the proprioception signaling of the lumbar region. Further, the central processing is affected, and consequently, dysfunctional motor control adaptation appears [45]. Perturbation of the trunk control can also increase mechanical loading on the vertebral tissues [46]. According to Panjabi’s model of spinal stability, failure of the interplay of osteo-ligamentous spinal structure, active structure, and control systems can make the vertebral column unstable [47]. In elderly individuals, all these components are affected by the degenerative process, contributing to the modification of thoracic and lumbar curvature [48,49].
Although postural variables (THK and LLA) were not statistically significant in the analysis, we considered it relevant to keep and discuss them due to the important clinical implications they may have in the geriatric population. Thus, integrating these variables into the analysis contributes to a more comprehensive understanding of the biomechanical and functional context of low back pain among older people.
Another biological factor that could be associated with non-specific LBP is insufficient strength and endurance of the muscles. In chronic cases, LBP is more related to biological deconditioning, which includes the musculoskeletal system and physiological or cardiovascular aspects [50]. According to clinicians, LBP syndromes create discomfort, limitations of activity in everyday life, and, consequently, modification in body composition.
The results of this study demonstrated an association between PA, characteristics of body composition, and the incidence of disability defined by LBP. We observed statistically significant correlations between the scores of the ODI and WC (R2 = 0.063, p = 0.007), HC (R2 = 0.052, p = 0.014), WHR (R2 = 0.053, p < 0.05), BMI (R2 = 0.094, p = 0.001), and TF (R2 = 0.072, p = 0.004). Our empirical results are consistent with the conclusions of many authors [10,11,13,14]. However, each of these studies identifies only one of the factors as significantly related to ODI (physique, attitude, exercise, or condition). We conducted an analysis of four complementary factors that might affect the ODI (body composition, build, posture, and physical activity) in a specific group of older women.
Given the specific nature of the subjects that we had in this research (active, elderly women), the transposition of the results obtained to the general population may not be totally objective. Several important factors were not addressed in this paper and might deserve further analysis in future research. These factors are gender differences [51], cultural environment [52], cognitive health [53], and psychological factors [54]. However, analyzing the results obtained in our research, in which ODI, WC, HC, WHR, BMI, and TF were correlated with low back pain, with caution, we can state that people that are sedentary and have worse physical status may exhibit greater lower back pain.
The linear regression analysis demonstrated a weak relationship between ODI and WC (F(1, 113) = 7.574, p = 0.007). However, the R2 value of 0.063 indicates that ODI explains only 6.3% of the variability in WC. The ODI did not significantly correlate with HC (F(1, 113) = 6.257, p = 0.014, R2 = 0.52) or WHR (F(1, 113) = 6.342, p = 0.013, R2 = 0.053). The outcomes from the study of You et al. [55] suggest that subjects with an increased WHR are susceptible to developing LBP. Trujillo et al. [56] confirms that in a large study sample, the subjects with greater hip and WC experienced severe pain.
A weak relationship was observed between ODI and BMI (F(1, 113) = 11.660, p = 0.001). The R2 value of 0.094 indicates a medium effect size of ODI on BMI. Mintarjo [36] identified being overweight as a potential risk factor for degenerative disc pathologies in a similar study design. The study results indicate that BMI significantly affects LBP, with a chi-squared test value of 0.015 (p < 0.05). Furthermore, the findings reveal that subjects with an increased BMI are 6.089 times more likely to develop LBP.
A weak regression was found between ODI and TF (F(1, 113) = 8.806, p = 0.004, R2 = 0.072), indicating that ODI explained approximately 7.2% of the variance in TF. The correlation between LBP and body composition is well-documented. You et al. [35] suggest that an augment of 20% in body fat mass increases the risk of LBP. Also, Glänzel et al. [57] demonstrated that in rural workers with LBP, the sample group showed body composition deviation.
However, the results of the study were not wholly consistent with the statement that spinal curvatures are a determinant of self-reported disability. Perhaps the causes of disability include the feedback between obesity and low levels of physical activity. With these two variables, sedentary lifestyles and the respective sedentary body position are conducive to the involution of body posture and increased kyphosis. Therefore, the prevention of back pain should be supported by conscious and purposive activity aimed at compensating for motor deficits to change the habitual position of individual body segments. Adequately chosen specific or directional movements are recommended when the patient already suffers from pain syndrome, whereas general fitness exercises play a preventive role. The European Commission recommends such activities in their guidelines for acute and chronic LBP syndromes (Working Group B13 European Cooperation in the Field of Scientific and Technical Research—COST) [58].
Study limitations
Although this study aimed to identify the relationships and impacts of specific selected variables among older women, an important focus should be determining cause-and-effect relationships. Therefore, we recommend further research that explicitly aims to identify these causes. Also, future studies should consider a more comprehensive assessment of the potential confounding factors of the elderly population, which we consider a limitation of our study. Even though we made efforts to standardize data collection and minimize bias, factors such as hormonal changes, bone density, muscle strength, previous injuries, or lifestyle factors may introduce variability that could affect the observed associations. The last point is about the low R2 values that indicate limited explanatory power of the regression models, which may reduce the generalizability of the results.
5. Conclusions
This study did not establish a direct correlation between low back pain syndromes and spinal curvatures in the sagittal plane. Only these three factors (PA, body build, and body composition), in conjunction with age, contributed to a statistically significant risk of experiencing pain. To address these issues, educational initiatives should be implemented for older adults. These programs should promote specific, purposeful, and tailored physical activities to enhance health, encourage ergonomic lifestyles, and help maintain proper body posture during work and leisure activities. Preventive measures should also focus on avoiding static body positions, managing weight, and teaching correct techniques for lifting and moving heavy objects.
Author Contributions
Conceptualization, B.R., D.I.A. and A.Z.; data curation, B.R., E.A.P. and B.A.A.; formal analysis, B.R., E.A.P. and B.A.A.; funding acquisition, D.I.A., E.A.P., I.M. and B.A.A.; investigation, B.R., K.G. and A.Z.; methodology, B.R. and A.Z.; project administration, B.R., D.I.A. and A.Z.; resources, D.I.A., K.G., E.A.P., I.M. and A.Z.; software, B.R., B.A.A. and A.Z.; supervision, D.I.A.; validation, D.I.A., K.G., E.A.P., I.M., B.A.A. and A.Z.; visualization, K.G., E.A.P., I.M. and B.A.A.; writing—original draft, B.R. and A.Z.; writing—review and editing, B.R., D.I.A., K.G., E.A.P., I.M. and A.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The research protocol was approved on 29 October 2020 by the Bioethics Committee at the Jerzy Kukuczka Academy of Physical Education in Katowice, Poland (No. 9 with addendum 29.10.2020) and met the ethical standards of the Declaration of Helsinki, 2013.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The original contributions presented in this study are included in this article; further inquiries can be directed to the corresponding author. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Acknowledgments
A great thank you to all collaborators and subjects for their availability and contribution to this study. D.I.A., E.A.P., and B.A.A. thank the “Vasile Alecsandri” University in Bacău, Romania, for the support and assistance provided.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Andreassen, S.N.; Ben Ezra, M.; Scheibye-Knudsen, M. A defined human aging phenome. Aging 2019, 11, 5786–5806. [Google Scholar] [CrossRef] [PubMed]
- Kędra, A.; Kolwicz-Gańko, A.; Kędra, P.; Bochenek, A.; Czaprowski, D. Back pain in physically inactive students compared to physical education students with a high and average level of physical activity studying in Poland. BMC Musculoskelet. Disord. 2017, 18, 501. [Google Scholar] [CrossRef] [PubMed]
- Antohe, B.A.; Uysal, H.Ş.; Panaet, A.E.; Iacob, G.S.; Rață, M. The Relationship between Magnetic Resonance Imaging and Functional Tests Assessment in Patients with Lumbar Disk Hernia. Healthcare 2023, 11, 2669. [Google Scholar] [CrossRef] [PubMed]
- Chou, L.; Cicuttini, F.M.; Urquhart, D.M.; Anthony, S.N.; Sullivan, K.; Seneviwickrama, M.; Briggs, A.M.; Wluka, A.E. People with low back pain perceive need for non-biomedical services in workplace, financial, social and household domains: A systematic review. J. Physiother. 2018, 64, 74–83. [Google Scholar] [CrossRef]
- Zhou, T.; Salman, D.; McGregor, A.H. Recent clinical practice guidelines for the management of low back pain: A global comparison. BMC Musculoskelet. Disord. 2024, 25, 344. [Google Scholar] [CrossRef]
- Duncan, R.A.; Hewson, G.C. Back pain in children: Dig a bit deeper. Eur. J. Emerg. Med. 2005, 12, 317–319. [Google Scholar] [CrossRef]
- Mahajan, A.; Patni, R.; Verma, S. Low Back Pain and Menopause. J. Mid-Life Health 2019, 4, 163–164. [Google Scholar] [CrossRef]
- Johannesdottir, F.; Allaire, B.; Anderson, D.E.; Samelson, E.J.; Kiel, D.P.; Bouxsein, M.L. Population-based study of age- and sex-related differences in muscle density and size in thoracic and lumbar spine: The Framingham study. Osteoporos. Int. 2018, 29, 1569–1580. [Google Scholar] [CrossRef]
- Bizzoca, D.; Solarino, G.; Pulcrano, A.; Brunetti, G.; Moretti, A.M.; Moretti, L.; Piazzolla, A.; Moretti, B. Gender-Related Issues in the Management of Low-Back Pain: A Current Concepts Review. Clin. Pract. 2023, 13, 1360–1368. [Google Scholar] [CrossRef]
- Tuz, J.; Maszczyk, A.; Zwierzchowska, A. The use of characteristics and indicators of body construction as predictors in the identification of the angle values of the physiological curves of the spine in sequential objective testing—mathematical models. Balt. J. Health Phys. Act. 2023, 15, 2. [Google Scholar] [CrossRef]
- Hira, K.; Nagata, K.; Hashizume, H.; Asai, Y.; Oka, H.; Tsutsui, S.; Takami, M.; Iwasaki, H.; Muraki, S.; Akune, T.; et al. Relationship of sagittal spinal alignment with low back pain and physical performance in the general population. Sci. Rep. 2021, 11, 20604. [Google Scholar] [CrossRef] [PubMed]
- Comachio, J.; Magalhães, M.O.; de Moura Campos Carvalho e Silva, A.P.; Marques, A.P. A cross-sectional study of associations between kinesiophobia, pain, disability, and quality of life in patients with chronic low back pain. Adv. Rheumatol. 2018, 58, 8. [Google Scholar] [CrossRef] [PubMed]
- Malewar, M.R.; Shah, K.D. Correlation between Pain, Kinesiophobia and Physical Activity Level in Patients with Chronic Low Back Pain Aged between 30 to 50 Years. Int. J. Sci. Healthc. Res. 2021, 6, 359–365. [Google Scholar] [CrossRef]
- Baek, S.; Park, H.-W.; Kim, G. Associations Between Trunk Muscle/Fat Composition, Narrowing Lumbar Disc Space, and Low Back Pain in Middle-Aged Farmers: A Cross-Sectional Study. Ann. Rehabil. Med. 2022, 46, 122–132. [Google Scholar] [CrossRef]
- Zhan, Y.; Liu, X. Effects of physical activity and sedentary behaviors on cardiovascular disease and the risk of all-cause mortality in overweight or obese middle-aged and older adults. Front. Public Health 2024, 12, 1302783. [Google Scholar] [CrossRef]
- Cleven, L.; Syrjanen, J.A.; Geda, Y.E.; Christenson, L.R.; Petersen, R.C.; Vassilaki, M.; Woll, A.; Krell-Roesch, J. Association between physical activity and longitudinal change in body mass index in middle-aged and older adults. BMC Public Health 2023, 23, 202. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 19 April 2025).
- Boutevillain, L.; Dupeyron, A.; Rouch, C.; Richard, E.; Coudeyre, E. Facilitators and barriers to physical activity in people with chronic low back pain: A qualitative study. PLoS ONE 2017, 12, e0179826. [Google Scholar] [CrossRef]
- Mziray, M.; Żuralska, R.; Gaworska-Krzemińska, A.; Domagała, P.; Kosińska, T.; Postrożny, D. Analysis of selected health problems of elderly patients. Nurs. Probl. Probl. Pielęgniarstwa 2014, 22, 62–67. [Google Scholar]
- Linton, S.J. A review of psychological risk factors in back and neck pain. Spine 2000, 25, 1148–1156. [Google Scholar] [CrossRef]
- Pincus, T.; Burton, A.K.; Vogel, S.; Field, A.P. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 2002, 27, E109–E120. [Google Scholar] [CrossRef]
- Patel, K.V.; Guralnik, J.M.; Dansie, E.J.; Turk, D.C. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain 2013, 154, 2649–2657. [Google Scholar] [CrossRef]
- Rodrigues, C.P.; Silva, R.A.; Nasrala Neto, E.; Andraus, R.A.C.; Fernandes, M.T.P.; Fernandes, K.B.P. Analysis of Functional Capacity in Individuals with and Without Chronic Lower Back Pain. Acta Ortop. Bras. 2017, 25, 143–146. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. 2013. Available online: https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/ (accessed on 12 March 2025).
- Fairbank, J.C.; Couper, J.; Davies, J.B.; O’Brien, J.P. The Oswestry low back pain disability questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar] [PubMed]
- Tudor-Locke, C.; Craig, C.L.; Thyfault, J.P.; Spence, J.C. A step-defined sedentary lifestyle index: <5000 steps/day. Appl. Physiol. Nutr. Metab. 2013, 38, 100–114. [Google Scholar] [CrossRef] [PubMed]
- Dobosiewicz, K. Nonspecific back pain in children and adolescents—Biomechanical, neurophysiological, and psychosocial factors. Neurol. Dziec. 2006, 30, 51–57. [Google Scholar]
- Zwierzchowska, A.; Tuz, J. Evaluation of the impact of sagittal curvatures on musculoskeletal disorders in young people. Med. Pract. 2018, 69, 29–36. [Google Scholar]
- Centers for Disease Control and Prevention. NHANES Anthropometry Procedures Manual 2019–2020; National Center for Health Statistics: Hyattsville, MD, USA, 2020; p. 11. [Google Scholar]
- World Health Organization. Waist Circumference and Waist–Hip Ratio: Report of a WHO Expert Consultation; WHO Press: Geneva, Switzerland, 2008; Available online: https://www.who.int/publications/i/item/9789241501491 (accessed on 12 March 2025).
- Zwierzchowska, A.; Kantyka, J.; Rosołek, B.; Nawrat-Szołtysik, A.; Małecki, A. Sensitivity and Specificity of Anthropometric Indices in Identifying Obesity in Women over 40 Years of Age and Their Variability in Subsequent Decades of Life. Biology 2022, 11, 1804. [Google Scholar] [CrossRef]
- Hoogendoorn, W.E.; Bongers, P.M.; de Vet, H.C.W.; Douwes, M.; Koes, B.W.; Miedema, M.C.; Ariëns, G.A.M.; Bouter, L.M. Flexion and Rotation of the Trunk and Lifting at Work Are Risk Factors for Low Back Pain. Spine 2000, 25, 3087–3092. [Google Scholar] [CrossRef]
- Drzał-Grabiec, J.; Snela, S.; Rykała, J.; Podgórska, J.; Banaś, A. Changes in the body posture of women occurring with age. BMC Geriatr. 2013, 13, 108. [Google Scholar] [CrossRef]
- Anwajler, J.; Barczyk, K.; Wojna, D.; Ostrowska, B.; Skolimowski, T. Characteristics of body posture in the sagittal plane in elderly residents of nursing homes. Gerontol. Pol. 2010, 3, 134–139. [Google Scholar]
- Singh, D.K.; Bailey, M.; Lee, R. Biplanar Measurement of Thoracolumbar Curvature in Older Adults Using an Electromagnetic Tracking Device. Arch. Phys. Med. Rehabil. 2010, 91, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Kado, D.M. The rehabilitation of hyperkyphotic posture in the elderly. Eur. J. Phys. Rehabil. Med. 2009, 45, 583–593. [Google Scholar] [PubMed]
- Kado, D.M.; Huang, M.H.; Barrett-Connor, E.; Greendale, G.A. Hyperkyphotic Posture and Poor Physical Functional Ability in Older Community-Dwelling Men and Women: The Rancho Bernardo Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2005, 60, 633–637. [Google Scholar] [CrossRef]
- Kado, D.M.; Huang, M.H.; Nguyen, C.B.; Barrett-Connor, E.; Greendale, G.A. Hyperkyphotic posture and risk of injurious falls in older persons: The Rancho Bernardo Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2007, 62, 652–657. [Google Scholar] [CrossRef]
- Hirose, D.; Ishida, K.; Nagano, Y.; Takahashi, T.; Yamamoto, H. Posture of the trunk in the sagittal plane is associated with gait in community-dwelling elderly population. Clin. Biomech. 2004, 19, 57–63. [Google Scholar] [CrossRef]
- Sinaki, M.; Brey, R.H.; Hughes, C.A.; Larson, D.R.; Kaufman, K.R. Balance disorder and increased risk of falls in osteoporosis and kyphosis: Significance of kyphotic posture and muscle strength. Osteoporos. Int. 2005, 16, 1004–1010. [Google Scholar] [CrossRef]
- Takahashi, T.; Ishida, K.; Hirose, D.; Nagano, Y.; Okumiya, K.; Nishinaga, M.; Matsubayashi, K.; Doi, Y.; Tani, T.; Yamamoto, H. Trunk deformity is associated with a reduction in outdoor activities of daily living and life satisfaction in community-dwelling older people. Osteoporos. Int. 2005, 16, 273–279. [Google Scholar] [CrossRef]
- Kado, D.M.; Huang, M.H.; Karlamangla, A.S.; Barrett-Connor, E.; Greendale, G.A. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: A prospective study. J. Am. Geriatr. Soc. 2004, 52, 1662–1667. [Google Scholar] [CrossRef]
- Leveille, S.G.; Guralnik, J.M.; Hochberg, M.; Hirsch, R.; Ferrucci, L.; Langlois, J.; Rantanen, T.; Ling, S. Low Back Pain and Disability in Older Women: Independent Association with Difficulty but Not Inability to Perform Daily Activities. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1999, 54, M487–M493. [Google Scholar] [CrossRef]
- Bozorgmehr, A.; Zahednejad, S.; Salehi, R.; Ansar, N.N.; Abbasi, S.; Mohsenifar, H.; Villafañe, J.H. Relationships between muscular impairments, pain, and disability in patients with chronic nonspecific low back pain: A cross-sectional study. J. Exerc. Rehabil. 2018, 14, 1041–1047. [Google Scholar] [CrossRef]
- Meier, M.L.; Vrana, A.; Schweinhardt, P. Low back pain: The potential contribution of supraspinal motor control and proprioception. Neuroscientist 2019, 6, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Van Dieën, J.H.; Reeves, N.P.; Kawchuk, G.; van Dillen, L.; Hodges, P.W. Motor control changes in low-back pain: Divergence in presentations and mechanisms. J. Orthop. Sports Phys. Ther. 2019, 49, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Willigenburg, N.W.; Kingma, I.; Hoozemans, M.J.M.; van Dieën, J.H. Precision control of trunk movement in low back pain patients. Hum. Mov. Sci. 2013, 1, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Michalska, J.; Kamieniarz, A.; Sobota, G.; Stania, M.; Juras, G.; Słomka, K.J. Age-related changes in postural control in older women: Transitional tasks in step initiation. BMC Geriatr. 2021, 21, 17. [Google Scholar] [CrossRef]
- Heidsieck, C.; Gajny, L.; Travert, C.; Lazennec, J.Y.; Skalli, W. Effect of postural alignment alteration with age on vertebral strength. Osteoporos. Int. 2022, 33, 443–451. [Google Scholar] [CrossRef]
- Roren, A.; Daste, C.; Coleman, M.; Rannou, F.; Freyssenet, D.; Moro, C.; Lefèvre-Colau, M.-M.; Nguyen, C. Physical activity and low back pain: A critical narrative review. Ann. Phys. Rehabil. Med. 2023, 66, 101650. [Google Scholar] [CrossRef]
- Gorini, S.; Camajani, E.; Cava, E.; Feraco, A.; Armani, A.; Amoah, I.; Filardi, T.; Wu, X.; Strollo, R.; Caprio, M.; et al. Gender differences in eating habits and sports preferences across age groups: A cross-sectional study. J. Transl. Med. 2025, 23, 312. [Google Scholar] [CrossRef]
- Carella, M.; Misuraca, R. Gender Differences and Physical Limitations in the Association Between Subjective Well-Being and Cultural Consumption Among Older People. J. Happiness Stud. 2025, 26, 38. [Google Scholar] [CrossRef]
- Passarello, N.; Troisi Lopez, E.; Gigliotta, O.; Turriziani, P.; Lucidi, F.; Mandolesi, L. Can an active lifestyle maintain cognitive efficiency in older adults? A pilot study of the relationship between physical activity and graphic fluency. BMC Psychol. 2025, 13, 312. [Google Scholar] [CrossRef]
- Cunningham, C.; O’ Sullivan, R.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports 2020, 30, 816–827. [Google Scholar] [CrossRef]
- You, Q.; Jiang, Q.; Li, D.; Wang, T.; Wang, S.; Cao, S. Waist circumference, waist-hip ratio, body fat rate, total body fat mass and risk of low back pain: A systematic review and meta-analysis. Eur. Spine J. 2021, 31, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Trujillo, F.A.; Thomas, H.A.; Berwal, D.; Rajulapati, N.; DiMarzio, M.; Pilitsis, J.G. Hip and waist circumference correlations with demographic factors and pain intensity in patients with chronic pain. Pain Manag. 2024, 14, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Mintarjo, J.A. Overweight BMI as a Risk Factor for Low Back Pain: An Observational Study from Primary Health Care. Int. J. Res. Rev. 2024, 11, 337–339. [Google Scholar] [CrossRef]
- Airaksinen, O.; Brox, J.I.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.; Mannion, A.F.; Reis, S.; Staal, J.B.; Ursin, H.; et al. Chapter 4 European guidelines for the management of chronic nonspecific low back pain. Eur. Spine J. 2006, 15 (Suppl. 2), s192–s300. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).