Abstract
Background/Objectives: The aging population has increased the demand for home modifications to support aging in place. However, existing research primarily focuses on fall prevention and physical safety, leaving gaps in understanding long-term sustainability, social engagement, and cost-effectiveness. Additionally, the interaction between home modifications and health-related changes remains under-explored. This study systematically reviews home modifications, addressing these gaps by considering functional independence, quality of life, caregiving burden, and technological advancements. Methods: A systematic review was conducted following PRISMA 2020 guidelines. One researcher and an external expert performed study selection, data extraction, and quality assessment. Thematic analysis and narrative synthesis were applied to compare study results. Results: Among 20 studies, 13 (65%) confirmed the effectiveness of home modifications in fall prevention, functional independence, and cost savings. Seven studies (35%) highlighted housing accessibility and lifestyle factors. However, few studies examined personalized interventions, smart home technologies, and long-term adaptability. Conclusions: This study emphasizes the need for personalized, technology-driven, and long-term adaptable home modifications. Future research should explore smart home innovations, interdisciplinary approaches, and policy implementation feasibility to develop sustainable aging-in-place strategies. By adopting a holistic perspective, this study provides a new framework for advancing aging-in-place strategies.
1. Introduction
The rapid progression of global aging has heightened interest in the living arrangements and residential environments of older adults [1]. According to the United Nations, the proportion of individuals aged 65 and older worldwide is projected to reach 16% by 2050, with some regions surpassing 25% [1]. Additionally, the global population of individuals aged 80 and older is expected to triple by 2050, significantly increasing the demand for appropriate housing and social support systems [2]. Amid this demographic shift, the concept of aging in place (AIP) has gained substantial attention, emphasizing the ability of older adults to live independently and safely in their own homes rather than in institutionalized care settings [3]. AIP extends beyond remaining in one’s residence; it involves creating an environment that fosters physical and psychological stability, autonomy, and overall well-being [3]. A recent AARP study [4] found that over 87% of adults aged 65 and older would prefer to remain in their current home as they age. However, U.S. Census Bureau data indicate that only 10% of American homes are adequately designed for aging populations [5]. Additionally, in the Netherlands, more than 40,000 households occupied by individuals aged 65 and older are categorized as unsuitable for aging residents [6,7]. This evidence underscores that residential environments pose a major barrier to aging in place, a challenge prevalent across European nations, particularly for individuals aged 80 and older [8]. The ability of older adults to age in place is closely associated with emotional stability, social connectivity, and quality of life. At a policy level, AIP is regarded as a cost-effective strategy to reduce long-term care facility admissions and alleviate social costs [9]. However, age-related declines in physical function increase fall risk, limit mobility, and create environmental barriers, hindering independent living [10]. In response, home environment modifications (HEMs) have been proposed as a critical intervention strategy [11].
As physical and cognitive function declines, environmental barriers increasingly impact independence and safety [12]. The discrepancy between environmental demands and an individual’s functional capacity exacerbates disability [13,14], contributing to increased fall risk [15], emergency department visits [16], and transitions to long-term care facilities [17,18]. Falls occurring within the home are a major health concern, with environmental factors being a primary cause [19,20]. Previous systematic reviews have demonstrated that home modifications improve functional performance and reduce falls among older adults with various health conditions [21]. Wahl et al. (2009) [13] examined the impact of home modifications on disability-related outcomes and found that these interventions significantly enhance functional performance.
Gitlin (1998) [22] defined home environment modifications as a comprehensive strategy, including structural renovations, assistive devices, visual cues, memory aids, furniture rearrangement, removal of hazardous items, and task simplification. Occupational therapy guidelines define home modifications as interventions that adapt the environment to enhance usability, safety, and independence [23]. The home modification process involves assessment, solution implementation, training, and evaluation.
The interaction between an individual’s physical and cognitive abilities and the built environment significantly influences functional independence and quality of life. According to the environmental press theory, balance is maintained when the environment supports an individual’s capabilities. However, if environmental demands exceed functional capacity, environmental pressure increases, leading to a decline in quality of life. The physical and cognitive capabilities of older adults interact with their living environment, affecting residential satisfaction and independent living. When housing environments impose excessive demands beyond an individual’s diminished functional capacity, disability and dependence increase, necessitating tailored home modifications [24]. Home modifications are also closely linked to the person–environment–occupation (PEO) model. This model emphasizes the dynamic interaction among personal (physical, psychological, and cognitive), environmental (physical and social), and occupational (daily activity) factors, which together determine functional independence and quality of life in older adults [25]. Natalia et al. [25] particularly highlight that smart home technologies, ramp installations, and bathroom modifications are essential home adaptations that enhance independent living for older adults. These findings suggest that home modifications are a critical strategy for improving functional performance, reducing nursing home admissions, and enhancing overall quality of life.
Existing studies on home modifications for older adults have primarily focused on fall prevention and the maintenance of physical function, often providing only a partial assessment of their overall effectiveness. However, in a super-aged society, a more comprehensive approach is required—one that extends beyond physical safety to encompass functional independence, quality of life, caregiving burden, cost-effectiveness, and social participation. Unlike previous studies that examined home modifications in isolation, this study adopts a holistic perspective by integrating socioeconomic factors and technological advancements to develop practical and sustainable intervention strategies. To achieve this objective, this study employs a systematic review methodology to examine the intervention methods, effectiveness, accessibility, and policy support associated with home modifications for aging in place. Additionally, it evaluates both the short-term and long-term impacts of these modifications, providing evidence-based recommendations for customized intervention models and policy frameworks that ensure sustainability and practical applicability in an aging society.
The key research questions of this study are as follows:
- (1)
- Primary Research Question
- -
- What is the comprehensive impact of home modifications on aging in place among older adults?
- (2)
- Secondary Research Questions
- -
- What are the primary types and specific applications of home modifications for older adults?
- -
- What are the multidimensional effects of home modifications on aging in place?
- -
- What are the interactions and comprehensive impacts of health changes and home modifications among older adults?
This study aims to provide scientific evidence to guide policy development, healthcare interventions, and future research, ultimately contributing to the enhancement of aging-in-place strategies.
2. Materials and Methods
2.1. Study Design
Based on the PRISMA 2020 checklist, a systematic literature review was conducted on home modifications for older adults living in the community. This review identified and categorized relevant studies and synthesized their findings and differences.
The review protocol and full methodological details were preregistered in the Open Science Framework (OSF) to ensure transparency and reproducibility. The registration is publicly accessible via the following DOI: https://doi.org/10.17605/OSF.IO/MJGN6 (accessed on 25 March 2025) (Registration No. 10.17605/OSF.IO/MJGN6).
2.2. Eligibility Criteria for Study Inclusion
Studies were included if they met all eligibility criteria simultaneously. These were applied concomitantly based on the PICO framework, a widely used approach for formulating research questions in evidence-based practice. The PICO framework consists of four key components: participants (P), intervention (I), comparison (C), and outcomes (O), which guide the systematic selection of relevant studies.
- (1)
- Participants: Older adults aged 60 years or older living in their own homes, not in hospitals or institutional settings (studies including participants with a mean age of 60 years or older were also eligible). Both healthy older adults and those with health conditions were included.
- (2)
- Intervention: Studies implementing home modifications for older adults in their own residences, rather than in hospitals or institutions. Home modifications included structural changes (e.g., door widening, ramp installation, and improved accessibility) and the installation of assistive devices inside or outside the home (e.g., grab bars, handrails, and elevators) using either low-technology or high-technology approaches.
- (3)
- Comparison: Studies that described the content and methods of home modifications and methods of measuring effectiveness. Studies without comparison groups were also included.
- (4)
- Outcomes: Studies examining the content and methods of home modifications for aging in place, effectiveness assessments before and after implementation, and their impact on various outcomes, including fall risk reduction, caregiving needs and burden, functional independence (activities of daily living), occupational participation, and life satisfaction (quality of life). The effectiveness and association between home modifications and aging in place were also evaluated.
The primary inclusion criteria were based on published studies discussing home modification interventions provided in community settings. Studies were included if they met the following definition of home modifications:
Home modifications refer to changes in the residential environment to help individuals live more independently and safely in their own homes while reducing the risk of injury for both care recipients and caregivers. Home modifications include structural changes (e.g., door widening, ramp installation, and improved accessibility) and the installation of assistive devices inside and outside the home (e.g., grab bars, handrails, and elevators).
The exclusion criteria were as follows:
- (1)
- Studies focusing on hospital and institutional environmental modifications.
- (2)
- Studies that targeted individuals with functional disabilities but did not specifically focus on older adults.
- (3)
- Studies that implemented home modifications but did not evaluate their effectiveness.
- (4)
- Studies deemed irrelevant or duplicate studies.
- (5)
- Studies without full-text availability or only available in abstract form.
- (6)
- Review articles, letters, study protocols, poster presentations, and non-original articles such as books.
- (7)
- Conference presentations, academic conference abstracts, and dissertations.
2.3. Search Strategy
Following the Cochrane Handbook for Systematic Reviews of Interventions, a comprehensive search was conducted in three online databases—Medline, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL)—for relevant publications between 1 January 2010 and 16 July 2024. Two keyword clusters were applied to ensure comprehensive coverage of relevant studies (Table 1).

Table 1.
Keywords related to old age and home modification.
2.4. Study Selection
A researcher and an external expert conducted the study selection, data extraction, and quality assessment. Two reviewers independently evaluated each selected study according to the search procedure. Initially, studies were screened based on their titles and abstracts following the inclusion criteria outlined in the PICO section. Disagreements regarding study inclusion were resolved through consensus. The two reviewers then assessed the full texts of the included studies to determine final eligibility for the review. Any disagreements about inclusion were again resolved through discussion. Additionally, an external expert independently reviewed all stages of the study selection process to minimize researcher bias and enhance the reliability of the process.
2.5. Data Extraction Process
First, two reviewers evaluated the relevance of each study to the research question and objectives based on the title, abstract, and keyword information and conducted data analysis accordingly. The following data were extracted from each study and recorded in a Microsoft Excel spreadsheet: title, author(s), publication year, journal, study country, study design, type of home modifications, participant characteristics, assessment tools, outcomes, and effectiveness.
This systematic review analyzed various aspects of home modification interventions supporting aging in place for older adults. After assessing the general characteristics of the included studies, key research themes such as fall prevention effects, environmental modifications for older adults with cognitive decline, and the impact of home modifications on quality of life were classified to structure the study findings. Thematic analysis and content analysis methodologies were applied to categorize study topics, compare and organize similarities and differences across studies, and interpret the findings using a narrative synthesis approach, considering heterogeneity among the studies. The results were presented in tabular format for clarity.
2.6. Study Quality Assessment
A researcher and an external expert conducted a qualitative assessment of 20 selected studies. The Physiotherapy Evidence Database (PEDro) scale and the Methodological Index for Nonrandomized Studies (MINORS) were used to evaluate the methodological quality of the selected studies. The PEDro scale was applied to assess randomized controlled trials (RCTs), while MINORS was used for non-randomized controlled studies. Two independent reviewers used these tools to evaluate the level of evidence in each study. In cases where the reviewers’ opinions differed, consensus was reached through discussion to determine the final quality score.
The PEDro scale is a validated tool for assessing the methodological quality of RCTs, using a binary response system (‘Yes’ or ‘No’), with a maximum score of 10 points (number of ‘Yes’ responses). Based on methodological criteria, the quality assessment was categorized as follows: scores of 9–10 were rated as ‘excellent’, 6–8 as ‘good’, 4–5 as ‘fair’, and below 4 as ‘poor’ [26].
For non-randomized controlled studies, the MINORS score was used. The maximum ideal score for non-comparative studies was 16, whereas for comparative studies, the maximum was 24 [27]. The items are scored 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate). The global ideal score is 16 for non-comparative studies and 24 for comparative studies. The methodological quality percentage was then calculated and classified as follows: less than 25% was considered ‘very low methodological quality’, 25–49% as ‘low quality’, 50–74% as ‘moderate quality’, and 75% or higher as ‘high quality’. This classification approach, using continuous criteria, has been reported in previous research [28].
3. Results
3.1. Literature Search and Selection
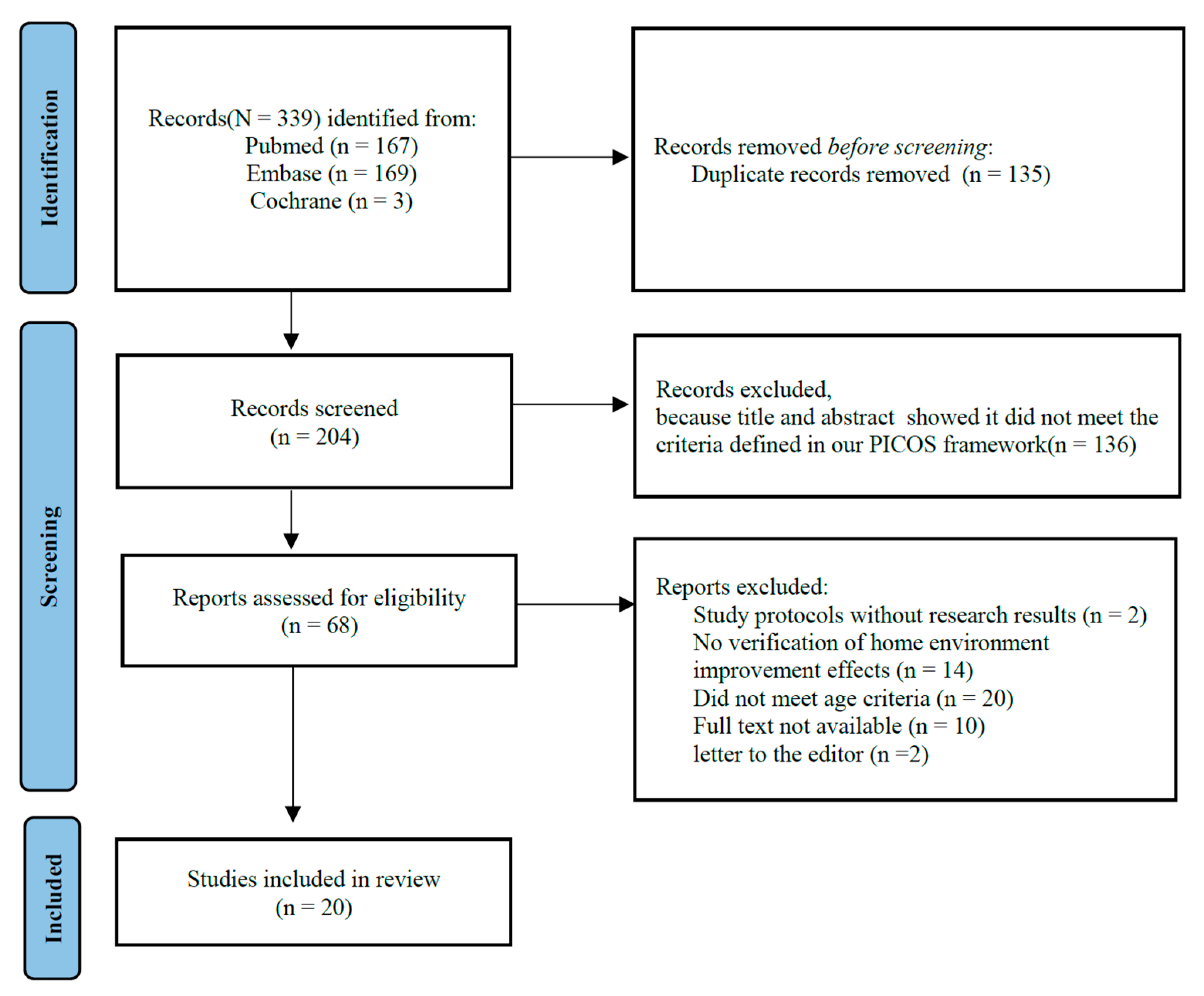
A total of 339 studies were initially identified through the search process. After removing 135 duplicate studies, the remaining studies were assessed based on the inclusion criteria. As a result, 136 studies were excluded. A full-text evaluation was conducted on 68 studies, after which an additional 48 studies were excluded. Consequently, 20 studies were finally included in this systematic review (Figure 1).
Figure 1.
PRISMA flowchart shows details of the processes related to the identification, screening, and selection processes. PICO = participants, interventions, comparisons, outcomes study design.
3.2. Study Quality Assessment
The PEDro scale was applied to five randomized controlled trials (RCTs), while the MINORS scale was used to assess 15 non-randomized controlled trials (NCTs). The PEDro scale scores for all five RCTs were 9 points, indicating an ‘Excellent’ quality rating (Table 2). The MINORS scale scores for 14 studies, based on a maximum score of 16, ranged from 6 points (‘Low’) to 14 points (‘High’), while one study, evaluated based on a maximum score of 24, received a score of 23 points (‘High’) (Table 3).

Table 2.
PEDro scale score.

Table 3.
MINORS score.
3.3. General Characteristics of Studies
The general characteristics of the studies were summarized based on the author, year, title, journal name, study location, study design, target group, sample size, mean participant age, and gender distribution. The data in Table 4 are presented in descending order, prioritizing the most recent publications.

Table 4.
General characteristics of studies.
Among the 20 studies analyzed, 12 (60%) were conducted within the past five years, with the United States representing the largest proportion (five studies, 25%). Regarding study design, there were five randomized controlled trials (25%) and 15 non-randomized controlled trials (75%). The target population primarily included older adults aged 60 and older, accounting for 12 studies (60%), including individuals with a history of falls. The remaining studies focused on individuals with functional impairments, such as those with Parkinson’s disease, dementia, cognitive decline, or disabilities. In terms of gender distribution, 17 studies (85%) reported a higher proportion of male participants, while one study (5%) had more female participants. The remaining two studies (10%) either did not specify gender distribution or deemed it inapplicable. Participants’ ages ranged from their 60s to 80s, reflecting a diverse older adult population.
3.4. Intervention Type, Outcome Measurements, and Main Results of Studies
Table 5 summarizes the intervention types, session frequency and duration, outcome measurement tools, key findings, and the overall effectiveness of home modifications. All studies examined home modification interventions and their impact. Three studies [22,34,36] indirectly assessed home modifications’ role in improving residential environments. A total of 15 studies lacked a control group. Eight studies [14,22,34,37,39,42,43,44] conducted a single evaluation and data collection session, while most studies implemented home modifications following an initial assessment and conducted follow-up evaluations. The number of sessions primarily referred to home visits for evaluation. Five studies [21,32,33,40,41] included four sessions, another five studies [29,30,31,35,38] included three sessions, one study [36] had two sessions, and one study [45] included five sessions. The study with five sessions conducted 90 min home visits, providing both interventions and education. Evaluations were generally scheduled weekly, monthly, or every two to three months.

Table 5.
Intervention type, outcome measurements, and main results of studies.
Regarding outcome measurement tools, the Falls Efficacy Scale, assessing fear of falling, was used in four studies [21,30,35,41], while fall incidence was reported in two studies [32,44]. The Housing Enabler (HE), measuring residential accessibility, was used in two studies [14,36], and the Katz ADL, evaluating functional independence, was employed in two studies [38,40]. The EuroQol Questionnaire, assessing the quality of life, appeared in two studies [33,40]. The Westmead Home Safety Assessment (WeHSA) was used in one study [21]. Additional tools were used to measure independent living, fall risk, home safety, functional mobility, and balance.
Key findings indicated that fall reduction was reported in seven studies [21,30,32,35,38,44,45], while six studies [14,29,30,33,43,45] observed improved mobility. Increased functional independence was reported in four studies [31,42,44,45], and quality-of-life enhancement in four studies [30,31,40,44]. A decrease in fear of falling was noted in four studies [29,32,35,40]. Other findings included improved adherence to home modifications, enhanced accessibility after barrier removal, reduced home safety risks, decreased anxiety and depression, shorter caregiving time, and greater self-efficacy.
Regarding effectiveness, studies were classified as “Effective” if statistically significant improvements were observed across all measured outcomes. Studies where some outcomes showed statistical significance but lacked consistent overall results or had methodological limitations were categorized as “Correlation Identified”. Among the 20 studies, 13 (65%) [21,29,30,32,33,35,37,38,39,40,42,44,45] found home modifications to be effective, contributing to fall reduction, improved functional independence, and better quality of life. Notably, bathroom modifications, grab bars, and stair railings were identified as the most impactful interventions. Additionally, reductions in emergency hospitalizations and caregiver burden were reported following home modifications.
Meanwhile, seven studies (35%) [14,22,31,34,36,41,43] found that home modifications were strongly associated with residential accessibility and lifestyle factors. These studies suggested that effectiveness varied based on socioeconomic status and living environment. Some reported that older adults in need of home modifications did not actively receive interventions. While home modifications improved functional independence and quality of life, some studies also noted a potential increase in caregiver burden as a negative consequence.
3.5. Home Modification Details of Studies
Table 6 summarizes the home modifications analyzed in 20 studies. Mobility and accessibility improvements and bathroom safety enhancements were implemented in all studies (100%), including threshold removal, doorway widening, stair lift installation, grab bars, and non-slip mats. Fall prevention measures were applied in 18 studies (90%), incorporating non-slip flooring, lighting improvements, and mobility training.

Table 6.
Home modification details of studies.
Kitchen and living space modifications were present in 15 studies (75%), while support for independent living was included in 14 studies (70%), involving cooking area adjustments and assistive device provision. Stair safety enhancements (12 studies, 60%) and lighting improvements (10 studies, 50%) were also emphasized. In contrast, hazard removal (eight studies, 40%) and outdoor environment modifications (seven studies, 35%) were reported less frequently.
3.6. A Multidimensional Analysis of Home Modification for Aging in Place Among Older Adults
This study provides a comprehensive analysis of the impact of home modifications on aging in place among older adults (Table 7). The findings include both statistically significant results and notable trends, even when statistical significance was not observed. The analysis examined the effects of home modifications on fall prevention (12 studies), activities of daily living (ADL) improvement (six studies), quality-of-life enhancement (five studies), and home safety improvements (four studies). Additional areas of research included housing accessibility (two studies), modifications for older adults with cognitive decline (two studies), caregiver burden reduction (two studies), cost-effectiveness analysis (two studies), and socioeconomic disparities (two studies).

Table 7.
A multidimensional analysis of home modification for aging in place among older adults.
Notably, fall prevention and increased independence were the most prominent effects, while housing accessibility and tailored interventions contributed to improved quality of life. Home modifications also reduced caregiver burden, emphasizing the need for economic and policy support. These findings highlight the importance of continued research and policy initiatives to promote independent living and a safe home environment for older adults.
3.7. Integrated Analysis of Health Changes and Home Modification Among Older Adults
This study analyzed the effectiveness of home modifications from three perspectives: age-related physical changes, the maintenance of physical function and balance, and cognitive function changes (Table 8).

Table 8.
Integrated analysis of health changes and home modification among older adults.
First, home modifications effectively prevented falls, maintained functional independence, and improved quality of life. Interventions such as grab bars, non-slip mats, and stair railings significantly reduced fall incidence, particularly in high-risk areas like bathrooms. Enhanced home accessibility improved mobility and increased the likelihood of aging in place.
Second, combining home modifications with exercise was the most effective strategy for maintaining physical function and balance. These interventions improved mobility, reduced fear of falling, and enhanced physical independence. Notably, grab bars and stair railings played a crucial role in stability and movement.
Third, for older adults with cognitive impairment, home modifications that maintained familiar environments while enhancing safety were essential. Gradual adjustments, rather than abrupt changes, supported memory retention and spatial awareness.
Additionally, home modifications contributed to cost savings by preventing falls, with the greatest cost-effectiveness observed in high-risk groups. However, some studies noted an increase in caregiver burden, highlighting the need for integrated support measures.
In conclusion, systematic and tailored home modifications addressing physical, functional, and cognitive changes are essential for fall prevention and independent living. These findings emphasize the necessity of a multidimensional intervention strategy.
4. Discussion
Previous studies have primarily examined the individual effects of home modifications, focusing on fall prevention, physical function maintenance, and accessibility improvements. However, this study goes beyond physical safety, analyzing home modifications as a key factor in promoting aging in place from a multidimensional perspective. Specifically, it considers the impact of technological advancements and policy support on the effectiveness and accessibility of home modifications, emphasizing the need for practical and sustainable intervention strategies. Through this integrated approach, the study explores the broader impact on older adults’ well-being and, based on these findings, proposes theoretical implications, practical applications, and future research directions.
4.1. Methodological Considerations
This study conducted a systematic literature review following PRISMA 2020 guidelines to examine the multidimensional effects of home modifications in promoting aging in place for older adults. To enhance study reliability, clear inclusion and exclusion criteria were established. Methodological quality was assessed using the PEDro and MINORS scales: PEDro for randomized controlled trials (RCTs) [47] and MINORS for non-randomized studies. However, due to the nature of home modifications, blinding participants and intervention providers was inherently challenging in RCTs, leading to methodological limitations. Many studies also received low MINORS scores on prospective data collection, objective outcome evaluation, follow-up periods, and sample size estimation. Future research should incorporate independent evaluators, objective assessment tools, and adequate follow-up periods to address these limitations.
This study reviewed research from 2010 to 2024 to reflect advancements in home modification policies, assistive technologies, and interventions. However, focusing on recent studies may introduce publication bias, as studies with significant positive effects are more likely to be published. To mitigate this, future systematic reviews should include gray literature, such as government reports, conference proceedings, and unpublished studies [48].
Significant heterogeneity was observed across studies in intervention methods, assessment tools, and participant characteristics, limiting meta-analysis feasibility. Assessment methods ranged from self-reports and clinician evaluations to biomechanical measurements, reducing comparability and generalizability. Future research should adopt standardized assessment tools, such as the Housing Enabler [49] or Westmead Home Safety Assessment (WeHSA) [50], and apply statistical measures like I2 statistics and subgroup analyses to quantify heterogeneity [51,52]. A key limitation was the lack of long-term follow-up data, making it difficult to assess the sustained effects of home modifications. Future studies should establish appropriate follow-up periods, employ objective outcome measures, and use bias assessment tools [53], such as ROBINS-I [54], to enhance reliability. Sensitivity analyses [51] will further strengthen the findings’ validity. By addressing these methodological limitations and proposing specific improvements, future research can provide more robust, evidence-based home modification strategies to effectively support aging in place for older adults.
4.2. Primary Types and Specific Applications of Home Modifications for Older Adults
This study analyzed 20 studies to identify specific home modifications aimed at improving mobility, safety, and independence among older adults. The findings revealed that mobility and accessibility improvements (100%) and bathroom safety enhancements (100%) were the most common modifications, playing a crucial role in fall prevention and safe indoor movement. The most frequently implemented fall prevention strategies (90%) included non-slip flooring, stair handrails, and improved lighting.
Kitchen and living space modifications (75%) primarily focused on adjusting cabinet heights and optimizing cooking areas. Independent living support interventions (70%) involved adjustable beds, assistive devices, and caregiver education programs. Additionally, stair safety enhancements (60%) and lighting improvements (50%) were widely adopted, with an increasing shift toward LED lighting and sensor-based automation. However, hazard removal (40%) and outdoor modifications (35%) were implemented less frequently, suggesting the need for further research and policy support. Future studies should prioritize outdoor accessibility improvements, including ramps, threshold removal, doorway widening, and slip-resistant walkways [21].
These findings underscore that home modifications extend beyond structural changes, representing a multidimensional intervention supporting mobility, safety, and independent living. The widespread adoption of mobility and bathroom modifications highlights their fundamental importance. Additionally, the growing emphasis on fall prevention, lighting improvements, and smart technologies reflects an increasing shift toward technology-driven solutions. The trend toward personalized home modifications has led to the adoption of assistive devices, caregiver education, and smart home technologies, such as automated lighting, motorized blinds, and IoT-based home systems.
Despite the growing recognition of smart home technology, research on its effectiveness and evaluation methodologies remains limited [55]. Future studies should adopt systematic evaluation frameworks to assess its impact. The Technology Acceptance Model (TAM) can quantify user-friendliness, ease of use, and perceived usefulness of smart home systems [51]. Smart-sensor-based fall prevention should be evaluated using objective metrics, such as fall incidence, severity, and emergency response time [56]. The cost-effectiveness and sustainability of IoT-based smart homes should be analyzed through installation costs, maintenance expenses, and long-term viability [57]. Lastly, user satisfaction and real-world impact should be assessed through surveys and in-depth interviews to provide qualitative insights [56]. By applying these systematic methodologies, future research can generate empirical evidence, advancing a clearer, more structured understanding of smart home technologies in supporting aging in place.
4.3. The Multidimensional Effects of Home Modifications on Aging in Place Among Older Adults
In this study, a multidimensional analysis of home modifications aimed at supporting aging in place among older adults was conducted, examining their effects on fall prevention, functional independence, quality of life, household stability, environmental safety, accessibility, cognitive decline, caregiver burden, cost-effectiveness, and socioeconomic disparities. Home modifications are an effective intervention for fall prevention, with even greater benefits when combined with exercise programs. A systematic review by Stark et al. [56] found that home modifications significantly reduced fall risk and increased activity participation among older adults with physical impairments. Similarly, Chase et al. [58] reported that older adults who participated in both home modifications and regular exercise programs had a significantly lower incidence of falls compared to those receiving only home modifications. These findings confirm the complementary role of home modifications and exercise in maximizing fall prevention outcomes, emphasizing the need for continuous assessment and individualized adjustments based on functional changes.
Home modifications also contribute to improved quality of life, independence, and psychological stability. However, some studies indicate limitations, including a slight increase in caregiver burden. While modifications improve mobility and social participation, they may also place additional demands on caregivers [59]. Certain studies suggest that home modifications alone may not always be sufficient and are most effective when tailored to individual living environments and functional abilities [60]. Therefore, a personalized home modification strategy that considers functional capacity, cognitive status, and lifestyle is essential. Additionally, technology-driven interventions, such as smart home systems, may further enhance effectiveness. These findings highlight the need for meticulously designed home modifications to promote safe and independent living, along with policies supporting personalized interventions.
For older adults with cognitive impairments, home modifications have been effective in reducing falls and improving functional abilities, though they have also been associated with a slight increase in caregiver burden. This may be due to the challenges older adults with cognitive impairments face in adapting to environmental changes, requiring caregivers to provide continuous monitoring and support after modifications. To address this, gradual adjustments rather than abrupt changes should be implemented, along with caregiver education and expert involvement [61]. While home modifications can reduce caregiver burden and promote independence, sudden environmental changes may cause confusion among those with cognitive impairments. Caregivers often struggle to anticipate their full impact, potentially increasing their burden. Therefore, a gradual approach, caregiver education, and expert intervention are critical to maximizing effectiveness [62]. Generally, home modifications have also proven to be effective in reducing caregiving time and burden, with bathroom modifications being one of the most widely implemented interventions. However, as older adults adapt to modified environments, the role of caregivers may expand, requiring complementary support measures. A multifaceted approach, including gradual adjustments and caregiver education, should be integrated into home modification planning. Additionally, long-term policy support is essential to reduce the overall caregiver burden [63,64].
Home modifications are a cost-effective intervention, particularly for high-risk populations. Low-cost modifications, such as grab bars and improved lighting, are highly cost-effective, while full-scale renovations, though beneficial in the long term, require substantial initial investment. However, research on the cost-effectiveness of home modifications remains limited. Future studies should conduct comprehensive cost-effectiveness analyses comparing low-cost vs. high-cost modifications and traditional home modifications vs. smart-home-technology-based interventions to optimize public funding allocation.
Access to home modification programs varies based on socioeconomic factors such as residential location, disability status, and income level. Research has highlighted that socioeconomic disparities may exclude low-income and rural older adults from receiving home modification services. Key policy initiatives addressing this issue include the Medicaid Waiver Program, Community Development Block Grant (CDBG), USDA Section 504 Program (U.S), Japan’s Long-Term Care Insurance Act, and the UK’s Disabled Facilities Grant (DFG) and Home Improvement Agencies (HIAs) model [65,66]. Future research should conduct a comparative analysis of successful policy models from the U.S., Japan, and the UK to establish a more defined strategic policy direction for supporting aging in place, tailored to the specific circumstances of each country. Additionally, standardized protocols should be developed for assessing and implementing home modifications, and interdisciplinary collaboration among occupational therapists, architects, and social workers should be promoted to enhance professional capacity and practical implementation.
4.4. The Interactions and Comprehensive Impacts of Health Changes and Home Modifications Among Older Adults
This study comprehensively analyzed the effects of home modifications for older adults from three key perspectives: physical aging changes, maintenance of physical function and balance, and cognitive function changes. These factors are interconnected rather than independent, requiring an integrated approach to maximize their benefits. The interaction between age-related physical changes, such as muscle weakness, balance impairments, functional decline, and environmental modifications necessitates continuous and systematic interventions. As aging progresses, muscle weakness and balance impairments become major contributors to falls [67]. Studies indicate that home modifications, including handrail installation and optimized movement pathways, effectively mitigate physical function decline [68]. Systematic home modification programs have been shown to significantly reduce fall incidence rates [69]. Since home modifications play a critical role in compensating for functional decline, interventions should not be one-time measures but should involve regular monitoring and adjustments. As older adults’ physical needs evolve, continuous environmental assessments and modifications should be conducted. A customized approach that considers an individual’s lifestyle and residential environments is essential.
To maintain physical function and balance, a combined intervention of home modifications and exercise is necessary. Age-related musculoskeletal changes impact mobility and balance control [70]. Therefore, integrating balance and strength training exercises with home modifications enhances mobility and functional independence in older adults [71]. Research shows that installing stair handrails and non-slip flooring significantly improves balance, with even greater benefits observed when paired with structured exercise programs [72]. The integration of home modifications and exercise is crucial because it directly impacts physical function maintenance. Environmental modifications alone are insufficient to fully support mobility in older adults; a targeted exercise regimen focusing on balance and strength must be included. Regular balance and strength training is a highly effective strategy for improving mobility and autonomy in older adults.
For older adults with cognitive impairments, home modifications should preserve a familiar environment while enhancing safety to prevent falls and behavioral disturbances and to promote functional independence. Cognitive impairments can make adapting to environmental changes challenging, increasing fall risk. Maintaining familiar surroundings while incorporating safety measures such as handrails, improved lighting, and non-slip flooring effectively prevents falls and supports independence. Studies highlight that bathroom modifications are particularly effective in reducing fall risk [73]. An effective approach may involve starting with non-invasive adjustments, such as improved lighting, before gradually incorporating handrails or furniture rearrangement.
To achieve these objectives, customized support programs tailored to older adults’ health conditions are necessary. Additionally, collaborative efforts between governments and local communities are essential for implementing home modification policies. With these combined efforts, older adults can live more safely and independently.
5. Conclusions
This study systematically and comprehensively analyzed the effects of home modifications in supporting aging in place for older adults. The findings indicate that home modifications extend beyond structural changes, offering significant benefits in fall prevention, functional independence, quality of life, caregiver burden reduction, and cost-effectiveness. However, to maximize these effects, personalized interventions that consider an individual’s physical and cognitive characteristics and living environment, along with continuous maintenance and appropriate technology integration, are essential. Additionally, the impact of home modifications varies based on socioeconomic background, cognitive function, and physical condition, highlighting the need for a strategic and individualized approach.
5.1. Theoretical Implications
This study establishes that home modifications are not merely structural changes but a fundamental factor in promoting physical, psychological, and social well-being. Unlike previous research that primarily focused on isolated effects such as fall prevention and mobility improvement, this study integrates multiple intervention factors, analyzing the broader impact of home modifications on older adults’ overall lives. This approach addresses a gap in the literature regarding the multidimensional effects of home modifications and confirms their essential role in supporting aging in place. Additionally, the study emphasizes the need for standardized evaluation tools, such as the Housing Enabler and Westmead Home Safety Assessment, to enhance research consistency and comparability. Establishing a methodological framework through these standardized tools will enable more objective analysis of home modification effects.
5.2. Practical Applications
This study confirms that home modifications are a cost-effective intervention that reduces caregiver burden. However, accessibility to home modification programs remains limited for low-income and rural-dwelling older adults. To address these disparities, policymakers should reference successful financial support models, such as the Medicaid Waiver system, Community Development Block Grant (CDBG), and USDA Section 504 Rural Repair and Rehabilitation Grants in the United States, to develop more effective support systems. Additionally, the adoption of smart home technologies, such as sensor-based lighting and voice-controlled systems, should be actively promoted to enhance independence and convenience for older adults. Interdisciplinary collaboration among occupational therapists, architects, and social workers is essential for developing personalized home modification strategies that address the physical and cognitive needs of older adults. This approach should extend beyond physical modifications, creating a residential environment that supports long-term independence.
5.3. Future Research Directions
Future research should focus on comparative studies between smart home technology and traditional home modifications to identify the most effective intervention strategies. To evaluate the effectiveness of smart home technologies, studies should employ the Technology Acceptance Model (TAM) to assess older adults’ technology adoption rates and utilize sensor-based data to analyze fall incidence rates and severity. Additionally, a comparative cost-effectiveness analysis between smart home technologies and conventional home modifications should assess economic feasibility, considering both initial installation costs and long-term maintenance expenses. Further research should develop customized home modification models for diverse older adult populations, including those with severe physical impairments, mild dementia, and economic disadvantages, to determine the most suitable interventions for each group. Moreover, comparative policy analyses of home modification support programs in the United States, Japan, and the United Kingdom should be conducted to develop an optimal policy framework adaptable to various local communities. To achieve these goals, future research should incorporate standardized evaluation frameworks from the early stages of study design, ensuring systematic and objective analysis while prioritizing studies with high practical applicability.
This study contributes to enhancing safety and functional independence for older adults, ultimately facilitating successful aging in place. To achieve this, empirical studies must provide scientific evidence and conduct precise analyses of home modification effectiveness. With these efforts, older adults can maintain a safer and more independent lifestyle, ultimately leading to a healthier and more sustainable aging process.
Funding
This work was supported by Kyungnam University Foundation Grant, 2022 (Grant Number 20220047).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The article includes all data supporting the reported results; further details on the methodology are available from the corresponding author upon reasonable request.
Acknowledgments
Two external experts conducted the study selection, data extraction, and quality assessment for this study.
Conflicts of Interest
The author has no conflicts of interest to declare.
References
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights; United Nations: New York, NY, USA, 2019; ST/ESA/SER.A/430. [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division. World Social Report 2023: Leaving No One Behind in an Ageing World; United Nations: New York, NY, USA, 2023. [Google Scholar]
- Sixsmith, J.; Sixsmith, A. Aging in place in the United Kingdom. Aging Int. 2008, 32, 219–235. [Google Scholar] [CrossRef]
- Harrell, R.; Lynott, J.; Guzman, S.; Lampkin, C. What Is Livable? Community Preferences of Older Adults; AARP Public Policy Institute: Washington, DC, USA, 2014. [Google Scholar]
- Vespa, J.; Engelberg, J.; He, W. Old Housing, New Needs: Are U.S. Homes Ready for an Aging Population? U.S. Census Bureau: Washington, DC, USA, 2020; pp. 23–217.
- Leidelmeijer, K.; Iersel, J.V.; Leering, D. Monitor Investeren in de Toekomst–Ouderen en Langer Zelfstandig Wonen; RIGO: Amsterdam, The Netherlands, 2017; Available online: https://www.rigo.nl/ (accessed on 1 August 2024).
- de Klerk, M.; Verbeek-Oudijk, D.; Plaisier, I.; den Draak, M. Zorgen voor Thuiswonende Ouderen; Sociaal en Cultureel Planbureau: The Hague, The Netherlands, 2019; p. 103. [Google Scholar]
- Braubach, M.; Power, A. Housing conditions and risk: Reporting on a European study of housing quality and risk of accidents for older people. J. Hous. Elder. 2011, 25, 288–305. [Google Scholar] [CrossRef]
- Ratnayake, M.; Lukas, S.; Brathwaite, S.; Neave, J.; Henry, H. Aging in place: Are we prepared? Del. J. Public Health 2022, 8, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Gitlin, L.N. Conducting research on home environments: Lessons learned and new directions. Gerontologist 2003, 43, 628–637. [Google Scholar] [CrossRef]
- Lee, S.H.; Yu, S. Effectiveness of multifactorial interventions in preventing falls among older adults in the community: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2020, 106, 103564. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 9, CD007146. [Google Scholar] [CrossRef]
- Wahl, H.W.; Fänge, A.; Oswald, F.; Gitlin, L.N.; Iwarsson, S. The home environment and disability-related outcomes in aging individuals: What is the empirical evidence? Gerontologist 2009, 49, 355–367. [Google Scholar] [CrossRef]
- Pettersson, C.; Slaug, B.; Granbom, M.; Kylberg, M.; Iwarsson, S. Housing accessibility for senior citizens in Sweden: Estimation of the effects of targeted elimination of environmental barriers. Scand. J. Occup. Ther. 2018, 25, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Nicklett, E.; Lohman, M.; Smith, M. Neighborhood environment and falls among community-dwelling older adults. Int. J. Environ. Res. Public Health 2017, 14, 175. [Google Scholar] [CrossRef]
- Runyan, C.W.; Casteel, C.; Perkis, D.; Black, C.; Marshall, S.W.; Johnson, R.M.; Waller, A.E.; Viswanathan, S. Unintentional injuries in the home in the United States Part I: Mortality. Am. J. Prev. Med. 2005, 28, 73–79. [Google Scholar] [CrossRef]
- Gaugler, J.E.; Duval, S.; Anderson, K.A.; Kane, R.L. Predicting nursing home admission in the U.S: A meta-analysis. BMC Geriatr. 2007, 7, 13. [Google Scholar] [CrossRef]
- Freedman, V.A.; Spillman, B.C. The residential continuum from home to nursing home: Size, characteristics and unmet needs of older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2014, 69 (Suppl. S1), S42–S50. [Google Scholar] [CrossRef]
- Sophonratanapokin, B.; Sawangdee, Y.; Soonthorndhada, K. Effect of the living environment on falls among the elderly in Thailand. Southeast Asian J. Trop. Med. Public Health 2012, 43, 1537–1547. [Google Scholar] [PubMed]
- Zhang, L.; Ding, Z.; Qiu, L.; Li, A. Falls and risk factors of falls for urban and rural community-dwelling older adults in China. BMC Geriatr. 2019, 19, 379. [Google Scholar] [CrossRef]
- Stark, S.; Somerville, E.; Keglovits, M.; Conte, J.; Li, M.; Hu, Y.L.; Yan, Y. Protocol for the home hazards removal program (HARP) study: A pragmatic, randomized clinical trial and implementation study. BMC Geriatr. 2017, 17, 90. [Google Scholar] [CrossRef]
- Gitlin, L.N. Testing home modification interventions: Issues of theory, measurement, design, and implementation. Annu. Rev. Gerontol. Geriatr. 1998, 18, 190–246. [Google Scholar] [CrossRef]
- Siebert, C.; Smallfield, S.; Stark, S. Occupational Therapy Practice Guidelines for Home Modifications; AOTA Press: Bethesda, MD, USA, 2014. [Google Scholar]
- Byrnes, M.; Lichtenberg, P.A.; Lysack, C. Environmental Press, Aging in Place, and Residential Satisfaction of Urban Older Adults. J. Appl. Sociol./Sociol. Pract. 2006, 23, 50–77. [Google Scholar] [CrossRef]
- Natalia, M.; Yang, S.L.; Chen, Y.J.; Tzu, H.H.; Liao, C.P.; Huang, C.H.; Chou, Y.C. Person–Environment–Occupation Model in the Quality Improvement and Patient Safety Education: A Case Study. Clin. Case Rep. Int. 2023, 7, 1504. [Google Scholar] [CrossRef]
- Moseley, A.M.; Herbert, R.D.; Sherrington, C.; Maher, C.G. Evidence for physiotherapy practice: A survey of the Physiotherapy Evidence Database (PEDro). Aust. J. Physiother. 2002, 48, 43–49. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Braga, L.H.; Mijovic, H.; Farrokhyar, F.; Pemberton, J.; DeMaria, J.; Lorenzo, A.J. Antibiotic prophylaxis for urinary tract infections in antenatal hydronephrosis. Pediatrics 2013, 131, e251–e261. [Google Scholar] [CrossRef] [PubMed]
- Stasi, S.; Tsekoura, M.; Gliatis, J.; Sakellari, V. Motor control and ergonomic intervention home-based program: A pilot trial performed in the framework of the motor control home ergonomics elderlies’ prevention of falls. Cureus 2021, 13, e14336. [Google Scholar] [CrossRef] [PubMed]
- Tsekoura, M.; Stasi, S.; Gliatis, J.; Sakellari, V. Methodology of a home-based motor control exercise and ergonomic intervention programme for community-dwelling older people: The McHeELP study. J. Frailty Sarcopenia Falls 2021, 6, 153–162. [Google Scholar] [CrossRef]
- Jeon, Y.H.; Krein, L.; Simpson, J.M.; Szanton, S.L.; Clemson, L.; Naismith, S.L.; Low, L.-F.; Mowszowski, L.; Gonski, P.; Norman, R.; et al. Feasibility and potential effects of interdisciplinary home-based reablement program (I-HARP) for people with cognitive and functional decline: A pilot trial. Aging Ment. Health 2020, 24, 1916–1925. [Google Scholar] [CrossRef]
- Kamei, T.; Kajii, F.; Yamamoto, Y.; Irie, Y.; Kozakai, R.; Sugimoto, T.; Chigira, A.; Niino, N. Effectiveness of a home hazard modification program for reducing falls in urban community-dwelling older adults: A randomized controlled trial. JPN. J. Nurs. Sci. 2015, 12, 184–197. [Google Scholar] [CrossRef]
- Riera Arias, G.; Serra Corcoll, J.; Casadevall Arnaus, M.; Vidal-Alaball, J.; Ramírez-Morros, A.; Arnau Solé, G. Improving quality of life in older adults with the decline syndrome: The role of occupational therapy in primary care. Aten. Primaria 2024, 56, 102879. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Lee, M.J.; Kang, J. Exploring differences in home modification strategies according to household location and occupant disability status: 2019 American Housing Survey analysis. J. Appl. Gerontol. 2024, 43, 231–241. [Google Scholar] [CrossRef]
- Hawkins, M.; Goldhammer, T.; McClave, R.; Jenkins-Smith, E. Evaluation of a fall prevention program to reduce fall risk and fear of falling among community-dwelling older adults and adults with disabilities. Clin. Interv. Aging 2024, 19, 375–383. [Google Scholar] [CrossRef]
- Andersson, N.; Slaug, B.; Nilsson, M.H.; Iwarsson, S. Environmental barriers and housing accessibility problems for people with Parkinson’s disease: A three-year perspective. Scand. J. Occup. Ther. 2023, 30, 661–672. [Google Scholar] [CrossRef]
- Schiller, G.; Seligman, A.; Lubetsky, S.; DeCherrie, L.V.; Reckrey, J.; Kopke, V.; Bacher, N.; Bhatia, S.; Ornstein, K.A. A home repair and modification program embedded within Mount Sinai Visiting Doctors. J. Appl. Gerontol. 2023, 42, 879–887. [Google Scholar] [CrossRef]
- Yeni, C.; Yilmaz, M. Nurse-led home modification interventions for community-dwelling older adults with dementia and their impact on falls prevention. Br. J. Healthc. Assist. 2022, 16, 242–251. [Google Scholar] [CrossRef]
- Hollinghurst, J.; Daniels, H.; Fry, R.; Akbari, A.; Rodgers, S.; Watkins, A.; Hillcoat-Nallétamby, S.; Williams, N.; Nikolova, S.; Meads, D.; et al. Do home adaptation interventions help to reduce emergency fall admissions? A national longitudinal data-linkage study of 657,536 older adults living in Wales (UK) between 2010 and 2017. Age Ageing 2022, 51, afab201. [Google Scholar] [CrossRef] [PubMed]
- Schorderet, C.; Ludwig, C.; Wüest, F.; Bastiaenen, C.H.G.; de Bie, R.A.; Allet, L. Needs, benefits, and issues related to home adaptation: A user-centered case series applying a mixed-methods design. BMC Geriatr. 2022, 22, 526. [Google Scholar] [CrossRef] [PubMed]
- Malmgren Fänge, A.; Chiatti, C.; Axmon, A. One-year changes in activities of daily living, usability, falls and concerns about falling, and self-rated health for different housing adaptation client profiles. Int. J. Environ. Res. Public Health 2021, 18, 9704. [Google Scholar] [CrossRef]
- Carnemolla, P.; Bridge, C. Housing design and community care: How home modifications reduce care needs of older people and people with disability. Int. J. Environ. Res. Public Health 2019, 16, 1951. [Google Scholar] [CrossRef]
- Wilson, G.; Aitken, D.; Hodgson, P.; Bailey, C. The hidden impact of home adaptations: Using a wearable camera to explore lived experiences and taken-for-granted behaviours. Health Soc. Care Community 2019, 27, 1469–1480. [Google Scholar] [CrossRef]
- Wilson, N.; Kvizhinadze, G.; Pega, F.; Nair, N.; Blakely, T. Home modification to reduce falls at a health district level: Modeling health gain, health inequalities and health costs. PLoS ONE 2017, 12, e0184538. [Google Scholar] [CrossRef]
- Somerville, E.; Smallfield, S.; Stark, S.; Seibert, C.; Arbesman, M.; Lieberman, D. Occupational therapy home modification assessment and intervention. Am. J. Occup. Ther. 2016, 70, 7005395010p1–7005395010p3. [Google Scholar] [CrossRef]
- Harvey, L.A.; Mitchell, R.J.; Lord, S.R.; Close, J.C.T. Determinants of uptake of home modifications and exercise to prevent falls in community-dwelling older people. Aust. N. Z. J. Public Health 2014, 38, 585–590. [Google Scholar] [CrossRef]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Paez, A. Gray literature: An important resource in systematic reviews. J. Evid.-Based Med. 2017, 10, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Iwarsson, S.; Slaug, B. Housing Enabler: An Instrument for Assessing and Analyzing Accessibility Problems in Housing; Veten & Skapen HB/Staffanstorp: Nävlinge, Sweden, 2001. [Google Scholar]
- Clemson, L.; Fitzgerald, M.H.; Heard, R. Content validity of an assessment tool to identify home fall hazards: The Westmead Home Safety Assessment. Br. J. Occup. Ther. 1999, 62, 171–179. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.3; Cochrane: London, UK, 2022. [Google Scholar]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Altman, D.G. Practical Statistics for Medical Research; Chapman & Hall/CRC: Boca Raton, FL, USA, 2001. [Google Scholar]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Higgins, J.P.T. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Coughlin, J.F. Older Adults’ Adoption of Technology: An Integrated Approach to Identifying Determinants and Barriers. J. Prod. Innov. Manag. 2015, 32, 747–759. [Google Scholar] [CrossRef]
- Stark, S.; Keglovits, M.; Arbesman, M.; Lieberman, D. Effect of Home Modification Interventions on the Participation of Community-Dwelling Adults with Health Conditions: A Systematic Review. Am. J. Occup. Ther. 2017, 71, 7102290010p1–7102290010p11. [Google Scholar] [CrossRef]
- Peek, S.T.; Wouters, E.J.; van Hoof, J.; Luijkx, K.G.; Boeije, H.R.; Vrijhoef, H.J. Factors influencing acceptance of technology for aging in place: A systematic review. Int. J. Med. Inform. 2014, 83, 235–248. [Google Scholar] [CrossRef]
- Chase, C.A.; Mann, K.; Wasek, S.; Arbesman, M. Systematic Review of the Effect of Home Modification and Fall Prevention Programs on Falls and the Performance of Community-Dwelling Older Adults. Am. J. Occup. Ther. 2012, 66, 284–291. [Google Scholar] [CrossRef]
- Arora, A.; Mahajan, H. Impact of Built Environment on Fear of Falls among Older Adults: A Systematic Review. Arch. Phys. Med. Rehabil. 2024, 105, e151. [Google Scholar] [CrossRef]
- Pillay, J.; Gaudet, L.A.; Saba, S.; Vandermeer, B. Falls prevention interventions for community-dwelling older adults: Systematic review and meta-analysis of benefits, harms, and patient values and preferences. Syst. Rev. 2024, 13, 289. [Google Scholar] [CrossRef]
- Sourial, N.; Beuscart, J.B.; Posłuszny, Ł.; Calafiore, M.; Sousa, S.S.; Sansone, E.; Zuber, M.; Vedel, I.; COVERAGE Collaborative Group. Challenges and solutions in recruiting older vulnerable adults in research. Int. J. Public Health. 2024, 69, 1607247. [Google Scholar] [CrossRef]
- Damme, M.J.; Ray-Degges, S. A Qualitative Study on Home Modification of Rural Caregivers for People with Dementia. J. Hous. Elder. 2016, 30, 88–105. [Google Scholar] [CrossRef]
- Yang, S.Y.; Fu, S.H.; Hsieh, P.L.; Lin, Y.L.; Chen, M.C.; Lin, P.H. Improving the care stress, life quality, and family functions for family-caregiver in long-term care by home modification. Ind. Health 2022, 60, 485–497. [Google Scholar] [CrossRef]
- Aliberti, M.J.R.; Covinsky, K.E. Home Modifications to Reduce Disability in Older Adults with Functional Disability. JAMA Intern. Med. 2019, 179, 211–212. [Google Scholar] [CrossRef]
- Keglovits, M.; Stark, S. Home Modifications to Improve Function and Safety in the United States. J. Aging Environ. 2020, 34, 110–125. [Google Scholar] [CrossRef]
- Nagasawa, S. Long-term Care Insurance Act and Home Care. JMAJ 2015, 58, 23–26. [Google Scholar]
- Rubenstein, L.Z.; Josephson, K.R. Falls and Their Prevention in Elderly People: What Does the Evidence Show? Med. Clin. North Am. 2006, 90, 807–824. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, Y.; Yang, G.-Y.; Jin, K. Age-Related Dysfunction in Balance: A Comprehensive Review of Causes, Consequences, and Interventions. Aging Dis. 2024, 16, 1. [Google Scholar] [CrossRef]
- Ganz, D.A.; Latham, N.K. Prevention of Falls in Community-Dwelling Older Adults. N. Engl. J. Med. 2020, 382, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Sturnieks, D.L.; St George, R.; Lord, S.R. Balance Disorders in the Elderly. Neurophysiol. Clin. 2008, 38, 467–478. [Google Scholar] [CrossRef]
- Pizzigalli, L.; Filippini, A.; Ahmaidi, S.; Jullien, H.; Rainoldi, A. Prevention of Falling Risk in Elderly People: The Relevance of Muscular Strength and Symmetry of Lower Limbs in Postural Stability. J. Strength Cond. Res. 2011, 25, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Pynoos, J.; Steinman, B.A.; Nguyen, A.Q.D. Environmental Assessment and Modification as Fall-Prevention Strategies for Older Adults. Clin. Geriatr. Med. 2010, 26, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Montero-Odasso, M. Falls in Cognitively Impaired Older Adults: Implications for Risk Assessment and Prevention. J. Am. Geriatr. Soc. 2018, 66, 367–375. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).