Abstract
Angiogenesis, the formation of new blood vessels from pre-existing ones is a biological process that ensures an adequate blood flow is maintained to provide the cells with a sufficient supply of nutrients and oxygen within the body. Numerous soluble growth factors and inhibitors, cytokines, proteases as well as extracellular matrix proteins and adhesion molecules stringently regulate the multi-factorial process of angiogenesis. The properties and interactions of key angiogenic molecules such as vascular endothelial growth factors (VEGFs), fibroblast growth factors (FGFs) and angiopoietins have been investigated in great detail with respect to their molecular impact on angiogenesis. Since the discovery of angiogenic growth factors, much research has been focused on their biological actions and their potential use as therapeutic targets for angiogenic or anti-angiogenic strategies in a context-dependent manner depending on the pathologies. It is generally accepted that these factors play an indispensable role in angiogenesis. However, it is becoming increasingly evident that this is not their only role and it is likely that the angiogenic factors have important functions in a wider range of biological and pathological processes. The additional roles played by these molecules in numerous pathologies and biological processes beyond angiogenesis are discussed in this review.
1. Introduction
Angiogenesis is described as the development of new blood vessels from pre-existing ones. Under normal physiological conditions, the tightly regulated angiogenic process is essential for embryonic growth, wound healing and the female reproductive system [1,2]. Primarily, angiogenic growth factors such as vascular endothelial growth factors (VEGFs) and fibroblast growth factors (FGFs) induce the secretion of endothelial proteinases and plasminogen activators that cause the breakdown of the vessel basement membrane, allowing the cells to intrude the adjoining matrix [2]. Subsequently, the endothelial cells migrate, multiply and ultimately differentiate to give rise to a new, lumen-comprising vessel. Thereafter, the endothelial cells establish a new basement membrane and release additional factors such as platelet-derived growth factor (PDGF), which draws the supporting pericytes to interact externally with the endothelial cells in order to stabilize the newly formed vessels [2].
Angiogenic sprouting is coordinated by a gentle balance between several pro- and anti-angiogenic factors, such as VEGFs, FGFs, angiopoietins (Ang1–4), PDGF, transforming growth factor beta (TGFβ), tumor necrosis factor alpha (TNFα), integrins, adhesion molecules and matrix degrading enzymes [3]. Among the inducers of angiogenesis, the VEGFs, FGFs, and angiopoietins are well-studied and characterized, and probably the most essential angiogenic molecules. Therefore, the current review will focus on these three families of angiogenic growth factors.
Several pathological conditions, such as rheumatoid arthritis, diabetes, chronic kidney disease, cutaneous complications, neurodegenerative disorders, cancer and age-related macular degeneration (Figure 1) are characterized by excessive angiogenesis, where vessels grow in an unrestrained and deranged manner. Moreover, several pathological conditions also exist where these growth factors play diverse roles beyond angiogenesis such as modulation of the immune system, lipid metabolism, glucose metabolism, cellular differentiation and podocyte damage. In this review, we discuss several studies that underline new insights into how these angiogenic growth factor signaling pathways go awry in various pathological conditions. Finally, our review will shed light upon many exciting utilities of these growth factors as diagnostic agents as well as therapeutic targets.
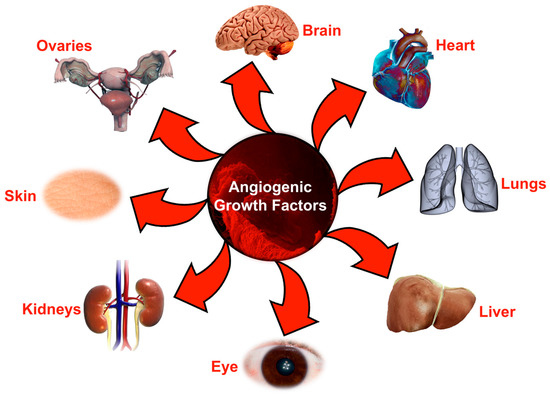
Figure 1.
Organs affected by angiogenic growth factors during various pathological conditions. Schematic diagram representing the most important organs in the body that are usually affected by impaired or excessive angiogenic signaling during initiation or progression of various pathologies.
2. Vascular Endothelial Growth Factor
Till date, there have been seven members identified in the VEGF family of cytokines: VEGF-A, VEGF-B, VEGF-C, VEGF-D, VEGF-E, VEGF-F, and Placental growth factor (PIGF) [4]. VEGF-A (commonly referred to as VEGF) exists as six mRNA splice variants—isoforms 121, 145, 165, 183, 189, and 206, depending upon the number of amino acids present [5]. All VEGF family members are characterized by the presence of a common VEGF homology domain and further consist of various isoforms with diverse functions in the human body. The VEGFs generally bind to three tyrosine kinase receptors: the fms-like tyrosine kinase (Flt-1/VEGF receptor-1; VEGFR-1), the fetal liver kinase (Flk-1/VEGFR-2/KDR), and Flt-4 (VEGFR-3) [4]. VEGFR-2 has been identified as the primary receptor for mediating mitogenesis and regulating vascular permeability [6,7]. Although the function of VEGFR-2 in endothelial cells has been investigated extensively, VEGFR-1 remains a relatively less studied receptor. Interestingly, in spite of having the greatest affinity for VEGF-A, VEGFR-1 possesses a relatively lower intrinsic kinase activity when compared to VEGFR-2, resulting in its inability to mediate mitogenesis [8]. However, VEGFR-1 plays important roles in endothelial cell division during the initial phases of vasculature development. Unlike VEGFR-1/2, VEGFR-3 is able to bind only VEGF-C and VEGF-D [9,10,11]. VEGFR-3 expression is primarily limited to lymphatic endothelial cells where it mediates a plethora of functions like cell migration, survival, and differentiation. VEGF-C binds to neuropilin-2 (NRP-2) and significantly facilitates lymphatic growth in cooperation with VEGFR-3 [9]. Additionally, a VEGF-A splice variant; VEGF-A165 uniquely binds to co-receptor neuropilin-1 (NRP-1) and significantly enhances its availability and binding to VEGFR-2 [12]. However, a very recent report indicated that NRP-1 mediates vascular permeability independently of VEGFR-2 activation [13]. Similarly, NRP-2 also binds VEGF-A165 with high affinity [14]. Preliminary investigations into NRP signaling suggested that due to the lack of kinase motif, NRPs were unable to mediate independent intracellular downstream signals upon ligand binding. Nonetheless, studies have indicated that NRP-1 regulates p130 (Cas) tyrosine phosphorylation through its intracellular domain during cell migration, which may explain its potential independent signaling mechanism [15,16]. Similar to VEGF members, PIGF can also bind both the neuropilins [17,18] and play important functions during angiogenesis. Interestingly, PIGF has been shown to specifically bind to VEGFR-1, with a possible indirect activation of VEGFR-2 through various mechanisms like transphosphorylation [19]. Readers are directed to a review by Hoeben and colleagues for a detailed description of all the VEGF isoforms and their corresponding receptors [4].
3. Role of Vascular Endothelial Growth Factors beyond Angiogenesis
Under physiological conditions, VEGFs regulate several developmental processes, including angiogenesis, lymphangiogenesis and neuronal development. However, they have extensive functions in several pathological processes affecting different organs in the human body. The current review will focus on some of the important pathologies associated with alterations in VEGF/VEGFR expression levels and not their mutations.
3.1. Rheumatoid Arthritis and Osteoarthritis
Rheumatoid arthritis (RA) is a persistent inflammatory disease of the joints whose detrimental effect often spreads beyond joints. RA is characterized by aberrant multiplication of synovial lining cells, causing enlargement of the synovial membrane. The synovia is often infiltrated with different immune cells like macrophages or lymphocytes [20]. Osteoarthritis (OA), commonly referred to as the “wear and tear” arthritis, is the most recurrent chronic non-inflammatory condition affecting the joints [21]. OA is characterized by degeneration of the hyaline cartilage that leads to severe stiffness and swelling, resulting in joint pain [22].
In an extensive review of the role of angiogenesis in arthritis, Walsh [23] described that the expression of VEGF-A121 isoform was notably increased in RA and OA conditions. The splice variants of VEGF-A; VEGF-A121 and VEGF-A189 were also detected in the osteoarthritic cartilage [24]. Importance of VEGF-A165, VEGFR-2, and NRP-1 has been well-studied in synovial angiogenesis occurring in RA [25,26]. Beyond its normal angiogenic function, VEGF-A has been shown to play crucial roles in chemotaxis for monocytes to enhance inflammatory response in the synovia [27]. Moreover, the induction of plasmin and matrix metalloproteinases through VEGF-A function is chiefly involved in degeneration of arthritic joints. Ballara et al. reported that the serum VEGF levels were significantly upregulated in patients with arthritis (RA, psoriatic, self-limiting arthritis and OA) when compared to healthy subjects [28]. Also, the serum VEGF levels were considerably greater in early RA patients in comparison to self-limiting arthritis patients. Another study by Lee and colleagues suggested that serum and synovial fluid VEGF levels were significantly greater in the RA patients than in the OA patients or healthy subjects [29]. Overall, these reports along with additional studies have described the importance and therapeutic benefit of VEGF/VEGFR-2 blockers and VEGF antagonists by ameliorating the symptoms of RA and OA [30,31,32,33,34]. Thalidomide (Apremilast, Celgene, Summit, NJ, United States) and paclitaxel (under the commercial name Paxceed™ Angiotech Pharmaceuticals Inc., Vancouver, BC, Canada) have already been tested in clinical trials for arthritic conditions. Interestingly, thalidomide has been shown to downregulate the expression of VEGF in human lung carcinoma cells [35]. However, the effect of paclitaxel on VEGF expression remains controversial, with one study indicating its ability to induce VEGF expression [36], while another demonstrating its VEGF-suppressive ability [37]. Although the Apremilast clinical study had to be terminated due to lack of efficacy [38], the long-term effectiveness of paclitaxel in RA patients is yet to be determined, in spite of its promising effect on cultured synovial cells from RA patients [39].
Similar to studies on VEGF-A, there have been numerous other studies investigating the roles of other VEGFs in RA and OA. Wauke et al. observed that VEGF-C protein was localized in several synovial lining cells, endothelial cells and stromal cells in RA synovial tissues [40]. Contrariwise, in synovial tissues obtained from OA patients, the VEGF-C protein was localized in the synovial lining cells and endothelial cells but with a lesser degree of expression [40]. Furthermore, the levels of the VEGF-C receptor; VEGFR-3 was significantly increased in RA than in OA. Immunostaining studies conducted on healthy and arthritic synovium indicated that VEGFR-3 + cells also co-expressed VEGFR-2 and other blood vessel markers [41]. Given the function of VEGF-C/VEGFR-3 in maintaining blood vessel fenestrations and synovial fluid formation, its ectopic expression in synovial microvessels could thus be partially explained. However, the exact functional implication and role in pathogenesis remain unclear. Also, VEGF-D was almost nonexistent in the synovial lining of RA patients. Finally, in a recent observational study, Kelly et al. showed a significant correlation between VEGF-C and VEGFR-3 expression with ultrasound assessment of synovitis in a cohort of early RA patients [42]. Taken together, all these studies imply the importance of VEGFs and their receptors in the progression of RA or OA; however, the mechanisms of action remain uncertain.
It is important to note that anti-VEGF/VEGFR therapies, particularly against cancer, have been associated with severe side-effects such as hypertension, gastro-intestinal toxicity, hypothyroidism, proteinuria, coagulation disorders, headache, dyspnea, fatigue, anorexia, stomatitis, diarrhea, neurotoxicity and thrombotic microangiopathy [43,44,45]. Additionally, repression of VEGF expression has been shown to produce significant defects in bleeding and clotting time in VEGF-repressed mice [46]. Due to the ability of VEGFR-2 to control blood pressure through regulation of nitric oxide synthase expression, anti-VEGFR-2 therapies could elevate the risk of hypertension significantly [47]. Therefore, careful measures need to be undertaken to ensure optimal and effective use of such therapies in such a way that the side-effects become manageable and pose less risk while treating pathological conditions.
3.2. Diabetes Mellitus and Associated Complications
Diabetes mellitus is a collection of metabolic disorders highlighted by hyperglycemia, resulting from impaired insulin secretion/action or both. This complex endocrine disease widely affects several organs in the body such as the eyes (retinas), kidneys, nervous system and vascular system. Primarily, VEGF-induced angiogenesis has been shown to play a major role in the pathogenesis of diabetic retinopathy through regulation of endothelial cell proliferation and vascular permeability [48]. However, beyond angiogenesis, both the VEGF-A165 and VEGF-A165b isoforms have shown essential neuroprotective functions in the retina [49,50]. These studies suggest that anti-VEGF therapies could be damaging to the retinal and sensory neurons, opening new avenues for investigating novel therapies against diabetic retinopathy.
In a recent cross-sectional case-control study conducted in patients with type 1 diabetes mellitus or type 2 diabetes mellitus, significant associations were reported between single nucleotide polymorphisms (SNPs) in the VEGF-C gene and the development of diabetic retinopathy, indicating a possible functional role of VEGF-C in the pathogenesis of the disease [51]. However, the exact mechanistic roles of VEGF-C and other VEGF isoforms in diabetic retinopathy remain unknown. The role of VEGFs in the renal pathophysiology of diabetic nephropathy has been diverse and complex [8]. It is known that glucose can directly or indirectly increase the expression of VEGF-A and VEGF-A/eNOS-NO glomerular relationships are central to the pathogenesis of diabetic nephropathy [52,53]. Blockade of the renin-angiotensin, a critical player in elevating VEGF-A, demonstrated promising results to impede the development and progress of diabetic nephropathy. Furthermore, several studies investigated the relationship of VEGF-A with the insulin receptors and nephrin in the setting of diabetic nephropathy [54,55,56] and uncovered their significant pathogenic role. In Zucker diabetic fatty (ZDF) rats, renal or glomerular VEGF mRNA concentration rose early in the course of diabetes and remained elevated till 7 months [57]. Expression of VEGF and VEGFR-1/2 were increased 2-fold in retina and glomeruli from ZDF or insulin-resistant rats, indicating their potential as therapeutic targets [58]. In line with this study, Schrijvers et al. showed that a VEGF-neutralizing antibody prevented glomerular hypertrophy in the ZDF rats [59]. It is important to note that the course of VEGF expression during progression of diabetic nephropathy has been reported to be different in various animal models of type 2 diabetes [8]. Therefore, one needs to be careful when selecting the animal model for studying diabetes and interpreting the results.
Patients with diabetes have a two to five times greater risk of cardiovascular disease [60,61]. Two-fold reductions in VEGF and VEGFR-2 were reported in ventricles from diabetic patients compared to healthy controls [50]. A breakthrough study by Yoon et al. showed that the lack of VEGF expression might affect microvascular homeostasis in the myocardium and thus play a vital role in the pathogenesis of diabetic cardiomyopathy in streptozotocin-induced diabetic rats [62]. Subsequently, it was observed that redox imbalance and/or changes in VEGF expression were responsible for diabetic cardiomyopathy in a murine type 1 diabetes model [63]. More recently, Shida et al. investigated the effects of fluvastatin on diabetic cardiomyopathy and observed that the cardiac function was significantly improved through a reduction in myocardial oxidative stress and increase in VEGF levels [64]. A gene therapy study by Zeng et al. showed that Apelin gene therapy amended diabetic cardiomyopathy through a significant increase in sirtuin 3 and VEGF/VEGFR-2 expression via reducing oxidative stress and endothelial cell apoptosis [65]. Apelin is a bioactive peptide isolated from bovine gastric extract, characterized as an endogenous ligand of the human G-protein-coupled receptor APLNR (Apelin receptor) [66]. These studies document that VEGF-A/VEGFR-2 expression is differentially regulated in most of the diabetes-associated complications. Recent animal studies have suggested that VEGF-B signaling could play important roles in insulin resistance, lipid distribution, and metabolism in type 2 diabetes. In accordance, a study by Sun and colleagues demonstrated a clinical association/correlation of circulating VEGF-B with hyperlipidemia and organ damage in type 2 diabetic patients [67]. However, precise roles of other VEGF isoforms in diabetes-associated complications, if any, need to be investigated in the future.
It has been shown that the prevalence of vascular calcification (excess deposits of calcium mineral in the vessel) is increased in patients with diabetes [68]. Also, coronary artery calcification is now a recognized surrogate endpoint in the studies of diabetes with patients older than 30 years [69]. Interestingly, Yadav et al. reported a significant correlation of VEGF genetic polymorphisms to aortic calcification [70]. In the same study, age, hypertension, diabetes, dyslipidemia, and hyperhomocysteinemia were shown to be the contributing factors for aortic calcification in association with different VEGF genotypes. While demonstrating a direct role, Mikhaylova and colleagues showed that VEGF could induce mineralization in vascular smooth muscle cells [71]. Nonetheless, additional studies are required to further understand the cellular mechanisms in mediating vascular calcification.
3.3. Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) is a lung disease characterized by chronic bronchitis and emphysema. A report by Liebow and colleagues indicated that COPD-affected lungs demonstrate loss of interalveolar septa, making the septa appear extremely thin [72]. At the mechanistic level, Koyama et al. revealed that diminished VEGF levels were observed in the bronchoalveolar lavage fluid from smokers, which could possibly explain the thin and avascular nature of septa [73]. Moreover, VEGF expression was notably reduced in patients with idiopathic pulmonary fibrosis and sarcoidosis in comparison to nonsmokers, with an even further decrease in VEGF levels in smokers.
In another study, Kasahara et al. observed that the transcript and protein levels of VEGF and its receptor VEGFR-2 were diminished in lungs obtained from COPD patients. An important proposition emerged from the study that abnormal VEGF activity and endothelial dysfunction may play a crucial role in the pathogenesis of emphysema [74]. However, it still remains undetermined if reduced VEGF activity is the cause or effect of COPD. A breakthrough study by the same group showed that blockade of VEGFR-2 (using SU5416) in vivo leads to alveolar cell apoptosis and pathogenesis of emphysema in rats [75]. Lastly, a controlled cross-sectional analysis in COPD patients exhibited that oxidative stress-caused epithelial cell injury may lead to diminished VEGF expression in the lungs, which may subsequently result in the progression of COPD [76]. Overall, all these findings emphasize the prominence of VEGF signaling in the pathogenesis of COPD.
3.4. Endometriosis, Preeclampsia, and Ovarian Hyperstimulation Syndrome
Endometriosis is a medical condition characterized by pelvic pain due to an unusual manifestation of endometrial tissue outside the uterus [77]. It was believed that viable endometrial cells could give rise to endometriotic lesions when implanted into the peritoneal cavity through backward menstruation [78]. These ectopic lesions displayed a remarkable growth, leading to the progression of endometriosis. While examining the mechanisms, a direct correlation was observed between VEGF-A in the peritoneal fluid and endometriosis in women [79,80]. In the same year, McLaren and colleagues demonstrated that peritoneal fluid macrophages expressed steroid hormone receptors, VEGFR-1 and VEGFR-2 [80]. Moreover, these macrophages secreted VEGF-A under the influence of ovarian steroid hormones. VEGF receptors’ expression and the migratory reaction were notably greater in women with endometriosis, however, the potential of anti-angiogenic therapy against this disease warrants additional inquiry.
Preeclampsia is a pregnancy-related condition illustrated by high blood pressure accompanied by endothelial injury and dysfunction [81,82]. Several factors have been identified contributing towards endothelial damage such as deficiency of antithrombotic and vasodilator factors and increased concentrations of vasoconstrictor products, pro-thrombotic products, fibronectin concentrations and thrombomodulin. Additionally, neutrophil and platelet activation plays a pivotal role in vascular damage and endothelial dysfunction [83,84,85]. Although it is still unclear what prompts this chain reaction leading to endothelial dysfunction in preeclampsia, recent evidence has indicated that reduced fetoplacental perfusion and abnormal release of aforementioned factors in circulation may result in endothelial injury and consequent medical symptoms [86]. There have been controversies regarding the serum VEGF-A concentrations in women detected with preeclampsia [85,86] and future studies need to be undertaken to resolve the controversies surrounding VEGF-A and its diagnostic/therapeutic potential in preeclampsia. In addition to VEGF-A, VEGFRs have also been shown to have important roles in the pathogenesis of preeclampsia. It was demonstrated that VEGFR-1 expression was increased in patients with severe preeclampsia [87]. Interestingly, soluble VEGFR-1 (sVEGFR-1), an antagonist of VEGF and PIGF, was shown to upregulated in preeclampsia [88]. Moreover, delivery of sVEGFR-1 to pregnant rats induced hypertension, proteinuria, and glomerular endotheliosis, the classic lesion of preeclampsia [88], suggesting a plausible role of circulating sVEGFR-1 in its pathogenesis [89]. As a result, excessive circulating sVEGFR-1 splice variants have been proposed as predictive candidates causing the development of preeclampsia [90]. More recently, VEGFR-1 SNPs were associated with preeclampsia in a Philippine population [91]. Similarly, evidence indicated that differential activation of VEGFR-2 was associated with increased placental angiogenesis in early- as well as late-onset preeclampsia [92], however, mechanistic studies are warranted to pinpoint the exact function of VEGFR-2 in the pathogenesis of this clinical condition.
The ovarian hyperstimulation syndrome (OHSS) is another medical condition that occasionally affects the ovaries upon administration of fertility medicines to stimulate ovulation [93,94]. Enlargement of ovaries and enhanced vascular permeability are major contributing factors in the pathogenesis of OHSS. Several studies have reported elevated serum levels of VEGF during OHSS but it remains uncertain if this rise is the cause or effect of OHSS [95,96,97]. A case-control study reported that polymorphisms of VEGF and VEGF receptors were related to the incidence of OHSS [98]. Moreover, novel strategies inhibiting VEGF activity resulted in the reduction of alterations and severity associated with OHSS in rats [99,100]. Given the therapeutic benefit offered by VEGF antagonists, drugs targeting VEGF should certainly be contemplated for the prevention of OHSS [101].
3.5. Psoriasis
Psoriasis is a prevalent chronic skin disorder depicted by persistent red skin plaques frequently covered with loose scales, which may often be itchy and painful [102]. It is also characterized by infiltration of inflammatory cells and unusual growth of blood vessels that allows meeting the nutritional requirements of the hyperplastic epidermis. Detmar et al. determined that TGFα and EGF play essential roles in the synthesis of VEGF-A and its secretion by keratinocytes in psoriasis [103]. This finding was supported by the observed overexpression of TGFα and EGF receptors. Additionally, elevated levels of serum VEGF-A were observed in psoriasis patients [104]. However, additional research needs to be undertaken to investigate if this phenomenon is due to VEGF-A overproduction in the skin and subsequent leakage in the circulation or due to some genetic defect. Moreover, overexpression of VEGF in keratinocytes led to a significant increase in dermal angiogenesis and resulted in a psoriasis-like phenotype, emphasizing a central role of VEGF in the pathogenesis of skin disorders [105,106]. Neovastat (AE-941), an angiogenesis inhibitor has been shown to alleviate the clinical symptoms of patients suffering from psoriasis [107], indicating that anti-angiogenesis could be an effective strategy against psoriasis [108].
3.6. Neurodegenerative Disorders
The role of vascular growth factors in neurodegenerative disorders has intrigued researchers across the world. A seminal genetic study discovered that targeted aberrations in the promoter region of mice Vegf gene (VEGF∂/∂ mice) lead to adult-onset motoneuron degeneration, indicative of amyotrophic lateral sclerosis (ALS) [89]. In the same VEGF∂/∂ mice, although VEGF levels in the spinal cord were suppressed by about 25% and had no prominent flaws in angiogenesis, neural perfusion was notably reduced, resulting in chronic ischemia of motoneurons. A human study conducted in at least 3 European populations observed that low plasma levels of VEGF owing to faulty transcription and translation correlated with an elevated risk of ALS [109]. Additionally, the secondary effects of elevated VEGF accompanying the ischemic insult and inflammatory response associated with neurodegeneration could be detrimental as excess VEGF expression often results in hemangiomas, microvascular leakage, bleeding and edema, among others.
Several studies have investigated the neuroprotective effects of VEGF through its receptors VEGFR-2 and NRP-1 present in motoneurons [110]. It has been postulated in VEGF∂/∂ mice suffering from ALS that lack of VEGF survival signal may be responsible for the motoneuron degeneration [111]. In another study using VEGF∂/∂ mice, Lambrechts et al. demonstrated that these mice were abnormally vulnerable to continued paralysis post spinal cord ischemia and VEGF-A treatment protected mice against motoneuron death [109]. Furthermore, while clarifying the neuroprotective effect of VEGF signaling, VEGFR-2 overexpression delayed the motoneuron deterioration in another well-established ALS mouse model [112]. Confirming the neuroprotective role of VEGF, several in vitro studies have shown the pro-survival effects of VEGF against cell death when cultured motoneurons were exposed to hypoxia, oxidative stress, serum starvation [111], and superoxide dismutase-1 [113]. It is worthwhile to investigate these protective effects of VEGF in other neurodegenerative disorders, particularly due to the role of VEGF receptors in several neural cells [111,114,115] and the functional benefit offered by VEGF in different types of neurons [115,116], astrocytes [117], microglial cells [118] and Schwann cells [119].
3.7. Organ Fibrosis via Endothelial-to-Mesenchymal Transition
Matrix-yielding fibroblasts have multifactorial origins in fibrotic pathologies, with organ fibrosis via endothelial-to-mesenchymal transition (EndMT) being an important contributor towards fibrosis [120]. EndMT is an extreme form of cellular plasticity where endothelial cells lose typical cobblestone morphology and gain myofibroblast-like features and peculiar spindle-shaped morphology related to mesenchymal cells [121,122]. Although EndMT has been implicated in its physiological role during heart valve formation [123], recent evidence has indicated an additional role of this process in a variety of organ fibrosis disorders like renal [124], cardiac [125], pulmonary [126] and tumor fibrosis [127]. It has been shown that VEGF-A inhibits EndMT through VEGFR-2 signaling and has contrasting effects via VEGFR-1, where it promotes EndMT through decreasing the bioavailability of VEGF-A for VEGFR-2 [128]. Although the role of EndMT and VEGF has been investigated in kidney fibrosis [129], the exact roles and mechanisms of fibrosis in other organs remain undetermined. Furthermore, given the multifactorial role of VEGF in tumors, it remains important to investigate the VEGF-EndMT link in tumor fibrosis. Recently, our preliminary data indicated that cilia; the hair-like projection protruding from the cells, also regulated EndMT through modulation of VEGF-A expression in endothelial cells. Specifically, loss of endothelial cilia led to reduced expression of VEGF-A, leading to enhanced EndMT in vitro and increased organ fibrosis in vivo (unpublished data). Given the importance of EndMT and VEGF in different pathologies, future studies should focus on the causal role of this physiological process in great details.
VEGFs are also involved in the vascular pathology associated with most cases of Alzheimer’s disease, tumors, cerebral ischemia and coronary/peripheral artery disease; however, readers are directed to other reviews for detailed information regarding the same [130,131,132,133]. Additionally, VEGFs have emerged as important determinants and biomarkers for disease mortality and morbidity in several pathological conditions such as sepsis [134,135] or peripheral artery stenosis [136]. However, the potential role of VEGFs during initiation and progression of these conditions has not been studied till date.
4. Fibroblast Growth Factor
Interestingly, the first pro-angiogenic molecule to be ever recognized was the basic fibroblast growth factor (FGF2) [137]. Similar to the VEGF superfamily of growth factors, the FGF family is extensive and comprises of at least 20 factors that are categorized into 6 subfamilies depending on the sequence variation and phylogeny. Unlike most of the other growth factors, the widely studied FGFs; FGF1 and FGF2, do not contain the cytoplasmic signals for their extracellular expression. As a result, their role in angiogenesis had been uncertain for a long time until various studies indicated an alternative mechanism for their extracellular export [138]. Although FGFs display a great affinity to surface heparan sulfate proteoglycans (HSPGs), their biological function is mainly carried out via receptor tyrosine kinases, denoted FGFR1, 2, 3 and 4 [139,140] that arise through alternative splicing [141]. Extensive genetic studies have demonstrated the indispensable role of FGF signaling in angiogenesis and readers are directed to relevant research articles for further information [142,143,144,145]. It is important to note that FGF2 is a more potent angiogenic factor than VEGF-A [146] and hence could be a more viable anti-angiogenic target where FGF signaling outweighs the effect of VEGF signaling.
5. Role of Fibroblast Growth Factors beyond Angiogenesis
The family of FGFs regulates a plethora of developmental processes, including brain patterning, branching morphogenesis, and limb development. Different FGFs are involved in diverse disease conditions. It is beyond the scope of current review to mention disease association of each FGF isoform, however, the most relevant and well-studied FGF-disease links have been discussed. The detrimental genetic disorders that arise from FGF and FGFR mutations have been reviewed elsewhere in detail [147,148].
5.1. Non-Alcoholic Fatty Liver Disease
Non-alcoholic fatty liver disease (NAFLD) is a broad term encompassing several metabolic liver diseases like fatty liver (steatosis), non-alcoholic steatohepatitis (NASH) and liver cirrhosis [149,150]. The incidence of NAFLD is quite common with most patients demonstrating none to very few symptoms. However, in some cases of an extreme form of the disease (e.g., NASH), the excessive fat accumulation could cause hepatic inflammation and damage the liver. In its more serious manifestation, NAFLD can cause complete liver failure. Several risk factors such as obesity, dyslipidemia (abnormal amount of lipids in the blood) and insulin resistance are associated with NAFLD [151,152,153].
Hanaka and colleagues [154] observed a noteworthy function of FGF5 and role of diet in the progression of NASH (specifically hepatic fibrosis) using Fgf5-null mice. However, future investigations are necessary to elucidate the mechanisms linking FGF5, diet, and NASH. Remarkably, in patients with NASH and hepatic steatosis, serum FGF21 concentrations were notably elevated and correlated with the degree of steatosis, indicating its great utility as a serum biomarker for diagnosis [155,156]. Interestingly, in patients with severe NAFLD, FGF21 was significantly decreased owing to the damaged liver [157], suggesting a possible correlation between FGF21 with the degree of disease. In mouse models for NASH, the serum FGF21 levels and its expression in the liver were reported to be drastically high [158,159]. In diet-induced obese mice suffering from NAFLD, Xu et al. [158] described that administering FGF21 reduced body weight and whole-body fat mass, blood glucose, insulin and lipid levels, and reversed hepatic steatosis. Very recent studies have suggested that modulation of miR-49 [160] and miR-212 [161] offered a protective function against NAFLD by targeting FGF21. Taken together these results indicate that FGF21 plays a vital role in multiple metabolic syndromes and has the potential to become an influential therapeutic option to alleviate the symptoms of NAFLD.
Contrastingly, in pediatric NAFLD, serum FGF21 and FGF19 are inversely associated with hepatic damage and these findings may have crucial associations for pinpointing the exact mechanisms of NAFLD progression in adults versus children [162].
5.2. Vascular Calcification
Vascular calcification is a condition where large deposits of calcium mineral are progressively found in main arteries, reducing their elasticity and disturbing the cardiovascular hemodynamics [163,164]. This results in substantial morbidity and mortality mostly in individuals aged >60 years [165]. In subjects from the Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS) study, higher serum FGF23 quantities were independently related with weakened vasoreactivity and augmented arterial stiffness [166]. Furthermore, Ozkok et al. reported a correlation between the coronary artery calcification score (CACS) and FGF23, indicating that FGF23 might have a substantial role in the development of vascular calcification, particularly during the initial steps in hemodialysis patients [167]. A significant association between FGF23 and vascular calcification was also reported in peritoneal dialysis patients [168]. Furthermore, in a cross-sectional study in patients with suspected coronary artery disease, serum FGF23 levels were associated with coronary calcification. Interestingly, in patients who underwent CACS, serum FGF23 levels were associated with vascular calcification, hinting a possible involvement of FGF23 in the formation of atherosclerotic process [169]. Finally, in a recent study with hemodialysis patients, high-flux hemodialysis benefitted the patients through a reduction in the serum FGF23 levels and subsequent reduction in vascular calcification [170].
Overall, these studies indicate a vital role of FGF23 in vascular calcification, a process commonly associated with chronic kidney disease (CKD) and coronary artery disease. Mechanistically, the FGF23/klotho axis has been comprehensively investigated in the vascular calcification process and metabolic disorders involving the same [171]. Additionally, Zhu et al. revealed the essentiality of the ERK1/2 signaling pathway for FGF23 in promoting vascular smooth muscle cell calcification [172].
5.3. Cardiac Hypertrophy
Cardiac hypertrophy is an abnormal thickening of the myocardium, resulting in smaller-sized left and right ventricles of the heart and subsequent impaired heart function. Studies have indicated a connection between circulating FGF23 levels and cardiovascular pathologies such as left ventricular hypertrophy. Left ventricular hypertrophy is highly predominant in CKD settings, therefore, such associations have been primarily investigated in patients with CKD [173]. Furthermore, recent studies have identified activation of FGFR4 as the primary event facilitating the effects of FGF23 on left ventricular hypertrophy, thus postulating novel mechanistic insights and therapeutic targets [174,175,176].
Reports have indicated that circulating concentrations of calcium, phosphorus, and 1,25-dihydroxy vitamin D3 (1,25(OH)2D3) are not only linked with vascular calcification but also with ventricular hypertrophy [177]. Van Ballegooijen et al. showed that increased parathyroid hormone (PTH) levels were associated with left ventricular mass and cardiac troponin T in patients with chronic kidney disease [178] and that FGF23 inhibited its expression and production. Interestingly, 1,25(OH)2D3 stimulated the expression of FGF23 mRNA in osteoblast cell cultures, suggesting a physiologic role of FGF23 to act as a counter regulatory phosphaturic hormone for maintaining phosphate homeostasis in the presence of vitamin D [179]. FGF23 has a dual role in regulating calcitriol (active metabolite of vitamin D) synthesis. Firstly, it downregulates expression of Cyp27b1 gene that translates into 1-alpha-hydroxylase, the enzyme responsible for switching 25(OH)D3 to 1,25-(OH)2D3. Secondly, it also activates the degradation pathway through upregulation of 24-hydroxylase, the enzyme disabling 1,25(OH)2D3 [179,180]. Thus, due to the complex roles of calcium, phosphorus, vitamin D and PTH in cardiovascular pathologies, and the ability of FGF23 to regulate each, makes FGF23 a central player and a therapeutic target in cardiac dysfunction.
Some of the other FGFs have also been shown to play pivotal roles in cardiac repair. For example, FGF2 acts as an essential watchdog of cell proliferation, angiogenesis, collagen production, cardiomyocyte hypertrophy, scar contraction and left ventricular contractile function during infarct repair [181]. In a breakthrough discovery, Faul and colleagues showed a causal function of FGF23 in the pathogenesis of left ventricular hypertrophy [182]. They observed that recurrently elevated FGF23 levels via intramyocardial and intravenous injections of FGF23 in mice, led to high rates of ventricular hypertrophy and mortality. An extensive review by Itoh and Ohta described the pathophysiological roles of FGF signaling in the heart [183]. Mechanistically, FGF2 promotes cardiac hypertrophy and fibrosis through MAPK signaling via the activation of FGFR1c [183,184]. Contrastingly, another FGF isoform; FGF16 showed preventive roles since it competed with FGF2 for binding to the FGFR1c [185]. Also, FGF21 blocked cardiac hypertrophy by activating MAPK signaling through the activation of FGFR1c along with co-receptor βKlotho [186]. Moreover, FGF23 provoked cardiac hypertrophy through calcineurin/NFAT signaling without αKlotho co-receptor [182,187]. While high molecular weight isoform of FGF2 induced hypertrophy through ERK activation, FGF23 depended profoundly on PLC-γ-calcineurin-NFAT activation [188,189]. Together these results indicate that FGFs are involved in cardiac remodeling via distinctive molecular mechanisms.
5.4. Atherosclerosis
Atherosclerosis is characterized by narrowing of the arteries due to building up of plaque inside them [190]. It is a common cause of heart attacks, strokes, and peripheral vascular disease. Chow et al. demonstrated for the first time that increased serum FGF21 concentrations positively correlate with carotid atherosclerosis in a group of Southern Chinese subjects [191]. A cross-sectional study by Semba et al. reported an association between FGF21 levels and hypertension in 744 community-dwelling adults that had participated in the Baltimore Longitudinal Study of Aging [192]. In an interesting study involving aerobic exercises, Yang and colleagues reported that a 3-month combined exercise program reduced the FGF21 quantities as well as arterial rigidity in overweight Korean women [193]. A recent study examining the molecular mechanisms for progression of atherosclerosis showed that the extent of coronary atherosclerosis strongly correlated with the loss of endothelial FGFR1 expression, activation of endothelial TGF-β signaling and the degree of EndMT [194].
Furthermore, FGF/TGF-β signaling cross-talk was discovered as an important regulator of smooth muscle cell phenotypic switch and a major contributor to atherosclerotic plaque growth in mice [195]. Subsequent examination of human coronary arteries with varying grades of atherosclerosis exhibited a robust correlation between the activation of FGF signaling, loss of TGFβ signaling and augmented disease severity. In a rat model of atherosclerosis, FGF21 markedly amended the atherosclerotic symptoms through a reduction in serum levels of total triglyceride, low-density lipoprotein cholesterol, and total cholesterol, accompanied by an increase in the serum levels of high-density lipoprotein cholesterol HDL-C [196]. In vitro, FGF21 prevented cell apoptosis by inhibiting the MAPK pathway. Lastly, a plethora of recent studies has indicated the crucial role of FGF23 in the pathogenesis of atherosclerosis, implicating its utility as a biomarker as well as a therapeutic target [177,197,198,199,200,201,202,203].
5.5. Chronic Kidney Disease (CKD)
CKD is referred to as the continuing loss of kidney function. Under such conditions, the normal function of the kidneys to filter-out wastes and surplus fluids from blood and excrete in the urine is severely affected. During the end stage of this disease, threatening levels of fluid, creatinine, electrolytes and wastes could accumulate in the body [204]. Although FGFs gained much attention due to their clinical relevance in patients with CKD, a majority of the studies were focused on FGF23 and its role in CKD. Studies investigating the function of FGFs (primarily FGF23) as diagnostic markers, causal factors, and therapeutic targets are briefly mentioned in Table 1.

Table 1.
Diverse roles of fibroblast growth factor (FGF) isoforms in diseases of the kidney.
5.6. Lung Disease
In a comprehensive review, Hines and Sun highlighted the importance of FGF, Notch, and Wnt signaling pathways in the development of lung and lung repair pathways [216]. Indeed, after naphthalene injury in mice, parabronchial smooth muscle cells secreted FGF10 to activate Notch signaling and induced Snail expression to induct repair process in the injured lung [217]. Furthermore, FGF10 expression was amplified in smooth muscle cells in the presence of Wnt signaling. FGF10 signaling consequently augmented the Notch pathway leading to a transient epithelial-mesenchymal transition (EMT) in the airway.
Investigating the contributions of other FGF isoforms, Coffey et al. demonstrated that FGF9 protein was aberrantly overexpressed in areas of active cellular hyperplasia, metaplasia, and fibrotic expansion of idiopathic pulmonary fibrosis (IPF) lungs [218]. Similarly, elevated expression of FGF1/FGFRs in the pathogenic regions of IPF suggested that aberrant FGF1-FGFR signaling may contribute to the pathogenesis of lung fibrosis [219]. Additionally, FGF1 was able to revert TGFβ1-induced EMT through MAPK/ERK kinase pathway in alveolar epithelial-like cell lines [220]. FGF strong inhibitor (capable of binding FGFs and blocking FGFR signaling), showed a robust potential to alleviate bleomycin-induced lung fibrosis through inhibiting the expression of α-smooth muscle actin and collagen deposit. Contrastingly, transplantation of FGF7-lentivirus-transduced hematopoietic stem cells diminished bleomycin-induced lung injury, showing the potential of cell-based gene therapy in the lungs [221]. FGF2 has been shown to be required for epithelial recovery, but not for pulmonary fibrosis, in response to bleomycin, which calls for more studies to explore the role of FGF2 as a profibrotic growth factor in vivo [222]. A recent study by Joannes and colleagues demonstrated that FGF9 and FGF18 foster survival and migration in IPF, and prevent in vitro myofibroblast differentiation of human lung fibroblasts [223]. Finally, several small molecule inhibitors/drugs/products have been tested in pre-clinical and clinical studies for their efficacy against lung diseases through modulation of FGF signaling [224,225,226,227,228,229].
5.7. Cutaneous Inflammation
Inflammation of the skin may arise due to a variety of reasons such as radiation, thermal burns or skin injuries/diseases, and in such instances effective wound healing is fundamental for the maintenance of skin integrity. Several studies have indicated the contribution of FGF signaling pathway in skin repair processes. One such study revealed that loss of the IIIb splice variants of FGFR1 and FGFR2 in keratinocytes led to a gradual loss of skin appendages, cutaneous inflammation, keratinocyte over proliferation, and epidermal hyperplasia (thickening of the skin; acanthosis) [230]. Furthermore, FGFs 7, 10, and 22 that stimulate both FGFR1b and 2b, are abundantly expressed in both normal and wounded skin and are critical for maintaining the epidermal wall. Depending upon the FGF isoform, receptor activation can either be autocrine (FGF22) or paracrine (FGF7 and FGF10) [230,231].
In an attempt to understand the mechanisms of hair follicle regeneration, Gay et al. discovered that γδT-cells (a type of T lymphocytes) were important sources of FGF9, which is essential for hair follicle regeneration after wounding [232]. In a mouse model, they found that FGF9 from γδ T cells activated Wnt expression and consequent Wnt activation in fibroblasts. Furthermore, these activated fibroblasts then express FGF9, thus amplifying Wnt activity through a feedback loop, leading to regeneration of hair follicles. Werner et al. showed that FGF2, FGF5, and FGFR1/2 were significantly upregulated upon skin injury, thus indicating the prominence of FGF signaling in wound healing [233]. Intriguingly, a peptide mimetic of FGF2 (FGF-P) protected against acute radiation-induced injury and showed great potential as a future therapeutic option against thermal burns, ischemic wound healing, and tissue regeneration [234]. Finally, an antibacterial protein from the venom of Crotalus adamanteus (diamondback rattlesnake) toxin-II (CaTx-II, of rattlesnake) when utilized for treating wounded mice exhibited noteworthy wound closure and complete healing, accompanied by upregulation in FGF2 levels and other wound healing associated cytokines [235]. Taken together these studies emphasize the central function of effective FGF signaling in the inhibition of cutaneous inflammation.
5.8. Alzheimer’s Disease
Alzheimer’s disease is a progressive mental condition due to widespread deterioration of the brain that is often associated with impaired memory. The nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF) have been widely studied with respect to their role in the pathogenesis of Alzheimer’s disease [236]. Remarkably, FGF2 demonstrates notable functional similarities with neutrophins. For example, FGF2 prevented the neuronal damage and neurofibrillary tangles-like antigenic changes post-glucose deprivation in the brain [237]. Interestingly, FGF2 interacted with BDNF to activate Akt and ERK to offer neuroprotection [238,239]. Several studies reported an induction and binding of FGF2 to the plaques and neurofibrillary tangles in brains affected by Alzheimer’s disease [240,241,242], and in cerebrospinal fluid (CSF) obtained from Alzheimer’s disease patients [243]. Cummings and colleagues showed that FGF2 attracts neurites into plaques and subsequently a damaged neurite may stimulate FGF2 production resulting in further neuritic attraction [244]. While elucidating the distribution of FGFR1 in the cortex and hippocampus of patients with Alzheimer’s disease, immunoreactivity of the FGFR1 (that binds FGF1/2) was augmented in responsive astrocytes, neighboring senile plaques in patients with Alzheimer’s disease when compared to age-matched controls [245].
At the molecular level, it has been determined that the microtubule-related Tau protein is more phosphorylated at certain residues in Alzheimer’s disease paired helical filaments than in normal brain [246,247]. FGF2 stimulation resulted in augmented Tau phosphorylation in neuronal cultures [248] via elevated expression of Tau kinase GSK-3β and Tau protein [249,250,251]. A recent study by Hong et al. showed that the treatment of rats with Puerarin (an isoflavone used for treating Alzheimer’s disease) could considerably improve behavioral performance and the heightened neurogenesis and Tau protein phosphorylation possibly via the FGF2/GSK-3 signaling pathway [252]. A novel synthetic compound that mimics the neuroprotective properties of FGF2 (SUN11602) perfected memory and learning deficits in the hippocampal-lesioned rats through prevention of neuronal death and/or promotion of neurite outgrowth, confirming the utility of such agents for treating neurodegenerative diseases such as Alzheimer’s disease [253]. The presence of senile plaques is one of the key pathological hallmarks of Alzheimer’s disease. These plaques are mainly comprised of potentially toxic amyloid beta-peptide (Abeta) that is produced from a family of Abeta-containing precursor proteins (APP). Interestingly, analogous to NGF, FGF2 acts on the APP promoter, enhances APP transcription and the secretion of sAPP [254,255]. Moreover, when cultures of microglia and astrocytes were exposed to a synthetic homolog of Abeta, they synthesized more FGF2 and promoted the proliferation and morphological alteration of microglia that may contribute to the process of plaque growth [256]. Also, double transgenic mice overexpressing APP and FGF2 exhibited a greater mortality rate than mice expressing APP only, indicating that FGF2 transgene overexpression could augment the deleterious effects of APP [257].
Lastly, the FGF1 levels in serum and CSF were significantly higher in Alzheimer’s disease patients [258]. Although FGF1 may be involved in the pathophysiology of Alzheimer’s disease similar to FGF2, more studies need to be commenced to deduce the exact molecular signaling pathways.
5.9. Corneal Fibrosis
The cornea is the transparent layer in front of the eye, which is composed of an extremely organized group of cells and proteins. The corneal endothelium plays a vital function in maintaining corneal hydration and corneal clearness. Unlike most of the other cells in the human body, adult corneal endothelial cells (CECs) are mitotically inactive, being stopped at the G1 phase of the cell cycle [259]. Although mitogenic FGF2 is present in the Descemet’s membrane (membrane between the corneal proper substance and endothelium) [260], corneal endothelium maintains its anti-proliferative nature throughout its lifetime. However, upon corneal injury, corneal endothelium employs two diverse wound repair pathways. Firstly, via the regenerative pathway, CECs are substituted by migration and spreading of surviving endothelial cells. Secondly, the non-regenerative pathway (or fibrosis), by which altered endothelial cells recommence multiplication, change their cellular morphology and collagen phenotypes, resulting in the generation of an atypical fibrillar extracellular matrix (ECM). A clinical manifestation of such an event is the development of a collagenous retrocorneal fibrous membrane (RCFM) between Descemet’s membrane and the corneal endothelium that causes impaired vision [261].
While unraveling the molecular mechanisms of RCFM formation, studies revealed that FGF2 exerts a dominant role in EndMT that may contribute to corneal fibrosis significantly. Specifically, FGF2 demonstrated a regulatory role in cell cycle progression through degradation of p27Kip1 (p27), a negative controller of the G1 phase of the cell cycle [262,263]. Furthermore, FGF2 increased the steady-state concentrations of α1(I) collagen mRNA by stabilizing the message and subsequently secreting type I collagen into the extracellular space [264]. The same study concluded that FGF2 mediated corneal EndMT through the action of phosphatidylinositol (PI) PI3-kinase. In accordance with EndMT characteristics, FGF2 also induced phenotypic switching where cells changed from atypical cobblestone/polygonal shape to a spindle-shaped/fibroblastic morphology [263]. In vitro, interleukin-1β (IL-1β) induced FGF2 through the PI3-kinase and p38 pathways in CECs and acted as a regulatory switch for FGF2-induced EndMT [265]. Similar findings were reported in vivo when it was discovered that polymorphonuclear leukocytes that intrude the anterior chamber are the main source of IL-1β, which successively facilitates FGF2 production in the corneal endothelium [266]. Together these results provide a primary mechanistic link between injury-associated inflammation and FGF2-induced EndMT.
In a rabbit model of carbon dioxide laser injury, FGF10 significantly abridged inflammation, stromal edema, fibrosis and corneal neovascularization, indicating a major role of FGF10 in the regulation of corneal epithelial wound healing [267].
6. Angiopoietins
Angiopoietins are a family of vascular growth factors, comprising of three structurally linked proteins, termed Angiopoietin-1 (Ang-1), Angiopoietin-2 (Ang-2), and Angiopoietin-3/4 (Ang-3/4) [268]. Ang-1 and Ang-2 remain the most studied with respect to their function during physiological development. These ligands are considered crucial for vascular differentiation through angiogenesis and also participate in the maintenance of blood vessels as well as lymphatic vessels in late gestation and in adult animals [268,269,270]. Ang-1 and Ang-2 bind to the Tie2 (tyrosine kinase with Ig and EGF homology domain 2) receptor tyrosine kinase, whose expression is specific to the blood endothelial cells [271,272]. Interestingly, Ang-1 activates Tie2 as observed via augmented tyrosine phosphorylation of Tie2, while Ang-2 inhibits receptor activation and Ang-1-induced phosphorylation by competitively binding to the receptor. The homologous receptor Tie1 is relatively less well-studied. Due to its expression on developing endothelia, it is postulated that Tie1 inhibits Ang-1-induced Tie2 phosphorylation, thereby delivering a regulatory mechanism for signaling during early development [273].
7. Role of Angiopoietins beyond Angiogenesis
Endothelial dysfunction is associated with many pathological states. Studies focusing on the angiopoietins in dysfunctional blood vessels have provided further data supporting their multiple biological roles in angiogenesis. Some of the major findings involving the role of angiopoietins beyond angiogenesis have been summarized in Table 2 and Table 3. We have included the studies showing the role of angiopoietins in vascular calcification, diabetic retinopathy, diabetic nephropathy, chronic kidney disease, inflammatory bowel disease, pulmonary hypertension, and psoriasis. Additionally, angiopoietins have important causal or diagnostic roles in arthritis [274,275,276,277,278,279,280,281], psoriasis [282], and infertility [283,284,285]. For a detailed role of angiopoietins in ischemia, readers are directed to several excellent reviews [286,287,288].

Table 2.
Distinct roles of angiopoietin isoforms in diseases of the blood vessels, diabetes-associated complications and kidney.

Table 3.
Distinct roles of angiopoietin isoforms in diseases of the bowel, lungs, and skin.
Furthermore, angiopoietin-like proteins (ANGPTLs) are a family of proteins structurally similar to the angiopoietins that are involved in a plethora of physiological and pathophysiological processes. Eight ANGPTLs have been discovered (ANGPTL1 to ANGPTL8) to date. Several elegant reviews exist describing their function in various diseases [289,290,291,292,293,294].
8. Conclusions
Numerous studies have documented the indispensable role of VEGFs, FGFs, and angiopoietins in angiogenesis and related disorders. Functions in vascular permeability, mitogenesis, endothelial cell proliferation, vessel maturation and lymphangiogenesis have been extensively described (Figure 2). Additionally, these growth factors are also actively involved in other angiogenesis-related cellular processes like cell adhesion, cellular differentiation, and recruitment of inflammatory cells.
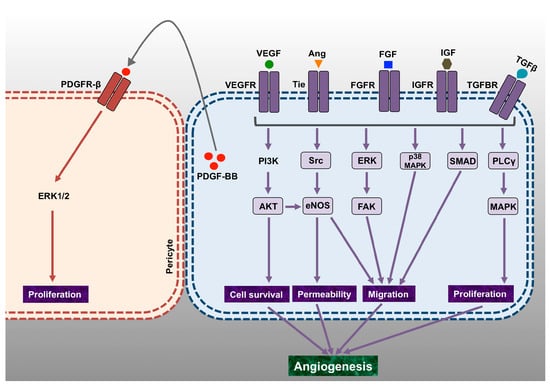
Figure 2.
Overview of the major signaling pathways that mediate proliferation, vascular permeability, cell migration and cell survival, leading to angiogenesis. The schematic diagram represents some of the most important angiogenic growth factors and their signaling via respective cell-surface receptors that leads to proliferative, invasive, vasodilatory and permeability alterations fundamental for cell invasion and angiogenesis. Some of these pathways that are functional during normal physiological conditions can also participate in several pathophysiological processes. PDGFR: Platelet-Derived Growth Factor Receptor; IGF: Insulin-Like Growth Factor; ERK: Extracellular Signal–Regulated Kinase; MAPK: Mitogen-Activated Protein Kinase; PI3K: Phosphatidylinositide 3-Kinase; PLC: Phospholipase C; eNOS: Endothelial Nitric Oxide Synthase; FAK: Focal Adhesion Kinase.
Substantial research has established the myriad pathological processes that involve angiogenic signaling. Therefore, contemplation of broader biological functions of these factors may elucidate the unusual and distinctive roles played by these angiogenic growth factors during disease initiation and progression. These mechanistic insights would lead to the discovery of novel therapies involving recombinant proteins, small molecules, antibodies and gene therapy in the future. Pathological conditions like arthritis, diabetes, kidney disorders, psoriasis, pulmonary and cardiovascular complications and Parkinson’s disease have been treated by angiogenic growth factor-based therapies in several pre-clinical studies. Although the therapeutic potential has been demonstrated in adult humans, the considerable task remains on hand to prevent and treat these diseases at birth. Further mechanistic studies unraveling the intricate roles played by these growth factors will allow to target disorders, both in utero and post-natally. Owing to their multifactorial function in various angiogenesis-independent processes, we believe that it will be more precise to consider these ‘angiogenic factors’, as wide-ranging ‘endothelial factors’. With this comprehensive description of biological activities beyond angiogenesis, these growth factors may emerge as important biomarkers and therapeutic targets in more, as yet unknown pathological conditions.
Acknowledgments
We thank members of the Leong-Poi lab and our collaborators at St. Michael’s Hospital for their valuable contributions to some of the results discussed in this review. This work was supported in part by the Heart and Stroke Foundation of Canada Grant-in-Aid (G-17-0018688) to K.K.S.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Papetti, M.; Herman, I.M. Mechanisms of normal and tumor-derived angiogenesis. Am. J. Physiol. Cell Physiol. 2002, 282, C947–C970. [Google Scholar] [CrossRef] [PubMed]
- Chung, A.S.; Lee, J.; Ferrara, N. Targeting the tumour vasculature: Insights from physiological angiogenesis. Nat. Rev. Cancer 2010, 10, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Distler, J.H.; Hirth, A.; Kurowska-Stolarska, M.; Gay, R.E.; Gay, S.; Distler, O. Angiogenic and angiostatic factors in the molecular control of angiogenesis. Q. J. Nucl. Med. 2003, 47, 149–161. [Google Scholar] [PubMed]
- Hoeben, A.; Landuyt, B.; Highley, M.S.; Wildiers, H.; Van Oosterom, A.T.; De Bruijn, E.A. Vascular endothelial growth factor and angiogenesis. Pharmacol. Rev. 2004, 56, 549–580. [Google Scholar] [CrossRef] [PubMed]
- Harper, S.J.; Bates, D.O. VEGF-A splicing: The key to anti-angiogenic therapeutics? Nat. Rev. Cancer 2008, 8, 880–887. [Google Scholar] [CrossRef] [PubMed]
- Flamme, I.; von Reutern, M.; Drexler, H.C.; Syed-Ali, S.; Risau, W. Overexpression of vascular endothelial growth factor in the avian embryo induces hypervascularization and increased vascular permeability without alterations of embryonic pattern formation. Dev. Biol. 1995, 171, 399–414. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; Sanyal, S.; Mukhopadhyay, D. Tyrosine residues 951 and 1059 of vascular endothelial growth factor receptor-2 (KDR) are essential for vascular permeability factor/vascular endothelial growth factor-induced endothelium migration and proliferation, respectively. J. Biol. Chem. 2001, 276, 32714–32719. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, M. Vascular endothelial growth factor receptor-1 (VEGFR-1/Flt-1): A dual regulator for angiogenesis. Angiogenesis 2006, 9, 225–230, discussion 231. [Google Scholar] [CrossRef] [PubMed]
- Adams, R.H.; Alitalo, K. Molecular regulation of angiogenesis and lymphangiogenesis. Nat. Rev. Mol. Cell Biol. 2007, 8, 464–478. [Google Scholar] [CrossRef] [PubMed]
- Joukov, V.; Pajusola, K.; Kaipainen, A.; Chilov, D.; Lahtinen, I.; Kukk, E.; Saksela, O.; Kalkkinen, N.; Alitalo, K. A novel vascular endothelial growth factor, VEGF-C, is a ligand for the Flt4 (VEGFR-3) and KDR (VEGFR-2) receptor tyrosine kinases. EMBO J. 1996, 15, 290–298. [Google Scholar] [PubMed]
- Achen, M.G.; Jeltsch, M.; Kukk, E.; Makinen, T.; Vitali, A.; Wilks, A.F.; Alitalo, K.; Stacker, S.A. Vascular endothelial growth factor D (VEGF-D) is a ligand for the tyrosine kinases VEGF receptor 2 (Flk1) and VEGF receptor 3 (Flt4). Proc. Natl. Acad. Sci. USA 1998, 95, 548–553. [Google Scholar] [CrossRef] [PubMed]
- Herzog, B.; Pellet-Many, C.; Britton, G.; Hartzoulakis, B.; Zachary, I.C. VEGF binding to NRP1 is essential for VEGF stimulation of endothelial cell migration, complex formation between NRP1 and VEGFR2, and signaling via FAK Tyr407 phosphorylation. Mol. Biol Cell 2011, 22, 2766–2776. [Google Scholar] [CrossRef] [PubMed]
- Roth, L.; Prahst, C.; Ruckdeschel, T.; Savant, S.; Westrom, S.; Fantin, A.; Riedel, M.; Heroult, M.; Ruhrberg, C.; Augustin, H.G. Neuropilin-1 mediates vascular permeability independently of vascular endothelial growth factor receptor-2 activation. Sci. Signal. 2016, 9, ra42. [Google Scholar] [CrossRef] [PubMed]
- Gluzman-Poltorak, Z.; Cohen, T.; Herzog, Y.; Neufeld, G. Neuropilin-2 is a receptor for the vascular endothelial growth factor (VEGF) forms VEGF-145 and VEGF-165 [corrected]. J. Biol. Chem. 2000, 275, 18040–18045. [Google Scholar] [CrossRef] [PubMed]
- Evans, I.M.; Yamaji, M.; Britton, G.; Pellet-Many, C.; Lockie, C.; Zachary, I.C.; Frankel, P. Neuropilin-1 signaling through p130Cas tyrosine phosphorylation is essential for growth factor-dependent migration of glioma and endothelial cells. Mol. Cell. Biol. 2011, 31, 1174–1185. [Google Scholar] [CrossRef] [PubMed]
- Pellet-Many, C.; Frankel, P.; Evans, I.M.; Herzog, B.; Junemann-Ramirez, M.; Zachary, I.C. Neuropilin-1 mediates PDGF stimulation of vascular smooth muscle cell migration and signalling via p130Cas. Biochem. J. 2011, 435, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Migdal, M.; Huppertz, B.; Tessler, S.; Comforti, A.; Shibuya, M.; Reich, R.; Baumann, H.; Neufeld, G. Neuropilin-1 is a placenta growth factor-2 receptor. J. Biol. Chem. 1998, 273, 22272–22278. [Google Scholar] [CrossRef] [PubMed]
- Gaur, P.; Bielenberg, D.R.; Samuel, S.; Bose, D.; Zhou, Y.; Gray, M.J.; Dallas, N.A.; Fan, F.; Xia, L.; Lu, J.; et al. Role of class 3 semaphorins and their receptors in tumor growth and angiogenesis. Clin. Cancer Res. 2009, 15, 6763–6770. [Google Scholar] [CrossRef] [PubMed]
- Autiero, M.; Waltenberger, J.; Communi, D.; Kranz, A.; Moons, L.; Lambrechts, D.; Kroll, J.; Plaisance, S.; De Mol, M.; Bono, F.; et al. Role of PlGF in the intra- and intermolecular cross talk between the VEGF receptors Flt1 and Flk1. Nat. Med. 2003, 9, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Zampeli, E.; Vlachoyiannopoulos, P.G.; Tzioufas, A.G. Treatment of rheumatoid arthritis: Unraveling the conundrum. J. Autoimmun. 2015, 65, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Thijssen, E.; van Caam, A.; van der Kraan, P.M. Obesity and osteoarthritis, more than just wear and tear: Pivotal roles for inflamed adipose tissue and dyslipidaemia in obesity-induced osteoarthritis. Rheumatology 2015, 54, 588–600. [Google Scholar] [CrossRef] [PubMed]
- Burr, D.B.; Gallant, M.A. Bone remodelling in osteoarthritis. Nat. Rev. Rheumatol. 2012, 8, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Walsh, D.A. Angiogenesis and arthritis. Rheumatology 1999, 38, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Pufe, T.; Petersen, W.; Tillmann, B.; Mentlein, R. The splice variants VEGF121 and VEGF189 of the angiogenic peptide vascular endothelial growth factor are expressed in osteoarthritic cartilage. Arthritis Rheumatol. 2001, 44, 1082–1088. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, J.; Wan, L.; Sun, Y.; Wang, F.; Qi, Y.; Huang, C. Up-regulated expressions of HIF-1alpha, VEGF and CD34 promote synovial angiogenesis in rats with adjuvant arthritis. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 2015, 31, 1053–1056. [Google Scholar] [PubMed]
- Raatz, Y.; Ibrahim, S.; Feldmann, M.; Paleolog, E.M. Gene expression profiling and functional analysis of angiogenic markers in murine collagen-induced arthritis. Arthritis Res. Ther. 2012, 14, R169. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, M.; Hosoda, Y.; Hirose, S.; Okada, Y.; Ikeda, E. Expression of vascular endothelial growth factor isoforms and their receptors Flt-1, KDR, and neuropilin-1 in synovial tissues of rheumatoid arthritis. J. Pathol. 2000, 191, 426–433. [Google Scholar] [CrossRef]
- Ballara, S.; Taylor, P.C.; Reusch, P.; Marme, D.; Feldmann, M.; Maini, R.N.; Paleolog, E.M. Raised serum vascular endothelial growth factor levels are associated with destructive change in inflammatory arthritis. Arthritis Rheumatol. 2001, 44, 2055–2064. [Google Scholar] [CrossRef]
- Lee, S.S.; Joo, Y.S.; Kim, W.U.; Min, D.J.; Min, J.K.; Park, S.H.; Cho, C.S.; Kim, H.Y. Vascular endothelial growth factor levels in the serum and synovial fluid of patients with rheumatoid arthritis. Clin. Exp. Rheumatol. 2001, 19, 321–324. [Google Scholar] [PubMed]
- Kim, H.Y.; Park, S.Y.; Lee, S.W.; Lee, H.R.; Lee, W.S.; Rhim, B.Y.; Hong, K.W.; Kim, C.D. Inhibition of HMGB1-induced angiogenesis by cilostazol via SIRT1 activation in synovial fibroblasts from rheumatoid arthritis. PLoS ONE 2014, 9, e104743. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Zhang, Y.; Liu, C.; Guo, W.; Li, X.; Su, X.; Wan, H.; Sun, Y.; Lin, N. Anti-angiogenic effect of triptolide in rheumatoid arthritis by targeting angiogenic cascade. PLoS ONE 2013, 8, e77513. [Google Scholar] [CrossRef] [PubMed]
- Barranco, C. Osteoarthritis: Animal data show VEGF blocker inhibits post-traumatic OA. Nat. Rev. Rheumatol. 2014, 10, 638. [Google Scholar] [CrossRef] [PubMed]
- Nagai, T.; Sato, M.; Kobayashi, M.; Yokoyama, M.; Tani, Y.; Mochida, J. Bevacizumab, an anti-vascular endothelial growth factor antibody, inhibits osteoarthritis. Arthritis Res. Ther. 2014, 16, 427. [Google Scholar] [CrossRef] [PubMed]
- Rossi, D.; Modena, V.; Sciascia, S.; Roccatello, D. Rheumatoid arthritis: Biological therapy other than anti-TNF. Int. Immunopharmacol. 2015, 27, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liu, X.; Wang, J.; Wang, Z.; Jiang, W.; Reed, E.; Zhang, Y.; Liu, Y.; Li, Q.Q. Thalidomide down-regulates the expression of VEGF and bFGF in cisplatin-resistant human lung carcinoma cells. Anticancer Res. 2003, 23, 2481–2487. [Google Scholar] [PubMed]
- Kim, H.S.; Oh, J.M.; Jin, D.H.; Yang, K.H.; Moon, E.Y. Paclitaxel induces vascular endothelial growth factor expression through reactive oxygen species production. Pharmacology 2008, 81, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, R.; Vermeulen, L.C.; Jiang, Z.; Lau, E.; Kolesar, J.M. Gemcitabine and paclitaxel suppress the production of vascular endothelial growth factor induced by deferoxamine in human non-small cell lung cancer A549 cells. Exp. Ther. Med. 2010, 1, 853–857. [Google Scholar] [CrossRef] [PubMed]
- Genovese, M.C.; Jarosova, K.; Cieslak, D.; Alper, J.; Kivitz, A.; Hough, D.R.; Maes, P.; Pineda, L.; Chen, M.; Zaidi, F. Apremilast in Patients With Active Rheumatoid Arthritis: A Phase II, Multicenter, Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Study. Arthritis Rheumatol. 2015, 67, 1703–1710. [Google Scholar] [CrossRef] [PubMed]
- Kurose, A.; Yoshida, W.; Yoshida, M.; Sawai, T. Effects of paclitaxel on cultured synovial cells from patients with rheumatoid arthritis. Cytometry 2001, 44, 349–354. [Google Scholar] [CrossRef]
- Wauke, K.; Nagashima, M.; Ishiwata, T.; Asano, G.; Yoshino, S. Expression and localization of vascular endothelial growth factor-C in rheumatoid arthritis synovial tissue. J. Rheumatol. 2002, 29, 34–38. [Google Scholar] [PubMed]
- Paavonen, K.; Mandelin, J.; Partanen, T.; Jussila, L.; Li, T.F.; Ristimaki, A.; Alitalo, K.; Konttinen, Y.T. Vascular endothelial growth factors C and D and their VEGFR-2 and 3 receptors in blood and lymphatic vessels in healthy and arthritic synovium. J. Rheumatol. 2002, 29, 39–45. [Google Scholar] [PubMed]
- Kelly, S.; Bombardieri, M.; Humby, F.; Ng, N.; Marrelli, A.; Riahi, S.; DiCicco, M.; Mahto, A.; Zou, L.; Pyne, D.; et al. Angiogenic gene expression and vascular density are reflected in ultrasonographic features of synovitis in early Rheumatoid Arthritis: An observational study. Arthritis Res. Ther. 2015, 17, 58. [Google Scholar] [CrossRef] [PubMed]
- Roodhart, J.M.; Langenberg, M.H.; Witteveen, E.; Voest, E.E. The molecular basis of class side effects due to treatment with inhibitors of the VEGF/VEGFR pathway. Curr. Clin. Pharmacol. 2008, 3, 132–143. [Google Scholar] [CrossRef] [PubMed]
- Kamba, T.; McDonald, D.M. Mechanisms of adverse effects of anti-VEGF therapy for cancer. Br. J. Cancer 2007, 96, 1788–1795. [Google Scholar] [CrossRef] [PubMed]
- Eremina, V.; Jefferson, J.A.; Kowalewska, J.; Hochster, H.; Haas, M.; Weisstuch, J.; Richardson, C.; Kopp, J.B.; Kabir, M.G.; Backx, P.H.; et al. VEGF inhibition and renal thrombotic microangiopathy. N. Engl. J. Med. 2008, 358, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Hao, L.; Zhang, S.; Ji, Y.; Zhang, Y.; Lu, X.; Shi, B.; Pei, H.; Wang, Y.; Chen, D.; et al. Genetic repression of mouse VEGF expression regulates coagulation cascade. IUBMB Life 2010, 62, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Facemire, C.S.; Nixon, A.B.; Griffiths, R.; Hurwitz, H.; Coffman, T.M. Vascular endothelial growth factor receptor 2 controls blood pressure by regulating nitric oxide synthase expression. Hypertension 2009, 54, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Mansoor, S.; Sharma, A.; Sapkal, A.; Sheth, J.; Falatoonzadeh, P.; Kuppermann, B.; Kenney, M. Diabetic retinopathy and VEGF. Open Ophthalmol. J. 2013, 7, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Jin, K.L.; Mao, X.O.; Greenberg, D.A. Vascular endothelial growth factor: Direct neuroprotective effect in in vitro ischemia. Proc. Natl. Acad. Sci. USA 2000, 97, 10242–10247. [Google Scholar] [CrossRef] [PubMed]
- Beazley-Long, N.; Hua, J.; Jehle, T.; Hulse, R.P.; Dersch, R.; Lehrling, C.; Bevan, H.; Qiu, Y.; Lagreze, W.A.; Wynick, D.; et al. VEGF-A165b is an endogenous neuroprotective splice isoform of vascular endothelial growth factor A in vivo and in vitro. Am. J. Pathol. 2013, 183, 918–929. [Google Scholar] [CrossRef] [PubMed]
- Kaidonis, G.; Burdon, K.P.; Gillies, M.C.; Abhary, S.; Essex, R.W.; Chang, J.H.; Pal, B.; Pefkianaki, M.; Daniell, M.; Lake, S.; et al. Common Sequence Variation in the VEGFC Gene Is Associated with Diabetic Retinopathy and Diabetic Macular Edema. Ophthalmology 2015, 122, 1828–1836. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.N.; Raij, L.; Mundel, P. Role of angiotensin II in the development of nephropathy and podocytopathy of diabetes. Curr. Diabetes Rev. 2011, 7, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Veron, D.; Aggarwal, P.K.; Velazquez, H.; Kashgarian, M.; Moeckel, G.; Tufro, A. Podocyte-specific VEGF-a gain of function induces nodular glomerulosclerosis in eNOS null mice. J. Am. Soc. Nephrol. 2014, 25, 1814–1824. [Google Scholar] [CrossRef] [PubMed]
- Coward, R.J.; Welsh, G.I.; Koziell, A.; Hussain, S.; Lennon, R.; Ni, L.; Tavare, J.M.; Mathieson, P.W.; Saleem, M.A. Nephrin is critical for the action of insulin on human glomerular podocytes. Diabetes 2007, 56, 1127–1135. [Google Scholar] [CrossRef] [PubMed]
- Reddy, G.R.; Kotlyarevska, K.; Ransom, R.F.; Menon, R.K. The podocyte and diabetes mellitus: Is the podocyte the key to the origins of diabetic nephropathy? Curr. Opin. Nephrol. Hypertens. 2008, 17, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Tufro, A.; Veron, D. VEGF and podocytes in diabetic nephropathy. Semin. Nephrol. 2012, 32, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, K.; Makita, Z.; Yamagishi, S.; Atsumi, T.; Miyoshi, H.; Obara, S.; Ishida, M.; Ishikawa, S.; Yasumura, K.; Koike, T. Suppression of transforming growth factor beta and vascular endothelial growth factor in diabetic nephropathy in rats by a novel advanced glycation end product inhibitor, OPB-9195. Diabetologia 1999, 42, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Chou, E.; Suzuma, I.; Way, K.J.; Opland, D.; Clermont, A.C.; Naruse, K.; Suzuma, K.; Bowling, N.L.; Vlahos, C.J.; Aiello, L.P.; et al. Decreased cardiac expression of vascular endothelial growth factor and its receptors in insulin-resistant and diabetic States: A possible explanation for impaired collateral formation in cardiac tissue. Circulation 2002, 105, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Schrijvers, B.F.; Flyvbjerg, A.; Tilton, R.G.; Lameire, N.H.; De Vriese, A.S. A neutralizing VEGF antibody prevents glomerular hypertrophy in a model of obese type 2 diabetes, the Zucker diabetic fatty rat. Nephrol. Dial. Transplant. 2006, 21, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Martin-Timon, I.; Sevillano-Collantes, C.; Segura-Galindo, A.; Del Canizo-Gomez, F.J. Type 2 diabetes and cardiovascular disease: Have all risk factors the same strength? World J. Diabetes 2014, 5, 444–470. [Google Scholar] [CrossRef] [PubMed]
- Nichols, G.A.; Gullion, C.M.; Koro, C.E.; Ephross, S.A.; Brown, J.B. The incidence of congestive heart failure in type 2 diabetes: An update. Diabetes Care 2004, 27, 1879–1884. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.S.; Uchida, S.; Masuo, O.; Cejna, M.; Park, J.S.; Gwon, H.C.; Kirchmair, R.; Bahlman, F.; Walter, D.; Curry, C.; et al. Progressive attenuation of myocardial vascular endothelial growth factor expression is a seminal event in diabetic cardiomyopathy: Restoration of microvascular homeostasis and recovery of cardiac function in diabetic cardiomyopathy after replenishment of local vascular endothelial growth factor. Circulation 2005, 111, 2073–2085. [Google Scholar] [PubMed]
- Han, B.; Baliga, R.; Huang, H.; Giannone, P.J.; Bauer, J.A. Decreased cardiac expression of vascular endothelial growth factor and redox imbalance in murine diabetic cardiomyopathy. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H829–H835. [Google Scholar] [CrossRef] [PubMed]
- Shida, T.; Nozawa, T.; Sobajima, M.; Ihori, H.; Matsuki, A.; Inoue, H. Fluvastatin-induced reduction of oxidative stress ameliorates diabetic cardiomyopathy in association with improving coronary microvasculature. Heart Vessels 2014, 29, 532–541. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; He, X.; Hou, X.; Li, L.; Chen, J.X. Apelin gene therapy increases myocardial vascular density and ameliorates diabetic cardiomyopathy via upregulation of sirtuin 3. Am. J. Physiol. Heart Circ. Physiol. 2014, 306, H585–H597. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.K.; Cheng, R.; Nguyen, T.; Fan, T.; Kariyawasam, A.P.; Liu, Y.; Osmond, D.H.; George, S.R.; O’Dowd, B.F. Characterization of apelin, the ligand for the APJ receptor. J. Neurochem. 2000, 74, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.Y.; Lee, C.C.; Hsieh, M.F.; Chen, C.H.; Chou, K.M. Clinical association of circulating VEGF-B levels with hyperlipidemia and target organ damage in type 2 diabetic patients. J. Biol. Regul. Homeost. Agents 2014, 28, 225–236. [Google Scholar] [PubMed]
- Schurgin, S.; Rich, S.; Mazzone, T. Increased prevalence of significant coronary artery calcification in patients with diabetes. Diabetes Care 2001, 24, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Snell-Bergeon, J.K.; Budoff, M.J.; Hokanson, J.E. Vascular calcification in diabetes: Mechanisms and implications. Curr. Diabetes Rep. 2013, 13, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Yadav, B.K.; Hong, Y.; Shin, B.S. Correlation of VEGF genetic polymorphisms and lipid profile to aortic calcification. Gene 2014, 550, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Mikhaylova, L.; Malmquist, J.; Nurminskaya, M. Regulation of in vitro vascular calcification by BMP4, VEGF and Wnt3a. Calcif. Tissue Int. 2007, 81, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Liebow, A.A. Pulmonary emphysema with special reference to vascular changes. Am. Rev. Respir. Dis. 1959, 80(Part 2), 67–93. [Google Scholar] [PubMed]
- Koyama, S.; Sato, E.; Haniuda, M.; Numanami, H.; Nagai, S.; Izumi, T. Decreased level of vascular endothelial growth factor in bronchoalveolar lavage fluid of normal smokers and patients with pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2002, 166, 382–385. [Google Scholar] [CrossRef] [PubMed]
- Kasahara, Y.; Tuder, R.M.; Cool, C.D.; Lynch, D.A.; Flores, S.C.; Voelkel, N.F. Endothelial cell death and decreased expression of vascular endothelial growth factor and vascular endothelial growth factor receptor 2 in emphysema. Am. J. Respir. Crit. Care Med. 2001, 163 Pt 1, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Kasahara, Y.; Tuder, R.M.; Taraseviciene-Stewart, L.; Le Cras, T.D.; Abman, S.; Hirth, P.K.; Waltenberger, J.; Voelkel, N.F. Inhibition of VEGF receptors causes lung cell apoptosis and emphysema. J. Clin. Investig. 2000, 106, 1311–1319. [Google Scholar] [CrossRef] [PubMed]
- Kanazawa, H.; Yoshikawa, J. Elevated oxidative stress and reciprocal reduction of vascular endothelial growth factor levels with severity of COPD. Chest 2005, 128, 3191–3197. [Google Scholar] [CrossRef] [PubMed]
- Imesch, P.; Fink, D. Endometriosis Update 2016. Praxis 2016, 105, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Oosterlynck, D.J.; Meuleman, C.; Sobis, H.; Vandeputte, M.; Koninckx, P.R. Angiogenic activity of peritoneal fluid from women with endometriosis. Fertil. Steril. 1993, 59, 778–782. [Google Scholar] [CrossRef]
- Shifren, J.L.; Tseng, J.F.; Zaloudek, C.J.; Ryan, I.P.; Meng, Y.G.; Ferrara, N.; Jaffe, R.B.; Taylor, R.N. Ovarian steroid regulation of vascular endothelial growth factor in the human endometrium: implications for angiogenesis during the menstrual cycle and in the pathogenesis of endometriosis. J. Clin. Endocrinol. Metab. 1996, 81, 3112–3118. [Google Scholar] [PubMed]
- McLaren, J.; Prentice, A.; Charnock-Jones, D.S.; Smith, S.K. Vascular endothelial growth factor (VEGF) concentrations are elevated in peritoneal fluid of women with endometriosis. Hum. Reprod. 1996, 11, 220–223. [Google Scholar] [CrossRef] [PubMed]
- Phipps, E.; Prasanna, D.; Brima, W.; Jim, B. Preeclampsia: Updates in Pathogenesis, Definitions, and Guidelines. Clin. J. Am. Soc. Nephrol. 2016, 11, 1102–1113. [Google Scholar] [CrossRef] [PubMed]
- Liberis, A.; Stanulov, G.; Ali, E.C.; Hassan, A.; Pagalos, A.; Kontomanolis, E.N. Pre-eclampsia and the vascular endothelial growth factor: A new aspect. Clin. Exp. Obstet. Gynecol. 2016, 43, 9–13. [Google Scholar] [PubMed]
- Gibson, J.L.; Lyall, F.; Boswell, F.; Young, A.; Maccuish, A.C.; Greer, I.A. Circulating cell adhesion molecule concentrations in diabetic women during pregnancy. Obstet. Gynecol. 1997, 90, 874–879. [Google Scholar] [CrossRef]
- Clark, C.J.; Boswell, F.; Greer, I.A.; Lyall, F. Treatment of endothelial cells with serum from women with preeclampsia: Effect on neutrophil adhesion. J. Soc. Gynecol. Investig. 1997, 4, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Lyall, F.; Greer, I.A.; Boswell, F.; Fleming, R. Suppression of serum vascular endothelial growth factor immunoreactivity in normal pregnancy and in pre-eclampsia. Br. J. Obstet. Gynaecol. 1997, 104, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Roberts, W.G.; Palade, G.E. Neovasculature induced by vascular endothelial growth factor is fenestrated. Cancer Res. 1997, 57, 765–772. [Google Scholar] [PubMed]
- Helske, S.; Vuorela, P.; Carpen, O.; Hornig, C.; Weich, H.; Halmesmaki, E. Expression of vascular endothelial growth factor receptors 1, 2 and 3 in placentas from normal and complicated pregnancies. Mol. Hum. Reprod. 2001, 7, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Maynard, S.E.; Min, J.Y.; Merchan, J.; Lim, K.H.; Li, J.; Mondal, S.; Libermann, T.A.; Morgan, J.P.; Sellke, F.W.; Stillman, I.E.; et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J. Clin. Investig. 2003, 111, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Tsatsaris, V.; Goffin, F.; Munaut, C.; Brichant, J.F.; Pignon, M.R.; Noel, A.; Schaaps, J.P.; Cabrol, D.; Frankenne, F.; Foidart, J.M. Overexpression of the soluble vascular endothelial growth factor receptor in preeclamptic patients: Pathophysiological consequences. J. Clin. Endocrinol. Metab. 2003, 88, 5555–5563. [Google Scholar] [CrossRef] [PubMed]
- Souders, C.A.; Maynard, S.E.; Yan, J.; Wang, Y.; Boatright, N.K.; Sedan, J.; Balyozian, D.; Cheslock, P.S.; Molrine, D.C.; Simas, T.A. Circulating Levels of sFlt1 Splice Variants as Predictive Markers for the Development of Preeclampsia. Int. J. Mol. Sci. 2015, 16, 12436–12453. [Google Scholar] [CrossRef] [PubMed]
- Amosco, M.D.; Villar, V.A.; Naniong, J.M.; David-Bustamante, L.M.; Jose, P.A.; Palmes-Saloma, C.P. VEGF-A and VEGFR1 SNPs associate with preeclampsia in a Philippine population. Clin. Exp. Hypertens. 2016, 38, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Escudero, C.; Celis, C.; Saez, T.; San Martin, S.; Valenzuela, F.J.; Aguayo, C.; Bertoglia, P.; Roberts, J.M.; Acurio, J. Increased placental angiogenesis in late and early onset pre-eclampsia is associated with differential activation of vascular endothelial growth factor receptor 2. Placenta 2014, 35, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Smith, V.; Osianlis, T.; Vollenhoven, B. Prevention of Ovarian Hyperstimulation Syndrome: A Review. Obstet. Gynecol. Int. 2015, 2015, 514159. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, L.; Humaidan, P. Ovarian hyperstimulation syndrome in the 21st century: The role of gonadotropin-releasing hormone agonist trigger and kisspeptin. Curr. Opin. Obstet. Gynecol. 2015, 27, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Christenson, L.K.; Stouffer, R.L.; Burry, K.A.; Patton, P.E. Vascular endothelial growth factor levels in serum and follicular fluid of patients undergoing in vitro fertilization. Fertil. Steril. 1997, 68, 305–311. [Google Scholar] [CrossRef]
- Artini, P.G.; Fasciani, A.; Monti, M.; Luisi, S.; D’Ambrogio, G.; Genazzani, A.R. Changes in vascular endothelial growth factor levels and the risk of ovarian hyperstimulation syndrome in women enrolled in an in vitro fertilization program. Fertil. Steril. 1998, 70, 560–564. [Google Scholar] [CrossRef]
- Ferrara, N.; Chen, H.; Davis-Smyth, T.; Gerber, H.P.; Nguyen, T.N.; Peers, D.; Chisholm, V.; Hillan, K.J.; Schwall, R.H. Vascular endothelial growth factor is essential for corpus luteum angiogenesis. Nat. Med. 1998, 4, 336–340. [Google Scholar] [CrossRef] [PubMed]
- Nouri, K.; Haslinger, P.; Szabo, L.; Sator, M.; Schreiber, M.; Schneeberger, C.; Pietrowski, D. Polymorphisms of VEGF and VEGF receptors are associated with the occurrence of ovarian hyperstimulation syndrome (OHSS)-a retrospective case-control study. J. Ovarian Res. 2014, 7, 54. [Google Scholar] [CrossRef] [PubMed]
- Scotti, L.; Abramovich, D.; Pascuali, N.; Irusta, G.; Meresman, G.; Tesone, M.; Parborell, F. Local VEGF inhibition prevents ovarian alterations associated with ovarian hyperstimulation syndrome. J. Steroid Biochem. Mol. Biol. 2014, 144 Pt B, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Cenksoy, C.; Cenksoy, P.O.; Erdem, O.; Sancak, B.; Gursoy, R. A potential novel strategy, inhibition of vasopressin-induced VEGF secretion by relcovaptan, for decreasing the incidence of ovarian hyperstimulation syndrome in the hyperstimulated rat model. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 174, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Naredi, N.; Talwar, P.; Sandeep, K. VEGF antagonist for the prevention of ovarian hyperstimulation syndrome: Current status. Med. J. Armed Forces India 2014, 70, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Bronckers, I.M.; Paller, A.S.; van Geel, M.J.; van de Kerkhof, P.C.; Seyger, M.M. Psoriasis in Children and Adolescents: Diagnosis, Management and Comorbidities. Paediatr. Drugs 2015, 17, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Detmar, M.; Brown, L.F.; Claffey, K.P.; Yeo, K.T.; Kocher, O.; Jackman, R.W.; Berse, B.; Dvorak, H.F. Overexpression of vascular permeability factor/vascular endothelial growth factor and its receptors in psoriasis. J. Exp. Med. 1994, 180, 1141–1146. [Google Scholar] [CrossRef] [PubMed]
- Bhushan, M.; McLaughlin, B.; Weiss, J.B.; Griffiths, C.E. Levels of endothelial cell stimulating angiogenesis factor and vascular endothelial growth factor are elevated in psoriasis. Br. J. Dermatol. 1999, 141, 1054–1060. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.P.; Li, B.; Hylton, D.; Detmar, M.; Yancopoulos, G.D.; Rudge, J.S. Transgenic delivery of VEGF to mouse skin leads to an inflammatory condition resembling human psoriasis. Blood 2003, 102, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Kunstfeld, R.; Hirakawa, S.; Hong, Y.K.; Schacht, V.; Lange-Asschenfeldt, B.; Velasco, P.; Lin, C.; Fiebiger, E.; Wei, X.; Wu, Y.; et al. Induction of cutaneous delayed-type hypersensitivity reactions in VEGF-A transgenic mice results in chronic skin inflammation associated with persistent lymphatic hyperplasia. Blood 2004, 104, 1048–1057. [Google Scholar] [CrossRef] [PubMed]
- Sauder, D.N.; Dekoven, J.; Champagne, P.; Croteau, D.; Dupont, E. Neovastat (AE-941), an inhibitor of angiogenesis: Randomized phase I/II clinical trial results in patients with plaque psoriasis. J. Am. Acad. Dermatol. 2002, 47, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Canavese, M.; Altruda, F.; Ruzicka, T.; Schauber, J. Vascular endothelial growth factor (VEGF) in the pathogenesis of psoriasis—A possible target for novel therapies? J. Dermatol. Sci. 2010, 58, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Lambrechts, D.; Storkebaum, E.; Morimoto, M.; Del-Favero, J.; Desmet, F.; Marklund, S.L.; Wyns, S.; Thijs, V.; Andersson, J.; van Marion, I.; et al. VEGF is a modifier of amyotrophic lateral sclerosis in mice and humans and protects motoneurons against ischemic death. Nat. Genet. 2003, 34, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Storkebaum, E.; Carmeliet, P. VEGF: A critical player in neurodegeneration. J. Clin. Investig. 2004, 113, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Oosthuyse, B.; Moons, L.; Storkebaum, E.; Beck, H.; Nuyens, D.; Brusselmans, K.; Van Dorpe, J.; Hellings, P.; Gorselink, M.; Heymans, S.; et al. Deletion of the hypoxia-response element in the vascular endothelial growth factor promoter causes motor neuron degeneration. Nat. Genet. 2001, 28, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Storkebaum, E.; Lambrechts, D.; Dewerchin, M.; Moreno-Murciano, M.P.; Appelmans, S.; Oh, H.; Van Damme, P.; Rutten, B.; Man, W.Y.; De Mol, M.; et al. Treatment of motoneuron degeneration by intracerebroventricular delivery of VEGF in a rat model of ALS. Nat. Neurosci. 2005, 8, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Xu, W.; Luo, C.; Gozal, D.; Liu, R. VEGF-induced activation of the PI3-K/Akt pathway reduces mutant SOD1-mediated motor neuron cell death. Brain Res. Mol. Brain Res. 2003, 111, 155–164. [Google Scholar] [CrossRef]
- Sondell, M.; Kanje, M. Postnatal expression of VEGF and its receptor Flk-1 in peripheral ganglia. Neuroreport 2001, 12, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Sondell, M.; Lundborg, G.; Kanje, M. Vascular endothelial growth factor has neurotrophic activity and stimulates axonal outgrowth, enhancing cell survival and Schwann cell proliferation in the peripheral nervous system. J. Neurosci. 1999, 19, 5731–5740. [Google Scholar] [PubMed]
- Svensson, B.; Peters, M.; Konig, H.G.; Poppe, M.; Levkau, B.; Rothermundt, M.; Arolt, V.; Kogel, D.; Prehn, J.H. Vascular endothelial growth factor protects cultured rat hippocampal neurons against hypoxic injury via an antiexcitotoxic, caspase-independent mechanism. J. Cereb. Blood Flow Metab. 2002, 22, 1170–1175. [Google Scholar] [CrossRef] [PubMed]
- Krum, J.M.; Mani, N.; Rosenstein, J.M. Angiogenic and astroglial responses to vascular endothelial growth factor administration in adult rat brain. Neuroscience 2002, 110, 589–604. [Google Scholar] [CrossRef]
- Forstreuter, F.; Lucius, R.; Mentlein, R. Vascular endothelial growth factor induces chemotaxis and proliferation of microglial cells. J. Neuroimmunol. 2002, 132, 93–98. [Google Scholar] [CrossRef]
- Schratzberger, P.; Schratzberger, G.; Silver, M.; Curry, C.; Kearney, M.; Magner, M.; Alroy, J.; Adelman, L.S.; Weinberg, D.H.; Ropper, A.H.; et al. Favorable effect of VEGF gene transfer on ischemic peripheral neuropathy. Nat. Med. 2000, 6, 405–413. [Google Scholar] [PubMed]
- Piera-Velazquez, S.; Li, Z.; Jimenez, S.A. Role of endothelial-mesenchymal transition (EndoMT) in the pathogenesis of fibrotic disorders. Am. J. Pathol. 2011, 179, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Medici, D.; Shore, E.M.; Lounev, V.Y.; Kaplan, F.S.; Kalluri, R.; Olsen, B.R. Conversion of vascular endothelial cells into multipotent stem-like cells. Nat. Med. 2010, 16, 1400–1406. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.K.; Lovren, F.; Pan, Y.; Quan, A.; Ramadan, A.; Matkar, P.N.; Ehsan, M.; Sandhu, P.; Mantella, L.E.; Gupta, N.; et al. The essential autophagy gene ATG7 modulates organ fibrosis via regulation of endothelial-to-mesenchymal transition. J. Biol. Chem. 2015, 290, 2547–2559. [Google Scholar] [CrossRef] [PubMed]
- Markwald, R.R.; Fitzharris, T.P.; Smith, W.N. Sturctural analysis of endocardial cytodifferentiation. Dev. Biol. 1975, 42, 160–180. [Google Scholar] [CrossRef]
- Li, J.; Qu, X.; Bertram, J.F. Endothelial-myofibroblast transition contributes to the early development of diabetic renal interstitial fibrosis in streptozotocin-induced diabetic mice. Am. J. Pathol. 2009, 175, 1380–1388. [Google Scholar] [CrossRef] [PubMed]
- Zeisberg, E.M.; Tarnavski, O.; Zeisberg, M.; Dorfman, A.L.; McMullen, J.R.; Gustafsson, E.; Chandraker, A.; Yuan, X.; Pu, W.T.; Roberts, A.B.; et al. Endothelial-to-mesenchymal transition contributes to cardiac fibrosis. Nat. Med. 2007, 13, 952–961. [Google Scholar] [CrossRef] [PubMed]
- Nataraj, D.; Ernst, A.; Kalluri, R. Idiopathic pulmonary fibrosis is associated with endothelial to mesenchymal transition. Am. J. Respir. Cell Mol. Biol. 2010, 43, 129–130. [Google Scholar] [CrossRef] [PubMed]
- Zeisberg, E.M.; Potenta, S.; Xie, L.; Zeisberg, M.; Kalluri, R. Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Res. 2007, 67, 10123–10128. [Google Scholar] [CrossRef] [PubMed]
- Paruchuri, S.; Yang, J.H.; Aikawa, E.; Melero-Martin, J.M.; Khan, Z.A.; Loukogeorgakis, S.; Schoen, F.J.; Bischoff, J. Human pulmonary valve progenitor cells exhibit endothelial/mesenchymal plasticity in response to vascular endothelial growth factor-A and transforming growth factor-beta2. Circ. Res. 2006, 99, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Srivastava, S.P.; Kanasaki, M.; He, J.; Kitada, M.; Nagai, T.; Nitta, K.; Takagi, S.; Kanasaki, K.; Koya, D. Interactions of DPP-4 and integrin beta1 influences endothelial-to-mesenchymal transition. Kidney Int. 2015, 88, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Sopova, K.; Gatsiou, K.; Stellos, K.; Laske, C. Dysregulation of neurotrophic and haematopoietic growth factors in Alzheimer’s disease: From pathophysiology to novel treatment strategies. Curr. Alzheimer Res. 2014, 11, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Augustin, H.G. Translating angiogenesis research into the clinic: The challenges ahead. Br. J. Radiol. 2003, 76, S3–S10. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Zhou, H.; Lu, J.; Qu, Y.; Yu, D.; Tong, Y. Vascular endothelial growth factor: An attractive target in the treatment of hypoxic/ischemic brain injury. Neural Regen. Res. 2016, 11, 174–179. [Google Scholar] [PubMed]
- Rasmussen, H.S.; Rasmussen, C.S.; Macko, J. VEGF gene therapy for coronary artery disease and peripheral vascular disease. Cardiovasc. Radiat. Med. 2002, 3, 114–117. [Google Scholar] [CrossRef]
- Yano, K.; Liaw, P.C.; Mullington, J.M.; Shih, S.C.; Okada, H.; Bodyak, N.; Kang, P.M.; Toltl, L.; Belikoff, B.; Buras, J.; et al. Vascular endothelial growth factor is an important determinant of sepsis morbidity and mortality. J. Exp. Med. 2006, 203, 1447–1458. [Google Scholar] [CrossRef] [PubMed]
- Van der Flier, M.; van Leeuwen, H.J.; van Kessel, K.P.; Kimpen, J.L.; Hoepelman, A.I.; Geelen, S.P. Plasma vascular endothelial growth factor in severe sepsis. Shock 2005, 23, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Han, L.; Xu, X.; Tang, H.; Wang, H.; Wei, B. Serum biomarkers VEGF-C and IL-6 are associated with severe human Peripheral Artery Stenosis. J. Inflamm. 2015, 12, 50. [Google Scholar] [CrossRef] [PubMed]
- Shing, Y.; Folkman, J.; Sullivan, R.; Butterfield, C.; Murray, J.; Klagsbrun, M. Heparin affinity: Purification of a tumor-derived capillary endothelial cell growth factor. Science 1984, 223, 1296–1299. [Google Scholar] [CrossRef] [PubMed]
- Dow, J.K.; deVere White, R.W. Fibroblast growth factor 2: Its structure and property, paracrine function, tumor angiogenesis, and prostate-related mitogenic and oncogenic functions. Urology 2000, 55, 800–806. [Google Scholar] [CrossRef]
- Vlodavsky, I.; Bar-Shavit, R.; Ishai-Michaeli, R.; Bashkin, P.; Fuks, Z. Extracellular sequestration and release of fibroblast growth factor: A regulatory mechanism? Trends Biochem. Sci. 1991, 16, 268–271. [Google Scholar] [CrossRef]
- Cross, M.J.; Claesson-Welsh, L. FGF and VEGF function in angiogenesis: Signalling pathways, biological responses and therapeutic inhibition. Trends Pharmacol. Sci. 2001, 22, 201–207. [Google Scholar] [CrossRef]
- Johnson, D.E.; Williams, L.T. Structural and functional diversity in the FGF receptor multigene family. Adv. Cancer Res. 1993, 60, 1–41. [Google Scholar] [PubMed]
- Deng, C.X.; Wynshaw-Boris, A.; Shen, M.M.; Daugherty, C.; Ornitz, D.M.; Leder, P. Murine FGFR-1 is required for early postimplantation growth and axial organization. Genes Dev. 1994, 8, 3045–3057. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Weinstein, M.; Li, C.; Naski, M.; Cohen, R.I.; Ornitz, D.M.; Leder, P.; Deng, C. Fibroblast growth factor receptor 2 (FGFR2)-mediated reciprocal regulation loop between FGF8 and FGF10 is essential for limb induction. Development 1998, 125, 753–765. [Google Scholar] [PubMed]
- Lee, S.H.; Schloss, D.J.; Swain, J.L. Maintenance of vascular integrity in the embryo requires signaling through the fibroblast growth factor receptor. J. Biol. Chem. 2000, 275, 33679–33687. [Google Scholar] [CrossRef] [PubMed]
- Dono, R.; Texido, G.; Dussel, R.; Ehmke, H.; Zeller, R. Impaired cerebral cortex development and blood pressure regulation in FGF-2-deficient mice. EMBO J. 1998, 17, 4213–4225. [Google Scholar] [CrossRef] [PubMed]
- Seghezzi, G.; Patel, S.; Ren, C.J.; Gualandris, A.; Pintucci, G.; Robbins, E.S.; Shapiro, R.L.; Galloway, A.C.; Rifkin, D.B.; Mignatti, P. Fibroblast growth factor-2 (FGF-2) induces vascular endothelial growth factor (VEGF) expression in the endothelial cells of forming capillaries: An autocrine mechanism contributing to angiogenesis. J. Cell Biol. 1998, 141, 1659–1673. [Google Scholar] [CrossRef] [PubMed]
- Teven, C.M.; Farina, E.M.; Rivas, J.; Reid, R.R. Fibroblast growth factor (FGF) signaling in development and skeletal diseases. Genes Dis. 2014, 1, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Beenken, A.; Mohammadi, M. The FGF family: Biology, pathophysiology and therapy. Nat. Rev. Drug Discov. 2009, 8, 235–253. [Google Scholar] [CrossRef] [PubMed]
- Williams, T. Metabolic Syndrome: Nonalcoholic Fatty Liver Disease. FP Essent. 2015, 435, 24–29. [Google Scholar] [PubMed]
- Ahmed, A.; Wong, R.J.; Harrison, S.A. Nonalcoholic Fatty Liver Disease Review: Diagnosis, Treatment, and Outcomes. Clin. Gastroenterol. Hepatol. 2015, 13, 2062–2070. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Cruz, A.; Gomez-Miranda, L.M.; Diaz Ramirez, G.; Carvali Meza, N.Y.; Bacardi-Gascon, M. Adiposity as a risk factor of non alcoholic fat disease; systematic review. Nutr. Hosp. 2014, 29, 771–775. [Google Scholar] [PubMed]
- Yilmaz, Y.; Younossi, Z.M. Obesity-associated nonalcoholic fatty liver disease. Clin. Liver Dis. 2014, 18, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Gruben, N.; Shiri-Sverdlov, R.; Koonen, D.P.; Hofker, M.H. Nonalcoholic fatty liver disease: A main driver of insulin resistance or a dangerous liaison? Biochim. Biophys. Acta 2014, 1842, 2329–2343. [Google Scholar] [CrossRef] [PubMed]
- Hanaka, H.; Hamada, T.; Ito, M.; Nakashima, H.; Tomita, K.; Seki, S.; Kobayashi, Y.; Imaki, J. Fibroblast growth factor-5 participates in the progression of hepatic fibrosis. Exp. Anim. 2014, 63, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, Y.; Eren, F. Identification of a support vector machine-based biomarker panel with high sensitivity and specificity for nonalcoholic steatohepatitis. Clin. Chim. Acta 2012, 414, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Chan, H.L.; Wong, G.L.; Choi, P.C.; Chan, A.W.; Chan, H.Y.; Chim, A.M.; Yeung, D.K.; Chan, F.K.; Woo, J.; et al. Non-invasive diagnosis of non-alcoholic steatohepatitis by combined serum biomarkers. J. Hepatol. 2012, 56, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.; Xia, M.; Chang, X.; Xu, Q.; Bian, H.; Zeng, M.; Rao, S.; Yao, X.; Tu, Y.; Jia, W.; et al. Circulating fibroblast growth factor 21 levels are closely associated with hepatic fat content: A cross-sectional study. PLoS ONE 2011, 6, e24895. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Lloyd, D.J.; Hale, C.; Stanislaus, S.; Chen, M.; Sivits, G.; Vonderfecht, S.; Hecht, R.; Li, Y.S.; Lindberg, R.A.; et al. Fibroblast growth factor 21 reverses hepatic steatosis, increases energy expenditure, and improves insulin sensitivity in diet-induced obese mice. Diabetes 2009, 58, 250–259. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, N.; Takahashi, S.; Zhang, Y.; Krausz, K.W.; Smith, P.B.; Patterson, A.D.; Gonzalez, F.J. Role of fibroblast growth factor 21 in the early stage of NASH induced by methionine- and choline-deficient diet. Biochim. Biophys. Acta 2015, 1852, 1242–1252. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Lv, D.; Zhao, Y.; Chen, X.; Song, M.; Liu, J.; Bei, Y.; Wang, F.; Yang, W.; Yang, C. miR-149 controls non-alcoholic fatty liver by targeting FGF-21. J. Cell Mol. Med. 2016, 20, 1603–1608. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Bei, Y.; Liu, J.; Dimitrova-Shumkovska, J.; Kuang, D.; Zhou, Q.; Li, J.; Yang, Y.; Xiang, Y.; Wang, F.; et al. miR-212 downregulation contributes to the protective effect of exercise against non-alcoholic fatty liver via targeting FGF-21. J. Cell Mol. Med. 2016, 20, 204–216. [Google Scholar] [CrossRef] [PubMed]
- Alisi, A.; Ceccarelli, S.; Panera, N.; Prono, F.; Petrini, S.; De Stefanis, C.; Pezzullo, M.; Tozzi, A.; Villani, A.; Bedogni, G.; et al. Association between Serum Atypical Fibroblast Growth Factors 21 and 19 and Pediatric Nonalcoholic Fatty Liver Disease. PLoS ONE 2013, 8, e67160. [Google Scholar] [CrossRef] [PubMed]
- Allison, M.A.; Criqui, M.H.; Wright, C.M. Patterns and risk factors for systemic calcified atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Wayhs, R.; Zelinger, A.; Raggi, P. High coronary artery calcium scores pose an extremely elevated risk for hard events. J. Am. Coll. Cardiol. 2002, 39, 225–230. [Google Scholar] [CrossRef]
- Demer, L.L.; Tintut, Y. Vascular calcification: Pathobiology of a multifaceted disease. Circulation 2008, 117, 2938–2948. [Google Scholar] [CrossRef] [PubMed]
- Mirza, M.A.; Larsson, A.; Lind, L.; Larsson, T.E. Circulating fibroblast growth factor-23 is associated with vascular dysfunction in the community. Atherosclerosis 2009, 205, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Ozkok, A.; Kekik, C.; Karahan, G.E.; Sakaci, T.; Ozel, A.; Unsal, A.; Yildiz, A. FGF-23 associated with the progression of coronary artery calcification in hemodialysis patients. BMC Nephrol. 2013, 14, 241. [Google Scholar] [CrossRef] [PubMed]
- Asicioglu, E.; Kahveci, A.; Arikan, H.; Koc, M.; Tuglular, S.; Ozener, C.I. Fibroblast growth factor-23 levels are associated with vascular calcifications in peritoneal dialysis patients. Nephron Clin. Pract. 2013, 124, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Peng, C.; Huang, W.; Zhang, J.; Xia, M.; Zhang, Y.; Ling, W. Circulating fibroblast growth factor 23 is associated with angiographic severity and extent of coronary artery disease. PLoS ONE 2013, 8, e72545. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Cui, Q.Q.; Ning, J.P.; Fu, S.S.; Liao, X.H. High-Flux Hemodialysis Benefits Hemodialysis Patients by Reducing Serum FGF-23 Levels and Reducing Vascular Calcification. Med. Sci. Monit. 2015, 21, 3467–3473. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, K.; Nagano, N.; Nitta, K. Klotho/FGF23 Axis in CKD. Contrib. Nephrol. 2015, 185, 56–65. [Google Scholar] [PubMed]
- Zhu, D.; Mackenzie, N.C.; Millan, J.L.; Farquharson, C.; MacRae, V.E. A protective role for FGF-23 in local defence against disrupted arterial wall integrity? Mol. Cell. Endocrinol. 2013, 372, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Shibata, K.; Fujita, S.; Morita, H.; Okamoto, Y.; Sohmiya, K.; Hoshiga, M.; Ishizaka, N. Association between circulating fibroblast growth factor 23, alpha-Klotho, and the left ventricular ejection fraction and left ventricular mass in cardiology inpatients. PLoS ONE 2013, 8, e73184. [Google Scholar] [CrossRef]
- Wyatt, C.M.; Drueke, T.B. Fibroblast growth factor receptor 4: The missing link between chronic kidney disease and FGF23-induced left ventricular hypertrophy? Kidney Int. 2016, 89, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Leifheit-Nestler, M.; Grosse Siemer, R.; Flasbart, K.; Richter, B.; Kirchhoff, F.; Ziegler, W.H.; Klintschar, M.; Becker, J.U.; Erbersdobler, A.; Aufricht, C.; et al. Induction of cardiac FGF23/FGFR4 expression is associated with left ventricular hypertrophy in patients with chronic kidney disease. Nephrol. Dial. Transplant. 2016, 31, 1088–1099. [Google Scholar] [CrossRef] [PubMed]
- Grabner, A.; Amaral, A.P.; Schramm, K.; Singh, S.; Sloan, A.; Yanucil, C.; Li, J.; Shehadeh, L.A.; Hare, J.M.; David, V.; et al. Activation of Cardiac Fibroblast Growth Factor Receptor 4 Causes Left Ventricular Hypertrophy. Cell Metab. 2015, 22, 1020–1032. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.Y.; Ma, H.X. Significant roles of anti-aging protein klotho and fibroblast growth factor 23 in cardiovascular disease. J. Geriatr. Cardiol. 2015, 12, 439–447. [Google Scholar] [PubMed]
- Van Ballegooijen, A.J.; Visser, M.; Kestenbaum, B.; Siscovick, D.S.; de Boer, I.H.; Gottdiener, J.S.; deFilippi, C.R.; Brouwer, I.A. Relation of vitamin D and parathyroid hormone to cardiac biomarkers and to left ventricular mass (from the Cardiovascular Health Study). Am. J. Cardiol. 2013, 111, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Tang, W.; Zhou, J.; Stubbs, J.R.; Luo, Q.; Pi, M.; Quarles, L.D. Fibroblast growth factor 23 is a counter-regulatory phosphaturic hormone for vitamin D. J. Am. Soc. Nephrol. 2006, 17, 1305–1315. [Google Scholar] [CrossRef] [PubMed]
- Donate-Correa, J.; Muros-de-Fuentes, M.; Mora-Fernandez, C.; Navarro-Gonzalez, J.F. FGF23/Klotho axis: Phosphorus, mineral metabolism and beyond. Cytokine Growth Factor Rev. 2012, 23, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Virag, J.A.; Rolle, M.L.; Reece, J.; Hardouin, S.; Feigl, E.O.; Murry, C.E. Fibroblast growth factor-2 regulates myocardial infarct repair: Effects on cell proliferation, scar contraction, and ventricular function. Am. J. Pathol. 2007, 171, 1431–1440. [Google Scholar] [CrossRef] [PubMed]
- Faul, C.; Amaral, A.P.; Oskouei, B.; Hu, M.C.; Sloan, A.; Isakova, T.; Gutierrez, O.M.; Aguillon-Prada, R.; Lincoln, J.; Hare, J.M.; et al. FGF23 induces left ventricular hypertrophy. J. Clin. Investig. 2011, 121, 4393–4408. [Google Scholar] [CrossRef] [PubMed]
- Itoh, N.; Ohta, H. Pathophysiological roles of FGF signaling in the heart. Front. Physiol. 2013, 4, 247. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Ibrahimi, O.A.; Olsen, S.K.; Umemori, H.; Mohammadi, M.; Ornitz, D.M. Receptor specificity of the fibroblast growth factor family. The complete mammalian FGF family. J. Biol. Chem. 2006, 281, 15694–15700. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.Y.; Sontag, D.P.; Detillieux, K.A.; Cattini, P.A. FGF-16 is released from neonatal cardiac myocytes and alters growth-related signaling: A possible role in postnatal development. Am. J. Physiol. Cell Physiol. 2008, 294, C1242–C1249. [Google Scholar] [CrossRef] [PubMed]
- Planavila, A.; Redondo, I.; Hondares, E.; Vinciguerra, M.; Munts, C.; Iglesias, R.; Gabrielli, L.A.; Sitges, M.; Giralt, M.; van Bilsen, M.; et al. Fibroblast growth factor 21 protects against cardiac hypertrophy in mice. Nat. Commun. 2013, 4, 2019. [Google Scholar] [CrossRef] [PubMed]
- Faul, C. Fibroblast growth factor 23 and the heart. Curr. Opin. Nephrol. Hypertens. 2012, 21, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Santiago, J.J.; McNaughton, L.J.; Koleini, N.; Ma, X.; Bestvater, B.; Nickel, B.E.; Fandrich, R.R.; Wigle, J.T.; Freed, D.H.; Arora, R.C.; et al. High molecular weight fibroblast growth factor-2 in the human heart is a potential target for prevention of cardiac remodeling. PLoS ONE 2014, 9, e97281. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, B.J.; Molkentin, J.D. Calcium-calcineurin signaling in the regulation of cardiac hypertrophy. Biochem. Biophys. Res. Commun. 2004, 322, 1178–1191. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.H.; Khang-Loon, H. Carotid atherosclerosis. Definition, pathogenesis, and clinical significance. Neuroimaging Clin. N. Am. 1996, 6, 801–810. [Google Scholar] [PubMed]
- Chow, W.S.; Xu, A.; Woo, Y.C.; Tso, A.W.; Cheung, S.C.; Fong, C.H.; Tse, H.F.; Chau, M.T.; Cheung, B.M.; Lam, K.S. Serum fibroblast growth factor-21 levels are associated with carotid atherosclerosis independent of established cardiovascular risk factors. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 2454–2459. [Google Scholar] [CrossRef] [PubMed]
- Semba, R.D.; Crasto, C.; Strait, J.; Sun, K.; Schaumberg, D.A.; Ferrucci, L. Elevated serum fibroblast growth factor 21 is associated with hypertension in community-dwelling adults. J. Hum. Hypertens. 2013, 27, 397–399. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.J.; Hong, H.C.; Choi, H.Y.; Yoo, H.J.; Cho, G.J.; Hwang, T.G.; Baik, S.H.; Choi, D.S.; Kim, S.M.; Choi, K.M. Effects of a three-month combined exercise programme on fibroblast growth factor 21 and fetuin-A levels and arterial stiffness in obese women. Clin. Endocrinol. 2011, 75, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.Y.; Qin, L.; Baeyens, N.; Li, G.; Afolabi, T.; Budatha, M.; Tellides, G.; Schwartz, M.A.; Simons, M. Endothelial-to-mesenchymal transition drives atherosclerosis progression. J. Clin. Investig. 2015, 125, 4514–4528. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.Y.; Qin, L.; Li, G.; Tellides, G.; Simons, M. Smooth muscle FGF/TGFbeta cross talk regulates atherosclerosis progression. EMBO Mol. Med. 2016, 8, 712–728. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Wang, C.; Liu, L.; Li, Y.; Li, X.; Cai, J.; Wang, H. Effects of fibroblast growth factor 21 on cell damage in vitro and atherosclerosis in vivo. Can. J. Physiol. Pharmacol. 2014, 92, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Llaurado, G.; Megia, A.; Cano, A.; Gimenez-Palop, O.; Simon, I.; Gonzalez-Sastre, M.; Berlanga, E.; Fernandez-Veledo, S.; Vendrell, J.; Gonzalez-Clemente, J.M. FGF-23/Vitamin D Axis in Type 1 Diabetes: The Potential Role of Mineral Metabolism in Arterial Stiffness. PLoS ONE 2015, 10, e0140222. [Google Scholar] [CrossRef] [PubMed]
- Dimas, G.; Iliadis, F.; Tegos, T.; Spiroglou, S.; Kanellos, I.; Karamouzis, I.; Savopoulos, C.; Hatzitolios, A.; Grekas, D. 4a.05: Circulating Fgf-23 as an Independent Correlate of Hypertension and Atherosclerosis in Early Stages of Ckd. J. Hypertens. 2015, 33 (Suppl. S1), e50. [Google Scholar] [CrossRef] [PubMed]
- Akin, F.; Celik, O.; Altun, I.; Ayca, B.; Diker, V.O.; Satilmis, S.; Sahin, C. Relationship of fibroblast growth factor 23 and fetuin—A to coronary atherosclerosis. J. Diabetes Complicat. 2015, 29, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Feng, S.; Han, O.Y.; Shen, H.Y.; Jin, D.H.; Shi, Y.B. Role of fibroblast growth factor-23 in the pathogenesis of atherosclerosis in peritoneal dialysis patients. Genet. Mol. Res. 2015, 14, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Alonso, A.; Misialek, J.R.; Eckfeldt, J.H.; Selvin, E.; Coresh, J.; Chen, L.Y.; Soliman, E.Z.; Agarwal, S.K.; Lutsey, P.L. Circulating fibroblast growth factor-23 and the incidence of atrial fibrillation: The Atherosclerosis Risk in Communities study. J. Am. Heart Assoc. 2014, 3, e001082. [Google Scholar] [CrossRef] [PubMed]
- Mathew, J.S.; Sachs, M.C.; Katz, R.; Patton, K.K.; Heckbert, S.R.; Hoofnagle, A.N.; Alonso, A.; Chonchol, M.; Deo, R.; Ix, J.H.; et al. Fibroblast growth factor-23 and incident atrial fibrillation: The Multi-Ethnic Study of Atherosclerosis (MESA) and the Cardiovascular Health Study (CHS). Circulation 2014, 130, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Kestenbaum, B.; Sachs, M.C.; Hoofnagle, A.N.; Siscovick, D.S.; Ix, J.H.; Robinson-Cohen, C.; Lima, J.A.; Polak, J.F.; Blondon, M.; Ruzinski, J.; et al. Fibroblast growth factor-23 and cardiovascular disease in the general population: The Multi-Ethnic Study of Atherosclerosis. Circ. Heart Fail. 2014, 7, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C.Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef] [PubMed]
- Urakawa, I.; Yamazaki, Y.; Shimada, T.; Iijima, K.; Hasegawa, H.; Okawa, K.; Fujita, T.; Fukumoto, S.; Yamashita, T. Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature 2006, 444, 770–774. [Google Scholar] [CrossRef] [PubMed]
- Fliser, D.; Kollerits, B.; Neyer, U.; Ankerst, D.P.; Lhotta, K.; Lingenhel, A.; Ritz, E.; Kronenberg, F.; Group, M.S.; Kuen, E.; et al. Fibroblast growth factor 23 (FGF23) predicts progression of chronic kidney disease: The Mild to Moderate Kidney Disease (MMKD) Study. J. Am. Soc. Nephrol. 2007, 18, 2600–2608. [Google Scholar] [CrossRef] [PubMed]
- Isakova, T.; Xie, H.; Yang, W.; Xie, D.; Anderson, A.H.; Scialla, J.; Wahl, P.; Gutierrez, O.M.; Steigerwalt, S.; He, J.; et al. Fibroblast growth factor 23 and risks of mortality and end-stage renal disease in patients with chronic kidney disease. JAMA 2011, 305, 2432–2439. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, O.M.; Mannstadt, M.; Isakova, T.; Rauh-Hain, J.A.; Tamez, H.; Shah, A.; Smith, K.; Lee, H.; Thadhani, R.; Juppner, H.; et al. Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N. Engl. J. Med. 2008, 359, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Pavik, I.; Jaeger, P.; Ebner, L.; Wagner, C.A.; Petzold, K.; Spichtig, D.; Poster, D.; Wuthrich, R.P.; Russmann, S.; Serra, A.L. Secreted Klotho and FGF23 in chronic kidney disease Stage 1 to 5: A sequence suggested from a cross-sectional study. Nephrol. Dial. Transplant. 2013, 28, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Floege, J.; Kriz, W.; Schulze, M.; Susani, M.; Kerjaschki, D.; Mooney, A.; Couser, W.G.; Koch, K.M. Basic fibroblast growth factor augments podocyte injury and induces glomerulosclerosis in rats with experimental membranous nephropathy. J. Clin. Investig. 1995, 96, 2809–2819. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Nie, L.; He, T.; Yang, K.; Xiao, T.; Wang, S.; Huang, Y.; Zhang, J.; Wang, J.; Sharma, K.; et al. Klotho suppresses renal tubulo-interstitial fibrosis by controlling basic fibroblast growth factor-2 signalling. J. Pathol. 2014, 234, 560–572. [Google Scholar] [CrossRef] [PubMed]
- Rossaint, J.; Oehmichen, J.; Van Aken, H.; Reuter, S.; Pavenstadt, H.J.; Meersch, M.; Unruh, M.; Zarbock, A. FGF23 signaling impairs neutrophil recruitment and host defense during CKD. J. Clin. Investig. 2016, 126, 962–974. [Google Scholar] [CrossRef] [PubMed]
- Rossini, M.; Cheunsuchon, B.; Donnert, E.; Ma, L.J.; Thomas, J.W.; Neilson, E.G.; Fogo, A.B. Immunolocalization of fibroblast growth factor-1 (FGF-1), its receptor (FGFR-1), and fibroblast-specific protein-1 (FSP-1) in inflammatory renal disease. Kidney Int. 2005, 68, 2621–2628. [Google Scholar] [CrossRef] [PubMed]
- Silswal, N.; Touchberry, C.D.; Daniel, D.R.; McCarthy, D.L.; Zhang, S.; Andresen, J.; Stubbs, J.R.; Wacker, M.J. FGF23 directly impairs endothelium-dependent vasorelaxation by increasing superoxide levels and reducing nitric oxide bioavailability. Am. J. Physiol. Endocrinol. Metab. 2014, 307, E426–E436. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, J.; Ebert, T.; Bachmann, A.; Kralisch, S.; Lossner, U.; Kratzsch, J.; Stolzenburg, J.U.; Dietel, A.; Beige, J.; Anders, M.; et al. Serum levels of fibroblast growth factor-21 are increased in chronic and acute renal dysfunction. Clin. Endocrinol. 2014, 80, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Hines, E.A.; Sun, X. Tissue crosstalk in lung development. J. Cell. Biochem. 2014, 115, 1469–1477. [Google Scholar] [CrossRef] [PubMed]
- Volckaert, T.; Dill, E.; Campbell, A.; Tiozzo, C.; Majka, S.; Bellusci, S.; De Langhe, S.P. Parabronchial smooth muscle constitutes an airway epithelial stem cell niche in the mouse lung after injury. J. Clin. Investig. 2011, 121, 4409–4419. [Google Scholar] [CrossRef] [PubMed]
- Coffey, E.; Newman, D.R.; Sannes, P.L. Expression of fibroblast growth factor 9 in normal human lung and idiopathic pulmonary fibrosis. J. Histochem. Cytochem. 2013, 61, 671–679. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, B.; Korfei, M.; Henneke, I.; Sibinska, Z.; Tian, X.; Hezel, S.; Dilai, S.; Wasnick, R.; Schneider, B.; Wilhelm, J.; et al. Increased FGF1-FGFRc expression in idiopathic pulmonary fibrosis. Respir. Res. 2015, 16, 83. [Google Scholar] [CrossRef] [PubMed]
- Ramos, C.; Becerril, C.; Montano, M.; Garcia-De-Alba, C.; Ramirez, R.; Checa, M.; Pardo, A.; Selman, M. FGF-1 reverts epithelial-mesenchymal transition induced by TGF-{beta}1 through MAPK/ERK kinase pathway. Am. J. Physiol. Lung Cell. Mol. Physiol. 2010, 299, L222–L231. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, S.; Scotton, C.J.; McNulty, K.; Nye, E.; Stamp, G.; Laurent, G.; Bonnet, D.; Janes, S.M. Bone marrow stem cells expressing keratinocyte growth factor via an inducible lentivirus protects against bleomycin-induced pulmonary fibrosis. PLoS ONE 2009, 4, e8013. [Google Scholar] [CrossRef] [PubMed]
- Guzy, R.D.; Stoilov, I.; Elton, T.J.; Mecham, R.P.; Ornitz, D.M. Fibroblast growth factor 2 is required for epithelial recovery, but not for pulmonary fibrosis, in response to bleomycin. Am. J. Respir. Cell Mol. Biol. 2015, 52, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Joannes, A.; Brayer, S.; Besnard, V.; Marchal-Somme, J.; Jaillet, M.; Mordant, P.; Mal, H.; Borie, R.; Crestani, B.; Mailleux, A.A. FGF9 and FGF18 in idiopathic pulmonary fibrosis promote survival and migration and inhibit myofibroblast differentiation of human lung fibroblasts in vitro. Am. J. Physiol. Lung Cell Mol. Physiol. 2016, 310, L615–L629. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Shi, C.; Meng, X.; Zhang, K.; Li, X.; Wang, C.; Xiang, Z.; Hu, K.; Han, X. Inhibition of Wnt/beta-catenin signaling suppresses bleomycin-induced pulmonary fibrosis by attenuating the expression of TGF-beta1 and FGF-2. Exp. Mol. Pathol. 2016, 101, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Qu, Y.; Zhang, G.; Ji, Y.; Zhua, H.; Lv, C.; Jiang, W. Protective role of gambogic acid in experimental pulmonary fibrosis in vitro and in vivo. Phytomedicine 2016, 23, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Woodcock, H.V.; Maher, T.M. Nintedanib in idiopathic pulmonary fibrosis. Drugs Today 2015, 51, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Qu, Y.; Zhang, L.; Kang, Z.; Jiang, W.; Lv, C. Ponatinib ameliorates pulmonary fibrosis by suppressing TGF-beta1/Smad3 pathway. Pulm. Pharmacol. Ther. 2015, 34, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kumral, A.; Iscan, B.; Tuzun, F.; Micili, S.C.; Arslan, M.K.; Tugyan, K.; Duman, N.; Ozkan, H. Bacillus Calmette-Guerin vaccination: A novel therapeutic approach to preventing hyperoxic lung injury. J. Matern. Fetal Neonatal Med. 2015, 28, 1950–1956. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Ji, Y.; Kang, Z.; Lv, C.; Jiang, W. Protocatechuic aldehyde ameliorates experimental pulmonary fibrosis by modulating HMGB1/RAGE pathway. Toxicol. Appl. Pharmacol. 2015, 283, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Meyer, M.; Muller, A.K.; Bohm, F.; Grose, R.; Dauwalder, T.; Verrey, F.; Kopf, M.; Partanen, J.; Bloch, W.; et al. Fibroblast growth factor receptors 1 and 2 in keratinocytes control the epidermal barrier and cutaneous homeostasis. J. Cell Biol. 2010, 188, 935–952. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.; Ugarte, K.; Chen, N.; Yachi, P.; Fuchs, E.; Boismenu, R.; Havran, W.L. A role for skin gammadelta T cells in wound repair. Science 2002, 296, 747–749. [Google Scholar] [CrossRef] [PubMed]
- Gay, D.; Kwon, O.; Zhang, Z.; Spata, M.; Plikus, M.V.; Holler, P.D.; Ito, M.; Yang, Z.; Treffeisen, E.; Kim, C.D.; et al. Fgf9 from dermal gammadelta T cells induces hair follicle neogenesis after wounding. Nat. Med. 2013, 19, 916–923. [Google Scholar] [CrossRef] [PubMed]
- Werner, S.; Peters, K.G.; Longaker, M.T.; Fuller-Pace, F.; Banda, M.J.; Williams, L.T. Large induction of keratinocyte growth factor expression in the dermis during wound healing. Proc. Natl. Acad. Sci. USA 1992, 89, 6896–6900. [Google Scholar] [CrossRef] [PubMed]
- Casey-Sawicki, K.; Zhang, M.; Kim, S.; Zhang, A.; Zhang, S.B.; Zhang, Z.; Singh, R.; Yang, S.; Swarts, S.; Vidyasagar, S.; et al. A basic fibroblast growth factor analog for protection and mitigation against acute radiation syndromes. Health Phys. 2014, 106, 704–712. [Google Scholar] [CrossRef] [PubMed]
- Samy, R.P.; Kandasamy, M.; Gopalakrishnakone, P.; Stiles, B.G.; Rowan, E.G.; Becker, D.; Shanmugam, M.K.; Sethi, G.; Chow, V.T. Wound healing activity and mechanisms of action of an antibacterial protein from the venom of the eastern diamondback rattlesnake (Crotalus adamanteus). PLoS ONE 2014, 9, e80199. [Google Scholar] [CrossRef] [PubMed]
- Allen, S.J.; Watson, J.J.; Dawbarn, D. The neurotrophins and their role in Alzheimer’s disease. Curr. Neuropharmacol. 2011, 9, 559–573. [Google Scholar] [CrossRef] [PubMed]
- Cheng, B.; Mattson, M.P. Glucose deprivation elicits neurofibrillary tangle-like antigenic changes in hippocampal neurons: Prevention by NGF and bFGF. Exp. Neurol. 1992, 117, 114–123. [Google Scholar] [CrossRef]
- Johnson-Farley, N.N.; Patel, K.; Kim, D.; Cowen, D.S. Interaction of FGF-2 with IGF-1 and BDNF in stimulating Akt, ERK, and neuronal survival in hippocampal cultures. Brain Res. 2007, 1154, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Kiprianova, I.; Schindowski, K.; von Bohlen und Halbach, O.; Krause, S.; Dono, R.; Schwaninger, M.; Unsicker, K. Enlarged infarct volume and loss of BDNF mRNA induction following brain ischemia in mice lacking FGF-2. Exp. Neurol. 2004, 189, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Pinilla, F.; Cummings, B.J.; Cotman, C.W. Induction of basic fibroblast growth factor in Alzheimer’s disease pathology. Neuroreport 1990, 1, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Sasaki, H.; Katagiri, T.; Sasaki, H.; Koiwai, K.; Youki, H.; Totsuka, S.; Ishii, T. The binding of basic fibroblast growth factor to Alzheimer’s neurofibrillary tangles and senile plaques. Neurosci. Lett. 1991, 122, 33–36. [Google Scholar] [CrossRef]
- Stieber, A.; Mourelatos, Z.; Gonatas, N.K. In Alzheimer’s disease the Golgi apparatus of a population of neurons without neurofibrillary tangles is fragmented and atrophic. Am. J. Pathol. 1996, 148, 415–426. [Google Scholar] [PubMed]
- Hanneken, A.; Frautschy, S.; Galasko, D.; Baird, A. A fibroblast growth factor binding protein in human cerebral spinal fluid. Neuroreport 1995, 6, 886–888. [Google Scholar] [CrossRef] [PubMed]
- Cummings, B.J.; Su, J.H.; Cotman, C.W. Neuritic involvement within bFGF immunopositive plaques of Alzheimer’s disease. Exp. Neurol. 1993, 124, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Takami, K.; Matsuo, A.; Terai, K.; Walker, D.G.; McGeer, E.G.; McGeer, P.L. Fibroblast growth factor receptor-1 expression in the cortex and hippocampus in Alzheimer’s disease. Brain Res. 1998, 802, 89–97. [Google Scholar] [CrossRef]
- Gong, C.X.; Lidsky, T.; Wegiel, J.; Zuck, L.; Grundke-Iqbal, I.; Iqbal, K. Phosphorylation of microtubule-associated protein tau is regulated by protein phosphatase 2A in mammalian brain. Implications for neurofibrillary degeneration in Alzheimer’s disease. J. Biol. Chem. 2000, 275, 5535–5544. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, K.; Liu, F.; Gong, C.X.; Grundke-Iqbal, I. Tau in Alzheimer disease and related tauopathies. Curr. Alzheimer Res. 2010, 7, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Burack, M.A.; Halpain, S. Site-specific regulation of Alzheimer-like tau phosphorylation in living neurons. Neuroscience 1996, 72, 167–184. [Google Scholar] [CrossRef]
- Butt, A.M.; Dinsdale, J. Fibroblast growth factor 2 mediated disruption of myelin-forming oligodendrocytes in vivo is associated with increased tau immunoreactivity. Neurosci. Lett. 2005, 375, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Tatebayashi, Y.; Lee, M.H.; Li, L.; Iqbal, K.; Grundke-Iqbal, I. The dentate gyrus neurogenesis: A therapeutic target for Alzheimer’s disease. Acta Neuropathol. 2003, 105, 225–232. [Google Scholar] [PubMed]
- Tatebayashi, Y.; Haque, N.; Tung, Y.C.; Iqbal, K.; Grundke-Iqbal, I. Role of tau phosphorylation by glycogen synthase kinase-3beta in the regulation of organelle transport. J. Cell Sci. 2004, 117 Pt 9, 1653–1663. [Google Scholar] [CrossRef] [PubMed]
- Hong, X.P.; Chen, T.; Yin, N.N.; Han, Y.M.; Yuan, F.; Duan, Y.J.; Shen, F.; Zhang, Y.H.; Chen, Z.B. Puerarin Ameliorates D-Galactose Induced Enhanced Hippocampal Neurogenesis and Tau Hyperphosphorylation in Rat Brain. J. Alzheimers Dis. 2016, 51, 605–617. [Google Scholar] [CrossRef] [PubMed]
- Ogino, R.; Murayama, N.; Noshita, T.; Takemoto, N.; Toba, T.; Oka, T.; Narii, N.; Yoshida, S.; Ueno, N.; Inoue, T. SUN11602 has basic fibroblast growth factor-like activity and attenuates neuronal damage and cognitive deficits in a rat model of Alzheimer’s disease induced by amyloid beta and excitatory amino acids. Brain Res. 2014, 1585, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.W.; Lahiri, D.K. Regulation of promoter activity of the APP gene by cytokines and growth factors: Implications in Alzheimer’s disease. Ann. N.Y. Acad. Sci. 2002, 973, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Rossner, S.; Ueberham, U.; Schliebs, R.; Perez-Polo, J.R.; Bigl, V. Neurotrophin binding to the p75 neurotrophin receptor is necessary but not sufficient to mediate NGF-effects on APP secretion in PC-12 cells. J. Neural Transm. Suppl. 1998, 54, 279–285. [Google Scholar] [PubMed]
- Araujo, D.M.; Cotman, C.W. Beta-amyloid stimulates glial cells in vitro to produce growth factors that accumulate in senile plaques in Alzheimer’s disease. Brain Res. 1992, 569, 141–145. [Google Scholar] [CrossRef]
- Carlson, G.A.; Borchelt, D.R.; Dake, A.; Turner, S.; Danielson, V.; Coffin, J.D.; Eckman, C.; Meiners, J.; Nilsen, S.P.; Younkin, S.G.; et al. Genetic modification of the phenotypes produced by amyloid precursor protein overexpression in transgenic mice. Hum. Mol. Genet. 1997, 6, 1951–1959. [Google Scholar] [CrossRef] [PubMed]
- Mashayekhi, F.; Hadavi, M.; Vaziri, H.R.; Naji, M. Increased acidic fibroblast growth factor concentrations in the serum and cerebrospinal fluid of patients with Alzheimer’s disease. J. Clin. Neurosci. 2010, 17, 357–359. [Google Scholar] [CrossRef] [PubMed]
- Joyce, N.C. Proliferative capacity of the corneal endothelium. Prog. Retin. Eye Res. 2003, 22, 359–389. [Google Scholar] [CrossRef]
- Kay, E.P.; Gu, X.; Ninomiya, Y.; Smith, R.E. Corneal endothelial modulation: A factor released by leukocytes induces basic fibroblast growth factor that modulates cell shape and collagen. Investig. Ophthalmol. Vis. Sci. 1993, 34, 663–672. [Google Scholar]
- Waring, G.O., III. Posterior collagenous layer of the cornea. Ultrastructural classification of abnormal collagenous tissue posterior to Descemet’s membrane in 30 cases. Arch. Ophthalmol. 1982, 100, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G.; Kay, E.P. Two populations of p27 use differential kinetics to phosphorylate Ser-10 and Thr-187 via phosphatidylinositol 3-Kinase in response to fibroblast growth factor-2 stimulation. J. Biol. Chem. 2007, 282, 6444–6454. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G.; Kay, E.P. Involvement of two distinct ubiquitin E3 ligase systems for p27 degradation in corneal endothelial cells. Investig. Ophthalmol. Vis. Sci. 2008, 49, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Ko, M.K.; Kay, E.P. Regulatory role of FGF-2 on type I collagen expression during endothelial mesenchymal transformation. Investig. Ophthalmol. Vis. Sci. 2005, 46, 4495–4503. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G.; Kay, E.P. Common and distinct pathways for cellular activities in FGF-2 signaling induced by IL-1beta in corneal endothelial cells. Investig. Ophthalmol. Vis. Sci. 2009, 50, 2067–2076. [Google Scholar] [CrossRef] [PubMed]
- Song, J.S.; Lee, J.G.; Kay, E.P. Induction of FGF-2 synthesis by IL-1beta in aqueous humor through P13-kinase and p38 in rabbit corneal endothelium. Investig. Ophthalmol. Vis. Sci. 2010, 51, 822–829. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhou, X.; Ma, J.; Tian, H.; Jiao, Y.; Zhang, R.; Huang, Z.; Xiao, J.; Zhao, B.; Qian, H.; et al. Effects of keratinocyte growth factor-2 on corneal epithelial wound healing in a rabbit model of carbon dioxide laser injury. Biol. Pharm. Bull. 2010, 33, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Yancopoulos, G.D.; Davis, S.; Gale, N.W.; Rudge, J.S.; Wiegand, S.J.; Holash, J. Vascular-specific growth factors and blood vessel formation. Nature 2000, 407, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Suri, C.; Jones, P.F.; Patan, S.; Bartunkova, S.; Maisonpierre, P.C.; Davis, S.; Sato, T.N.; Yancopoulos, G.D. Requisite role of angiopoietin-1, a ligand for the TIE2 receptor, during embryonic angiogenesis. Cell 1996, 87, 1171–1180. [Google Scholar] [CrossRef]
- Wu, X.; Liu, N. The role of Ang/Tie signaling in lymphangiogenesis. Lymphology 2010, 43, 59–72. [Google Scholar] [PubMed]
- Davis, S.; Aldrich, T.H.; Jones, P.F.; Acheson, A.; Compton, D.L.; Jain, V.; Ryan, T.E.; Bruno, J.; Radziejewski, C.; Maisonpierre, P.C.; et al. Isolation of angiopoietin-1, a ligand for the TIE2 receptor, by secretion-trap expression cloning. Cell 1996, 87, 1161–1169. [Google Scholar] [CrossRef]
- Maisonpierre, P.C.; Suri, C.; Jones, P.F.; Bartunkova, S.; Wiegand, S.J.; Radziejewski, C.; Compton, D.; McClain, J.; Aldrich, T.H.; Papadopoulos, N.; et al. Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science 1997, 277, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Partanen, J.; Dumont, D.J. Functions of Tie1 and Tie2 receptor tyrosine kinases in vascular development. Curr. Top. Microbiol. Immunol. 1999, 237, 159–172. [Google Scholar] [PubMed]
- DeBusk, L.M.; Chen, Y.; Nishishita, T.; Chen, J.; Thomas, J.W.; Lin, P.C. Tie2 receptor tyrosine kinase, a major mediator of tumor necrosis factor alpha-induced angiogenesis in rheumatoid arthritis. Arthritis Rheumatol. 2003, 48, 2461–2471. [Google Scholar] [CrossRef] [PubMed]
- Takahara, K.; Iioka, T.; Furukawa, K.; Uchida, T.; Nakashima, M.; Tsukazaki, T.; Shindo, H. Autocrine/paracrine role of the angiopoietin-1 and -2/Tie2 system in cell proliferation and chemotaxis of cultured fibroblastic synoviocytes in rheumatoid arthritis. Hum. Pathol. 2004, 35, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Scott, B.B.; Zaratin, P.F.; Gilmartin, A.G.; Hansbury, M.J.; Colombo, A.; Belpasso, C.; Winkler, J.D.; Jackson, J.R. TNF-alpha modulates angiopoietin-1 expression in rheumatoid synovial fibroblasts via the NF-kappa B signalling pathway. Biochem. Biophys. Res. Commun. 2005, 328, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Hashiramoto, A.; Sakai, C.; Yoshida, K.; Tsumiyama, K.; Miura, Y.; Shiozawa, K.; Nose, M.; Komai, K.; Shiozawa, S. Angiopoietin 1 directly induces destruction of the rheumatoid joint by cooperative, but independent, signaling via ERK/MAPK and phosphatidylinositol 3-kinase/Akt. Arthritis Rheumatol. 2007, 56, 2170–2179. [Google Scholar] [CrossRef] [PubMed]
- Kurosaka, D.; Hirai, K.; Nishioka, M.; Miyamoto, Y.; Yoshida, K.; Noda, K.; Ukichi, T.; Yanagimachi, M.; Furuya, K.; Takahashi, E.; et al. Clinical significance of serum levels of vascular endothelial growth factor, angiopoietin-1, and angiopoietin-2 in patients with rheumatoid arthritis. J. Rheumatol. 2010, 37, 1121–1128. [Google Scholar] [CrossRef] [PubMed]
- Krausz, S.; Garcia, S.; Ambarus, C.A.; de Launay, D.; Foster, M.; Naiman, B.; Iverson, W.; Connor, J.R.; Sleeman, M.A.; Coyle, A.J.; et al. Angiopoietin-2 promotes inflammatory activation of human macrophages and is essential for murine experimental arthritis. Ann. Rheum. Dis. 2012, 71, 1402–1410. [Google Scholar] [CrossRef] [PubMed]
- Kanakaraj, P.; Puffer, B.A.; Yao, X.T.; Kankanala, S.; Boyd, E.; Shah, R.R.; Wang, G.; Patel, D.; Krishnamurthy, R.; Kaithamana, S.; et al. Simultaneous targeting of TNF and Ang2 with a novel bispecific antibody enhances efficacy in an in vivo model of arthritis. mAbs 2012, 4, 600–613. [Google Scholar] [CrossRef] [PubMed]
- Tasaki, Y.; Shimizu, M.; Inoue, N.; Mizuta, M.; Nakagishi, Y.; Wada, T.; Yachie, A. Disruption of vascular endothelial homeostasis in systemic juvenile idiopathic arthritis-associated macrophage activation syndrome: The dynamic roles of angiopoietin-1 and -2. Cytokine 2016, 80, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wolfram, J.A.; Diaconu, D.; Hatala, D.A.; Rastegar, J.; Knutsen, D.A.; Lowther, A.; Askew, D.; Gilliam, A.C.; McCormick, T.S.; Ward, N.L. Keratinocyte but not endothelial cell-specific overexpression of Tie2 leads to the development of psoriasis. Am. J. Pathol. 2009, 174, 1443–1458. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Xie, H.; Ji, J.; Zhou, X.; Goltzman, D.; Miao, D. Defective female reproductive function in 1,25(OH)2D-deficient mice results from indirect effect mediated by extracellular calcium and/or phosphorus. Am. J. Physiol. Endocrinol. Metab. 2010, 299, E928–E935. [Google Scholar] [CrossRef] [PubMed]
- Tal, R.; Seifer, D.B.; Grazi, R.V.; Malter, H.E. Angiopoietin-1 and angiopoietin-2 are altered in polycystic ovarian syndrome (PCOS) during controlled ovarian stimulation. Vasc. Cell 2013, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Scotti, L.; Abramovich, D.; Pascuali, N.; Durand, L.H.; Irusta, G.; de Zuniga, I.; Tesone, M.; Parborell, F. Inhibition of angiopoietin-1 (ANGPT1) affects vascular integrity in ovarian hyperstimulation syndrome (OHSS). Reprod. Fertil. Dev. 2016, 28, 690–699. [Google Scholar] [CrossRef] [PubMed]
- Hilbert, T.; Klaschik, S. The angiopoietin/TIE receptor system: Focusing its role for ischemia-reperfusion injury. Cytokine Growth Factor Rev. 2015, 26, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Novotny, N.M.; Lahm, T.; Markel, T.A.; Crisostomo, P.R.; Wang, M.; Wang, Y.; Tan, J.; Meldrum, D.R. Angiopoietin-1 in the treatment of ischemia and sepsis. Shock 2009, 31, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Chopp, M. Vascular endothelial growth factor and angiopoietins in focal cerebral ischemia. Trends Cardiovasc. Med. 2002, 12, 62–66. [Google Scholar] [CrossRef]
- Thorin-Trescases, N.; Thorin, E. Angiopoietin-like-2: A multifaceted protein with physiological and pathophysiological properties. Expert Rev. Mol. Med. 2014, 16, e17. [Google Scholar] [CrossRef] [PubMed]
- Kadomatsu, T.; Endo, M.; Miyata, K.; Oike, Y. Diverse roles of ANGPTL2 in physiology and pathophysiology. Trends Endocrinol. Metab. 2014, 25, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.J.; Teo, Z.; Sng, M.K.; Zhu, P.; Tan, N.S. Emerging roles of angiopoietin-like 4 in human cancer. Mol. Cancer Res. 2012, 10, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Zhu, P.; Goh, Y.Y.; Chin, H.F.; Kersten, S.; Tan, N.S. Angiopoietin-like 4: A decade of research. Biosci. Rep. 2012, 32, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Kadomatsu, T.; Tabata, M.; Oike, Y. Angiopoietin-like proteins: Emerging targets for treatment of obesity and related metabolic diseases. FEBS J. 2011, 278, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Oike, Y.; Tabata, M. Angiopoietin-like proteins—Potential therapeutic targets for metabolic syndrome and cardiovascular disease. Circ. J. 2009, 73, 2192–2197. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.C.; Chiang, W.C.; Tsai, M.H.; Chou, Y.H.; Pan, S.Y.; Chang, Y.T.; Yeh, P.Y.; Chen, Y.T.; Chiang, C.K.; Chen, Y.M.; et al. Angiopoietin-2-induced arterial stiffness in CKD. J. Am. Soc. Nephrol. 2014, 25, 1198–1209. [Google Scholar] [CrossRef] [PubMed]
- Joussen, A.M.; Poulaki, V.; Tsujikawa, A.; Qin, W.; Qaum, T.; Xu, Q.; Moromizato, Y.; Bursell, S.E.; Wiegand, S.J.; Rudge, J.; et al. Suppression of diabetic retinopathy with angiopoietin-1. Am. J. Pathol. 2002, 160, 1683–1693. [Google Scholar] [CrossRef]
- Hammes, H.P.; Lin, J.; Wagner, P.; Feng, Y.; Vom Hagen, F.; Krzizok, T.; Renner, O.; Breier, G.; Brownlee, M.; Deutsch, U. Angiopoietin-2 causes pericyte dropout in the normal retina: Evidence for involvement in diabetic retinopathy. Diabetes 2004, 53, 1104–1110. [Google Scholar] [CrossRef] [PubMed]
- Pfister, F.; Wang, Y.; Schreiter, K.; vom Hagen, F.; Altvater, K.; Hoffmann, S.; Deutsch, U.; Hammes, H.P.; Feng, Y. Retinal overexpression of angiopoietin-2 mimics diabetic retinopathy and enhances vascular damages in hyperglycemia. Acta Diabetol. 2010, 47, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Rangasamy, S.; Srinivasan, R.; Maestas, J.; McGuire, P.G.; Das, A. A potential role for angiopoietin 2 in the regulation of the blood-retinal barrier in diabetic retinopathy. Investig. Ophthalmol. Vis. Sci. 2011, 52, 3784–3791. [Google Scholar] [CrossRef] [PubMed]
- Park, S.W.; Yun, J.H.; Kim, J.H.; Kim, K.W.; Cho, C.H.; Kim, J.H. Angiopoietin 2 induces pericyte apoptosis via alpha3beta1 integrin signaling in diabetic retinopathy. Diabetes 2014, 63, 3057–3068. [Google Scholar] [CrossRef] [PubMed]
- Cahoon, J.M.; Rai, R.R.; Carroll, L.S.; Uehara, H.; Zhang, X.; O’Neil, C.L.; Medina, R.J.; Das, S.K.; Muddana, S.K.; Olson, P.R.; et al. Intravitreal AAV2.COMP-Ang1 Prevents Neurovascular Degeneration in a Murine Model of Diabetic Retinopathy. Diabetes 2015, 64, 4247–4259. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.H.; Park, S.W.; Kim, J.H.; Park, Y.J.; Cho, C.H.; Kim, J.H. Angiopoietin 2 induces astrocyte apoptosis via alphavbeta5-integrin signaling in diabetic retinopathy. Cell Death Dis 2016, 7, e2101. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kim, W.; Moon, S.O.; Sung, M.J.; Kim, D.H.; Kang, K.P.; Jang, K.Y.; Lee, S.Y.; Park, B.H.; Koh, G.Y.; et al. Renoprotective effect of COMP-angiopoietin-1 in db/db mice with type 2 diabetes. Nephrol. Dial. Transplant. 2007, 22, 396–408. [Google Scholar] [CrossRef] [PubMed]
- Davis, B.; Dei Cas, A.; Long, D.A.; White, K.E.; Hayward, A.; Ku, C.H.; Woolf, A.S.; Bilous, R.; Viberti, G.; Gnudi, L. Podocyte-specific expression of angiopoietin-2 causes proteinuria and apoptosis of glomerular endothelia. J. Am. Soc. Nephrol. 2007, 18, 2320–2329. [Google Scholar] [CrossRef] [PubMed]
- Dessapt-Baradez, C.; Woolf, A.S.; White, K.E.; Pan, J.; Huang, J.L.; Hayward, A.A.; Price, K.L.; Kolatsi-Joannou, M.; Locatelli, M.; Diennet, M.; et al. Targeted glomerular angiopoietin-1 therapy for early diabetic kidney disease. J. Am. Soc. Nephrol. 2014, 25, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Li, T.; Zhang, C.; Chen, Q.; Li, Z.; Liu, J.; Wang, Y. Therapeutic effect of alprostadil in diabetic nephropathy: Possible roles of angiopoietin-2 and IL-18. Cell. Physiol. Biochem. 2014, 34, 916–928. [Google Scholar] [CrossRef] [PubMed]
- Khairoun, M.; van den Heuvel, M.; van den Berg, B.M.; Sorop, O.; de Boer, R.; van Ditzhuijzen, N.S.; Bajema, I.M.; Baelde, H.J.; Zandbergen, M.; Duncker, D.J.; et al. Early systemic microvascular damage in pigs with atherogenic diabetes mellitus coincides with renal angiopoietin dysbalance. PLoS ONE 2015, 10, e0121555. [Google Scholar] [CrossRef] [PubMed]
- David, S.; Kumpers, P.; Lukasz, A.; Fliser, D.; Martens-Lobenhoffer, J.; Bode-Boger, S.M.; Kliem, V.; Haller, H.; Kielstein, J.T. Circulating angiopoietin-2 levels increase with progress of chronic kidney disease. Nephrol. Dial. Transplant. 2010, 25, 2571–2576. [Google Scholar] [CrossRef] [PubMed]
- David, S.; John, S.G.; Jefferies, H.J.; Sigrist, M.K.; Kumpers, P.; Kielstein, J.T.; Haller, H.; McIntyre, C.W. Angiopoietin-2 levels predict mortality in CKD patients. Nephrol. Dial. Transplant. 2012, 27, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.C.; Lai, T.S.; Chiang, C.K.; Chen, Y.M.; Wu, M.S.; Chu, T.S.; Wu, K.D.; Lin, S.L. Angiopoietin-2 is associated with albuminuria and microinflammation in chronic kidney disease. PLoS ONE 2013, 8, e54668. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.C.; Chiu, Y.W.; Tsai, J.C.; Kuo, H.T.; Lee, S.C.; Hung, C.C.; Lin, M.Y.; Hwang, S.J.; Kuo, M.C.; Chen, H.C. Association of angiopoietin-2 with renal outcome in chronic kidney disease. PLoS ONE 2014, 9, e108862. [Google Scholar] [CrossRef] [PubMed]
- Bi, X.; Niu, J.; Ding, W.; Zhang, M.; Yang, M.; Gu, Y. Angiopoietin-1 attenuates angiotensin II-induced ER stress in glomerular endothelial cells via a Tie2 receptor/ERK1/2-p38 MAPK-dependent mechanism. Mol. Cell. Endocrinol. 2016, 428, 118–132. [Google Scholar] [CrossRef] [PubMed]
- Koutroubakis, I.E.; Xidakis, C.; Karmiris, K.; Sfiridaki, A.; Kandidaki, E.; Kouroumalis, E.A. Potential role of soluble angiopoietin-2 and Tie2 in patients with inflammatory bowel disease. Eur. J. Clin. Investig. 2006, 36, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Ganta, V.C.; Cromer, W.; Mills, G.L.; Traylor, J.; Jennings, M.; Daley, S.; Clark, B.; Mathis, J.M.; Bernas, M.; Boktor, M.; et al. Angiopoietin-2 in experimental colitis. Inflamm. Bowel Dis. 2010, 16, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Oikonomou, K.A.; Kapsoritakis, A.N.; Kapsoritaki, A.I.; Manolakis, A.C.; Tiaka, E.K.; Tsiopoulos, F.D.; Tsiompanidis, I.A.; Potamianos, S.P. Angiogenin, angiopoietin-1, angiopoietin-2, and endostatin serum levels in inflammatory bowel disease. Inflamm. Bowel Dis. 2011, 17, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Algaba, A.; Linares, P.M.; Encarnacion Fernandez-Contreras, M.; Figuerola, A.; Calvet, X.; Guerra, I.; de Pousa, I.; Chaparro, M.; Gisbert, J.P.; Bermejo, F. The effects of infliximab or adalimumab on vascular endothelial growth factor and angiopoietin 1 angiogenic factor levels in inflammatory bowel disease: Serial observations in 37 patients. Inflamm. Bowel Dis. 2014, 20, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.X.; Gu, S.Z.; Zhang, S.; Ren, Y.; Sang, L.X.; Dai, C. Angiopoietin and vascular endothelial growth factor expression in colorectal disease models. World J. Gastroenterol. 2015, 21, 2645–2650. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.D.; Campbell, A.I.; Robb, M.; Ng, D.; Stewart, D.J. Protective role of angiopoietin-1 in experimental pulmonary hypertension. Circ. Res. 2003, 92, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, C.C.; Du, L.; Chu, D.; Cho, A.J.; Kido, M.; Wolf, P.L.; Jamieson, S.W.; Thistlethwaite, P.A. Induction of pulmonary hypertension by an angiopoietin 1/TIE2/serotonin pathway. Proc. Natl. Acad. Sci. USA 2003, 100, 12331–12336. [Google Scholar] [CrossRef] [PubMed]
- Dewachter, L.; Adnot, S.; Fadel, E.; Humbert, M.; Maitre, B.; Barlier-Mur, A.M.; Simonneau, G.; Hamon, M.; Naeije, R.; Eddahibi, S. Angiopoietin/Tie2 pathway influences smooth muscle hyperplasia in idiopathic pulmonary hypertension. Am. J. Respir. Crit. Care Med. 2006, 174, 1025–1033. [Google Scholar] [CrossRef] [PubMed]
- Kugathasan, L.; Ray, J.B.; Deng, Y.; Rezaei, E.; Dumont, D.J.; Stewart, D.J. The angiopietin-1-Tie2 pathway prevents rather than promotes pulmonary arterial hypertension in transgenic mice. J. Exp. Med. 2009, 206, 2221–2234. [Google Scholar] [CrossRef] [PubMed]
- Kumpers, P.; Nickel, N.; Lukasz, A.; Golpon, H.; Westerkamp, V.; Olsson, K.M.; Jonigk, D.; Maegel, L.; Bockmeyer, C.L.; David, S.; et al. Circulating angiopoietins in idiopathic pulmonary arterial hypertension. Eur. Heart J. 2010, 31, 2291–2300. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Kim, H.S. Serial changes of serum endostatin and angiopoietin-1 levels in preterm infants with severe bronchopulmonary dysplasia and subsequent pulmonary artery hypertension. Neonatology 2014, 106, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, K.; Sapadin, A.; Shoji, T.; Fleischmajer, R.; Lebwohl, M. Altered expression of angiopoietins and Tie2 endothelium receptor in psoriasis. J. Investig. Dermatol. 2001, 116, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Markham, T.; Mullan, R.; Goldesn-Mason, L.; Rogers, S.; Bresnihan, B.; Fitzgerald, O.; Fearon, U.; Veale, D.J. Resolution of endothelial activation and down-regulation of Tie2 receptor in psoriatic skin after infliximab therapy. J. Am. Acad. Dermatol. 2006, 54, 1003–1012. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).