Supporting the Community’s Health Advocates: Initial Insights into the Implementation of a Dual-Purpose Educational and Supportive Group for Community Health Workers
Abstract
1. Introduction
2. Methods
2.1. Program Description
2.2. Developmental Evaluation Approach
2.3. Engagement Data
2.4. Ethics and Institutional Review Board (IRB) Statement
3. Results
3.1. Survey Completion
3.2. Participant Goals for Lunch and Learn Program
“I aim to establish best practices and share knowledge to enhance the support we provide to our clients. Additionally, I am seeking professional growth opportunities, as there are limited avenues for career advancement as a Community Health Worker (CHW) in Maryland. I hope to find opportunities that will contribute to both my professional development and the success of the organization.”
3.3. Topics of Interest for Lunch and Learn Program
3.4. Additional Supports for Lunch and Learn Program
3.5. Feedback and Revisions of the Lunch and Learn Program
“I just appreciate that there is a place for CHWs to gather.”
“I love this team and thank you so much.”
“You are the best support I have, so thank you.”
3.6. Evaluation of Core Competencies and Learning
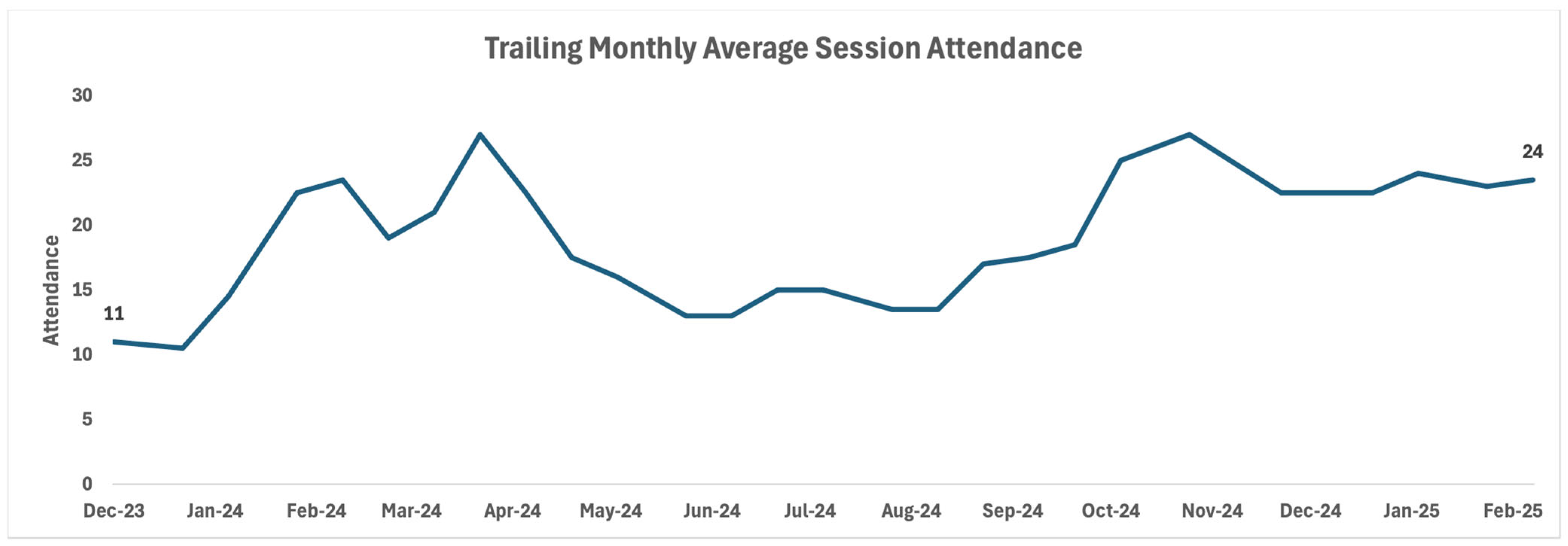
3.7. Lunch and Learn Engagement Data
4. Discussion
4.1. Program Impact and Findings
4.2. Participant Engagement and Professional Development
4.3. Global Relevance and Theoretical Framework
4.4. Limitations
4.5. Future Directions/Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Early, J.O.; Burke-Winkelmann, S.; Joshi, A. On the Front Lines of Prevention: Promotores de Salud and Their Role in Improving Primary Care for Latina Women, Families, and Communities. Glob. J. Health Educ. Promot. 2016, 17, 58–86. [Google Scholar] [CrossRef]
- Junghans, C.; Antonacci, G.; Williams, A.; Harris, M. Learning from the universal, proactive outreach of the Brazilian Community Health Worker model: Impact of a Community Health and Wellbeing Worker initiative on vaccination, cancer screening and NHS health check uptake in a deprived community in the UK. BMC Health Serv. Res. 2023, 23, 1092. [Google Scholar] [CrossRef] [PubMed]
- American Public Health Association. Available online: https://www.apha.org/apha-communities/member-sections/community-health-workers (accessed on 1 May 2025).
- Olaniran, A.; Smith, H.; Unkels, R.; Bar-Zeev, S.; van den Broek, N. Who is a community health worker?—A systematic review of definitions. Glob. Health Action 2017, 10, 1272223. [Google Scholar] [CrossRef] [PubMed]
- Galiatsatos, P.; Hailey-Fair, K.; Johnson, M.; Vanderpool, E.A.C.; Stewart, R.W.; Alexander, K.; Magsamen, S. Population health and community health: Brokering the two through art and community engagement. Front. Public Health 2024, 12, 1480795. [Google Scholar] [CrossRef] [PubMed]
- Hoops, K.; Bedner, A.; Kemper, E.; Aksamit, D.; O’Brien, C.; Johnson, M.K.; Stewart, R.W.; Maydan, D.D.; Hailey-Fair, K.; Galiatsatos, P. Demand for cardiopulmonary resuscitation and bleeding control skills training in an urban region: A feasibility review of a community engagement effort. Front. Public Health 2025, 13, 1339215. [Google Scholar] [CrossRef]
- Hartzler, A.L.; Tuzzio, L.; Hsu, C.; Wagner, E.H. Roles and functions of community health workers in primary care. Ann. Fam. Med. 2018, 16, 240–245. [Google Scholar] [CrossRef]
- Schmit, C.D.; Washburn, D.J.; LaFleur, M.; Martinez, D.; Thompson, E.; Callaghan, T. Community Health Worker Sustainability: Funding, Payment, and Reimbursement Laws in the United States. Public Health Rep. 2022, 137, 597–603. [Google Scholar] [CrossRef]
- Razai, M.S.; Kooner, P.; Majeed, A. Strategies and Interventions to Improve Healthcare Professionals’ Well-Being and Reduce Burnout. J. Prim. Care Community Health 2023, 14, 21501319231178641. [Google Scholar] [CrossRef]
- González-Rodríguez, R.; López-Castedo, A.; Pastor-Seller, E.; Verde-Diego, C. Burnout syndrome in the Health System: The case of social health workers. Enfermería Glob. 2020, 19, 152–161. [Google Scholar]
- Schaufeli, W.B.; Maassen, G.H.; Bakker, A.B.; Sixma, H.J. Stability and change in burnout: A 10-year follow-up study among primary care physicians. J. Occup. Organ. Psychol. 2011, 84, 248–267. [Google Scholar] [CrossRef]
- Papathanasiou, I.V. Work-related Mental Consequences: Implications of Burnout on Mental Health Status Among Health Care Providers. Acta Inf. Med. 2015, 23, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Rahman, R.; Ross, A.M.; Huang, D.; Kirkbride, G.; Chesna, S.; Rosenblatt, C. Predictors of burnout, compassion fatigue, and compassion satisfaction experienced by community health workers offering maternal and infant services in New York State. J. Community Psychol. 2023, 51, 1820–1838. [Google Scholar] [CrossRef] [PubMed]
- Salyers, M.P.; Bonfils, K.A.; Luther, L.; Firmin, R.L.; White, D.A.; Adams, E.L.; Rollins, A.L. The Relationship Between Professional Burnout and Quality and Safety in Healthcare: A Meta-Analysis. J. Gen. Intern. Med. 2017, 32, 475–482. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef]
- Aryankhesal, A.; Mohammadibakhsh, R.; Hamidi, Y.; Alidoost, S.; Behzadifar, M.; Sohrabi, R.; Farhadi, Z. Interventions on reducing burnout in physicians and nurses: A systematic review. Med. J. Islam. Repub. Iran. 2019, 33, 77. [Google Scholar] [CrossRef]
- Ceptureanu, S.I.; Ceptureanu, E.G.; Luchian, C.E.; Luchian, I. Community based programs sustainability. A multidimensional analysis of sustainability factors. Sustainability 2018, 10, 870. [Google Scholar] [CrossRef]
- Salsberg, J.; Macridis, S.; Garcia Bengoechea, E.; Macaulay, A.C.; Moore, S.; on behalf of the KSDPP School Travel Planning Committee. Engagement strategies that foster community self-determination in participatory research: Insider ownership through outsider championship. Fam. Pract. 2017, 34, 336–340. [Google Scholar] [CrossRef]
- Peterson, U.; Bergström, G.; Samuelsson, M.; Åsberg, M.; Nygren, Å. Reflecting peer-support groups in the prevention of stress and burnout: Randomized controlled trial. J. Adv. Nurs. 2008, 63, 506–516. [Google Scholar] [CrossRef]
- Hernandez-Salinas, C.; Marsiglia, F.F.; Oh, H.; Campos, A.P.; De La Rosa, K. Community Health Workers as Puentes/Bridges to Increase COVID-19 Health Equity in Latinx Communities of the Southwest U.S. J. Community Health 2023, 48, 398–413. [Google Scholar] [CrossRef]
- Schleiff, M.J.; Aitken, I.; Alam, M.A.; Damtew, Z.A.; Perry, H.B. Community health workers at the dawn of a new era: 6. Recruitment, training, and continuing education. Health Res. Policy Syst. 2021, 19, 113. [Google Scholar] [CrossRef]
- Brown, R.E. The process of community-building in distance learning classes. J. Asynchronous Learn. Netw. 2001, 5, 18–35. [Google Scholar] [CrossRef]
- Schwartz, S.L.; Wiley, J.L.; Kaplan, C.D. Community building in a virtual teaching environment. Adv. Soc. Work 2016, 17, 15–30. [Google Scholar] [CrossRef]
- Gabbay, J.; Le May, A. Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. BMJ 2004, 329, 1013. [Google Scholar] [CrossRef]
- Wieringa, S.; Greenhalgh, T. 10 years of mindlines: A systematic review and commentary. Implement. Sci. 2015, 10, 45. [Google Scholar] [CrossRef]
- Noar, A.P.; Jeffery, H.E.; Subbiah Ponniah, H.; Jaffer, U. The aims and effectiveness of communities of practice in healthcare: A systematic review. PLoS ONE 2023, 18, e0292343. [Google Scholar]
- Crawford, K.; Cordero, S.F.; Brasher, S.; Kaligotla, L.; Phan, Q.; Steiger, L.; Chicas, R.; Spaulding, A.; Swan, B.A. Evaluating the impact of a community health worker training program. J. Health Popul. Nutr. 2025, 44, 256. [Google Scholar]
- Alvisurez, J.; Clopper, B.; Felix, C.; Gibson, C.; Harpe, J.; Masterson, A.R.; Davis, B.; O’Keefe, E.; Humphries, D.; Perez-Escamilla, R. Funding Community Health Workers: Best Practices and the Way Forward; EliScholar: New Haven, CT, USA, 2013. [Google Scholar]
- Kash, B.A.; May, M.L.; Tai-Seale, M. Community health worker training and certification programs in the United States: Findings from a national survey. Health Policy 2007, 80, 32–42. [Google Scholar] [CrossRef]

| Themes | Topics |
|---|---|
| Health and Disease Topics | Narcan Training Overview Nutrition and Children’s Health Addressing Asthma & Lead Triggers in the Home Breast Cancer Screening Resources Lead Pipes and Water Cancer Screenings Vaccines Overdose/Opioid Crisis: How We Got Here and What Can Be Done Immunodeficiency Disorders |
| System and Resource Navigation | The Culture of Hospitals Outpatient Care Community Pharmacy Resources Hospital Resources and Survey Enrolling in Medicare/Enrolling in Private Insurance SNAP Benefits Advanced Care Planning Helping Clients Navigate MyChart |
| CHW Support and Professional Development | Health Literacy CHWs and Research CHW Burnout CHW Case Presentations CHW Roles Supporting Individuals with Rare Diseases |
| Community and Organizational Resources | Autism Society of Maryland/Pathfinders Caregiver Support Alzheimer’s Association of Maryland |
| 2024 | 2025 | |
|---|---|---|
| Most important | Networking | Problem solving/case work sharing |
| Support from fellow CHWs | Support from fellow CHWs | |
| Problem solving/case work sharing | Earning continuing education credits | |
| Least important | Earning continuing education credits | Networking |
| 2024 | 2025 | |
|---|---|---|
| Most important | Medical system information | Community resources |
| Support for CHWs | Health topics | |
| Community resources | Professional development | |
| Health topics | Medical system information | |
| Least important | Professional development | Support for CHWs |
| 2024 | 2025 | |
|---|---|---|
| Health topics | Pregnancy | Complementary/alternative medicine |
| HIV | Autism | |
| Palliative care | Chronic disease | |
| Oral health | Smoking cessation | |
| Eye health | Diabetes | |
| Autism | Healthy hearts | |
| Mental health | Asthma | |
| Nutrition | ||
| Children’s health | ||
| LGBTQ+ | ||
| Lead pipes | ||
| Water safety | ||
| Sickle cell | ||
| Insurance information | Medicare | Resources for uninsured patients |
| Medicaid | Navigating Medicare | |
| Commercial insurance | ||
| Applying to insurance | ||
| Open enrollment | ||
| SNAP qualifications | ||
| QMB or SLMB programs | ||
| Community resources | Adult protective services | Resources for unhoused |
| Therapy referrals | Transportation for Latino pop. | |
| UNICEF and WHO | Housing resources | |
| MTA mobility resources | Partnering with health lefts | |
| Black Mental Health Alliance | ||
| Autism Self-Advocacy Network | ||
| Safe Haven Baltimore | ||
| Autistic Women and Nonbinary Network | ||
| Professional development | Funding for CBOs | Healthcare system resources |
| Expert speakers | Using resources in communities | |
| Advocacy | ||
| Policy change | ||
| Health literacy | ||
| Effective communication | ||
| Networking support for resources | ||
| Networking support for jobs |
| Topic Area | Lunch and Learn Session Topic | One New Piece of Information Learned Today |
|---|---|---|
| Health | Autism | “Information about autism and how to be sensitive/culturally competent when navigating neurodivergence.” |
| “I learned that Stemming can be calming or due to anxiety.” | ||
| Alzheimer’s disease | “The information on how to get treated for early detection of Dementia.” | |
| “Risk factors for Alzheimer can be your lifestyle.” | ||
| Breast cancer | “That men can get breast cancer.” | |
| “Additional imaging required for dense breasts.” | ||
| Lead pipes and water | “That tap water is good for you [in Baltimore].” | |
| “I learned how our water Federal government works with local governments to make sure water sources and utilities work together to keep us safe.” | ||
| Resources | MyChart | “I have learned how to show patients how to navigate in my chart.” |
| “Learning how to in depth navigate MyChart and better understanding how to work the program. I did not have much experience previously so it was a nice general overview.” | ||
| Pathfinders for Autism | “More resources for help with patients diagnosed with Autism which I have a huge issue with obtaining information for patients & families.” | |
| “Resources on where to get help with finding help with autism. Also signs and what to look for.” | ||
| Professional development/ | CHW burnout | “Strategies to manage burnout.” |
| CHW Support | “Thinking of a box while taking deep breaths (4 and 4) was interesting and useful.” | |
| Health literacy | “I learned information in Health literacy and medical messaging.” | |
| “The real meaning of Health Literacy and Navigation.” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johnson, M.; Hailey-Fair, K.; Vanderpool, E.; DeJaco, V.; Chen, R.; Goersch, C.; Gately, U.E.; Toohey, A.; Galiatsatos, P. Supporting the Community’s Health Advocates: Initial Insights into the Implementation of a Dual-Purpose Educational and Supportive Group for Community Health Workers. Healthcare 2025, 13, 3288. https://doi.org/10.3390/healthcare13243288
Johnson M, Hailey-Fair K, Vanderpool E, DeJaco V, Chen R, Goersch C, Gately UE, Toohey A, Galiatsatos P. Supporting the Community’s Health Advocates: Initial Insights into the Implementation of a Dual-Purpose Educational and Supportive Group for Community Health Workers. Healthcare. 2025; 13(24):3288. https://doi.org/10.3390/healthcare13243288
Chicago/Turabian StyleJohnson, Marcie, Kimberly Hailey-Fair, Elisabeth Vanderpool, Victoria DeJaco, Rebecca Chen, Christopher Goersch, Ursula E. Gately, Amanda Toohey, and Panagis Galiatsatos. 2025. "Supporting the Community’s Health Advocates: Initial Insights into the Implementation of a Dual-Purpose Educational and Supportive Group for Community Health Workers" Healthcare 13, no. 24: 3288. https://doi.org/10.3390/healthcare13243288
APA StyleJohnson, M., Hailey-Fair, K., Vanderpool, E., DeJaco, V., Chen, R., Goersch, C., Gately, U. E., Toohey, A., & Galiatsatos, P. (2025). Supporting the Community’s Health Advocates: Initial Insights into the Implementation of a Dual-Purpose Educational and Supportive Group for Community Health Workers. Healthcare, 13(24), 3288. https://doi.org/10.3390/healthcare13243288






