Knowledge, Attitude and Practice Regarding Antibacterial and Their Resistance in Medellín-Colombia: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population, Sample, and Sampling
2.3. Survey
2.4. Data Analysis
3. Results
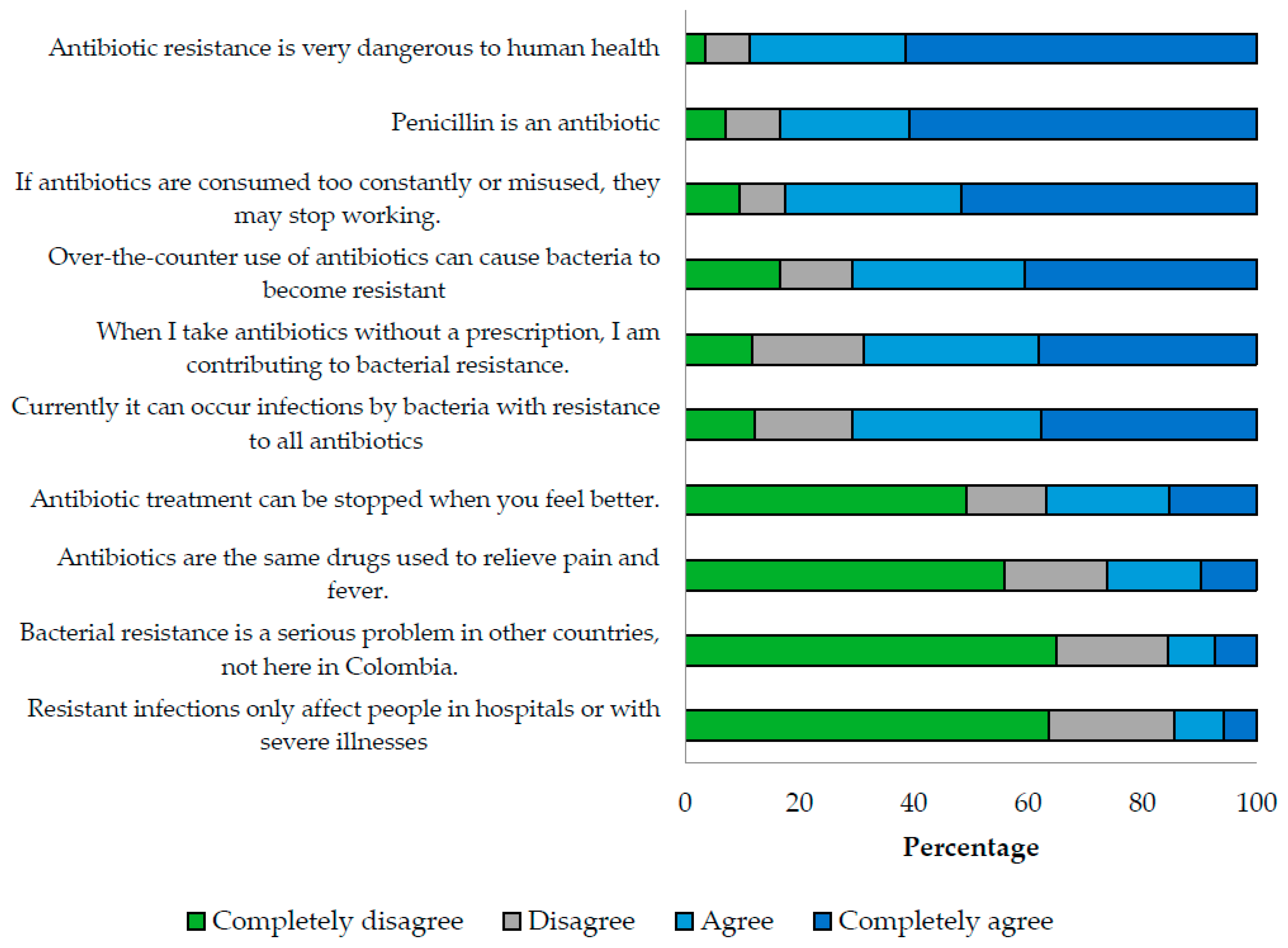
3.1. Knowledge Index
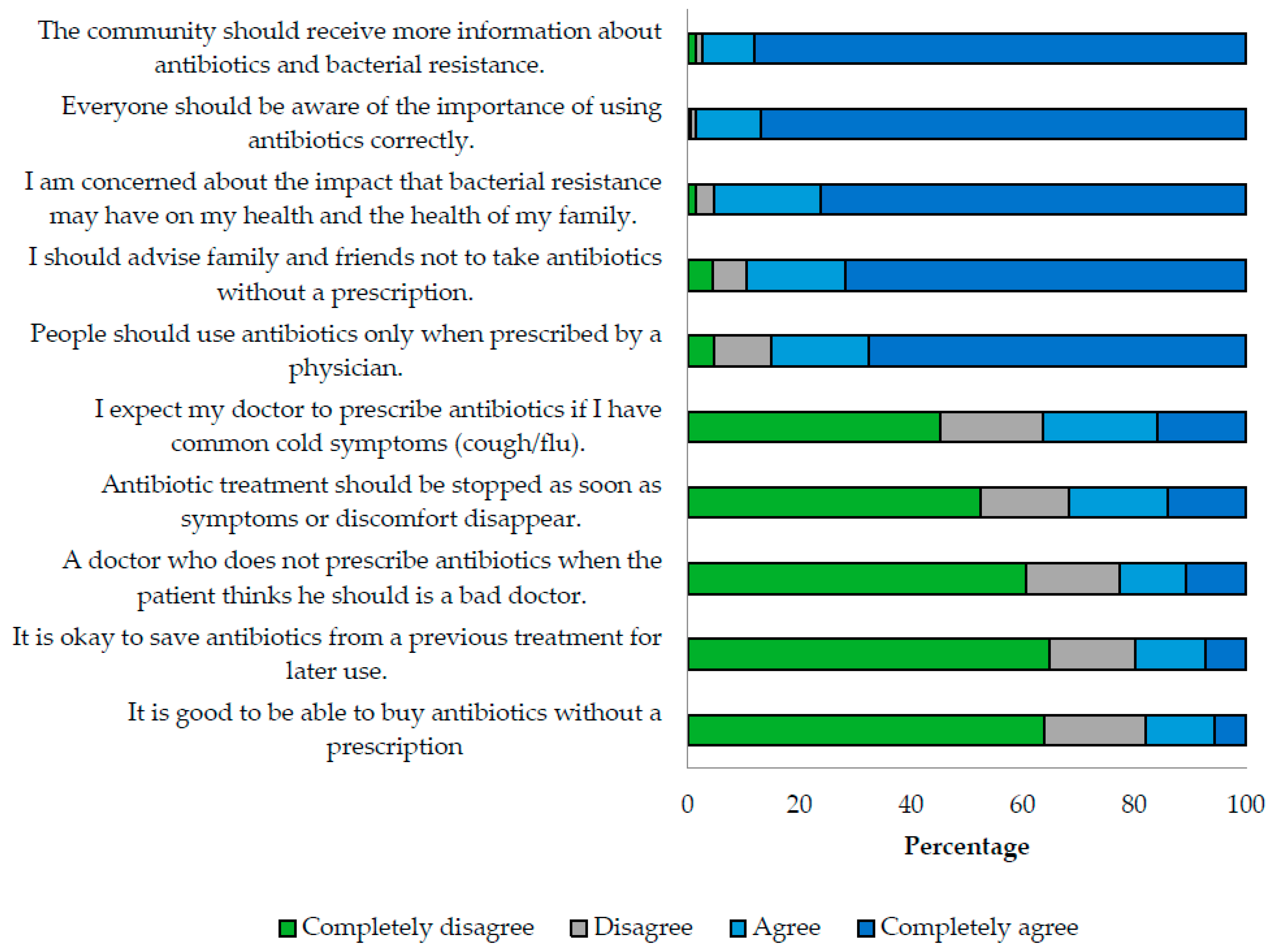
3.2. Attitude Index
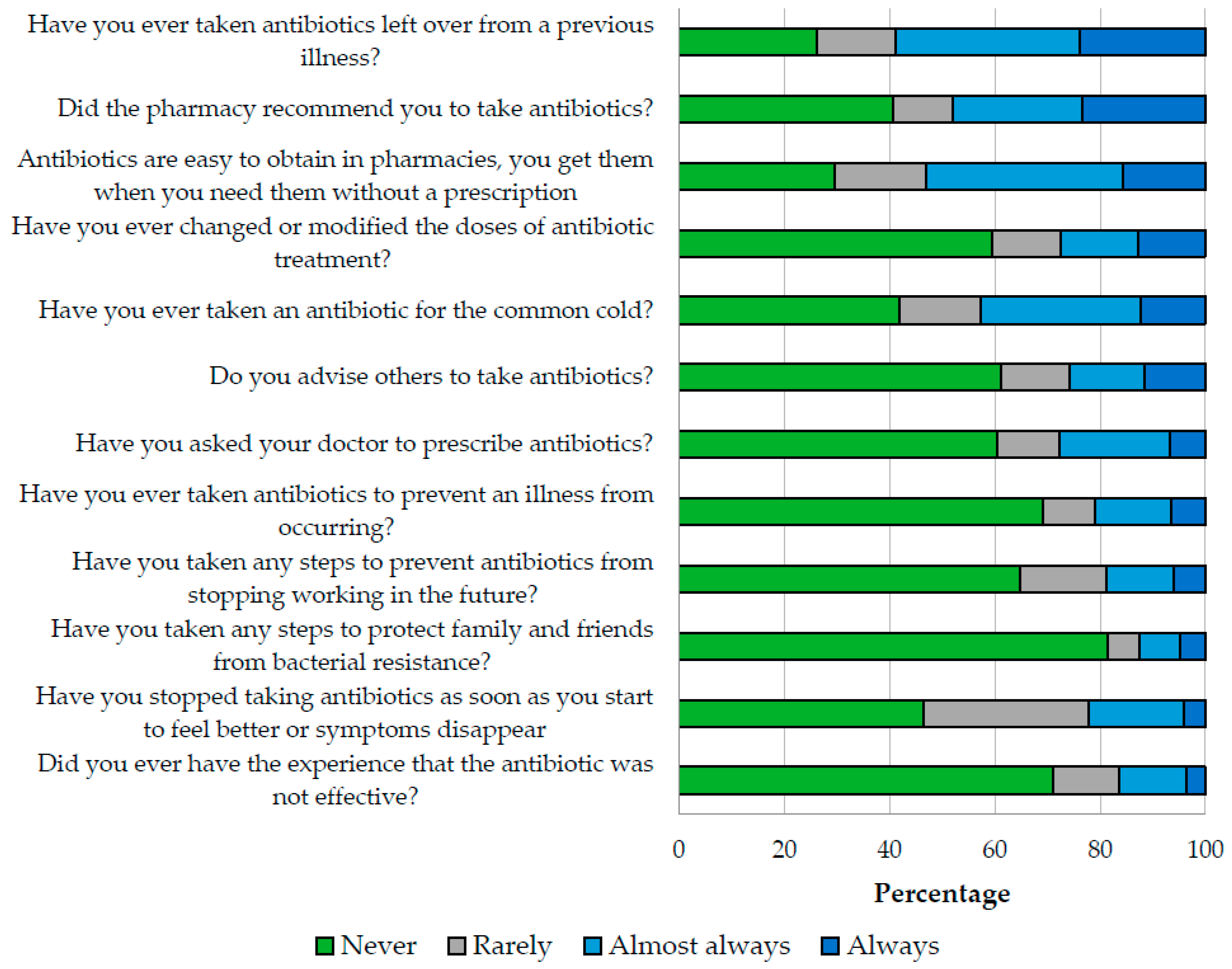
3.3. Practice Index
3.4. Factors Associated with Knowledge, Attitude and Practice
3.5. Relationship between Knowledge, Attitudes, and Practices
3.6. Psychometric Properties of the Instrument
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Ten Threats to Global Health in 2019. World Health Organization. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 20 February 2023).
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report: 2022; World Health Organization: 2022. Available online: https://www.who.int/publications/i/item/9789240062702 (accessed on 20 February 2023).
- Yezli, S.; Yassin, Y.; Mushi, A.; Maashi, F.; Aljabri, N.; Mohamed, G.; Bieh, K.; Awam, A.; Alotaibi, B. Knowledge, attitude and practice (KAP) survey regarding antibiotic use among pilgrims attending the 2015 Hajj mass gathering. Travel Med. Infect. Dis. 2019, 28, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Mason, T.; Trochez, C.; Thomas, R.; Babar, M.; Hesso, I.; Kayyali, R. Knowledge and awareness of the general public and perception of pharmacists about antibiotic resistance. BMC Public Health 2018, 18, 711. [Google Scholar] [CrossRef]
- General Assembly of the United Nations. Draft Political Declaration of the High-Level Meeting of the General Assembly on Antimicrobial Resistance; General Assembly of the United Nations: New York, NY, USA, 2016. [Google Scholar]
- Li, P.; Hayat, K.; Shi, L.; Lambojon, K.; Saeed, A.; Majid Aziz, M.; Liu, T.; Ji, S.; Gong, Y.; Feng, Z.; et al. Knowledge, attitude, and practices of antibiotics and antibiotic resistance among Chinese pharmacy customers: A multicenter survey study. Antibiotics 2020, 9, 184. [Google Scholar] [CrossRef]
- Zaidi, S.F.; Baroom, M.W.; Ibrahim Hanbashi, A.; Abdulaziz Alkhaibari, A.; Omar Yahya, A.; Alsalmi, M.; Alotaibi, R.; Nagro, A.; Anwar Khan, M.; Alshanberi, A.M. Cross-sectional survey among general population regarding knowledge and attitude toward antibiotic usage in western Saudi Arabia. Pharmacy 2021, 9, 98. [Google Scholar] [CrossRef] [PubMed]
- Farley, E.; van den Bergh, D.; Coetzee, R.; Stewart, A.; Boyles, T. Knowledge, attitudes and perceptions of antibiotic use and resistance among patients in South Africa: A cross-sectional study. S. Afr. J. Infect. Dis. 2019, 34, 118. [Google Scholar] [CrossRef] [PubMed]
- Bogale, A.A.; Amhare, A.F.; Chang, J.; Bogale, H.A.; Betaw, S.T.; Gebrehiwot, N.T.; Fang, Y. Knowledge, attitude, and practice of self-medication with antibiotics among community residents in Addis Ababa, Ethiopia. Expert Rev. Anti Infect. Ther. 2019, 17, 459–466. [Google Scholar] [CrossRef]
- Raupach-Rosin, H.; Rübsamen, N.; Schütte, G.; Raschpichler, G.; Chaw, P.S.; Mikolajczyk, R. Knowledge on antibiotic use, self-reported adherence to antibiotic intake, and knowledge on multi-drug resistant pathogens—Results of a population-based survey in Lower Saxony, Germany. Front. Microbiol. 2019, 10, 776. [Google Scholar] [CrossRef]
- Voidăzan, S.; Moldovan, G.; Voidăzan, L.; Zazgyva, A.; Moldovan, H. Knowledge, Attitudes And Practices Regarding The Use Of Antibiotics. Study On The General Population Of Mureş County, Romania. Infect. Drug Resist. 2019, 12, 3385–3396. [Google Scholar] [CrossRef]
- Jaja, O. A Survey of Public Knowledge and Attitude Related to Antibiotic Use and Antibiotic Resistance in Southwest Alberta; University of Lethbridge: Lethbridge, AB, Canada, 2017. [Google Scholar]
- Paredes, J.L.; Navarro, R.; Watanabe, T.; Morán, F.; Balmaceda, M.P.; Reateguí, A.; Elias, R.; Bardellini, M.; Ochoa, T.J. Knowledge, attitudes and practices of parents towards antibiotic use in rural communities in Peru: A cross-sectional multicentre study. BMC Public Health 2022, 22, 459. [Google Scholar] [CrossRef]
- National Response Plan for Antimicrobial Resistance. Colombia: Dirección de Medicamentos y Tecnologías en Salud; 2018. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/MET/plan-respuesta-resistencia-antimicrobianos.pdf (accessed on 25 March 2023).
- Higuita-Gutiérrez, L.F.; Roncancio Villamil, G.E.; Jiménez Quiceno, J.N. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: A cross-sectional descriptive study. BMC Public Health 2020, 20, 1861. [Google Scholar] [CrossRef] [PubMed]
- Lotero, A.M.; Ríos, Y. Situation of Pharmacies-Drugstores and Drugstores of the Municipality of Medellín/2021. Bachelor Thesis, Universidad de Antioquia, Medellín, Colombia, 2021. [Google Scholar]
- GERMEN. Surveillance of resistance to antibiotics in hospital institutions and their clinical laboratories in Valle de Aburrá. Colombia: Grupo GERMEN, 2019. Available online: https://www.grupogermen.org/pdf/PERFILES%20GERMEN%2017%20MARZO%202020.pdf (accessed on 25 March 2023).
- Alcaldía de Medellín. Demographic Profile 2016–2020 Total Medellin. Medellín: Alcaldía de Medellín; 2016–2020. Available online: https://www.medellin.gov.co/irj/go/km/docs/pccdesign/SubportaldelCiudadano_2/PlandeDesarrollo_0_17/IndicadoresyEstadsticas/Shared%20Content/Documentos/ProyeccionPoblacion2016-2020/Perfil%20Demogr%C3%A1fico%202016%20-%202020%20Total%20Medellin.pdf (accessed on 22 April 2023).
- Chan, M. Antimicrobial Resistance in the European Union and the world. World Health Organization; 2012. Available online: http://www.who.int/dg/speeches/2012/amr_20120314/en/ (accessed on 22 April 2023).
- Lim, J.M.; Duong, M.C.; Cook, A.R.; Hsu, L.Y.; Tam, C.C. Public knowledge, attitudes and practices related to antibiotic use and resistance in Singapore: A cross-sectional population survey. BMJ Open 2021, 11, e048157. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Antimicrobial Resistance. World Health Organization: 2016. Available online: https://apps.who.int/iris/bitstream/handle/10665/255204/9789243509761-spa.pdf (accessed on 22 April 2023).
- Funk, S.; Gilad, E.; Watkins, C.; Jansen, V.A. The spread of awareness and its impact on epidemic outbreaks. Proc Natl Acad Sci. USA 2009, 106, 6872–6877. [Google Scholar] [CrossRef] [PubMed]
- Langford, B.J.; Morris, A.M. Is it time to stop counseling patients to “finish the course of antibiotics”? Can. Pharm. J. 2017, 150, 349–350. [Google Scholar] [CrossRef] [PubMed]
- Michaelidou, M.; Karageorgos, S.A.; Tsioutis, C. Antibiotic Use and Antibiotic Resistance: Public Awareness Survey in the Republic of Cyprus. Antibiotics 2020, 9, 759. [Google Scholar] [CrossRef]
- DeSalle, R.; Wikins, J.; Kennett, R. A kiosk survey of perception, attitudes and knowledge (PAK) of Australians concerning microbes, antibiotics, probiotics and hygiene. Health Promot. J. Aust. 2022, 33, 838–851. [Google Scholar] [CrossRef]
- Goettsche, L.S.; Weig, E.A.; Chung, J.; Hoff, B.M.; Ince, D.; Wanat, K.A. Patient perceptions of antibiotic use and resistance at a single university dermatology. J. Dermatol. Treat. 2019, 30, 92–95. [Google Scholar] [CrossRef]
- Cuevas, C.; Batura, N.; Wulandari, L.P.L.; Khan, M.; Wiseman, V. Improving antibiotic use through behavior change: A systematic review of interventions evaluated in low- and middle-income countries. Health Policy Plan. 2021, 36, 594–605. [Google Scholar] [CrossRef]
- Lim, J.M.; Chhoun, P.; Tuot, S.; Om, C.; Krang, S.; Ly, S.; Hsu, L.Y.; Yi, S.; Tam, C.C. Public knowledge, attitudes and practices surrounding antibiotic use and resistance in Cambodia. JAC-Antimicrob. Resist. 2021, 3, dlaa115. [Google Scholar] [CrossRef]
- Holmes, A.H.; Moore, L.S.P.; Sundsfjord, A.; Steinbakk, M.; Regmi, S.; Karkey, A.; Guerin, P.J.; Piddock, L.J.V. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet 2016, 387, 176–187. [Google Scholar] [CrossRef]
- Parveen, S.; Garzon-Orjuela, N.; Amin, D.; McHugh, P.; Vellinga, A. Public health interventions to improve Antimicrobial Resistance awareness and behavioral change associated with antimicrobial use: A systematic review exploring the use of social media. Antibiotics 2022, 11, 669. [Google Scholar] [CrossRef]
- Barker, A.K.; Brown, K.; Ahsan, M.; Sengupta, S.; Safdar, N. Social determinants of antibiotic misuse: A qualitative study of community members in Haryana, India. BMC Public Health 2017, 17, 333. [Google Scholar] [CrossRef] [PubMed]
- Chandler, C.I.R. Current accounts of antimicrobial resistance: Stabilization, individualization and antibiotics as infrastructure. Palgrave Commun. 2019, 5, 53. [Google Scholar] [CrossRef] [PubMed]
- Mallah, N.; Rodríguez-Cano, R.; Figueiras, A.; Takkouche, B. Design, reliability and construct validity of a Knowledge, Attitude and Practice questionnaire on personal use of antibiotics in Spain. Sci. Rep. 2020, 10, 20668. [Google Scholar] [CrossRef] [PubMed]
- Johns, R. One Size Doesn’t Fit All: Selecting Response Scales For Attitude Items. J. Elect. Public Opin. Parties 2005, 15, 237–264. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Guillemin, F.; Bombardier, C.; Beaton, D. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J. Clin. Epidemiol. 1993, 46, 1417–1432. [Google Scholar] [CrossRef]
| n | % (CI 95%) | ||
|---|---|---|---|
| Age Group ǂ | Youth | 167 | 18.5 (16.1–21.1) |
| Adult | 515 | 57.1 (53.8–60.3) | |
| Older adult | 220 | 24.4 (21.7–27.3) | |
| Gender | Female | 474 | 52.6 (49.3–55.9) |
| Male | 427 | 47.4 (44.1–50.7) | |
| Economic status | Low | 414 | 47.5 (44.2–50.9) |
| Medium | 432 | 49.6 (46.3–52.9) | |
| High | 25 | 2.9 (1.9–4.1) | |
| Education level | None | 18 | 2.0 (1.2–3.1) |
| Primary school | 199 | 22.1 (19.4–24.9) | |
| High school | 286 | 31.7 (28.7–34.8) | |
| Technical school | 160 | 17.7 (15.4–20.3) | |
| College student | 107 | 11.9 (9.9–14.1) | |
| Professional | 132 | 14.6 (12.4–17.1) | |
| Healthcare career | No | 781 | 87.7 (85.4–89.7) |
| Yes | 110 | 12.3 (10.3–14.6) | |
| Knowledge | Attitudes | Practices | |
|---|---|---|---|
| Me (IQR) | Me (IQR) | Me (IQR) | |
| Age group | |||
| Youth | 73.3 (56.7–86.7) | 83.3 (70.0–93.3) | 61.1 (47.2–72.2) |
| Adult | 76.7 (63.3–86.7) | 83.3 (73.3–93.3) | 61.1 (50.0–75.0) |
| Older adult | 70.0 (60.0–80.0) | 80.0 (70.0–90.0) | 66.7 (52.8–80.6) |
| p-value ʄ | 0.001 * | 0.021 * | 0.006 * |
| Gender | |||
| Female | 76.7 (63.3–86.7) | 86.7 (76.7–93.3) | 63.9 (50.0–77.8) |
| Male | 73.3 (60.0–83.3) | 80.0 (70.0–90.0) | 61.1 (47.2–75.0) |
| p-value ʃ | 0.005 * | 0.001 * | 0.018 * |
| Economic status | |||
| Low | 70.0 (60.0–80.0) | 83.3 (70.0–90.0) | 61.1 (47.2–75.0) |
| Medium | 76.7 (65.0–90.0) | 86.7 (73.3–93.3) | 63.9 (52.8–77.8) |
| High | 80.0 (70.0–90.0) | 86.7 (76.7–93.3) | 61.1 (58.3–69.4) |
| p-value ʄ | 0.001 * | 0.003 * | 0.005 * |
| Education level | |||
| None | 61.7 (56.7–70.0) | 71.7 (63.3–80.0) | 58.3 (47.2–69.4) |
| Primary school | 66.7 (56.7–76.7) | 80.0 (70.0–86.7) | 63.9 (52.8–75.0) |
| High school | 70.0 (60.0–80.0) | 83.3 (70.0–90.0) | 58.3 (47.2–72.2) |
| Technical school | 76.7 (70.0–86.7) | 86.7 (76.7–93.3) | 61.1 (52.8–75.0) |
| College student | 83.3 (66.7–93.3) | 90.0 (76.7–96.7) | 66.7 (52.8–80.6) |
| Professional | 83.3 (76.7–93.3) | 90.0 (76.7–100) | 66.7 (51.4–80.6) |
| p-value ʄ | 0.001 * | 0.001 * | 0.008 * |
| Healthcare career | |||
| No | 70.0 (60.0–83.3) | 83.3 (73.3–90.0) | 61.1 (50.0–75.0) |
| Yes | 86.7 (73.3–96.7) | 90.0 (80.0–96.7) | 69.4 (55.6–80.6) |
| p-value ʃ | 0.001 * | 0.001 * | 0.002 * |
| Index | Variables of the Model | Regression Coefficient | CI 95% | p-Value | Coefficient of Determination |
|---|---|---|---|---|---|
| Knowledge | Healthcare career (Yes/No) | 6.224 | 3.170–9.279 | <0.001 | 17.2% |
| Education level ʃ | 3.257 | 0.993–4.792 | <0.001 | ||
| Gender (Female/Male) | 2.892 | 2.498–4.016 | 0.003 | ||
| Economic status ʃ | 2.645 | 0.837–4.453 | 0.004 | ||
| Attitudes | Knowledge Index | 0.387 | 0.331–0.443 | <0.001 | 23.1% |
| Gender (Female/Male) | 2.807 | 1.199–4.415 | <0.001 | ||
| Education level ʃ | 0.686 | 0.062–1.309 | 0.031 | ||
| Practices | Knowledge Index | 0.084 | 0.005–0.157 | 0.036 | 22.4% |
| Attitudes index | 0.552 | 0.468–0.636 | <0.001 | ||
| Age group ʃ | 2.858 | 1.273–4.443 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sampedro Restrepo, M.; González Gaviria, M.; Arango Bolaños, S.; Higuita-Gutiérrez, L.F. Knowledge, Attitude and Practice Regarding Antibacterial and Their Resistance in Medellín-Colombia: A Cross-Sectional Study. Antibiotics 2023, 12, 1101. https://doi.org/10.3390/antibiotics12071101
Sampedro Restrepo M, González Gaviria M, Arango Bolaños S, Higuita-Gutiérrez LF. Knowledge, Attitude and Practice Regarding Antibacterial and Their Resistance in Medellín-Colombia: A Cross-Sectional Study. Antibiotics. 2023; 12(7):1101. https://doi.org/10.3390/antibiotics12071101
Chicago/Turabian StyleSampedro Restrepo, Marcela, Manuela González Gaviria, Samuel Arango Bolaños, and Luis Felipe Higuita-Gutiérrez. 2023. "Knowledge, Attitude and Practice Regarding Antibacterial and Their Resistance in Medellín-Colombia: A Cross-Sectional Study" Antibiotics 12, no. 7: 1101. https://doi.org/10.3390/antibiotics12071101
APA StyleSampedro Restrepo, M., González Gaviria, M., Arango Bolaños, S., & Higuita-Gutiérrez, L. F. (2023). Knowledge, Attitude and Practice Regarding Antibacterial and Their Resistance in Medellín-Colombia: A Cross-Sectional Study. Antibiotics, 12(7), 1101. https://doi.org/10.3390/antibiotics12071101






