Abstract
Sensitive Skin Syndrome (SSS) has been the subject of intense research in the past several years. Recent reviews confirm that about 40% of the population report moderate or very sensitive skin, and an additional 30% report slightly sensitive skin. Although certain phenotypes are more susceptible, anyone can suffer from SSS and this condition can manifest in all anatomic sites. A wide variety of environmental and lifestyle factors can trigger SSS symptoms of itching, stinging, burning, pain, and tingling. In order to avoid such triggers, the SSS individuals often alter their behaviors and habits such as restricting their daily activities, and modifying the use of everyday products that non-sensitive individuals take for granted. In addition, there is an association between SSS and some common psychological problems. Sensitive skin symptoms such as itching, stinging, burning and pain can result in sleep disorders, fatigue, stress and anxiety. Conversely, lack of sleep and stress from external sources can make the SSS sufferer more prone to the symptoms. This becomes a vicious cycle that impacts consumers’ quality of life and well-being. We are beginning to understand the importance of the underlying causes that can impact skin conditions. However, in order to better understand the SSS individual, we need to also be aware of the psychological factors that can trigger and/or worsen this skin condition, as well as the psychological stresses the condition places on the individual.
1. Introduction
Sensitive Skin Syndrome (SSS) has been the subject of intense research in recent years. Anyone can suffer from SSS; however, there are certain characteristics, or host factors, that are more likely to be seen in SSS individuals. These include female gender, fair skin, higher susceptibility to sunburn and blushing, and skin phototypes I–IV [1]. Typically, there are no objective signs of skin irritation in subjects suffering from SSS. Rather the condition manifests as unpleasant sensations such as pruritus, stinging, burning, pain, and tingling sensations, in response to a wide variety of external and internal stimuli that normally should not provoke such sensations [2,3,4]. Due to the absence of consistent objective signs, such as redness or swelling, investigators have relied on a questionnaire-based approach to evaluate this condition. Several such studies have been conducted among populations around the world to evaluate the prevalence of SSS in the general population (reviewed in Farage, 2019 [5]). Chen et al.’s meta analysis representing 18 countries, and a total of 51,783 individuals showed around 71% of people self-reported SSS [6].
Sensitive skin can affect all anatomic sites including face, scalp, and the genital area [5,7]. As we will see in this review, this can have a significant impact on an individual’s everyday life. Often the individual must cope with other dermatologic disorders in addition to the SSS symptoms. An individual with SSS must identify and avoid a wide variety of factors that can trigger their symptoms. In turn, the manifestation of SSS symptoms and can trigger psychological effects.
2. Physiological Contributors to SSS
A number of physiological differences have been identified in individuals with SSS (Table 1). The epidermal layer of the skin of individuals with SSS has reduced barrier integrity due to differences in lipid composition with a decrease in ceramide and sphingolipid content [8]. This results in increasing the potential penetration of irritants and insufficient protection of nerve endings [5,8,9,10]. Increased vascular reactivity has been observed in individuals with SSS, resulting in more intense vascular reactions to irritants [11]. Roussaki–Schulze and colleagues reported that vascular reactions to methyl nicotinate in SSS subjects was 75 times higher compared to non-sensitive controls [12].

Table 1.
Some Physiological Elements Contributing to SSS.
Neurosensory dysfunction is another physiological element that contributes to SSS. Biopsies from SSS subjects demonstrated a decrease of peptidergic C-fiber density [14]. These fibers are involved in pain, itching and temperature perception. Degeneration of these fibers can induce hyper-reactivity of the remaining nerve endings and a result in allodynia [11]. An additional neurosensory component is an increase in Transient Receptor Potential Vanilloid-1 (TRPV1). This is a non-selective cation channel that responds to heat and low pH, and is related to nociception, neurogenic inflammation, and pruritus. TRPV-1 is also classically known as the capsaicin receptor [15,16]. Based on self-reported SSS skin biopsies, Ehnis–Pérez et al. found TRPV1 is dramatically upregulated in sensitive skin subjects [15].
Another important factor for SSS people is that they may also suffer from skin co-morbidities and additional skin disorders (Table 2). Just like SSS, rosacea is more common in individuals who are female with fair skin and hair, blue eyes, and lighter skin, i.e., phototypes I–III [17]. In a genome-wide association study (GWAS) involving 22,952 subjects, Chang and colleagues determined that rosacea is associated with several HLA alleles [18]. This is in line with the inflammatory nature of the syndrome. In a study involving 1000 individuals in Korea, 56.8% of whom had sensitive or very sensitive skin, Kim and colleagues found that the SSS group was over 3 times more likely to suffer from acne, atopic dermatitis, and facial blushing, and over 2 times more likely to suffer from seborrheic dermatitis compared to the non-sensitive group [19]. Brenaut and colleagues found a similar result in an Indian population [20]. In a study involving over 3000 individuals, SSS subjects were 2–4 times more likely to report atopic dermatitis, acne, psoriasis, vitiligo, rosacea, or contact dermatitis compared to the non-sensitive group [20].

Table 2.
Some Skin Co-morbidities Associated with SSS.
Sensitive skin has also been linked to sensitive eyes and eyelids, and irritable bowel syndrome [26,27]. It is proposed that these conditions may be related to the neurosensory dysfunctions identified in SSS, i.e., hyperexcitability of nerve endings, hyperactivation of sensor proteins resulting from upregulation of TRP channels, and alterations in nerve fiber density [26]. The histological findings and clinical signs of small fiber impairment with SSS are similar to those experienced in small-fiber neuropathy [28].
As part of a GWAS, Farage et al. evaluated 23,426 subjects’ responses and found that SSS individuals reported other skin complaints, specifically, contact dermatitis, freckles, atopic dermatitis, acne, and seborrheic dermatitis [25]. These authors found an association between SSS and several specific loci also associated with genes for rosacea, pigmentation, and skin cancer [25].
Other Host Related Factors
Aging can be another physiologic factor in sensitive skin. As an individual ages, the skin changes as it becomes thinner and drier, as well as replacing itself at a slower rate [29]. The elderly skin is also more prone to higher permeability but a reduced elasticity, tensile strength, vascularization and cellularity [29]. These physiological changes might lead one to conclude that older skin is more susceptible to irritant effects, and more likely to be sensitive. However, clinical assessments using known irritant materials suggest that skin irritation susceptibility generally decreases with age, as does the capacity to produce visible physiological signs of dermatological irritation [9,29,30,31,32]. Several studies have shown that the prevalence of SSS in older individuals is no different or lower than in younger individuals [19,23,33,34]. A 2010 study with 1039 individuals evaluated SSS at several body sites in the US [29]. No consistent pattern with age was seen when subjects were asked about sensitive skin in general, of the face or body, specifically. However, genital area skin sensitivity demonstrated an increase from 53% in subjects ≤ 30 years old to 66% in subjects ≥ 50 years old (Figure 1). This difference was mainly due to the females in the study.
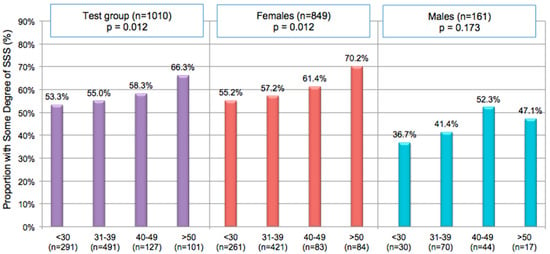
Figure 1.
Age and Gender Effect on Prevalence of Sensitive Genital Skin. Responders were asked if they had sensitive skin (“slight”, “moderate” or “very”) [35,36]. MH Chi-Square was used to test for correlations between perceptions of sensitive skin and age for responders overall and for each gender. Adapted from [37].
Another critical factor is the impact of hormonal fluctuations during the different consumer life stages on skin sensitivity. In both the dermis and epidermis, the skin has highly sensitive estrogen receptors, and variation of female hormones can have an impact on the skin [38]. Decreased estrogen levels can adversely affect barrier function, elasticity, blood circulation and vasomotor function. Farage’s study which included 1039 individuals demonstrated that the menstrual cycle was contributing to unpleasant genital skin in 61% of women with SSS and 40% of the non-sensitive skin women (p < 0.00001) [37]. Falcone and colleagues reported that women with more intense perimenstrual symptoms perceived their skin as more sensitive during some phases of the menstrual cycle compared to women with lower intensity symptoms (p = 0.002) [39]. Furthermore, 70% of postmenopausal women claiming SSS perceived their skin sensitivity increasing after menopause [39]. In general, among SSS women, products used for menstrual protection and hygiene have been shown to trigger significantly greater symptoms than non-sensitive women [37].
3. Psychological Effects of Skin Diseases
As mentioned earlier, individuals with SSS are more likely to also suffer from other skin disorders and co=morbidities. While most skin diseases are not associated with substantial functional impairment, they can have significant adverse effects on the psychological health of sufferers and the overall quality of life (QoL) [40]. Further, the presence of certain other psychological conditions, such as depression, anxiety, stress, and sleep disorders can lead to increased dermatologic symptoms [40]. Hong and colleagues proposed that the psychosocial and occupational impact of cutaneous illnesses can be comparable to other chronic medical conditions [41].
Yew and colleagues conducted an evaluation of an adult population in Singapore [42]. These investigators found that individuals who had a history of skin diseases scored significantly higher on the indices of depression (1.3 in patients vs. 0.6 in controls, p < 0.001), and loneliness (3.5 vs. 3.3, p = 0.002). In addition, the skin disease group scored significantly lower on the social network index (15.9 vs. 16.6, p = 0.043), and the health-related quality of life index (0.89 vs. 0.95, p < 0.001). Demographic measures revealed that participants with skin diseases were less likely to be employed, and more likely to have financial constraints and alcohol misuse when compared to their healthy counterparts [42]. Individuals with skin disease reported higher prevalence of chronic conditions such as diabetes, hypertension, pulmonary disease and arthritis [42]. Dalgard and colleagues conducted a study among 4994 participants (3635 patients and 1359 controls) to evaluate the psychological impact of dermatologic diseases [43]. Using the Hospital Anxiety and Depression (HAD) scale these investigators reported that, compared to control subjects, dermatologic patients had a higher incidence of depression (10.1% in patients vs. 4.3% in controls), anxiety (17.2% vs. 11.1%), and suicidal ideation (12.7% vs. 8.3%). Costeris and colleagues investigated the influence of dermatological disorders on self-esteem and perceived social support in three groups of subjects: patients with severe visible facial acne, patients with non-visible psoriasis/eczema, and control groups composed of participants without dermatologic disorder [44]. Both patient groups showed lower self-esteem and lower perceived social support compared to the control group.
Misery and colleagues evaluated approximately 2000 subjects (1003 women and 935 men) using Short-Form 12 (SF-12) to evaluate the overall QoL [45]. Calculations were made for a Physical Component Summary (PCS-12) and a Mental Component Summary (MCS-12). These investigators found that the MCS-12 score was impaired in individuals with SSS, and the impairment increased in parallel with the severity of the SSS. In a later study these authors showed a similar result with a larger sample of 5000 individuals (2557 women and 2443 men) [23].
In 2018, Misery and colleagues developed a 14-item instrument, the Burden of Sensitive Skin (BoSS) questionnaire, designed specifically to determine the impact of SSS on QoL [7,46]. The BoSS questionnaire is composed of items grouped into three dimensions: Self-Care, Daily Life, and Appearance. The BoSS mean total score for subjects without sensitive skin was 14.05. For subjects with sensitive facial skin the BoSS score was significantly worse at 25.61 (p < 0.001). Further, the sensitive subjects had worse scores for each of the 3 BoSS dimensions: Self-Care (14.93 for sensitive subjects vs. 8.20 for non-sensitive), Daily Life (4.64 vs. 2.10), and Appearance (6.03 vs. 3.76), all p < 0.001 (Figure 2) [46].
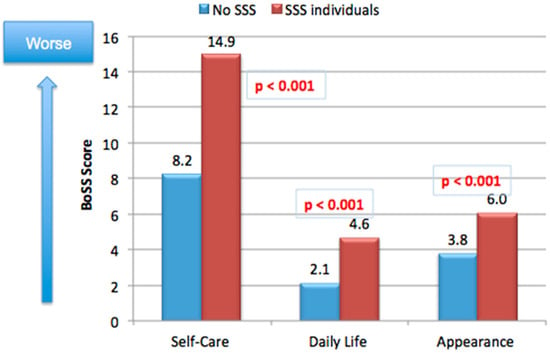
Figure 2.
Burden of Sensitive Skin (BoSS). Authors used the 14-item BoSS instrument to evaluate the impact of SSS on the quality of life [7,46]. The instrument evaluated three dimensions (Self-Care, Daily Life, and Appearance). Subjects included 100 women, 59 with self-declared sensitive skin and 41 without sensitive skin. Adapted from [46].
4. Impact of SSS on The Daily Life of Consumers
4.1. Consumers’ Behavior: Avoidance and Shopping Practices
Individuals with SSS have identified a wide variety of environmental factors that can trigger their symptoms (reviewed in [1]). These include extremes of humidity (dry or wet weather), extremes of temperature (cold or hot), wind, sun, air conditioning, dust and pollution (Table 3). Lifestyle and personal habits can also trigger symptoms, such as wearing rough fabrics, the use of cosmetics, and exposure to tobacco smoke. A wide array of triggering conditions must be avoided in order to circumvent the onset of SSS symptoms. Such avoidance may lead to a restriction of outdoor or indoor activities important for social interactions, leisure, recreation and fitness [35].

Table 3.
Reported Environmental and Lifestyle Triggers of SSS.
Factors that contribute to the symptoms of SSS may differ depending on age group. Among those who claimed to have sensitive skin, hot weather and rough fabrics were the factors most strongly associated with skin sensitivity among the oldest adults (aged 50 and above) and were specifically associated with genital skin sensitivity in this group (Table 4) [1]. Cold weather was most strongly associated with skin sensitivity in midlife (40–49 age group); and stress was the most important factor cited by younger adults (i.e., individuals under 40) [1]. The menstrual cycle was perceived to contribute to skin sensitivity by women of all age groups except those aged ≥50.

Table 4.
Perceptions about irritation due to environmental factors for those claiming genital skin sensitivity.
A large number of everyday products were identified by SSS individuals as potential triggers to SSS symptoms. These include facial products and cosmetics, personal care products, and common household products (Figure 3). A Cincinnati study reported by Farage with 1039 individuals reported that 68.4% of the study population claimed their skin was sensitive to some degree (very, moderately, or slightly) [49]. SSS seems to also influence shopping behavior and practices. Subjects claiming SSS were 5 times more likely to look for skin related claims on products (such as, “safe for sensitive skin” and “hypoallergenic”) compared to non-sensitive subjects (OR = 5.3) (Figure 4a), and 5 times more likely to avoid specific ingredients because the individual perceived they caused skin irritation (OR = 5.2) (Figure 4b).
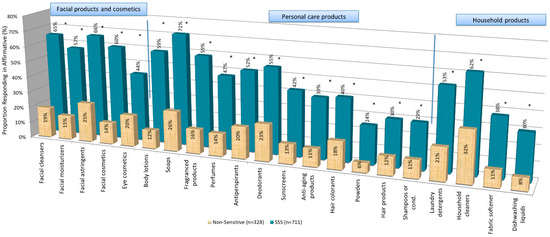
Figure 3.
Product Categories Reported to Trigger SSS Symptoms. Responders in the Cincinnati study were asked if a variety of categories of cosmetics, personal care and household products had ever caused adverse reactions to their skin [35,36]. For all product categories the proportion of SSS individuals who responded positively was significantly higher than the number of non-SSS individuals who responded positively. (* = p < 0.00001).
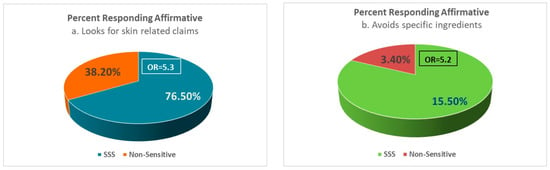
Figure 4.
SSS Consumers and Shopping Practices. In the Cincinnati study, responders were asked about specific shopping practices. Compared to the non-SS group, the SS subjects were far more likely to: (a) look for skin related claims on products (such as, “safe for sensitive skin” and “hypoallergenic”) (OR = 5.3), and (b) avoid specific ingredients when shopping (OR = 5.2).
Consumer product manufacturers are now fully aware of the need to develop products specifically for individuals with SSS. Our laboratory developed and validated a self-administered scientific tool, (the Farage Quality of Life [FQoLTM]), to assess the potential impact of a variety of consumer products on Health Related QoL (HRQoL) [50,51]. The tool consists of 27 general items scored on a Likert scale and covering Overall Quality of Life (1 item), Well-Being (12 items), and Energy and Vitality (14 items). The Well-Being domain has 3 subscales: Emotion, Self-Image, and Self-Competence; the Energy and Vitality domain also has 3 subscales: Personal Pleasure, Physical State, and Routine Activity. The resulting FQoLTM instrument has been used several times to evaluate the impact of various consumer products on the consumers’ quality of life [52].
4.2. Fatigue and Sleep Disorders
Fatigue has a high prevalence among patients with skin diseases [53]. In a study conducted in France by Misery and colleagues among 2502 individuals, these authors found the risk of fatigue was over four times greater for individuals with skin diseases compared to those with no skin diseases [54]. Sleep disorders and fatigue are common in patients with inflammatory skin disorders, such as psoriasis and chronic eczema [55], and have been reported as upstream drivers of other sensory disorders [48].
Itch and pain are major symptoms of sensitive skin and can contribute to sleep disorders [11]. In a 2019 publication, Schmelz reported that individuals classified as having sensitive skin experienced itching and pain sensations upon weak external stimuli that are not typically painful or itchy in individuals without sensitive skin [56]. Halioua and colleagues found that subjects suffering from cutaneous disorders had a significantly higher severity of sleep disorders compared to control subjects without cutaneous disorders (4.1 ± 2.51 versus 3.5 ± 2.3, respectively, p = 0.0019) [57]. These authors found that pain and pruritus were good predictors of sleep disturbance with odds ratios of 1.7 [95% CI 1.4–2.0] (p < 0.0001), and 1.6 [95% CI 1.3–2.0] (p < 0.0001), respectively.
Misery and colleagues conducted a survey among 5 different countries [48]. Participants were asked to rate the severity of sleep disorders and unpleasant skin sensations on numerical scales with 0 being no disturbance and 10 being the maximum. A score of <3 was considered mild, between 3 to ≤7 was considered moderate, and ≥7 was considered severe. Among the 10,743 participants 8296 subjects reported sleep disorders. Approximately half of these (4295 or 51.77%) also reported SSS. Subjects with SSS had significantly worse (higher) scores for sleep disorders (3.6 out of 10) compared to subjects without sensitive skin (1.6 out of 10) (p < 0.001) [48]. Xiao and colleagues found similar results in a China study which included 22,085 women [34]. These authors reported that SSS was more likely in individuals who slept 6 h compared to 8 h (OR 1.36, p = 0.001), and in individuals retiring at or later than 2 a.m. compared to 10 p.m. (OR 1.81, p = 0.007).
4.3. Stress, Anxiety and Depression
Depression, anxiety and emotional distress can have a deleterious effect on many conditions including dermatological diseases and may initiate the itch-scratch cycle [58]. Stressors such as helplessness and worrying may have a role in worsening the itch sensation of patients with skin diseases [59]. Dalgard and colleagues reported a study conducted with 3635 dermatology out- patients with common skin diseases and 1359 controls [43]. Subjects were administered the Hospital Anxiety and Depression Scale (HADS) questionnaire. Among the patient group, 35.6% reported stress compared with 30.6% of the controls (p < 0.001). In addition, the patient groups demonstrated a significantly higher prevalence of clinical depression (10.1% in patient group vs. 4.3% in the control group, p < 0.001), anxiety (17.2% vs. 11.1%, p < 0.001), and suicidal ideation (12.7% vs. 8.3%) [43].
Stress has been known to trigger dermatological conditions such as psoriasis, rosacea and atopic dermatitis [60,61,62]. In the study conducted by Farage, stress was identified as a contributing factor to skin irritation by 51% of the total subjects responders (485 out of 954) [47]. Stress was perceived as a contributor by 63% (415 out of 654) of SSS subjects, compared to 24% (70 out of 290) of the subjects without SSS (p < 0.0005) [1,47]. Saint–Martory and colleagues reported a similar result among 400 women in France, where about 61% of the participants who perceived sensitive skin of the face identified stress as a contributing factor [63].
In a study conducted by Misery and colleagues among 1000 subjects in the USA, skin reactivity to emotion was significantly higher among individuals who identified as having “sensitive” or “very sensitive” skin compared to individuals who identified as “slightly” or non-sensitive skin. (53% vs. 47%; p < 0.001) [33].
SSS individuals are more likely to feel stress. Misery and colleagues evaluated Quality of Life (QoL) using the SF-12 questionnaire [45]. Individuals with sensitive or very sensitive skin had a worse QoL than individuals without. In addition, the QoL deteriorated as the severity of sensitive skin increased. More recent studies have also shown similar results [23,64]. Stress was reported as a trigger of unpleasant skin symptoms by 63% of the SSS subjects in a study involving 1039 subjects [47]. In that same study responders in different age groups were asked if they had some degree of genital sensitivity, and whether or not specific environmental factors triggered the unpleasant sensations of SSS in the genital area [29]. Overall, 58% of individuals with irritation in the genital area claimed stress was a trigger. Xiao and colleagues reported that the likelihood of SSS increased with the amount of stress in the lifestyle [34]. Compared to individuals with no stress in their lives, SSS was more likely in individuals who experienced mild stress (OR 1.31, p = 0.001), or heavy stress (OR 1.57, p = 0.001).
4.4. The Stress of COVID Containment
Kluger and colleagues evaluated the potential effects of containment during the 2020–2021 COVID-19 pandemic and its effects on skin condition among subjects in 5 countries (Brazil, China, France, Russia and the USA) [65]. The study included 7170 individuals who reported they complied with containment procedures. Among those, 20.9% (1500 out of 7170) responded that their skin condition had worsened due to containment. The three main reported changes were drier skin (44.5%), skin rash (29.3%), and greasier skin (27%). The investigators suggested that mask wearing and stress may have contributed to skin condition changes. Subjects were then divided into a SSS group including 3410 individuals (47.6%) who reported they had sensitive or very sensitive facial skin, and a non-sensitive group including 3760 individuals (52.4%) who had skin that was not very sensitive or not at all sensitive. Individuals in the SSS group were more likely to report skin changes during containment compared to the non-sensitive group (27.7% vs. 14.8%, respectively, p < 0.00001).
As mentioned previously, our laboratory developed and validated an instrument to assess the potential impact of various consumer products on QoL (i.e., the FQoL) [50,51]. We were conducting a study among 63 healthy women aged 23–54 years old for a consumer product using the FQoLTM when the COVID-19 pandemic hit. We took advantage of this study to gain insights on the impact of COVID-19 on the different FQoLTM domains and sub-domains. Responses to the instrument had been collected on 19 February 2020 which was prior to the 15 March 2020 pandemic stay-at-home orders (i.e., Pre-COVID). A second set of responses were collected in the early days of the stay-at-home mandate (i.e., Early COVID), and a third set after 24 days of at-home confinement (i.e., Day 24 of COVID-19 on 7 April 2020). Results of the domain analyses in the previously unpublished study are presented in Figure 5. We observed a significant decline in overall quality of life, and in the Well-Being domain and the Energy and Vitality domain.
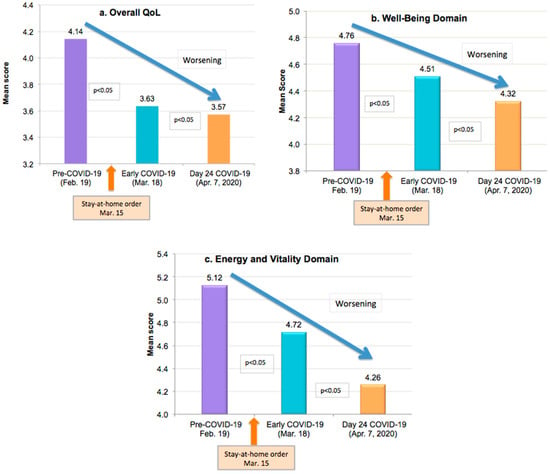
Figure 5.
Effect of COVID-19 Confinement on QoL. The study was conducted among 63 healthy women aged 23–54 years old. Responses to the FQoLTM were collected prior to the 2020 pandemic stay-at-home orders (19 February), 3 days after the 15 March stay-at-home orders (18 March), and 24 days after the stay-at-home orders (7 April). Mean scores for the overall QoL (a), the Well-Being Domain (b), and the Energy and Vitality Domain (c) are presented. The subdomains and domains were averages of responses to individual items within that grouping, and means were. evaluated using a paired t-test. The 2-sided p values are reported. All analyses were done using JMP Pro version 14.2.0 and SAS 9.4 (Baiyang Wang-Statistician).
When subdomains were further evaluated (Table 5), everyone exhibited a significant worsening of scores. One very interesting finding was within the Personal Pleasure subdomain. This subdomain includes questions about things individuals do for leisure and recreation. A large percentage of respondents (71.4%) checked the “not applicable” option, which is a true reflection of an absence of activities during the stay-at-home orders.

Table 5.
Quality of Life Pre- and Post-COVID Stay-At-Home Orders.
5. Conclusions
Many dermatological diseases are associated with problems such as depression, anxiety, stress, and sleep disorders. The same can be said for SSS. Although SSS does not present with objectively treatable signs and symptoms, individuals with SSS can suffer from the same psychological problems. In addition, individuals with SSS are more likely to suffer from co-morbidities and other skin disorders such as acne, atopic dermatitis, psoriasis, rosacea, vitiligo, or contact dermatitis. This can lead to feelings of helplessness and worry that can further exacerbate symptoms of SSS such as itch and irritation and can result in sleep disorders, fatigue, stress and anxiety. Conversely, lack of sleep and stress from these sources can make the SSS sufferer more prone to the symptoms. This becomes a vicious cycle that impacts consumers’ quality of life and well-being.
Individuals with SSS have identified a wide array of external factors that can trigger their symptoms, including weather and environmental conditions, and exposure to a multitude of household and personal products. Attempts to avoid such factors in order to circumvent the onset of SSS symptoms can result in restriction of outdoor or indoor activities important for social interactions, leisure, recreation and fitness. Questionnaire-based Quality of Life type instruments have demonstrated that sensitive skin subjects score worse in satisfaction with appearance, daily life and a sense of well-being. Subjects with SSS had significantly worse scores for sleep disorders compared to subjects without sensitive skin.
Becoming aware of the vicious psychological cycle that can impact SSS individual can help both the practitioner and consumer to understand, manage and develop more appropriate approaches and programs (i.e., treatments; therapies, etc.) to drive a more holistic well- being impact for SSS consumers.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The author would like to thank Terresa L. Nusair for technical assistance with the manuscript.
Conflicts of Interest
Author is an employee of the Procter and Gamble Company.
References
- Farage, M.A. Understanding the Sensitive Skin Subject to Achieve a More Holistic Diagnosis. Cosmetics 2021, 8, 81. [Google Scholar] [CrossRef]
- Bataille, A.; Gall-Ianotto, C.L.; Genin, E.; Misery, L. Sensitive Skin: Lessons from Transcriptomic Studies. Front. Med. 2019, 6, 115. [Google Scholar] [CrossRef]
- Misery, L.; Ständer, S.; Szepietowski, J.C.; Reich, A.; Wallengren, J.; Evers, A.W.; Takamori, K.; Brenaut, E.; Gall-Ianotto, C.L.; Fluhr, J.; et al. Definition of Sensitive Skin: An Expert Position Paper from the Special Interest Group on Sensitive Skin of the International Forum for the Study of Itch. Acta Derm. Venereol. 2017, 97, 4–6. [Google Scholar] [CrossRef]
- Berardesca, E.; Farage, M.; Maibach, H. Sensitive skin: An overview. Int. J. Cosmet. Sci. 2013, 35, 2–8. [Google Scholar] [CrossRef]
- Farage, M.A. The Prevalence of Sensitive Skin. Front. Med. 2019, 6, 98. [Google Scholar] [CrossRef]
- Chen, W.; Dai, R.; Li, L. The prevalence of self-declared sensitive skin: A systematic review and meta-analysis. J. Eur. Acad. Dermatol. Venereol. 2019, 34, 1779–1788. [Google Scholar] [CrossRef]
- Misery, L.; Jourdan, E.; Abadie, S.; Ezzedine, K.; Brenaut, E.; Huet, F.; Sayag, M.; Taieb, C. Development and validation of a new tool to assess the Burden of Sensitive Skin (BoSS). J. Eur. Acad. Dermatol. Venereol. 2018, 32, 2217–2223. [Google Scholar] [CrossRef]
- Cho, H.J.; Chung, B.Y.; Lee, H.B.; Kim, H.O.; Park, C.W.; Lee, C.H. Quantitative study of stratum corneum ceramides contents in patients with sensitive skin. J. Dermatol. 2012, 39, 295–300. [Google Scholar] [CrossRef]
- Cua, A.B.; Wilhelm, K.P.; Maibach, H.I. Cutaneous sodium lauryl sulphate irritation potential: Age and regional variability. Br. J. Dermatol. 1990, 123, 607–613. [Google Scholar] [CrossRef]
- Pons-Guiraud, A. Sensitive skin: A complex and multifactorial syndrome. J. Cosmet. Dermatol. 2004, 3, 145–148. [Google Scholar] [CrossRef]
- Misery, L.; Weisshaar, E.; Brenaut, E.; Evers, A.; Huet, F.; Ständer, S.; Reich, A.; Berardesca, E.; Serra-Baldrich, E.; Wallengren, J.; et al. Pathophysiology and management of sensitive skin: Position paper from the special interest group on sensitive skin of the International Forum for the Study of Itch (IFSI). J. Eur. Acad. Dermatol. Venereol. 2020, 34, 222–229. [Google Scholar] [CrossRef]
- Roussaki-Schulze, A.V.; Zafiriou, E.; Nikoulis, D.; Klimi, E.; Rallis, E.; Zintzaras, E. Objective biophysical findings in patients with sensitive skin. Drugs Exp. Clin. Res. 2005, 31, 17–24. [Google Scholar]
- Misery, L.; Loser, K.; Ständer, S. Sensitive skin. J. Eur. Acad. Dermatol. Venereol. 2016, 30 (Suppl. 1), 2–8. [Google Scholar] [CrossRef]
- Buhé, V.; Vié, K.; Guéré, C.; Natalizio, A.; Lhéritier, C.; Gall-Ianotto, C.; Huet, F.; Talagas, M.; Lebonvallet, N.; Marcorelles, P.; et al. Pathophysiological Study of Sensitive Skin. Acta Derm. Venereol. 2016, 96, 314–318. [Google Scholar] [CrossRef]
- Ehnis-Pérez, A.; Torres-Álvarez, B.; Cortés-García, D.; Hernández-Blanco, D.; Fuentes-Ahumada, C.; Castanedo-Cázares, J.P. Relationship between transient receptor potential vanilloid-1 expression and the intensity of sensitive skin symptoms. J. Cosmet. Dermatol. 2016, 15, 231–237. [Google Scholar] [CrossRef]
- Kueper, T.; Krohn, M.; Haustedt, L.O.; Hatt, H.; Schmaus, G.; Vielhaber, G. Inhibition of TRPV1 for the treatment of sensitive skin. Exp. Dermatol. 2010, 19, 980–986. [Google Scholar] [CrossRef]
- Mikkelsen, C.S.; Holmgren, H.R.; Kjellman, P.; Heidenheim, M.; Kappinnen, A.; Bjerring, P.; Huldt-Nystrøm, T. Rosacea: A Clinical Review. Dermatol. Rep. 2016, 8, 6387. [Google Scholar] [CrossRef]
- Chang, A.L.S.; Raber, I.; Xu, J.; Li, R.; Spitale, R.; Chen, J.; Kiefer, A.K.; Tian, C.; Eriksson, N.K.; Hinds, D.A.; et al. Assessment of the genetic basis of rosacea by genome-wide association study. J. Investig. Dermatol. 2015, 135, 1548–1555. [Google Scholar] [CrossRef]
- Kim, Y.R.; Cheon, H.I.; Misery, L.; Taieb, C.; Lee, Y.W. Sensitive skin in Korean population: An epidemiological approach. Skin Res. Technol. 2018, 24, 229–234. [Google Scholar] [CrossRef]
- Brenaut, E.; Misery, L.; Taieb, C. Sensitive Skin in the Indian Population: An Epidemiological Approach. Front. Med. 2019, 6, 29. [Google Scholar] [CrossRef]
- Wang, X.Y.; Liu, Y.Y.; Liu, Y.X.; Ma, W.W.; Zhang, J.W.; Liu, Z.J.; Liu, J.; Zhou, B.R.; Xu, Y. A predictive model for differential diagnosis between rosacea and sensitive skin: A cross-sectional study. Chin. Med. J. 2020, 133, 2132–2134. [Google Scholar] [CrossRef]
- Willis, C.M.; Shaw, S.; De Lacharriere, O.; Baverel, M.; Reiche, L.; Jourdain, R.; Bastien, P.; Wilkinson, J.D. Sensitive skin: An epidemiological study. Br. J. Dermatol. 2001, 145, 258–263. [Google Scholar] [CrossRef]
- Misery, L.; Jourdan, E.; Huet, F.; Brenaut, E.; Cadars, B.; Virassamynaïk, S.; Sayag, M.; Taieb, C. Sensitive skin in France: A study on prevalence, relationship with age and skin type and impact on quality of life. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 791–795. [Google Scholar] [CrossRef]
- Farage, M.A.; Bowtell, P.; Katsarou, A. Self-diagnosed sensitive skin in women with clinically diagnosed atopic dermatitis. Clin. Med. Dermatol. 2008, 2, 21–28. [Google Scholar]
- Farage, M.A.; Jiang, Y.; Tiesman, J.P.; Fontanillas, P.; Osborne, R. Genome-Wide Association Study Identifies Loci Associated with Sensitive Skin. Cosmetics 2020, 7, 49. [Google Scholar] [CrossRef]
- Misery, L.; Cochener, B.; Brenaut, E.; Séité, S.; Taieb, C. Association of sensitive skin with sensitive corneas and sensitive eyelids. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 1358–1362. [Google Scholar] [CrossRef]
- Misery, L.; Duboc, H.; Coffin, B.; Brenaut, E.; Huet, F.; Taieb, C. Association between two painful and poorly understood conditions: Irritable bowel and sensitive skin syndromes. Eur. J. Pain 2019, 23, 160–166. [Google Scholar] [CrossRef]
- Huet, F.; Misery, L. Sensitive skin is a neuropathic disorder. Exp. Dermatol. 2019, 28, 1470–1473. [Google Scholar] [CrossRef]
- Farage, M.A. Perceptions of Sensitive Skin with Age. In Textbook of Aging Skin, 2nd ed.; Farage, M.A., Miller, K.W., Maibach, H.I., Eds.; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Robinson, M.K. Population differences in acute skin irritation responses. Race, sex, age, sensitive skin and repeat subject comparisons. Contact Dermat. 2002, 46, 86–93. [Google Scholar] [CrossRef]
- Lejman, E.; Stoudemayer, T.; Grove, G.; Kligman, A.M. Age differences in poison ivy dermatitis. Contact Dermat. 1984, 11, 163–167. [Google Scholar] [CrossRef]
- Grove, G.L.; Duncan, S.; Kligman, A.M. Effect of ageing on the blistering of human skin with ammonium hydroxide. Br. J. Dermatol. 1982, 107, 393–400. [Google Scholar] [CrossRef]
- Misery, L.; Sibaud, V.; Merial-Kieny, C.; Taieb, C. Sensitive skin in the American population: Prevalence, clinical data, and role of the dermatologist. Int. J. Dermatol. 2011, 50, 961–967. [Google Scholar] [CrossRef]
- Xiao, X.; Qiao, L.; Ye, R.; Zuo, F. Nationwide Survey and Identification of Potential Stress Factor in Sensitive Skin of Chinese Women. Clin. Cosmet. Investig. Dermatol. 2020, 13, 867–874. [Google Scholar] [CrossRef]
- Farage, M.A. Does sensitive skin differ between men and women? Cutan. Ocul. Toxicol. 2010, 29, 153–163. [Google Scholar] [CrossRef]
- Farage, M.A.; Mandl, C.P.; Berardesca, E.; Maibach, H.I. Sensitive Skin in China. J. Cosmet. Dermatol. Sci. Appl. 2012, 2, 184–195. [Google Scholar] [CrossRef][Green Version]
- Farage, M.A. Sensitive skin in the genital area. Front. Med. 2019, 6, 142–154. [Google Scholar] [CrossRef]
- Farage, M.A.; Neill, S.; MacLean, A.B. Physiological changes associated with the menstrual cycle: A review. Obstet. Gynecol. Surv. 2009, 64, 58–72. [Google Scholar] [CrossRef]
- Falcone, D.; Richters, R.J.; Uzunbajakava, N.E.; Van Erp, P.E.; Van De Kerkhof, P.C. Sensitive skin and the influence of female hormone fluctuations: Results from a cross-sectional digital survey in the Dutch population. Eur. J. Dermatol. 2017, 27, 42–48. [Google Scholar] [CrossRef]
- Barankin, B.; DeKoven, J. Psychosocial effect of common skin diseases. Can. Fam. Physician 2002, 48, 712–716. [Google Scholar]
- Hong, J.; Koo, B.; Koo, J. The psychosocial and occupational impact of chronic skin disease. Dermatol. Ther. 2008, 21, 54–59. [Google Scholar] [CrossRef]
- Yew, Y.W.; Kuan, A.H.Y.; Ge, L.; Yap, C.W.; Heng, B.H. Psychosocial impact of skin diseases: A population-based study. PLoS ONE 2020, 15, e0244765. [Google Scholar] [CrossRef]
- Dalgard, F.J.; Gieler, U.; Tomas-Aragones, L.; Lien, L.; Poot, F.; Jemec, G.B.E.; Misery, L.; Szabo, C.; Linder, D.; Sampogna, F.; et al. The psychological burden of skin diseases: A cross-sectional multicenter study among dermatological out-patients in 13 European countries. J. Investig. Dermatol. 2015, 135, 984–991. [Google Scholar] [CrossRef]
- Costeris, C.; Petridou, M.; Ioannou, Y. Psychological Impact of Skin Disorders on Patients’ Self-esteem and Perceived Social Support. J. Dermatol. Ski. Sci. 2021, 3, 14–22. [Google Scholar]
- Misery, L.; Myon, E.; Martin, N.; Consoli, S.; Boussetta, S.; Nocera, T.; Taieb, C. Sensitive skin: Psychological effects and seasonal changes. J. Eur. Acad. Dermatol. Venereol. 2007, 21, 620–628. [Google Scholar] [CrossRef]
- Polena, H.; Chavagnac-Bonneville, M.; Misery, L.; Sayag, M. Burden of Sensitive Skin (BoSS) Questionnaire and Current Perception Threshold: Use as Diagnostic Tools for Sensitive Skin Syndrome. Acta Derm. Venereol. 2021, 101, adv00606. [Google Scholar] [CrossRef]
- Farage, M.A. Perceptions of sensitive skin: Changes in perceived severity and associations with environmental causes. Contact Dermat. 2008, 59, 226–232. [Google Scholar] [CrossRef]
- Misery, L.; Morisset, S.; Séité, S.; Brenaut, E.; Ficheux, A.S.; Fluhr, J.W.; Delvigne, V.; Taieb, C. Relationship between sensitive skin and sleep disorders, fatigue, dust, sweating, food, tobacco consumption or female hormonal changes: Results from a worldwide survey of 10 743 individuals. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 1371–1376. [Google Scholar] [CrossRef]
- Farage, M.A. How do perceptions of sensitive skin differ at different anatomical sites? An epidemiological study. Clin. Exp. Dermatol. 2009, 34, e521–e530. [Google Scholar] [CrossRef]
- Farage, M.A.; Nusair, T.L.; Hanseman, D.; Sherman, S.N.; Tsevat, J. The Farage Quality of Life Measure for Consumer Products: Development and Initial Implementation. Appl. Res. Qual. Life 2010, 5, 1–25. [Google Scholar] [CrossRef]
- Farage, M.A.; Rodenberg, C.; Chen, J. Translation and Validation of the Farage Quality of Life (FQoL) Instrument for Consumer Products into Traditional Chinese. Glob. J. Health Sci. 2013, 5, 1–12. [Google Scholar] [CrossRef][Green Version]
- Zhang, L.; Adique, A.; Sarkar, P.; Shenai, V.; Sampath, M.; Lai, R.; Qi, J.; Wang, M.; Farage, M.A. The Impact of Routine Skin Care on the Quality of Life. Cosmetics 2020, 7, 59. [Google Scholar] [CrossRef]
- Verhoeven, E.W.; Kraaimaat, F.W.; van de Kerkhof, P.C.; van Weel, C.; Duller, P.; van der Valk, P.G.; van den Hoogen, H.J.; Bor, J.H.; Schers, H.J.; Evers, A.W. Prevalence of physical symptoms of itch, pain and fatigue in patients with skin diseases in general practice. Br. J. Dermatol. 2007, 156, 1346–1349. [Google Scholar] [CrossRef]
- Misery, L.; Shourick, J.; Taieb, C. Prevalence and characterization of fatigue in patients with skin diseases. Acta Derm. Venereol. 2020, 100, adv00327. [Google Scholar] [CrossRef]
- Mostaghimi, L.; Hetzel, S. Insomnia and other sleep complaints in inflammatory versus noninflammatory skin disorders: An observational case-control study. Int. J. Dermatol. 2019, 58, 976–981. [Google Scholar] [CrossRef]
- Schmelz, M. Itch Processing in the Skin. Front. Med. 2019, 6, 167. [Google Scholar] [CrossRef]
- Halioua, B.; Misery, L.; Seite, S.; Delvigne, V.; Chelli, C.; Taieb, J.; Taieb, C. Influence of Skin Subjective Symptoms on Sleep Quality in Patients with Cutaneous Disorders: A Study of 2871 Subjects. Clin. Cosmet. Investig. Dermatol. 2021, 14, 143–152. [Google Scholar] [CrossRef]
- Osman, O.T.; Mufaddel, A.; Almugaddam, F.; Augusterfer, E.F. The psychiatric aspects of skin disorders. Expert Rev. Dermatol. 2011, 6, 195–209. [Google Scholar] [CrossRef]
- Verhoeven, E.W.; de Klerk, S.; Kraaimaat, F.W.; van de Kerkhof, P.C.; de Jong, E.M.; Evers, A.W. Biopsychosocial mechanisms of chronic itch in patients with skin diseases: A review. Acta Derm. Venereol. 2008, 88, 211–218. [Google Scholar]
- Huynh, T.T. Burden of Disease: The Psychosocial Impact of Rosacea on a Patient’s Quality of Life. Am. Health Drug Benefits 2013, 6, 348–354. [Google Scholar]
- Reich, A.; Wójcik-Maciejewicz, A.; Slominski, A.T. Stress and the skin. G. Ital. Dermatol. Venereol. 2010, 145, 213–219. [Google Scholar]
- Blount, B.W.; Pelletier, A.L. Rosacea: A common, yet commonly overlooked, condition. Am. Fam. Physician 2002, 66, 435–440. [Google Scholar]
- Saint-Martory, C.; Roguedas-Contios, A.M.; Sibaud, V.; Degouy, A.; Schmitt, A.M.; Misery, L. Sensitive skin is not limited to the face. Br. J. Dermatol. 2008, 158, 130–133. [Google Scholar] [CrossRef]
- Misery, L.; Jean-Decoster, C.; Mery, S.; Georgescu, V.; Sibaud, V. A new ten-item questionnaire for assessing sensitive skin: The Sensitive Scale-10. Acta Derm. Venereol. 2014, 94, 635–639. [Google Scholar] [CrossRef]
- Kluger, N.; Floc’h, C.L.; Niore, M.; Delvigne, V.; Dantec, G.L.; Taieb, C. Self-Reported Skin Sensation by People Who Have Experienced Containment During COVID-19 Pandemic. Clin. Cosmet. Investig. Dermatol. 2020, 13, 943–947. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).