Abstract
Mental health symptoms are highly prevalent in university students and have been further exacerbated following the COVID-19 pandemic. The aim of this study was to examine the prospective prediction of five mental health symptoms (anxiety, depression, insomnia, suicidality, substance misuse risk) on university non-completion. Baseline data were collected between July and September 2020 following the first UK lockdown and prior to the 2020/2021 academic year. Univariate binary logistic regression analyses were performed using data from 147 participants who were due to graduate at the end of the 2020/2021 academic year. Only substance misuse risk was found to predict university non-completion, with students with a higher risk of substance misuse more likely to not complete their university course. There appears to be an association between substance misuse risk and university non-completion; however, this was attenuated once study characteristic covariates (study level, changes in study hours and study engagement) were included, indicating possible associations between these variables. Future research should further consider the role of substance use in this population and the relationship with study characteristics, engagement and university completion.
1. Introduction
1.1. Prevalence of Mental Health Symptoms in University Students
Symptoms of poor mental health are highly prevalent amongst university students [1,2] and have been found to have worsened since the onset of the COVID-19 pandemic [3,4,5]. An increase in the symptoms of anxiety and depression has been found in university students following the COVID-19 pandemic, with as many as over 50% found to score above the clinical cut-off for anxiety and depression [6,7,8,9]. Insomnia symptoms also appear to be on the rise, with sleep problems reported to be increasing from 22.6% (2010) to 30.5% (2018) amongst a sample of university students [10]. The COVID-19 pandemic appears to have further exacerbated sleep problems in university students, with a systematic review examining sleep disturbances during the pandemic finding a 41.2% prevalence rate, compared to 36.7% in the general population [11]. However, it is worth noting that some parameters of sleep have improved since the onset of the pandemic, with an increase in total sleep time and improvement in the regularity of sleep timing observed in university students [12].
Of high concern is the increase in suicidal thoughts observed between 2010 and 2018 [13]. Not only have 21% of students reported suicidal thoughts, but similar rates have been seen for thoughts and acts of self-harm [13]. High rates of substance use within the university student population have also been found. In a sample of university students, less than half of undergraduates reported no alcohol, tobacco or other drug use, with 31.4%, 16.3% and 6.7% reporting one, two or three substance use behaviours, respectively [14]. That said, in a sample of US college students, although 26.9% and 15.1% of participants reported an increase in alcohol consumption and cannabis use, respectively, 34.4% and 25.9% reported a decrease in use following the onset of the COVID-19 pandemic [15].
1.2. Associations between Mental Health Symptoms and Academic Performance
Academic performance is most often explored in the context of academic achievement, defined through grades or grade point average (GPA) scores obtained by individuals during their studies [16]. Mental health symptoms have been associated with lower academic functioning in students [1], with higher symptoms of anxiety and depression associated with poorer academic performance [17], lower grades at university [2] and an increased likelihood of dropping a course at university [18]. Students with positive screens for anxiety and depression, using the GAD-7 and PHQ-9, have been found to be twice as likely to experience academic dissatisfaction than those with no positive screens [19]. Insomnia, disturbed sleep and more variable sleep quantity have also been associated with poorer academic outcomes, such as delayed study progress, poorer GPA scores and an increased risk of failed examinations or dropping a course [20,21,22,23]. Likewise, longer sleep duration, better sleep quality and more consistent sleep has been associated with greater academic performance [24]. Some evidence for associations between substance use and academic performance has also been found. Cigarette use, binge drinking, marijuana use and prescription and other drug use has been associated with lower self-reported GPA, and cigarette use has also been associated with an increased probability of dropping a course [21]. That said, students with poorer academic outcomes do not always report low wellbeing [25], and no significant effect of anxiety and depression symptoms on end of semester grades [18], as well as no significant differences in sleep quality between those with low and high grades [26], have been found.
1.3. Rationale and Research Aim
Previous research highlights inconsistencies in the associations between mental health symptoms and the academic performance of university students, with different methodologies, measures and student subpopulations used. Previous studies have used self-reported grades [17,18,22,26], which introduces the possibility of response bias; therefore, focusing on the non-completion of a university course provides a more objective outcome. The further examination of a number of mental health symptoms simultaneously, which are highly prevalent in the population and increasing following the onset of the COVID-19 pandemic, will provide a more comprehensive and objective picture regarding which may be potential risk factors of not completing a university course.
Thus, the aim of this study was to evaluate the association of a number of mental health symptoms with the academic outcomes of a sample of UK university students, adjusting for study characteristics and changes in circumstances as a result of the COVID-19 pandemic. The potential risk factors of students not completing their university course were investigated.
2. Materials and Methods
2.1. Study Design
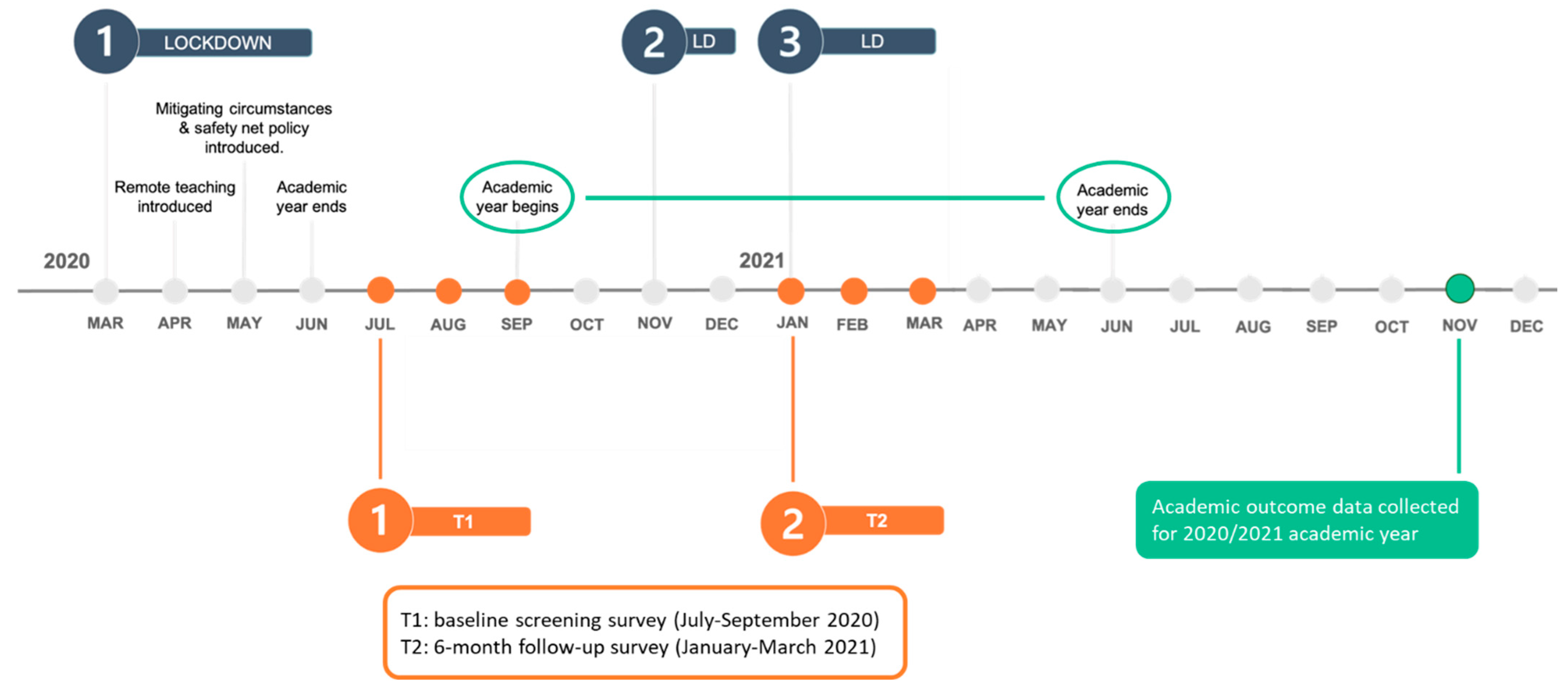
This study is part of a larger study (RECOVERS study) examining the impact of the COVID-19 pandemic on student wellbeing. The study comprised two online surveys (a baseline screening survey and a 6-month follow-up survey), which examined the prevalence and risk factors of five mental health symptoms, both cross-sectionally and longitudinally, during the COVID-19 pandemic. See Tang et al. (2022) for further details [9].
All procedures involving human subjects were approved by the Humanities and Social Sciences Research Ethics Committee of the University of Warwick, UK. All participants provided informed consent prior to starting the online survey. Only the cross-sectional component, which included an online survey completed by UK university students and young adults not at university was used in this study. For this study, only participants from a single university in the UK were included. The university is a public, campus-based university in the West Midlands of England, and one of the UK’s Russell Group universities. The academic outcome data of these participants, who gave consent for this to be accessed by the research team, were obtained from the university’s student records department.
The relationship between mental health symptoms and academic outcomes was then examined using the baseline screening survey data of the RECOVERS study. The baseline screening survey was open for participation between July and September 2020, which was just after the first UK lockdown and the final university term of the academic year. During this period, restrictions were easing, and the UK was returning to some level of ‘normality’. The academic data were collected in November 2021 for the 2020/2021 academic year. Over this academic year, universities were greatly impacted by lockdowns, ongoing changes in restrictions and how courses were delivered. Figure 1 provides further details on the study design and data collection time points.
Figure 1.
Timeline of the RECOVERS study and key moments of the COVID-19 pandemic during the university’s 2020/2021 academic year.
2.2. Participants
Participants recruited from a single university in the UK were recruited via convenience sampling. The study was advertised through university channels. A prize draw of four GBP 100 Amazon vouchers was introduced as an incentive to participate in the study in August 2020. The eligibility criteria were to be a current student enrolled at the university and at least 18 years old. For this study, participants who completed the baseline screening survey of the RECOVERS study were asked at the end of the survey if they gave permission for the research team to link their data to student records. Out of 716 participants who started the survey, 296 gave permission. From these participants, academic outcome data was available from student records for 150 of the participants who were due to graduate in the 2020/2021 academic year. Due to a lack of between-year progression data available from student records, participants who were not due to graduate were not included. This study, therefore, focused specifically on comparing participants who successfully completed their course and those who were identified as withdrawing, obtaining an extension or re-sitting their course.
Of the 150 participants whose academic data were available, 134 completed their university studies with 13 participants not completing their university studies due to either an extension, resitting or withdrawing from their course. A further three participants were unsuitable for analysis due to their status at the time the academic data was obtained (e.g., identified as completed studies but had returned to their own institution following a secondment). The mean age of participants was 23.97 (SD = 7.630). The majority of participants were female (66.0%) and of White/Caucasian ethnicity (58.9%).
2.3. Measures
2.3.1. Outcome Variable
Academic outcome data consisted of participants’ study status at the time of obtaining the data from student records (November 2021), and if applicable, final grade, i.e., first class. Participants’ data were categorised into whether they had completed their course and had been awarded their final grade or had not completed their course and were identified as having withdrawn, were currently within an extension period or were re-sitting. Data were coded as ‘have completed course’ (0) or ‘have not completed course’ (1).
2.3.2. Predictor Variables
The GAD-7 (General Anxiety Disorder Questionnaire) was used to assess for the presence of anxiety in the previous two weeks. Ratings range from ‘not at all’ (0) to ‘nearly every day’ (3). Example statements include ‘Feeling nervous, anxious or on edge’ and ‘Being so restless that it is hard to sit still’. Possible scores range from 0 to 21 with the following categories: none (0–4), mild (5–9), moderate (10–14) and severe (15–21) [27]. The Cronbach alpha coefficient was observed to be α = 0.904, indicative of high internal consistency (α ≥ 0.8) [28].
The PHQ-9 (Patient Health Questionnaire) was used to assess for the presence of depression in the previous two weeks. Ratings range from ‘not at all’ (0) to ‘nearly every day’ (3). Example statements include ‘Little interest or pleasure in doing things’ and ‘Feeling bad about yourself—or that you are a failure or have let yourself or your family down’. Possible scores range from 0 to 27 with the following categories: none (0–4), mild (5–9), moderate (10–14), moderately severe (15–19) and severe (20–27) [29]. The Cronbach alpha coefficient was observed to be α = 0.844, indicative of high internal consistency (α ≥ 0.8) [28].
The ISI-3 (Insomnia Severity Index) was used to assess participants’ presence and severity of insomnia symptoms. An example question is ‘How worried/distressed are you about your current sleep problem?’. Higher scores indicate greater difficulties. Possible scores range from 0 to 12. A total score of 7 to 12 indicates clinical insomnia [30]. The Cronbach alpha coefficient was observed to be α = 0.770, indicative of satisfactory internal consistency (α ≥ 0.7) [28].
The Suicide Behaviours Questionnaire-Revised (SBQ-R) includes four questions to assess the different dimensions of suicidality: lifetime suicide ideation/attempt, frequency of suicide ideation/attempt, threat of suicide attempt, and future suicidal behaviour. An example question is ‘Have you ever thought about or attempted to kill yourself?’. The total score ranges from 3 to 18, and a cut-off score of ≥7 is recommended for use in non-clinical samples [31]. The Cronbach alpha coefficient was observed to be α = 0.788, indicative of satisfactory internal consistency (α ≥ 0.7) [28].
The National Institute of Drug Abuse Alcohol Smoking Substance Involvement Screening Test (NIDA-ASSIST) was used to assess participants’ substance misuse risk. Seven Likert scale questions assess the frequency and impact of the use of four substances: alcohol, tobacco, prescription medication (for non-medical reasons, i.e., for reasons or in doses other than prescribed) and other substances. An example question is ‘In the past 3 months, how often have you had a strong desire or urge to use substances?’, with possible response options ranging from ‘Never’ to ‘Daily or almost daily’. Each question is weighted differently depending on the severity of the risk examined by the item: for example, the item asking participants ‘how often have you failed to do what was normally expected of you because of your use of (first drug, second drug, etc.)’ is weighted more heavily than the question ‘In the past three months, how often have you used the substances you mentioned (first drug, second drug, etc.)?’. The average total score for all substances is used to evaluate risk: low risk (0–3.49), moderate risk (3.5–26.49) and high risk (26.5–39) [32]. The Cronbach alpha coefficient was observed to be α = 0.704, indicative of satisfactory internal consistency (α ≥ 0.7) [28].
2.3.3. Covariates
Covariates included in the analyses were related to participants’ study characteristics and changes since the COVID-19 pandemic. These included study level (undergraduate or postgraduate), changes in hours of study (increased, decreased, stayed the same), changes in engagement with studies (better, worse, stayed the same) and financial changes (better, worse, stayed the same).
2.4. Data Analysis
All statistical analyses were performed using JASP (version 0.16.3) [33] with the exception of the weighted analyses which were performed on SPSS (version 27) [34].
Stabilised inverse probability scores were applied as weighted analyses [35,36]. The propensity score referred to the conditional probability of being a completer of the baseline screening survey and was calculated using three key demographic variables (age, gender and ethnicity) of all participants who started the survey. The inverse of the propensity score was then multiplied by the marginal probability of being a survey completer, which resulted in a stabilised inverse probability weight (SIPW). This weighting preserves the sample size whilst helping to balance potential biases, addressing the representativeness of the demographics of the sample, as a result of drop-out from the baseline screening survey.
Using the baseline screening survey, the characteristics of participants, including demographics, study characteristics and changes since the COVID-19 pandemic and mental health symptoms, were reported first using either mean and standard deviation or number and percentage.
Univariate binary logistic regression analyses were then performed using the baseline screening survey data. Due to the small sample size of the mental health predictors, separate logistic regression models were deemed to be more appropriate rather than running one regression analysis with several predictors.
For Model 1, one mental health predictor variable was included in each analysis (anxiety, depression, insomnia, suicidality, substance misuse risk). The outcome variable was whether participants had or had not completed their university course.
Model 2 then consisted of the mental health predictor variable with study characteristics and changes since the COVID-19 pandemic included as covariates. These were added in a separate block after the mental health predictor variable to examine any changes. As there were no significant changes after the application of weighted analyses, unweighted results were reported in the text with both unweighted and weighted beta estimates reported in the corresponding Table.
3. Results
3.1. Baseline Characteristics
One hundred and forty-seven participants were included in the analyses. The majority of participants were undergraduate students (65.3%) and were enrolled on a course full time (95.2%). The most common courses participants were enrolled on were Psychology (14.3%), Life Sciences (12.2%) and Statistics (8.2%). Most participants reported a decrease in study hours (50.3%), worse study engagement (58.5%) and worse financial status (35.9%) since the onset of the COVID-19 pandemic. As a group, participants were identified as experiencing mild levels of anxiety (M = 8.54, SD = 5.767) and depression (M = 8.34, SD = 5.686), not experiencing clinically significant insomnia symptoms (M = 3.93, SD = 3.638), not experiencing significant suicidality behaviours (M = 5.59, SD = 3.101), and were identified as low risk for substance misuse (M = 2.28, SD = 2.552).
Focusing on clinical symptoms, 17% were identified as experiencing severe levels of anxiety, with 15.7% experiencing between moderately severe and severe levels of depression. Additionally, 27.9% were experiencing clinical insomnia levels, with 26.5% at a higher risk of suicidality. There were no participants identified as being at high risk of substance misuse and 22.6% were identified as at moderate risk of substance misuse. See Table 1 for further details.

Table 1.
Participant characteristics at baseline.
3.2. Predictors of University Course Non-Completion
3.2.1. Anxiety
The chi-square tests for model comparisons did not show a significant improvement of a model in which anxiety was the only predictor (Model 1), χ2 (1) = 0.642, p = 0.423, Nagelkerke R2 = 0.010, compared to the intercept. When study characteristics and changes following COVID-19 were added as covariates (Model 2), there was a significant improvement in the model (χ2 (5) = 17.877, p = 0.003, Nagelkerke R2 = 0.254), with study level, study hours and study engagement identified as significant predictors. Postgraduates and participants identifying no change or a decrease in study hours and better study engagement since the pandemic were more likely to not complete their course (see Table 2).

Table 2.
Univariate logistic regression models examining predictors of university course non-completion.
3.2.2. Depression
The chi-square tests for model comparisons did not show a significant improvement of a model in which depression was the only predictor (Model 1), χ2 (1) = 2.032, p = 0.154, Nagelkerke R2 = 0.031, compared to the intercept. When study characteristics and changes following COVID-19 were added as covariates (Model 2), there was a significant improvement in the model (χ2 (5) = 19.876, p = 0.001, Nagelkerke R2 = 0.281), with study level, study hours and study engagement identified as significant predictors. Postgraduates and participants identifying no change or a decrease in study hours and better study engagement since the pandemic were more likely to not complete their course (see Table 2).
3.2.3. Insomnia
The chi-square tests for model comparisons did not show a significant improvement of a model in which insomnia was the only predictor (Model 1), χ2 (1) = 2.766, p = 0.096, Nagelkerke R2 = 0.041, compared to the intercept. When study characteristics and changes following COVID-19 were added as covariates (Model 2), there was a significant improvement in the model (χ2 (5) = 19.763, p = 0.001, Nagelkerke R2 = 0.280), with study level, study hours and study engagement identified as significant predictors. Postgraduates and participants identifying no change or a decrease in study hours and better study engagement since the pandemic were more likely to not complete their course (see Table 2).
3.2.4. Suicidality
The chi-square tests for model comparisons did not show a significant improvement of a model in which suicidality was the only predictor (Model 1), χ2 (1) = 1.033, p = 0.310, Nagelkerke R2 = 0.016, compared to the intercept. When study characteristics and changes following COVID-19 were added as covariates (Model 2), there was a significant improvement in the model (χ2 (5) = 18.717, p = 0.002, Nagelkerke R2 = 0.266), with study level, study hours and study engagement identified as significant predictors. Postgraduates and participants identifying no change or a decrease in study hours and better study engagement since the pandemic were more likely to not complete their course (see Table 2).
3.2.5. Substance Misuse Risk
The chi-square tests for model comparisons showed a significant improvement of a model in which substance misuse risk was the only predictor (Model 1) χ2 (1) = 4.224, p = 0.040, Nagelkerke R2 = 0.063, compared to the intercept. When study characteristics and changes following COVID-19 were added as covariates (Model 2), there was a further improvement in the model (χ2 (5) = 19.529, p = 0.002, Nagelkerke R2 = 0.277), with study level, study hours and study engagement identified as significant predictors. Postgraduates and participants identifying no change or a decrease in study hours and better study engagement since the pandemic were more likely to not complete their course. Substance misuse risk was, however, no longer a significant predictor in the full model (see Table 2).
3.2.6. Covariates
When study characteristics and changes following COVID-19 were added as covariates for each mental health predictor variable (Model 2), there was a significant improvement in each model, with study level and changes in study hours and study engagement identified as significant predictors. Postgraduates were more likely to not complete their university course compared to undergraduates. Students who identified no change or a decrease in study hours and better engagement with their studies since the pandemic were also more likely to not complete their university course.
When weighted analyses were performed for each mental health predictor, to account for potential attrition biases in participants demographics, there were no significant changes observed in the models. For each covariate identified as significant, only changes in study hours lost significance for the substance misuse risk variable once weighting was applied. There were no other significant changes observed (see Table 2).
4. Discussion
4.1. Summary of Findings
This study examined the prospective prediction of five mental health symptoms on university non-completion two years since the start of the COVID-19 pandemic. Only substance misuse risk was identified as a significant predictor of university non-completion, with students at a greater risk of substance misuse more likely to not complete their university course. Caution should be considered as the mean scores of substance misuse risk for both course completers and non-completers were found to be low. Although non-completers were categorised as ‘moderate risk’ compared to ‘low risk’ for course completers, the mean score of 3.8 is only just within the moderate range (3.5–26.49). This finding, however, supports previous studies where the associations between the use of substances and academic performance were seen [21].
Previous research has identified that when looking at alcohol use specifically, this was found to increase amongst university students following the start of the COVID-19 pandemic [37,38]. An increase in mood disorder symptoms was also found [38], with those experiencing higher symptoms of anxiety and depression, reporting larger increases in alcohol consumption [37]. As this study examined overall substance misuse risk, comprising alcohol, tobacco, prescription medication (for use other than prescribed) and other substances, it is unclear from this study which specific substances may be more significant risk factors of university students not completing their course. The further examination of specific substances used in the university student population could help identify the potential associations with academic outcomes and mental health symptoms.
The covariates of postgraduate students, no change or a decrease in study hours, and better engagement with studies since the onset of the COVID-19 pandemic, were associated with university non-completion. These findings suggest that changes in circumstances related to university studies following the pandemic as well as higher risk of substance misuse during this time may have more of an impact on university non-completion than mental health symptoms experienced. Substance misuse has been found to be used as a coping strategy when experiencing high stress [39], and previous research has highlighted that students who dropped out of their degree during their first year were less resilient, with lower perseverance, response to frustration, doubts regarding their capabilities and perceived lack of control identified [40]. Although the reasons students may be at risk of substance misuse in this study is unknown, further exploration could help identify why some students misuse substances, which substances pose the highest risk, the role they play in academic outcomes and the associations with coping, resiliency and wellbeing.
Anxiety, depression, insomnia and suicidality were not identified as predictors of university non-completion. Although students who did not complete their course displayed a higher severity of symptoms, these were not significantly higher than university completers and were within the mild or non-clinical range, which may partially explain the lack of significance observed. The findings support some previous studies where no significant effect of anxiety, depression or insomnia symptoms on academic outcomes were found [18,26], where the mean scores of anxiety and depression were also found to be below the cut-off for clinical symptoms. However, in general, associations between anxiety, depression and insomnia and academic performance were seen [2,17,20,21,22]. These studies often examined the academic outcomes of participants categorising both those with and without clinical symptoms, which may partially explain the significance found in these studies. These mixed findings warrant further exploration to understand whether there are specific aspects of anxiety, depression and insomnia, or possible mediating factors that may contribute to the academic outcomes of students. Scores on mental health outcomes do not consider impaired functioning as a result of experiencing symptoms and so focusing on students’ functioning and impairment would be worth exploring. This would allow identification of the consequences of experiencing high mental health symptoms and explore how to improve functioning and impairment in daily life.
Postgraduate students were identified as being at a higher risk of university non-completion compared to undergraduates. Previously, when examining a large sample of students cross-sectionally, being a younger age was found to be a predictor of more severe mental health symptoms [9]. These students may have found the changes and stressors associated with the pandemic more challenging than older students. Yet, previous research has also found higher levels of psychological distress in postgraduate researchers compared to undergraduate students, with 70% of postgraduate researchers experiencing symptoms of mild to severe psychological distress [41]. Findings of this study highlight being a postgraduate student, where the mean age is higher on average, is associated with university non-completion. The sense of isolation might be stronger in postgraduate students as a result of their course structure, and study characteristics common to postgraduate students, such as the reduced structure yet higher demands of a postgraduate degree and managing an appropriate work–life balance [42], may have a role to play in the relationship between mental health and university course completion.
A decrease or no change in study hours and better engagement with studies since the COVID-19 pandemic were also identified as risk factors for non-completion. Study engagement is a multi-faceted construct and three main components of engagement, namely behavioural, cognitive and emotional, have previously been identified [43]. Previous studies have found that, following transitions to online learning due to the COVID-19 pandemic, decreases in behavioural (e.g., participation in learning) and, to a larger extent, emotional engagement (e.g., attitudes towards the course), were seen [44,45]. Students’ interpretations of what ‘better’ engagement means in the context of this study is unknown. For example, if students identified engagement parameters such as increased flexibility and low intensity as ‘better’, yet have experienced a decrease in emotional engagement, these may pose an increased risk to study outcomes and non-completion. The COVID-19 pandemic appears to have had a significant impact on universities, and the changes in learning and study habits, and uncertainties surrounding these, have been significantly disruptive for students.
4.2. Limitations of the Study
There were some limitations of this study. First, only self-reported measures were included, which could introduce bias into the reporting of symptoms; however, due to the COVID-19 pandemic, the use of other measures was not possible. Furthermore, well-validated questionnaires were used to measure mental health symptoms. Future studies could incorporate additional objective measures, e.g., sleep parameters, to increase the validity of the findings.
Second, although the study was not cross-sectional, causality cannot be inferred as there are additional factors between the two timepoints that could have an influence on the course completion outcome. Changes in mental health symptoms and other characteristics over time were not explored in this study due to sample size considerations, a challenge experienced due to the pandemic. A longitudinal study examining changes in a number of factors over multiple timepoints could provide a more thorough view of potential risk factors that could lead to changes in academic performance and an increased risk of university non-completion and allow for analyses to examine possible mediators between mental health and university non-completion.
Given the attrition in the survey, both unweighted and weighted analyses were performed. The weighting should help to address the potential attrition biases of key demographics in the baseline screening survey, but not all aspects. The findings may therefore not be generalisable to the wider student population or representative of students from other university types or cultures. Although the sample size was relatively small and some caution should be considered in the interpretation of the findings, simulation studies have been performed to examine the recommendation of a minimum of 10 outcome events per predictor variable (EPV) for regressions. In this study, a sample size of 10 would have been considered appropriate for the univariate regression models (Model 1) with a single predictor variable, which was achieved. In Model 2, once study characteristic covariates were added, a minimum sample size of 50 would have been considered sufficient, which was not achieved, indicating that these results should be interpreted with caution. However, simulations do not appear to show substantial evidence for the 10 or more EPV rule, and the results of studies with 5–9 EPV were comparable to those with 10-16 EPV and should not be discounted [46]. Other factors have been found to be more influential than EPV, and it has been suggested that further research is conducted to provide guidance on sample size for logistic regression [46,47].
It is also worth noting that the majority of students finish their degree, with only a small percentage not completing their course and so the disparity between the two groups in this study is not unexpected. That said, it would be beneficial for future studies with a larger sample size to utilise a full model, including all predictors, to account for the limitations and potential bias observed when performing separate analyses and a small sample size. Despite the limitations discussed, this study provides evidence for which mental health symptoms, alongside study characteristics, may be potential risk factors of a student not completing their university course.
4.3. Implications for Future Research
Substance misuse risk appears to be a predictor of university non-completion. However, this study identifies substance misuse as a broad factor combining use of alcohol, nicotine, prescription medication (for reasons other than prescribed) and other substances. The specific mechanisms and reasons behind students’ risk of substance misuse, e.g., as a coping strategy, remains unclear. The association found can allow for further consideration of the role of substance misuse and how this might translate into study characteristics, study engagement and subsequent university course completion. The lack of statistical significance for other mental health symptoms is surprising and warrants further investigation alongside substance misuse risk. The exploration of factors associated with mental health symptoms and study characteristics, may help us to identify the largest contributors of course non-completion.
Postgraduate students appear to be at a greater risk of university non-completion compared to undergraduate students; however, the specific reasons for this remains unknown. Future studies could gather the information from postgraduate students about their experiences both related to their studies and to their wellbeing. Identifying why these students are at greater risk may help universities provide facilities to support postgraduate students during their time at university. Another surprising observation was that better engagement in studies since the onset of the COVID-19 pandemic was found to be a predictor of university course non-completion. Future studies could make use of standardised ‘work engagement’ measures to further explore the impacts of study characteristics on university course completion.
5. Conclusions
There appears to be an association between general substance misuse risk and university course non-completion. This was attenuated once study characteristics were accounted for, indicating possible associations between these variables. Postgraduate students and changes in studies following the pandemic appear to be consistent predictors of non-completion. Future research could further consider the role of substance misuse in this population, and the associations with study characteristics, study engagement and university course completion. Findings could help implement tailored services in university settings to support both the academic success and wellbeing of university students, especially in times of significant disruption to studies and university life, as has been observed during the COVID-19 pandemic.
Author Contributions
Conceptualisation, methodology, formal analysis, L.C. and N.K.Y.T.; data curation, L.C. and K.A.M.M.; writing—original draft preparation, L.C.; writing—review and editing, L.C., K.A.M.M., C.T., S.P.S., C.M. and N.K.Y.T. All authors have read and agreed to the published version of the manuscript.
Funding
L.C.’s PhD studentship is funded by the Engineering and Physical Sciences Research Council (EPSRC). S.P.S. is part-funded by the National Institute for Health Research (NIHR) Applied Research Collaboration West Midlands. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The Warwick RECOVERS study was funded by a University of Warwick Pro-Vice Chancellor (Research) COVID-19 Research Programme Award and supported by the Warwick Health Global Research Priorities.
Institutional Review Board Statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects were approved by the Humanities and Social Sciences Research Ethics Committee of the University of Warwick (HSSREC 173/19-20, on 11 June 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, L.C. The data are not publicly available owing to ethical restrictions, e.g., containing information that could compromise the privacy of research participants.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Bruffaerts, R.; Mortier, P.; Kiekens, G.; Auerbach, R.P.; Cuijpers, P.; Demyttenaere, K.; Green, J.G.; Nock, M.K.; Kessler, R.C. Mental Health Problems in College Freshmen: Prevalence and Academic Functioning. J. Affect. Disord. 2018, 225, 97–103. [Google Scholar] [CrossRef]
- Duffy, A.; Keown-Stoneman, C.; Goodday, S.; Horrocks, J.; Lowe, M.; King, N.; Pickett, W.; McNevin, S.H.; Cunningham, S.; Rivera, D.; et al. Predictors of Mental Health and Academic Outcomes in First-Year University Students: Identifying Prevention and Early-Intervention Targets. BJPsych Open 2020, 6, e46. [Google Scholar] [CrossRef]
- Liyanage, S.; Saqib, K.; Khan, A.F.; Thobani, T.R.; Tang, W.C.; Chiarot, C.B.; Alshurman, B.A.; Butt, Z.A. Prevalence of Anxiety in University Students during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 62. [Google Scholar] [CrossRef]
- Ochnik, D.; Rogowska, A.M.; Kuśnierz, C.; Jakubiak, M.; Schütz, A.; Held, M.J.; Arzenšek, A.; Benatov, J.; Berger, R.; Korchagina, E.V.; et al. Mental Health Prevalence and Predictors among University Students in Nine Countries during the COVID-19 Pandemic: A Cross-National Study. Sci. Rep. 2021, 11, 18644. [Google Scholar] [CrossRef]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Drakos, A.; Zuo, Q.K.; Huang, E. The Prevalence of Depressive Symptoms, Anxiety Symptoms and Sleep Disturbance in Higher Education Students during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Psychiatry Res. 2021, 301, 113863. [Google Scholar] [CrossRef]
- Husky, M.M.; Kovess-Masfety, V.; Swendsen, J.D. Stress and Anxiety among University Students in France during COVID-19 Mandatory Confinement. Compr. Psychiatry 2020, 102, 152191. [Google Scholar] [CrossRef]
- Evans, S.; Alkan, E.; Bhangoo, J.K.; Tenenbaum, H.; Ng-Knight, T. Effects of the COVID-19 Lockdown on Mental Health, Wellbeing, Sleep, and Alcohol Use in a UK Student Sample. Psychiatry Res. 2021, 298, 113819. [Google Scholar] [CrossRef]
- Chen, T.; Lucock, M. The Mental Health of University Students during the COVID-19 Pandemic: An Online Survey in the UK. PLoS ONE 2022, 17, e0262562. [Google Scholar] [CrossRef]
- Tang, N.K.Y.; McEnery, K.A.M.; Chandler, L.; Toro, C.; Walasek, L.; Friend, H.; Gu, S.; Singh, S.P.; Meyer, C. Pandemic and Student Mental Health: Mental Health Symptoms among University Students and Young Adults after the First Cycle of Lockdown in the UK. BJPsych Open 2022, 8, e138. [Google Scholar] [CrossRef]
- Sivertsen, B.; Vedaa, Ø.; Harvey, A.G.; Glozier, N.; Pallesen, S.; Aarø, L.E.; Lønning, K.J.; Hysing, M. Sleep Patterns and Insomnia in Young Adults: A National Survey of Norwegian University Students. J. Sleep Res. 2019, 28, e12790. [Google Scholar] [CrossRef]
- Jahrami, H.A.; Alhaj, O.A.; Humood, A.M.; Alenezi, A.F.; Fekih-Romdhane, F.; AlRasheed, M.M.; Saif, Z.Q.; Bragazzi, N.L.; Pandi-Perumal, S.R.; BaHammam, A.S.; et al. Sleep Disturbances during the COVID-19 Pandemic: A Systematic Review, Meta-Analysis, and Meta-Regression. Sleep Med. Rev. 2022, 62, 101591. [Google Scholar] [CrossRef]
- Wright, K.P.; Linton, S.K.; Withrow, D.; Casiraghi, L.; Lanza, S.M.; de la Iglesia, H.; Vetter, C.; Depner, C.M. Sleep in University Students Prior to and during COVID-19 Stay-at-Home Orders. Curr. Biol. 2020, 30, R797–R798. [Google Scholar] [CrossRef]
- Sivertsen, B.; Hysing, M.; Knapstad, M.; Harvey, A.G.; Reneflot, A.; Lønning, K.J.; O’Connor, R.C. Suicide Attempts and Non-Suicidal Self-Harm among University Students: Prevalence Study. BJPsych Open 2019, 5, e26. [Google Scholar] [CrossRef]
- El Ansari, W.; Salam, A. Multi-Substance Use Behaviors: Prevalence and Correlates of Alcohol, Tobacco and Other Drug (Atod) Use among University Students in Finland. Int. J. Environ. Res. Public Health 2021, 18, 6426. [Google Scholar] [CrossRef]
- Firkey, M.K.; Sheinfil, A.Z.; Woolf-King, S.E. Substance Use, Sexual Behavior, and General Well-Being of U.S. College Students during the COVID-19 Pandemic: A Brief Report. J. Am. Coll. Health 2022, 70, 2270–2275. [Google Scholar] [CrossRef]
- York, T.T.; Gibson, C.; Rankin, S. Defining and Measuring Academic Success. Pract. Assess. Res. Eval. 2015, 20, 5. [Google Scholar]
- Awadalla, S.; Davies, E.B.; Glazebrook, C. A Longitudinal Cohort Study to Explore the Relationship between Depression, Anxiety and Academic Performance among Emirati University Students. BMC Psychiatry 2020, 20, 448. [Google Scholar] [CrossRef]
- Gorman, E.L.; Burke, H.H.; Rubino, L.G.; Vargas, I.; Haeffel, G.J. Teasing Apart the Effect of Depression Specific and Anxiety Specific Symptoms on Academic Outcomes. Klin Spec Psihol (Clin. Psychol. Spec. Educ.) 2020, 9, 91–104. [Google Scholar] [CrossRef]
- Lipson, S.K.; Eisenberg, D. Mental Health and Academic Attitudes and Expectations in University Populations: Results from the Healthy Minds Study. J. Ment. Health 2018, 27, 205–213. [Google Scholar] [CrossRef]
- Hayley, A.C.; Sivertsen, B.; Hysing, M.; Vedaa, Ø.; Øverland, S. Sleep Difficulties and Academic Performance in Norwegian Higher Education Students. Br. J. Educ. Psychol. 2017, 87, 722–737. [Google Scholar] [CrossRef]
- Hartmann, M.E.; Prichard, J.R. Calculating the Contribution of Sleep Problems to Undergraduates’ Academic Success. Sleep Health 2018, 4, 463–471. [Google Scholar] [CrossRef]
- Vedaa, Ø.; Erevik, E.K.; Hysing, M.; Hayley, A.C.; Sivertsen, B. Insomnia, Sleep Duration and Academic Performance: A National Survey of Norwegian College and University Students. Sleep Med. X 2019, 1, 100005. [Google Scholar] [CrossRef]
- Bono, T.J.; Hill, P.L. Sleep Quantity and Variability during the First Semester at University: Implications for Well-Being and Academic Performance. Psychol. Health Med. 2021, 27, 931–936. [Google Scholar] [CrossRef]
- Okano, K.; Kaczmarzyk, J.R.; Dave, N.; Gabrieli, J.D.E.; Grossman, J.C. Sleep Quality, Duration, and Consistency Are Associated with Better Academic Performance in College Students. npj Sci. Learn. 2019, 4, 16. [Google Scholar] [CrossRef]
- Bücker, S.; Nuraydin, S.; Simonsmeier, B.A.; Schneider, M.; Luhmann, M. Subjective Well-Being and Academic Achievement: A Meta-Analysis. J. Res. Pers. 2018, 74, 83–94. [Google Scholar] [CrossRef]
- Jalali, R.; Khazaei, H.; Paveh, B.K.; Hayrani, Z.; Menati, L. The Effect of Sleep Quality on Students’ Academic Achievement. Adv. Med. Educ. Pract. 2020, 11, 497–502. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Nunnally, J.; Bernstein, I. Psychometric Theory, 3rd ed.; MacGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Thakral, M.; Von Korff, M.; McCurry, S.M.; Morin, C.M.; Vitiello, M.V. ISI-3: Evaluation of a Brief Screening Tool for Insomnia. Sleep Med. 2021, 82, 104–109. [Google Scholar] [CrossRef]
- Osman, A.; Bagge, C.; Gutierrez, P.; Konick, L.; Kooper, B.; Barrios, F. The Suicidal Behaviors Questionnaire- Revised (SBQ-R): Validation with Clinical and Nonclinical Samples. Assessment 2001, 8, 443–454. [Google Scholar] [CrossRef]
- National Institute for Health NIDA Quick Screen V1.0. Screening Measure. Available online: https://nida.nih.gov/sites/default/files/pdf/nmassist.pdf (accessed on 8 May 2020).
- JASP. JASP [Computer Software] 2022; Version 0.16.3; JASP: Amsterdam, The Netherlands, 2022. [Google Scholar]
- IBM Corp IBM SPSS Statistics for Windows. Version 27.0. 2020; SPSS Inc.: Chicago, IL, USA, 2020.
- Xu, S.; Ross, C.; Raebel, M.A.; Shetterly, S.; Blanchette, C.; Smith, D. Use of Stabilized Inverse Propensity Scores as Weights to Directly Estimate Relative Risk and Its Confidence Intervals. Value Health 2010, 13, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Pezzi, A.; Cavo, M.; Biggeri, A.; Zamagni, E.; Nanni, O. Inverse Probability Weighting to Estimate Causal Effect of a Singular Phase in a Multiphase Randomized Clinical Trial for Multiple Myeloma. BMC Med. Res. Methodol. 2016, 16, 150. [Google Scholar] [CrossRef] [PubMed]
- Lechner, W.V.; Laurene, K.R.; Patel, S.; Anderson, M.; Grega, C.; Kenne, D.R. Changes in Alcohol Use as a Function of Psychological Distress and Social Support Following COVID-19 Related University Closings. Addict. Behav. 2020, 110, 106527. [Google Scholar] [CrossRef]
- Charles, N.E.; Strong, S.J.; Burns, L.C.; Bullerjahn, M.R.; Serafine, K.M. Increased Mood Disorder Symptoms, Perceived Stress, and Alcohol Use among College Students during the COVID-19 Pandemic. Psychiatry Res. 2021, 296, 113706. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, M.C.; Hetrick, S.E.; Parker, A.G. The Impact of Stress on Students in Secondary School and Higher Education. Int. J. Adolesc. Youth 2020, 25, 104–112. [Google Scholar] [CrossRef]
- Ayala, J.C.; Manzano, G. Academic Performance of First-Year University Students: The Influence of Resilience and Engagement. High. Educ. Res. Dev. 2018, 37, 1321–1335. [Google Scholar] [CrossRef]
- Moss, R.A.; Gorczynski, P.; Sims-Schouten, W.; Heard-Laureote, K.; Creaton, J. Mental Health and Wellbeing of Postgraduate Researchers: Exploring the Relationship between Mental Health Literacy, Help-Seeking Behaviour, Psychological Distress, and Wellbeing. High. Educ. Res. Dev. 2022, 41, 1168–1183. [Google Scholar] [CrossRef]
- Levecque, K.; Anseel, F.; De Beuckelaer, A.; Van der Heyden, J.; Gisle, L. Work Organization and Mental Health Problems in PhD Students. Res. Policy 2017, 46, 868–879. [Google Scholar] [CrossRef]
- Fredricks, J.A.; Blumenfeld, P.C.; Paris, A.H. School Engagement: Potential of the Concept, State of the Evidence. Rev. Educ. Res. 2004, 74, 59–109. [Google Scholar] [CrossRef]
- Wester, E.R.; Walsh, L.L.; Arango-Caro, S.; Callis-Duehl, K.L. Student Engagement Declines in STEM Undergraduates during COVID-19–Driven Remote Learning. J. Microbiol. Biol. Educ. 2021, 22, 10–1128. [Google Scholar] [CrossRef]
- Daniels, L.M.; Goegan, L.D.; Parker, P.C. The Impact of COVID-19 Triggered Changes to Instruction and Assessment on University Students’ Self-Reported Motivation, Engagement and Perceptions. Soc. Psychol. Educ. 2021, 24, 299–318. [Google Scholar] [CrossRef] [PubMed]
- Vittinghoff, E.; McCulloch, C.E. Relaxing the Rule of Ten Events per Variable in Logistic and Cox Regression. Am. J. Epidemiol. 2007, 165, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Van Smeden, M.; De Groot, J.A.H.; Moons, K.G.M.; Collins, G.S.; Altman, D.G.; Eijkemans, M.J.C.; Reitsma, J.B. No Rationale for 1 Variable per 10 Events Criterion for Binary Logistic Regression Analysis. BMC Med. Res. Methodol. 2016, 16, 163. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).