Abstract
Background: Opioid analgesic therapy has been traditionally used for pain management; however, the variability in patient characteristics, complexity in evaluating pain, availability of treatment within facilities, and U.S. physicians overprescribing opioids have contributed to the current opioid epidemic. Despite large research efforts investigating the patterns of postsurgical pain management and influencing factors, it remains unclear how these overall trends vary across the varying sizes and available resources of academic hospitals, community hospitals, and outpatient surgery centers. The primary aim of this scoping review was to examine the patterns of contemporary postoperative pain management across healthcare settings, including academic medical centers, community hospitals, and outpatient surgery centers. Specifically, this study investigates how prescription practices for opioids, NSAIDs, and acetaminophen are influenced by patient demographics, including sex, race, gender, insurance status, and other social determinants of health (SDoH), to inform equitable and patient-centered pain management strategies. Methods: This study utilized The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) and was used as a reference checklist. The Arksey and O’Malley methodological framework was used to guide the review process. To ensure comprehensive coverage, searches were conducted across three major databases: PubMed, Embase, and Cochrane Library. Results: A total of 43 eligible studies were retained for analysis. The highest reported Healthy People 2030 category was Social and community context (n = 39), while the highest reported category of SDoH was age (n = 36). A total of 34 articles listed sex and age as SDoH. Additional SDoH examined were race/ethnicity (n = 17), insurance (n = 7), employment (n = 1), education (n = 4), and income (n = 1). This review suggests that there are significant gaps in the implementation of institution-specific, patient-centered, and equitable pain management strategies, particularly in academic hospitals, which our findings show have the highest rates of opioid and NSAID prescriptions (n = 26) compared to outpatient surgical centers (n = 8). Findings from our review of the literature demonstrated that while academic hospitals often adopt enhanced recovery protocols aimed at reducing opioid dependence, these protocols can fail to address the diverse needs of at-risk populations, such as those with chronic substance use, low socioeconomic status, or racial and ethnic minorities. Conclusions: Findings from this review are expected to have implications for informing both organizational-specific and nationwide policy recommendations, potentially leading to more personalized and equitable pain management strategies across different healthcare settings. These include guidelines for clinicians on addressing various aspects of postoperative pain management, including preoperative education, perioperative pain management planning, use of different pharmacological and nonpharmacological modalities, organizational policies, and transition to outpatient care.
1. Introduction
Postoperative pain management aims to reduce acute postsurgical pain for immediate relief to facilitate a smooth transition for patients when returning to normal function [1]. Inadequate pain control can lead to sensitization, increasing the risk of chronic pain, patient dissatisfaction, delayed mobilization, cardiac and pulmonary complications, and increased morbidity and mortality [1,2,3,4]. Postoperative pain management requires an individualized plan, including consideration of surgical factors, patient factors, and social determinants of health (SDoH), such as age, sex, race/ethnicity, history of chronic opioid use, income or educational status, and other comorbidities. It is dependent on subjective outcomes, like a patient’s perception of their pain severity, tolerance, and analgesic response [1,2,3,4]. Challenges can arise in specific patients, particularly those belonging to vulnerable groups, including pregnant, geriatric, neonatal, opioid-tolerant, or those with a history of substance use disorder [5]. Opioid analgesics have traditionally played a central role in postoperative pain management. However, variability in patient characteristics, the complexity of pain evaluation, and inconsistent access to treatment have contributed to widespread disparities in care. In the United States (U.S.), the overprescription of opioids has fueled the opioid epidemic, highlighting the need for a more balanced approach [1,2,3,4].
In response to rising opioid-related disorders and deaths, contemporary protocols advocate for a multimodal approach to pain relief. This strategy combines pharmacologic therapies, including opioids, NSAIDs, and acetaminophen, to target multiple pain pathways and minimize reliance on opioids [6,7,8]. Despite these risks, opioids remain a cornerstone of postoperative pain management due to their efficacy and history of use [6]. A review of inpatient records found that 80% of patients undergoing low-risk surgery were prescribed an opioid at discharge, and 80% of those prescriptions involved oxycodone or hydrocodone, which are frequently implicated in drug overdose deaths [9]. Though the opioid epidemic has changed institutional attitudes toward pain management, it is unclear the extent to which these changes have impacted practices for postoperative pain management [6]. For example, while a CDC report showed that overall opioid prescriptions peaked in 2010 and steadily decreased through to the study’s conclusion in 2015 [10], a review focused on inpatient postoperative analgesia showed that the rate of prescription of opioids remained stable over the same time period [11]. Further, there is a paucity of research describing how these practices differ across different institutions providing surgical care in the US. Given the significant risks associated with opioid prescriptions and the economic burden of opioid abuse, it is important to investigate whether initiatives aimed at reducing opioid use are being effectively implemented across various surgical care settings in the US, ensuring efficacious treatment while reducing harm.
Healthcare disparities in postoperative pain management are most evident in racial and ethnic minority groups, particularly among lower socioeconomic groups and in individuals with low levels of health literacy [12,13,14,15,16,17]. A meta-analysis of 12 studies showed that cost, socioeconomic status, insurance, and racial identity were the main influential factors affecting the timing and access to adequate care and recovery needs for orthopedic surgery patients from disadvantaged socioeconomic backgrounds [15]. Moreover, several studies highlighted in their findings that patients with private insurance received more expeditious surgical interventions compared to uninsured patients and those with public insurance [18,19,20]. Further, in the setting of acute pain, the odds of Black and Hispanic patients receiving analgesics in the emergency department were significantly lower than White patients [21,22]. In patients over 65 years old and in need of advanced rehabilitation services, White patients were 38% more likely to receive needed rehabilitation care compared to Black patients [21,22]. It was also reported that patients with income levels in the fiftieth percentile or higher were 52% more likely to receive rehabilitation compared to patients below the twenty-fifth percentile of income [21,22]. Hence, pain management care accessibility, affordability, and quality-related challenges remain, particularly when it comes to patients experiencing social determinants of health-imposed disparities. Strategies for equitable practices of postoperative pain management across healthcare settings are essential to ensure access in vulnerable population groups.
Postoperative pain management practices differ across different healthcare settings, such as academic hospitals, community hospitals, and outpatient surgical centers, due to differences in patient demographics, type and volume of procedures performed, and available resources [23]. In academic hospitals, there is a growing emphasis on the implementation of multimodal analgesia that often utilizes NSAIDs or acetaminophen to reduce dependency on opioids, driven by enhanced recovery protocols that aim for quicker patient mobilization and discharge [8]. While effective, these protocols are not widely standardized and have a large degree of heterogeneity in implementation that impacts drug prescriptions and patient outcomes [24]. Comparatively less research exists on the setting of community hospitals, which may aim for the same standards as large academic centers but may vary widely due to slower adoption and standardization of protocols and variation in resources and available training. Outpatient surgical centers have a unique challenge in pain management due to the necessity of immediate patient discharge. In this setting, the use of NSAIDs and acetaminophen is emphasized to avoid complications that could produce an unnecessary hospital admission [25]. Studies have shown that interventions such as The Standardization of Outpatient Procedure (STOP) protocol have been effective in reducing both the prescription of and utilization of opioids without impacting patient-reported average pain in the first seven days [26]. Ultimately, despite large research efforts investigating the patterns of postsurgical pain management and influencing factors, it remains unclear how these overall trends vary between the varying sizes and available resources of academic hospitals, community hospitals, and outpatient surgery centers. Additionally, very few studies have considered the role of SDoH in influencing the access and quality of postoperative pain management services received and the broader consequences this inflicts on underserved communities.
The primary aim of this scoping review is to examine the patterns of contemporary postoperative pain management across healthcare settings, including academic medical centers, community hospitals, and outpatient surgery centers. Specifically, this study investigates how prescription practices for opioids, NSAIDs, and acetaminophen are influenced by patient demographics, including sex, race, gender, insurance status, and other social determinants of health (SDoH), to inform equitable and patient-centered pain management strategies. By identifying variations in prescription patterns, this review aims to address a significant gap in understanding the intersection between healthcare settings and SDoH in postoperative care. The findings from this review are expected to have implications for informing policy recommendations and clinical practices that promote person-centered and equitable pain management strategies.
2. Methods
This study utilized The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR), which was used as a reference checklist [27]. To guide the review process, the Arksey and O’Malley methodological framework was used [28]. This framework involves five steps: (1) identifying research questions, (2) conducting the literature review, (3) choosing pertinent studies, (4) organizing the data systematically, and (5) compiling, summarizing, and presenting findings. This process ensures transparency and enhances the reliability and validity of the study.
2.1. Step 1: Identifying Research Questions
Two research questions were formulated for this study: (1) How does the rate of opioids, NSAIDs, and acetaminophen prescription for postoperative pain management vary between academic hospitals, community hospitals, and outpatient surgical centers? and (2) How are prescription patterns and postoperative pain management practices influenced by patient characteristics and social determinants of health (SDoH)?
2.2. Step 2: Conducting the Literature Review
Keywords and MeSH terms for the search strategy were developed in collaboration with a research librarian (TF), an expert in scoping review protocols. The search terms included postoperative pain management, analgesics, opioid, acetaminophen, opiates, anti-inflammatory agents, social determinants of health, sex, gender, race, ethnicity, insurance status, educational level, income level, academic medical centers, hospitals, outpatient clinics, community clinics, and university medical centers. To ensure comprehensive coverage, searches were conducted across three major databases: PubMed, Embase, and Cochrane Library. Databases were searched to identify peer-reviewed literature encompassing primary data sources, secondary data sources, and case reports. The literature review was completed over a period of one month, from January 2024 to February 2024. The article screening was carried out by the senior author (LS) and co-authors (AS, DL, SD, EM, JB, LAR, AG, SS, and AD).
2.3. Inclusion Criteria
The articles that were included were systematic reviews, meta-analyses, observational, experimental, descriptive, and case-control studies published in English between 2010 and the present. These studies specifically focused on the prescription rates of opioids, NSAIDs, and acetaminophen for postoperative pain management in a range of different settings in adults 18–75 years old. Studies included were carried out in the United States academic hospitals and/or community hospitals and/or outpatient surgical centers.
2.4. Exclusion Criteria
Excluded studies encompass case reports, clinical trials, and narrative reviews. Additionally, articles were excluded if they focused on the prescription of opioids, NSAIDs, and acetaminophen that did not pertain to postoperative pain management. Studies conducted in settings other than academic hospitals, community hospitals, or outpatient surgical centers were also not considered. Additional exclusion criteria were articles focusing on patients aged over 75 or under 18 years, articles published before 2010, studies conducted outside the United States, and non-English language articles.
2.5. Step 3: Selecting Studies Relevant to the Research Questions
All student co-authors (AS, DL, SD, EM, JB, LAR, AG, SS, and AD) extracted and summarized data from the relevant articles. The senior author (LS) reviewed all tabulated data to resolve any discrepancies. Initial categorization of data was conducted by co-authors (AS, DL, SD, EM, JB, SS, and AD) and was compared to independent categorization with reviewer pair (LAR and AG) and senior author (LS) for inter-rater reliability in a subsample of 80% (n = 34) of the studies. Inter-rater reliability was conducted in two rounds with discrepancies resolved by consensus discussion. The resulting inter-rater reliability was 90% for all data tabulated.
Summary tables included one evidence table describing study characteristics, types of SDOH, and outcomes. First, types of SDOH were listed and organized based on the five categories described by Healthy People 2030, which are Economic Stability, Education Access and Quality, Health Care Access and Quality, Neighborhood and Built Environment, and Social and Community Context [29]. The Healthy People 2030 is a set of science-based objectives with goals to observe progress and encourage and focus action [29]. Following the World Health Organization’s (WHO) call to address SDOH to preserve health and quality of life, The Healthy People 2030 first introduced SDOH objectives in 2010 [29].
Variance in rates of prescription of Opioids, NSAIDs, and Acetaminophen for postoperative pain management were reported (Table 1). Table 2 highlights the prevalence of prescription of opioids, NSAIDs, and acetaminophen for postoperative pain management across Academic Hospitals, Community Hospitals, and Outpatient surgical centers to focus on differences among these centers.

Table 1.
Study characteristics of included studies.

Table 2.
Variance in prescription rates based on SDoH and types of surgery for postoperative pain.
2.6. Steps 4 and 5: Charting the Data and Collation, Summarization, and Reporting of Results
Study characteristics were tabulated for primary author/year, study design, sample size, study population, age range, study purpose, type of SDOH, SDOH category based on HP 2030, type of postoperative pain, type of prescription, and variance in prescriptions rates based on SDOH (Table 1). Identified articles were arranged based on primary author/year, type of surgery, type of prescription, type of postoperative pain, and healthcare setting (Table 2).
3. Results
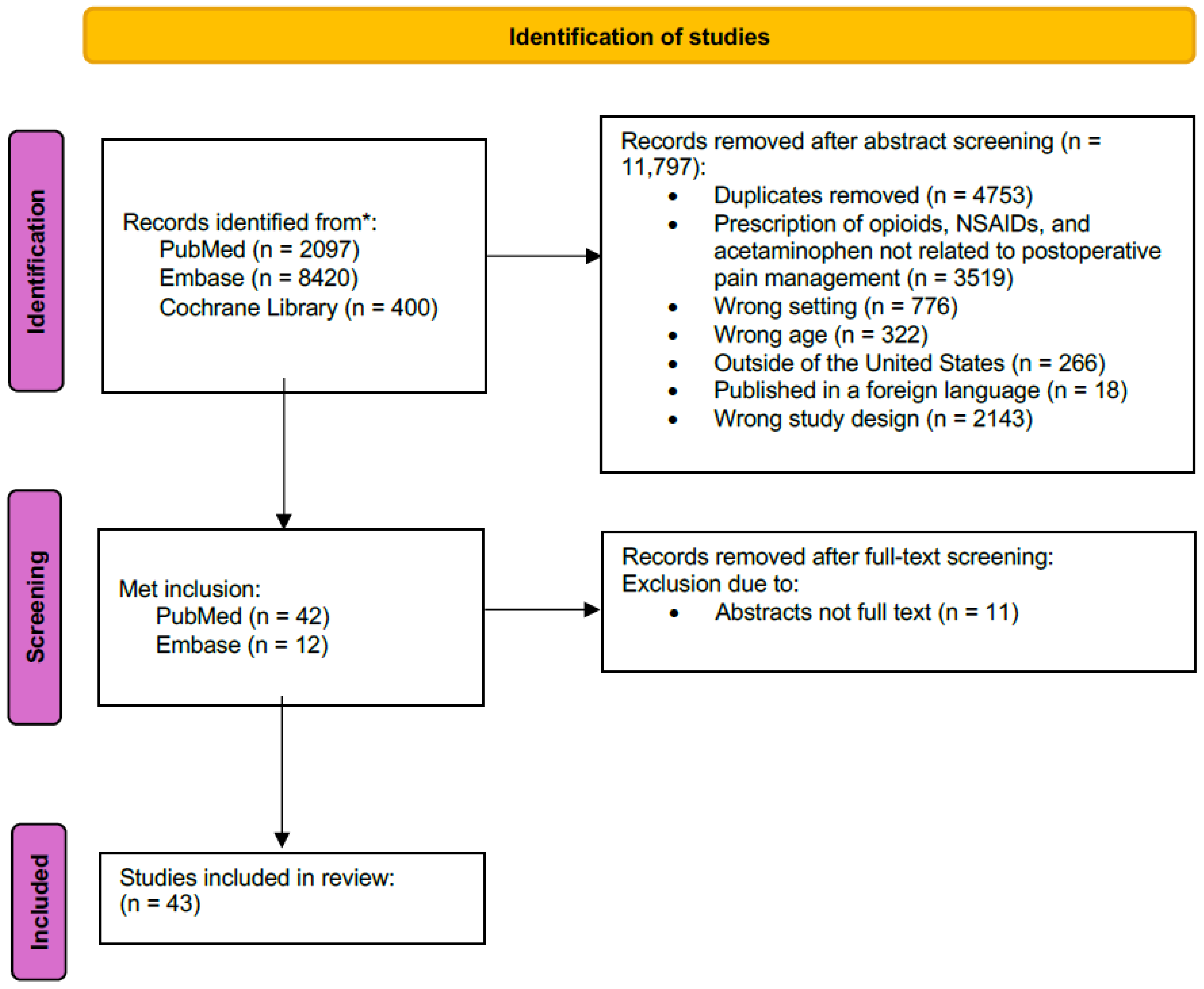
The initial study extraction generated 11,851 studies from PubMed (n = 2097), Embase (n = 8420), and Cochrane Library (n = 400). Studies were excluded if they had to do with the prescription of opioids, NSAIDs, and acetaminophen not related to postoperative pain management (n = 3519), were the wrong setting (n = 776), wrong age (n = 322), outside of the United States (n = 266), published in a foreign language (n = 18), or wrong study design (n = 2143). Duplicated studies were removed (n = 4753). A total of 54 studies met the inclusion criteria from PubMed (n = 42) and Embase (n = 12). An additional 11 studies were excluded following a full study review due to being abstracts and not full text. A total of 43 eligible studies were retained for analysis (Figure 1). The retained studies were published between 2016 and 2023. Most studies (n = 31/43, 72%) were published in the last 5 years. Study designs included retrospective cohort studies (n = 25), prospective cohort studies (n = 8), cross-sectional studies (n = 5), prospective-retrospective cohort studies (n = 2), retrospective case series (n = 1), systematic review (n = 1), and retrospective chart review (n =1). Sample size ranged from n = 58 to n = 852,111. The healthcare settings included academic hospitals (n = 26), outpatient surgical centers (n = 8), both academic medical centers and outpatient surgical facilities (n = 5), research databases (n = 2), and academic community hospitals (n = 2).
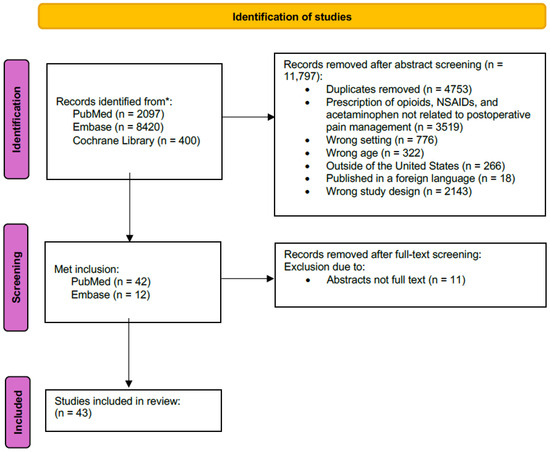
Figure 1.
PRISMA flow chart. * No tracing of references or grey literature was included in the identification process.
3.1. SDOH Explored and Classification Based on the Healthy People 2030 Categories
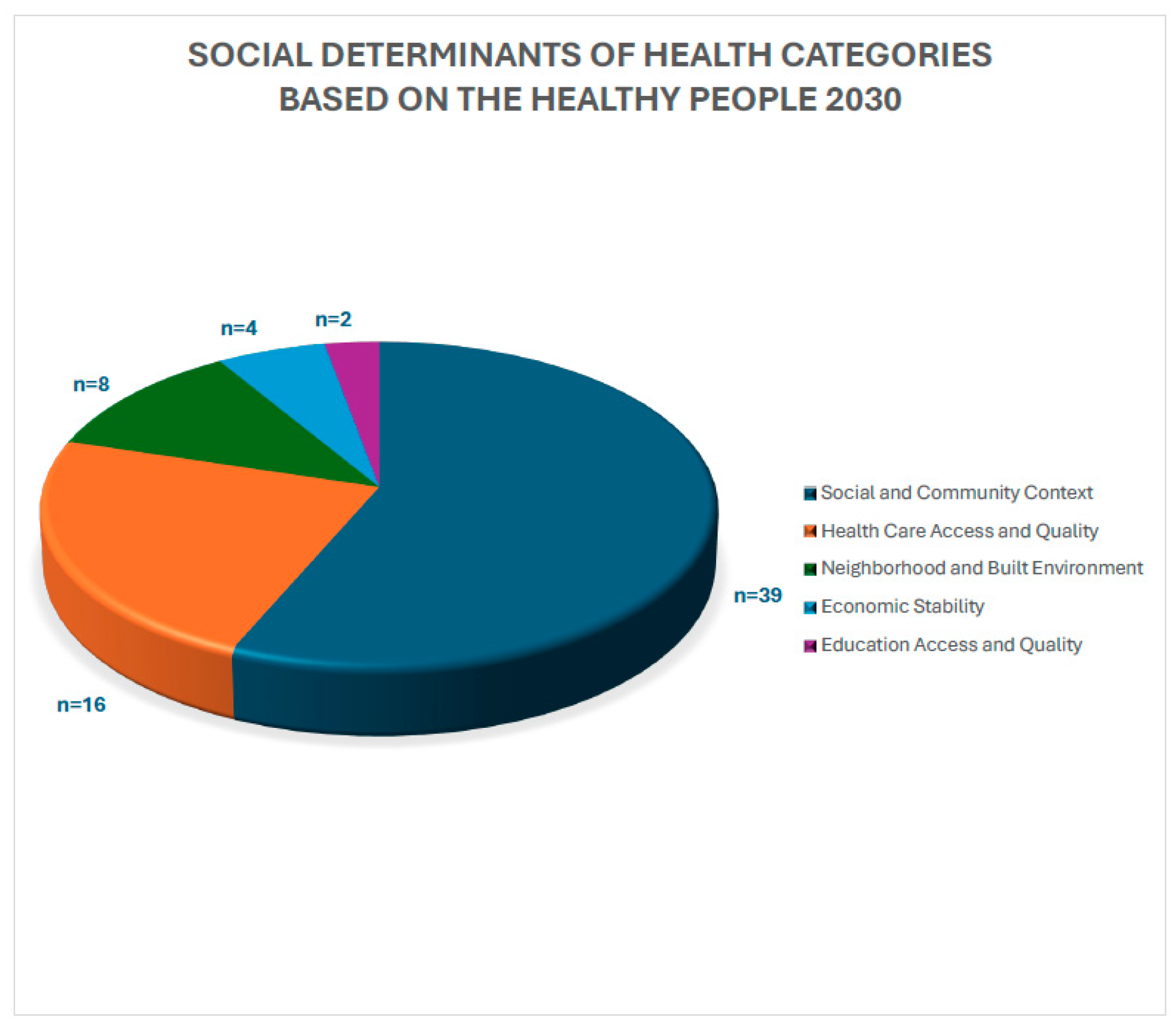
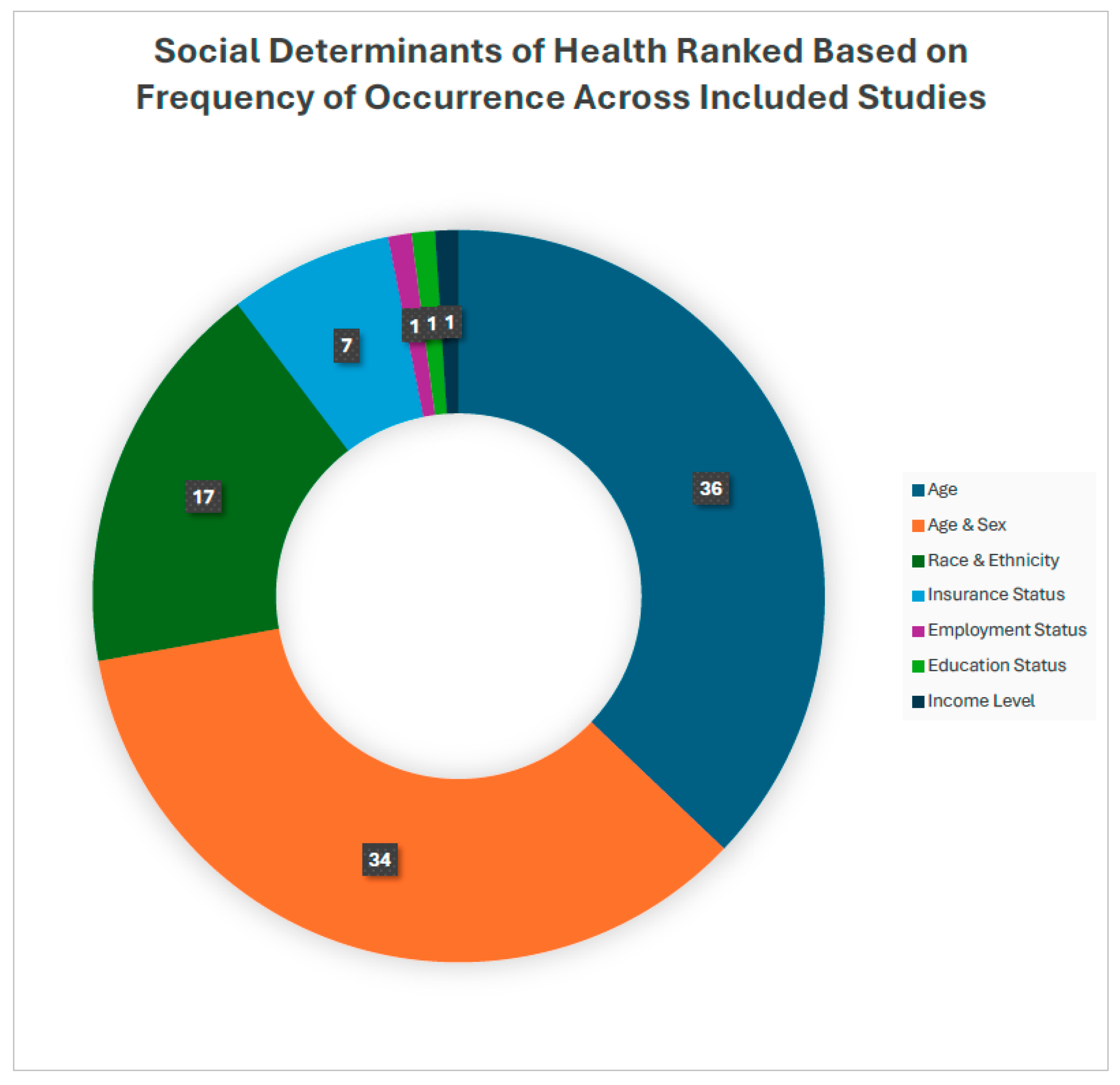
The Healthy People 2030 classification identifies public health priorities to help individuals, organizations, and communities across the United States improve health and well-being. Healthy People 2030 is the organization’s fifth version and was based on 40 years of knowledge and data. Their social determinants of health are defined by five categories: Economic stability, Education Access and Quality, Health Care Access and Quality, Neighborhood and Built Environment, and Social and Community Context. Economic stability focuses on employment programs, career counseling, and childcare opportunities to help people achieve steady employment. The education access and quality objective focuses on helping children do well in school and providing higher quality education. Healthcare access and quality focuses on improving healthcare insurance coverage rates, accessibility to primary care providers, and preventative care. The neighborhood and built environment objective seeks to help improve health and safety in the community through advocacy work at the local, state, and federal levels of government. Finally, social and community context focuses on social support by helping people find safe spaces in their communities. Based on these categories, the SDOH examined in this study were categorized based on the Health People 2030 categories. Healthy People 2030 categories reported by high to low frequency of occurrence were Social and community context (n= 39), Health care access and quality (n = 16), Neighborhood and Built Environment (n = 8), Economic Stability (n = 4), and Education Access and Quality (n = 2) (Figure 2). The highest reported category of SDoH was age (n = 36). A total of 34 articles listed sex and age as SDoH (Table 1). Additional SDoH examined were race/ethnicity (n = 17), insurance (n = 7), employment (n = 1), education (n = 4), and income (n = 1) (Figure 3).
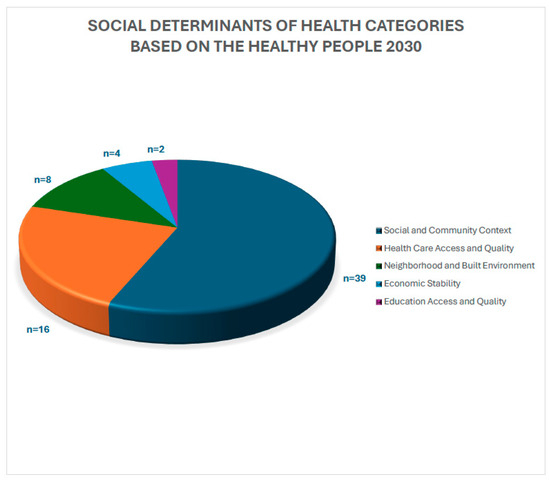
Figure 2.
Classification of social determinants of health based on the Healthy People 2030 five domain categories.
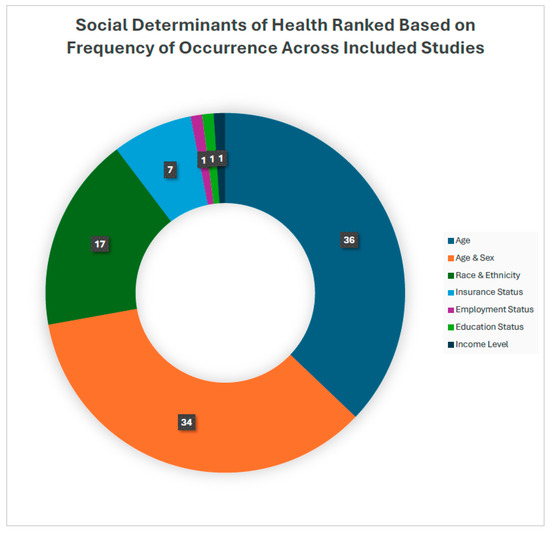
Figure 3.
Frequency of reported social determinants of health in postoperative pain management practices.
3.2. Variance in Prescription Rates Based on Healthcare Setting and SDoH
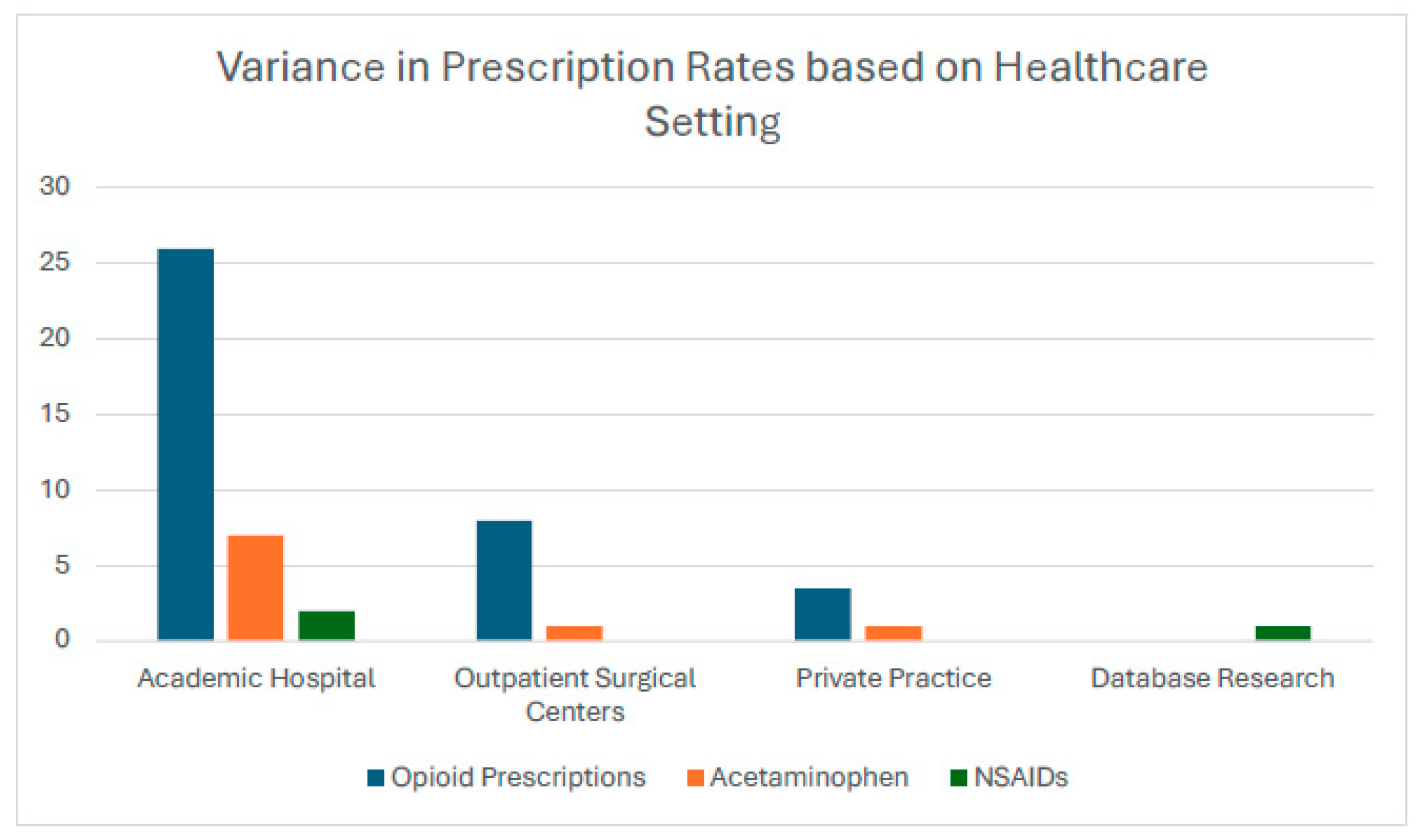
The highest rates of opioid prescriptions were reported in academic hospitals (n = 26) compared to outpatient surgical centers (n = 8). Other types of prescriptions included acetaminophen (n = 9; academic hospital (n = 7), outpatient surgical center (n = 1), and private practice/academic hospital (n = 1)) and NSAIDs (n = 3; academic hospital (n = 2) and database research (n = 1)) (Figure 4). A total of 24 out of 43 studies (Table 2) highlighted findings regarding the variance in opioid prescription rates based on SDoH, considering factors such as age, sex, race, income, insurance type and status, substance use, geographic location, education, and settings of care. Among the studies evaluating age, 11 examined its relationship with opioid use. Four studies reported no significant association between age and opioid prescriptions [41,54,64,70]. Conversely, seven studies indicated that younger patients were associated with higher rates of opioid use [35,37,55,59,62,68,69].
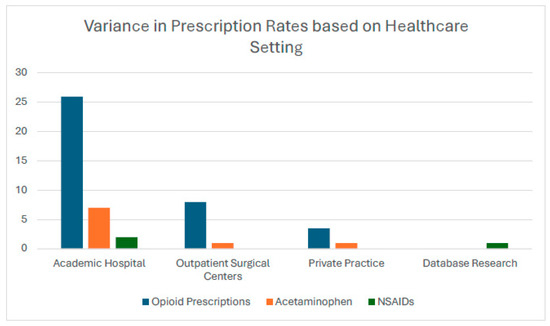
Figure 4.
Type of prescriptions based on healthcare setting.
In terms of sex, six studies investigated its impact on opioid prescriptions. Three studies found that males received higher opioid prescriptions compared to females [35,37], while one study indicated that female patients were more likely to be prescribed opioids [62]. However, Locketz et al. [54], Zipple et al. [70], and Qian et al. [64] reported no significant differences based on sex. Regarding race, five studies analyzed its association with opioid use. Three studies found no correlation between race and opioid prescriptions [57,59,70]. However, Letchuman et al. [53] reported that White patients received higher opioid doses than Black and Asian patients of similar demographics, while Bronstone et al. [36] highlighted a trend of high opioid prescriptions among Black patients. Income and insurance type were also evaluated in six studies (Table 2).
Waljee et al. [68] and Cooperman et al. [37] observed a negative correlation between income and opioid prescriptions, indicating that patients in higher-income areas were less likely to receive opioid refills. Conversely, O’Sullivan et al. [59] found that patients with Medicaid or Medicare were less likely to receive opioid prescriptions compared to those with private insurance. Additionally, Kim et al. [50] noted that self-pay patients and those on Medicaid tended to consume higher amounts of opioids. Lutsky et al. [56] reported that patients with commercial insurance utilized more opioids intraoperatively but filled fewer prescriptions postoperatively. In contrast, Bhashaym et al. [35] found no significant differences in opioid prescriptions based on insurance type. Substance use history was another important factor, with studies indicating that patients with a preoperative history of substance use or substance use disorders required higher opioid dosages [35,55,62]. As-Sanie et al. [31] further demonstrated that patients with chronic pain on medication needed greater opioid doses postoperatively. Keller et al. [48] examined the effects of geographic location and education, finding that patients in the Western U.S. exhibited higher rates of new persistent opioid use, whereas those with a Bachelor’s degree or higher had lower rates of opioid use. Lastly, in regard to care settings, Nouraee et al. [58] reported that fewer pills were prescribed and consumed in outpatient settings compared to inpatient ones (Table 2).
3.3. Types of Surgery of Postoperative Pain
The reviewed studies described a wide range of surgeries associated with acute and chronic postoperative pain. Types of surgeries included orthopedic, gynecologic, abdominal, cardiovascular, and otolaryngologic procedures. Acute postoperative pain was reported in the majority of studies (n = 41) following surgery completion, including laparoscopic cholecystectomy (n = 3) [30,41,66], total hip and knee arthroplasty (n = 2 for each) [51,58,59,62], bariatric surgeries such as sleeve gastrectomy and Roux-en-Y gastric bypass (n = 1) [39], otolaryngology procedures including middle ear and sinus surgeries (n = 2) [37,54], orthopedic procedures like ACL reconstruction and rotator cuff surgery (n = 3) [36,40,59], and cesarean sections (n = 2) [34,57]. Chronic postoperative pain was reported less (n = 3) but was observed in specific procedures, including spinal fusion (n = 2) [60,67], dialysis access surgery (n = 2) [45,65], and cytoreductive surgery (n = 1) [61] (Table 2).
4. Discussion
This scoping review explored postoperative pain management across various healthcare settings and how prescription practices for pain medications vary based on patient characteristics such as sex, race, gender, and insurance status. By examining variations in prescription rates and patterns, the study sought to address gaps in understanding how different healthcare settings and SDoH intersect in postoperative care, ultimately guiding policy recommendations and clinical practices for more personalized and equitable pain management strategies.
The highest reported SDoH in this paper was age, followed by sex. SDOH constitutes 80–90% of the modifiable factors that influence public health, which is not limited to surgical access and postoperative recovery [71]. All patients, regardless of race, ethnicity, sex, age, or socioeconomic status (SES), should receive adequate pain management after surgery to ensure health equity [71]. However, recent studies have noted healthcare disparities in postoperative pain management [72,73]. One theory for the observed differences in treatment among patients is the presence of healthcare providers’ unconscious biases toward patients [72,74]. In the context of older adults, providers might have concerns about adverse effects when prescribing opioids in elderly populations, ultimately leading providers to overlook patients’ pain management needs [74,75]. Rambachan et al. [76] found that older, hospitalized general medicine patients from minoritized groups with geriatric conditions are at risk for inequitable pain assessment, resulting in pain being under-assessed and inadequately treated. Similarly, this trend was seen in females and individuals with low socioeconomic status (SES), such as those with low household income, poor insurance status, or low level of education [72]. Furthermore, being a female was significantly associated with lower amounts of opioid administration after cardiac surgery [77]. Nevertheless, optimal postoperative pain relief has been a challenge for racial minorities and those with lower SES; for instance, although African American and Hispanic individuals reported a significantly higher pain intensity score, they were prescribed fewer opioids than their non-Hispanic White counterparts [72,73]. Language barriers between individuals and providers can perpetuate the low quality of care by either stemming from the provider’s cultural preconception regarding the patient’s pain tolerance or anticipated additional time required for pain assessment [74]. This disparity has shown that patients with limited English proficiency have a reduced propensity to request medication refills after discharge, contributing to diminished access to postoperative care [78]. Standardization of care is needed to reduce disparities in postoperative pain management [72].
Limited healthcare access, lack of insurance coverage, and prior or current substance use history have been significant barriers to opioid prescriptions and effective pain management, and the consequences of such disparities can lead to worsening the burden of the opioid epidemic on the healthcare system [79,80]. These findings further reiterate the importance of the highest ranking SDoH domain, the social and community context, highlighted in the Healthy People 2030 objectives as a crucial factor to consider in building an equitable context for the delivery of postoperative pain management practices across eclectic healthcare settings. Studies have revealed that Hispanic individuals are more likely to have self-pay visits for pain management compared to other populations, which might be a reflection of Hispanics being one of the largest uninsured groups in the US [79,81,82]. Having a lack of insurance coverage may lead providers to be hesitant with opioid management due to there being a need for frequent visits and monitoring [79]. Furthermore, long-acting opioids often face stricter regulations, and insurance coverage for these medications is less likely [83]. It has been noted that pharmacies in areas of non-White neighborhoods tend to have fewer opioid prescriptions available, which, when compounded with limited insurance coverage or lack of insurance, leads to inequities in pain management [79,83,84]. Other disparities associated with opioid prescription include prior substance use history, in which patients have described many negative feelings of stigmatization and discrimination, with clinicians labeling them as “drug addicts”, dismissing their pain, or clinicians being hesitant or completely refusing care for the patient’s pain [80]. Chronic pain is a major factor for increased opioid consumption, which emphasizes the need for adequate pain control after an operation and should not be withheld from patients with an active or prior substance use history because of the fear of worsening addiction or triggering a relapse [8,85]. For patients with opioid use, a higher dose is likely needed after surgery, and it has been noted that poorly treated pain can trigger relapses [8,85]. Moreover, interventions should focus on national medical policies, insurance, and healthcare systems, and providers are required to minimize discriminatory practices, with considerations of consultative expertise with pain specialists when it comes to postoperative pain management in patients with a substance use history [8,80,85].
Our review suggests that there are significant gaps in the implementation of institution-specific, patient-centered, and equitable pain management strategies, particularly in academic hospitals, which our findings show have the highest rates of opioid and NSAID prescriptions (n = 26) compared to outpatient surgical centers (n = 8). Findings from our review of the literature demonstrated that while academic hospitals often adopt enhanced recovery protocols aimed at reducing opioid dependence, these protocols can fail to address the diverse needs of at-risk populations, such as those with chronic substance use, low socioeconomic status, or racial and ethnic minorities. For example, insurance status and economic stability are important factors; patients with Medicaid or Medicare were found less likely to receive prescriptions compared to those with private insurance, which could leave vulnerable groups under-treated for pain [30]. Further, hospital-level factors influencing these disparities include differences in hospital case mix, trainee prescribing behaviors, and lack of standardized opioid prescribing guidelines, particularly in teaching environments [60]. These findings underscore the importance of implementing evidence-based, procedure-specific prescribing protocols to promote safer practices and reduce the risks associated with postoperative opioid use.
Although the focus of this study was hospital factors, in particular teaching hospital status, our results show that patient-level factors such as SDoH and procedure type contribute significantly to variation in postoperative opioid prescribing. The effects of some SDoH are not always unidirectional; when considering race, Letchuman et al. [64] found that White patients received more opioid prescriptions than Black and Asian patients of similar demographics, while Bronstone et al. [62] identified disproportionately high opioid prescription rates among Black patients. These findings highlight that postoperative pain management is influenced by SDoH but also that these effects are not consistent but instead are highly patient and setting-dependent. Additionally, inpatient surgical procedures in academic hospitals had the highest reported rates of opioid prescriptions for postoperative pain management. Disparities in pain management not only perpetuate inequities but also strain the healthcare system by contributing to suboptimal pain control, increased readmissions, and a heightened risk of chronic pain syndromes, underscoring the urgent need for tailored, equitable strategies to improve outcomes across all healthcare settings [86,87].
Moreover, a significant gap remains in the dissemination and implementation of clinical practice guidelines to promote evidence-based, effective, and safer postoperative pain management in children and adults. In 2016, the American Pain Society (APS), with input from the American Society of Anesthesiologists, commissioned an interdisciplinary expert panel to develop such a type of guideline to provide recommendations that addressed various aspects of postoperative pain management, including preoperative education, perioperative pain management planning, use of different pharmacological and nonpharmacological modalities, organizational policies, and transition to outpatient care [8]. Initially drafted based on a systematic review, the recommendations highlight that optimal pain management should be initiated in the preoperative period to be able to culturally tailor the plan of care to reflect not only the patient’s specific needs [8]. However, out of the thirty-two recommendations, only four were supported by high-quality evidence, while eleven were formulated based on low-quality evidence. This is concerning since the majority of recommendations are in the areas of patient education and perioperative planning, patient assessment, organizational structures and policies, and transitioning to outpatient care. These gaps align with the findings from a comprehensive review examining pharmacologic and non-pharmacologic pain management strategies, evaluating their effectiveness, and identifying inconsistencies and gaps in current practices in emergency departments (ED) [88]. Key challenges in the ED environment consisted of time constraints, variability in clinical protocols, and challenges in addressing diverse patient populations, such as tailoring standardized plans to fit the needs of pediatric, geriatric, and chronic pain patients. Recommendations from highlighted studies include the importance of having standardized pain assessment tools and protocols to improve consistency in pain management, integration of innovative technological advances and multimodal approaches to enhance pain management practices, and improved training opportunities for ED staff [88]. Furthermore, enhanced patient education, active involvement in care, individualized non-pharmacological pain relief methods, and PCA use improve perceived pain relief and satisfaction with pain management, particularly when it comes to community healthcare settings in resource-constrained areas [89]. Therefore, the development of more effective and uniform pain management practices in healthcare ultimately leads to better patient outcomes and experiences; however, the continuous striving for ongoing research and adaptation of best practices to meet the evolving needs of patients in the community and academic healthcare settings is essential.
Limitations
Limitations of this study include the exclusion of case reports, case studies, and literature reviews from ‘grey literature’, which potentially limits the breadth of data collection. Our study was also limited in scope by not including tracing of reference lists from included studies, although a comprehensive search of relevant psychosocial databases was conducted involving an initial, secondary, and tertiary screening led by the senior author and co-authors. Further, while search terms used were intentionally broad to account for the diversity of surgical subspecialties in postoperative pain management, the unexpected omission of specific terms may have occurred. This risk was mitigated by collaboration with an expert librarian who developed a rigorous protocol and search strategy for this study. Moreover, our review was limited in scope to studies published in English solely and conducted in the United States. Future studies should broaden the search strategy to include global settings for a worldwide comparison of opioid prescription rates. Finally, the extraction of SDOH proved challenging, as most studies referred to these variables as sociodemographic factors rather than explicitly as SDOH. Future research should advocate for standardizing the nomenclature used for these determinants in the context of opioid prescriptions for postoperative pain management to enhance clarity and comparability. This, in turn, will allow further examination of the development of culturally sensitive and patient-centered approaches to pain management that account for socioeconomic and cultural differences.
5. Conclusions
In an era with a heightened focus on pain management, this review sheds light on the impact of SDoH on the continued variability of postoperative pain management across healthcare settings. Our findings emphasize the critical need for institution-specific, personalized, and equitable strategies that account for SDoH impacting patient needs. This, in turn, ensures enhanced access to individual-specific tailored pain management plans that take into account not only the patient’s medical needs but also their socioeconomic status, which affects access, quality, and affordability of pain management options received. Future research should focus on tailoring pain management protocols to specific populations and care settings, assessing their impact on both patient outcomes and system-wide efficiency. Refining these protocols will help establish a foundation for more effective, equitable, and optimal approaches to postoperative pain management. Researchers should also investigate the role of emerging digital health tools, such as telemedicine and mobile apps, in reducing disparities in postoperative pain management due to their effective and feasible reach and impact, along with their continuously evolving role in the delivery of healthcare services.
Author Contributions
Conceptualization: A.S. and L.S.; methodology: L.A.A.R., A.G. and T.F.; software: A.S., D.L., S.D., E.M., S.S. and J.B.; validation: M.M., P.K. and L.S.; formal analysis; A.S., D.L., S.D., E.M., J.B. and A.D. investigation: L.S.; resources: A.S., D.L. and L.S.; data curation: A.S., D.L., S.D., E.M., S.S., J.B. and A.D.; writing—original draft preparation: A.S., D.L., S.D., E.M., J.B., S.S., L.A.A.R., A.G. and A.D.; writing—review and editing: M.M., P.K. and L.S.; visualization: L.S.; supervision: L.S.; project administration: L.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors report no conflicts of interest.
References
- Horn, R.; Hendrix, J.; Kramer, J. Postoperative Pain Control; StatPearls: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK544298/ (accessed on 19 November 2024).
- Moussa, N.; Ogle, O.E. Acute Pain Management. Oral Maxillofac. Surg. Clin. N. Am. 2022, 34, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Chen, E.; Qian, X. A Narrative Review on Perioperative Pain Management Strategies in Enhanced Recovery Pathways—The Past, Present and Future. J. Clin. Med. 2021, 10, 2568. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, A.; Lirk, P. Multimodal Analgesia. Anesthesiol. Clin. 2022, 40, 455–468. [Google Scholar] [CrossRef] [PubMed]
- Paladini, A.; Rawal, N.; Coca Martinez, M.; Trifa, M.; Montero, A.; Pergolizzi, J., Jr.; Pasqualucci, A.; Narvaez Tamayo, M.A.; Varrassi, G.; De Leon Casasola, O. Advances in the Management of Acute Postsurgical Pain: A Review. Cureus 2023, 15, e42974. [Google Scholar] [CrossRef] [PubMed]
- Dowell, D.; Ragan, K.R.; Jones, C.M.; Baldwin, G.T.; Chou, R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain—United States, 2022. MMWR Recomm. Rep. 2022, 71, 1–95. [Google Scholar] [CrossRef] [PubMed]
- Bernard, S.A.; Chelminski, P.R.; Ives, T.J.; Ranapurwala, S.I. Management of Pain in the United States—A Brief History and Implications for the Opioid Epidemic. Health Serv. Insights 2018, 11, 1178632918819440. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Gordon, D.B.; de Leon-Casasola, O.A.; Rosenberg, J.M.; Bickler, S.; Brennan, T.; Carter, T.; Cassidy, C.L.; Chittenden, E.H.; Degenhardt, E.; et al. Management of Postoperative Pain: A Clinical Practice Guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J. Pain 2016, 17, 131–157. [Google Scholar] [CrossRef] [PubMed]
- Hah, J.M.; Bateman, B.T.; Ratliff, J.; Curtin, C.; Sun, E. Chronic Opioid Use After Surgery: Implications for Perioperative Management in the Face of the Opioid Epidemic. Anesth. Analg. 2017, 125, 1733–1740. [Google Scholar] [CrossRef]
- Guy, G.P., Jr.; Zhang, K.; Bohm, M.K.; Losby, J.; Lewis, B.; Young, R.; Murphy, L.B.; Dowell, D. Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 697–704. [Google Scholar] [CrossRef]
- Bykov, K.; Patorno, E.; Franklin, J.M.; Vine, S.M.; Bateman, B.T. Postoperative inpatient utilization of opioid and opioid-sparing analgesics in the United States hospitals, 2007–2017. Pharmacoepidemiol. Drug Saf. 2021, 30, 390–394. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Community-Based Solutions to Promote Health Equity in the United States; Baciu, A.; Negussie, Y.; Geller, A.; Weinstein, J.N. The State of Health Disparities in the United States; National Academies Press (US): Washington, DC, USA, 2017. [Google Scholar]
- Singh, J.A.; Lu, X.; Rosenthal, G.E.; Ibrahim, S.; Cram, P. Racial disparities in knee and hip total joint arthroplasty: An 18- year analysis of national Medicare data. Ann. Rheum. Dis. 2014, 73, 2107–2115. [Google Scholar] [CrossRef] [PubMed]
- Usiskin, I.; Misra, D. Racial disparities in elective total joint arthroplasty for osteoarthritis. ACR Open Rheumatol. 2022, 4, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Stafford, C.D., II; Keitt, F.; Irvin, L. Health disparities in the management of ACL injuries: How socioeconomic status, insurance, and race influence care. PMR 2022, 14, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Baraga, M.G.; Smith, M.K.; Tanner, J.P.; Kaplan, L.D.; Lesniak, B.P. Anterior cruciate ligament injury and access to care in South Florida: Does insurance status play a role? J. Bone Jt. Surg. Am. 2012, 94, e183. [Google Scholar] [CrossRef]
- Khanna, K.; Janghala, A.; Pandya, N. The effect of insurance status and race on access to care for pediatric and adolescent patients with anterior cruciate ligament injury. J. Health Disparities Res. Pract. 2018, 11, 6. [Google Scholar]
- Meghani, S.H. Corporatization of Pain Medicine: Implications for Widening Pain Care Disparities. Pain Med. 2011, 12, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Sinatra, R. Causes and Consequences of Inadequate Management of Acute Pain. Pain Med. 2010, 11, 1859–1871. [Google Scholar] [CrossRef] [PubMed]
- Keeney, T.; Jette, A.M.; Freedman, V.A.; Cabral, H. Racial differences in patterns of use of rehabilitation services among adults 65 and older racial differences in use of rehabilitation. J. Am. Geriatr. Soc. 2017, 65, 2707–2712. [Google Scholar] [CrossRef]
- Livingston-Rosanoff, D.; Aiken, T.; Rademacher, B.; Glover, C.; Skelton, P.; Paulson, M.; Lawson, E.H. Overprescription of opioids following outpatient anorectal surgery: A single-institution study. Dis. Colon Rectum 2020, 63, 1541–1549. [Google Scholar] [CrossRef] [PubMed]
- Matteson, K.A.; Schimpf, M.O.; Jeppson, P.C.; Thompson, J.C.; Gala, R.B.; Balgobin, S.; Gupta, A.; Hobson, D.; Olivera, C.; Singh, R.; et al. Prescription opioid use for acute pain and persistent opioid use after gynecologic surgery: A systematic review. Obstet. Gynecol. 2023, 141, 681–696. [Google Scholar] [CrossRef]
- Dobie, K.H.; Tiwari, V.; Shi, Y.; Shotwell, M.S.; Sandberg, W.S. Transition from Private to Academic Anesthesia Provision Changes Process and Patient Centered Outcomes in an Ambulatory Surgery Center. J. Med. Syst. 2020, 44, 204. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.M.; Panwar, R.; Borle, A.; Goudra, B.; Trikha, A.; van Wagensveld, B.A.; Sinha, A. Efficiency and Safety Effects of Applying ERAS Protocols to Bariatric Surgery: A Systematic Review with Meta-Analysis and Trial Sequential Analysis of Evidence. Obes. Surg. 2017, 27, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Wang, L.; Coroneos, C.J.; Voineskos, S.H.; Paul, J. Managing postoperative pain in adult outpatients: A systematic review and meta-analysis comparing codeine with NSAIDs. Can. Med. Assoc. J. 2021, 193, E895–E905. [Google Scholar] [CrossRef] [PubMed]
- Hartford, L.B.; Murphy, P.B.; Gray, D.K.; Maciver, A.; Clarke, C.F.M.; Allen, L.J.; Garcia-Ochoa, C.; Leslie, K.A.; Van Koughnett, J.A.M. The Standardization of Outpatient Procedure (STOP) Narcotics after anorectal surgery: A prospective non-inferiority study to reduce opioid use. Tech. Coloproctol. 2020, 24, 563–571. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Office of Disease Prevention and Health Promotion. Social Determinants of Health. Health.gov. 2023. Available online: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed on 15 August 2023).
- Allan, L.D.; Coyne, C.; Byrnes, C.M.; Galet, C.; Skeete, D.A. Tackling the opioid epidemic: Reducing opioid prescribing while maintaining patient satisfaction with pain management after outpatient surgery. Am. J. Surg. 2020, 220, 1108–1114. [Google Scholar] [CrossRef]
- As-Sanie, S.; Till, S.R.; Mowers, E.L.; Lim, C.S.; Skinner, B.D.; Fritsch, L.; Tsodikov, A.; Dalton, V.K.; Clauw, D.J.; Brummett, C.M. Opioid Prescribing Patterns, Patient Use, and Postoperative Pain After Hysterectomy for Benign Indications. Obstet. Gynecol. 2017, 130, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Asanad, K.; Nusbaum, D.J.; Samplaski, M.K. National opioid prescription patterns and patient usage after routine vasectomy. Andrologia 2020, 52, e13563. [Google Scholar] [CrossRef] [PubMed]
- Asmaro, K.; Fadel, H.A.; Haider, S.A.; Pawloski, J.; Telemi, E.; Mansour, T.R.; Chandra, A.; Bazydlo, M.; Robin, A.M.; Lee, I.Y.; et al. Reducing Superfluous Opioid Prescribing Practices After Brain Surgery: It Is Time to Talk About Drugs. Neurosurgery 2021, 89, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Bateman, B.T.; Cole, N.M.; Maeda, A.; Burns, S.M.; Houle, T.T.; Huybrechts, K.F.; Clancy, C.R.; Hopp, S.B.; Ecker, J.L.; Ende, H.; et al. Patterns of Opioid Prescription and Use After Cesarean Delivery. Obstet. Gynecol. 2017, 130, 29–35. [Google Scholar] [CrossRef]
- Bhashyam, A.R.; Keyser, C.; Miller, C.P.; Jacobs, J.; Bluman, E.; Smith, J.T.; Chiodo, C. Prospective Evaluation of Opioid Use After Adoption of a Prescribing Guideline for Outpatient Foot and Ankle Surgery. Foot Ankle Int. 2019, 40, 1260–1266. [Google Scholar] [CrossRef]
- Bronstone, A.B.; Leonardi, C.; Kubilay, T.; Plessl, D.S.; Morreale, P.J.; Tortorich, G.M.; Krause, P.C. Dramatic Reduction in Opioid Prescribing for Common Outpatient Orthopaedic Lower Extremity Surgical Procedures at a Louisiana University-Based Safety-Net Hospital After Enactment of Opioid-Limiting State Legislation. J. Am. Acad. Orthop. Surg. 2022, 30, e405–e414. [Google Scholar] [CrossRef]
- Cooperman, S.P.; Jin, M.C.; Qian, Z.J.; Alyono, J.C. National Trends in Opioid Prescriptions Following Outpatient Otologic Surgery, 2005–2017. Otolaryngol. Neck Surg. 2021, 164, 841–849. [Google Scholar] [CrossRef]
- Cron, D.C.; Hwang, C.; Hu, H.M.; Lee, J.S.; Dupree, J.M.; Syrjamaki, J.D.; Chung, K.C.; Brummett, C.M.; Englesbe, M.J.; Waljee, J.F. A statewide comparison of opioid prescribing in teaching versus nonteaching hospitals. Surgery 2019, 165, 825–831. [Google Scholar] [CrossRef]
- Ford, J.; Kindel, T.; Higgins, R.M.; Lak, K.L.; Hetzel, E.; Gould, J.C. Examining current patterns of opioid prescribing and use after bariatric surgery. Surg. Endosc. 2022, 36, 2564–2569. [Google Scholar] [CrossRef] [PubMed]
- Fujii, M.H.; Hodges, A.C.; Russell, R.L.; Roensch, K.; Beynnon, B.; Ahern, T.P.; Holoch, P.; Moore, J.S.; Ames, S.E.; MacLean, C.D. Post-Discharge Opioid Prescribing and Use after Common Surgical Procedure. J. Am. Coll. Surg. 2018, 226, 1004–1012. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.V.; McMahon, M.L.; Stucke, R.S.; Barth, R.J. Wide Variation and Excessive Dosage of Opioid Prescriptions for Common General Surgical Procedures. Ann. Surg. 2017, 265, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Hite, M.A.; McCutcheon, T.; Feng, M.P.; Ford, M.M.; Geiger, T.M.; Hopkins, M.B.; Muldoon, R.L.; Irlmeier, R.; Fa, A.; Ye, F.; et al. Opioid Utilization in Outpatient Anorectal Surgery: An Opportunity for Improvement. J. Surg. Res. 2023, 291, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Holst, K.A.; Thiels, C.A.; Ubl, D.S.; Blackmon, S.H.; Cassivi, S.D.; Nichols, F.C.I.I.I.; Shen, K.R.; Wigle, D.A.; Thomas, M.; Makey, I.A.; et al. Postoperative Opioid Consumption in Thoracic Surgery Patients: How Much Is Actually Used? Ann. Thorac. Surg. 2020, 109, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
- Jandali, D.B.; Vaughan, D.; Eggerstedt, M.; Ganti, A.; Scheltens, H.; Ramirez, E.A.; Revenaugh, P.C.; Al-Khudari, S.; Smith, R.M.; Stenson, K.M. Enhanced recovery after surgery in head and neck surgery: Reduced opioid use and length of stay. Laryngoscope 2020, 130, 1227–1232. [Google Scholar] [CrossRef]
- Janek, K.C.; Bennett, K.M.; Imbus, J.R.; Danobeitia, J.S.; Philip, J.L.; Melnick, D.M. Patterns of opioid use in dialysis access procedures. J. Vasc. Surg. 2020, 72, 1018–1024. [Google Scholar] [CrossRef] [PubMed]
- Jawad, B.A.; Lam, K.K.; Cecola, C.F.; McCoul, E.D. Opioid Use After Elective Otolaryngologic Surgery at a Teaching Institution. Ochsner. J. 2022, 22, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Katz, A.P.; Misztal, C.; Ghiam, M.K.; Hoffer, M.E. Changes in Single-Specialty Postoperative Opioid Prescribing Patterns in Response to Legislation: Single-Institution Analysis Over Time. Otolaryngol. Neck. Surg. 2021, 164, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Keller, D.S.; Kenney, B.C.; Harbaugh, C.M.; Waljee, J.F.; Brummett, C.M. A national evaluation of opioid prescribing and persistent use after ambulatory anorectal surgery. Surgery 2021, 169, 759–766. [Google Scholar] [CrossRef]
- Kelley, J.J.; Hill, S.; Deem, S.; Hale, N.E. Post-Operative Opioid Prescribing Practices and Trends Among Urology Residents in the United States. Cureus 2020, 12, e12014. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.; Matzon, J.L.; Abboudi, J.; Jones, C.; Kirkpatrick, W.; Leinberry, C.F.; Liss, F.E.; Lutsky, K.F.; Wang, M.L.; Maltenfort, M.; et al. A Prospective Evaluation of Opioid Utilization After Upper-Extremity Surgical Procedures: Identifying Consumption Patterns and Determining Prescribing Guidelines. J. Bone Jt. Surg. 2016, 98, e89. [Google Scholar] [CrossRef] [PubMed]
- Kirkness, C.S.; McAdam-Marx, C.; Unni, S.; Young, J.; Ye, X.; Chandran, A.; Peters, C.L.; Asche, C.V. Characterization of Patients Undergoing Total Hip Arthroplasty in a Real-World Setting and Pain-Related Medication Prescriptions for Management of Postoperative Pain. J. Pain Palliat. Care Pharmacother. 2013, 27, 235–243. [Google Scholar] [CrossRef]
- Kulik, A.; Bykov, K.; Choudhry, N.K.; Bateman, B.T. Non-steroidal anti-inflammatory drug administration after coronary artery bypass surgery: Utilization persists despite the boxed warning: NSAIDS AFTER CARDIAC SURGERY. Pharmacoepidemiol. Drug Saf. 2015, 24, 647–653. [Google Scholar] [CrossRef]
- Letchuman, V.; He, L.; Mummaneni, P.V.; Agarwal, N.; Campbell, L.J.; Shabani, S.; Chan, A.K.; Abrecht, C.R.; Miller, C.; Sankaran, S.; et al. Racial Differences in Postoperative Opioid Prescribing Practices in Spine Surgical Patients. Neurosurgery 2023, 92, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Locketz, G.D.; Brant, J.D.; Adappa, N.D.; Palmer, J.N.; Goldberg, A.N.; Loftus, P.A.; Chandra, R.K.; Bleier, B.S.; Mueller, S.K.; Orlandi, R.R.; et al. Postoperative Opioid Use in Sinonasal Surgery. Otolaryngol. Neck Surg. 2019, 160, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Long, S.M.; Lumley, C.J.; Zeymo, A.; Davidson, B.J. Prescription and Usage Pattern of Opioids after Thyroid and Parathyroid Surgery. Otolaryngol. Neck Surg. 2019, 160, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Lutsky, K.; Hozack, B.; Lucenti, L.; Kwok, M.; Beredjiklian, P.K. Post-operative Opioid, Benzodiazepine and Sedative Usage in Medicare versus Commercial Insurance Hand Surgery Patients. Arch. Bone Jt. Surg. 2021, 9, 319–322. [Google Scholar] [CrossRef] [PubMed]
- McKinnish, T.R.; Lewkowitz, A.K.; Carter, E.B.; Veade, A.E. The impact of race on postpartum opioid prescribing practices: A retrospective cohort study. BMC Pregnancy Childbirth 2021, 21, 434. [Google Scholar] [CrossRef] [PubMed]
- Nouraee, C.M.; McGaver, R.S.; Schaefer, J.J.; O’Neill, O.R.; Anseth, S.D.; Lehman-Lane, J.; Uzlik, R.M.; Giveans, M.R. Opioid-Prescribing Practices Between Total Knee and Hip Arthroplasty in an Outpatient Versus Inpatient Setting. J. Healthc. Qual. 2022, 44, 95–102. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, L.R.; Shofer, F.S.; Delgado, M.K.; Agarwal, A.K.; Humbyrd, C. Are There Differences in Postoperative Opioid Prescribing Across Racial and Ethnic Groups? Assessment of an Academic Health System. Clin. Orthop. 2023, 481, 1504–1511. [Google Scholar] [CrossRef]
- Ong, K.L.; Stoner, K.E.; Yun, B.M.; Lau, E.; Edidin, A.A. Baseline and postfusion opioid burden for patients with low back pain. Am. J. Manag. Care 2018, 24, e234–e240. [Google Scholar] [PubMed]
- Owusu-Agyemang, P.; Cata, J.P.; Kapoor, R.; Speer, B.B.; Bellard, B.; Feng, L.; Gottumukkala, V. Patterns and predictors of outpatient opioid use after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Int. J. Hyperth. 2019, 36, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.; Stranges, P.M.; Bobko, A.; Yan, C.H.; Thambi, M. Changes in postoperative inpatient and outpatient opioid utilization after pharmacist-led order set standardization and education for total knee and hip replacement at an academic medical center. JACCP J. Am. Coll. Clin. Pharm. 2022, 5, 163–173. [Google Scholar] [CrossRef]
- Prabhu, M.C.; Jacob, K.C.; Patel, M.R.; Nie, J.W.; Hartman, T.J.; Singh, K. Multimodal analgesic protocol for cervical disc replacement in the ambulatory setting: Clinical case series. J. Clin. Orthop. Trauma 2022, 35, 102047. [Google Scholar] [CrossRef] [PubMed]
- Qian, Z.J.; Alyono, J.C.; Woods, O.D.; Ali, N.; Blevins, N.H. A Prospective Evaluation of Postoperative Opioid Use in Otologic Surgery. Otol. Neurotol. 2019, 40, 1194–1198. [Google Scholar] [CrossRef]
- Santos-Parker, J.R.; Yoshida, M.; Hallway, A.K.; Englesbe, M.J.; Woodside, K.J.; Howard, R.A. Postoperative Opioid Prescription and Use After Outpatient Vascular Access Surgery. J. Surg. Res. 2021, 264, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Sim, V.; Hawkins, S.; Gave, A.A.; Bulanov, A.; Elabbasy, F.; Khoury, L.; Panzo, M.; Sim, E.; Cohn, S. How low can you go: Achieving postoperative outpatient pain control without opioids. J. Trauma Acute Care Surg. 2019, 87, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Thiels, C.A.; Ubl, D.S.; Yost, K.J.; Dowdy, S.C.; Mabry, T.M.; Gazelka, H.M.; Cima, R.R.; Habermann, E.B. Results of a Prospective, Multicenter Initiative Aimed at Developing Opioid-prescribing Guidelines After Surgery. Ann. Surg. 2018, 268, 457–468. [Google Scholar] [CrossRef]
- Waljee, J.F.; Zhong, L.; Hou, H.; Sears, E.; Brummett, C.; Chung, K.C. The Use of Opioid Analgesics following Common Upper Extremity Surgical Procedures: A National, Population-Based Study. Plast. Reconstr. Surg. 2016, 137, 355e–364e. [Google Scholar] [CrossRef] [PubMed]
- Young, B.T.; Zolin, S.J.; Ferre, A.; Ho, V.P.; Harvey, A.R.; Beel, K.T.; Tseng, E.S.; Conrad-Schnetz, K.; Claridge, J.A. Effects of Ohio’s opioid prescribing limit for the geriatric minimally injured trauma patient. Am. J. Surg. 2020, 219, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Zipple, M.; Braddock, A. Success of Hospital Intervention and State Legislation on Decreasing and Standardizing Postoperative Opioid Prescribing Practices. J. Am. Coll. Surg. 2019, 229, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Devin, C.L.; Shaffer, V.O. Social Determinants of Health and Impact in Perioperative Space. Clin. Colon Rectal Surg. 2023, 36, 206–209. [Google Scholar] [CrossRef] [PubMed]
- HealthPartners Institute; Magnan, S. Social Determinants of Health 101 for Health Care: Five Plus Five. NAM Perspect. 2017, 7. [Google Scholar] [CrossRef]
- Thurston, K.L.; Zhang, S.J.; Wilbanks, B.A.; Billings, R.; Aroke, E.N. A Systematic Review of Race, Sex, and Socioeconomic Status Differences in Postoperative Pain and Pain Management. J. Perianesth. Nurs. 2023, 38, 504–515. [Google Scholar] [CrossRef]
- Perry, M.; Baumbauer, K.; Young, E.E.; Dorsey, S.G.; Taylor, J.Y.; Starkweather, A.R. The Influence of Race, Ethnicity and Genetic Variants on Postoperative Pain Intensity: An Integrative Literature Review. Pain Manag. Nurs. 2019, 20, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Harbell, M.W.; Maloney, J.; Anderson, M.A.; Attanti, S.; Kraus, M.B.; Strand, N. Addressing Bias in Acute Postoperative Pain Management. Curr. Pain Headache Rep. 2023, 27, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Karris, M.Y.; Danilovich, M. Editorial: Chronic Pain and Health Disparities in Older Adults with Complex Needs. Front. Pain Res. 2022, 3, 941476. [Google Scholar] [CrossRef] [PubMed]
- Rambachan, A.; Neilands, T.B.; Karliner, L.; Covinsky, K.; Fang, M.; Nguyen, T. Pain management inequities by demographic and geriatric-related variables in older adult inpatients. J. Am. Geriatr. Soc. 2024, 72, 3000–3010. [Google Scholar] [CrossRef] [PubMed]
- Karamesinis, A.D.; Neto, A.S.; Shi, J.; Fletcher, C.; Hinton, J.; Xing, Z.; Penny-Dimri, J.C.; Ramson, D.; Liu, Z.; Plummer, M.; et al. Sex Differences in Opioid Administration After Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2024, 38, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, K.H.; Rambachan, A.; Ward, D.T.; Manuel, S.P. Language barriers and postoperative opioid prescription use after total knee arthroplasty. Explor. Res. Clin. Soc. Pharm. 2022, 7, 100171. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; McHenry, N.; Gulati, S.; Shah, I.; Sheth, S.G. Racial and Ethnic Disparities in Opioid Prescriptions for Patients with Abdominal Pain: Analysis of the National Ambulatory Medical Care Survey. J. Clin. Med. 2023, 12, 5030. [Google Scholar] [CrossRef]
- Cooke, A.; Castellanos, S.; Koenders, S.; Joshi, N.; Enriquez, C.; Olsen, P.; Miaskowski, C.; Kushel, M.; Knight, K.R. The intersection of drug use discrimination and racial discrimination in the management of chronic non-cancer pain in United States primary care safety-net clinics: Implications for healthcare system and clinic-level changes. Drug Alcohol Depend. 2023, 250, 110893. [Google Scholar] [CrossRef] [PubMed]
- Tolbert, J.; Drake, P.; Damico, A. Key Facts About the Uninsured Population. KFF. 18 December 2023. Available online: https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/ (accessed on 1 December 2024).
- US Census Bureau. Health Insurance Coverage in the United States: 2023. Available online: https://www.census.gov/library/publications/2024/demo/p60-284.html (accessed on 20 December 2024).
- Disparities in Opioid Access for Cancer Pain at End of Life. 14 February 2023. Available online: https://www.cancer.gov/news-events/cancer-currents-blog/2023/disparities-opioids-cancer-pain-end-of-life (accessed on 1 December 2024).
- Morrison, R.S.; Wallenstein, S.; Natale, D.K.; Senzel, R.S.; Huang, L.L. “We Don’t Carry That”—Failure of Pharmacies in Predominantly Nonwhite Neighborhoods to Stock Opioid Analgesics. N. Engl. J. Med. 2000, 342, 1023–1026. [Google Scholar] [CrossRef]
- Zhao, S.; Chen, F.; Feng, A.; Han, W.; Zhang, Y. Risk Factors and Prevention Strategies for Postoperative Opioid Abuse. Pain Res. Manag. 2019, 2019, 7490801. [Google Scholar] [CrossRef]
- Patel, A.R.; Sarkisova, N.; Smith, R.; Gupta, K.; VandenBerg, C.D. Socioeconomic status impacts outcomes following pediatric anterior cruciate ligament reconstruction. Medicine 2019, 98, e15361. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, A.K.; Gadkari, C.; Singh, A.; Pundkar, A. Optimizing Pain Management in Emergency Departments: A Comprehensive Review of Current Analgesic Practices. Cureus 2024, 16, e69789. [Google Scholar] [CrossRef] [PubMed]
- Khalil, H.; Shajrawi, A.; Al-Smadi, A.M.; Bani-Issa, W.; Ahmed, F.R.; AbuSharour, L.; Yateem, N.A.; Yousef, K. Examining postoperative care: Predictors of perceived pain relief and satisfaction with pain management after orthopedic surgeries. Int. J. Orthop. Trauma Nurs. 2025, 56, 101159. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).