Abstract
Symptoms of depression represent a significant burden to patients with breast cancer, not only because of the psychological stress associated with their diagnosis, but also because of the adverse effects of its treatment. We reviewed the clinical trials examining the management of the symptoms of depression in breast cancer patients through different non-pharmacological interventions in different databases (PubMed, Embase, Scopus, and the American Psychological Association). Cognitive behavioural therapy, interpersonal psychotherapy or psychodynamic psychotherapy, as well as acceptance and commitment therapy have been effective in improving symptoms of depression in cancer patients with moderate to severe symptoms. Physical exercise, yoga, mindfulness, and support groups have been shown to benefit patients with mild depressive symptoms. These interventions not only showed positive results in interventions in women with breast cancer in terms of the symptoms of depression, but also highlighted their benefits for comorbid anxiety, stress, and poor sleep quality; moreover, it is suggested that these interventions should be leveraged to manage mental health issues in breast cancer patients. The molecular effects of these interventions, such as the reduction in inflammatory cytokines and cortisol levels, have seldom been reported and need further studies.
Keywords:
depression; chemotherapy; oestrogens; progesterone; mood; sleep; quality of life; yoga; mindfulness 1. Introduction
Breast cancer (BC) is the most common type of cancer diagnosed in women and one of the main causes of mortality from this disease in this population [1]. Despite advances in cancer treatments and the resulting lower mortality rates, this type of cancer remains a serious public health problem. In part, this is because of the multiple debilitating symptoms that arise because of the surgery, chemotherapy, radiotherapy (RT), and/or biological therapy used to treat this disease [2]. Evidence suggests there is a robust, causal relationship between stressful life events and depression [3]. BC survivors tend to experience an increase in depression symptoms following their diagnosis [4] and often experience adverse physical and psychological symptoms that can persist for years after completing treatment, negatively affecting both their quality of life and health functionality [5,6].
Women who have faced BC report a series of symptoms, either as a direct consequence of the disease or as side effects of the treatment [7]. The psychological symptoms include stress, anxiety, depression, fear of recurrence, and impaired cognitive functioning [8], while the physical symptoms include pain, fatigue, and sleep disorders [8]. Symptoms of depression are common in patients with BC, with the prevalence of clinically significant symptoms reaching up to 46% [9]. These rates are at least double those observed in women in the general population. Indeed, a cohort study of 40,849 Swedish women with BC found that patients with invasive cancer had a 60% higher risk of developing depression and anxiety within 10 years of diagnosis, compared to the general female population [10]. Symptoms of depression are associated with several negative consequences, including an increased risk of suicide, functional impairment, lack of treatment adherence, and prolonged hospital stays [11]. In this sense, a population-based cohort study that assessed the risk of various adverse mental health outcomes in women with a history of BC compared to women who had never had the disease revealed that survival was positively associated with anxiety and depression [12].
Consequently, BC patients face a high risk of depression, highlighting the need for specialised care and a strong support system [13]. Non-pharmacological interventions represent therapeutic approaches that dispense with the use of medications [14]. They are crucial for various reasons, as they not only relieve physical and psychological symptoms, such as anxiety, depression, and stress, but also improve quality of life through the implementation of psychological therapies, such as cognitive behavioural therapy (CBT) [15,16,17], emotional and social support through support groups [18,19], relaxation and mindfulness techniques [20,21,22], supervised physical exercise [23,24], and occupational therapy, among other strategies designed to promote the emotional and psychological well-being of patients [25]. Non-pharmacological interventions are fundamental to a holistic approach in the treatment of depression in women with BC, providing emotional, psychological, and physical benefits that complement and improve the outcomes of conventional medical treatment.
Carrying out this review of the clinical trial literature is justified by the need to update and expand the existing evidence on non-pharmacological interventions for depressive symptoms in women with BC. There is a previous systematic review and meta-analysis on randomised controlled trials (RCTs) that covered studies up to 2017 [26]. The results of this meta-analysis showed that psychotherapy and yoga, or spiritual growth techniques combined with physical activity treatments, are useful in reducing depressive symptoms in women with non-metastatic BC, whether on active or recently completed BC treatment. However, this meta-analysis does not specify the severity of depressive symptoms in that population. Our review covered clinical trials conducted in the last 10 years to the current date and included women with localised or metastatic BC. The women included in the studies were at different stages of the disease: some were in active treatment, others had completed treatment, and some were survivors. Both those with mild to severe depressive symptoms and those with a clinical diagnosis of depression were considered. This update is essential to provide a more complete and updated view on the effectiveness of non-pharmacological interventions in this population. The inclusion of recent studies will allow us to identify new strategies or approaches that could be more effective in the treatment of depression in women with BC, regardless of the severity of symptoms. In addition, this review seeks to answer key research questions, such as this one: What scientific evidence supports the effects of non-pharmacological treatments in reducing depressive symptoms in women with breast cancer? In addition, secondary questions will be explored, such as this one: What is the comparative effectiveness of different non-pharmacological therapies according to the severity of depressive symptoms in these patients?
The findings of this review will be of great relevance to clinical practice, as they will provide updated evidence that will guide health professionals towards the most effective interventions to improve the emotional well-being and quality of life of these patients.
2. Materials and Methods
2.1. Literature Search
To ensure a comprehensive overview, we conducted a comprehensive literature search that included controlled trials and spanned multiple databases, including PubMed, Embase, Scopus, and those of the American Psychological Association (APA). This search was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
To ensure the completeness of the search, we used keywords such as “breast cancer”, “depression symptoms”, “depression”, “hormones”, “chemotherapy”, “psychological symptoms”, and “clinical trials”. The searches covered publications from 2010 to 2024.
2.2. Inclusion and Exclusion Criteria
The following inclusion criteria were applied: (1) interventions based on non-pharmacological therapies; (2) assessment of psychological symptoms such as anxiety, depression or stress; (3) study design: clinical trials; (4) language: studies published in English or Spanish; (5) accessibility: studies with full text available.
On the other hand, studies were excluded if (1) they evaluated only pharmacological treatments or surgeries without combination with non-pharmacological therapies; (2) they were case reports, narrative reviews, editorials, abstracts or conference proceedings; (3) they did not present clinically relevant results; (4) they were published in languages other than English or Spanish with no translation available; (5) they did not have access to the full text.
2.3. Analysis of Selected Studies
The results of the database search were imported into Mendeley, a web platform used to manage the selection process and eliminate duplicate citations. All identified articles were reviewed in detail, starting with an analysis of their abstract to assess their relevance. In addition to electronic search, a manual search was performed on the references of the retrieved articles to ensure the inclusion of all relevant studies.
Relevant data were extracted and recorded in a previously designed standardised table, which included information such as author, study design, year of publication, country of origin, participants, research objectives, and main findings.
3. Results
3.1. Study Design and Sample Characteristics
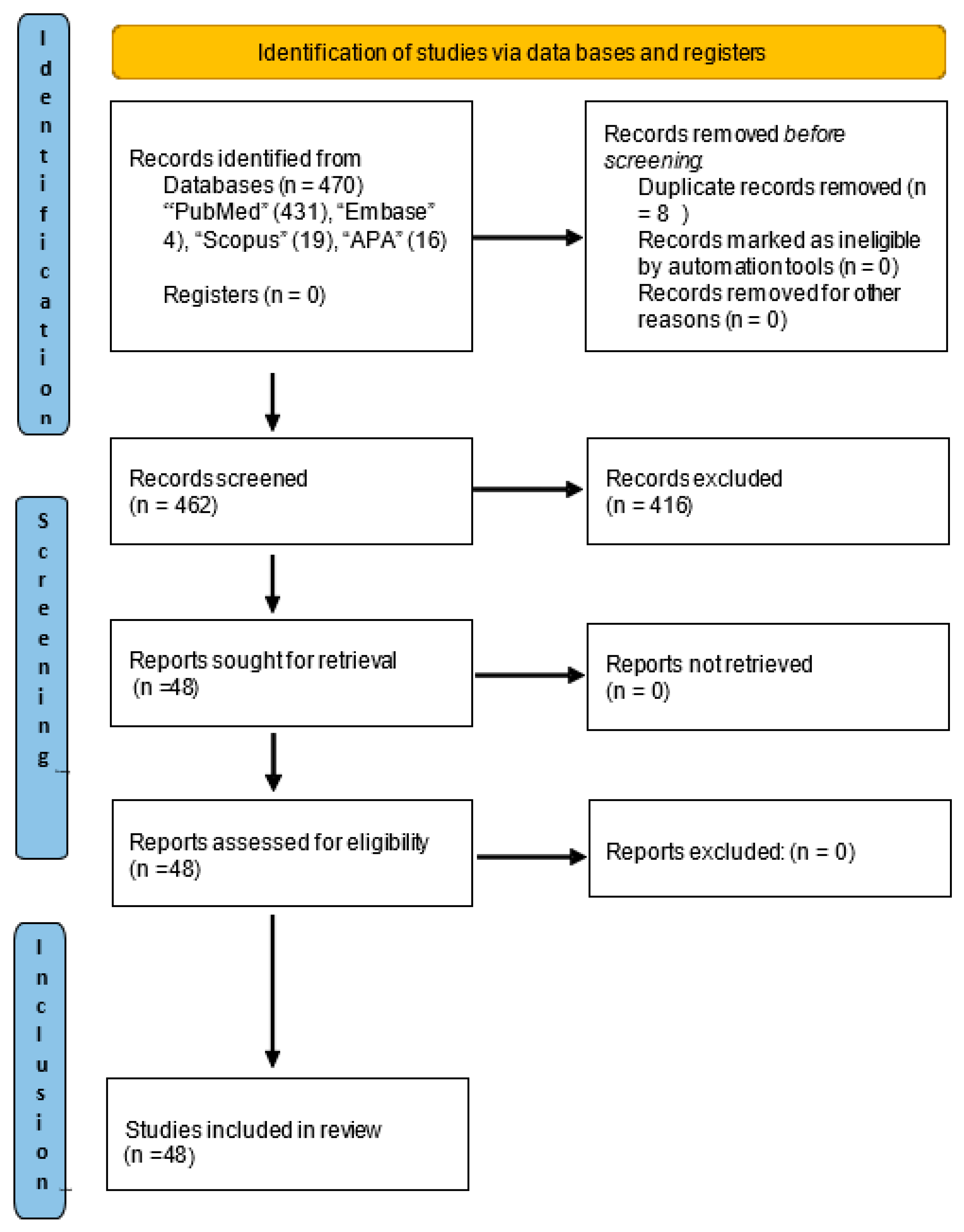
Forty-eight relevant studies were identified, the selection process for which is detailed in the PRISMA flowchart (Figure 1). In addition, a manual search was performed in the reference list of the selected studies, which allowed the identification of two additional articles [20,23]. In total, these studies included 3920 women and assessed the effects of various interventions designed to reduce symptoms of depression in patients with BC (Table 1). Of these, 48 studies were clinical trials with control groups [19,20,23,24,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70] and had employed a wide range of therapeutic approaches, while 2 studies were classified as observational [71,72]. Two of the latter had carried out comprehensive analyses to monitor the progress of cognitive behavioural interventions [71,72].
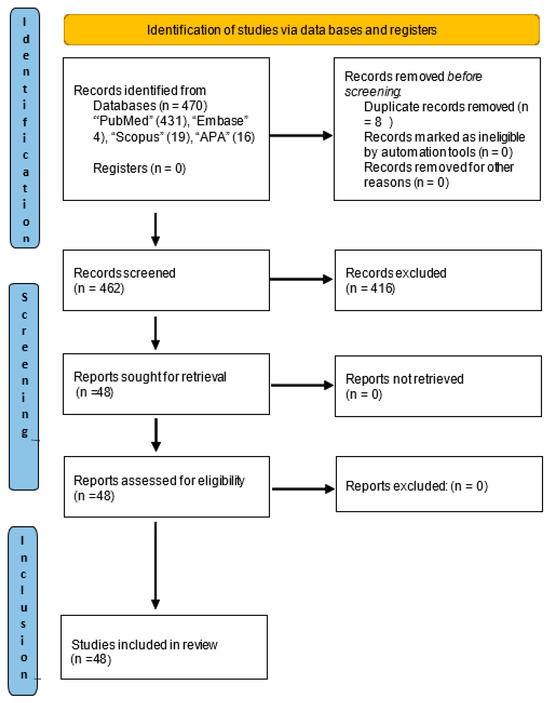
Figure 1.
Literature review workflow based on PRISMA statement.

Table 1.
The characteristics of the studies reporting significant effects regarding depressive symptoms after these interventions.
Together, these studies represented a comprehensive overview of the current landscape of intervention strategies and observational approaches in the context of BC and depression. The research had been performed on women with localised BC at clinical stages 0 to III [19,20,23,28,29,32,37,38,39,41,42,43,44,48,49,50,53,54,57,59,60,64,66,69,72], stage IV (metastatic) BC [30,31,45,58,62,70], or survivors of stage I–IV BC [27,33,34,36,40,47,51,55,56,63,68,71]. However, some of the articles had not specified the clinical stage of the patients that had participated in the interventions [24,35,46,52,61,65,67]. In these cases, the symptoms of depression were examined in women after having completed their active treatments, which included surgery, RT, and chemotherapy [19,20,23,24,33,34,36,38,40,43,44,46,47,49,51,55,56,57,58,59,60,63,66,68,71,72]. Other studies evaluated these symptoms while women with BC were undergoing active treatment, including RT, chemotherapy, hormone therapy, or concomitant treatments [27,28,31,32,37,39,45,48,52,53,54,61,65,69,70]. The symptoms of depression were also investigated in women scheduled for biopsies [35] or surgeries, such as lumpectomies or mastectomies [29,41,42]. Additionally, some studies had examined the symptoms of depression in women who were not scheduled to receive RT or chemotherapy during the study timeline [64]. Other studies did not specify the type of treatment received [30,62,67].
3.2. Interventions Implemented to Alleviate Depression Symptoms in Women with Breast Cancer
In these studies, specific interventions based on cognitive behavioural therapies, mindfulness [20,30,31,36,38,41,42,46,49,51,52,56,57,58,60,65,66,67,68,70,71,72], yoga sessions [32,34,37,39,66], psychological support programmes [33,45,48,50,53,54,55,59,62], and integrated approaches combining various treatment modalities (such as physical exercise programmes [23,24,27,28,40,43,47,63,64], dance therapy [19,61,69], and music therapy [29,35]. These varied methods underscored the importance of tailoring interventions to individual patient needs to provide a comprehensive approach that considers both the physical and emotional aspects of their well-being during BC treatment. In this review, we have summarised the results of specific interventions designed to reduce depression symptoms.
3.3. Psychotherapy
In the studies analysed, various interventions had been implemented to alleviate depression symptoms in women with BC. The results revealed that mindful awareness practises (MAPs) reduced the symptoms of depression from pre-intervention to post-intervention compared to the controls [49,57]. Another work evaluated an internet-delivered mindfulness-based cognitive therapy (iMBCT) programme that had resulted in an immediate decrease in depression symptoms compared to the control group [56]. A similar approach, based on stress reduction and mindfulness, also demonstrated a reduction in the symptoms of depression in treated women [58]. Furthermore, an intervention that combined cognitive therapy (CT) and bright light exposure (BLT) showed a greater decrease in depression symptoms compared to the waiting list control group [60].
The application of psychoeducational cognitive behavioural therapy (CBT) also effectively reduced depression symptoms in BC survivors during follow-up [44]. Another work implemented a cognitive behavioural stress management (CBSM) intervention in BC survivors with 5- and 11-year follow-ups [71,72]; women who received the CBSM intervention reported fewer symptoms of depression compared to those in the control group, even up to 15 years later [72]. Another study was based on metacognitive therapy (MCT) and highlighted a decrease in the mean depression score in the intervention group [65]. In turn, the use of acceptance and commitment therapy (ACT) reduced the symptoms of depression compared to the control group [67]. Cognitive behavioural therapy activity stimulation (CBT-AP) showed a significant reduction in the symptoms of depression from baseline to a 3-month follow-up [70]. Furthermore, the implementation of a positive affect skills intervention resulted in reductions in depression and negative affect after 1 month of follow-up [30].
A study based on the Reimagine (symptom self-monitoring) curriculum demonstrated reductions in depression symptoms [36]. In turn, research that implemented mindfulness-based art therapy (MBAT) led to a decrease in depression in the intervention group [38]. Another work implemented a group expression intervention delivered by nurses, which resulted in a decrease in the symptoms of depression compared to the control group [41]. The implementation of a ‘personalised navigation’ intervention by nurses resulted in a long-term decrease in depression levels in the intervention group after 12 months [46]. Work using a mental subtraction meditation (MSM) intervention also reported a decrease in depression [51]. Finally, the REBECCA trial demonstrated that nursing symptom screening and navigation decreased several psychological symptoms, including depression. Hence, all of the findings reported above underscore the effectiveness of a variety of interventions in managing the symptoms of depression in women with BC [52].
In terms of psychotherapy interventions for women with BC and symptoms of depression, a nurse-led programme showed improvements in mood and depression in the intervention group [54]. In turn, a speech therapy programme with psychological and nutritional counselling for 8 weeks resulted in lower depression scores in the intervention group [59]. In a compelling study, women with BC were divided into three conditions: greater self-regulation (ESR), self-regulation (SR), and facts about cancer (CF). In the ESR, the participants wrote about their stressful cancer-related experiences and coping strategies in the first week, deep feelings about BC in the second week, and positive thoughts about the experience in the third week. The instructions were the same for the SR, but the order of weeks 1 and 2 was swapped. Finally, in the CF, the participants wrote objectively about their cancer diagnosis and treatment. Interestingly, the participants in the ESR group showed improvements in the symptoms of depression, while the SR group did not differ from the CF condition. These results suggest that the order of the writing sessions was important and that promoting emotional disclosure before cognitive reappraisal had long-term mental health benefits [33].
Another work implemented supportive care interventions adapted from interpersonal psychotherapy, which resulted in decreased depression scores in the intervention group [55]. However, other researchers found that, although there were improvements in the symptoms of depression both before and after interpersonal psychotherapy (PTI), problem-solving therapy (PST), or brief supportive psychotherapy (BSP), there were no significant differences between these three groups [62]. Similarly, interpersonal psychotherapy implemented in another work also showed improvements in the symptoms of depression in the intervention group [45]. Elsewhere, the use of the short-term psychodynamic psychotherapy (STPP) alleviated depression in the intervention group [48]. In contrast, in two online support group interventions, the usual care (UC) group had lower levels of depression compared to the enhanced prosocial group (P-ISG) [50]. In a psychoeducational intervention compared to a support group, both groups showed improvements over time but no differences in emotional distress were found between them [53].
On the other hand, we found one trial that did not show significant results regarding improvements in depressive symptoms by using the Mindfulness-Based Stress Reduction Program for Breast Cancer (MBSR-BC), the participants in the experimental group showed a tendency to greater improvement in depressive symptoms compared to the control group; however, this difference did not reach statistical significance [20].
3.4. Yoga
Work based on a mindfulness yoga intervention together with conventional mindfulness showed that mindfulness yoga was more effective in reducing the symptoms of depression [66]. However, other researchers did not find changes in depression symptoms in the intervention group. Nonetheless, these authors emphasised that the symptoms of depression had increased in the control group during the 8-week waiting time for the intervention and that these symptoms decreased upon its reception, while there were no significant results in the intervention group that participated in yoga sessions [32]. Similarly, a yoga intervention implemented for 8 weeks did not improve depression and anxiety levels in its participants [37]. Moreover, a 12-week yoga intervention produced no changes in patient depression levels [34]. In the same vein, a yoga intervention lasting 6 weeks did not produce improvements in the symptoms of depression [39].
3.5. Physical Activity
Work on exercise interventions for women with BC and symptoms of depression was quite varied. Firstly, the administration of 12 supervised social cognitive theory exercise sessions in the BEAT Cancer intervention over 3 months produced improvements in the symptoms of depression up to 3 months later [63]. In turn, changes in physical activity behaviour also reduced depression symptoms from the beginning to the end of another intervention [64]. Similarly, compared to the control group, the symptoms of depression reduced in a 24-week lifestyle intervention that combined three supervised exercise sessions with a healthy eating programme [28].
Another comprehensive study conducted a supervised physical activity intervention using four strategies (supervised exercise sessions, facility access, daily activity promotion, and Fitbit self-monitoring) and applied a full factorial design. These researchers reported a decrease in the symptoms of depression across the entire sample during the 6-month intervention. In turn, the participants who received the active life every day intervention comprising strategies that may positively impact depression symptoms beyond the effect of increased physical activity (i.e., goal setting and social support) experienced even greater symptom reductions [40].
Elsewhere, a Tai-Chi exercise intervention lasting 8 weeks showed lower depression scores compared to the control group [43]. In relation to the aforementioned work, completing a Baduanjin exercise intervention 3 days a week also resulted in improvements in the symptoms of depression because of this specific exercise [47]. However, a Kyusho Jitsu intervention that included martial arts exercises, self-defence, pain cognition, stretching, and physical toning produced no changes in terms of depression symptoms [27].
The study group received a 3-day-a-week aerobic exercise programme for 12 weeks at the gym in 50 min sessions and a home-based resistance exercise programme to be performed at least twice a week for 60 min. This study showed that aerobic and resistance exercise decreased depression levels in women who had previously received breast cancer treatments [24].
On the other hand, in this randomised controlled clinical trial, a home-based exercise programme was implemented for the experimental group, with 20 to 30 min sessions, three times a week for six weeks, starting 72 h after each chemotherapy cycle. However, no statistically significant differences were found in the mean depression score between the two groups, either immediately after the intervention or one month later [23].
The absence of significant results in the reduction in depressive symptoms could be attributed to several factors. First, the duration and intensity of the exercise programme may have been insufficient to generate a significant impact on the participants’ mental health, especially considering that patients undergoing chemotherapy may experience fluctuations in their physical and emotional state.
Furthermore, the timing of the exercises could have influenced the effectiveness of the intervention. Since the sessions were conducted 72 h after each chemotherapy cycle, a period when the side effects of the treatment are typically more intense, it is possible that the participants had difficulty adhering to the programme or that physical discomfort reduced the psychological benefits of exercise. This, in turn, could have limited its impact on reducing depressive symptoms.
3.6. Dance Therapy
Regarding dance interventions in these women, in the study that adapted a Chinese ‘square dance’ folk dance, the participants who completed the 16-week intervention reported a lower incidence of the symptoms of depression compared to the controls [69]. Similarly, patients who completed 12 weeks of belly dance classes showed improvements in depression symptoms after the intervention [61]. However, this study did not show significant results in reducing depressive symptoms. The intervention involved dance movement therapy (DMT), with a programme specifically designed for breast cancer patients. This consisted of six 1.5 h sessions, conducted twice a week for three consecutive weeks, throughout radiotherapy treatment. The lack of significant results may be due to the insufficient duration and intensity of the intervention. The dance movement therapy (DMT) programme was conducted for only three weeks, with a total of six sessions. This period may have been too short to generate a significant impact on depressive symptoms. In addition, due to the timing of the intervention: DMT was applied during radiotherapy, a phase of treatment that can generate fatigue, physical discomfort, and emotional stress. These factors could have limited the participants’ ability to fully engage in the intervention, reducing its effectiveness in improving mood [19].
3.7. Music Therapy
In the study that combined the use of music therapy and progressive muscle relaxation training in women after having undergone a radical mastectomy, the patients in the intervention group experienced an improvement in their depression levels [29]. Another important study conducted an intervention using either hypnosis or music. In the former, women scheduled to receive a breast biopsy listened to a hypnosis recording that included induction and deepening phases, as well as suggestions to reduce their anxiety and pain and to increase their physical relaxation and emotional well-being; at the end, they were provided with suggestions for self-hypnosis. The music group listened to the same audio, but only its background music and without the suggestions. Interestingly, these authors reported a reduction in depression levels both the intervention groups compared to the control group [35].
Notably, eight studies focused on implementing music therapy interventions in women with BC and symptoms of depression did not change. For example, although the depression scores were reduced in an internet-based cognitive behavioural therapy (iCBT) intervention group, these results were not statistically significant [68]. Surprisingly, depression scores increased in another study that taught a comprehensive educational course on psychological stress and management skills to women with metastatic BC undergoing 5–6 weeks of RT [31]. Additionally, the Swedish Interactive Rehabilitation Information (SIRI) computer-based educational programme did not reduce depression and anxiety levels in its study participants [42].
3.8. Effects on the Other Psychological Symptoms: Anxiety, Stress, and Sleep Levels
Many other studies not only showed positive results in terms of depression symptoms but also highlighted the relevance of these interventions in relation to anxiety, stress, and sleep quality. For instance, the MAP-based intervention mentioned above also benefited insomnia symptoms for up to 6 months of follow-up [57]. Additionally, MAPS, another MAP-based intervention, resulted in short-term reductions in perceived stress, sleep disturbances, and increased peace, meaning, and positive affect [49]. The iMBCT-based intervention had long-term effects on anxiety but did not reduce perceived stress or insomnia severity [56]. In contrast, compared to waiting list controls, there were improvements in sleep disturbances in the group receiving GSH-MBI-guided self-help interventions, and these benefits were maintained at 3 month of follow-ups [58]. Lastly, a nurse-led psychological intervention programme also improved anxiety and insomnia symptoms [54].
Other authors demonstrated that patients undergoing CT experienced a reduction in anxiety after treatment [60] and similarly, applied psychoeducational CBT effectively reduced anxiety symptoms during follow-up [44]. The use of MBAT also decreased anxiety level [38]. A group expression intervention delivered by nurses produced a decrease in anxiety symptoms compared to the control group [41], as did a personalised nursing navigation intervention in a long-term follow-up [46]. Finally, a MSM intervention group experienced a reduction in both anxiety and perceived stress [51].
Another study implemented a speech therapy programme with psychological and nutritional counselling that resulted in lower anxiety scores [59], while supportive health education (SHE) interpersonal psychotherapy produced decreased anxiety scores. In the study by Belay et al., there were reduced anxiety symptoms in the intervention group that received interpersonal psychotherapy; these patients were also offered information on sleep hygiene, which helped improve their sleep quality [55]. In a similar vein, a lower incidence of sleep disturbances was reported in the group practising the Chinese folk dance compared to the controls [69]. Furthermore, a music therapy intervention and progressive muscle relaxation training in patients with BC after a radical mastectomy improved anxiety symptoms in the intervention group and resulted in shorter mean hospital stays [29]. Lastly, applied hypnosis reduced stress and anxiety symptoms compared to the control group [35].
Other authors showed that engaging in yoga was strongly associated with fatigue and improved sleep quality but did not impact depression [34]. In turn, implementation of the BEAT Cancer intervention showed improvements in anxiety up to 3 months later [63]. Another study showed that a physical activity behaviour change intervention reduced psychosocial distress in BC survivors [64]. Similarly, the application of a Kyusho Jitsu intervention reduced patient scores on the anxiety subscale from baseline up to 6 months follow-up [27]. Likewise, Tai Chi exercises effectively relieved sleep disorders compared to the control group [43].
Although no significant changes in depressive symptoms were observed between the yoga- and control groups, a notable reduction in inflammation was evident immediately after treatment in the yoga group. Three months after treatment, lower plasma concentrations of IL-6, TNF-α, and IL-1β were still present in the patients from the yoga- compared to the control group. BC patients submitted to a combined intervention based on yoga and stretching displayed a reduction in the cortisol slope at the end of the radiotherapy treatment, the participants in the yoga group showed a significantly steeper cortisol slope compared to the control group [34].
4. Discussion
As shown in this review, several non-pharmacological interventions can improve the symptoms of depression in patients with BC. These mainly target physical or psychosocial factors and encompass at least nine different therapeutic strategies, although exercise [23,24,27,28,40,43,47,63,64], psychotherapy [20,33,45,48,50,53,54,55,59,62], and yoga [32,34,37,39,66], alongside meditation, all stand out [30,31,36,38,41,42,46,49,51,52,56,57,58,60,65,66,67,68,70,71,72].
The significant improvements in depressive symptoms observed in these interventions can be attributed to a combination of factors. Stress reduction through psychotherapies such as mindfulness and cognitive behavioural therapy helps patients manage stress and anxiety, which in turn can decrease depressive symptoms [88,89]. Cognitive behavioural therapy has consistently been shown to benefit symptoms of depression. Furthermore, the optimisation of emotional regulation and increased psychological flexibility, facilitated by interpersonal psychotherapy and group therapies, offer a safe space for patients to express their emotions and receive support. The power of positive expectations that patients have, along with social support, provides a sense of belonging and emotional support, which is crucial for mental health and the reduction in depressive symptoms [25]. Traditionally, psychotherapy models were developed and applied in an individual setting, although exceptions exist. The hope of group psychotherapy has always been to provide a similar level of effectiveness. Research suggests that, in fact, group therapy is equally effective as individual therapy [90].
The available evidence on the effectiveness of yoga in reducing symptoms of depression is positive, especially when combined with meditation. However, the effects of exercise on the control of depressive symptoms associated with BC treatment remain inconsistent. These differences between studies may be due to variations in the duration of interventions and other methodological factors. Despite these inconsistencies, a reduction in depression symptoms has been observed with aerobic exercise. However, the potential benefit of exercise may have been underestimated, as clinical trials evaluating this factor also showed benefits in the control group. For ethical reasons, these studies could not restrict exercise due to its known positive effects on physical health. Together, yoga, meditation, and aerobic exercise offer a holistic approach that addresses both the psychological and physical aspects of depression in BC patients. These therapies not only help manage depressive symptoms, but also improve patients’ overall quality of life by promoting physical and mental health [91].
It should be noted that various interventions have been shown to be effective in patients with both moderate and severe depressive symptoms. Many studies recommend the use of cognitive behavioural therapy CBT), behavioural activation, mindfulness-based stress reduction, and interpersonal therapy (IPT) in an individual format. All evidence-based psychotherapeutic treatments for major depressive disorder demonstrated similar and notable improvements in depressive symptoms [62]. Interpersonal therapy (IPT) has been shown to be effective in patients with breast cancer and depression, as it helps to cope with the changes in life and interpersonal relationships associated with the disease. Its approach allows patients to adapt to new role dynamics, express their expectations, and mobilise social support, which contributes to alleviating depressive symptoms [62]. Studies have shown that IPT improves anxiety, depression, and quality of life in women with moderate depression [45]. Furthermore, one study found that twice as many patients with breast cancer and clinical depression achieved remission after receiving short-term psychodynamic psychotherapy compared to the control group (44% vs. 23%) [48]. These findings highlight the crucial role of psychotherapy in emotional management before, during, and after breast cancer treatment. By providing strategies to cope with interpersonal difficulties, fostering self-care, and promoting resilience, psychotherapy helps patients rebuild their identity and regain emotional balance in their recovery process.
This clinical trial evaluated the efficacy of Acceptance and Commitment Therapy (ACT) in women with severe depression due to breast cancer, achieving a reduction in depressive symptoms. The intervention consisted of eight weekly 90 min sessions, promoting acceptance of thoughts and emotions related to the disease, as well as the development of greater psychological flexibility, the main objective of ACT [67].
Likewise, other clinical trials have demonstrated reductions in mild depressive symptoms through various interventions, including: Cognitive Behavioural Therapy (CBT [44], mindfulness practises (MAP) [49,57], mindfulness-based cognitive therapy online mindfulness (iMBCT) [56], face-to-face mindfulness-based interventions (MBI) [58], mindfulness-based art therapy (MBAT) [38], mental subtraction meditation (MSM) [51], combined therapies such as meditation and yoga [66]. Other effective strategies included logotherapy, nutritional counselling [59], physical exercise such as Kyusho Jitsu or Baduanjin [27,47], and the ALED intervention, which combined goal setting and social support, showing benefits in reducing depression beyond the impact of physical exercise [40].
Furthermore, clinical trials that conducted online psychosocial interventions, such as telephone interpersonal intervention (TIPC) and supportive health education (SHE) [54], as well as the LILAC positive affect skills intervention, with sessions both in person and online [30]. The “Reimagine” programme included activities such as attending group meetings and completing cognitive reframing and mind–body exercises [36]. The results suggest that interventions delivered online or face-to-face were effective in reducing mild depressive symptoms.
Clinical trials demonstrated the efficacy of support groups in reducing mild depressive symptoms. A standard support group (S-ISG), focused on information sharing, emotional support, and positive change skill development, was compared to an enhanced prosocial support group (P-ISG), which included advice on how to support others online. Reductions in depression score were observed in the S-ISG group [50]. In addition, the study evaluated psychoeducational group interventions (PEG), focusing on health education, stress management, and problem solving, compared to support groups (SG), which offered emotional support and reduced isolation. Both approaches showed improvements in anxiety and depression over time [53].
Interventions for mild, moderate, and severe depression show similar results, with approaches such as CBT, mindfulness, and meditation having been shown to be effective at all levels. These therapies share the goal of modifying negative thought patterns and strengthening coping skills, promoting positive changes in emotional management [92]. However, the intensity and combination of techniques vary depending on the severity of symptoms. For mild depression, interventions are usually less intensive, focusing on meditation and mindfulness. In contrast, moderate to severe cases require more structured strategies, such as advanced CBT techniques, combined with other therapies and even pharmacological treatment when necessary.
But there are also differences in the results of these interventions on mild, moderate, and severe depressive symptoms. It could be due to the degree of intervention. Moderate and severe depressive symptoms often require more intensive and structured interventions, such as ACT and IPT, which offer a more in-depth approach to addressing emotional and functional crises. In contrast, mild depressive symptoms can be managed effectively with more general, accessible, and less intensive interventions such as stress-reduction meditation, mindfulness-based art therapy, physical exercise, and support groups, which are effective, but less specific. Due to the duration and frequency of the therapies. Therapies for moderate and severe depression, such as CBT and IPT, often involve longer duration and frequency of sessions. For mild depressive symptoms, interventions may be of shorter duration and frequency, better suited to less intensive needs and providing positive results with a smaller investment of time.
The impact of other interventions on the symptoms of depression are also unclear, partly because of the wide range of therapeutic strategies considered, which made it very hard to compare them or estimate a global effect. Therefore, we instead grouped the studies together, allowing us to consider their dimensions and characterise them in more homogeneous groups, according to the strategies they had implemented. Another factor that made it difficult to globally evaluate the impact of these interventions was the range in their implementation formats: from several times a week up to several months. Thus, further work to compare the intensity and duration of the interventions will be necessary to elucidate the minimum requirements for such interventions to produce beneficial effects.
In psychotherapy clinical trials, both the placebo effect and the placebo response may occur. The placebo effect is a psychobiological phenomenon in which the patient’s improvement is due to factors such as his or her positive expectations and belief in the efficacy of the treatment. The placebo response, in contrast, encompasses all changes in the patient’s health following an inactive treatment, including variations in symptoms before and after the intervention [93,94]. In psychotherapy, the placebo response can be influenced by environmental and psychosocial factors, such as the therapeutic relationship, the therapist’s support, and the setting in which the therapy takes place. These elements, supported by empirical evidence, play a key role in therapeutic outcomes [95,96,97,98].
The placebo effect is widely recognised in biomedical research and medical practice, although its neurobiology and neuropsychology are still limited in understanding [99]. However, recent research in areas such as pain, depression, and Parkinson’s disease has shed light on some of the neurobiological mechanisms of the placebo effect. It has been observed that both conscious expectation and unconscious behavioural conditioning processes are fundamental in this phenomenon. These processes can trigger the release of endogenous neurotransmitters such as dopamine, serotonin, and endorphins, which are related to well-being and can mimic expected or conditioned pharmacological effects, i.e., the placebo effect [99]. Although the placebo effect has traditionally been considered to operate primarily on a psychological level, more recent research has revealed that it can also trigger physiological responses in the body. Belief in the effectiveness of treatment can activate areas of the brain associated with emotional regulation and well-being, such as the prefrontal cortex, which could contribute to the reduction in depression symptoms and improvement of mood [100]. In anxiety and depression, placebo responses are associated with increased activity in neural networks related to emotional regulation [101,102]. The main neural pathways through which expectations and memories could influence peripheral immune functions include the neocortical-sympathetic-immune axis, which encompasses limbic and hypothalamic relays; the hypothalamic–pituitary–adrenal immune axis and the brainstem–vagus–cholinergic pathway. Therefore, placebo effects may benefit end-organ functioning and the overall health of the individual through the healing power of beliefs, positive expectations, and conditioning processes [99].
Diagnosing depression in BC patients involves a comprehensive approach that considers psychological and somatic symptoms. Mild to moderate depressive symptoms can be difficult to differentiate from somatic symptoms of BC for several reasons. First, there is significant overlap in symptoms: fatigue, loss of appetite, and insomnia are common in both depression and cancer and their treatments [103,104]. These shared symptoms may make it difficult to accurately identify depression in BC patients. Additionally, the natural emotional reaction to receiving a cancer diagnosis and undergoing aggressive treatments can trigger a variety of emotions, such as sadness, anxiety, and worry. These emotions are normal and expected responses to such a stressful situation and do not necessarily indicate the presence of clinical depression. However, this emotional reaction can mask or complicate the diagnosis of depression [105]. Changes in quality of life due to side effects of cancer treatment may contribute to depressive symptoms, making them difficult to distinguish [24]. Additionally, stigma and denial, where some patients minimise or deny their emotional symptoms due to the stigma associated with depression or the perception that expressing negative emotions is a sign of weakness, may prevent patients from seeking or accepting help for their emotional problems, which in turn complicates the proper diagnosis and treatment of depression [106].
These reasons underscore the importance of a comprehensive and careful assessment by healthcare professionals to differentiate between depressive symptoms and somatic symptoms of cancer. It is crucial that professionals use multidisciplinary approaches that consider both the psychological and somatic aspects of the patient, and that they maintain open and non-judgmental communication with patients to ensure accurate diagnosis and treatment. A proper diagnosis of depression is of vital importance as it allows health professionals to implement effective non-pharmacological interventions, such as psychotherapy, cognitive behavioural therapy, emotional and social support, and other interventions discussed in this literature review. These interventions have been shown to be effective in reducing depressive symptoms, regardless of their severity. These interventions have shown that they can significantly improve the emotional well-being and quality of life of BC patients who present with depressive symptoms.
Limitations of the Review
This review has certain limitations that should be taken into account when interpreting and generalising the results. Firstly, the search for articles was conducted in English and Spanish, which might have excluded relevant studies published in other languages.
Secondly, the methodological heterogeneity of the selected clinical trials and interventions analysed made it difficult to compare the results of the studies included in this review. The heterogeneity in the interventions and outcome variables, the differences in the populations as within the BC there were women in the studies who had previously undergone chemotherapy, concomitant hormonal therapy or only undergone surgery and the wide age range of the patients may be a difficulty in generalising the benefits of each type of intervention. The lack of quality analysis of these clinical trials due to different experimental design, e.g., with or without control group, with or without randomisation, is a limitation when analysing their effects. Each type of intervention has different mechanisms of action, which complicates direct comparison and uniform assessment of their efficacy in addressing the improvement of depressive symptoms. This challenge is further compounded by the cultural heterogeneity of the participating population, which is explained in more detail in the next section. To reduce this heterogeneity, we recommend using guidelines such as PRISMA or CONSORT in future research to improve methodological consistency.
Third, each study had its own criteria for measuring the efficacy of the interventions, as well as different inclusion criteria, so it is possible that the studies did not take into account the possibility of confounding variables. Furthermore, the use of different scales to measure depressive symptoms introduces variability in the results, which may complicate comparison between studies and compromise the overall conclusions.
5. Conclusions
This review highlights the importance of considering non-pharmacological interventions to manage the symptoms of depression in patients undergoing BC therapy. There appears to be good scientific evidence to support the inclusion of yoga and mindfulness practises in standard-of-care interventions to manage depression symptoms in patients with BC. Furthermore, CBT can also be useful in cases with clinical depression, both with a CT approach focusing on moods and thoughts or with behavioural therapy specifically targeting actions and behaviours.
Nonetheless, the implementation of non-pharmacological interventions to manage depression symptoms in clinical practice is still lacking, with most such interventions focusing mainly on the use of antidepressant drugs. These medications have variable response rates that can likely be improved by simultaneously applying non-pharmacological interventions. However, this combined approach is rarely adopted in clinical practice, partly because of the high economic cost of the human resources required to implement these practises. Indeed, in countries with public health systems, these types of interventions are not included in the healthcare services available in hospitals or primary care centres, meaning that patients must access them through non-profit organisations, patient associations, or private clinics.
Increased physical activity may reduce the burden of depression symptoms in patients with BC but the current evidence in this regard is still ambiguous. Because these intervention strategies may differentially impact the symptoms of depression, more work will be required to assess the exercise types, duration, and frequency required to achieve a minimal clinically important difference (MCID) in BC survivors. Considering patient perspectives may also be helpful, given that effect sizes alone cannot indicate the clinical relevance of an intervention because the outcome itself determines this factor.
The MCID is defined as the smallest difference in a domain of interest, without problematic side effects or excessive cost, perceived by patients as beneficial and that would justify a change in their therapeutic management. Thus, this metric could be used as a starting point to pinpoint the cutoff for clinical relevance and in this sense, psychotherapy, pharmacotherapy, and combined treatments have all been shown to have effect sizes above this threshold. Notably, several international oncology societies now recommend exercise in all cancer patients and so its use in the treatment of depression symptoms will likely increase. Thus, more detailed analyses of the efficacy of such programmes to reduce the burden of depression in patients with BC will be warranted to inform the design and optimisation of behavioural interventions for these patients.
Although not overtly considered in the articles included in this review, in our opinion, the use of objective biomarkers measured in biological samples (e.g., blood, saliva, and hair, etc.) could also help to objectively analyse non-pharmacological interventions in terms of psychological alterations. The molecular effects of non-pharmacological interventions have been addressed in few studies focusing on inflammatory cytokines (IL-6, TNF-α, and IL-1β) and the hypothalamic–pituitary–adrenal (HPA) activation hormone, cortisol, and deserve further attention as a biomarker for non-pharmacological interventions as well. The term biomarker refers to any objectively measurable property that is reproducible, reliable, inexpensive, and non-invasive that can serve as a proxy for a normal or pathological biological process or a therapeutic intervention response. Thus, the identification and use of diagnostic biomarkers to distinguish the presence or absence of the symptoms of depression and of treatment biomarkers to predict responses to therapeutic interventions would clearly be beneficial.
Biomarkers are also categorised into trait, state, and endophenotype markers. Trait biomarkers are persistent and highlight biological processes that existed before the onset of the disorder that play a causal role in its pathophysiology. Thus, these biomarkers could be used to determine which individuals are at risk of BC. State biomarkers are transient and related to the clinical condition and so would be present at the onset and during BC but normalise with its remission. Endophenotypic biomarkers are a subgroup of trait biomarkers marking genes involved in certain conditions, and so they are persistent and more common in BC patient family members than in the general population.
As a solution to the problem of the low sensitivity and specificity of single biomarkers, some authors recommend the use of biomarker panels containing several biological factors for the diagnosis of depression and evaluation of its treatment responses. Thus, when trying to measure clinical differences in different therapeutic approaches to treating depression in patients with BC, using a wider range of neuroimaging, genetic, epigenetic, proteomic, and metabolomic biomarkers to incorporate multiple biological abnormalities would likely be beneficial.
Author Contributions
These authors contributed equally to this work. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors have no relevant affiliations or financial involvement with any organisations or entities that have a financial interest in, or financial conflicts with, the subject matter or materials discussed in this manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants, patents received or pending, and royalties.
References
- DeSantis, C.E.; Ma, J.; Gaudet, M.M.; Newman, L.A.; Miller, K.D.; Sauer, A.G.; Jemal, A.; Siegel, R.L. Breast Cancer Statistics, 2019. CA Cancer J. Clin. 2019, 69, 438–451. [Google Scholar] [CrossRef] [PubMed]
- Reich, R.R.; Lengacher, C.A.; Alinat, C.B.; Kip, K.E.; Paterson, C.; Ramesar, S.; Han, H.S.; Ismail-Khan, R.; Johnson-Mallard, V.; Moscoso, M.; et al. Mindfulness-Based Stress Reduction in Post-Treatment Breast Cancer Patients: Immediate and Sustained Effects Across Multiple Symptom Clusters. J. Pain. Symptom Manag. 2017, 53, 85. [Google Scholar] [CrossRef] [PubMed]
- Hammen, C. Stress and Depression. Annu. Rev. Clin. Psychol. 2005, 1, 293–319. [Google Scholar] [CrossRef]
- García-Sánchez, J.; Mafla-España, M.A.; Torregrosa, M.D.; Cauli, O. Adjuvant Aromatase Inhibitor Treatment Worsens Depressive Symptoms and Sleep Quality in Postmenopausal Women with Localized Breast Cancer: A One-Year Follow-up Study. Breast 2022, 66, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Dodd, M.J.; Cho, M.H.; Cooper, B.A.; Miaskowski, C. The Effect of Symptom Clusters on Functional Status and Quality of Life in Women with Breast Cancer. Eur. J. Oncol. Nurs. 2010, 14, 101–110. [Google Scholar] [CrossRef]
- Kenne Sarenmalm, E.; Browall, M.; Gaston-Johansson, F. Symptom Burden Clusters: A Challenge for Targeted Symptom Management. A Longitudinal Study Examining Symptom Burden Clusters in Breast Cancer. J. Pain. Symptom Manag. 2014, 47, 731–741. [Google Scholar] [CrossRef]
- Lengacher, C.A.; Reich, R.R.; Post-White, J.; Moscoso, M.; Shelton, M.M.; Barta, M.; Le, N.; Budhrani, P. Mindfulness Based Stress Reduction in Post-Treatment Breast Cancer Patients: An Examination of Symptoms and Symptom Clusters. J. Behav. Med. 2012, 35, 86–94. [Google Scholar] [CrossRef]
- Esper, P.; Heidrich, D. Symptom Clusters in Advanced Illness. Semin. Oncol. Nurs. 2005, 21, 20–28. [Google Scholar] [CrossRef]
- Kim, S.H.; Son, B.H.; Hwang, S.Y.; Han, W.; Yang, J.H.; Lee, S.; Yun, Y.H. Fatigue and Depression in Disease-Free Breast Cancer Survivors: Prevalence, Correlates, and Association with Quality of Life. J. Pain. Symptom Manag. 2008, 35, 644–655. [Google Scholar] [CrossRef]
- Yang, H.; Brand, J.S.; Fang, F.; Chiesa, F.; Johansson, A.L.V.; Hall, P.; Czene, K. Time-Dependent Risk of Depression, Anxiety, and Stress-Related Disorders in Patients with Invasive and in Situ Breast Cancer. Int. J. Cancer 2017, 140, 841–852. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Chan, M.; Bhatti, H.; Halton, M.; Grassi, L.; Johansen, C.; Meader, N. Prevalence of Depression, Anxiety, and Adjustment Disorder in Oncological, Haematological, and Palliative-Care Settings: A Meta-Analysis of 94 Interview-Based Studies. Lancet Oncol. 2011, 12, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Carreira, H.; Williams, R.; Funston, G.; Stanway, S.; Bhaskaran, K. Associations between Breast Cancer Survivorship and Adverse Mental Health Outcomes: A Matched Population-Based Cohort Study in the United Kingdom. PLoS Med. 2021, 18, e1003504. [Google Scholar] [CrossRef] [PubMed]
- Maunsell, E.; Brisson, J.; Deschi’nes, L. Psychological Distress After Initial Treatment of Breast Cancer Assessment of Potential Risk Factors. Cancer 1992, 70, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Cramp, F.; Hewlett, S.; Almeida, C.; Kirwan, J.R.; Choy, E.H.S.; Chalder, T.; Pollock, J.; Christensen, R. Non-Pharmacological Interventions for Fatigue in Rheumatoid Arthritis. Cochrane Database Syst. Rev. 2013, 2013, CD008322. [Google Scholar] [CrossRef]
- Cobeanu, O.; David, D. Alleviation of Side Effects and Distress in Breast Cancer Patients by Cognitive-Behavioral Interventions: A Systematic Review and Meta-Analysis. J. Clin. Psychol. Med. Settings 2018, 25, 335–355. [Google Scholar] [CrossRef]
- Jassim, G.A.; Doherty, S.; Whitford, D.L.; Khashan, A.S. Psychological Interventions for Women with Non-Metastatic Breast Cancer. Cochrane Database Syst. Rev. 2023, 2023, CD008729. [Google Scholar] [CrossRef]
- Mustafa, M.; Carson-Stevens, A.; Gillespie, D.; Edwards, A.G.K. Psychological Interventions for Women with Metastatic Breast Cancer. Cochrane Database Syst. Rev. 2013, 2013, CD004253. [Google Scholar] [CrossRef]
- Guarino, A.; Polini, C.; Forte, G.; Favieri, F.; Boncompagni, I.; Casagrande, M. The Effectiveness of Psychological Treatments in Women with Breast Cancer: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 209. [Google Scholar] [CrossRef]
- Ho, R.T.H.; Fong, T.C.T.; Lo, P.H.Y.; Ho, S.M.Y.; Lee, P.W.H.; Leung, P.P.Y.; Spiegel, D.; Chan, C.L.W. Randomized Controlled Trial of Supportive-Expressive Group Therapy and Body-Mind-Spirit Intervention for Chinese Non-Metastatic Breast Cancer Patients. Support. Care Cancer 2016, 24, 4929–4937. [Google Scholar] [CrossRef][Green Version]
- Lengacher, C.A.; Reich, R.R.; Paterson, C.L.; Ramesar, S.; Park, J.Y.; Alinat, C.; Johnson-Mallard, V.; Moscoso, M.; Budhrani-Shani, P.; Miladinovic, B.; et al. Examination of Broad Symptom Improvement Resulting from Mindfulness-Based Stress Reduction in Breast Cancer Survivors: A Randomized Controlled Trial. J. Clin. Oncol. 2016, 34, 2827–2834. [Google Scholar] [CrossRef]
- Ye, M.; Du, K.; Zhou, J.; Zhou, Q.; Shou, M.; Hu, B.; Jiang, P.; Dong, N.; He, L.; Liang, S.; et al. A Meta-Analysis of the Efficacy of Cognitive Behavior Therapy on Quality of Life and Psychological Health of Breast Cancer Survivors and Patients. Psychooncology 2018, 27, 1695–1703. [Google Scholar] [CrossRef] [PubMed]
- Eyles, C.; Leydon, G.M.; Hoffman, C.J.; Copson, E.R.; Prescott, P.; Chorozoglou, M.; Lewith, G. Mindfulness for the Self-Management of Fatigue, Anxiety, and Depression in Women with Metastatic Breast Cancer: A Mixed Methods Feasibility Study. Integr. Cancer Ther. 2015, 14, 42–56. [Google Scholar] [CrossRef] [PubMed]
- Mostafaei, F.; Azizi, M.; Jalali, A.; Salari, N.; Abbasi, P. Effect of Exercise on Depression and Fatigue in Breast Cancer Women Undergoing Chemotherapy: A Randomized Controlled Trial. Heliyon 2021, 7, e07657. [Google Scholar] [CrossRef] [PubMed]
- Aydin, M.; Kose, E.; Odabas, I.; Bingul, B.M.; Demirci, D.; Aydin, Z. The Effect of Exercise on Life Quality and Depression Levels of Breast Cancer Patients. Asian Pac. J. Cancer Prev. 2021, 22, 725–732. [Google Scholar] [CrossRef]
- Brown, T.; Cruickshank, S.; Noblet, M. Specialist Breast Care Nurses for Support of Women with Breast Cancer. Cochrane Database Syst. Rev. 2021, 2021, CD005634. [Google Scholar] [CrossRef]
- Coutiño-Escamilla, L.; Piña-Pozas, M.; Tobías Garces, A.; Gamboa-Loira, B.; López-Carrillo, L. Non-Pharmacological Therapies for Depressive Symptoms in Breast Cancer Patients: Systematic Review and Meta-Analysis of Randomized Clinical Trials. Breast 2019, 44, 135–143. [Google Scholar] [CrossRef]
- Salchow, J.L.; Strunk, M.A.; Niels, T.; Steck, J.; Minto, C.A.; Baumann, F.T. A Randomized Controlled Pilot Trial About the Influence of Kyusho Jitsu Exercise on Self-Efficacy, Fear, Depression, and Distress of Breast Cancer Patients within Follow-up Care. Integr. Cancer Ther. 2021, 20, 15347354211037955. [Google Scholar] [CrossRef]
- Saxton, J.M.; Scott, E.J.; Daley, A.J.; Woodroofe, M.N.; Mutrie, N.; Crank, H.; Powers, H.J.; Coleman, R.E. Effects of an Exercise and Hypocaloric Healthy Eating Intervention on Indices of Psychological Health Status, Hypothalamic-Pituitary-Adrenal Axis Regulation and Immune Function after Early-Stage Breast Cancer: A Randomised Controlled Trial. Breast Cancer Res. 2014, 16, R39. [Google Scholar] [CrossRef]
- Zhou, K.; Li, X.; Li, J.; Liu, M.; Dang, S.; Wang, D.; Xin, X. A Clinical Randomized Controlled Trial of Music Therapy and Progressive Muscle Relaxation Training in Female Breast Cancer Patients after Radical Mastectomy: Results on Depression, Anxiety and Length of Hospital Stay. Eur. J. Oncol. Nurs. 2015, 19, 54–59. [Google Scholar] [CrossRef]
- Cheung, E.O.; Cohn, M.A.; Dunn, L.B.; Melisko, M.E.; Morgan, S.; Penedo, F.J.; Salsman, J.M.; Shumay, D.M.; Moskowitz, J.T. A Randomized Pilot Trial of a Positive Affect Skill Intervention (Lessons in Linking Affect and Coping) for Women with Metastatic Breast Cancer. Psychooncology 2017, 26, 2101–2108. [Google Scholar] [CrossRef]
- Li, Z.; Geng, W.; Yin, J.; Zhang, J. Effect of One Comprehensive Education Course to Lower Anxiety and Depression among Chinese Breast Cancer Patients during the Postoperative Radiotherapy Period—One Randomized Clinical Trial. Radiat. Oncol. 2018, 13, 111. [Google Scholar] [CrossRef] [PubMed]
- Lanctôt, D.; Dupuis, G.; Marcaurell, R.; Anestin, A.S.; Bali, M. The Effects of the Bali Yoga Program (BYP-BC) on Reducing Psychological Symptoms in Breast Cancer Patients Receiving Chemotherapy: Results of a Randomized, Partially Blinded, Controlled Trial. J. Complement. Integr. Med. 2016, 13, 405–412. [Google Scholar] [CrossRef]
- Lu, Q.; Yeung, N.C.Y.; Tsai, W.; Kim, J.H.J. The Effects of Culturally Adapted Expressive Writing Interventions on Depressive and Anxiety Symptoms among Chinese American Breast Cancer Survivors: A Randomized Controlled Trial. Behav. Res. Ther. 2023, 161, 104244. [Google Scholar] [CrossRef] [PubMed]
- Kiecolt-Glaser, J.K.; Bennett, J.M.; Andridge, R.; Peng, J.; Shapiro, C.L.; Malarkey, W.B.; Emery, C.F.; Layman, R.; Mrozek, E.E.; Glaser, R. Yoga’s Impact on Inflammation, Mood, and Fatigue in Breast Cancer Survivors: A Randomized Controlled Trial. J. Clin. Oncol. 2014, 32, 1040–1049. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Jáuregui, T.; Téllez, A.; Juárez-García, D.; García, C.H.; García, F.E. Clinical Hypnosis and Music In Breast Biopsy:A Randomized Clinical Trial. Am. J. Clin. Hypn. 2018, 61, 244–257. [Google Scholar] [CrossRef]
- Smith, S.K.; MacDermott, K.; Amarasekara, S.; Pan, W.; Mayer, D.; Hockenberry, M. Reimagine: A Randomized Controlled Trial of an Online, Symptom Self-Management Curriculum among Breast Cancer Survivors. Support. Care Cancer 2019, 27, 1775–1781. [Google Scholar] [CrossRef]
- Taso, C.J.; Lin, H.S.; Lin, W.L.; Chen, S.M.; Huang, W.T.; Chen, S.W. The Effect of Yoga Exercise on Improving Depression, Anxiety, and Fatigue in Women with Breast Cancer: A Randomized Controlled Trial. J. Nurs. Res. 2014, 22, 155–164. [Google Scholar] [CrossRef]
- Jang, S.H.; Kang, S.Y.; Lee, H.J.; Lee, S.Y. Beneficial Effect of Mindfulness-Based Art Therapy in Patients with Breast Cancer—A Randomized Controlled Trial. Explor. J. Sci. Heal. 2016, 12, 333–340. [Google Scholar] [CrossRef]
- Chandwani, K.D.; Perkins, G.; Nagendra, H.R.; Raghuram, N.V.; Spelman, A.; Nagarathna, R.; Johnson, K.; Fortier, A.; Arun, B.; Wei, Q.; et al. Randomized, Controlled Trial of Yoga in Women with Breast Cancer Undergoing Radiotherapy. J. Clin. Oncol. 2014, 32, 1058–1065. [Google Scholar] [CrossRef]
- Rethorst, C.D.; Carmody, T.J.; Argenbright, K.E.; Mayes, T.L.; Hamann, H.A.; Trivedi, M.H. Considering Depression as a Secondary Outcome in the Optimization of Physical Activity Interventions for Breast Cancer Survivors in the PACES Trial: A Factorial Randomized Controlled Trial. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 47. [Google Scholar] [CrossRef]
- Wang, G.; Li, Z.; Luo, X.; Wei, R.; Liu, H.; Yang, J.; Lyu, J.; Jiang, X. Effects of Nurse-Led Supportive-Expressive Group Intervention for Post-Traumatic Growth among Breast Cancer Survivors: A Randomized Clinical Trial. J. Nurs. Scholarsh. 2022, 54, 434–444. [Google Scholar] [CrossRef] [PubMed]
- Ventura, F.; Sawatzky, R.; Öhlén, J.; Karlsson, P.; Koinberg, I. Challenges of Evaluating a Computer-Based Educational Programme for Women Diagnosed with Early-Stage Breast Cancer: A Randomised Controlled Trial. Eur. J. Cancer Care 2017, 26, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Yao, L.Q.; Kwok, S.W.H.; Tan, J.Y.; Wang, T.; Liu, X.L.; Bressington, D.; Chen, S.L.; Huang, H.Q. The Effect of an Evidence-Based Tai Chi Intervention on the Fatigue-Sleep Disturbance-Depression Symptom Cluster in Breast Cancer Patients: A Preliminary Randomised Controlled Trial. Eur. J. Oncol. Nurs. 2022, 61, 102202. [Google Scholar] [CrossRef] [PubMed]
- Ren, W.; Qiu, H.; Yang, Y.; Zhu, X.; Zhu, C.; Mao, G.; Mao, S.; Lin, Y.; Shen, S.; Li, C.; et al. Randomized Controlled Trial of Cognitive Behavioural Therapy for Depressive and Anxiety Symptoms in Chinese Women with Breast Cancer. Psychiatry Res. 2019, 271, 52–59. [Google Scholar] [CrossRef]
- Belay, W.; Kaba, M.; Labisso, W.L.; Tigeneh, W.; Sahile, Z.; Zergaw, A.; Ejigu, A.; Baheretibeb, Y.; Gufue, Z.H.; Haileselassie, W. The Effect of Interpersonal Psychotherapy on Quality of Life among Breast Cancer Patients with Common Mental Health Disorder: A Randomized Control Trial at Tikur Anbessa Specialized Hospital. Support. Care Cancer 2022, 30, 965–972. [Google Scholar] [CrossRef]
- Mertz, B.G.; Dunn-Henriksen, A.K.; Kroman, N.; Johansen, C.; Andersen, K.G.; Andersson, M.; Mathiesen, U.B.; Vibe-Petersen, J.; Dalton, S.O.; Envold Bidstrup, P. The Effects of Individually Tailored Nurse Navigation for Patients with Newly Diagnosed Breast Cancer: A Randomized Pilot Study. Acta Oncol. (Madr.) 2017, 56, 1682–1689. [Google Scholar] [CrossRef]
- Ying, W.; Min, Q.W.; Lei, T.; Na, Z.X.; Li, L.; Jing, L. The Health Effects of Baduanjin Exercise (a Type of Qigong Exercise) in Breast Cancer Survivors: A Randomized, Controlled, Single-Blinded Trial. Eur. J. Oncol. Nurs. 2019, 39, 90–97. [Google Scholar] [CrossRef]
- Beutel, M.E.; Weißflog, G.; Leuteritz, K.; Wiltink, J.; Haselbacher, A.; Ruckes, C.; Kuhnt, S.; Barthel, Y.; Imruck, B.H.; Zwerenz, R.; et al. Efficacy of Short-Term Psychodynamic Psychotherapy (STPP) with Depressed Breast Cancer Patients: Results of a Randomized Controlled Multicenter Trial. Ann. Oncol. 2014, 25, 378–384. [Google Scholar] [CrossRef]
- Bower, J.E.; Crosswell, A.D.; Stanton, A.L.; Crespi, C.M.; Winston, D.; Arevalo, J.; Ma, J.; Cole, S.W.; Ganz, P.A. Mindfulness Meditation for Younger Breast Cancer Survivors: A Randomized Controlled Trial. Cancer 2015, 121, 1231–1240. [Google Scholar] [CrossRef]
- Lepore, S.J.; Buzaglo, J.S.; Lieberman, M.A.; Golant, M.; Greener, J.R.; Davey, A. Comparing Standard Versus Prosocial Internet Support Groups for Patients With Breast Cancer: A Randomized Controlled Trial of the Helper Therapy Principle. J. Clin. Oncol. 2014, 32, 4081. [Google Scholar] [CrossRef]
- Yun, M.R.; Song, M.; Jung, K.H.; Yu, B.J.; Lee, K.J. The Effects of Mind Subtraction Meditation on Breast Cancer Survivors’ Psychological and Spiritual Well-Being and Sleep Quality: A Randomized Controlled Trial in South Korea. Cancer Nurs. 2017, 40, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Bidstrup, P.E.; Johansen, C.; Kroman, N.; Belmonte, F.; Duriaud, H.; Dalton, S.O.; Andersen, K.G.; Mertz, B. Effect of a Nurse Navigation Intervention on Mental Symptoms in Patients With Psychological Vulnerability and Breast Cancer: The REBECCA Randomized Clinical Trial. JAMA Netw. Open 2023, 6, e2319591. [Google Scholar] [CrossRef] [PubMed]
- Bredal, I.S.; Kåresen, R.; Smeby, N.A.; Espe, R.; Sørensen, E.M.; Amundsen, M.; Aas, H.; Ekeberg, Ø. Effects of a Psychoeducational versus a Support Group Intervention in Patients with Early-Stage Breast Cancer: Results of a Randomized Controlled Trial. Cancer Nurs. 2014, 37, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Choi, K.S.; Han, K.; Kim, H.W. A Psychological Intervention Programme for Patients with Breast Cancer under Chemotherapy and at a High Risk of Depression: A Randomised Clinical Trial. J. Clin. Nurs. 2018, 27, 572–581. [Google Scholar] [CrossRef]
- Badger, T.A.; Segrin, C.; Sikorskii, A.; Pasvogel, A.; Weihs, K.; Lopez, A.M.; Chalasani, P. Randomized Controlled Trial of Supportive Care Interventions to Manage Psychological Distress and Symptoms in Latinas with Breast Cancer and Their Informal Caregivers. Psychol. Health 2020, 35, 87–106. [Google Scholar] [CrossRef]
- Nissen, E.R.; O’Connor, M.; Kaldo, V.; Højris, I.; Borre, M.; Zachariae, R.; Mehlsen, M. Internet-Delivered Mindfulness-Based Cognitive Therapy for Anxiety and Depression in Cancer Survivors: A Randomized Controlled Trial. Psychooncology 2020, 29, 68–75. [Google Scholar] [CrossRef]
- Bower, J.E.; Partridge, A.H.; Wolff, A.C.; Thorner, E.D.; Irwin, M.R.; Joffe, H.; Petersen, L.; Crespi, C.M.; Ganz, P.A. Targeting Depressive Symptoms in Younger Breast Cancer Survivors: The Pathways to Wellness Randomized Controlled Trial of Mindfulness Meditation and Survivorship Education. J. Clin. Oncol. 2021, 39, 3473. [Google Scholar] [CrossRef]
- Shao, D.; Zhang, H.; Cui, N.; Sun, J.; Li, J.; Cao, F. The Efficacy and Mechanisms of a Guided Self-Help Intervention Based on Mindfulness in Patients with Breast Cancer: A Randomized Controlled Trial. Cancer 2021, 127, 1377–1386. [Google Scholar] [CrossRef]
- Raji Lahiji, M.; Sajadian, A.; Haghighat, S.; Zarrati, M.; Dareini, H.; Raji Lahiji, M.; Razmpoosh, E. Effectiveness of Logotherapy and Nutrition Counseling on Psychological Status, Quality of Life, and Dietary Intake among Breast Cancer Survivors with Depressive Disorder: A Randomized Clinical Trial. Support. Care Cancer 2022, 30, 7997–8009. [Google Scholar] [CrossRef]
- Desautels, C.; Savard, J.; Ivers, H.; Savard, M.H.; Caplette-Gingras, A. Treatment of Depressive Symptoms in Patients with Breast Cancer: A Randomized Controlled Trial Comparing Cognitive Therapy and Bright Light Therapy. Health Psychol. 2018, 37, 1–13. [Google Scholar] [CrossRef]
- Boing, L.; Baptista, F.; Pereira, G.S.; Sperandio, F.F.; Moratelli, J.; Cardoso, A.A.; Borgatto, A.F.; de Azevedo Guimarães, A.C. Benefits of Belly Dance on Quality of Life, Fatigue, and Depressive Symptoms in Women with Breast Cancer—A Pilot Study of a Non-Randomised Clinical Trial. J. Bodyw. Mov. Ther. 2018, 22, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Blanco, C.; Markowitz, J.C.; Hellerstein, D.J.; Nezu, A.M.; Wall, M.; Olfson, M.; Chen, Y.; Levenson, J.; Onishi, M.; Varona, C.; et al. A Randomized Trial of Interpersonal Psychotherapy, Problem Solving Therapy, and Supportive Therapy for Major Depressive Disorder in Women with Breast Cancer. Breast Cancer Res. Treat. 2019, 173, 353–364. [Google Scholar] [CrossRef] [PubMed]
- Rogers, L.Q.; Courneya, K.S.; Anton, P.M.; Verhulst, S.; Vicari, S.K.; Robbs, R.S.; McAuley, E. Effects of a Multicomponent Physical Activity Behavior Change Intervention on Fatigue, Anxiety, and Depressive Symptomatology in Breast Cancer Survivors: Randomized Trial. Psychooncology 2017, 26, 1901–1906. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.J.; Hunter, G.R.; Norian, L.A.; Turan, B.; Rogers, L.Q. Ease of Walking Associates with Greater Free-Living Physical Activity and Reduced Depressive Symptomology in Breast Cancer Survivors: Pilot Randomized Trial. Support. Care Cancer 2018, 26, 1675–1683. [Google Scholar] [CrossRef]
- Zahedian, E.; Bahreini, M.; Ghasemi, N.; Mirzaei, K. Group Meta-Cognitive Therapy and Depression in Women with Breast Cancer: A Randomized Controlled Trial. BMC Womens Health 2021, 21, 111. [Google Scholar] [CrossRef]
- Liu, W.; Liu, J.; Ma, L.; Chen, J. Effect of Mindfulness Yoga on Anxiety and Depression in Early Breast Cancer Patients Received Adjuvant Chemotherapy: A Randomized Clinical Trial. J. Cancer Res. Clin. Oncol. 2022, 148, 2549–2560. [Google Scholar] [CrossRef]
- Ghorbani, V.; Zanjani, Z.; Omidi, A.; Sarvizadeh, M. Efficacy of Acceptance and Commitment Therapy (ACT) on Depression, Pain Acceptance, and Psychological Flexibility in Married Women with Breast Cancer: A Pre- and Post-Test Clinical Trial. Trends Psychiatry Psychother. 2021, 43, 126–133. [Google Scholar] [CrossRef]
- Akkol-Solakoglu, S.; Hevey, D. Internet-Delivered Cognitive Behavioural Therapy for Depression and Anxiety in Breast Cancer Survivors: Results from a Randomised Controlled Trial. Psychooncology 2023, 32, 446–456. [Google Scholar] [CrossRef]
- He, X.; Ng, M.S.N.; Choi, K.C.; So, W.K.W. Effects of a 16-Week Dance Intervention on the Symptom Cluster of Fatigue-Sleep Disturbance-Depression and Quality of Life among Patients with Breast Cancer Undergoing Adjuvant Chemotherapy: A Randomized Controlled Trial. Int. J. Nurs. Stud. 2022, 133, 104317. [Google Scholar] [CrossRef]
- Getu, M.A.; Wang, P.; Addissie, A.; Seife, E.; Chen, C.; Kantelhardt, E.J. The Effect of Cognitive Behavioural Therapy Integrated with Activity Pacing on Cancer-Related Fatigue, Depression and Quality of Life among Patients with Breast Cancer Undergoing Chemotherapy in Ethiopia: A Randomised Clinical Trial. Int. J. Cancer 2023, 152, 2541–2553. [Google Scholar] [CrossRef]
- Stagl, J.M.; Antoni, M.H.; Lechner, S.C.; Bouchard, L.C.; Blomberg, B.B.; Glück, S.; Derhagopian, R.P.; Carver, C.S. Randomized Controlled Trial of Cognitive Behavioral Stress Management in Breast Cancer: A Brief Report of Effects on 5-Year Depressive Symptoms. Health Psychol. 2015, 34, 176. [Google Scholar] [CrossRef] [PubMed]
- Stagl, J.M.; Bouchard, L.C.; Lechner, S.C.; Blomberg, B.B.; Gudenkauf, L.M.; Jutagir, D.R.; Glück, S.; Derhagopian, R.P.; Carver, C.S.; Antoni, M.H. Long-Term Psychological Benefits of Cognitive-Behavioral Stress Management for Women with Breast Cancer: 11-Year Follow-up of a Randomized Controlled Trial. Cancer 2015, 121, 1873–1881. [Google Scholar] [CrossRef] [PubMed]
- Salkind, N. Beck Depression Inventory. Encycl. Meas. Stat. 2013, 1–4. [Google Scholar] [CrossRef]
- Carleton, R.N.; Thibodeau, M.A.; Teale, M.J.N.; Welch, P.G.; Abrams, M.P.; Robinson, T.; Asmundson, G.J.G. The Center for Epidemiologic Studies Depression Scale: A Review with a Theoretical and Empirical Examination of Item Content and Factor Structure. PLoS ONE 2013, 8, e58067. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606. [Google Scholar] [CrossRef]
- Levis, B.; Benedetti, A.; Thombs, B.D.; DEPRESsion Screening Data (DEPRESSD) Collaboration. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ 2019, 365, l1476. [Google Scholar] [CrossRef]
- Passik, S.D.; Kirsh, K.L.; Donaghy, K.B.; Theobald, D.E.; Lundberg, J.C.; Holtsclaw, E.; Dugan, W.M. An Attempt to Employ the Zung Self-Rating Depression Scale as a “lab Test” to Trigger Follow-up in Ambulatory Oncology Clinics: Criterion Validity and Detection. J. Pain. Symptom Manag. 2001, 21, 273–281. [Google Scholar] [CrossRef]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for Depression in Well Older Adults: Evaluation of a Short Form of the CES-D. Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Kroenke, K.; Strine, T.W.; Spitzer, R.L.; Williams, J.B.W.; Berry, J.T.; Mokdad, A.H. The PHQ-8 as a Measure of Current Depression in the General Population. J. Affect. Disord. 2009, 114, 163–173. [Google Scholar] [CrossRef]
- McNair, P.M.; Lorr, M.; Droppleman, L.F. POMS Manual, 2nd ed.; Educational and Industrial Testing Service: San Diego, CA, USA, 1981. [Google Scholar]
- KKarlin, B.E.; Creech, S.K.; Grimes, J.S.; Clark, T.S.; Meagher, M.W.; Morey, L.C. The Personality Assessment Inventory with chronic pain patients: Psychometric properties and clinical utility. J. Clin. Psychol. 2005, 61, 1571–1585. [Google Scholar] [CrossRef] [PubMed]
- Rush, A.J.; Trivedi, M.H.; Ibrahim, H.M.; Carmody, T.J.; Arnow, B.; Klein, D.N.; Markowitz, J.C.; Ninan, P.T.; Kornstein, S.; Manber, R.; et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): A Psychometric Evaluation in Patients with Chronic Major Depression. Biol. Psychiatry 2003, 54, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Zhao, J.; Phillips, M.; Liu, J.; Cai, M.; Sun, S.; Huang, M. Validity and Reliability of the Chinese Hamilton Depression Rating Scale. Br. J. Psychiatry 1988, 152, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Smith, A.; Gibbons, C.; Alonso, J.; Valderas, J. The National Institutes of Health Patient-Reported Outcomes Measurement Information System (PROMIS): A View from the UK. Patient Relat. Outcome Meas. 2018, 9, 345–352. [Google Scholar] [CrossRef]
- HAMILTON, M. Development of a Rating Scale for Primary Depressive Illness. Br. J. Soc. Clin. Psychol. 1967, 6, 278–296. [Google Scholar] [CrossRef]
- Park, S.; Sato, Y.; Takita, Y.; Tamura, N.; Ninomiya, A.; Kosugi, T.; Sado, M.; Nakagawa, A.; Takahashi, M.; Hayashida, T.; et al. Mindfulness-Based Cognitive Therapy for Psychological Distress, Fear of Cancer Recurrence, Fatigue, Spiritual Well-Being, and Quality of Life in Patients With Breast Cancer—A Randomized Controlled Trial. J. Pain. Symptom Manag. 2020, 60, 381–389. [Google Scholar] [CrossRef]
- Schell, L.K.; Monsef, I.; Wöckel, A.; Skoetz, N. Mindfulness-Based Stress Reduction for Women Diagnosed with Breast Cancer. Cochrane Database Syst. Rev. 2019, 2019, CD011518. [Google Scholar] [CrossRef]
- Burlingame, G.M.; Jensen, J.L. Small Group Process and Outcome Research Highlights: A 25-Year Perspective. Int. J. Group. Psychother. 2017, 67, S194–S218. [Google Scholar] [CrossRef]
- Liu, L.; Tan, H.; Yu, S.; Yin, H.; Baxter, G.D. The Effectiveness of Tai Chi in Breast Cancer Patients: A Systematic Review and Meta-Analysis. Complement. Ther. Clin. Pract. 2020, 38, 101078. [Google Scholar] [CrossRef]
- Iannopollo, L.; Cristaldi, G.; Borgese, C.; Sommacal, S.; Silvestri, G.; Serpentini, S. Mindfulness Meditation as Psychosocial Support in the Breast Cancer Experience: A Case Report. Behav. Sci. 2022, 12, 216. [Google Scholar] [CrossRef]
- Schedlowski, M.; Enck, P.; Rief, W.; Bingel, U. Neuro-Bio-Behavioral Mechanisms of Placebo and Nocebo Responses: Implications for Clinical Trials and Clinical Practice. Pharmacol. Rev. 2015, 67, 697–730. [Google Scholar] [CrossRef] [PubMed]
- Enck, P.; Zipfel, S. Placebo Effects in Psychotherapy: A Framework. Front. Psychiatry 2019, 10, 456. [Google Scholar] [CrossRef] [PubMed]
- FRANK, J.D. The Influence of Patients’ and Therapists’ Expectations on the Outcome of Psychotherapy. Br. J. Med. Psychol. 1968, 41, 349–356. [Google Scholar] [CrossRef]
- Finniss, D.G.; Kaptchuk, T.J.; Miller, F.; Benedetti, F. Biological, Clinical, and Ethical Advances of Placebo Effects. Lancet 2010, 375, 686–695. [Google Scholar] [CrossRef] [PubMed]
- Colloca, L.; Benedetti, F. Placebo Analgesia Induced by Social Observational Learning. PAIN® 2009, 144, 28–34. [Google Scholar] [CrossRef]
- Enck, P.; Bingel, U.; Schedlowski, M.; Rief, W. The Placebo Response in Medicine: Minimize, Maximize or Personalize? Nat. Rev. Drug Discov. 2013, 12, 191–204. [Google Scholar] [CrossRef]
- Pacheco-López, G.; Engler, H.; Niemi, M.B.; Schedlowski, M. Expectations and Associations That Heal: Immunomodulatory Placebo Effects and Its Neurobiology. Brain Behav. Immun. 2006, 20, 430–446. [Google Scholar] [CrossRef]
- Benedetti, F. Mechanisms of Placebo and Placebo-Related Effects across Diseases and Treatments. Annu. Rev. Pharmacol. Toxicol. 2008, 48, 33–60. [Google Scholar] [CrossRef]
- Leuchter, A.F.; Cook, I.A.; Witte, E.A.; Morgan, M.; Abrams, M. Changes in Brain Function of Depressed Subjects during Treatment with Placebo. Am. J. Psychiatry 2002, 159, 122–129. [Google Scholar] [CrossRef]
- Petrovic, P.; Dietrich, T.; Fransson, P.; Andersson, J.; Carlsson, K.; Ingvar, M. Placebo in Emotional Processing—Induced Expectations of Anxiety Relief Activate a Generalized Modulatory Network. Neuron 2005, 46, 957–969. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Casado, A.; Álvarez-Bustos, A.; de Pedro, C.G.; Méndez-Otero, M.; Romero-Elías, M. Cancer-Related Fatigue in Breast Cancer Survivors: A Review. Clin. Breast Cancer 2021, 21, 10–25. [Google Scholar] [CrossRef] [PubMed]
- Kwak, A.; Jacobs, J.; Haggett, D.; Jimenez, R.; Peppercorn, J. Evaluation and Management of Insomnia in Women with Breast Cancer. Breast Cancer Res. Treat. 2020, 181, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Tsaras, K.; Papathanasiou, I.V.; Mitsi, D.; Veneti, A.; Kelesi, M.; Zyga, S.; Fradelos, E.C. Assessment of Depression and Anxiety in Breast Cancer Patients: Prevalence and Associated Factors. Asian Pacific J. Cancer Prev. 2018, 19, 1661–1669. [Google Scholar] [CrossRef]
- Lueboonthavatchai, P. Prevalence and Psychosocial Factors of Anxiety and Depression in Breast Cancer Patients. J. Med. Assoc. Thail. 2007, 90, 2164–2174. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).