Abstract
Background: Nursing leadership is associated with a host of benefits for patient outcomes and health services. Pressures relating to the COVID-19 pandemic saw many relatively inexperienced nurses thrust into leadership roles, often with little notice. In response to this situation, The Tasmanian Health Service—Hospitals South created the Leadership Excellence in Practice Program (L-EPP) as a way of developing the leadership skills of its nurses and midwives. This study aimed to describe the development of the L-EPP and to evaluate it from the perspective of its participants and their peers. Methods: A longitudinal mixed-methods study was conducted using data from the first two offerings of the L-EPP. The L-EPP employs a blended learning model comprised of e-learning, work-integrated learning and face-to-face workshops. Surveys targeting the participants’ leadership abilities were completed at numerous time points by participants themselves, their peers, and their managers. Results: A total of 57 participants completed the program. Workshop surveys indicated that these sessions were generally well-received by participants. Significant improvements were observed in several domains of leadership, from the perspective of the participants themselves and their peers and managers. Conclusions: The program was well-received by its participants, and would serve as a useful template for other organisations seeking to build the leadership capacity of their nurses and midwives. This may be particularly useful to organisations seeking to upskill their existing staff and prevent further attrition of nurses and midwives in the wake of the pandemic.
1. Introduction
At a broad level, leadership can be defined as “a process whereby an individual influences a group of individuals to achieve a common goal” [1] (p. 3). Leadership is a contextual phenomenon, meaning that factors such as the current organisational climate and team dynamics will influence which styles of leadership are most effective [2]. In a nursing context, effective leadership has long been associated with a host of positive outcomes, including improved patient outcomes [3,4,5], job satisfaction [6] and organisational performance [7]. The need to promote nursing leadership development has been recognised by several professional bodies (e.g., the International Council of Nurses, and the Australian College of Nursing) who now offer leadership development programs to their members [8,9]. Such courses often contain a didactic component as well as ongoing support to participants (e.g., in the form of mentoring, and career coaching) [8]. While such programs are undoubtedly beneficial, there is a recognition that leadership as a context-specific phenomenon, is something that must also be developed and delivered in-house (e.g., by supplementing learnings with workshops held on-site) [10]. In-house programs also have the advantage of being tailored towards the organisation’s needs and are delivered by people who are familiar with current challenges faced by the organisation [11].
The arrival of the COVID-19 pandemic in 2020 presented another set of challenges to the development of leadership in the profession of nursing. Faced with higher rates of illness and staff burnout, many nurses left the industry [12], in what some commentators have referred to as ‘The Great Attrition’ [13]. One observed effect of this attrition was that many relatively junior nurses were required to take on roles vacated by their more senior counterparts, often at short notice [14]. In Tasmania, Australia, it was recognised that nurses and midwives in this category who were employed by the state’s health service could benefit from leadership development opportunities, given that prior to the pandemic, such opportunities were primarily targeted towards more experienced nurses and midwives. This observation was supported by a 2020 systematic review of leadership development programs delivered in Australian hospitals [15] which found that most programs aimed to upskill nurses who were already in leadership or managerial roles, as opposed to fostering new leaders. The same review highlighted that little emphasis had traditionally been placed on the formal evaluation of programs, with most studies limiting their focus to the satisfaction of program participants [15]. This is problematic, given the large investment required to develop and conduct such programs [16].
In light of this perceived gap in the literature and the emerging challenges noted above, the Tasmanian Health Service—Hospitals South (THS-S) developed its Leadership Excellence in Practice Program (L-EPP) as a tailored solution for its local setting. The aim of the current study is to describe the development of the L-EPP and to evaluate the L-EPP from the perspective of the initial cohort of participants who completed the Program and their peers. Conducting this study will help to refine the L-EPP itself, while also aiding other health services seeking to develop similar programs.
Background
The L-EPP was created by a team of Clinical Nurse Educators (CNEs) from the Tasmanian Health Service—Hospitals South’s (THS-S) Centre for Education and Research- Nursing & Midwifery (CERNM) throughout the course of 2021. This team of CNEs (herein referred to as the development team) also co-authored this manuscript. The L-EPP is underpinned by Transformational leadership, as the Tasmanian Health Service has committed to seek ‘Magnet’ accreditation. Magnet is a North American nursing program that strives towards an innovative work culture that leads nursing and midwifery in the provision of high-quality care [17]. One of the components of Magnet is transformational leadership, regarded as one of the most effective leadership styles in health services. In Transformational leadership, a leader mobilises employees’ motivations toward a shared vision by inspiring them to perform at a high level to produce better patient and organisational outcomes [18]. The L-EPP was created using an existing framework developed by the CERNM in 2019, known as the Excellence in Practice Program (EPP) framework. The EPP framework itself was created following an internal review of the CERNM’s activities, which considered how the unit could improve major clinical and professional issues in the health service. The review identified that many of the educational programs being delivered were not being thoroughly evaluated afterwards, and hence, there was a need for a new framework with a focus on evaluation.
Under the EPP framework, focused learning experiences are provided over a 3-month period, using a structured model of blended learning, work-integrated projects (WIPs), and supported and self-directed learning [19]. A blended learning model was chosen for several reasons. Providing foundational and theoretical learning through online delivery means that the valuable face-to-face time in the workshops can be focused on interactive activities and group-based learning. The online learning components can be self-paced between workshops, which can address some of the barriers nurses and midwives may have in accessing continuing education, including workload demands, shift work, and staff shortages [20]. The content of the L-EPP was determined following an extensive literature review of current best practices, and also consultation with stakeholders within the THS-S (e.g., in-house subject matter experts, potential participants).
A WIP was incorporated into the framework to provide an opportunity for translating the knowledge and skills acquired into practice. According to Frenk et al., transformative educational models that integrate theoretical learning with practical application are essential for preparing health professionals to meet the complex demands of modern healthcare systems [21]. The authors emphasise that such approaches foster continuous professional development and lifelong learning, which are essential for maintaining high standards of patient care and adapting to evolving healthcare environments [21]. By engaging in WIPs, nurses and midwives can directly apply their learning to real-world clinical settings, thereby enhancing their competencies and improving health outcomes. This hands-on experience not only solidifies their theoretical knowledge, but also equips them with the skills necessary to navigate the practical challenges they will face in their professional roles [21].
2. Materials and Methods
2.1. Design
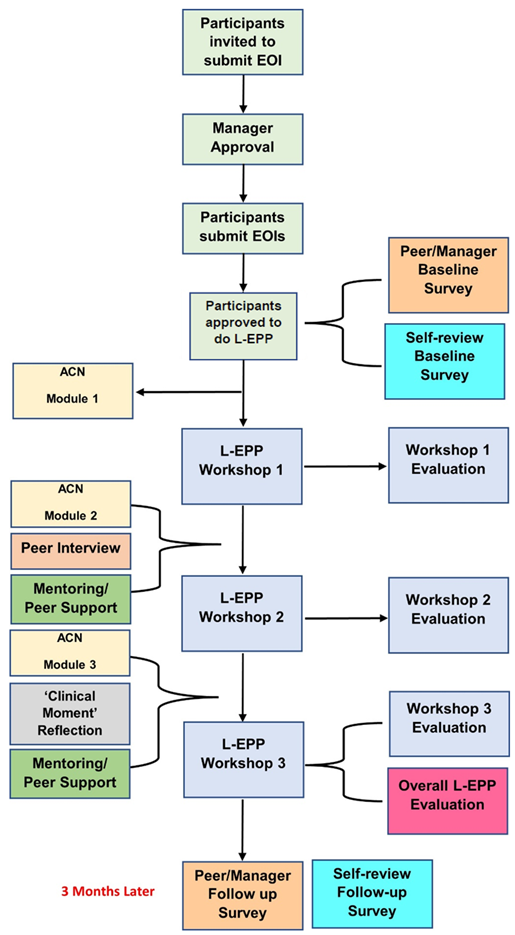
A longitudinal mixed-methods study was conducted using survey data relating to two consecutive offerings of the L-EPP; the inaugural Program in 2021 and its second iteration in 2022. Quantitative and qualitative survey data were analysed separately and then presented using Kirkpatrick’s Four Levels of Training Evaluation model [22]. A longitudinal design was chosen to measure changes in learners’ behaviour (a key aspect of Kirkpatrick’s model) [22]. Behaviour changes in the context of this study are defined as the degree to which participants apply what they learned during the L-EPP when in practice [23]. Furthermore, Kirkpatrick’s model provides a clear structure for how outcomes can be measured; allowing organisations to improve their educational interventions [24]. Appendix A shows the flow of participants through the L-EPP in both years.
2.2. Setting
The THS-S includes the Royal Hobart Hospital, which is the largest of four tertiary care centres in the Australian state of Tasmania, with a capacity of 566 beds [25]. As of 2019, there were 1662 nurses and 106 midwives employed by the THS-S.
2.3. Sample
The study used a purposive sample, whereby all nurses and midwives employed by the THS-S at Grade 2–4 level (including those currently working on a casual/per-diem basis) were sent an email inviting them to submit an expression of interest (EOI) in completing the L-EPP. This cohort was targeted following a needs assessment of existing leadership development opportunities within the organisation, which highlighted that no opportunities were currently available to this group. Nurses and midwives employed by external agencies were not targeted, as it would be difficult for such individuals to complete WIPs mandated by the program. Nurses and midwives were selected for this program as it is the remit of the development team to provide educational opportunities to this group. Details of the L-EPP were also advertised on the THS-S intranet. This intranet page and the invitation email advised recipients that they were eligible to participate in the L-EPP if they were a direct care enrolled or registered nurse or midwife employed at Grade 2–4 level with greater than 12 months’ experience, following the initial date of registration in their profession. Participants needed the endorsement of their line manager in order to apply, and also needed to agree to pay $120AUD to complete a suite of online learning modules delivered by the Australian College of Nursing (ACN), which are discussed further below. An optional strengths assessment and coaching session were also offered to participants in this email, at an additional cost of $30AUD.
In addition to the above criteria, applicants were required to answer a series of questions about what they hoped to gain by undertaking the L-EPP (i.e., their learning objectives). Applications were then assessed on the perceived benefit each applicant would obtain from completing the L-EPP. Applicants whose learning objectives could not be met by the L-EPP were referred to more suitable learning opportunities available in the organisation. Consideration was also given to the participants’ roles and workplaces, to ensure that the cohort was diverse and broadly representative of the wider population of nurses and midwives in the THS-S. A total of 57 participants commenced the L-EPP during the study period (30 in 2021, 27 in 2022) who were the focus of this evaluation study. Enrolments were capped at this number in both years, as this was deemed to be the maximum number possible whilst still providing participants with an optimal experience.
2.4. The Leadership Excellence in Practice Program
The L-EPP employs a blended learning model comprised of three components: (1) e-learning, (2) work-integrated learning (WIL), and (3) face-to-face workshops, all of which were facilitated by the development team. As noted above, the e-learning component of the L-EPP was comprised of three online modules hosted by the ACN. These modules, which are listed below, were chosen as they were readily available and evidence-based resources which the team deemed suitable for the THS-S’s organisational context. It was also hoped that by becoming members of the ACN and accessing its library of resources, participants would be more likely to undertake modules on other topics and engage with this professional body more broadly. The timing of these modules was designed to align with the content of each upcoming workshop. Accordingly, participants completed the first module before the first workshop, the second module before the second workshop, and the third before the third workshop.
- Module One: Foundational Concepts in Nursing Leadership
- Module Two: Staff Engagement and Communication
- Module Three: Professional Issues in Contemporary Nursing
The WIL phase required L-EPP participants to develop and undertake a relevant WIP within their workplace, which was based upon an identified need in their workplace. Three face-to-face workshops were held 4–6 weeks apart. Participants were issued with a set of pre-reading documents to prepare themselves for each workshop. Workshops one and two each consisted of seven interactive sessions on various topics delivered by the development team and a number of experienced leaders from the broader Tasmanian healthcare system.
The third workshop was comprised of five-minute presentations from each of the participants about the process they took to conduct their WIL projects, followed by five minutes of question time from the audience. This day concluded with an address from experienced leaders from various levels of the healthcare system. The delivery of the 2021 workshops was slightly refined using participant feedback prior to the 2022 offering. Specifically, one session was altered after participants in the 2021 cohort indicated that its content was pitched at too high a level for them. Workshop topics and learning outcomes otherwise remained the same in both years.
Several activities also took place between workshops. Firstly, each member of the development team was allocated 5–6 participants to provide support during the Program. In addition to being a point of contact for any queries, team members also held a series of optional online ‘drop-in sessions’ for their allocated participants, where attendees could ask questions of the team member and their fellow participants (e.g., “how can I access data to inform my WIP?”). These sessions were also used as an opportunity to develop participants’ critical thinking skills. Further opportunities for participants to network with each other were made possible by using a ‘Learning Hub’ intranet page, where participants could post queries to, and collaborate with, other L-EPP participants. The hub also provided updates from facilitators, and access to presentations and other learning resources from the workshops.
Between workshops two and three, participants had the option to complete a ‘Clinical Moment’ reflective piece, in which they reflected on an episode of leadership in practice. Participants who underwent the strengths assessment mentioned above were offered a coaching session with a member of the development team (KS; an accredited coach), in which they could explore their identified strengths, and how these are expressed in their place of work and their leadership journey. Lastly, participants also took part in a compulsory ‘buddying’ activity, whereby each participant selected another participant to interview about their objectives in undertaking the Program, and the nature and challenges of their leadership journey. Appendix B displays the L-EPP’s 13 learning outcomes which were mapped to the Program’s three modes of delivery mentioned above. Participants were not required to pay any money in order to take part in the program, however, they did stand to gain from their participation through the acquisition of new skills.
2.5. Data Collection
Participants completed surveys addressing their own leadership capabilities at baseline (i.e., prior to their first workshop) and at follow-up, which occurred three months after the third workshop in both years. This interval was used to allow sufficient time for the participants’ learning to be embedded. The questions for this survey required participants to rate their perceived ability in 22 aspects of leadership, 16 of which were Zenger and Folkman’s leadership competencies [26] with the remainder being created by the development team. The rating of competencies was done using a 10-point scale (10 being the highest rating, 1 being the lowest). Surveys addressing the same leadership competencies, albeit from the perspective of the participant’s current manager and a peer-nominated by the participant, were also completed at baseline and follow-up.
Surveys in relation to each individual workshop were completed by participants during a 30-min window set aside at the conclusion of that workshop. These required participants to rate the presentation and time (duration) of each workshop session using 4 and 3-point Likert scales, respectively. The content of each workshop session was rated using binary responses of ‘relevant’ and ‘irrelevant’. Paper surveys were used in the 2021 Program, while the 2022 Program used a QR code linked to an online survey portal, which participants could scan and complete using their devices. Each workshop survey also contained five free-text questions, targeting which aspects of the day participants felt were most/least useful, and the extent to which they had learned skills which could be applied in their workplaces. An ‘overarching’ survey was distributed to participants upon completion of their third workshop, which addressed the program as a whole. These surveys consisted of 11 free-text questions, which targeted the overall impact the Program had on participants across a number of domains (e.g., skills acquired, behaviour changes). Each of the above surveys was created by the development team.
2.6. Data Analysis
All data were analysed upon completion of the second offering’s follow-up period by two academics. These academics were selected on account of their expertise, and because they were not involved in the development, delivery or ongoing administration of the L-EPP. Data relating to both the 2021 and 2022 iterations of the L-EPP were pooled together for analysis. Quantitative data were analysed in IBM SPSS Version 29.0 (Armonk, NY, USA) using descriptive statistics (frequencies, means, percentages). Paired samples t-tests were also used to determine whether there had been improvements in participants’ leadership abilities from baseline to follow-up. Missing pre or post-data (e.g., from participants, their peers or managers failing to return baseline and/or follow-up surveys) were excluded pairwise. Qualitative data were analysed using a thematic analysis framework [27]. The analysis involves the following stages: code material; identify themes construct thematic networks; describe and explore thematic networks; and interpret patterns. This inductive analysis is carried out by developing basic themes, organising themes, and overarching global themes, in combination with a deductive approach, whereby the first three levels of Kirkpatrick’s model [22] served as global themes: Reaction, Learning and Behaviour. This hybrid approach of using both inductive and deductive analysis complements each other, and prevents salient data from being missed, thus increasing the rigour of the analysis.
Kirkpatrick’s Evaluation Framework
Once all quantitative and qualitative data had been analysed, the data were merged and presented using Kirkpatrick’s evaluation framework, which assesses training and education programs using a four-level approach [22]. For the purpose of the current study, only the first three levels of Kirkpatrick’s model were utilised. Table 1 shows what is targeted by each of the first three levels of Kirkpatrick’s model, along with which data sources were used to inform each level in the current study.

Table 1.
Levels of Kirkpatrick’s Model and Accompanying Data Sources.
3. Results
3.1. Description of Sample
The inaugural L-EPP ran from May to August 2021, while the second iteration ran slightly longer (from May until November 2022), owing to the need to postpone one workshop due to the effects of COVID-19. Of the participants who commenced the L-EPP in both years, 27 followed it through to completion in 2021, while only 17 completed the 2022 L-EPP. This attrition resulted in missing data for the pre-post appraisals. After missing data were excluded pairwise, the appraisal data from the participants themselves, their peers, and managers, had matched pairs of N = 27, N = 12 and N = 14, respectively. Most (>90%) participants were female and were registered nurses or midwives employed at the Grade 3–4 level, with only two participants who were Grade 2 level enrolled nurses. Participants in both years were employed in a variety of different areas within the health service, with representation from a host of medical, surgical, a community-based teams, along with mental health. In both years, twelve participants opted to undertake the abovementioned strengths assessment and coaching.
3.2. Kirkpatrick’s Model Level 1—Participants’ Reaction to the L-EPP
Table 2 summarises the participants’ reactions to the sessions comprising each of the L-EPP’s three workshops. The content of the workshops was almost unanimously (97%) regarded as being relevant. A majority of respondents (57%) stated that the presentation of the workshops was excellent, while the number of respondents who found the presentations to be inadequate was negligibly small (<1%). Most respondents (84%) found the duration of sessions within the workshops to be adequate, however, there were smaller numbers of participants who found the duration of some sessions to be inadequate or excessive (4% and 11% of respondents, respectively). Table 3 presents the qualitative data analysis including global themes, categories and codes. The global theme of value adding and waste aligned well with level 1 of Kirkpatrick’s model, as participants expressed their reaction to the L-EPP. Participants felt that the presenters and educators encouraged them to learn from others. This learning was identified when participants spoke about the health service improvement projects they carried out as part of the Program.

Table 2.
Participants’ Reaction to the L-EPP.

Table 3.
Qualitative Data Analysis.
Some of the other projects… are applicable to our unit; they have been inspiring and increased my awareness of other gaps within my unit.
Other participants articulated that the Program added value to their professional life. This was expressed as becoming a mindful leader who could make a difference.
It felt practical and relevant and made me feel like I could achieve something that would make a difference.
One participant noted that some of the content related to Quality and Safety was duplicated from an existing in-house Quality and Safety Course.
I have already covered most of the content in other workshops.
Participants expressed that a small number of components of the Program were not value-adding and improvements were required. One such component was the session in relation to evidence-based practice and leadership.
I feel I got lost in the presentation and the different abbreviations and systems.
3.3. Kirkpatrick’s Model Level 2—Learning
The global theme ‘Learning to see’ entails skills that developed during the Program, which involves assessing the current state of care provision issues, and after an issue has been identified, a plan is developed to address the issue. This was followed by actions taken to implement improvements.
This leadership course—helped me see improvements that could be made in our unit and now I can influence, motivate, and inspire others.
The Program helped participants to understand themselves as leaders and it increased their awareness of what a leader should or should not be. It gave them insight into skills they would like to learn, and it changed their views about leadership.
This Program changed my point of view about a leader. I got more clear understanding of leadership qualities.
It appeared that collaboration was a central component of the Program, encouraged by the opportunities for participants to work together and through recognising each other’s experience and ways of working.
Identifying all the different personalities and experience of others and importance to ask/seek multiple viewpoints to get good understanding.
This program has helped me step outside my comfort zone and engage with my peers, a skill I have been able to transfer to clinical practice.
3.4. Kirkpatrick’s Model Level 3—Behaviour
Table 4 summarises the participants’ improvements in various leadership capabilities, from the perspective of the participants themselves, their nominated peer, and their current manager. Participants reported significant improvements in all but one domain ‘Is comfortable with, and values input of experts’. Ratings by the participants showed improvements in all 22 domains, however, only five of these were statistically significant. Ratings from participants’ managers showed a similar pattern; while some degree of improvement was observed in all 22 domains, only 14 of these results were statistically significant. There were no instances where participants (either from their own perspective, or that of their peers or managers) were found to have a decreased capability over time. The global theme ‘understanding leadership’ includes the codes being-self-aware, being reflective, seeking others and changing views. Particularly, self-awareness and seeking others played a large role in understanding leadership, as participants started to recognise personality traits within themselves and other people. This recognition of others became clear through actively seeking mentors.

Table 4.
Participants’ Pre-Post Improvements in Leadership Domains †.
Thinking and seeking out important people. ‘Mentors’ for different aspects in working life will help me to have multiple viewpoints.
Many participants learnt how to become better leaders, and they articulated this by having gained enhanced knowledge and skills, building on their existing leadership foundation.
I have a foundation to build upon my understanding and practice in leadership.
Completing the Program increased participants’ confidence, and many felt better equipped to help champion change in their workplace and to handle conflict.
There are challenges within in my workplace that I feel prepared to manage now.
I am more able to reach positive outcomes in conflict and scenarios which prior may have overwhelmed me.
The final global theme ‘collaborative ways of working’ involves the motivation to work together and contributed to building networks and sharing of knowledge.
I have been establishing connections with staff outside my practice area by sharing knowledge about things that I use in my area.
4. Discussion
This study evaluated a leadership program developed for direct care nurses and midwives. Our findings demonstrate that this program, which was designed and delivered by in-house CNEs, has greatly benefited the initial cohort of participants who undertook it. These findings also indicate that the EPP framework is an appropriate platform for providing education on leadership development. In relation to Level 1 of Kirkpatrick’s Model (reaction), it is evident that the Program was generally very well-received by the participants. The main criticism in this regard came from a relatively small number of respondents who found the duration of certain workshop sessions to be excessive, with a smaller number reporting that the sessions were too brief. Some participants found the content of the session on evidence-based practice to be in need of improvement. On reflection, this session may have too been complex for nurses and midwives working in direct care roles, and perhaps would have been better pitched towards a more appropriate level.
Central to Level 2 of Kirkpatrick’s model (learning) [22] was the evidence of collaboration between participants, contributing to effective networks and leadership development. This is consistent with Paterson and colleagues, who found that nurses in their leadership program who shared thoughts and reflections, contributed to clarity and coherence in relation to continuous building of personal leadership capacity [28]. The Program’s WIPs contributed to creating insights and learning, and it is important to note that the benefit of these projects will likely be reaped by both the participants themselves (e.g., in the form of increased confidence and competency) and to the wider organisation, in the form of improved systems and processes consistent with other studies investigation the outcomes of WIPs [29,30].
The high number of significant improvements in leadership capabilities reported by the participants may be partly due to participants initially underestimating their own abilities. Indeed, the participants’ appraisal of their baseline ability to create a SMART goal was the lowest mean rating given by any party at any timepoint, and by a substantial margin. This tendency to downplay one’s abilities has been shown to be particularly pronounced among women [31], who comprised a majority of the current study’s participants. The lack of significant improvements in participants’ leadership capabilities from the perspective of their peers is likely due to the fact that, in many cases, baseline ratings were quite high. This is exemplified in the findings for ‘Is an asset, value adding to the team and organisation’ and ‘Practices self-development’, which, despite having mean ratings at follow-up of over 9/10, were both statistically non-significant improvements. This finding is in contrast with other studies where supervisors and peers reported on participants’ improvements in performance as a leader [32,33]. It is unknown why peers in this study ranked the leadership capabilities high and this warrants further investigation.
As Australia’s only island state, Tasmania was able to effectively insulate itself from the initial wave of COVID-19 cases by preventing all non-essential travel into the state. This policy was relaxed in December 2021, when the state government reopened borders to all arrivals from interstate and abroad, resulting in a sharp increase in the number of COVID-19 cases in the proceeding months. This increase, and the resulting strain on the state’s health service, occurred during the running and follow-up period of the 2022 L-EPP, and is a likely explanation for the high rates of missing data observed in the peer and manager surveys for that year. For instance, it is possible that participants were unwell themselves, or had otherwise disengaged from the Program after the final workshop day, and were reluctant to ask their peers or managers to complete a non-essential task such a survey during this busy period. This phenomenon was observed elsewhere during the COVID-19 pandemic, whereby healthcare facilities were asked to restrict all non-essential activities [34]. The post-COVID-19 era has been characterised by high rates of staff turnover, burnout, and a considerable number of nurses and midwives leaving the industry altogether [35]. The local context in which the L-EPP took place has not been immune to these forces, with rates of anxiety, depression, and post-traumatic stress disorder being reported previously [36]. The arrival of the L-EPP in the midst of the pandemic likely played a role in decreasing staff members’ intention to leave, as it represents a much-needed form of organisational support [37]. The L-EPP serves as a prime example of how other healthcare organisations can enhance their workforce capacity by implementing a similar program, as the design of the L-EPP is potentially a good fit for organisations who share a passion for leadership development and strive to retain well educated nursing staff.
This study has limitations which must be acknowledged. As noted above, data in relation to Level 4 of Kirkpatrick’s model (Results) are not presented in the current study. Given that the study participants represent only a small portion of the organisation’s workforce, it would be ill-advisable to draw links between the L-EPP and changes in broader system performance, such as reduced costs and improved quality. Further research is needed to look at the L-EPP’s impact on ‘Level 4a’ as described by Frich and colleagues [38], focusing on organisational results from the perspective of the participants and their subordinates (e.g., in terms of their job satisfaction, career progression and staff retention) among other factors. A second limitation relates to the fact that the study did not employ a control group, and hence, it is possible that reported improvements may be partly attributed to factors other than participation in the program. Another limitation of our study is that the surveys completed by participants at the close of each workshop had not been validated prior to being used.
5. Conclusions
Structured leadership development opportunities at the level of clinical nursing and midwifery are essential to improving patient and organisational outcomes. The development of the L-EPP and its longitudinal evaluation have demonstrated that participants have made improvements in almost all domains of leadership development. This, in turn, suggests that the Program has made a difference in building leadership capability within the THS-S, and potentially preventing some attrition of its staff. It is hoped that the success of this Program can be replicated in other health services within Tasmania and Australia, many of whom would be facing similar challenges.
Author Contributions
M.D.: Methodology, Formal analysis, Writing—Original Draft, Writing—Review & Editing. P.J.V.D.: Methodology, Formal analysis, Writing—Original Draft, Writing—Review & Editing. K.C.: Conceptualization, Writing—Original Draft, Writing—Review & Editing. K.S.: Conceptualization, Writing—Original Draft, Writing—Review & Editing. J.C.: Conceptualization, Writing—Original Draft, Writing—Review & Editing. S.F.: Conceptualization, Writing—Original Draft, Writing—Review & Editing. A.M.: Conceptualization, Writing—Original Draft, Writing—Review & Editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved on 12 December 2022 by the Tasmanian Human Research Ethics Committee (Project ID 27668).
Informed Consent Statement
Informed consent was waived because the study was conducted using data from the first two offerings of the L-EPP.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author(s).
Conflicts of Interest
Authors K.C., S.F., K.S., J.C. and A.M. are employed by the Tasmanian Health Service—Hospitals South, however, to minimise any biases, these five authors were not involved in the evaluation of the L-EPP, which was handled exclusively by P.J.V.D. and M.D.
Appendix A. The Flow of Participants Through L-EPP
Appendix B. L-EPP Learning Objectives
| 1. To assist participants with professional development, clinical progression and professional growth and goal achievement |
| 2. To assist participants in developing lifelong learning capability in the area of leadership |
| 3. To engage participants in active learning as an approach for focusing professional effectiveness in the practice setting |
| 4. To identify areas of need and address them using a structured and outcome-related educational framework to improve patient and staff safety |
| 5. To improve organisational leadership capacity within the nursing and midwifery workforce |
| 6. To recognise and utilise leadership capabilities skills and knowledge in clinical practice, leading others in practice |
| 7. To develop knowledge and skills in using leadership facilitation frameworks to gain self and situational awareness to assist in practicing in a leadership role |
| 8. To identify participants’ own strengths and develop their knowledge and skills in critical self-reflection, to inform areas for own self-development relating to self and emotional awareness |
| 9. To reflect on participants’ own learning in an environment of high support and high challenge |
| 10. To identify ways of working to support group and team collaboration |
| 11. To develop communication strategies for engaging with teams in collaborative ways of working |
| 12. To understand the benefits of a multi-disciplinary team in leadership |
| 13. To demonstrate increasing positive leadership qualities in practice |
References
- Northouse, P.G. Leadership: Theory and Practice; Sage Publications: Thousand Oaks, CA, USA, 2021. [Google Scholar]
- Cummings, G.G.; Tate, K.; Lee, S.; Wong, C.A.; Paananen, T.; Micaroni, S.P.; Chatterjee, G.E. Leadership styles and outcome patterns for the nursing workforce and work environment: A systematic review. Int. J. Nurs. Stud. 2018, 85, 19–60. [Google Scholar] [CrossRef] [PubMed]
- Paterson, K.; Henderson, A.; Trivella, A. Educating for leadership: A programme designed to build a responsive health care culture. J. Nurs. Manag. 2010, 18, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Davidson, P.M.; Elliott, D.; Daly, J. Clinical leadership in contemporary clinical practice: Implications for nursing in Australia. J. Nurs. Manag. 2006, 14, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Boyle, S.M. Nursing unit characteristics and patient outcomes. Nurs. Econ. 2004, 22, 111. [Google Scholar]
- Specchia, M.L.; Cozzolino, M.R.; Carini, E.; Di Pilla, A.; Galletti, C.; Ricciardi, W.; Damiani, G. Leadership Styles and Nurses’ Job Satisfaction. Results of a Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 1552. [Google Scholar] [CrossRef]
- Germain, P.B.; Cummings, G.G. The influence of nursing leadership on nurse performance: A systematic literature review. J. Nurs. Manag. 2010, 18, 425–439. [Google Scholar] [CrossRef]
- International Council of Nurses. Global Nursing Leadership Institute (GLNI). Available online: https://www.icn.ch/how-we-do-it/nna-development-leadership-programmes/global-nursing-leadership-institutetm-gnli (accessed on 14 September 2024).
- Australian College of Nursing. Institute of Leadership. Available online: https://iol.acn.edu.au/ (accessed on 14 September 2024).
- Cummings, G.G.; Lee, S.; Tate, K.; Penconek, T.; Micaroni, S.P.M.; Paananen, T.; Chatterjee, G.E. The essentials of nursing leadership: A systematic review of factors and educational interventions influencing nursing leadership. Int. J. Nurs. Stud. 2021, 115, 103842. [Google Scholar] [CrossRef]
- Phillips, N.; Byrne, G. Enhancing frontline clinical leadership in an acute hospital trust. J. Clin. Nurs. 2013, 22, 2625–2635. [Google Scholar] [CrossRef]
- Tolksdorf, K.H.; Tischler, U.; Heinrichs, K. Correlates of turnover intention among nursing staff in the COVID-19 pandemic: A systematic review. BMC Nurs. 2022, 21, 174. [Google Scholar] [CrossRef]
- Baboolall, D.; Berlin, G.; Fusaro, R.; Rahilly, L. Nurses and the Great Attrition; McKinsey Company: New York, NY, USA, 2022. [Google Scholar]
- Ren, H.; Li, P.; Xue, Y.; Xin, W.; Yin, X.; Li, H. Global Prevalence of Nurse Turnover Rates: A Meta—Analysis of 21 Studies from 14 Countries. J. Nurs. Manag. 2024, 2024, 5063998. [Google Scholar] [CrossRef]
- Pizzirani, B.; O’Donnell, R.; Skouteris, H.; Crump, B.; Teede, H. Clinical leadership development in Australian healthcare: A systematic review. Intern. Med. J. 2020, 50, 1451–1456. [Google Scholar] [CrossRef] [PubMed]
- Jeyaraman, M.M.; Qadar, S.M.Z.; Wierzbowski, A.; Farshidfar, F.; Lys, J.; Dickson, G.; Grimes, K.; Phillips, L.A.; Mitchell, J.I.; Van Aerde, J. Return on investment in healthcare leadership development programs. Leadersh. Health Serv. 2018, 31, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Lal, M.M.; Pabico, C.G. Magnet® and pathway: Partners for nursing excellence. JONA J. Nurs. Adm. 2021, 51, 175–176. [Google Scholar] [CrossRef]
- Iqbal, K.; Fatima, T.; Naveed, M. The impact of transformational leadership on nurses’ organizational commitment: A multiple mediation model. Eur. J. Investig. Health Psychol. Educ. 2019, 10, 262–275. [Google Scholar] [CrossRef]
- Tasmanian Health Service. Excellence in Practice Progams: Governance Framework; Tasmanian Health Service: Hobart, Australia, 2025.
- Arnaert, A.; Ahmad, H.; Ponzoni, N.; Oliver, C.; Grugel-Park, A. Blending learning: The preferred choice of clinical nurse educators to provide continuing professional development. J. Nurs. Educ. Pract. 2020, 10, 58. [Google Scholar] [CrossRef]
- Frenk, J.; Chen, L.; Bhutta, Z.A.; Cohen, J.; Crisp, N.; Evans, T.; Fineberg, H.; Garcia, P.; Ke, Y.; Kelley, P. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet 2010, 376, 1923–1958. [Google Scholar] [CrossRef]
- Kirkpatrick, J.D.; Kirkpatrick, W.K. Kirkpatrick’s Four Levels of Training Evaluation; Association for Talent Development: Alexandria, VA, USA, 2016. [Google Scholar]
- Reio, T.G., Jr.; Rocco, T.S.; Smith, D.H.; Chang, E. A critique of Kirkpatrick’s evaluation model. New Horiz. Adult Educ. Hum. Resour. Dev. 2017, 29, 35–53. [Google Scholar] [CrossRef]
- Allen, L.M.; Hay, M.; Palermo, C. Evaluation in health professions education—Is measuring outcomes enough? Med. Educ. 2022, 56, 127–136. [Google Scholar] [CrossRef]
- Tasmanian Audit Office. Royal Hobart Hospital Redevelopment Project. 2019. Available online: https://www.audit.tas.gov.au/publication/royal-hobart-hospital-redevelopment-project/ (accessed on 12 September 2024).
- Zenger, J.H.; Folkman, J.R.; Edinger, S.K. Making yourself indispensable. Harv. Bus. Rev. 2011, 89, 84–90. [Google Scholar]
- Attride-Stirling, J. Thematic networks: An analytic tool for qualitative research. Qual. Res. 2001, 1, 385–405. [Google Scholar] [CrossRef]
- Paterson, K.; Henderson, A.; Burmeister, E. The impact of a leadership development programme on nurses’ self-perceived leadership capability. J. Nurs. Manag. 2015, 23, 1086–1093. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, R.; Vermunt, J.D. Professional learning, organisational change and clinical leadership development outcomes. Med. Educ. 2021, 55, 252–265. [Google Scholar] [CrossRef] [PubMed]
- Van Dam, P.J.; Griffin, P.; Reeves, N.S.; Prior, S.J.; Paton, B.; Verma, R.; Giles, A.; Kirkwood, L.; Peterson, G.M. Learning in practice: Collaboration is the way to improve health system outcomes. Healthcare 2019, 7, 90. [Google Scholar] [CrossRef] [PubMed]
- Kay, K.; Shipman, C. The confidence gap. Atlantic 2014, 14, 1–18. [Google Scholar]
- Packard, T.; Jones, L. An outcomes evaluation of a leadership development initiative. J. Manag. Dev. 2015, 34, 153–168. [Google Scholar] [CrossRef]
- Schmitt, A.; Den Hartog, D.N.; Belschak, F.D. Transformational leadership and proactive work behaviour: A moderated mediation model including work engagement and job strain. J. Occup. Organ. Psychol. 2016, 89, 588–610. [Google Scholar] [CrossRef]
- Yanow, S.K.; Good, M.F. Nonessential Research in the New Normal: The Impact of COVID-19. Am. J. Trop. Med. Hyg. 2020, 102, 1164–1165. [Google Scholar] [CrossRef]
- Falatah, R. The impact of the coronavirus disease (COVID-19) pandemic on nurses’ turnover intention: An integrative review. Nurs. Rep. 2021, 11, 787–810. [Google Scholar] [CrossRef]
- Marsden, K.M.; Robertson, I.; Porter, J. Stressors, manifestations and course of COVID-19 related distress among public sector nurses and midwives during the COVID-19 pandemic first year in Tasmania, Australia. PLoS ONE 2022, 17, e0271824. [Google Scholar] [CrossRef]
- Poon, Y.-S.R.; Lin, Y.P.; Griffiths, P.; Yong, K.K.; Seah, B.; Liaw, S.Y. A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: A systematic review with future directions. Hum. Resour. Health 2022, 20, 70. [Google Scholar] [CrossRef]
- Frich, J.C.; Brewster, A.L.; Cherlin, E.J.; Bradley, E.H. Leadership development programs for physicians: A systematic review. J. Gen. Intern. Med. 2015, 30, 656–674. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).