Abstract
Background/Objectives: Older patients are more susceptible to the process of understanding and retrieving information. To provide adequate preoperative information, reduce their vulnerability and anxiety, and thereby facilitate pre-, intra-, and postoperative care, the adoption of new information technologies is essential. This study aimed to explore elderly patients’ experiences and perceptions of a Virtual Reality (VR)-based preoperative informational tool designed for individuals scheduled to undergo TKA. Method: A qualitative content analysis was conducted from February to June 2025 based on 14 semi-structured post-discharge interviews. Participants were recruited as part of a randomized controlled trial. Results: One main theme and two categories describe patients’ experiences of using VR information, which is perceived as a valuable supplement to standard preoperative information. The category “Using VR as an information tool” includes how patients experienced the immersive environment, how it affected them, and their views on using the VR glasses. The category “Apply the information provided” described how patients evaluated and applied the VR content in relation to their expectations and the actual surgical experience. Conclusions: Immersive virtual reality (VR) shows promise as a preoperative information tool, improving patients’ understanding of the perioperative process and supporting engagement in their own care. Its effectiveness depends on reliable technical performance and adaptation to individual needs. VR should complement, not replace, communication with healthcare professionals. Further research is needed to identify optimal timing for VR delivery and its impact on preoperative anxiety and patient experience.
1. Introduction
Total knee arthroplasty (TKA) is one of the most commonly performed elective orthopedic procedures worldwide, driven by the aging population and the increasing demand for a longer active life [1]. In Denmark alone, more than 10,000 primary knee arthroplasties are performed annually, and the numbers are expected to rise due to demographic shifts and increasing life expectancy [2]. Internationally, similar trends are observed; for instance, in the United States, the annual volume of TKA is projected to exceed 1.5 million by 2030 [3]. The primary patient population consists of older adults, often with multiple comorbidities, making preoperative optimization and education particularly critical for this group [4]. Older patients often face unique challenges in understanding complex preoperative information due to factors such as cognitive decline, hearing or visual impairments, and unfamiliarity with medical terminology [5]. This heterogeneous patient group includes many individuals who undergo repeated procedures or bilateral knee surgery. Consequently, variations in information needs are influenced by patients’ social context, level of health literacy, and previous experiences [6,7]. Traditional methods of information delivery, such as written materials or verbal consultations, may be insufficient to ensure adequate comprehension and retention in this demographic [8,9,10]. Consequently, patients may undergo surgery with unrealistic expectations, elevated anxiety levels, or limited understanding of the perioperative process [9,10,11], which can place additional strain on healthcare resources and reduce overall system efficiency [12]. Patient satisfaction and perceived surgical success have been shown to correlate strongly with the degree to which preoperative expectations are fulfilled [13]. Ensuring that patients are adequately informed and mentally prepared for surgery contributes to improved emotional well-being and better clinical outcomes, including reduced postoperative pain, shorter hospital stays, lower complication rates, and faster functional recovery [14,15].
Virtual Reality (VR) has emerged as a promising technological tool, offering immersive environments that can support patients’ mental preparation for surgery [16,17].
VR technology enables users to experience complete immersion within an artificial environment featuring interactive visual, auditory, and motor domains. By presenting three-dimensional multimedia that can be manipulated and delivered through head-mounted displays and noise-reducing headphones, VR enables patients to engage with a controlled, interactive representation of the perioperative environment—such as the operating theater, preoperative waiting area, and post-anesthesia care unit (PACU)—with the potential to foster psychological readiness and a sense of reassurance before surgery [18,19,20,21]. Although both written and VR-based methods aim to inform and prepare patients, they differ in their mode of delivery, cognitive load, and potential emotional impact. Traditional methods are static and require active interpretation, whereas VR offers a multimodal learning experience that may reduce cognitive demands by presenting information in a contextualized visual format [18,21,22]. Cybersickness is a notable limitation of VR, which is affected by technology, content, and duration of exposure. However, further research is needed to understand better the impact of user-related factors, such as age and gender [23]. Given that older individuals are not typically familiar with immersive digital technologies, there is a particular need to explore how they engage with and respond to VR-based information. For this group, receiving clear and understandable preoperative information may represent a significant opportunity to regain a sense of control in an otherwise unfamiliar clinical setting. Feeling informed and capable may further contribute to an enhanced patient’s sense of competence and encourage active involvement in their care. Such experiences resonate strongly with the principles of person-centered care, which emphasize the value of acknowledging patients’ capabilities. Despite the increasing use of immersive digital technologies, such as VR, in healthcare, research exploring elderly patients’ experiences with these tools for preoperative information remains limited.
While previous studies have examined the use of VR for patient education in various contexts [24], most have primarily focused on quantitative outcomes, such as anxiety and knowledge scores [25,26]. However, there remains limited research exploring the experiences of patients scheduled to undergo TKA in receiving preoperative information through immersive VR environments.
Understanding how elderly patients perceive and engage with VR in the surgical pathway is crucial, particularly in procedures associated with anxiety and extensive rehabilitation, including TKA. Therefore, this study aimed to explore elderly patients’ experiences and perceptions of a VR-based preoperative informational tool designed for individuals scheduled to undergo TKA.
2. Method
2.1. Study Design
A qualitative design was chosen to explore patients’ subjective experiences and meanings related to using VR as preoperative information. A qualitative approach enabled an understanding of perceived usefulness, realism, and emotional responses beyond numerical outcomes [27].
Data were collected through individual, semi-structured interviews. A qualitative content analysis, as described by Graneheim and Lundman [24], was used to identify patterns, variations, differences, and similarities in the participants’ perceptions. This study followed the Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines [28].
2.2. The Settings and Participants
The study was conducted at a public anesthetic department in Denmark, where pre-anesthesia assessment before TKA surgery is routinely performed as part of the standardized clinical care pathway. Participants were recruited from the VR intervention arm of the ongoing randomized controlled trial. A total of 14 patients were included for individual interviews using convenience sampling from the intervention group in the randomized controlled trial (RCT; registered at ClinicalTrials.gov: NCT06292663).
Patients allocated to the intervention group received a VR experience that illustrated their patient’s journey during the scheduled preoperative assessment at the hospital, one to two weeks before surgery. The VR session lasted approximately eight minutes and was delivered via a PICO G3 4K (Qingdao, China) head-mounted display (HMD) in a quiet consultation room. A trained healthcare professional was present to introduce the equipment, assist with setup, and address any immediate questions.
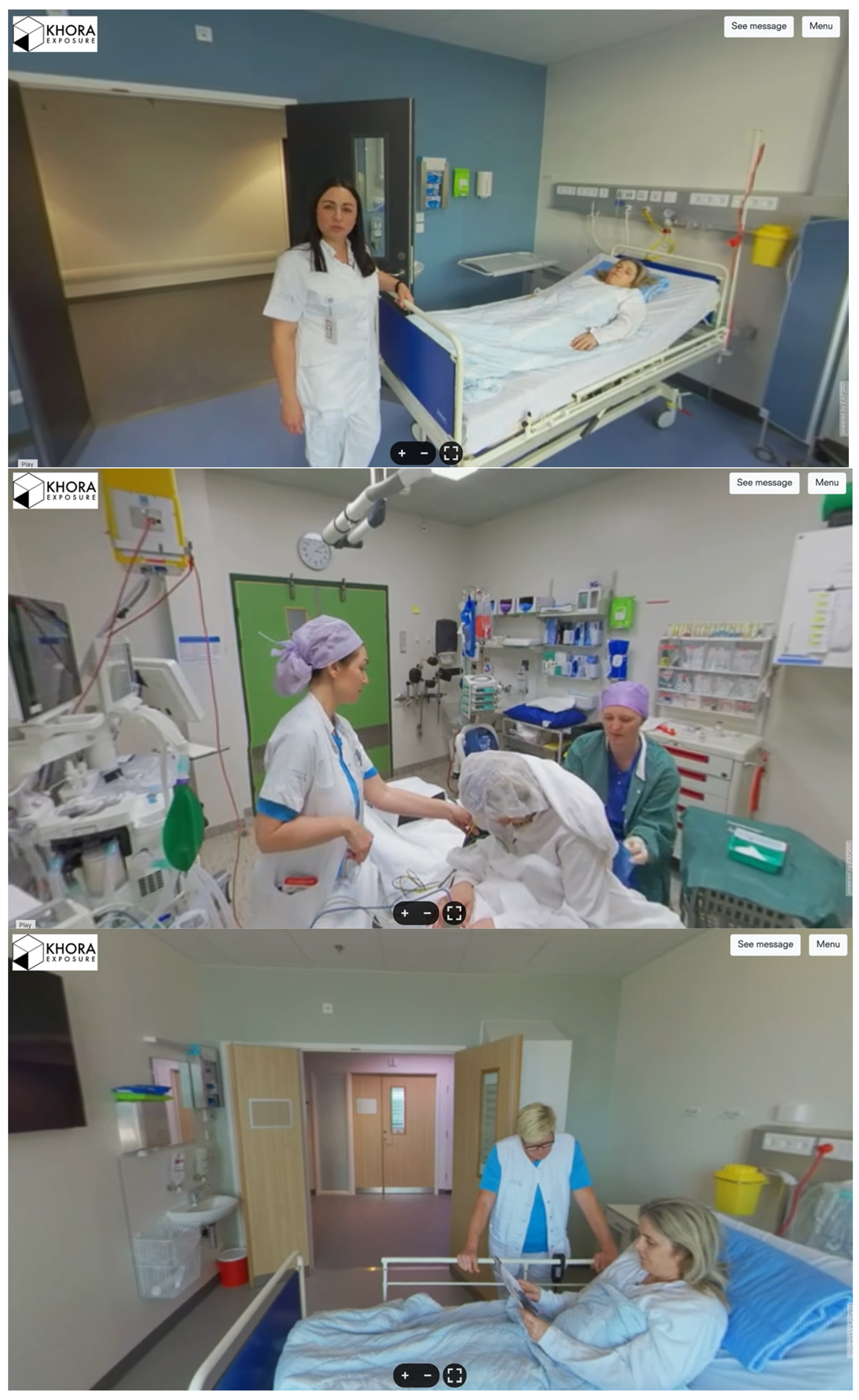
The VR content was developed in partnership with the Danish technology firm KHORA (Copenhagen, Denmark) [29], providing a guided and immersive walkthrough of the patients’ surgical journey from admission to postoperative recovery. The content presents the patient’s journey on the day of surgery from a first-person perspective, recorded with a 360° camera. The film follows a patient entering the ward, meeting the nurse, entering the operating theatre (excluding footage of the surgery itself), awakening in the recovery area, and ending when the patient returns to the ward. The narrative is voice-guided with natural ambient sound, filmed under standard lighting conditions from a standing viewpoint to simulate the patient’s perspective. All scenes were filmed using natural clinical lighting and edited in sequential order, without the addition of any effects. The narrative followed the chronological flow of the surgical day.
Figure 1 provides example screenshots of the content.
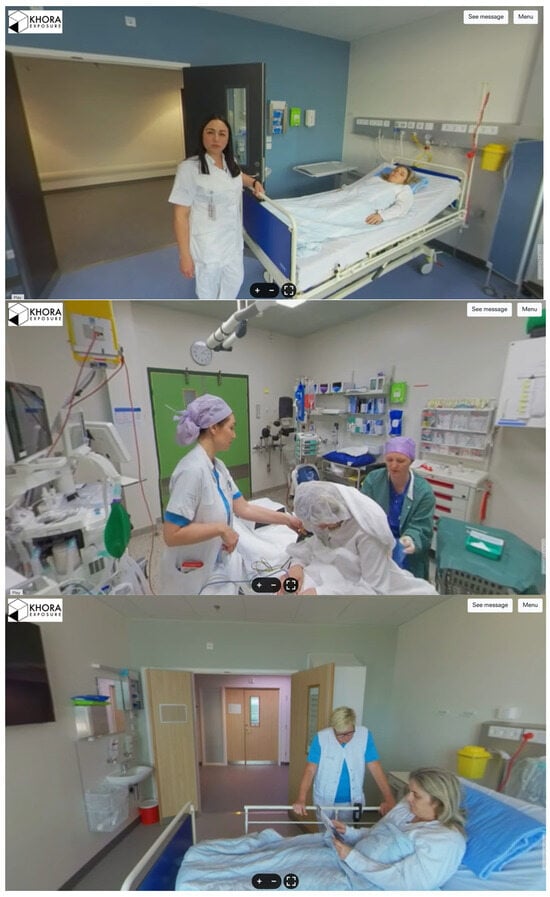
Figure 1.
Screenshots of VR content.
Patients were eligible for inclusion if they were scheduled for TKA under spinal anesthesia, aged 18 years or older, capable of understanding the study protocol, including its potential risks and benefits, and provided written informed consent. Patients were excluded if they were unable to read or understand Danish, were deemed uncooperative by the investigators, suffered from claustrophobia or related anxiety disorders, had conditions preventing the use of VR equipment, or had significant visual or auditory impairments that could interfere with the VR experience. The characteristics of the participants are presented in Table 1.

Table 1.
Characteristics of Study Participants (n = 14).
2.3. Data Collection
Participants were contacted after hospital discharge and invited to participate in the qualitative study. As part of the initial trial enrollment process, all participants were informed that they might be approached for a follow-up qualitative interview to explore their experiences with the intervention in the future. The study was explained both orally and in a written informed consent form. All interviews were subsequently conducted via telephone within two to four weeks postoperatively to capture recent experiences.
A semi-structured interview guide was used based on research on whether VR could be considered part of the surgical pathway [30]. The guide included open-ended questions beginning with the question “Can you describe your thoughts on the 360 VR experience you saw before the surgery?” All questions were designed to explore participants’ perceptions of VR-based preoperative information, their emotional and cognitive responses to the technology, how the information aligned with their experience, and the perceived usefulness of the intervention in preparing for surgery and recovery. K.L.L. and M.J. conducted all interviews, which were audio-recorded using an encrypted, password-protected tablet device, and later transcribed by Viceron.com (Copenhagen, Denmark). Interviews were conducted by telephone at times chosen by the participants, in settings they selected themselves, all of which were in their homes.
Telephone interviews, which lasted a median of 10.5 min (range 6.5–16 min), were conducted between February and June 2025, with a median of 12 days (range 7–23 days) post-discharge. Data saturation was considered reached when at least two consecutive interviews produced no new codes or subcategories relevant to the research question [27].
The number of participants included in this study appears sufficient, particularly as the sample represents a homogenous group within a narrowly defined research topic [31].
2.4. Data Analysis
Interview recordings were transcribed using Viceron.com. To ensure accuracy, all transcribed recordings were verified by the researchers against the original audio recordings. When the text was imprecise due to the use of the AI Tool, the text was corrected accordingly. All interviews were.
The transcribed text was systematically analyzed using a qualitative content analysis approach [32]. The analysis focused on both manifest and latent content, starting with each transcript being read multiple times to gain a comprehensive understanding of its content. CS and KL were mainly responsible for the analysis. NVivo v.14.24.3 (Denver, CO, USA) was used to extract 92 meaning units of the text relevant to the research aim, which were identified and condensed while preserving their core meanings. The condensed meaning units were labeled with 12 codes. In the analysis, codes were compared and grouped into six subcategories, which were then abstracted into two broader categories, as described by Graneheim and Lundman [32]. The main theme, latent content, describes the phenomena. Examples of data analysis are listed in Table 2.

Table 2.
Examples from data analysis.
3. Ethical Considerations
The study received ethical approval from The Region Zealand, Approval No: EMN-2023–08767. This study was conducted in accordance with the Declaration of Helsinki, the General Data Protection Regulation (GDPR), and applicable national data protection laws. All participants were informed about the study and provided written and audio-recorded consent prior to their participation.
4. Results
The Main Theme, “Individualized VR information with VR means additional value to the patient experience,” is illustrated by the categories “Using VR as an information tool” and “Apply the information provided,” with subcategories, presented in Table 3. Describing patients’ experiences of receiving preoperative information through VR head-mounted devices in relation to their TKA.

Table 3.
Overview of the results.
4.1. Using VR as an Information Tool
This category describes the experience of wearing glasses and engaging in immersive activities, as well as their impact on the patient’s emotions.
4.2. Adapting to VR Glasses
Patients generally described their experience of using VR glasses as novel and engaging. Well, that was the first time I tried it. Wearing a pair of glasses like that, it seemed like you were in the operating room and on the way in, and all that. Yeah, it was very lifelike (Patient 10).
For many, this was their first encounter with VR technology, and their reactions ranged from fascination to initial discomfort. Most patients quickly adapted to the unfamiliar equipment, with one noting, “Of course, it felt strange with those glasses, but I got used to it very quickly” (P4). However, several challenges that impact the overall experience have been described. Some patients noted technical limitations, including issues with sound synchronization and the need to physically turn their head or rotate their body to follow visual content. This occasionally resulted in mismatches between the audio and visuals, requiring patients to adjust their position to engage with the 360-degree view fully. These challenges led some patients to express skepticism about the technology, suggesting that the same content may have been equally effective when presented on a standard screen. Although these technical issues did not dominate the overall impression, they were described as minor annoyances that slightly interfered with the intended immersive experience. Despite this, the patients were able to see the benefits and potential.
4.3. Take Part in an Immersive Experience
This category reveals how patients experienced the immersive experience of the VR system. Several patients described the sensation of “being there” in the hospital environment, described as “Very realistic, like being in the operating room and on the way in” (P10).
Visual and auditory elements were appreciated for making the information more engaging and easier to understand. Patients emphasized that detailed imagery helped them retain content more effectively than traditional paper-based formats. For many, the experience was described as either positive or exciting. The immersive experience was highly valued and perceived as educational and therefore considered useful by the patients. The VR-based information influenced the patients’ emotional state before surgery. While some patients reported feeling calm or unconcerned from the outset, others described how the video contributed to their reassurance and reduced their anxiety. Several patients indicated that the VR experience helped them feel more at ease and secure by providing familiarity with the clinical setting. “Yes, it’s like you’re being held by the hand the whole way through” (P5). Additionally, the impact of the VR experience could also serve to de-dramatize patients’ expectations of how the procedure was expected to be carried out. Patients also reported that the VR content helped alleviate their fears or clarify previous concerns. The visual content provided more prosperous and diverse information than traditional written information. Others, however, reported no emotional impact either because they had no pre-existing fear or because the video confirmed what they had already expected. Thus, those who were not nervous or emotionally affected before the procedure experienced no differences. Although participants were asked, according to the interview guide, whether the VR experience affected their expectations regarding pain during the surgical process, none spontaneously reported any influence on their perception of pain.
4.4. Apply the Information Provided
This category describes the perception when the VR content did not match the real experience. Additionally, how the content met expectations before surgery influenced the compliance and understanding of the process.
4.5. Discrepancies Between VR and Clinical Experience Are Annoying
Patients reacted when the VR-based information was not fully aligned with their real-world clinical experience. Although the information was not perceived as intentionally misleading, some patients felt it was inaccurate. While a few considered the discrepancies to be minor and unimportant, others found them misleading or frustrating, which affected their perception of the technology. Patients commented that the VR film presented a “too polished” version of the surgical experience. They expressed that they missed important procedural details, such as variations in spinal anesthesia, and that it may take several attempts to succeed with spinal anesthesia.
“They should inform patients more that sometimes it doesn’t work the first time” (P13).
Patients noted that the clinical pathway they encountered on the day of surgery did not always correspond precisely with that shown in the VR simulation. Variations included differences in the number of staff members present during specific stages or where specific procedures were performed. “For example, they weren’t as good at hitting my spine or spinal cord compared to the Virtual Reality version and things like that.” (P8). However, these discrepancies were not experienced as problematic and did not negatively influence patients’ overall sense of preparedness or trust in the care they received.
4.6. Influence on Expectations and Compliance
This category describes how the VR-based information influenced patients’ expectations regarding the entire surgical procedure and their ability to comply with instructions. For several patients, the VR experience primarily confirmed their existing expectations. For them, nothing changed; they received confirmation, which illustrates how the VR content validated their existing expectations. Others described a better sense of procedural clarity, which helped them feel more secure and ready to comply with instructions: “Yes, yes, I knew I had to curl up and those things—so yes, it was fine” (P2). A few patients found the information less impactful, reporting that their expectations remained unchanged or that there was a mismatch due to prior negative experiences. Some noted that they would have preferred more detailed information about the surgical procedure. Overall, their influence on expectations and compliance ranged from reassurance and confirmation to a perceived lack of added value. They emphasized that the use of precise language without reliance on medical jargon was highly beneficial. Patients described how the VR experience contributed to their understanding of the procedural tasks, thereby increasing their sense of deeper understanding. For many, the visualization of the patient journey provided clarity and confirmed their existing understanding of the tasks that would take place on the day of surgery. It also helped them prepare for participation and decision-making, in which they could be involved. Patients found it interesting to prepare for what was going to be an actively involved experience. This was perceived as an advantage in understanding the process step by step. “It gave me an insight into what was going to happen, and the process—I was happy about that” (P1). For some patients, the VR session confirmed what they already knew, whereas others described it as adding a new dimension to their preparation. The experience was that it was essential to gain insight into the process, observe different environments, and develop an understanding of how it works.
5. Discussion
The main finding of this study was that a contextualized visual format for information, combined with VR, provides added value to patients. This is particularly true when tailored to meet each patient’s specific information needs. This type of presentation offers clarity on aspects that are often overlooked in traditional written and oral information delivery. Particularly valuable is the immersive format, which engages multiple senses featuring interactive visual, auditory, and motor domain elements [30].
The head-mounted display was generally perceived as easy to use and well accepted by the patients in this study. In line with a scoping review [33], patients consider VR beneficial for improving their understanding of medical information. Schubbe et al. [34] conducted a systematic review and meta-analysis, demonstrating that the use of pictorial health information enhances knowledge and understanding among patients and consumers, particularly benefiting individuals with lower health literacy. Patients in the current study highlighted the added value of visuals and found the pre-information video more detailed and easier to comprehend. Many people are visual learners, which may explain the positive effects of VR [35]. None of the patients experienced cybersickness despite using fully immersive VR. Nevertheless, it remains essential that traditional information materials are available for patients who are unable or unwilling to engage in VR technology for various reasons. Some problematic occasions and technical issues required patients to turn their heads to view the content fully, which was bothersome. Although this issue was resolved, it underscores the importance of technical reliability and the significance of healthcare professionals’ attitudes. In a study of multidisciplinary hospital staff, Shiner et al. [36] found that despite limited previous VR experience, the healthcare professionals expressed positive attitudes toward VR but noted barriers such as inadequate IT support, limited technical skills, and time constraints.
The immersive experience allowed patients to construct knowledge from their own perspective through self-driven, interactive processes. Since patients often have a limited and varied understanding of the perioperative pathway, VR helped address their individual needs. For some, it was valuable to gain insight into the roles of different healthcare professionals and the timing of their involvement. For those who had undergone the same surgery previously, the experience served as an update or confirmation, whereas for first-time patients, it provided entirely new information. Some patients were already calm and without worries, but still appreciated the VR experience, which made them feel equally or even more secure. These findings align with van der Linde-van den Bor’s study [6] that examined patients’ information needs and perceptions of VR in preoperative patient education.
Many patients expressed worries and concerns regarding the procedure. The immersive experience helped de-escalate and calm them, reduce anxiety, and foster a sense of security and positivity, as they knew what would happen and what was expected of them. Previous studies have also demonstrated that VR education reduces anxiety and fear, while improving patient satisfaction across various healthcare settings, yielding positive results [17,24]. Insights into what would happen and what would be expected helped reduce the asymmetrical relationship between patients and healthcare professionals. With greater knowledge gained through VR, patients in the current study perceived that they could participate more actively in their care and decision-making. Vogel et al. [37] identified several barriers to shared decision-making. To overcome these challenges, patients must be recognized as having the competence and authority to engage meaningfully in the process. None of the patients in this study reported that VR affected their perioperative pain experience. This aligns with the findings of a randomized controlled trial by Bekelis et al. [18], in which patients who were exposed to a preoperative immersive VR experience during the perioperative period reported greater satisfaction, improved preparedness, and reduced stress. However, no differences were observed in pain levels.
Many patients felt that VR presented an idealized version of the process that did not reflect potential difficulties. For example, more healthcare staff were present during the actual procedure than were depicted in the VR experience. Several patients reported experiencing multiple attempts before spinal anesthesia was successfully administered, which left them feeling unprepared because the VR scenario depicted only a single successful attempt. One possible way to address this and accommodate individual information needs could be a solution, such as that used in the study by van Rijn et al. [24], where patients were given the option to access additional information about specific rooms or procedures within the VR environment if they wished.
In contrast, VR content met patient expectations positively. The use of explicit language and the absence of medical terms were considered beneficial. Improvements, such as a better understanding of the positioning required during spinal anesthesia, have contributed to increased compliance. However, the perceptions of those with previous negative experiences remained unchanged. The complexity of patients’ heterogeneous information needs, influenced by personal preferences and previous hospital experiences, is confirmed in a study by van der Linde-van den Bor et al. (2022) [6].
The primary advantage of VR is its immersive experience, which fosters emotional engagement, a quality often lacking in traditional information methods. Patients in this study also highly valued the opportunity to gain insight into the process, as it helped them prepare for situations in which they could actively participate and make informed choices. From a clinical perspective, VR can be a valuable supplement to existing preoperative education methods.
Methodological Considerations
The current study aimed to investigate elderly patients’ experiences and perceptions of a preoperative informational tool with VR for patients scheduled to undergo TKA. The qualitative content analysis was a suitable method for investigating the perspectives and perceptions of patients who had used VR. To enhance the credibility, dependability, confirmability, and transferability of this study, we rigorously followed all the steps described by Granheim and Lundman [32]. The inclusion of patients did not consider whether patients had previously undergone knee replacement; 10 of 14 patients had prior experience with the procedure.
The depth of patients’ responses when reflecting on receiving information via VR in interviews may be strongly influenced by their previous experiences and knowledge. This factor accounts for the observed variation in interview duration. Although the interviews were relatively short (averaging 10 min), data saturation was achieved, as recurring themes emerged, and participants provided rich and focused reflections on their VR experiences. Telephone interviews were chosen to minimize participant burden and allow patients to respond from the comfort of their own homes. Although nonverbal cues were not captured, previous studies suggest that telephone interviews can obtain equally rich verbal data and enhance openness in sensitive contexts [26,38]. Prior experience with TKA surgery provides patients with a basis for reflection, which is essential for how they assimilate information delivered via VR. However, as information needs are highly individual, this is not considered to have affected the study’s credibility [32]. An equal gender distribution ensured that the perceptions and experiences of both genders were reflected. However, the present study did not stratify experiences by gender, age, or educational level. Future research could explore whether these demographic factors influence how patients perceive and benefit from VR-based information. The technical issues that required patients to move their heads to follow the presentation may have affected the study’s credibility [32]. However, these problems were correctable, highlighting the importance of providing prompt technical support. Considering the rapid development of VR technology, the dependability of this study is strengthened by its short data collection period [32]. The fact that two researchers conducted the interviews may have influenced the dependability [32]. To minimize this risk, the interviews were conducted consistently, using a standardized interview guide.
The confirmability is strengthened by discussions of the findings among all authors during data analysis [32]. Any discrepancies were resolved through dialogue and re-examination of the transcripts. Furthermore, a clear description of the interviews and analysis is provided, with the results presented and illustrated with quotations to facilitate readers’ assessment of the study’s transferability [32].
6. Conclusions
Information delivered through immersive VR improved both the subjective and objective understanding of the perioperative process and promoted conditions for patient involvement in their own care. VR technology has the potential to meet individual information needs. The challenges lie in ensuring that technical solutions function as intended and in optimizing the conditions for delivering information according to individual needs. Technology, however, cannot replace the information provided by healthcare professionals; rather, it should be regarded as a valuable complement that enhances, but does not substitute for, human interaction and clinical expertise.
Moreover, the optimal timing for delivering preoperative information requires further investigation to determine when it yields the most significant benefit within the perioperative process. Future research should also address the effects of VR-based information on patients’ anxiety and preoperative worry.
Author Contributions
K.L.L., C.S., A.G. and P.J. contributed to the conception and design of the study. Investigation, K.L.L., M.J. and N.W.C. Data analysis and interpretation of data, K.L.L., C.S. and P.J. Drafting the article, and final approval of the version to be submitted K.L.L., C.S. and P.J. Revising it critically for important intellectual content, and final approval of the version to be submitted C.S., A.A., A.G. and P.J. All authors have read and agreed to the published version of the manuscript.
Funding
Interreg Öresund-Kattegat-Skagerrak Co-financing by the European Union (NYPSID 20358639).
Institutional Review Board Statement
Ethical approval was granted by the Ethics Committee, Approval No: EMN-2023–08767 on 27 October 2023. The study adheres to the principles outlined in the Helsinki Declaration.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The qualitative data on which this analysis was conducted are not publicly available due to ethical concerns regarding the confidentiality of participants. Further, consent was not obtained from participants to share information from interview transcripts with third parties not involved in the research, and the ethical approval for this study does not permit the sharing of such information.
Acknowledgments
The authors would like to thank the participants who shared their experiences and contributed to the insights of this study.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could be perceived to influence their work.
References
- Gao, J.; Xing, D.; Dong, S.; Lin, J. The primary total knee arthroplasty: A global analysis. J. Orthop. Surg. 2020, 15, 190. [Google Scholar] [CrossRef]
- Robertsson, O.; Bizjajeva, S.; Fenstad, A.M.; Furnes, O.; Lidgren, L.; Mehnert, F.; Odgaard, A.; Pedersen, A.B.; Havelin, L.I. Knee arthroplasty in Denmark, Norway and Sweden. Acta Orthop. 2010, 81, 82–89. [Google Scholar] [CrossRef]
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J. Bone Joint Surg. Am. 2018, 100, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Moisan, P.; Martel, S.; Montreuil, J.; Bernstein, M.; Tanzer, M.; Hart, A. Episode-of-care costs of total knee arthroplasty: Outpatient versus inpatient postoperative care protocol. Knee 2024, 51, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Greco, M.; Calgaro, G.; Cecconi, M. Management of hospital admission, patient information and education, and immediate preoperative care. Saudi J. Anaesth. 2023, 17, 517. [Google Scholar] [CrossRef]
- van der Linde-van den Bor, M.; Frans-Rensen, S.A.; Slond, F.; Liesdek, O.C.D.; de Heer, L.M.; Suyker, W.J.L.; Jaarsma, T.; Weldam, S.W. Patients’ voices in the development of pre-surgical patient education using virtual reality: A qualitative study. PEC Innov. 2022, 1, 100015. [Google Scholar] [CrossRef] [PubMed]
- Mahdi, A.; Nyman, M.H.; Wretenberg, P. How do orthopaedic surgeons inform their patients before knee arthroplasty surgery? A cross-sectional study. BMC Musculoskelet Disord. 2018, 19, 414. [Google Scholar] [CrossRef]
- Speros, C. More than Words: Promoting Health Literacy in Older Adults. OJIN Online J. Issues Nurs. 2009, 14, 5. Available online: https://ojin.nursingworld.org/table-of-contents/volume-14-2009/number-3-september-2009/health-literacy-in-older-adults/ (accessed on 12 May 2025). [CrossRef]
- Shen, H.; Masingboon, K.; Samartkit, N. Factors related to preoperative uncertainty among patients with breast cancer in Wenzhou, China: A cross-sectional study. Belitung Nurs. J. 2023, 9, 236–243. [Google Scholar] [CrossRef]
- Amprachim, S.E.; Vlamis, J.; Nikolaou, V.S.; Pneumaticos, S.G. Role of Preoperative Information and Education of Patients Undergoing Total Hip Arthroplasty: A Narrative Review of the Literature. Cureus 2024, 16, e66094. [Google Scholar] [CrossRef]
- Ali, Z.; Ahsan, Z.; Liaqat, N.; Din, I.U. Bridging the gap: Evaluation of preoperative patients’ education by comparing expectations and real-perioperative surgical experiences: A mixed-methods descriptive cross-sectional study. BMC Health Serv. Res. 2024, 24, 964. [Google Scholar] [CrossRef] [PubMed]
- Darville-Beneby, R.; Lomanowska, A.M.; Yu, H.C.; Jobin, P.; Rosenbloom, B.N.; Gabriel, G.; Daudt, H.; Negraeff, M.; Di Renna, T.; Hudspith, M.; et al. The Impact of Preoperative Patient Education on Postoperative Pain, Opioid Use, and Psychological Outcomes: A Narrative Review. Can. J. Pain. 2023, 7, 2266751. [Google Scholar] [CrossRef] [PubMed]
- Waljee, J.; McGlinn, E.P.; Sears, E.D.; Chung, K.C. Patient expectations and patient-reported outcomes in surgery: A systematic review. Surgery. 2014, 155, 799–808. [Google Scholar] [CrossRef]
- Hanalis-Miller, T.; Nudelman, G.; Ben-Eliyahu, S.; Jacoby, R. The Effect of Pre-operative Psychological Interventions on Psychological, Physiological, and Immunological Indices in Oncology Patients: A Scoping Review. Front. Psychol. 2022, 13, 839065. Available online: https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2022.839065/full (accessed on 28 April 2025). [CrossRef]
- Henn, R.F.; Kang, L.; Tashjian, R.Z.; Green, A. Patients’ preoperative expectations predict the outcome of rotator cuff repair. J. Bone Joint Surg. Am. 2007, 89, 1913–1919. [Google Scholar] [CrossRef]
- Singh, N.; Kanaujia, S.K.; Singh, M.K.; Shukla, N.; Siddiqui, A.K.; Kohli, M. Effect of Virtual Reality Glasses and Melody on Cortisol and Adrenocorticotropic Hormone Levels in Patients with Knee Replacement Surgery Under Combined Spinal Epidural Anaesthesia. Cureus 2024, 16, e63017. [Google Scholar] [CrossRef]
- Hermans, A.N.L.; Betz, K.; Verhaert, D.V.M.; Uijl, D.W.D.; Clerx, K.; Debie, L.; Lahaije, M.; Vernooy, K.; Linz, D.; Weijs, B. 360° Virtual reality to improve patient education and reduce anxiety towards atrial fibrillation ablation. EP Eur. 2023, 25, 855–862. [Google Scholar] [CrossRef]
- Bekelis, K.; Calnan, D.; Simmons, N.; MacKenzie, T.A.; Kakoulides, G. Effect of an Immersive Preoperative Virtual Reality Experience on Patient Reported Outcomes: A Randomized Controlled Trial. Ann. Surg. 2017, 265, 1068–1073. [Google Scholar] [CrossRef]
- Shepherd, T.; Trinder, M.; Theophilus, M. Does virtual reality in the perioperative setting for patient education improve understanding? A scoping review. Surg. Pract. Sci. 2022, 10, 100101. [Google Scholar] [CrossRef]
- Kim, J.; Kim, D.; Oh, S.H.; Kwon, H. Virtual reality for preoperative patient education: Impact on satisfaction, usability, and burnout from the perspective of new nurses. World J. Clin. Cases. 2024, 12, 6204–6216. [Google Scholar] [CrossRef]
- Gendia, A.; Rehman, M.; Cota, A.; Gilbert, J.; Clark, J. Can virtual reality technology be considered as a part of the surgical care pathway? Ann. R. Coll. Surg. Engl. 2023, 105, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Heidegger, T.; Nuebling, M.; Germann, R.; Borg, H.; Flückiger, K.; Coi, T.; Husemann, Y. Patient satisfaction with anesthesia care: Information alone does not lead to improvement. Can. J. Anesth. 2004, 51, 801–805. [Google Scholar] [CrossRef] [PubMed]
- Saredakis, D.; Szpak, A.; Birckhead, B.; Keage, H.A.D.; Rizzo, A.; Loetscher, T. Factors Associated with Virtual Reality Sickness in Head-Mounted Displays: A Systematic Review and Meta-Analysis. Front. Hum. Neurosci. 2020, 14, 96. [Google Scholar] [CrossRef] [PubMed]
- van Rijn, M.M.; de Heer, L.M.; Nieuwenhuis-Wendt, J.; van der Kaaij, N.P.; Moolenaar, E.G.; van der Ham, D.H.; van der Plank, L.; Westland, H.; Weldam, S.W. Use of virtual reality in preoperative education of cardiac surgery patients—A feasibility study. Patient Educ. Couns. 2024, 129, 108394. [Google Scholar] [CrossRef]
- Güneş, H.; Sarıtaş, S. The Effects of Virtual Reality Intervention Before Total Knee Arthroplasty on Pain, Anxiety, and Vital Signs. Clin. Simul. Nurs. 2024, 87, 101410. Available online: https://www.nursingsimulation.org/article/S1876-1399(23)00024-5/abstract (accessed on 12 May 2025). [CrossRef]
- Quinn, R.P.; Gutek, B.A.; Walsh, J.T. Telephone Interviewing: A Reappraisal and a Field Experiment. Basic. Appl. Soc. Psychol. 1980, 1, 127–153. [Google Scholar] [CrossRef]
- Malterud, K. Qualitative research: Standards, challenges, and guidelines. Lancet 2001, 358, 483–488. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Khora [Internet]. Available online: https://Khora.com (accessed on 12 May 2025).
- Aliwi, I.; Schot, V.; Carrabba, M.; Duong, P.; Shievano, S.; Caputo, M.; Wray, J.; de Vecchi, A.; Biglino, G. The Role of Immersive Virtual Reality and Augmented Reality in Medical Communication: A Scoping Review. J. Patient Exp. 2023, 10, 23743735231171562. [Google Scholar] [CrossRef]
- Hennink, M.; Kaiser, B.N. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc. Sci. Med. 2022, 292, 114523. [Google Scholar] [CrossRef]
- Graneheim, U.H.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today. 2004, 24, 105–112. [Google Scholar] [CrossRef] [PubMed]
- van der Kruk, S.R.; Zielinski, R.; MacDougall, H.; Hughes-Barton, D.; Gunn, K.M. Virtual reality as a patient education tool in healthcare: A scoping review. Patient Educ. Couns. 2022, 105, 1928–1942. [Google Scholar] [CrossRef] [PubMed]
- Schubbe, D.; Scalia, P.; Yen, R.W.; Saunders, C.H.; Cohen, S.; Elwyn, G.; van den Muijsenbergh, M.; Durand, M.A. Using pictures to convey health information: A systematic review and meta-analysis of the effects on patient and consumer health behaviors and outcomes. Patient Educ. Couns. 2020, 103, 1935–1960. [Google Scholar] [CrossRef] [PubMed]
- Jawed, S.; Amin, H.U.; Malik, A.S.; Faye, I. Classification of Visual and Non-visual Learners Using Electroencephalographic Alpha and Gamma Activities. Front. Behav. Neurosci. 2019, 13, 86. [Google Scholar] [CrossRef]
- Shiner, C.T.; Croker, G.; McGhee, J.; Faux, S.G. Perspectives on the use of Virtual Reality within a public hospital setting: Surveying knowledge, attitudes, and perceived utility among health care professionals. BMC Digit. Health. 2024, 2, 18. [Google Scholar] [CrossRef]
- Vogel, A.; Guinemer, C.; Fürstenau, D. Patients’ and healthcare professionals’ perceived facilitators and barriers for shared decision-making for frail and elderly patients in perioperative care: A scoping review. BMC Health Serv. Res. 2023, 23, 197. [Google Scholar] [CrossRef]
- Vogl, S. Telephone Versus Face-to-Face Interviews: Mode Effect on Semistructured Interviews with Children. Sociol. Methodol. 2013, 43, 133–177. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).