Abstract
Background: The increasing demand for care in hospital settings, often at a high intensity, requires organizing work according to 24 h shifts. Nevertheless, shift work (SW), especially at night, alters the circadian rhythm, negatively affecting the psychophysical health of nurses, compromising their quality of life, and jeopardizing patient safety. Shift-work-related diseases (SWDs) can arise from these disruptions. Methods: This systematic review aims to evaluate the effects of several types of medical, psychotherapeutic, and educational interventions and strategies on shift-work-related diseases (SWDs). The databases PubMed, Embase, Web of Science, and Cochrane were searched using the MESH terms “shift work” and “nurses” from January 2015 to March 2025. A total of 43 articles were included in the final analysis. Results: Quantitative findings from the studies showed, for example, improvements in sleep quality scores ranging from 15% to 40% with optimized shift planning, reductions in fatigue scores by 20–35% through strategic napping, and moderate effect sizes for light therapy interventions. Physical activity and relaxation techniques were associated with a 10–25% improvement in subjective well-being indices, while meal timing interventions led to reductions in gastrointestinal symptom prevalence by up to 18%. The selected articles were discussed by dividing them according to the type of intervention applied to shift nurses, namely improvement of shift planning, light and temperature modulation, introduction of napping, supplementation, meal management, psychotherapy, sleep education, physical activity, relaxation techniques and yoga, music therapy, and aromatherapy. This categorization was performed to highlight the range of strategies tested and their relative quantitative impact. Conclusions: There is evidence that SWDs can be mitigated through targeted interventions and strategies. The limitations of the studies examined include small sample sizes, extreme heterogeneity of follow-up, the few numbers of randomized controlled trials, and the prevalence of female or Intensive Care Unit nurses in study samples. Further research should focus on large-scale randomized controlled trials, multicenter longitudinal studies, and the evaluation of the most promising interventions—particularly light therapy, optimized shift scheduling, and structured napping protocols—to assess their long-term efficacy and generalizability.
1. Introduction
Shift work (SW) refers to any work schedule that falls outside the traditional daytime hours of 7 a.m. to 6 p.m. It includes evening, night, and rotating shifts, which are common in industries requiring 24 h operations, such as healthcare, law enforcement, transportation, and emergency services [1]. In nursing, SW is essential to ensure continuous patient care, but it often leads to disruptions in circadian rhythms, sleep deprivation, and fatigue [2]. These factors can negatively impact nurses’ health, increasing the risk of stress, metabolic disorders, cardiovascular diseases (CVDs), and reduced cognitive performance [3]. Additionally, SW affects social and family life, contributing to burnout and job dissatisfaction. To mitigate shift-work-related diseases (SWDs), proper scheduling strategies, sufficient rest periods, and ergonomic work arrangements are crucial in improving nurses’ well-being and maintaining high-quality patient care [4].
SW has significant effects on sleep, mainly due to disruptions in the natural circadian rhythm, leading to various health issues, including sleep disorders like insomnia and excessive daytime sleepiness [5]. Nursing staff working in a two-shift system often experience these disturbances due to the demands of night shifts, which suppress melatonin production, a hormone crucial for regulating sleep. The most notable SWDs are often related to sleep quality, with individuals reporting difficulty both falling asleep and maintaining sleep, particularly when transitioning between day and night shifts. This leads to sleep deprivation, which is linked to an increased risk of CVDs, metabolic issues, and even certain types of cancers, such as breast cancer in women, as SW has been recognized as a potential carcinogen by the International Agency for Research on Cancer. Moreover, the sleep disturbances caused by SW can have a detrimental impact on job performance, increasing fatigue and lowering cognitive function, which could affect the quality of healthcare services provided [6,7,8,9,10].
The effects of SW on the cardiovascular system have been widely studied because long-term exposure to night SW increases the risk of hypertension and coronary heart disease (CHD) [11]. Specifically, working more than five night shifts per month and slowly rotating shifts (that is, always attending the same shift for a certain period of time rather than changing shifts quickly in a week) significantly increased the likelihood of hypertension [12]. A prospective cohort study of female nurses showed that the duration of rotating night SW was positively correlated with an elevated risk of CHD. This association was more pronounced in the early years of exposure and persisted even after adjusting for other risk factors [13,14,15,16]. In addition, the adverse effects of SW on the cardiovascular system accumulate over time, with a significant increase in CHD risk observed in those who worked rotating night shifts for extended periods [17,18,19,20,21].
It has been found that sleep disturbances, poor sleep quality, and sleep deprivation negatively affect metabolic health, increasing the risks for obesity, type 2 diabetes, hypertension, and metabolic syndrome (MetS) [22,23,24,25,26].
Moreover, nurses working shift schedules tend to develop irregular eating habits, poor dietary choices, and lower physical activity levels, which further exacerbate metabolic issues such as weight gain and higher body fat percentages. The relationship between SW and metabolic dysfunction is complex and multifactorial, involving both direct physiological effects, such as hormonal imbalances (e.g., altered cortisol and insulin levels), and indirect lifestyle factors, such as disrupted eating patterns and physical inactivity. Irregular sleep patterns and inconsistent meal timings are significant contributors to these metabolic issues [27,28,29]. Nurses who consume a higher proportion of their daily caloric intake after 7 p.m., often due to irregular work hours, tend to have a higher prevalence of MetS [26,30,31,32,33].
Night SW has been associated with an increased risk of various cancers, including breast and colorectal cancer [34]. Long-term exposure to circadian disruption can affect processes such as cell proliferation and DNA repair, as well as the suppression of melatonin, a hormone with potential anticancer properties [35,36,37,38,39]. While evidence for a link between night SW and breast cancer is relatively stronger, studies on other cancers like colorectal and thyroid cancer remain inconclusive, with some suggesting a modest increase in risk associated with sleep difficulties among night shift workers [40]. However, the overall evidence for a direct causal relationship between SW and cancer risk remains weak, and further research is needed to better understand the mechanisms involved [41,42,43,44,45].
Night SW increases the risk of several neurological diseases, altering sleep circadian rhythms and melatonin levels, which are crucial for cognitive health. Disruption of these processes has been associated with cognitive decline, including impairments in working memory and attention, with night shifts causing the most significant decline in these areas [46]. Additionally, prolonged exposure to night SW, particularly lasting 20 or more years, has been linked to an increased risk of multiple sclerosis (MS) [47,48]. While the overall evidence does not consistently support a direct link between SW and MS, long-term exposure may contribute to the onset of definite MS [49].
SW significantly affects psychosocial well-being in nursing, with nurses working irregular or rotating shifts experiencing higher levels of psychological diseases, such as anxiety, depression, and stress [50,51,52,53,54,55,56]. These conditions are worsened by long working hours and disrupted sleep patterns, contributing to burnout and fatigue. Persistent night SW is linked to increased mood and neurotic disorders [57]. Additionally, factors like low social support, lack of control over shift schedules, and inadequate staffing worsen these psychosocial risks [58]. SW also impacts nurses’ work-family balance, with rotating shifts leading to more work-family conflicts and reduced work–life quality [59]. Nurses with more control over their shift schedules report lower burnout and exhaustion [60,61,62,63,64,65]. Hence, SW poses significant psychosocial risks for nurses, affecting their mental health and job performance [66,67,68].
On the other hand, SW has significant effects on patient safety, primarily due to the impact on healthcare workers’ fatigue, sleep deprivation, and overall alertness. Particularly, SW extended 12 h or longer contributes to physical and mental exhaustion, which increases the likelihood of medical errors, including medication mistakes and procedural lapses. Studies show that fatigue leads to slower reaction times, decreased attention, and a higher risk of oversight in patient care [67,69,70,71,72]. Additionally, sleep disruption, particularly from night SW, can impair cognitive function and increase the chance of errors. The cumulative effect of long shifts and irregular working hours compromises the quality of care, as healthcare workers are less able to stay focused and make critical decisions. Herein, while SW is essential for providing 24/7 healthcare, its negative impact on worker well-being poses a significant risk to patient safety, giving rise to the need for better management of shift patterns and work hours in healthcare settings (Figure 1) [68,73,74,75,76].
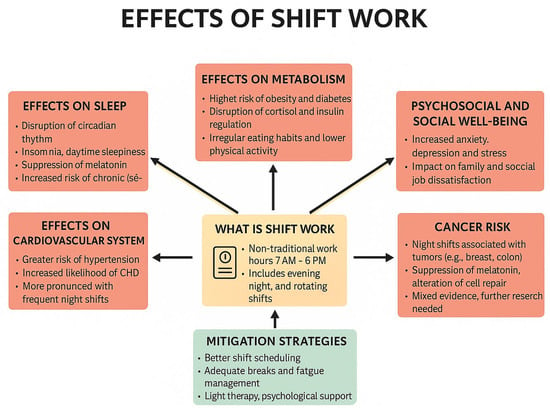
Figure 1.
A visual guide of how shift work (SW) affects health and well-being. The red boxes illustrate the adverse health and psychosocial effects associated with shift work, whereas the green box presents evidence-based mitigation strategies aimed at reducing these negative outcomes.
This systematic review aims to evaluate the effectiveness of medical, psychotherapeutic, and educational approaches to mitigate nurses’ SWDs. In addition, evidence-based guidelines were provided to help healthcare institutions implement more effective measures to support shift-working nurses, ensuring their well-being and improving patient care quality.
2. Materials and Methods
2.1. PICO Question
“Can shift-working nurses (P) benefit from various strategies and interventions (I) compared with the control group (C) in terms of improvement of health and quality of life and occupational risk reduction (O)?” (Population: nurses on SW; Intervention: medical, psychotherapeutic, and educational interventions and strategies to reduce SWDs and improve quality of life; Comparison: control group of nurses on SW who do not implement such strategies and interventions (may be absent in some articles); Outcome: improved health and quality of life for shift nurses, reduced occupational risks.)
2.2. Research Protocol
This systematic review was conducted following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) 2020 guidelines and registered in the International Prospective Register of Systematic Review Registry guidelines (PROSPERO; ID: 1014195; https://doi.org/10.1136/bmj.n71).
2.3. Search Processing
Four electronic databases, namely PubMed, Scopus, Web of Science, and Cochrane, were consulted to find articles that match our topic, dating from 1 January 2015 to 3 March 3 2025. The following Medical Subject Heading (MESH) terms were used: “shift work” AND “nurses” (Table 1).

Table 1.
Article screening strategy.
2.4. Inclusion and Exclusion Criteria
Articles were selected if they met the following inclusion criteria: (1) human subjects; (2) English language; (3) randomized controlled trials, clinical trials, cohort studies, and observational studies; (4) nurses performing SW; (5) research time limits; and (6) open access.
The exclusion criteria applied were the following: (1) other languages except English; (2) reviews, meta-analyses, and case reports; (3) population not relevant; and (4) outcomes not relevant.
2.5. Data Processing
Three reviewers (L.C., L.F., and I.T.) independently screened the records according to the inclusion criteria. The variables extracted were the characteristics of the study population (both male and female shift nurses of all ages), the interventions to mitigate nurses’ SWDs (type, dosage, duration, frequency), the control group (shift work nurses who do not receive such interventions), methodological aspects (study design, sample size, analysis method, risk of bias), and outcomes (type of SWD improved, measurement of effects on study population, duration of follow-up). The reviewers crosschecked each other’s selected articles. The discrepancies were resolved through root cause analysis, data cleaning and transformation, re-extraction of data in some cases, documentation of the discrepancies to ensure transparency and future reference, and an expert consultation (F.I.).
The selected articles were downloaded into Zotero (version 6.0.15).
2.6. Quality Assessment
The quality of the included papers was assessed by two reviewers, M.C.F. and G.D., using the ROBINS-I, which is a tool developed to assess the risk of bias in the results of non-randomized studies that compare the health effects of two or more interventions. Seven domains were evaluated, and each was assigned a degree of bias, namely (1) bias due to confounding, (2) bias in selection of participants into the study, (3) bias in classification of the intervention, (4) bias due to deviations from intended interventions, (5) bias due to missing data, (6) bias in measurement of the outcome, and (7) bias in selection of the reported result. A third reviewer (F.I.) was questioned in case of any doubt.
3. Results
3.1. Characteristics of the Included Articles
A total of 460 records were identified using the keywords “shift work” and “nurses.” When applicable, the automatic filters entered were as follows: human subjects, only English articles, only clinical studies, and no reviews. The databases consulted were PubMed (139), Scopus (99), Web of Science (185), and Cochrane (37). All records were uploaded to an Excel file.
During the screening phase, inclusion and exclusion criteria were applied based on title and abstract analysis. Only studies focusing on strategies and interventions that can be implemented to reduce the effects of SW on nurses were selected. Studies concerning the effects of SW on nurses but focusing on other areas, such as negative effects on nurses’ mental and physical health, increased risks to the patient, and advantages and disadvantages of SW on nurses’ organization of daily life, were considered off-topic. After screening, 347 articles were excluded by analyzing the title and abstract, leading to 113 records. Then, duplicates (36) were removed manually, resulting in the selection of 77 records. Among the included studies, both interventional and observational designs (longitudinal and cross-sectional) were considered eligible if they evaluated strategies or interventions targeting the effects of shift work.
At the end of the eligibility process, 43 studies were included in the final analysis. The process is illustrated in the flowchart of Figure 2, and in Table 2 there is a summary of Interventions and Main Outcomes.
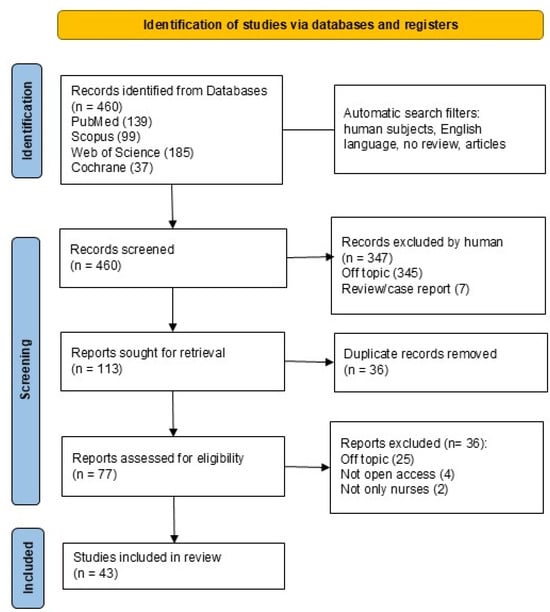
Figure 2.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) 2020 flowchart (https://doi.org/10.1136/bmj.n71).

Table 2.
Summary table of interventions and main outcomes.
3.2. Quality Assessment and Risk of Bias of Included Articles
The risk of bias assessment, in Table 3, conducted with the ROBINS-I tool on the 43 included studies showed that most presented a moderate risk in at least two domains, particularly bias due to confounding and bias in measurement of outcomes, where over 60% of studies raised concerns. This finding reflects the frequent lack of adequate control for potential confounding variables and the predominant use of subjective assessment tools (questionnaires and self-reports) rather than objective measures. Bias in the classification of interventions and bias due to deviations from intended interventions were the domains with the highest proportion of high risk, especially in studies without clearly defined intervention protocols. Missing data was a relevant issue in about one-third of the studies, with potential implications for internal validity and generalizability. Only the studies by Pahlevanzadeh M.J. et al. and de Bruijn L. et al. showed a low risk of bias across all domains, indicating strong methodological rigor. At the opposite extreme, seven studies reported high risk in multiple domains, often associated with deviations from intended interventions and inaccurate intervention classification. Overall, these results suggest that the conclusions of this review should be interpreted with caution: although positive evidence was identified for several strategies, the overall strength of the evidence is limited by the heterogeneous methodological quality of the available studies.

Table 3.
Overall risk of bias assessment in studies: analysis based on ROBINS-I.
The following tables show the characteristics of the selected studies and their relevant findings, divided by SWD improvement intervention, namely (1) the effects of work schedules, flexibility, and recovery time; (2) the effects of individual tolerance factors and chronotype; (3) the effects of satisfaction questionnaires; (4) the effects of light and temperature modulation; (5) the effects of supplementation; (6) the effects of meal management; (7) the effects of physical activity, relaxation techniques, and yoga; (8) the effects of physiotherapy; (9) the effects of sleep education; and (10) the effects of music therapy and aromatherapy.(Table 4, Table 5, Table 6, Table 7, Table 8, Table 9, Table 10, Table 11, Table 12 and Table 13).

Table 4.
Studies concerning the effects of work schedules, flexibility, and recovery time on nurses’ shift-work-related diseases (SWDs).

Table 5.
Studies concerning the effects of individual tolerance factors and chronotype on nurses’ shift-work-related diseases (SWDs).

Table 6.
Studies concerning the effects of satisfaction questionnaires on nurses’ shift-work-related diseases (SWDs).

Table 7.
Studies concerning the effects of light and temperature modulation on nurses’ shift-work-related diseases (SWDs).

Table 8.
Studies concerning the effects of supplementation on nurses’ shift-work-related diseases (SWDs).

Table 9.
Studies concerning the effects of meal management on nurses’ shift-work-related diseases (SWDs).

Table 10.
Studies concerning the effects of physical activity, relaxation techniques, and yoga on nurses’ shift-work-related diseases (SWDs).

Table 11.
Studies concerning the effects of physiotherapy on nurses’ shift-work-related diseases (SWDs).

Table 12.
Studies concerning the effects of sleep education on nurses’ shift-work-related diseases (SWDs).

Table 13.
Studies concerning the effects of music therapy and aromatherapy on nurses’ shift-work-related diseases (SWDs).
4. Discussion
4.1. Shift Planning
4.1.1. Work Schedules, Flexibility, and Recovery Time
Several studies have investigated the planning of shift schedules and how different models of nurse rostering impact nurse performance, engagement, and fatigue. Many authors agree that excessively long shifts should be avoided, and an adequate number of days off should be allowed after a night shift. Dall’Ora et al. reported in their cross-sectional study that 12 h shifts reduced opportunities for continuing education, patient discussions, and continuity of care, highlighting a trade-off between staffing efficiency and quality of care [79]. Niu et al., in the prospective longitudinal, parallel-group comparative study, reinforced the biological difficulty of adjusting to night shifts, demonstrating that cortisol rhythms require at least two days off to normalize [77]. These findings support the importance of allowing sufficient recovery time and structuring shifts around the natural human circadian rhythm [77]. Complementing these findings, Kubo et al., in a non-randomized controlled cross-over study, tested a targeted intervention by extending restart breaks after consecutive night shifts [82]. Allowing extended restart breaks from 31 to 55 h after consecutive night shifts led to reduced subjective fatigue and psychological distress, although no significant improvements were observed in objective physiological markers, namely vital exhaustion, distress, hair cortisol, salivary C-reactive protein, and sleep mattress sensor sensation [82]. Likewise, Waage et al. demonstrated in a longitudinal cohort study that reducing night shifts in the last year or eliminating quick returns significantly improved outcomes for nurses suffering from SWDs, thereby reinforcing the importance of tailoring schedules to individual biological predispositions [81]. In comparison, Shiffer et al. pointed out in a cross-sectional study the significance of rotation direction: clockwise schedules were associated with better sleep quality and work–life balance compared to counterclockwise rotations [78]. Conversely, Inoue et al. presented in a survey-based observational study a more optimistic perspective: under variable shift systems—particularly those structured with restorative breaks and opportunities for social interaction—nurses reported sustained work engagement [78]. According to the authors, the variable shift system proves effective, and nurses should be allowed to opt for a break based on conversation or rest [80].
4.1.2. Individual Factors and Chronotype in Shift Tolerance
Nursing managers should consider individual nurse characteristics and their preferences to be able to arrange tailor-made shifts. For this purpose, they can use the help of mathematical models, digital media, and surveys. Self-scheduling of shifts should also be encouraged. A key characteristic to consider is the chronotype. Chronotype, genetically defined and modulated by the environment, correlates with individual preferences for sleep–wake rhythms and depends on the secretion of cortisol and melatonin from the hypothalamic-pituitary axis. There are three main categories of chronotype: morning types, evening types, and neither type, the latter being the most adaptable to various shifts.
In two descriptive cohort studies, Bülbül et al. and de Bruijn et al. both found that evening-type nurses, despite being more likely to work night shifts, experienced poorer sleep quality and lower overall well-being. In contrast, intermediate chronotypes performed better, as their natural rhythms aligned more closely with typical shift patterns [85,87]. Therefore, chronotype is associated with shift type preference and sleep disorders in nurses [85,87]. These findings are consistent with the results of the cross-sectional study by Jung et al., who emphasized that SW tolerance is influenced by a combination of individual tolerance factors, namely age and number of children, chronotype, job stress, social support, and lifestyle habits, indicating that adaptation is multifactorial rather than only schedule dependent [85,87]. Individual SW tolerance factors can influence insomnia, depression, and fatigue. Similarly, in a multicenter cross-sectional study, Li et al. found that work-related quality of life and chronotype were stronger predictors of sleep quality than the specific shift pattern itself among maternal and child health nurses [86]. Nursing managers should take into account nurses’ chronotype and quality of work life and make interventions that affect both sleep-related modifiable factors (such as frequent caffeine intake and irregular meals) and non-modifiable factors (e.g., age and chronotype) [86].
Pahlevanzadeh et al. proposed a justice-based scheduling model that incorporated nurse preferences and performance metrics, based on a mathematical model of integer binary programming [84]. After the application of this mathematical model, the tax of absenteeism and the number of performance complaints decreased by 40% and 50%, respectively. In parallel, nurses’ satisfaction increased by 30%. This suggests that, in some cases, personal and psychosocial factors may have a greater impact than structural scheduling characteristics [84].
In conclusion, these studies underscore the potential benefits of chronotype-aware scheduling and tailor-made interventions as strategies for improving nurses’ health, sleep quality, and overall work performance.
4.1.3. Satisfaction Questionnaires
The role of the organizational environment has emerged as a critical factor influencing SWDs. According to the cross-sectional study by Dehring et al., organizational climate significantly impacts nurse health; notably, rotating shift workers reported the highest levels of psychological distress [88]. However, supportive factors such as supervisor engagement and task orientation were found to buffer these negative effects [88]. Similarly, Abed Al Ahad et al., in a longitudinal study, investigated shift-specific job satisfaction and found that satisfaction levels were highest when nurses experienced manageable workloads and minimal rationing of care [89]. Together, these studies highlight the importance of organizational support, continuous workload monitoring, and evidence-informed scheduling practices in promoting a healthier and more sustainable SW environment [89]. Consistent with these concerns, Lee et al. reported in a descriptive study on compliance with ergonomic scheduling guidelines in South Korea, primarily due to institutional barriers and a lack of formal training for staff involved in roster creation [90]. In addition, in a qualitative single case study, Booker et al. also revealed widespread under-preparation among scheduling personnel, where fatigue-related risks were frequently neglected in favor of lifestyle-oriented self-rostering [91]. While self-rostering may offer greater flexibility, it can inadvertently lead to increased fatigue if not accompanied by proper guidance and fatigue risk management strategies grounded in scientific evidence [91]. The methodological study for instrument development by Shin et al. focuses on developing and validating a tool to assess the quality of a healthy work environment for shift nurses in South Korea [92]. Based on frameworks from the World Health Organization and the American Association of Critical-Care Nurses, the authors created a 23-item instrument covering five key areas: physical gratification, psychological stability, independent competency, collaborative relationships, and structural support [92]. The tool was found to be reliable and valid, showing good internal consistency and test–retest reliability. Its goal is to help improve nurse well-being, reduce burnout, and ultimately enhance patient care by identifying and improving aspects of the work environment [92].
4.2. Light and Temperature Modulation
It has been shown that intense light, even of short duration, confers acute positive effects on nurses working night shifts, including increased subjective alertness and a reduction in insomnia, anxiety, and depression [117]. Griepentrog et al. conducted a randomized crossover trial exposing Intensive Care Unit (ICU) nurses to 1500–2000 lux white light during 10 h of the night shift [93]. They found a significant reduction in subjective sleepiness but a paradoxical increase in psychomotor errors, suggesting that while alertness improved, cognitive precision may have declined under intense lighting [93]. In contrast, Bjorvatn et al. examined the effects of timed bright light exposure (10,000 lux) during three consecutive night shifts. Their placebo-controlled crossover study found that bright light reduced “heavy eyelids” (a subjective marker of sleepiness) but did not improve performance on the Karolinska Sleepiness Scale (KSS) or the Psychomotor Vigilance Task [94]. Moreover, no significant changes were observed in post-shift recovery, highlighting the limited long-term benefit of bright light when poorly timed or inconsistently applied. The study by Bjorvatn et al. (2021) emphasizes that bright light exposure (10,000 lux) can help delay the circadian rhythm, especially when administered progressively later across consecutive night shifts—from 2:00 to 3:00 on the first night, 3:00–4:00 on the second, and 4:00–5:00 on the third [94]. While both studies report short-term alertness benefits, they differ in terms of how well those benefits translate into functional outcomes such as vigilance and error rates.
Opposing the bright light paradigm, Hoshi et al. explored whether minimum night lighting (110 lux) could better support circadian alignment [95]. Their quasi-experimental study found that fatigue and sleepiness were significantly higher under dim lighting compared to brighter conditions (410 lux), with no improvement in post-shift sleep quality [95]. Importantly, no significant changes were found in patient safety incidents, suggesting that dimmer lighting may reduce visual alertness without offering meaningful physiological recovery. The study by Hoshi et al. found that working under dim light conditions (<120 lux) during the night shift did not improve fatigue, sleepiness, or sleep quality compared to brighter conditions (~410 lux). Importantly, light levels above 120 lux—even for short durations—were shown to suppress melatonin and disrupt circadian rhythms. [95]. This contrasts with the intended physiological rationale: that reduced lux levels might help maintain melatonin rhythms and improve adaptation. However, the lack of measurable benefits in fatigue or sleep, combined with the practical challenges of navigating darker environments, suggests that minimum lighting strategies may be less viable for safety-critical environments like hospitals.
Besides light, the other environmental factor that can be easily changed in work environments is temperature. It was discovered that preset hospital temperatures vary between 20 °C and 25 °C and temperatures above 25 °C can cause discomfort, impairing work performance in hospital settings. Furthermore, it has been found that the body temperature is lower at night due to circadian rhythms [92]. Kim et al. explored the effects of ambient temperature (23 °C vs. 26 °C) on night-shift nurses [96]. Their crossover study found that thermal comfort improved significantly at 23 °C, as did body temperature regulation, though there were no significant differences in fatigue, sleepiness, or adaptation scores between temperature conditions. Interestingly, urinary melatonin levels dropped more sharply at 23 °C, indicating a possible trade-off between physical comfort and hormonal circadian rhythms [96].
4.3. Supplementation
The supplements evaluated for mitigating sleep disturbances in shift-working nurses are melatonin and zinc [97,98]. In an RCT, Sadeghniiat-Haghighi et al. evaluated the effects of 3 mg of melatonin in shift workers with delayed sleep onset. Melatonin supplementation was administered 30 min before the workers’ usual sleep time following their night shift. The intervention significantly reduced sleep onset latency and improved sleep efficiency, though it had no measurable effect on total sleep time or wakefulness after sleep onset [97]. These results support melatonin’s short-term utility in addressing circadian misalignment, particularly in individuals with symptom-specific sleep initiation issues. However, the study’s generalizability is limited by the absence of long-term follow-up and its reliance on actigraphy rather than more robust objective sleep measures like polysomnography [97].
Gholipour Baradari et al. examined the role of zinc supplementation (220 mg every 72 h for one month) in a sample of ICU nurses with both poor sleep quality and low serum zinc levels. The study reported significant improvements in subjective sleep quality and sleep latency, alongside a notable increase in serum zinc concentration [98]. These findings suggest a biological link between micronutrient status and sleep regulation, consistent with prior research on zinc’s antioxidant and neuromodulatory roles. Unlike the melatonin study, which targeted circadian regulation, this intervention addressed nutritional deficiency as a potential root cause of sleep disturbance. Zinc supplementation was administered shortly before the sleep episode, typically between 9:00 p.m. and 11:00 p.m. [98].
Critically, while these interventions yielded positive short-term results, they differ in mechanism and application: melatonin primarily affects circadian rhythm realignment, while zinc appears to influence sleep quality through physiological restoration and nutritional correction.
4.4. Meal Management
Nutrition during night shifts is a crucial factor for the well-being and performance of healthcare workers, as it directly affects circadian rhythm regulation, blood glucose levels, and overall physical and psychological health.
The recent RCT by Suyoto et al. examined the impact of glycemic index (GI) and meal frequency on glycemic control in a sample of night-shift nurses. The findings highlighted that the quality of carbohydrates consumed plays a more critical role than meal frequency. Specifically, consuming either one or three high-GI meals during the night led to a significant increase in blood glucose levels and glycemic variability, whereas low-GI meals—even when eaten more than once and without fasting—did not negatively affect the glycemic profile. These results suggest that, during night shifts, favoring low-GI foods can help prevent metabolic disturbances, avoiding both prolonged fasting and the glycemic spikes associated with simple sugars [99].
In parallel, the RCT by Leedo et al. assessed the impact of providing healthy meals at the workplace on mood, reaction time, and dietary intake among both daytime and shift healthcare workers. Although no significant changes were found in reaction time, shift workers reported notable improvements in mood during the intervention period, including reduced fatigue, increased vitality, and an overall improvement in emotional well-being. Additionally, the intervention led to healthier eating habits, with increased intake of fiber, complex carbohydrates, and water, and a reduction in fat consumption [100]. A study by Molzof et al. found that higher food intake during night shifts was associated with increased lipid levels, regardless of macronutrient composition, highlighting the role of meal timing in cardiometabolic risk among shift-working nurses [116].
Selecting low-GI foods can help stabilize blood glucose levels and prevent fluctuations that impair alertness and performance. In addition, the availability of balanced and hydrating meals in the workplace can positively influence mood, an especially relevant factor in emotionally demanding clinical environments.
4.5. Physical Activity, Relaxation Techniques, and Yoga
Structured physical activity has shown promising results in reducing stress, preventing musculoskeletal disorders, and enhancing overall quality of life. Several studies have investigated different modalities of exercise—supervised, home-based, or mind–body oriented—adapting them to the specific demands of SW.
The RCT by Matsugaki et al. highlighted the benefits of a workplace exercise program supervised by physical therapists for shift-working nurses. After 12 weeks of aerobic and resistance training, the supervised group demonstrated significant improvements in aerobic capacity, muscular strength, and several biochemical markers (such as high-density lipoprotein cholesterol and adiponectin), along with a notable reduction in depressive symptoms. Although the adherence rate was similar between the supervised and voluntary (self-guided) groups, the superior outcomes in the supervised group suggest that the presence of a physiotherapist provided essential motivational and technical support, enhancing the effectiveness of the intervention [101].
The recent experimental study by Baek et al. evaluated a smartphone-based home workout program developed to promote physical activity during the Coronavirus Disease 2019 (COVID-19) pandemic. Participants reported significant improvements in sleep quality, fatigue, musculoskeletal symptoms, and psychological resilience, further confirming the value of digital health programs that combine accessibility with motivational support. While no significant changes were observed in work performance, the intervention demonstrated the potential of mobile-based solutions as sustainable and customizable tools to enhance nurse well-being, particularly during times of health system strain [102].
A more relaxation-focused approach was explored by the randomized crossover trial by Miyoshi, who investigated the effects of restorative yoga on SW nurses. After four weeks of regular home practice, participants reported a significant reduction in perceived stress compared to their usual stress management methods (such as sleeping, shopping, or socializing). Although no significant changes were observed in vital signs, the subjective improvement in well-being suggests that restorative yoga may positively impact psychological health, offering an accessible and autonomous strategy for coping with occupational stress [103].
Targeted physical activity interventions—despite their differences in delivery and structure (at home or during SW)—can significantly benefit the health of SW nurses. Professional supervision, mobile health technologies, and flexible mind–body practices emerge as key factors in facilitating their adoption, adherence, and sustainability.
4.6. Psychotherapy
In the last two years, several authors have explored innovative psychotherapy approaches—often combining digital technologies and cognitive strategies—to reduce burnout, improve sleep quality, and strengthen emotional regulation.
The RCT by Baek et al. tested the effectiveness of a personalized artificial intelligence (AI)-assisted intervention for reducing burnout among nurses. The algorithm tailored the intervention content—which included mindfulness, Acceptance and Commitment Therapy, reflective writing, and laughter therapy—based on each participant’s individual psychological profile. Results showed a significant reduction in burnout, especially in dimensions related to patient interaction, highlighting the potential of intelligent technologies as flexible and scalable tools to support the psychological health of healthcare workers [104].
Similarly, the RCT by Ell et al. investigated the efficacy of digital cognitive behavioral therapy for insomnia. The intervention led to significant improvements in sleep quality and sleep efficiency and a reduction in psychological distress. Participants also reported improved daytime functioning, suggesting that well-designed digital solutions can serve as practical resources for addressing sleep disorders among shift workers [105].
A more comprehensive approach was adopted by Wenhua Liu et al. through a Complex Interactive Multimodal Intervention. This program combined digital education, social platform support, personalized feedback, and nurse-led coaching. The results showed a significant reduction in perceived stress, depression, and sleepiness among healthcare workers. Although physiological parameters (such as heart rate variability) remained unchanged, the intervention still demonstrated the positive psychological impact of flexible and personalized digital tools [106]. Finally, Lu et al. explored the role of confiding as an emotional regulation strategy among shift-working nurses during the COVID-19 pandemic. The intervention, based on reflective writing about received social support, significantly improved interpersonal emotion regulation and, to a lesser extent, sleep quality. However, no significant differences were found in depression levels or intrapersonal emotional regulation, suggesting that the primary benefit stemmed from acknowledging and valuing social support rather than from individual cognitive processing [107]. These studies underscore the effectiveness of personalized, digitally assisted, and relationship-centered interventions in supporting the psychological health of nursing staff. AI, digital platforms, and reflective techniques emerge as promising tools for preventing and treating nurses’ SWDs.
4.7. Sleep Education
The literature has increasingly emphasized sleep optimization through strategic napping during night SW. Two recent observational studies by Watanabe et al. confirmed the importance of both nap duration and quality in reducing drowsiness and fatigue. The first longitudinal study showed that naps lasting at least 90 min were associated with less post-nap sleepiness and lower end-of-shift fatigue. However, only 30% of nurses achieved this duration due to environmental factors such as noise and electronic device use. The second study further emphasized the role of sleep quality, revealing that naps with ≥70% sleep efficiency and ≥120 min in bed were the most effective. Individual factors—such as sleep reactivity and pre-nap behaviors like screen use—significantly influenced outcomes [108,109]. These results were supported by the experimental study by Oriyama et al., which assessed the effects of 120 min naps taken at different times during a simulated 16 h night shift. The data indicated that naps between 00:00 and 2:00 offered the greatest benefits in terms of reduced sleepiness and improved cognitive performance in the early morning hours, compared to naps taken at other times. However, increased post-nap sleep inertia highlighted the complexity of nap timing and management in clinical settings [110].
From a behavioral perspective, the qualitative study by Albakri et al. provided valuable insights into the individual sleep strategies adopted by nurses. “Good sleepers” tended to implement structured routines before, during, and after shifts—such as modifying the sleep environment, engaging in physical activity, and avoiding stimulants. In contrast, “poor sleepers” often lacked effective strategies, suggesting the need for personalized educational programs to improve sleep hygiene among nursing staff [109].
The descriptive study by Elif et al. highlighted the significant influence of individual chronotype on the quality of life of shift-working nurses. Specifically, evening-type nurses, more frequently assigned to night shifts, reported lower scores in both the physical and mental components of the Short-Form Health Survey (SF-36) compared to their morning-type or intermediate-type colleagues. These findings underscore the importance of considering chronotype in shift scheduling to promote well-being and prevent psychological distress [114]. Aligned with this approach, the RCT by Booker et al. evaluated the effectiveness of a personalized sleep and SW coaching program versus a control group receiving only nutritional advice. Although no significant differences were observed in sick leave, the intervention group showed marked improvements in insomnia, anxiety, depression, and sleep quality—particularly among those at higher risk for SWDs. These findings highlight the potential benefits of tailored, multidimensional interventions in supporting nurses’ physical and psychological health [111]. This evidence underlines the value of integrated, multi-level interventions, including shift personalization based on chronotype, structured nap planning, sleep education, and psychological support—to mitigate the adverse consequences of SWDs.
4.8. Music Therapy and Aromatherapy
In the recent literature, an increasing number of studies have explored the effectiveness of holistic non-pharmacological interventions—such as music therapy, aromatherapy, and animal-assisted interventions—as complementary approaches in promoting the physical and psychological well-being of SW nurses.
Music therapy has proven particularly effective in supporting mental health and sleep among nurses with circadian rhythm sleep disorders. The retrospective study by Wang et al. demonstrated that integrating music therapy with pharmacological treatment using melatonin receptor-2 agonists led to a significant improvement in sleep quality and a reduction in anxiety and depression symptoms, with an overall effectiveness rate of 85.56% compared to 50.56% in the control group [112].
Similarly, the RCT by Zamanifar et al. demonstrated that music therapy—alone or in combination with aromatherapy—significantly reduced anxiety levels among clinical nurses [113]. Lee et al. compared the effects of music therapy and aromatherapy on stress, quality of life, and happiness among shift nurses. Both interventions led to significant improvements compared to the control group, with benefits observed in both subjective well-being and physiological markers. The study employed objective measures such as heart rate variability, demonstrating a positive biological impact [114]. Moreover, the RCT by Nasiri A. et al. showed that the inhalation of rosemary essential oil during night shifts significantly reduced sleepiness and improved alertness, as measured by the KSS and the Epworth Sleepiness Scale [115].
Overall, this evidence supports the use of accessible, free side effects and non-invasive interventions—such as music therapy, aromatherapy, and pet therapy—as effective tools to manage stress, improve emotional balance, enhance sleep quality, and boost alertness among SW nurses.
Figure 3 correlates the type of nurses’ SWDs with the specific strategies and interventions to prevent or treat it to provide schematic guidelines extrapolated from the reviewed articles.
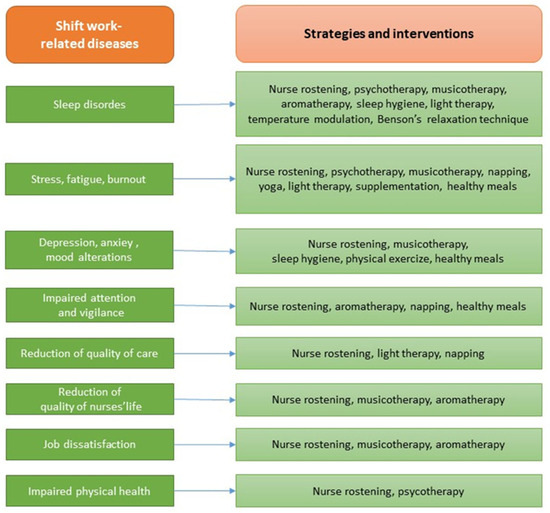
Figure 3.
Guidelines for the treatment of nurses’ shift-work-related diseases (SWDs).
This study presents several limitations. First, the RCTs reviewed numbered 14 out of 47, the remainder being essentially prospective/observational in nature. Another limitation is the non-representative population, as the sample consists mainly of female or ICU nurses, and there is variation in follow-up duration. Specifically, the most distant evaluation from the intervention was performed after 6 years, whereas the closest evaluation was performed exactly at the end of the intervention. Finally, the authors used different types of validated scales, often in the form of questionnaires or self-reported assessments, which makes it difficult to homogenize the results.
4.9. Strengths and Limitations
From a practical perspective, these findings suggest that nursing managers should prioritize the following:
- Chronotype-aware and flexible scheduling supported by mathematical or digital rostering tools;
- Structured opportunities for restorative napping;
- Integration of low-GI nutritional options during night shifts;
- Access to supervised or digitally supported physical activity programs;
- Incorporation of evidence-based psychological support programs, potentially AI-assisted;
- Availability of low-cost, low-risk complementary interventions such as music therapy or aromatherapy.
Future research should focus on large-scale randomized controlled trials and multicenter longitudinal studies to better evaluate the long-term efficacy, cost-effectiveness, and scalability of the most promising strategies—particularly chronotype-based scheduling, timed light exposure, and multimodal digital health interventions. Greater standardization of outcome measures (e.g., validated sleep quality scales, biochemical markers) would enhance comparability across studies.
A key strength of this review is the comprehensive scope, which includes both well-established and emerging interventions, offering a broad overview of current strategies against SWDs. The inclusion of multiple study designs and international samples enhances the generalizability of the observations. However, limitations include the heterogeneity of study designs, small sample sizes, inconsistent follow-up durations, and a predominance of female ICU nurses, which may limit applicability to other settings. The variability in intervention protocols also makes it difficult to determine the relative effectiveness of each strategy.
5. Conclusions
SW, especially at night, alters the circadian rhythm, negatively affecting nurses’ mental and physical health, impairing their quality of life, and jeopardizing patient safety.
The interventions or strategies identified to prevent and treat nurses’ SWDs are the following: improved SW planning (nurse rostering); modulation of light and temperature; administration of supplements (e.g., melatonin and zinc); introduction of napping; provision of healthy meals; physical activity, relaxation techniques, and yoga; sleep hygiene education programs; psychotherapy and coaching programs; and, finally, alternative approaches such as music therapy and aromatherapy.
The delivery of such strategies and interventions can be implemented through tailor-made approaches, as well as using mathematical models and digital media. For example, nursing managers could conduct surveys to identify nurses’ individual preferences, tolerance factors, and individual chronotypes and then enter these parameters into dedicated digital applications to ensure satisfactory shifts. It would also be advisable to install light and temperature sensors in departments and invest in educational and psychotherapeutic training programs. In the long run, these investments would save on healthcare costs related to patient risks and employee illnesses.
The parameters most evaluated in the various studies were sleep quality and stress/fatigue level, followed by nurse satisfaction, quality of life, alertness, general mental and physical health, and quality of care.
Further research is mandatory to assess whether the above-mentioned medical, psychotherapeutic, and educational interventions should be systematically performed by nursing managers to improve nurses’ quality of life and quality of care.
Author Contributions
Conceptualization, M.C.F.; methodology, A.D.I., and A.M.I.; software, M.C.F., L.C., and A.P.; validation, G.D., F.I., and G.M.; formal analysis, L.F., I.T., and A.P.; resources, A.D.I., and A.M.I.; data curation, L.C., and I.T.; writing—original draft preparation, L.C., L.F., and I.T.; writing—review and editing, L.F., L.C., I.T., and M.C.F.; visualization, A.D.I., A.M.I., and G.M.; supervision, F.I., and G.D.; project administration, F.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable. All figures are produced by the authors.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| AI | Artificial Intelligence |
| CHD | Coronary Heart Disease |
| CI | Confidence Interval |
| COVID-19 | Coronavirus Disease 2019 |
| CVD | Cardiovascular Disease |
| DNA | Deoxyribonucleic Acid |
| GI | Glycemic Index |
| KSS | Karolinska Sleepiness Scale |
| ICU | Intensive Care Unit |
| MetS | Metabolic Syndrome |
| MS | Multiple Sclerosis |
| RCT | Randomized Controlled Trial |
| SW | Shift Work |
| SWD | Shift-Work-Related Diseases |
References
- Rosa, D.; Terzoni, S.; Dellafiore, F.; Destrebecq, A. Systematic Review of Shift Work and Nurses’ Health. Occup. Med. 2019, 69, 237–243. [Google Scholar] [CrossRef]
- Imes, C.C.; Barthel, N.J.; Chasens, E.R.; Dunbar-Jacob, J.; Engberg, S.J.; Feeley, C.A.; Fennimore, L.A.; Godzik, C.M.; Klem, M.L.; Luyster, F.S.; et al. Shift Work Organization on Nurse Injuries: A Scoping Review. Int. J. Nurs. Stud. 2023, 138, 104395. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, J.T.; Karlsen, S.; Stayner, L.; Hansen, J.; Andersen, Z.J. Shift Work and Overall and Cause-Specific Mortality in the Danish Nurse Cohort. Scand. J. Work. Environ. Health 2017, 43, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Min, A.; Hong, H.C.; Kim, Y.M. Work Schedule Characteristics and Occupational Fatigue/Recovery among Rotating-Shift Nurses: A Cross-Sectional Study. J. Nurs. Manag. 2022, 30, 463–472. [Google Scholar] [CrossRef]
- Di Muzio, M.; Dionisi, S.; Di Simone, E.; Cianfrocca, C.; Di Muzio, F.; Fabbian, F.; Barbiero, G.; Tartaglini, D.; Giannetta, N. Can Nurses’ Shift Work Jeopardize the Patient Safety? A Systematic Review. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 4507–4519. [Google Scholar] [CrossRef]
- Cooper, P.G. A Call for a Paradigm Shift in Nursing and Healthcare Leadership. Nurs. Forum 2008, 43, 1. [Google Scholar] [CrossRef]
- Barton, J.; Spelten, E.R.; Smith, L.R.; Totterdell, P.A.; Folkard, S. A Classification of Nursing and Midwifery Shift Systems. Int. J. Nurs. Stud. 1993, 30, 65–80. [Google Scholar] [CrossRef]
- White, E. A Comparison of Nursing Education and Workforce Planning Initiatives in the United States and England. Policy Politics Nurs. Pract. 2017, 18, 173–185. [Google Scholar] [CrossRef]
- Beckman, R.J.; Hutton, S.; Czekanski, E.; Vance, K.; Mohr, D.C. A Comparison of Shift Length and Nursing and Quality Outcomes in Acute Inpatient Mental Health Units. J. Nurs. Adm. 2022, 52, 560–565. [Google Scholar] [CrossRef]
- Niu, S.-F.; Chu, H.; Chen, C.-H.; Chung, M.-H.; Chang, Y.-S.; Liao, Y.-M.; Chou, K.-R. A Comparison of the Effects of Fixed- and Rotating-Shift Schedules on Nursing Staff Attention Levels: A Randomized Trial. Biol. Res. Nurs. 2013, 15, 443–450. [Google Scholar] [CrossRef]
- Ashraf, H.; Bodapati, A.; Hanif, A.; Okafor, D.K.; Katyal, G.; Kaur, G.; Khan, S. Safety and Efficacy of Biologic Therapies (Ustekinumab and Vedolizumab) in the Treatment of Inflammatory Bowel Disease (IBD): A Systematic Review. Cureus 2023, 15, e48338. [Google Scholar] [CrossRef] [PubMed]
- Kivimäki, M.; Virtanen, M.; Elovainio, M.; Väänänen, A.; Keltikangas-Järvinen, L.; Vahtera, J. Prevalent Cardiovascular Disease, Risk Factors and Selection out of Shift Work. Scand. J. Work. Environ. Health 2006, 32, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Feng, T.; Booth, B.M.; Baldwin-Rodríguez, B.; Osorno, F.; Narayanan, S. A Multimodal Analysis of Physical Activity, Sleep, and Work Shift in Nurses with Wearable Sensor Data. Sci. Rep. 2021, 11, 8693. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.-E.; Kim, T.-Y.; Yoo, H.-S.; Chae, M.S. A Postanaesthesia Workload Instrument Can Provide Objective Information Promoting Appropriate Workload Distribution between Day and Evening Shift Nursing Staff in the Postanaesthesia Care Unit: A Prospective Observational Cohort Study. Eur. J. Anaesthesiol. 2022, 39, 722–724. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Corelli, R.; Inchingolo, A.M.; Dipalma, G. Surgical treatment of depressed scar: A simple technique. Int. J. Med. Sci. 2011, 8, 377–379. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Manias, E.; Aitken, R.; Peerson, A.; Parker, J.; Wong, K. Agency-Nursing Work: Perceptions and Experiences of Agency Nurses. Int. J. Nurs. Stud. 2003, 40, 269–279. [Google Scholar] [CrossRef]
- Lim, S.; Han, K.; Cho, H.; Baek, H. Shift-Work Nurses’ Work Environments and Health-Promoting Behaviours in Relation to Sleep Disturbance: A Cross-Sectional Secondary Data Analysis. J. Clin. Nurs. 2019, 28, 1538–1545. [Google Scholar] [CrossRef]
- Silva, R.M.d.; Zeitoune, R.C.G.; Lenz, F.C.D.; Pretto, C.R.; Santos, K.M.D.; Magnago, T.S.B.d.S.; Centenaro, A.P.F.C. Sleep Duration and Quality of Brazilian Nursing Staff Who Work in Shifts. Rev. Bras. Enferm. 2024, 77, e20230167. [Google Scholar] [CrossRef]
- Niu, S.-F.; Miao, N.-F.; Liao, Y.-M.; Chi, M.-J.; Chung, M.-H.; Chou, K.-R. Sleep Quality Associated with Different Work Schedules: A Longitudinal Study of Nursing Staff. Biol. Res. Nurs. 2017, 19, 375–381. [Google Scholar] [CrossRef]
- Buja, A.; Zampieron, A.; Mastrangelo, G.; Petean, M.; Vinelli, A.; Cerne, D.; Baldo, V. Strain and Health Implications of Nurses’ Shift Work. Int. J. Occup. Med. Environ. Health 2013, 26, 511–521. [Google Scholar] [CrossRef]
- Wakui, T. Study on Work Load of Matrons under Shift Work in a Special Nursing Home for the Elderly. Ind. Health 2000, 38, 280–288. [Google Scholar] [CrossRef]
- Congdon, J.; Craft, J.; Christensen, M. Are We Measuring Nursing Workflow Correctly? A Literature Review. Br. J. Nurs. 2020, 29, 1252–1259. [Google Scholar] [CrossRef]
- Bae, S.-H.; Fabry, D. Assessing the Relationships between Nurse Work Hours/Overtime and Nurse and Patient Outcomes: Systematic Literature Review. Nurs. Outlook 2014, 62, 138–156. [Google Scholar] [CrossRef] [PubMed]
- Buss, J. Associations between Obesity and Stress and Shift Work among Nurses. Workplace Health Saf. 2012, 60, 453–458, quiz 459. [Google Scholar] [CrossRef] [PubMed]
- Giorgi, F.; Mattei, A.; Notarnicola, I.; Petrucci, C.; Lancia, L. Can Sleep Quality and Burnout Affect the Job Performance of Shift-Work Nurses? A Hospital Cross-Sectional Study. J. Adv. Nurs. 2018, 74, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Morse, L.; Duncan, H.; Apen, L.V.; Reese, K.; Crawford, C.L. Centralized Scheduling of Nursing Staff: A Rapid Review of the Literature. Nurs. Adm. Q. 2024, 48, 347–358. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Servili, A.; Inchingolo, A.M.; Dipalma, G. A Hypothetical Correlation between Hyaluronic Acid Gel and Development of Cutaneous Metaplastic Synovial Cyst. Head Face Med. 2010, 6, 13. [Google Scholar] [CrossRef]
- Malcangi, G.; Patano, A.; Morolla, R.; De Santis, M.; Piras, F.; Settanni, V.; Mancini, A.; Di Venere, D.; Inchingolo, F.; Inchingolo, A.D.; et al. Analysis of Dental Enamel Remineralization: A Systematic Review of Technique Comparisons. Bioengineering 2023, 10, 472. [Google Scholar] [CrossRef]
- Dipalma, G.; Inchingolo, A.D.; Inchingolo, A.M.; Piras, F.; Carpentiere, V.; Garofoli, G.; Azzollini, D.; Campanelli, M.; Paduanelli, G.; Palermo, A.; et al. Artificial Intelligence and Its Clinical Applications in Orthodontics: A Systematic Review. Diagnostics 2023, 13, 3677. [Google Scholar] [CrossRef]
- Banning, J.A. Chronic fatigue and shift work. Can. Nurse 1991, 87, 3. [Google Scholar]
- Kalra, Y. Chronotype and Nursing Shift Work. Am. J. Nurs. 2025, 125, 64. [Google Scholar] [CrossRef] [PubMed]
- Tuominen, O.; Lundgren-Laine, H.; Teperi, S.; Salanterä, S. Comparing the Two Techniques for Nursing Staff Rescheduling to Streamline Nurse Managers’ Daily Work in Finland. Comput. Inform. Nurs. 2020, 38, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Albert-Sabater, J.A.; Martínez, J.M.; Baste, V.; Moen, B.E.; Ronda-Perez, E. Comparison of Menstrual Disorders in Hospital Nursing Staff According to Shift Work Pattern. J. Clin. Nurs. 2016, 25, 3291–3299. [Google Scholar] [CrossRef]
- Inchingolo, F.; Santacroce, L.; Ballini, A.; Topi, S.; Dipalma, G.; Haxhirexha, K.; Bottalico, L.; Charitos, I.A. Oral Cancer: A Historical Review. Int. J. Environ. Res. Public Health 2020, 17, 3168. [Google Scholar] [CrossRef] [PubMed]
- Coffey, L.C.; Skipper, J.K.J.; Jung, F.D. Nurses and Shift Work: Effects on Job Performance and Job-Related Stress. J. Adv. Nurs. 1988, 13, 245–254. [Google Scholar] [CrossRef]
- Stimpfel, A.W.; Fatehi, F.; Kovner, C. Nurses’ Sleep, Work Hours, and Patient Care Quality, and Safety. Sleep Health 2020, 6, 314–320. [Google Scholar] [CrossRef]
- Amritzer, M.A.; Muntlin, Å.; Berg, L.M.; Göransson, K.E. Nursing Staff Ratio and Skill Mix in Swedish Emergency Departments: A National Cross-Sectional Benchmark Study. J. Nurs. Manag. 2021, 29, 2594–2602. [Google Scholar] [CrossRef]
- Kalisch, B.J.; Lee, H. Nursing Teamwork, Staff Characteristics, Work Schedules, and Staffing. Health Care Manag. Rev. 2009, 34, 323–333. [Google Scholar] [CrossRef]
- Zverev, Y.P.; Misiri, H.E. Perceived Effects of Rotating Shift Work on Nurses’ Sleep Quality and Duration. Malawi Med. J. 2009, 21, 19–21. [Google Scholar] [CrossRef][Green Version]
- Haghayegh, S.; Liu, Y.; Zhang, Y.; Strohmaier, S.; Papantoniou, K.; Markt, S.; Giovannucci, E.; Schernhammer, E. Rotating Night Shift Work and Bladder Cancer Risk in Women: Results of Two Prospective Cohort Studies. Int. J. Environ. Res. Public Health 2023, 20, 2202. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Patano, A.; Di Pede, C.; Inchingolo, A.D.; Palmieri, G.; de Ruvo, E.; Campanelli, M.; Buongiorno, S.; Carpentiere, V.; Piras, F.; et al. Autologous Tooth Graft: Innovative Biomaterial for Bone Regeneration. Tooth Transformer® and the Role of Microbiota in Regenerative Dentistry. A Systematic Review. J. Funct. Biomater. 2023, 14, 132. [Google Scholar] [CrossRef] [PubMed]
- Malcangi, G.; Patano, A.; Ciocia, A.M.; Netti, A.; Viapiano, F.; Palumbo, I.; Trilli, I.; Guglielmo, M.; Inchingolo, A.D.; Dipalma, G.; et al. Benefits of Natural Antioxidants on Oral Health. Antioxidants 2023, 12, 1309. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Paracchini, L.; de Angelis, F.; Cielo, A.; Orefici, A.; Spitaleri, D.; Santacroce, L.; Gheno, E.; Palermo, A. Biomechanical Behaviour of a Jawbone Loaded with a Prosthetic System Supported by Monophasic and Biphasic Implants. Oral Implantol. 2016, 9, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Minetti, E.; Dipalma, G.; Palermo, A.; Patano, A.; Inchingolo, A.D.; Inchingolo, A.M.; Inchingolo, F. Biomolecular Mechanisms and Case Series Study of Socket Preservation with Tooth Grafts. J. Clin. Med. 2023, 12, 5611. [Google Scholar] [CrossRef]
- Bellocchio, L.; Inchingolo, A.D.; Inchingolo, A.M.; Lorusso, F.; Malcangi, G.; Santacroce, L.; Scarano, A.; Bordea, I.R.; Hazballa, D.; D’Oria, M.T.; et al. Cannabinoids Drugs and Oral Health-From Recreational Side-Effects to Medicinal Purposes: A Systematic Review. Int. J. Mol. Sci. 2021, 22, 8329. [Google Scholar] [CrossRef]
- Parhizkar, S.; Holtzman, D.M. The Night’s Watch: Exploring How Sleep Protects against Neurodegeneration. Neuron 2025, 113, 817–837. [Google Scholar] [CrossRef]
- Jørgensen, J.T.; Hansen, J.; Westendorp, R.G.J.; Nabe-Nielsen, K.; Stayner, L.T.; Simonsen, M.K.; Andersen, Z.J. Shift Work and Incidence of Dementia: A Danish Nurse Cohort Study. Alzheimer’s Dement. 2020, 16, 1268–1279. [Google Scholar] [CrossRef]
- Esmaily, A.; Jambarsang, S.; Mohammadian, F.; Mehrparvar, A.H. Effect of Shift Work on Working Memory, Attention and Response Time in Nurses. Int. J. Occup. Saf. Ergon. 2022, 28, 1085–1090. [Google Scholar] [CrossRef]
- Papantoniou, K.; Massa, J.; Devore, E.; Munger, K.L.; Chitnis, T.; Ascherio, A.; Schernhammer, E.S. Rotating Night Shift Work and Risk of Multiple Sclerosis in the Nurses’ Health Studies. Occup. Environ. Med. 2019, 76, 733–738. [Google Scholar] [CrossRef]
- Simunić, A.; Gregov, L. Conflict between Work and Family Roles and Satisfaction among Nurses in Different Shift Systems in Croatia: A Questionnaire Survey. Arh. Hig. Rada Toksikol. 2012, 63, 189–197. [Google Scholar] [CrossRef]
- Minelli, A.; Di Palma, M.; Rocchi, M.B.L.; Ponzio, E.; Barbadoro, P.; Bracci, M.; Pelusi, G.; Prospero, E. Cortisol, Chronotype, and Coping Styles as Determinants of Tolerance of Nursing Staff to Rotating Shift Work. Chronobiol. Int. 2021, 38, 666–680. [Google Scholar] [CrossRef]
- Feldman, K.; Rohan, A.J. Data-Driven Nurse Staffing in the Neonatal Intensive Care Unit. MCN Am. J. Matern. Child. Nurs. 2022, 47, 249–264. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Inchingolo, A.M.; Dipalma, G. Comparison between traditional surgery, CO2 and Nd:Yag laser treatment for generalized gingival hyperplasia in Sturge-Weber syndrome: A retrospective study. J. Investig. Clin. Dent. 2010, 1, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Pisarski, A.; Bohle, P.; Callan, V.J. Effects of Coping Strategies, Social Support and Work-Nonwork Conflict on Shift Worker’s Health. Scand. J. Work. Environ. Health 1998, 24 (Suppl. 3), 141–145. [Google Scholar] [PubMed]
- Min, A.; Kim, Y.M.; Yoon, Y.S.; Hong, H.C.; Kang, M.; Scott, L.D. Effects of Work Environments and Occupational Fatigue on Care Left Undone in Rotating Shift Nurses. J. Nurs. Scholarsh. 2021, 53, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Onrubia, I.M.; Resta Sánchez, E.J.; Cabañero Contreras, T.; Perona Moratalla, A.B.; Molina Alarcón, M. Emergency Nursing Staff’s Well-Being, Burnout, and Sleep on 12-Hour Shifts. Enferm. Clin. 2025, 35, 102141. [Google Scholar] [CrossRef]
- Jørgensen, J.T.; Rozing, M.P.; Westendorp, R.G.J.; Hansen, J.; Stayner, L.T.; Simonsen, M.K.; Andersen, Z.J. Shift Work and Incidence of Psychiatric Disorders: The Danish Nurse Cohort Study. J. Psychiatr. Res. 2021, 139, 132–138. [Google Scholar] [CrossRef]
- Vitale, E.; Lupo, R.; Artioli, G.; Mea, R.; Lezzi, P.; Conte, L.; De Nunzio, G. How Shift Work Influences Anxiety, Depression, Stress and Insomnia Conditions in Italian Nurses: An Exploratory Study. Acta Biomed. 2023, 94, e2023102. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Ejebu, O.-Z.; Ball, J.; Griffiths, P. Shift Work Characteristics and Burnout among Nurses: Cross-Sectional Survey. Occup. Med. 2023, 73, 199–204. [Google Scholar] [CrossRef]
- Camerino, D.; Conway, P.M.; Sartori, S.; Campanini, P.; Estryn-Béhar, M.; van der Heijden, B.I.J.M.; Costa, G. Factors Affecting Work Ability in Day and Shift-Working Nurses. Chronobiol. Int. 2008, 25, 425–442. [Google Scholar] [CrossRef]
- Kim, M.; Kim, J.-H.; Jung, Y.W.; Seong, S.J.; Kim, S.-Y.; Yoon, H.-J.; Lee, S.-S.; Kim, H.-J.; Ku, B.-S.; Cho, H.-Y. Gynecologic Problems and Healthcare Behavior by Shift Patterns in Korean Nursing Staff. PLoS ONE 2022, 17, e0276282. [Google Scholar] [CrossRef] [PubMed]
- Stimpfel, A.W.; Aiken, L.H. Hospital Staff Nurses’ Shift Length Associated with Safety and Quality of Care. J. Nurs. Care Qual. 2013, 28, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.M.; Hobbs, B.B. Impact of Shift Work on the Health and Safety of Nurses and Patients. Clin. J. Oncol. Nurs. 2006, 10, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Gonge, H.; Buus, N. Individual and Workplace Factors That Influence Psychiatric Nursing Staff’s Participation in Clinical Supervision: A Survey Study and Prospective Longitudinal Registration. Issues Ment. Health Nurs. 2010, 31, 345–354. [Google Scholar] [CrossRef]
- Saksvik-Lehouillier, I.; Bjorvatn, B.; Hetland, H.; Sandal, G.M.; Moen, B.E.; Magerøy, N.; Akerstedt, T.; Pallesen, S. Individual, Situational and Lifestyle Factors Related to Shift Work Tolerance among Nurses Who Are New to and Experienced in Night Work. J. Adv. Nurs. 2013, 69, 1136–1146. [Google Scholar] [CrossRef]
- Galanti, T.; Cortini, M.; Giudice, G.F.; Zappalà, S.; Toscano, F. Safeguarding Nurses’ Mental Health: The Critical Role of Psychosocial Safety Climate in Mitigating Relational Stressors and Exhaustion. AIMS Public Health 2024, 11, 905–917. [Google Scholar] [CrossRef]
- Clark, A.; Moule, P.; Topping, A.; Serpell, M. Rescheduling Nursing Shifts: Scoping the Challenge and Examining the Potential of Mathematical Model Based Tools. J. Nurs. Manag. 2015, 23, 411–420. [Google Scholar] [CrossRef]
- Inchingolo, F.; Ballini, A.; Mura, S.; Farronato, D.; Cirulli, N.; Pettini, F.; Gheno, E.; Vermesan, D.; Pederzoli, P.; Resta, G.; et al. Use of Platelet Rich Fibrin and Bio-OSS/SINT-Oss for Implant-Prosthetic Rehabilitation in Maxillary Atrophy with Sinus Pathology: A 48-Month Follow-Up. Eur. J. Inflamm. 2015, 13, 58–65. [Google Scholar] [CrossRef]
- de Cordova, P.B.; Phibbs, C.S.; Stone, P.W. Perceptions and Observations of Off-Shift Nursing. J. Nurs. Manag. 2013, 21, 283–292. [Google Scholar] [CrossRef]
- Weng, P.-W.; Chang, W.-P. Relationship between Shift Type and Sleep Quality in Rotating-Shift Nurses with Chronotype as a Moderator Variable. Int. Nurs. Rev. 2025, 72, e13010. [Google Scholar] [CrossRef]
- Salah, R.A.; Malak, M.Z.; Bani Salameh, A.K. Relationship between Shift-Work and Life-Style Behaviors among Emergency Department Nurses in Jordan. Arch. Environ. Occup. Health 2022, 77, 27–34. [Google Scholar] [CrossRef]
- Silva-Costa, A.; Rotenberg, L.; Griep, R.H.; Fischer, F.M. Relationship between Sleeping on the Night Shift and Recovery from Work among Nursing Workers—The Influence of Domestic Work. J. Adv. Nurs. 2011, 67, 972–981. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Pacifici, A.; Gargari, M.; Inchingolo, A.D.; Inchingolo, A.M.; Dipalma, G.; Marrelli, M.; Abenavoli, F.M.; Pacifici, L. Use of Dermal-Fat Grafts in the Post-Oncological Reconstructive Surgery of Atrophies in the Zygomatic Region: Clinical Evaluations in the Patients Undergone to Previous Radiation Therapy. Head Face Med. 2012, 8, 33. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Corelli, R.; Inchingolo, A.M.; Dipalma, G. Upper Eyelid Reconstruction: A Short Report of an Eyelid Defect Following a Thermal Burn. Head Face Med. 2009, 5, 26. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Di Pede, C.; Garibaldi, M.; Ciocia, A.M.; et al. Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report. Medicina 2022, 58, 603. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.M.; Malcangi, G.; Costa, S.; Fatone, M.C.; Avantario, P.; Campanelli, M.; Piras, F.; Patano, A.; Ferrara, I.; Di Pede, C.; et al. Tooth Complications after Orthodontic Miniscrews Insertion. Int. J. Environ. Res. Public Health 2023, 20, 1562. [Google Scholar] [CrossRef]
- Niu, S.-F.; Chung, M.-H.; Chu, H.; Tsai, J.-C.; Lin, C.-C.; Liao, Y.-M.; Ou, K.-L.; O’Brien, A.P.; Chou, K.-R. Differences in Cortisol Profiles and Circadian Adjustment Time between Nurses Working Night Shifts and Regular Day Shifts: A Prospective Longitudinal Study. Int. J. Nurs. Stud. 2015, 52, 1193–1201. [Google Scholar] [CrossRef]
- Shiffer, D.; Minonzio, M.; Dipaola, F.; Bertola, M.; Zamuner, A.R.; Dalla Vecchia, L.A.; Solbiati, M.; Costantino, G.; Furlan, R.; Barbic, F. Effects of Clockwise and Counterclockwise Job Shift Work Rotation on Sleep and Work-Life Balance on Hospital Nurses. Int. J. Environ. Res. Public Health 2018, 15, 2038. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Griffiths, P.; Emmanuel, T.; Rafferty, A.M.; Ewings, S. The RN4CAST Consortium 12-hr Shifts in Nursing: Do They Remove Unproductive Time and Information Loss or Do They Reduce Education and Discussion Opportunities for Nurses? A Cross-sectional Study in 12 European Countries. J. Clin. Nurs. 2020, 29, 53–59. [Google Scholar] [CrossRef]
- Inoue, M.; Takano, M.; Ueno, C.; Mori, M.; Morimatsu, Y.; Matsumoto, Y.; Kushino, N.; Ishitake, T. Advantages of the Variable Shift System, and Effective Use of Break Time to Better Support the Work Engagement of Nurses on Extended Day Shifts. Kurume Med. J. 2020, 65, 155–168. [Google Scholar] [CrossRef]
- Waage, S.; Pallesen, S.; Moen, B.E.; Vedaa, Ø.; Thun, E.; Vikanes Buchvold, H.; Blytt, K.M.; Harris, A.; Bjorvatn, B. Changes in Work Schedule Affect the Prevalence of Shift Work Disorder among Norwegian Nurses—A Two Year Follow-up Study. Chronobiol. Int. 2021, 38, 924–932. [Google Scholar] [CrossRef]
- Kubo, T.; Matsumoto, S.; Izawa, S.; Ikeda, H.; Nishimura, Y.; Kawakami, S.; Tamaki, M.; Masuda, S. Shift-Work Schedule Intervention for Extending Restart Breaks after Consecutive Night Shifts: A Non-Randomized Controlled Cross-Over Study. Int. J. Environ. Res. Public Health 2022, 19, 15042. [Google Scholar] [CrossRef]
- Jung, H.-S.; Lee, B. Contributors to Shift Work Tolerance in South Korean Nurses Working Rotating Shift. Appl. Nurs. Res. 2015, 28, 150–155. [Google Scholar] [CrossRef]
- Pahlevanzadeh, M.J.; Jolai, F.; Goodarzian, F.; Ghasemi, P. A New Two-Stage Nurse Scheduling Approach Based on Occupational Justice Considering Assurance Attendance in Works Shifts by Using Z-Number Method: A Real Case Study. RAIRO-Oper. Res. 2021, 55, 3317–3338. [Google Scholar] [CrossRef]
- Bülbül, E.; ÇeliK, S.; Özkan, A.; Akbaş, G. Assessment of the Chronotypes of Nurses Working in Shifts and the Quality of Their Lives. Clin. Exp. Health Sci. 2023, 13, 491–496. [Google Scholar] [CrossRef]
- Li, J.-N.; Chen, X.-Q.; Jiang, X.-M.; Zheng, Q.-X.; Pan, Y.-Q.; Zhu, Y.; Huang, L.; Liu, R.-L. Exploring the Associations between Chronotype, Night Shift Work Schedule, Quality of Work Life, and Sleep Quality among Maternal and Child Health Nurses: A Multicentre Cross-Sectional Study. J. Nurs. Manag. 2023, 2023, 1811732. [Google Scholar] [CrossRef]
- De Bruijn, L.; Berentzen, N.E.; Vermeulen, R.C.H.; Vlaanderen, J.J.; Kromhout, H.; Van Leeuwen, F.E.; Schaapveld, M. Chronotype in Relation to Shift Work: A Cohort Study among 37,731 Female Nurses. J. Sleep Res. 2024, 34, e14308. [Google Scholar] [CrossRef]
- Dehring, T.; Von Treuer, K.; Redley, B. The Impact of Shift Work and Organisational Climate on Nurse Health: A Cross-Sectional Study. BMC Health Serv. Res. 2018, 18, 586. [Google Scholar] [CrossRef]
- Abed Al Ahad, M.; Elbejjani, M.; Simon, M.; Ausserhofer, D.; Abu-Saad Huijer, H.; Dhaini, S.R. Variability, Shift-specific Workloads and Rationed Care Predictors of Work Satisfaction among Registered Nurses Providing Acute Care: A Longitudinal Study. Nurs. Open 2022, 9, 1190–1199. [Google Scholar] [CrossRef]
- Lee, J.; Jeong, I.S. Compliance with Recommendations on Work Schedule for Shift Nurses in South Korea. Saf. Health Work 2021, 12, 255–260. [Google Scholar] [CrossRef]
- Booker, L.A.; Mills, J.; Bish, M.; Spong, J.; Deacon-Crouch, M.; Skinner, T.C. Nurse Rostering: Understanding the Current Shift Work Scheduling Processes, Benefits, Limitations, and Potential Fatigue Risks. BMC Nurs. 2024, 23, 295. [Google Scholar] [CrossRef]
- Shin, S.-H.; Lee, E.-H. Development and Validation of a Quality of Healthy Work Environment Instrument for Shift Nurses. BMC Nurs. 2024, 23, 37. [Google Scholar] [CrossRef]
- Griepentrog, J.E.; Labiner, H.E.; Gunn, S.R.; Rosengart, M.R. Bright Environmental Light Improves the Sleepiness of Nightshift ICU Nurses. Crit. Care 2018, 22, 295. [Google Scholar] [CrossRef]
- Bjorvatn, B.; Pallesen, S.; Waage, S.; Thun, E.; Blytt, K.M. The Effects of Bright Light Treatment on Subjective and Objective Sleepiness during Three Consecutive Night Shifts among Hospital Nurses—A Counter-Balanced Placebo-Controlled Crossover Study. Scand. J. Work Environ. Health 2021, 47, 145–153. [Google Scholar] [CrossRef]
- Hoshi, H.; Iwasa, H.; Goto, A.; Yasumura, S. Effects of Working Environments with Minimum Night Lighting on Night-Shift Nurses’ Fatigue and Sleep, and Patient Safety. BMJ Open Qual. 2022, 11, e001638. [Google Scholar] [CrossRef]
- Kim, J.H.; Song, Y. The Effects of Indoor Ambient Temperature at Work on Physiological Adaptation in Night Shift Nurses. J. Nurs. Manag. 2020, 28, 1098–1103. [Google Scholar] [CrossRef]
- Sadeghniiat-Haghighi, K.; Bahrami, H.; Aminian, O.; Meysami, A.; Khajeh-Mehrizi, A. Melatonin Therapy in Shift Workers with Difficulty Falling Asleep: A Randomized, Double-Blind, Placebo-Controlled Crossover Field Study. Work 2016, 55, 225–230. [Google Scholar] [CrossRef]
- Gholipour Baradari, A.; Alipour, A.; Mahdavi, A.; Sharifi, H.; Nouraei, S.M.; Emami Zeydi, A. The Effect of Zinc Supplementation on Sleep Quality of ICU Nurses: A Double Blinded Randomized Controlled Trial. Workplace Health Saf. 2018, 66, 191–200. [Google Scholar] [CrossRef]
- Suyoto, P.S.; de Rijk, M.G.; de Vries, J.H.; Feskens, E.J. The Effect of Meal Glycemic Index and Meal Frequency on Glycemic Control and Variability in Female Nurses Working Night Shifts: A Two-Arm Randomized Cross-Over Trial. J. Nutr. 2024, 154, 69–78. [Google Scholar] [CrossRef]
- Leedo, E.; Beck, A.M.; Astrup, A.; Lassen, A.D. The Effectiveness of Healthy Meals at Work on Reaction Time, Mood and Dietary Intake: A Randomised Cross-over Study in Daytime and Shift Workers at an University Hospital. Br. J. Nutr. 2017, 118, 121–129. [Google Scholar] [CrossRef]
- Matsugaki, R.; Kuhara, S.; Saeki, S.; Jiang, Y.; Michishita, R.; Ohta, M.; Yamato, H. Effectiveness of Workplace Exercise Supervised by a Physical Therapist among Nurses Conducting Shift Work: A Randomized Controlled Trial. J. Occup. Health 2017, 59, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Baek, Y.; Han, K.; Kim, J.; Yoo, H.Y. Smartphone-Based Home Workout Program for Shift-Work Nurses Working during the COVID-19 Pandemic. Nurs. Health Sci. 2022, 24, 708–716. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, Y. Restorative Yoga for Occupational Stress among Japanese Female Nurses Working Night Shift: Randomized Crossover Trial. J. Occup. Health 2019, 61, 508–516. [Google Scholar] [CrossRef]
- Baek, G.; Cha, C. AI-Assisted Tailored Intervention for Nurse Burnout: A Three-Group Randomized Controlled Trial. Worldviews Evid. Based Nurs. 2025, 22, e70003. [Google Scholar] [CrossRef]
- Ell, J.; Brückner, H.A.; Johann, A.F.; Steinmetz, L.; Güth, L.J.; Feige, B.; Järnefelt, H.; Vallières, A.; Frase, L.; Domschke, K.; et al. Digital Cognitive Behavioural Therapy for Insomnia Reduces Insomnia in Nurses Suffering from Shift Work Disorder: A Randomised-Controlled Pilot Trial. J. Sleep. Res. 2024, 33, e14193. [Google Scholar] [CrossRef]
- Liu, W.; Wang, Q.; Zheng, D.; Mei, J.; Lu, J.; Chen, G.; Wang, W.; Ding, F. The Effects of a Complex Interactive Multimodal Intervention on Personalized Stress Management Among Health Care Workers in China: Nonrandomized Controlled Study. J. Med. Internet Res. 2024, 26, e45422. [Google Scholar] [CrossRef]
- Lu, C.; Sun, Y.; Wang, C.; Chen, T.; Tang, Y. The Effects of Confiding on Shift Work Nurses’ Emotion Regulation and Self-Perceived Well-Being: An Online Randomized Controlled Trial. Behav. Sci. 2025, 15, 9. [Google Scholar] [CrossRef]
- Watanabe, K.; Sugimura, N.; Shishido, I.; Konya, I.; Yamaguchi, S.; Yano, R. Effects of 90 Min Napping on Fatigue and Associated Environmental Factors among Nurses Working Long Night Shifts: A Longitudinal Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 9429. [Google Scholar] [CrossRef]
- Watanabe, K.; Shishido, I.; Ito, Y.M.; Yano, R. Quantity and quality of napping to mitigate fatigue and sleepiness among nurses working long night shifts: A prospective observational study. J. Physiol. Anthropol. 2025, 44, 1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Booker, L.A.; Sletten, T.L.; Barnes, M.; Alvaro, P.; Collins, A.; Chai-Coetzer, C.L.; McMahon, M.; Lockley, S.W.; Rajaratnam, S.M.W.; Howard, M.E. The Effectiveness of an Individualized Sleep and Shift Work Education and Coaching Program to Manage Shift Work Disorder in Nurses: A Randomized Controlled Trial. J. Clin. Sleep Med. 2022, 18, 1035–1045. [Google Scholar] [CrossRef]
- Albakri, U.; Smeets, N.; Kant, I.; Meertens, R. Strategies That Nurses Working Irregular Night Shifts Use to Improve Sleep Quality: A Qualitative Study among Good and Poor Sleepers. J. Adv. Nurs. 2024, 80, 2038–2050. [Google Scholar] [CrossRef]
- Oriyama, S.; Miyakoshi, Y.; Rahman, M.M. The Effects of a 120-Minute Nap on Sleepiness, Fatigue, and Performance during 16-Hour Night Shifts: A Pilot Study. J. Occup. Health 2019, 61, 368–377. [Google Scholar] [CrossRef]
- Comparative Effects of Music Therapy and Aromatherapy on Stress, Quality of Life, and Happiness Among Shift Nurses in Korea: A Randomized Controlled Trial. Available online: https://jkbns.org/journal/view.php?number=657 (accessed on 29 March 2025).
- Wang, X.; Feng, T.; Liu, S.; Ruan, J. Application of Music Therapy in Improving the Sleep Quality and Mental Health of Nurses with Circadian Rhythm Sleep Disorders Caused by Work Shifts. Noise Health 2024, 26, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Zamanifar, S.; Bagheri-Saveh, M.I.; Nezakati, A.; Mohammadi, R.; Seidi, J. The Effect of Music Therapy and Aromatherapy with Chamomile-Lavender Essential Oil on the Anxiety of Clinical Nurses: A Randomized and Double-Blind Clinical Trial. J. Med. Life 2020, 13, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Molzof, H.E.; Wirth, M.D.; Burch, J.B.; Shivappa, N.; Hebert, J.R.; Johnson, R.L.; Gamble, K.L. The Impact of Meal Timing on Cardiometabolic Syndrome Indicators in Shift Workers. Chronobiol. Int. 2017, 34, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Nasiri, A.; Boroomand, M.M. The Effect of Rosemary Essential Oil Inhalation on Sleepiness and Alertness of Shift-Working Nurses: A Randomized, Controlled Field Trial. Complement. Ther. Clin. Pract. 2021, 43, 101326. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).



