Abstract
Purpose: This systematic review aimed to evaluate the effectiveness of virtual reality (VR) technology in cardiac rehabilitation (CR) patients, focusing on cardiopulmonary function, quality of life, adherence, and satisfaction. Methods: Conducted following PRISMA guidelines and registered on PROSPERO (CRD42025643632), this study systematically searched PubMed, Web of Science, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, Scopus, CNKI, and Wanfang Data. Meta-analysis was performed using RevMan 5.4 to assess the impact of VR interventions on cardiopulmonary function, quality of life (QOL), adherence, and satisfaction compared to conventional CR programs. Results: Twenty studies were included. Meta-analysis revealed that VR improved the 6 min walk test distance (MD: 34.9, 95% CI: 24.43, 45.37; p < 0.00001, I2 = 67%) and QOL (SMD: 0.63, 95% CI: 0.09, 1.17; p = 0.002, I2 = 86%). However, evidence regarding adherence and satisfaction was inconclusive. Conclusions: VR technology outperforms traditional CR in enhancing cardiopulmonary function and quality of life. While it might improve patient adherence, further research is necessary to confirm these findings.
1. Introduction
Cardiovascular diseases (CVDs) represent the predominant cause of global mortality, exerting a profound economic strain on healthcare systems worldwide. According to the American Heart Association, CVDs accounted for approximately 19.41 million deaths annually, with healthcare expenditures in the United States alone reaching $417.9 billion in 2021 [1]. Beyond the financial burden, CVDs significantly impaired patients’ quality of life, necessitating effective and accessible interventions [2]. International guidelines include cardiac rehabilitation (CR) as a cornerstone of secondary prevention [3,4,5,6,7]. Integrating medical evaluation, supervised exercise, risk factor modification, and patient education, CR has been demonstrated to be cost-effective [8] and clinically beneficial, with a community observational study revealing a greater than 12% reduction in 10-year all-cause mortality among Coronary Artery Bypass Grafting (CABG) patients enrolled in CR programs [9]. Furthermore, outpatient cardiac rehabilitation has demonstrated a mortality and morbidity reduction of approximately 25% compared to standard care [10,11]. Despite these compelling benefits, CR utilization remained suboptimal, with referral and participation rates ranging from 20% to 30% among eligible patients [10], and only 34% of referred patients enrolling in programs [12]. Among nations with low to middle incomes, these challenges were exacerbated by resource limitations, insufficient CR infrastructure, and exclusion from national health insurance schemes [13].
Virtual reality (VR), an innovative and rapidly advancing field, offers a promising solution to these barriers. VR utilizes computer-generated, immersive, three-dimensional environments to provide sensory feedback, enhancing user engagement and motivation [2]. Recent studies have explored the application of VR in CR, demonstrating its potential to mitigate negative emotional conditions like anxiety, depression, and stress [14,15,16,17,18,19,20,21,22]. VR may advance health equity and be more cost-effective, given the limited resources and lack of inclusion in national health insurance schemes [2,23,24]. However, the impact of VR on cardiopulmonary function remains controversial. For instance, Chen et al. [14] proposed that virtual reality could enhance motor performance in patients engaging in CR, whereas Blasco-Peris et al. [25] reported contradictory findings. This divergence might be explained by the limited sample size in the latter investigation, potentially resulting in insufficient statistical power to identify a significant effect. And its effects on broader health indicators are yet to be conclusively established, such as quality of life, patient satisfaction, and adherence.
This study aimed to address these critical gaps by systematically evaluating the efficacy of VR-based CR programs in enhancing cardiorespiratory fitness, QOL, and adherence among cardiovascular patients, compared to traditional CR approaches. By synthesizing the latest evidence, this research sought to elucidate the potential of VR to redefine conventional paradigms in CR, offering insights that could redefine rehabilitation paradigms and improve patient outcomes. The findings hold profound implications for clinical practice, policy-making, and the broader adoption of digital health technologies in cardiovascular care, ultimately contributing to the global effort to reduce the burden of CVDs.
2. Methods
2.1. Study Design
This research was conducted in strict accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 2020 [26] and prospectively registered with PROSPERO (ID: CRD42025643632). A systematic methodology was implemented, including standardized search strategies, dual-independent screening, and quality assessment to ensure transparency and reproducibility.
2.2. Literature Search and Screening
Two researchers systematically and independently searched it in nine databases, including PubMed, Web of Science, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library, Embase, Scopus, Wanfang Data, CNKI, and VIP database, from inception to 28 July 2025. The search method was in the form of mesh terms and keywords, such as “virtual reality” or “virtual gam*” or “virtual therapy*” or “Exergames*” or “Wii”; AND “Cardiovascular Disease” or “Cardiac Event*” or “Heart Disease” or “Cardiac Disorder*” or “Heart failure” or “cardiac rehabilitation” or “rehabilitation training” or “exercise training rehabilitation”, etc. In addition, we performed citation searches. The systematic retrieval process is provided in the Supplementary Table S1.
2.3. Eligibility Criteria
According to the PICOS principle, we set the inclusion and exclusion criteria. P (Population): Population with cardiovascular diseases involved in cardiac rehabilitation. I (Intervention): Intervention in the form of an exercise-based virtual reality rehabilitation program or exercise games, including immersive and non-immersive virtual environments. C (Comparison): Traditional cardiac rehabilitation or usual care. O (Outcomes): This study utilized the 6 min walk test (6MWT) and adherence as primary outcomes, with QOL and patient satisfaction assessed as secondary endpoints. The 6MWT was employed as a robust functional capacity indicator, reflecting cardiopulmonary fitness. This measure is widely adopted in clinical settings owing to its practicality, standardized protocol, and strong reproducibility [27,28]. Adherence was defined as the proportion of prescribed treatment sessions completed by the patient. Satisfaction was defined as the level of contentment with the treatment. S (Study design): A randomized controlled (RCT) design. Protocols, grey literature, and qualitative studies were excluded due to the exclusion criteria.
2.4. Data Extraction
First, all identified studies were imported into the reference management tool (NoteExpress V4.0). After removing repetitions, two researchers independently read the titles and abstracts one by one to obtain the preliminary results. Second, the full text should be reviewed against the eligibility criteria to select the relevant studies and extract data. Third, when a controversial article was encountered, a third researcher was involved in the discussion and consultation to make a decision.
2.5. Quality Evaluation
Initial assessments for risk of bias were conducted independently by two reviewers using the Cochrane Risk of Bias Tool 2 (RoB 2) [29]. The degree of agreement between reviewers was subsequently assessed, yielding a Cohen’s kappa statistic of 0.741 (p < 0.001), which indicates substantial consistency. To resolve disagreements, a third reviewer was consulted to reach a final consensus.
2.6. Data Integration and Analysis
Data analysis was performed using the software Review Manager (RevMan) version 5.4. For continuous outcomes, weighted mean difference (WMD) was used to assess 6MWT, and for the QOL that were assessed using different questionnaires, we used standardized mean difference (SMD) as the merging statistic and chi-square tests to determine inter-study heterogeneity. In accordance with Cochrane Handbook recommendations, heterogeneity was assessed through examination of study characteristics, sensitivity analyses, and subgroup analyses, with the sources of heterogeneity interpreted and reported. The confidence interval was 95%, and p < 0.05 indicated that the study was statistically significant.
3. Results
3.1. Study Selection
The database search obtained 1265 articles, of which 465 duplicates were removed, and 698 were excluded by reading the title and abstract. A total of 102 articles underwent preliminary screening based on their titles and abstracts; by reading the full text, we excluded 82 articles, 11 articles could not obtain the complete data, 28 were unrelated to outcome, 12 were non-randomized controlled trials, and 25 interventions did not meet criteria, 4 subjects did not meet criteria, 2 were data not extractable/applicable, and finally, 20 articles were included. The literature and the search flow chart are shown in Figure 1:
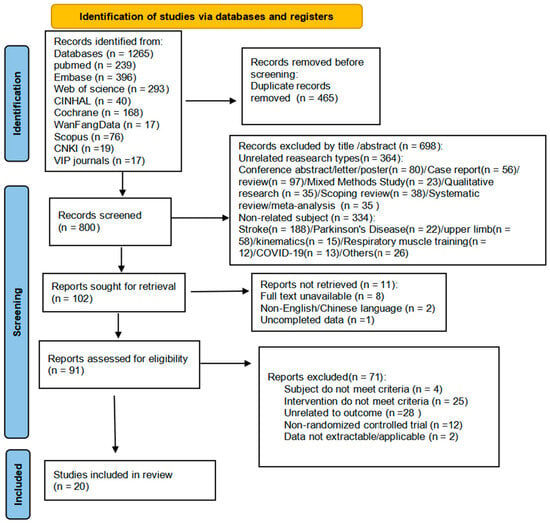
Figure 1.
Flow diagram of study selection.
3.2. Study Characteristics
We included 20 studies from 2013 to 2025, including five studies [2,29,30,31,32] in the Americas (four in Brazil [2,29,30,31] and one in the United States [32]), seven in Europe [33,34,35,36,37,38,39] (two in Spain [35,38], two in Portugal [34,37], one in Ireland [33], one in Finland [39], one in Sweden [36]), and eight in Asia [40,41,42,43,44,45,46,47] (four in China [40,41,42,43,47], two in Thailand [45,46], and one in Japan [44]). The study population was mainly ischemic heart disease, heart failure, patients after PCI, or patients undergoing cardiac rehabilitation, etc. Six studies [2,30,31,34,35,37] used the Kinect console for intervention; two studies used [33,36] Nintendo Wii games; one study [32] used the Bionautica Trails system, a biotrajectory system developed in the United States; one study [45] used Toucher, an upper limb movement software developed in Singapore; one study [44] used a balance movement assist robot developed in Japan; and one study [47] used the PICO neo 3, a Chinese device; one [39] employed novel technology-equipped tablets in Finnish households; and one study [43] use BioMaster Virtual scenario interactive training system in China. Another four studies [29,41,42,46] did not describe the type of VR device used. The studies are characterized in Table 1. VR intervention measures and control group details are given in Table S2.

Table 1.
Study characteristics table.
3.3. Risk Assessment of Quality Bias
Figure 2 presents all incorporated studies’ methodological quality evaluation results, detailing potential bias risks. Two studies [34,36] were at low risk of bias, thirteen studies [2,29,30,32,34,36,37,38,40,44,45,46,47] were at some concerns, and five [31,39,41,42,43] were assessed as high risk for bias. Of the included studies, 61.1% studies reported with low randomization bias; however, only 22.2% of the studies in domain 2, “Deviations from intended interventions”, reported low randomization bias as a result of VR being difficult to maintain blinding of the subjects and caregivers. In domain 3 “Missing outcome data” and domain 4 “Measurement of the outcome”, there are 63.9% studies that showed risk of bias and 30.6% studies reported some concerns. A total of 86.1% of studies showed a low risk of bias in domain 5 “Selection of the reported result”. The details are shown in Figure 2.
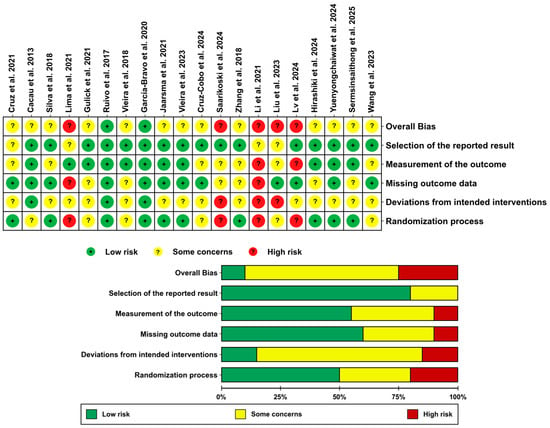
Figure 2.
Bias risk summary [2,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47].
3.4. Results from the Analysis of Variables
3.4.1. Cardiopulmonary Function
Figure 3 presents the pooled analysis of 6 min walking distance (6MWD) from twelve randomized controlled trials (n = 1335) [29,30,32,35,36,38,40,41,42,45,46,47] (MD: 34.9, 95% CI: 24.43, 45.37; p = 0.0004), though with substantial heterogeneity (I2 = 67%). Subgroup analyses revealed significant improvements in Cardiac Surgery Group (MD: 40.29 m, 95% CI: 10.16 to 70.42; p = 0.009; I2 = 63%), Coronary heart disease or heart failure group (MD: 36.38 m, 95% CI: 21.79 to 50.97; p < 0.00001; I2 = 0%), and Post-PCI or IABP group (MD: 29.24 m, 95% CI: 23.79 to 34.68; p < 0.00001; I2 = 0%). Subgroup differences were substantial (I2 = 0%), suggesting condition-specific efficacy. We omitted each study one at a time to perform a sensitivity analysis. The results showed that I2 changed from 67% to 0% and p < 0.00001 in Cacau et al. 2013 [29], which might explain the source of heterogeneity. The results are shown in Figure S1.
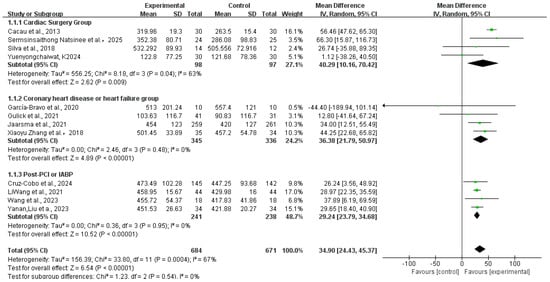
Figure 3.
Meta-analysis of the 6 min walking distance in summary [29,30,32,35,36,38,40,41,42,45,46,47]. Green squares: study weight; horizontal lines: 95% confidence intervals; diamond: pooled effect.
3.4.2. Quality of Life
Nine studies [29,31,33,34,35,39,40,44,47,48] reported the effect on quality of life. One study [35] was excluded from the meta-analysis due to a standard deviation of zero, which violates its statistical assumptions. Three studies [29,31,44] used the Functional Independence Measure (FIM) scale for measurement, three studies [35,40,47] used the SF-36 questionnaire, two studies [33,34] used the MacNew questionnaire, and one study [39] used the 15-D questionnaire. The results indicated that virtual reality technology enhanced the QOL for CR patients. SMD: 0.63,95% CI:0.09, 1.17; p = 0.0002, I2 = 86%, as shown in Figure 4. Sensitivity analysis employing the leave-one-out method did not pinpoint the origin of heterogeneity. We intended to conduct subgroup analyses according to different measurement scales. However, due to an insufficient number of studies (fewer than three) in certain subgroups (e.g., the ‘Macnew’ and ‘15-D’ subgroups), quantitative meta-analysis was not conducted for these groups to ensure statistical robustness.
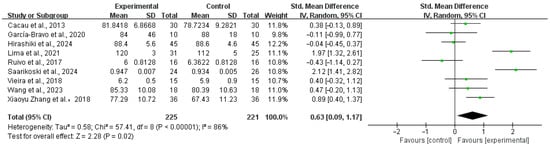
Figure 4.
Meta-analysis of the QOL in summary [29,31,33,34,35,39,40,44,47]. Green squares: study weight; horizontal lines: 95% confidence intervals; diamond: pooled effect.
3.4.3. Adherence
Seven studies [2,32,33,35,37,39,43] addressed adherence; the findings are suggestive of a potential benefit of virtual reality (VR) for improving adherence among CR patients, despite the lack of meta-analysis due to the different measurements. Adherence in four studies [2,33,37,39] was calculated as the percentage of patients attending the CR. One study [32] measured it by the number of people completing the recommended number of treatments by stage, and one study [43] categorized participants by adherence level (full, partial, non-adherent) and reported the proportion of each category as a percentage of the total population. Another study [35] did not report the results, although it described calculating by attendance at treatment. The impact on patient adherence outcomes is shown in Table 2.

Table 2.
Summary of adherence findings.
3.4.4. Satisfaction
Only two of the included studies [32,38] reported patient satisfaction scores, and the results of both studies indicated that patients responded more positively to treatment, with no statistical difference between in the virtual reality and control groups.
4. Discussion
This systematic review and meta-analysis aimed to evaluate the efficacy of virtual reality (VR)-based cardiac rehabilitation (CR) in improving cardiopulmonary function, QOL, adherence, and satisfaction among patients with cardiovascular diseases (CVDs). Our findings demonstrated that VR may improve cardiorespiratory fitness, particularly in patients who received early-phase intervention. However, the effect on quality of life requires cautious interpretation. And the evidence regarding adherence and satisfaction remains inconclusive. Compared with the previous systematic evaluation, the strength of this systematic review included adherence as the primary outcome measure and assessed the impact of the application of VR technology on adherence to cardiac rehabilitation. Although the progress of cardiopulmonary function and QOL was analyzed in the previous systematic evaluation, few studies were included, and the conclusions were inconsistent. Four studies [14,17,18,19] showed a possible improvement in cardiopulmonary function; three studies [20,25,49] showed no statistical difference and were unproven in terms of quality of life. Therefore, this study comprehensively summarized the evidence on cardiopulmonary function and QOL, increased the number of included studies, and improved the quality of the evidence. We also added analyses on adherence and satisfaction, which were not commonly found in previous systematic reviews.
4.1. Cardiopulmonary Function
The improvement in cardiorespiratory fitness, as measured by the 6 min walk test (6MWT), is a central finding of this study. The pooled analysis indicates that VR-based CR programs significantly outperform traditional CR in enhancing exercise capacity. These results are consistent with the findings of previous studies, which suggest that VR’s immersive and interactive nature can motivate patients to engage more actively in rehabilitation exercises [18]. Notably, subgroup analyses revealed that patients with cardiac surgery (MD: 40.29) and coronary heart disease or heart failure (MD: 36.38) benefited more than post-PCI (MD: 29.24). A potential factor contributing to these findings is the early initiation of the intervention [29,45]. This supports the earlier propositions put forth by several researchers [25,50]. The heterogeneity (I2 = 0%) and p = 0.46 in these subgroups strengthen the reliability of these findings. The physiological mechanisms by which VR interventions enhance patients’ cardiopulmonary function remain incompletely understood. Evidence from neurorehabilitation indicates that VR modulates neuroplasticity through sensory feedback, motor learning, and cognitive engagement [51]. Paralleling the neural activation mechanisms of portable neuromodulation techniques such as FES, tSCS, and tDCS [52]. Recent studies [53] further indicated that VR environments—even at constant exercise intensity—can elicit elevated subjective fatigue and cardiovascular responses through immersive scenarios (e.g., virtual slopes). Additionally, the visual stimuli provided by virtual reality can assist in regulating the brain’s cognitive systems, thereby influencing patients’ perceptions [54], and indirectly motivating them to increase their exercise engagement. In the future, more quantitative research can be added to further explore the physiological mechanisms by which VR affects cardiopulmonary function.
4.2. Quality of Life (QOL)
QOL is a crucial prognostic indicator of cardiovascular disease. Our study found that virtual reality intervention demonstrated a small and statistically marginal improvement in patient QOL, with considerable heterogeneity observed across the included studies. Nine studies contributed data to the meta-analysis on this outcome measure. Three studies [35,40,47] analyzed the impact on QOL on eight dimensions, including somatic functioning, role limitations, pain, socialization, and mental health, and reported higher scores in the intervention group. Evidence regarding between-group differences, especially in mental health outcomes, is limited to a single study [40], highlighting the need for further investigation to confirm these results. In contrast, three studies [35,40,47] assessed the total FIM scores, and no significant difference was observed between the two groups. In previous systematic reviews, Blasco-Peris et al. [25] and Peinado-Rubia et al. [17] conducted meta-analyses on QOL and showed small, non-statistically significant improvements in QOL, which is consistent with the findings in our analysis. Differently, our study added three studies that used FIM as a measurement tool, yielding statistically different results. Subgroup analyses were not conducted in this study due to limited data. Future research should incorporate standardized core outcome sets to further evaluate the effect of VR on QOL in CR patients.
4.3. Adherence
The role of VR in improving CR adherence remains inconclusive. This systematic review was not quantitatively analyzed due to limited studies and inconsistent measurement tools. Three studies [2,39,43] reported significant between-group differences, while Gulick et al. [32] observed higher completion rates in controls, attributing non-adherence primarily to external factors (e.g., work resumption, insurance issues). Two studies [33,37] were underpowered to detect a difference in median attendance, which might explain the nonsignificant finding. In addition, we retrieved two ongoing studies that may provide further insights [24,55], though preliminary evidence suggests a potential trend toward improved adherence with VR, consistent with findings in neurological rehabilitation [56]. Future research efforts should therefore aim to incorporate larger, diverse populations from multiple centers to corroborate these preliminary observations. Adherence is an important indicator used to measure the quality of cardiac rehabilitation, and there is no standardized measurement. Most studies have used adherence as measured by treatment attendance, while a few studies have reported dropout or withdrawal rates [57]. It demonstrated a dose–response correlation between participation in CR sessions and long-term results, with an estimated 1% reduction in mortality per CR session attended [58,59,60]. Evidence suggested a dose-dependent effect, where participation in thirty-six or more sessions correlated with significantly lower four-year risks of all-cause mortality and acute myocardial infarction relative to lower intervention frequencies. Thus, the American College of Cardiology/American Heart Association Task Force on Performance Measures recommends that ≥36 cardiac rehabilitation sessions be classified as a complete dose and used as the clinical target for cardiac rehabilitation quality measures [61]. In addition, the factors impacting patient adherence are complex. Studies have shown that higher social motivation, fewer sleep problems, and higher motor competence and self-efficacy are independently associated with patient motor adherence [62,63]. In terms of how virtual reality promotes adherence in rehabilitation, Micheluzzi et al. [64,65] proposed a mid-range theory to outline the mechanism of its effectiveness, which suggested that the effects of virtual displays on an individual consist of proximal and distal outcomes. Proximal outcomes were categorized as psychological (motivation, self-efficacy, mood) and physical (pain management, muscle strength) responses, and the distal outcomes were categorized as adherence, which interacted with each other. Virtual reality technology promotes the distraction of negative external stimuli associated with illness and healthcare environments, as well as the perception of positive emotions, through the activation of distal mediators, thus improving patient adherence. Interventional studies could be added to this in the future. The gamified elements of VR, such as real-time feedback and goal-oriented tasks, may enhance patient motivation and adherence to exercise regimens [66,67].
4.4. Satisfaction
Two studies [32,35] reflected patient satisfaction with the treatment, primarily attributed to the VR experience itself and its content design, though it was not comparable to traditional cardiac rehabilitation. Despite the high variability between studies, its positive impact on patient treatment has been supported by other literature. For example, Morgan H. et al. [65] utilized an immersive VR video for preoperative education of cardiac catheterization patients, which was effective in reducing preoperative anxiety and improving patient satisfaction. The application of VR as a supplementary approach for managing postoperative pain [68] could improve patient satisfaction, especially in patients undergoing laparoscopic surgery [69]. These findings emphasized VR’s potential in pain management, psychological care, and rehabilitation. However, given the subjective nature of satisfaction measures, future research should focus on comparative analyses across populations, VR program designs, and short-, medium-, and long-term outcomes.
Although the benefits of VR in enhancing cardiac rehabilitation outcomes are evident, practical implementation still faces certain challenges, such as limited acceptance among elderly patients and those with low awareness of VR technology [67]. Prolonged use of VR can cause motion sickness, along with high costs, limited reimbursement options, and insufficient training resources. Additionally, for patients with different conditions (such as atrial fibrillation), the anxiety stemming from the disease itself should be taken into account. Future research may draw upon successful rehabilitation models, such as the multidisciplinary approach proposed by Angelica Cersosimo et al. [70] integrating VR interventions into standard care pathways to deliver customized rehabilitation programs for patients across diverse settings, such as remote or home environments.
4.5. Limitations
This study has several limitations. The primary limitation of this review is the scarcity of available data across the included studies, which precluded quantitative meta-analysis and definitive conclusions, particularly regarding patient compliance and satisfaction, limiting the strength of our conclusions and reducing the overall evidence quality. Secondly, significant heterogeneity was observed across studies, particularly in cardiopulmonary function and QOL outcomes, likely due to variations in patient populations (e.g., participant demographics, baseline disease severity) and VR intervention protocols (including VR intervention parameters and types). Although Standardized Mean Differences (SMDs) were used to enable pooling, the combination of heterogeneous quality of life instruments may introduce bias. Thirdly, the lack of standardized measurement criteria for adherence and satisfaction posed analytical challenges. Although we attempted to minimize publication bias by extracting data from a consistent post-intervention period (2–3 months), some studies only reported short-term follow-up data. Additionally, to ensure the quality of evidence, this study did not include grey literature, which may have resulted in the omission of some unpublished data. Methodological enhancements in future studies should encompass sufficient statistical power through expanded recruitment, standardized data collection procedures, and proactive monitoring of VR-related side effects. Additionally, more rigorous studies are needed to elucidate VR’s impact on adherence and satisfaction while emphasizing the risk of bias assessment.
5. Conclusions
In conclusion, this study provides compelling evidence that VR-based CR can enhance cardiorespiratory fitness and QOL in CVD patients. However, the inconclusive findings on adherence and satisfaction highlight the need for further research to optimize VR interventions and address methodological challenges. By advancing our understanding of VR’s potential and limitations, this study contributes to the ongoing evolution of digital health technologies in cardiovascular care, offering a new idea for future research and clinical practice.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare13222969/s1, Table S1: The search strategy of the systematic review and meta-analysis; Table S2: Details of VR Intervention Measures and Control Group; Figure S1: Sensitivity analysis of the 6MWT in summary [29,30,32,35,36,38,40,41,42,45,46,47]. Green squares: study weight; horizontal lines: 95% confidence intervals; diamond: pooled effect.
Author Contributions
Q.C. made the primary contribution to this manuscript. Q.Z. and F.L. made a second contribution to this manuscript. H.Y. and S.W. were responsible for the academic guidance and review of the article. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
This paper has no funding support and no conflict of interest statement.
References
- Martin, S.S.; Aday, A.W.; Allen, N.B.; Almarzooq, Z.I.; Anderson, C.A.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Bansal, N.; Beaton, A.Z.; et al. 2025 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation 2025, 151, e41–e660. [Google Scholar]
- Da Cruz, M.M.; Ricci-Vitor, A.L.; Borges, G.L.; Da Silva, P.F.; Turri-Silva, N.; Takahashi, C.; Grace, S.L.; Vanderlei, L.C. A Randomized, Controlled, Crossover Trial of Virtual Reality in Maintenance Cardiovascular Rehabilitation in a Low-Resource Setting: Impact on Adherence, Motivation, and Engagement. Phys. Ther. 2021, 101, pzab071. [Google Scholar] [CrossRef]
- Riegel, B.; Moser, D.K.; Buck, H.G.; Dickson, V.V.; Dunbar, S.B.; Lee, C.S.; Lennie, T.A.; Lindenfeld, J.; Mitchell, J.E.; Treat-Jacobson, D.J.; et al. Self-Care for the Prevention and Management of Cardiovascular Disease and Stroke: A Scientific Statement for Healthcare Professionals From the American Heart Association. J. Am. Heart Assoc. 2017, 6, e006997. [Google Scholar] [CrossRef]
- Mehra, V.M.; Gaalema, D.E.; Pakosh, M.; Grace, S.L. Systematic review of cardiac rehabilitation guidelines: Quality and scope. Eur. J. Prev. Cardiol. 2020, 27, 912–928. [Google Scholar] [CrossRef]
- Task Force Members; Montalescot, G.; Sechtem, U.; Achenbach, S.; Andreotti, F.; Arden, C.; Budaj, A.; Bugiardini, R.; Crea, F.; Cuisset, T.; et al. 2013 ESC guidelines on the management of stable coronary artery disease: The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur. Heart J. 2013, 34, 2949–3003. [Google Scholar] [CrossRef]
- Balady, G.J.; Ades, P.A.; Bittner, V.A.; Franklin, B.A.; Gordon, N.F.; Thomas, R.J.; Tomaselli, G.F.; Yancy, C.W. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: A presidential advisory from the American Heart Association. Circulation 2011, 124, 2951–2960. [Google Scholar] [CrossRef]
- Ades, P.A. Cardiac rehabilitation and secondary prevention of coronary heart disease. N. Engl. J. Med. 2001, 345, 892–902. [Google Scholar] [CrossRef] [PubMed]
- Shepard, D.S.; Zakir, S.; Gaalema, D.E.; Ades, P.A. Cost-Effectiveness of Cardiac Rehabilitation in Older Adults with Coronary Heart Disease. J. Cardiopulm. Rehabil. Prev. 2024, 44, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Pack, Q.R.; Goel, K.; Lahr, B.D.; Greason, K.L.; Squires, R.W.; Lopez-Jimenez, F.; Zhang, Z.; Thomas, R.J. Participation in cardiac rehabilitation and survival after coronary artery bypass graft surgery: A community-based study. Circulation 2013, 128, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Khadanga, S.; Savage, P.; Keteyian, S.; Yant, B.; Gaalema, D.; Ades, P. Cardiac rehabilitation: The gateway for secondary prevention. Heart 2024, 110, 1427–1436. [Google Scholar] [CrossRef]
- Arena, R.; Williams, M.; Forman, D.E.; Cahalin, L.P.; Coke, L.; Myers, J.; Hamm, L.; Kris-Etherton, P.; Humphrey, R.; Bittner, V.; et al. Increasing referral and participation rates to outpatient cardiac rehabilitation: The valuable role of healthcare professionals in the inpatient and home health settings: A science advisory from the American Heart Association. Circulation 2012, 125, 1321–1329. [Google Scholar] [CrossRef] [PubMed]
- Sandesara, P.B.; Lambert, C.T.; Gordon, N.F.; Fletcher, G.F.; Franklin, B.A.; Wenger, N.K.; Sperling, L. Cardiac rehabilitation and risk reduction: Time to “rebrand and reinvigorate”. J. Am. Coll. Cardiol. 2015, 65, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Sérvio, T.C.; Britto, R.R.; de Melo Ghisi, G.L.; da Silva, L.P.; Silva, L.D.; Lima, M.M.; Pereira, D.A.; Grace, S.L. Barriers to cardiac rehabilitation delivery in a low-resource setting from the perspective of healthcare administrators, rehabilitation providers, and cardiac patients. BMC Health Serv. Res. 2019, 19, 615. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Cao, L.; Xu, Y.; Zhu, M.; Guan, B.; Ming, W.K. Effectiveness of virtual reality in cardiac rehabilitation: A systematic review and meta-analysis of randomized controlled trials. Int. J. Nurs. Stud. 2022, 133, 104323. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.; Zhang, M.; You, Z.; Kong, J. Meta-analysis of the application effects of virtual reality technology in cardiac rehabilitation patients. J. Cardiovasc. Dis. 2023, 31, 104–109. (In Chinese) [Google Scholar]
- Turan Kavradim, S.; Yangöz, Ş.T.; Özer, Z. Effectiveness of virtual reality interventions on physiological and psychological outcomes of adults with cardiovascular disease: A systematic review and meta-analysis. J. Nurs. Scholarsh. 2023, 55, 949–966. [Google Scholar] [CrossRef]
- Peinado-Rubia, A.B.; Verdejo-Herrero, A.; Obrero-Gaitan, E.; Osuna-Perez, M.C.; Cortes-Perez, I.; Garcia-Lopez, H. Non-Immersive Virtual Reality-Based Therapy Applied in Cardiac Rehabilitation: A Systematic Review with Meta-Analysis. Sensors 2024, 24, 903. [Google Scholar] [CrossRef]
- Jia, Y.Y.; Song, J.P.; Yang, L. Can virtual reality have effects on cardiac rehabilitation? An overview of systematic reviews. Curr. Probl. Cardiol. 2024, 49, 102231. [Google Scholar] [CrossRef]
- Zhang, M.; Liu, S.; Xiong, X.; Liu, M.; Wang, Y.; Yang, Y.; Xiang, Q. Effectiveness of virtual reality in cardiac rehabilitation patients for exercise capacity and negative emotions: A systematic review and meta-analysis. Medicine 2024, 103, e40812. [Google Scholar] [CrossRef]
- Wang, S.; Jiang, J.; Zhang, C.; Lv, M.; Xu, H.; Meng, H.; Guo, L. Effect of Virtual Reality-based Cardiac Rehabilitation on Mental Health and Cardiopulmonary Function of Individuals with Cardiovascular Disease: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2024, 106, 949–960. [Google Scholar] [CrossRef]
- Cortés-Pérez, I.; Obrero-Gaitán, E.; Verdejo-Herrero, A.; Zagalaz-Anula, N.; Romero-del-Rey, R.; García-López, H. Immersive virtual reality reduces depression, anxiety and stress in patients with cardiovascular diseases undergoing cardiac rehabilitation: A systematic review with meta-analysis. Heart Lung 2024, 70, 102–111. [Google Scholar] [CrossRef]
- Lear, S.A.; Singer, J.; Banner-Lukaris, D.; Horvat, D.; Park, J.E.; Bates, J.; Ignaszewski, A. Improving access to cardiac rehabilitation using the internet: A randomized trial. Stud. Health Technol. Inform. 2015, 209, 58–66. [Google Scholar] [PubMed]
- Marsden, J.; Dennett, R.; Gibbon, A.; Knight Lozano, R.; Freeman, J.A.; Bamiou, D.E.; Harris, C.; Hawton, A.; Goodwin, E.; Creanor, S.; et al. Vestibular Rehabilitation in Multiple Sclerosis: Randomized Controlled Trial and Cost-Effectiveness Analysis Comparing Customized with Booklet Based Vestibular Rehabilitation for Vestibulopathy. Neurorehabil Neural Repair 2025, 39, 687–700. [Google Scholar] [CrossRef] [PubMed]
- Brewer, L.C.; Abraham, H.; Clark, I.I.I.D.; Echols, M.; Hall, M.; Hodgman, K.; Kaihoi, B.; Kopecky, S.; Krogman, A.; Leth, S.; et al. Efficacy and Adherence Rates of a Novel Community-Informed Virtual World-Based Cardiac Rehabilitation Program: Protocol for the Destination Cardiac Rehab Randomized Controlled Trial. J. Am. Heart Assoc. 2023, 12, e30883. [Google Scholar] [CrossRef] [PubMed]
- Blasco-Peris, C.; Fuertes-Kenneally, L.; Vetrovsky, T.; Sarabia, J.M.; Climent-Paya, V.; Manresa-Rocamora, A. Effects of Exergaming in Patients with Cardiovascular Disease Compared to Conventional Cardiac Rehabilitation: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3492. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Sullivan, M.J.; Thompson, P.J.; Fallen, E.L.; Pugsley, S.O.; Taylor, D.W.; Berman, L.B. The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure. Can. Med. Assoc. J. 1985, 132, 919–923. [Google Scholar]
- Cacau, L.D.; Oliveira, G.U.; Maynard, L.G.; Araújo Filho, A.A.; Silva Junior, W.M.; Cerqueria Neto, M.L.; Antoniolli, A.R.; Santana-Filho, V.J. The use of the virtual reality as intervention tool in the postoperative of cardiac surgery. Rev. Bras. Cir. Cardiovasc. 2013, 28, 281–289. [Google Scholar] [CrossRef]
- Silva, J.P.; Novaes, L.F.; Santos, L.C.; Galindo, B.P.; Cavalcante, M.A.; Araújo, B.C.; Pacagnelli, F.L.; Freire, A.P. Effects of Conventional and Virtual Reality Cardiovascular Rehabilitation in Body Composition and Functional Capacity of Patients with Heart Diseases: Randomized Clinical Trial. Int. J. Cardiovasc. Sci. 2018, 31, 619–629. [Google Scholar] [CrossRef]
- Lima, H.D.; Souza, R.D.; e Santos, A.S.; Borges, D.L.; Guimaraes, A.R.; Ferreira, G.V.; Barros, R.M.; Cordeiro, A.L. Virtual reality on pulmonary function and functional independence after coronary artery bypass grafting: Clinical trial. Am. J. Cardiovasc. Dis. 2020, 10, 499–505. [Google Scholar] [PubMed]
- Gulick, V.; Graves, D.; Ames, S.; Krishnamani, P.P. Effect of a Virtual Reality-Enhanced Exercise and Education Intervention on Patient Engagement and Learning in Cardiac Rehabilitation: Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e23882. [Google Scholar] [CrossRef]
- dos Santos Ruivo, J.M.; Karim, K.; O’Shea, R.; Oliveira, R.C.; Keary, L.; O’Brien, C.; Gormley, J.P. In-class Active Video Game Supplementation and Adherence to Cardiac Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2017, 37, 274–278. [Google Scholar] [CrossRef]
- Vieira, Á.; Melo, C.; Machado, J.; Gabriel, J. Virtual reality exercise on a home-based phase III cardiac rehabilitation program, effect on executive function, quality of life and depression, anxiety and stress: A randomized controlled trial. Disabil. Rehabil. Assist. Technol. 2018, 13, 112–123. [Google Scholar] [CrossRef]
- García-Bravo, S.; Cano-de-la-Cuerda, R.; Domínguez-Paniagua, J.; Campuzano-Ruiz, R.; Barreñada-Copete, E.; López-Navas, M.J.; Araujo-Narváez, A.; García-Bravo, C.; Florez-Garcia, M.; Botas-Rodríguez, J.; et al. Effects of Virtual Reality on Cardiac Rehabilitation Programs for Ischemic Heart Disease: A Randomized Pilot Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 8472. [Google Scholar] [CrossRef]
- Jaarsma, T.; Klompstra, L.; Ben Gal, T.; Ben Avraham, B.; Boyne, J.; Bäck, M.; Chialà, O.; Dickstein, K.; Evangelista, L.; Hagenow, A.; et al. Effects of exergaming on exercise capacity in patients with heart failure: Results of an international multicentre randomized controlled trial. Eur. J. Heart Fail. 2021, 23, 114–124. [Google Scholar] [CrossRef] [PubMed]
- Vieira, Á.; Melo, C.; Noites, A.; Machado, J.; Mendes, J. Home-based Virtual Reality Exercise Program During the Maintenance Stage of Cardiac Rehabilitation: A Randomized Controlled Trial. Int. J. Cardiovasc. Sci. 2023, 36, e20190177. [Google Scholar] [CrossRef]
- Cruz-Cobo, C.; Bernal-Jiménez, M.Á.; Calle, G.; Gheorghe, L.L.; Gutiérrez-Barrios, A.; Cañadas, D.; Tur, J.A.; Vázquez-García, R.; Santi-Cano, M.J. Efficacy of a Mobile Health App (eMOTIVA) Regarding Compliance with Cardiac Rehabilitation Guidelines in Patients with Coronary Artery Disease: Randomized Controlled Clinical Trial. JMIR Mhealth Uhealth 2024, 12, e55421. [Google Scholar] [CrossRef]
- Saarikoski, E.O.; Roiha, E.T.; Kiviniemi, A.M.; Cerdán-De-las-Heras, J.; Perkiömäki, J.; Kaikkonen, K.S.; Tulppo, M.P. Adherence to exercise after an acute coronary syndrome: A 6-month randomized controlled trial. Front. Physiol. 2024, 15, 1319907. [Google Scholar] [CrossRef]
- Zhang, X.; Zhao, H. Application of Baduanjin combined with virtual rehabilitation training system in exercise rehabilitation of elderly patients with stable angina. Glob. Chin. Med. 2018, 11, 1233–1237. (In Chinese) [Google Scholar]
- Wang, L. Virtual Home Exercise Rehabilitation Using Digital Technology: Effects on Physical and Emotional Improvement in Coronary Heart Disease Patients After Interventional Surgery. Nurs. Pract. Res. 2021, 18, 333–337. (In Chinese) [Google Scholar]
- Liu, Y.; Wu, H.; Han, H.; Zang, S.; Ren, Y.; Zhang, J.; Zhang, H. The Impact of Bridge Exercise Combined with Virtual Reality Rehabilitation Training on Physiological and Psychological Functions in Patients with Intra-Aortic Balloon Antegrade Traction. Gen. Nurs. 2023, 21, 2956–2958. (In Chinese) [Google Scholar]
- Lv, L.; Wen, F.; Yan, Q.; Jia, J.; Liu, S. Application of Immersive Virtual Reality Technology in Cardiac Rehabilitation Education for Patients with Percutaneous Coronary Intervention. J. Prev. Med. Inf. 2024, 40, 1120–1125, 1132. (In Chinese) [Google Scholar]
- Hirashiki, A.; Shimizu, A.; Kamihara, T.; Kokubo, M.; Hashimoto, K.; Ueda, I.; Sato, K.; Kawamura, K.; Itoh, N.; Murohara, T.; et al. Randomized Controlled Trial of Cardiac Rehabilitation Using the Balance Exercise Assist Robot in Older Adults with Cardiovascular Disease. J. Cardiovasc. Dev. Dis. 2024, 11, 133. [Google Scholar] [CrossRef] [PubMed]
- Yuenyongchaiwat, K.; Boonkawee, T.; Pipatsart, P.; Tavonudomgit, W.; Sermsinsaithong, N.; Songsorn, P.; Charususin, N.; Harnmanop, S.; Namdaeng, P.; Kulchanarat, C.; et al. Effects of virtual exercise on cardio-pulmonary performance and depression in cardiac rehabilitation phase I: A randomized control trial. Physiother. Res. Int. 2024, 29, e2066. [Google Scholar] [CrossRef] [PubMed]
- Sermsinsaithong, N.; Yuenyongchaiwat, K.; Thanawattano, C.; Buekban, C.; Kulchanarat, C.; Buranapuntalug, S.; Wattanananont, K.; Satdhabudha, O. Effects of a Home-Based Rehabilitation Exercise Program on Cardiorespiratory Performance in Community-Dwelling Adults Who Underwent Heart Surgery: Randomized Controlled Trial. JMIR Rehabil. Assist. Technol. 2025, 12, v12i–v18i. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yang, S.L.; Luo, S.X.; Tong, H.; Fang, Q.; Guo, Y.Z. Effects of virtual reality in phase I cardiac rehabilitation training for elderly coronary heart disease patients after percutaneous coronary intervention. Sheng Li Xue Bao 2023, 75, 953–961. [Google Scholar] [PubMed]
- Klompstra, L.; Hägglund, E.; Jaarsma, T.; Kato, N.P.; Strömberg, A. Effects of exergaming and yoga on exercise capacity and physical and mental health in heart failure patients: A randomized sub-study. Eur. J. Cardiovasc. Nurs. 2025, 24, 389–398. [Google Scholar] [CrossRef]
- Bashir, Z.; Misquith, C.; Shahab, A.; Has, P.; Bukhari, S. The impact of Virtual Reality on Anxiety and Functional Capacity in Cardiac Rehabilitation: A Systematic Review and Meta-analysis. Curr. Probl. Cardiol. 2023, 48, 101628. [Google Scholar] [CrossRef] [PubMed]
- Klompstra, L.; Jaarsma, T.; Stromberg, A. Exergaming to increase the exercise capacity and daily physical activity in heart failure patients: A pilot study. BMC Geriatr. 2014, 14, 119. [Google Scholar] [CrossRef]
- Wankhede, N.L.; Koppula, S.; Ballal, S.; Doshi, H.; Kumawat, R.; Raju, S.; Arora, I.; Sammeta, S.S.; Khalid, M.; Zafar, A.; et al. Virtual reality modulating dynamics of neuroplasticity: Innovations in neuro-motor rehabilitation. Neuroscience 2025, 566, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Bartloff, J.; Lanotte, F.; O’Brien, M.K.; Jayaraman, A. Advancing gait rehabilitation through wearable technologies: Current landscape and future directions. Expert Rev. Med. Devices 2025, 22, 1105–1116. [Google Scholar] [CrossRef]
- Bruce, R.M.; Rafferty, G.F.; Finnegan, S.L.; Sergeant, M.; Pattinson, K.T.; Runswick, O.R. Incongruent virtual reality cycling exercise demonstrates a role of perceived effort in cardiovascular control. J. Physiol. 2025, 603, 5149–5161. [Google Scholar] [CrossRef]
- Takeo, Y.; Hara, M.; Otsuru, N.; Taihei, T.; Kawasoe, R.; Sugata, H. Modulation of thermal perception by VR-based visual stimulation to the embodied virtual body. Behav. Brain Res. 2025, 480, 115395. [Google Scholar] [CrossRef]
- Micheluzzi, V.; Casu, G.; Sanna, G.D.; Canu, A.; Iovino, P.; Caggianelli, G.; Vellone, E. Improving adherence to rehabilitation for heart failure patients through immersive virtual reality (VIRTUAL-HF): A protocol for a randomized controlled trial. Contemp. Clin. Trials 2024, 138, 107463. [Google Scholar] [CrossRef]
- Alwadai, B.; Lazem, H.; Almoajil, H.; Hall, A.J.; Mansoubi, M.; Dawes, H. Telerehabilitation and Its Impact Following Stroke: An Umbrella Review of Systematic Reviews. J. Clin. Med. 2024, 14, 50. [Google Scholar] [CrossRef] [PubMed]
- Annesi, J.J.; Mazas, J. Effects of virtual reality-enhanced exercise equipment on adherence and exercise-induced feeling states. Percept. Mot. Ski. 1997, 85 Pt 1, 835–844. [Google Scholar] [CrossRef] [PubMed]
- Hammill, B.G.; Curtis, L.H.; Schulman, K.A.; Whellan, D.J. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation 2010, 121, 63–70. [Google Scholar] [CrossRef]
- Doll, J.A.; Hellkamp, A.; Thomas, L.; Ho, P.M.; Kontos, M.C.; Whooley, M.A.; Boyden, T.F.; Peterson, E.D.; Wang, T.Y. Effectiveness of cardiac rehabilitation among older patients after acute myocardial infarction. Am. Heart J. 2015, 170, 855–864. [Google Scholar] [CrossRef]
- Martin, B.J.; Hauer, T.; Arena, R.; Austford, L.D.; Galbraith, P.D.; Lewin, A.M.; Knudtson, M.L.; Ghali, W.A.; Stone, J.A.; Aggarwal, S.G. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation 2012, 126, 677–687. [Google Scholar] [CrossRef]
- Thomas, R.J.; Balady, G.; Banka, G.; Beckie, T.M.; Chiu, J.; Gokak, S.; Ho, P.M.; Keteyian, S.J.; King, M.; Lui, K.; et al. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J. Am. Coll. Cardiol. 2018, 71, 1814–1837. [Google Scholar] [CrossRef] [PubMed]
- Jaarsma, T.; Klompstra, L.; Strömberg, A.; Ben Gal, T.; Mårtensson, J.; van der Wal, M.H.; HF-Wii Study Team; Jaarsma, T.; Strömberg, A.; Klompstra, L.; et al. Exploring factors related to non-adherence to exergaming in patients with chronic heart failure. ESC Heart Fail 2021, 8, 4644–4651. [Google Scholar] [CrossRef]
- Klompstra, L.; Jaarsma, T.; Strömberg, A.; Evangelista, L.S.; van der Wal, M.H. Exercise Motivation and Self-Efficacy Vary Among Patients with Heart Failure—An Explorative Analysis Using Data from the HF-Wii Study. Patient Prefer. Adherence 2021, 15, 2353–2362. [Google Scholar] [CrossRef]
- Micheluzzi, V.; Vellone, E.; Iovino, P. A Situation-Specific Theory on the Use of Immersive Virtual Reality in Rehabilitation for Patients with Disabilities. Holist. Nurs. Pract. 2025, 39, 71–79. [Google Scholar] [CrossRef]
- Morgan, H.; Nana, M.; Phillips, D.; Gallagher, S. The Effect of a VIrtual RealiTy Immersive Experience Upon Anxiety Levels, Procedural Understanding, and Satisfaction in Patients Undergoing CArdiac CaTHeterization: The VIRTUAL CATH Trial. J. Invasive Cardiol. 2021, 33, E681–E686. [Google Scholar] [CrossRef]
- Dias, P.; Silva, R.; Amorim, P.; Lains, J.; Roque, E.; Serôdio, I.; Pereira, F.; Santos, B.S. Using Virtual Reality to Increase Motivation in Poststroke Rehabilitation. IEEE Comput. Graph. Appl. 2019, 39, 64–70. [Google Scholar] [CrossRef]
- da Cruz, M.M.; Grigoletto, I.; Ricci-Vitor, A.L.; da Silva, J.M.; Franco, M.R.; Vanderlei, L.C. Perceptions and preferences of patients with cardiac conditions to the inclusion of virtual reality-based therapy with conventional cardiovascular rehabilitation: A qualitative study. Braz. J. Phys. Ther. 2022, 26, 100419. [Google Scholar] [CrossRef]
- Groninger, H.; Stewart, D.; Fisher, J.M.; Tefera, E.; Cowgill, J.; Mete, M. Virtual reality for pain management in advanced heart failure: A randomized controlled study. Palliat. Med. 2021, 35, 2008–2016. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.; Elshazly, T.; Pokuri, K.; Apai, C.; Rothkrug, A.; Hasoon, J.; Chung, M.; Ye, Z.; Bhayani, S.; Kaye, A.D.; et al. Virtual Reality for Postoperative Pain Management: A Review of Current Evidence. Curr. Pain Headache Rep. 2024, 28, 1307–1319. [Google Scholar] [CrossRef] [PubMed]
- Cersosimo, A.; Condello, F.; Colombo, F.; Pierucci, N.; Arabia, G.; Matteucci, A.; Metra, M.; Adamo, M.; Vizzardi, E.; LAFazia, V.M. Cardiac rehabilitation in patients with atrial fibrillation. Minerva Cardiol. Angiol. 2025. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).