Abstract
This review documents the status of AMR education and awareness in the WHO African region, as well as specific initiatives by its member states in implementing education and awareness interventions, as a strategic objective of the Global Action Plan on AMR, i.e., improve knowledge and understanding on AMR through effective communication, education, and training. A systematic search was conducted in Google Scholar, PubMed, and African Journals Online Library according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines, for articles published in English. Retrieval and screening of articles was performed using a structured search protocol following a pre-set inclusion/exclusion criterion. Eighty-five published articles reporting 92 different studies from 19 Member States met inclusion criteria and were included in the final qualitative synthesis. Nigeria (21) and Ethiopia (16) had most of the studies, while the rest were distributed across the remaining 17 Member States. The majority of the articles were on knowledge, attitude, and practices with regard to AMR and antimicrobial use and most of them documented a general lack and suboptimal knowledge, poor attitude and practices, and widespread self-medication. This review shows low levels of knowledge of AMR coupled with extensive misuse of antimicrobial medicines by different target audiences. These findings underscore the urgent need for enhanced and context-specific educational and positive behavioural change interventions.
1. Introduction
Antimicrobial resistance (AMR) has been acknowledged as one of the top ten public health threats facing humanity [1]. It is a complex and multidimensional problem, threatening not only human and animal health, but also regional, national, and global security, and the economy. O’Neil’s 2014 report projected that AMR will cause 10 million deaths annually by 2050 and will result in between 2% to 3.5% less in gross domestic product (GDP), if not adequately and urgently addressed [2]. The report by the Global Research on Antimicrobial Resistance (GRAM) project estimated that 4.95 million deaths were associated globally with bacterial resistance in 2019 and, of these, 1.27 million deaths were directly attributable to resistance [3]. The consequences of AMR are more calamitous in low to middle-income countries (LMICs) and their development agenda due to the occurrence of more prevalent infectious diseases.
In response to the threat of AMR in the context of the One Health approach, in 2015 the World Health Organization (WHO) endorsed a Global Action Plan (GAP) on AMR that serves as a blueprint for country-specific National Action Plans (NAPs) [4]. One of the objectives highlighted in both the GAP and country NAPs is the need to improve awareness and understanding of antimicrobial resistance through effective communication, education, and training, the umbrella for the other four strategic objectives [4,5]. The GAP calls for among other things, increased national AMR awareness targeting different audiences/demographics in human health, animal health, and agricultural practices, establishing AMR as a core component of awareness campaigns, professional education, training, certification, and development across sectors, as well as the inclusion of antimicrobial use (AMU) and resistance in school curricula to promote better understanding and awareness [4].
Antimicrobial use and misuse across sectors and the spread of resistant pathogens and resistance determinants within and between sectors have been cited as the major drivers of AMR [6,7]. Antimicrobial use is largely influenced by knowledge, expectations, nature of practices, interactions of prescribers and patients, economic incentives, characteristics of the health system, and the regulatory environment [8]. This is largely because there still remains a major gap in implementing education and awareness interventions on judicious use of antimicrobials for the different target audiences in the region [9,10]. Countries have mostly confined their education and awareness activities to global commemorations, particularly, the World AMR Awareness Week (WAAW), which is usually characterized by small-scale AMR campaigns scattered around different sectors. Considering the complexity of AMR and its cross-cutting as well as multisectoral dimensions, episodic interventions are inadequate to impact or trigger sustainable behavioural change. We sought to document the level of awareness and understanding of AMR in the WHO African Region as well as the deployment of effective communication, education, and training.
2. Materials and Methods
2.1. Data Sources and Search Strategy
A systematic search was carried out in Google Scholar, PubMed, and African Journals Online Library according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. Published articles on AMR awareness and understanding documented from original studies conducted in the 47 countries of the WHO African Region were obtained. The search was carried out using relevant keywords which were pooled together using the Boolean term “OR”. The keywords were combined to form a final search strategy using the Boolean term “AND” as shown in Table 1. There was no restriction on the year of publication.

Table 1.
Search Strategy.
2.2. Selection Criteria
The criteria for inclusion of the articles in the qualitative synthesis were: The articles must be original and published in English, they should document findings related to AMR awareness, understanding, education, communication, and training in countries within the WHO African Region, and must be available in full text.
2.3. Article Selection Process
The initial 729,727 records from the databases were screened according to the relevance of the title. Of the 165 remaining articles, 44 duplicates (articles from more than one database) were removed. The retained articles (121) were further screened for inclusion by reading through the abstract and noting the presence of one or more of the keywords. The final screening was based on the inclusion criteria stated above and the articles that did not meet all the criteria were excluded from the final synthesis. Figure 1 shows the stepwise process of selection of the 85 articles for qualitative synthesis.
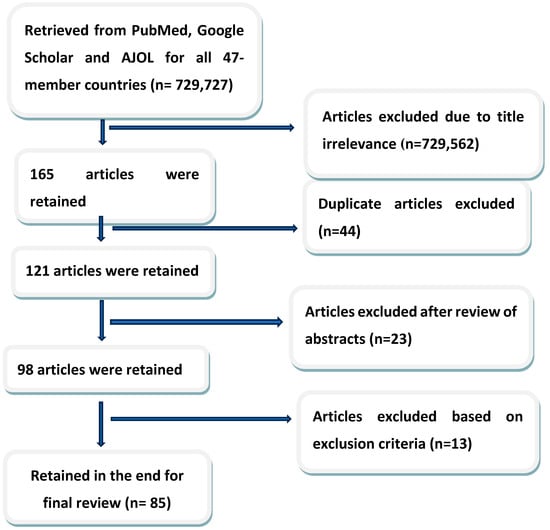
Figure 1.
Diagram of the search and selection of review articles.
2.4. Data Extraction/Qualitative Synthesis
Relevant information synthesized from each article included the country where the study was conducted and the year of publication, the type of research tools and how they were deployed (questionnaires, self-administered or interviewer administered; physical or online/web-based), study settings (urban, semi-urban or rural), study participants (general public, students, healthcare workers, outpatients/hospitalized patients, veterinarians, farmers, etc.), number of study participants, as well as key findings including knowledge, understanding and awareness levels, trainings, and other relevant findings.
3. Results
The 85 articles available for qualitative synthesis reported 92 (80 single-country studies and five multi-country studies) original studies within the WHO African Region (Table 2). The selected studies were from 19 countries including Nigeria (21), Ethiopia (16), Tanzania (8), Zambia (8), Ghana (7), South Africa (7), Uganda (5), and others, as shown in Figure 2.

Table 2.
Summary of findings from qualitative synthesis of articles from studies across the countries in the WHO African Region.
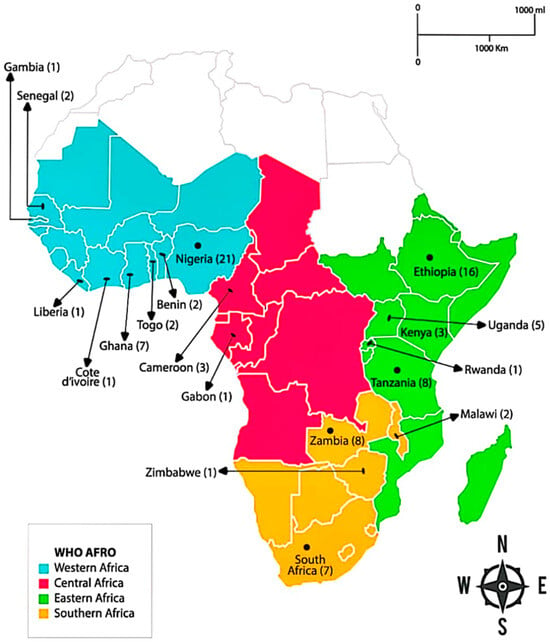
Figure 2.
Map showing distribution of published articles on AMR awareness in WHO AFRO.
The majority of the country surveys were among human healthcare practitioners (32, 34.8%) and undergraduate healthcare students (21, 22.8%). The country surveys also involved general public/community dwellers (11), animal producers/farmers (10), patients (5), veterinary drug retailers and dispensers (4), community drug retailers (2), and veterinarians and veterinary paraprofessionals (2). Three other studies surveyed more than one group of respondents.
Human healthcare professionals (HCPs) generally have good knowledge of AMR as a global and national problem; it is, however, less appreciated as an issue in their local institutions or wards in day-to-day practice. Many HCPs perceived AMR as a problem for individuals who misuse antibiotics. Most HCPs identified drivers of AMR as overuse and misuse, fewer of the professionals identified other factors promoting the emergence and spread of AMR such as lack of antibiograms, lack of antibiotic treatment guidelines, poor hospital hygiene and infection prevention and control measures, and lack of awareness campaigns and education. Only one study conveyed that AMR can be promoted by poor access to antimicrobials. Many studies documented poor training on AMR among human HCPs, some reported low levels of formal training or up-to-date AMR information with the few available knowledge acquired as far back as during medical training. Some studies clearly reported requests by HCPs for more education on AMR; a study among Ethiopian medical interns reported that as high as 94% of respondents wanted more education on AMR. The review further shows that AMR knowledge levels/scores differed significantly across different professionals; it was generally better among physicians and pharmacists when compared to nurses and other HCPs (Table 2). In addition, two separate studies among dispensers in community retail outlets/patent medicine vendors showed overall good knowledge of AMR and its drivers, the knowledge however did not have an impact on their daily practice; the majority of them dispensed antimicrobials without prescription.
Six studies involved veterinary care workers and revealed that awareness and knowledge of AMR were higher among pharmacists than other veterinary drug dispensers. A third of all the dispensers in one of the studies knew that AMR could be caused by misuse. Good knowledge of veterinary pharmacists was associated with work experience of more than one year. A study of veterinary paraprofessionals in five community districts revealed that most did not attend refresher courses and seminars on AMR.
Twenty-six studies engaged university undergraduate students including 21 studies of human health care students (medical students—8; pharmacy students—3; medical laboratory science students—1; combined healthcare students—10), 3 studies of veterinary students, and 2 studies involving students in general. Pharmacy students and medical students had better knowledge of AMR, its drivers, and how AMR could be curtailed when compared with nursing students, medical laboratory science students, and other paramedical students. The knowledge level is generally poor among university students studying non-healthcare-related courses. In fact, one of the surveys involving 1320 participants showed that general university students displayed less knowledge than community dwellers that self-medication promotes AMR. The review also revealed that students at higher levels had better knowledge of AMR than those at lower levels. Most studies revealed a robust knowledge among healthcare students that AMR constitutes a global problem, many studies however revealed poor students’ knowledge that it is a local hospital problem affecting routine practice. Healthcare students in many studies did not also recognise that hand hygiene and IPC measures play important roles in the control of AMR. The review also showed a complete absence or inadequacy of training on AMR in healthcare.
Ten studies across the countries were among animal farmers among who were poultry farmers (5) and pastoralists/livestock farmers (3). Awareness and knowledge of AMR are generally poor and may vary across different country regions, and such awareness could be better among commercial than subsistent poultry farmers. The studies showed that many farmers did not perceive AMR as a public health issue, some perceived it as a problem of foreign countries, and some perceived it as a local problem that only affects individuals who regularly take antibiotics. The studies also showed that large numbers of farmers did not see antimicrobial use in animals as a promoter of AMR while many farmers did not have the knowledge that drug-resistant organisms can be transmitted from animals to humans.
The five studies among hospital patients (three in-patients and two out-patients) showed poor awareness and knowledge of AMR. The studies showed that a large number of patients neither know that inappropriate use of antimicrobials promotes AMR nor know that resistant infections prolong hospitalization and increase healthcare costs. A study, however, showed that the knowledge that AMR could affect mortality was good.
A review of the 11 studies which incorporated community dwellers and the general public showed a low level of awareness and education on AMR and poor knowledge of drivers of AMR. It further showed the possibilities of geographical variation in AMR knowledge. A study revealed that more than 50% of the public did not know that AMR is difficult to treat, and another study showed that more than 40% of the public did not know that AMR is more costly to treat. Less than one-tenth knew that hand washing can prevent transmission of AMR. Furthermore, knowledge of AMR was noted to be better among respondents with higher levels of education.
4. Discussion
Antimicrobial use is mostly influenced by knowledge, perception, prevailing attitudes, and practices on antimicrobials. Education and awareness play a critical role in addressing the use of antimicrobials and ultimately AMR, as it is an overarching objective that cuts across the other four objectives of both the global action plan and member state’s Action Plans for control of AMR. Expeditious and effective implementation of the One Health national plans to mitigate AMR requires an all-encompassing, robust, and society-wide education utilising target-specific, efficient communication strategies aimed at the government and policymakers, healthcare workers, veterinarians, animal farmers and food producers, community drug vendors, and high school, undergraduate, and graduate students, as well as the general public.
Despite a majority of countries (74%, 23/31) in the region holding regular public awareness campaigns against AMR and its drivers [95], our review of the literature highlighted poor levels of awareness and knowledge on AMR across societal strata. One of the key weapons against AMR is public awareness/engagement which, if conducted taking into account context-specific determinants and elements of behaviour change, has the potential of engendering behavioural change among the public bearing in mind that AMR is a society-wide issue demanding specified roles to be played by everyone [96]. The fact that the public is generally unaware of AMR and its dare consequences calls for aggressive orientation and community engagements among member countries with the full participation of the governments’ relevant sectors, civil society, non-governmental organisation, and the media for concerted and coordinated activities towards communicating AMR and its deleterious consequences to the populace in an effective manner for enhanced understanding. A previous report suggests that such community engagement, deploying context-driven community approaches as well as tools including appropriately packaged and positioned messaging, can go a long way to facilitate expected behavioural change in LMICs [97].
This review noted an inappreciable knowledge of AMR even among human HCWs; findings in a multi-country survey across Ghana, Nigeria, and Tanzania are particularly noteworthy showing that respondents with good awareness of AMR was not up to 60% in the majority of the countries and awareness scores differed significantly among the different professionals within each country [36]. This review also noted in two separate Nigerian studies that more than 40% of human HCWs even in urban centres do not have knowledge of AMR [63,66]. Our review findings therefore corroborate what was previously noted in a scoping review which documented global knowledge gaps on AMR in human health including in AMR burden and drivers as well as awareness and education, and with the African region leading the gap chart [98]. Even in studies where AMR knowledge levels were reported to be high among human healthcare professionals, high proportions neither know the extent of AMR nor its effect that AMR could lead to treatment failure [11,12]. In addition, some HCWs neither saw AMR as a problem in their local HCF nor appreciated its impact on their daily routine practice, with such knowledge dearth even documented among physicians in tertiary HCFs [15,37,43], with attendant serious consequences on healthcare cost and patient outcomes. Good knowledge of practices leading to overuse and misuse of antimicrobials driving AMR is noted among most HCWs; however, there are still widespread knowledge deficits on other key drivers such as lack of antibiogram as well as poor hand hygiene and IPC measures, two studies carried out in Ethiopia and Zambia [17,90] and another three conducted in Benin, Cameroun, and Uganda [12.15,83], respectively, documented knowledge gaps in the important roles of antibiogram and IPC measures in AMR. The review further showed in several studies the higher knowledge level of AMR among physicians and pharmacists compared with levels in other HCWs including nurses. It was also found in several studies that human HCWs had poor training on AMR; the majority had no current knowledge and a few claimed that the last training they had dated back to their student years. Our findings in this regard equally relate with those of a systematic governance analysis which reviewed the contents of NAPs on AMR from 114 countries and revealed that the scoring for education was about the lowest of the 18 domains [99], highlighting that basic and continuous education on AMR for health-care workers need to be robustly established in most countries. There is an important need among the member countries in the region for deliberate efforts and activities to institutionalise AMR education as part of workforce education in relevant sectors taking the form of pre-service training, or in-service training which demands champions and resources. In the human health sector, for example, countries can leverage the curricula guide provided by the World Health Organisation (WHO) for health workers’ education and training to develop a template for continuous professional development [100]. In addition, AMR learning should also be incorporated into high school and university curricula-based education.
Furthermore, the findings justify the use of unconventional approaches to systematizing education thereby promoting and ensuring sustainable behaviour change for addressing AMR threats. Countries within the region can leverage several educational initiatives targeted at different groups of people to improve awareness and education on AMR, for example, e-Bug Europe and MicroMundo for pre-university students, the “Do Bugs Need Drugs” program which is an initiative of Alberta Health Services and the British Columbia Centre for Disease Control, WHO-AFRO regional debate initiative which took place in Senegal during the 2022 continental World AMR Awareness Week celebration, the debate kit launched by of the Spanish National Plan for AMR, and the ReAct Campaign which educate on the nature as well as drivers of AMR. There are other smaller initiatives such as the “Bugs in Bangkok” board game, and the WHO-supported Dr. Ameyo Stella Adadevoh (DRASA) Health Trust model which provided a club way to teach secondary school students about AMR in Nigeria [101,102]. Likewise, the potential usefulness of social media for AMR awareness and education has not been appreciably explored in the region; in fact, the utility of social media for combating AMR has been regarded as a neglected approach especially in low- and middle-income countries [103]. It is therefore instructive that countries adapt and where possible deploy social media platforms for education and information dissemination, particularly among the youths in whom its use is highly rising and has a high tendency to bring about change in attitudes, practices, and perceptions and, ultimately, behaviour [104].
Farmers across the region showed abysmal levels of knowledge of AMR, many of them neither correlated the use of antimicrobials on their animals to AMR nor fathomed a possibility that resistant bugs could be transmitted from animals to humans. For example, a study from Ethiopia involving 571 rural farmers documented that only 41% knew that excessive use of antimicrobials in their animals can cause AMR. In the same vein, a Cameroon study of 358 farmers, among several others, reported a deficit in the knowledge that AMR could be transmitted from their animals to humans or the environment [13,27]. These findings have been well corroborated in a systematic review among poultry farmers which revealed that only 43% had knowledge about AMR and only about 50% understood the impacts of AMR on poultry, human health, and the environment [105]. The fact that knowledge of AMR is worse in LMICs had been earlier reported in a review of 103 multiregional study articles which showed that farmers in Africa and Asia demonstrated grossly deficient knowledge of AMR as compared with their counterparts from Europe [106]. The responsibility therefore rests on member countries to be committed to providing flexible methods to educate and inform community farmers about AMR which can be facilitated by existing platforms such as appropriate broadcast media for wide reach. Successes recorded by some countries can be replicated and upscaled by many other countries, a typical example is the poultry farmer field schools by FAO in Ghana and Kenya which facilitated a knowledge-driven reduction in antibiotic use in birds, improvement in IPC practices and enhancement of patronage with animal health professionals [107]. Furthermore, fortifying AMR education among veterinary and para-veterinary workers is a step in the right direction for the stepdown of robust knowledge to farmers. Being animal health practitioners and health extension workers, their education provides a direct impact on farmers’ knowledge of animal husbandry and drug resistance. Such education can be well guided at the level of the undergraduate and can utilise various platforms and tools including online-based resources deployed for enhanced education on antimicrobial resistance and antimicrobial use [108]. The region will do good by leveraging on previously used initiatives to strengthen veterinary training to incorporate AMR education [109].
5. Conclusions
To the best of our knowledge, this review is the first to document the status of AMR education and awareness in the WHO African Region. This review opens up the knowledge gaps in AMR across the board and sheds light on the need to design evidence-based, pragmatic, cost-effective, targeted interventions to improve public awareness and knowledge of AMR. The review reveals a need for improved educational strategies within member countries focusing on the inclusive academic curriculum at all levels of studies, continuous professional development, as well as utilising innovative and context-specific approaches for effective and sustained awareness and education on AMR.
6. Limitation
Articles included in this systematic review were restricted only to those published in English.
Author Contributions
Conceptualisation, W.F. and O.K.; Literature Review, W.F., O.K. and A.O.A.; Writing—Original Draft Preparation, W.F. and O.K.; Writing—Review and Editing, W.F., O.K., A.O.A., A.T.A., O.I.O., Y.A.A. and L.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The information presented in this review is available in open access journals, as indicated in Table 1 and under references.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ten Health Issues WHO Will Tackle This Year. Available online: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 (accessed on 1 October 2019).
- Review on Antimicrobial Resistance. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. 2014. Available online: http://amrrevieworg/sites/default/files/160525_Final%20paper_with%20coverpdf (accessed on 1 October 2019).
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Action Plan on Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Lee, C.R.; Lee, J.H.; Kang, L.W.; Jeong, B.C.; Lee, S.H. Educational effectiveness, target, and content for prudent antibiotic use. Biomed. Res. Int. 2015, 214021. [Google Scholar] [CrossRef] [PubMed]
- McEwen, S.A.; Collignon, P.J. Antimicrobial Resistance: A One Health Perspective. Microbiol. Spectr. 2018, 6, 521–547. [Google Scholar] [CrossRef]
- Lambrou, A.S.; Innes, G.K.; O’Sullivan, L.; Luitel, H.; Bhattarai, R.K.; Basnet, H.B.; Heaney, C.D. Policy implications for awareness gaps in antimicrobial resistance (AMR) and antimicrobial use among commercial Nepalese poultry producers. Glob. Health Res. Policy 2021, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde (BR). Systems for Improved Access to Pharmaceuticals and Services; Pesquisa de avaliação dos usuários do SITETB.; Ministério da Saúde (BR): São Paulo, Brasil, 2016. [Google Scholar]
- Mudenda, S.; Malama, S.; Munyeme, M.; Hang’ombe, B.M.; Mainda, G.; Kapona, O.; Mukosha, M.; Yamba, K.; Bumbangi, F.N.; Mfune, R.L.; et al. Awareness of Antimicrobial Resistance and Associated Factors among Layer Poultry Farmers in Zambia: Implications for Surveillance and Antimicrobial Stewardship Programs. Antibiotics 2022, 11, 383. [Google Scholar] [CrossRef]
- Ndukui, J.G.; Gikunju, J.K.; Aboge, G.O.; Mbaria, J.M. Antimicrobial Use in Commercial Poultry Production Systems in Kiambu County, Kenya: A Cross-Sectional Survey on Knowledge, Attitudes and Practices. Open J. Anim. Sci. 2021, 11, 658–681. [Google Scholar] [CrossRef]
- Dougnon, V.; Chabi, Y.; Koudokpon, H.; Agbankpe, J.; Sefounon, R.; Alle, D.; Bankole, H.; Baba-Moussa, L. Prescription of antibiotics as a source of emerging antibiotic resistance: Knowledge, attitudes, and practices of medical staff in the Dassa-Glazoué and Savalou-Bantè’s health zones (Benin, West Africa). Int. J. One Health 2020, 6, 34–40. [Google Scholar] [CrossRef]
- Allabi, A.C.; Agbo, A.G.; Boya, B.; Mudenda, S. Antimicrobial Stewardship: Knowledge and Attitudes of Pharmacy Staff on Antibiotic Dispensing Patterns, Use and Resistance in Benin. Pharmacol. Pharm. 2023, 14, 189–214. [Google Scholar] [CrossRef]
- Moffo, F.; Mouiche, M.M.; Kochivi, F.L.; Dongmo, J.B.; Djomgang, H.K.; Tombe, P.; Mbah, C.K.; Mapiefou, N.P.; Mingoas, J.K.; Awah-Ndukum, J. Knowledge, attitudes, practices and risk perception of rural poultry farmers in Cameroon to antimicrobial use and resistance. Prev. Vet. Med. 2020, 182, 105087. [Google Scholar] [CrossRef]
- Djuikoue, C.I.; Nana, C.D.; Pamela, N.N.; Ekeu, D.N.; Wanda, G.; Guegang, C.G.; Farid, W.; Longo-Mbenza, B.; Venant, T.; Adiogo, D.; et al. Prescribers’, Dispensers’ and Users’ Knowledge, Attitudes and Practices Relative to Antimicrobial Resistance in Douala, Cameroon. World J. Public Health 2022, 7, 111–118. [Google Scholar]
- Domche Ngongang, S.C.; Basera, W.; Mendelson, M. Tertiary hospitals physician’s knowledge and perceptions towards antibiotic use and antibiotic resistance in Cameroon. BMC Infect. Dis. 2021, 21, 1116. [Google Scholar] [CrossRef] [PubMed]
- Bedekelabou, A.P.; Oyetola, D.W.; Coulibaly, Z.L.; Akinsola, O.; Bada-Alambedji, R. First assessment of the knowledge, attitudes, and practices of health actors in Togo and Ivory Coast in regard to antibiotic resistance. Int. J. One Health 2022, 8, 108–123. [Google Scholar] [CrossRef]
- Abera, B.; Kibret, M.; Mulu, W. Knowledge and beliefs on antimicrobial resistance among physicians and nurses in hospitals in Amhara Region, Ethiopia. BMC Pharmacol. Toxicol. 2014, 15, 26. [Google Scholar] [CrossRef]
- Zeru, H.; Gemechu, A.; Andualem, T.; Seid, H.; Mengesha, F. Awareness of veterinary drug retail outlets on antimicrobial resistance and its containment strategy in Ethiopia. Pharmacovigil Pharmacoepi 2019, 2, 17–21. [Google Scholar] [CrossRef]
- Mersha, A.G. Attitude and perception of medical interns about antimicrobial resistance: A multi center cross-sectional study in Ethiopia. Antimicrob. Resist. Infect. Control 2018, 4, 149. [Google Scholar] [CrossRef] [PubMed]
- Geta, K.; Kibret, M. Knowledge, attitudes and practices of animal farm owners/workers on antibiotic use and resistance in Amhara region, north western Ethiopia. Sci. Rep. 2021, 11, 21211. [Google Scholar] [CrossRef]
- Mengesha, Y.; Manaye, B.; Moges, G. Assessment of Public Awareness, Attitude, and Practice Regarding Antibiotic Resistance in Kemissie Town, Northeast Ethiopia: Community-Based Cross-Sectional Study. Infect. Drug Resist. 2020, 13, 3783–3789. [Google Scholar] [CrossRef]
- Simegn, W.; Moges, G. Awareness and knowledge of antimicrobial resistance and factors associated with knowledge among adults in Dessie City, Northeast Ethiopia: Community-based cross-sectional study. PLoS ONE 2022, 17, e0279342. [Google Scholar] [CrossRef]
- Simegn, W.; Dagnew, B.; Weldegerima, B.; Dagne, H. Knowledge of Antimicrobial Resistance and Associated Factors Among Health Professionals at the University of Gondar Specialized Hospital: Institution-Based Cross-Sectional Study. Front. Public Health 2022, 10, 790892. [Google Scholar] [CrossRef]
- Fetensa, G.; Wakuma, B.; Tolossa, T.; Fekadu, G.; Bekuma, T.T.; Fayisa, L.; Etafa, W.; Bekela, T.; Besho, M.; Hiko, N.; et al. Knowledge and Attitude Towards Antimicrobial Resistance of Graduating Health Science Students of Wollega University. Infect. Drug Resist. 2020, 3, 3937–3944. [Google Scholar] [CrossRef]
- Gebrehiwot, Z.; Tadiwos, Y. Knowledge and Beliefs of Health Care Professionals Towards Antimicrobial Resistance in Hiwot Fana Specialized University Hospital, in Harar, Ethiopia. Infect. Drug Resist. 2020, 13, 2027–2035. [Google Scholar] [CrossRef]
- Geta, K.; Kibret, M. Knowledge, Attitudes and Practices of Patients on Antibiotic Resistance and Use in Public Hospitals of Amhara Regional State, Northwestern Ethiopia: A Cross-Sectional Study. Infect. Drug Resist. 2022, 15, 193–209. [Google Scholar] [CrossRef] [PubMed]
- Gebeyehu, D.T.; Bekele, D.; Mulate, B.; Gugsa, G.; Tintagu, T. Knowledge, attitude and practice of animal producers towards antimicrobial use and antimicrobial resistance in Oromia zone, north eastern Ethiopia. PLoS ONE 2021, 16, e0251596. [Google Scholar] [CrossRef]
- Zelellw, D.A.; Bizuayehu, H.M. Knowledge and Attitude of Students on Antimicrobial Resistance at Debre Markos University, Ethiopia. Int. J. Public Health Sci. 2016, 5, 384–391. [Google Scholar]
- Seid, M.A.; Hussen, M.S. Knowledge and attitude towards antimicrobial resistance among final year undergraduate paramedical students at University of Gondar, Ethiopia. BMC Infect. Dis. 2018, 18, 312. [Google Scholar] [CrossRef] [PubMed]
- Tafa, B.; Endale, A.; Bekele, D. Paramedical staff knowledge and attitudes towards antimicrobial resistance in Dire Dawa, Ethiopia: A cross sectional study. Ann. Clin. Microbiol. Antimicrob. 2017, 16, 64. [Google Scholar] [CrossRef]
- Belachew, S.A.; Hall, L.; Selvey, L.A. Community drug retail outlet staff’s knowledge, attitudes and practices towards non-prescription antibiotics use and antibiotic resistance in the Amhara region, Ethiopia with a focus on non-urban towns. Antimicrob. Resist. Infect. Control 2022, 11, 64. [Google Scholar] [CrossRef]
- Dejene, H.; Birhanu, R.; Tarekegn, Z.S. Knowledge, attitude and practices of residents toward antimicrobial usage and resistance in Gondar, Northwest Ethiopia. One Health Outlook 2022, 4, 10. [Google Scholar] [CrossRef]
- Adegbite, B.R.; Edoa, J.R.; Schaumburg, F.; Alabi, A.S.; Adegnika, A.A.; Grobusch, M.P. Knowledge and perception on antimicrobial resistance and antibiotics prescribing attitude among physicians and nurses in Lambaréné region, Gabon: A call for setting-up an antimicrobial stewardship program. Antimicrob. Resist. Infect. Control 2022, 11, 44. [Google Scholar] [CrossRef]
- Sanneh, B.; Jallow, H.S.; Singhateh, Y.; Sabally, B.; Sey, A.P.; Jallow, A.W.; Jallow, T.; Baldeh, I.; Sambou, S.M.; Jah, S.L. Knowledge, attitude and practice of health care workers on antibiotic resistance and usage in the Gambia. GSC Biol. Pharm. Sci. 2020, 13, 007–015. [Google Scholar] [CrossRef]
- Asante, K.P.; Boamah, E.A.; Abdulai, M.A.; Buabeng, K.O.; Mahama, E.; Dzabeng, F.; Gavor, E.; Annan, E.A.; Owusu-Agyei, S.; Gyansa-Lutterodt, M. Ghana Antimicrobial Resistance Working Group. Knowledge of antibiotic resistance and antibiotic prescription practices among prescribers in the Brong Ahafo Region of Ghana; a cross-sectional study. BMC Health Serv. Res. 2017, 17, 422. [Google Scholar] [CrossRef]
- Pinto Jimenez, C.; Pearson, M.; Hennessey, M.; Nkereuwem, E.; Crocker, C.; Egbujo, U.; Hendriks, J.; Smith, S.; Whanpuch, P.; Manongi, R.; et al. Awareness of antibiotic resistance: A tool for measurement among human and animal health care professionals in LMICs and UMICs. J. Antimicrob. Chemother. 2023, 78, 620–635. [Google Scholar] [CrossRef] [PubMed]
- Labi, A.K.; Obeng-Nkrumah, N.; Bjerrum, S.; Aryee, N.A.A.; Ofori-Adjei, Y.A.; Yawson, A.E.; Newman, M.J. Physicians’ knowledge, attitudes, and perceptions concerning antibiotic resistance: A survey in a Ghanaian tertiary care hospital. BMC Health Serv. Res. 2018, 18, 126. [Google Scholar] [CrossRef] [PubMed]
- Effah, C.Y.; Amoah, A.N.; Liu, H.; Agboyibor, C.; Miao, L.; Wang, J.; Wu, Y. A population-base survey on knowledge, attitude and awareness of the general public on antibiotic use and resistance. Antimicrob. Resist. Infect. Control 2020, 9, 105. [Google Scholar] [CrossRef]
- Anachinaba, I.A.; Adzitey, F.; Teye, G.A.; Brown, C.A.; Boateng, E.F. Knowledge and perception of consumers on microbiological meat safety, antibiotic resistance and residues in Tema metropolis, Ghana. J. Agric. Food Sci. 2022, 20, 135–153. [Google Scholar] [CrossRef]
- Sefah, I.A.; Akwaboah, E.; Sarkodie, E.; Godman, B.; Meyer, J.C. Evaluation of Healthcare Students’ Knowledge on Antibiotic Use, Antimicrobial Resistance and Antimicrobial Stewardship Programs and Associated Factors in a Tertiary University in Ghana: Findings and Implications. Antibiotics 2022, 11, 1679. [Google Scholar] [CrossRef]
- Otieku, E.; Fenny, A.P.; Labi, A.K.; Owusu-Ofori, A.K.; Kurtzhals, J.; Enemark, U. Knowledge, attitudes and practices regarding antimicrobial use and resistance among healthcare seekers in two tertiary hospitals in Ghana: A quasi-experimental study. BMJ Open 2023, 13, e065233. [Google Scholar] [CrossRef]
- Kamita, M.; Mutungi, J.K.; Mungai, S.; Mureithi, D.; Kijogi, C.; Kimani, R.; Ndegwa, D.; Maina, J.; Gitaka, J. A survey on knowledge, attitude, and practice about antibiotic prescribing and resistance among medical practitioners in Kenya. Research 2022, 5, 3. [Google Scholar] [CrossRef]
- Genga, E.; Achieng, L.; Njiri, F.; Ezzi, M. Knowledge, attitudes, and practice survey about antimicrobial resistance and prescribing among physicians in a hospital setting in Nairobi, Kenya. Afr. J. Resp. Med. 2017, 12, 3–7. [Google Scholar]
- Lubwama, M.; Onyuka, J.; Ayazika, K.T.; Ssetaba, L.J.; Siboko, J.; Daniel, O.; Mushi, M.F. Knowledge, attitudes, and perceptions about antibiotic use and antimicrobial resistance among final year undergraduate medical and pharmacy students at three universities in East Africa. PLoS ONE 2021, 16, e0251301. [Google Scholar] [CrossRef]
- Paye, P.D.; McClain, J. Knowledge, Attitude and Practice of antibiotics Resistance survey among healthcare professionals in selected health centers in Greater Monrovia, Liberia. Int. J. Sci. Res. Chem. 2022, 7, 1–13. [Google Scholar]
- Kainga, H.; Phonera, M.C.; Chikowe, I.; Chatanga, E.; Nyirongo, H.; Luwe, M.; Mponela, J.; Kachisi, V.; Kamanga, N.; Chulu, J.; et al. Determinants of Knowledge, Attitude, and Practices of Veterinary Drug Dispensers toward Antimicrobial Use and Resistance in Main Cities of Malawi: A Concern on Antibiotic Stewardship. Antibiotics 2023, 12, 149. [Google Scholar] [CrossRef] [PubMed]
- Kamoto, A.; Chapotera, G.; Suleman, F. Knowledge, attitude and perception on antimicrobial use and antimicrobial resistance among final year medical students in the College of Medicine, Malawi. Malawi Med. J. 2020, 32, 120–123. [Google Scholar] [CrossRef] [PubMed]
- Idoko, L.O.; Okafor, K.C.; Lolo, N.S. Assessment of Knowledge and Prevalence of antimicrobial use (AMU) among patients in a District Hospital in Abuja, Federal Capital Territory, Nigeria. Eur. J. Appl. Sci. 2023, 11, 182–202. [Google Scholar] [CrossRef]
- Okedo-Alex, I.; Madubueze, U.C.; Umeokonkwo, C.D.; Oka, O.U.; Adeke, A.S.; Okeke, K.C. Knowledge of antibiotic use and resistance among students of a medical school in Nigeria. Malawi Med. J. 2019, 31, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Awosan, K.J.; Ibitoye, P.K.; Abubakar, A.K. Knowledge, risk perception and practices related to antibiotic resistance among patent medicine vendors in Sokoto metropolis, Nigeria. Niger. J. Clin. Pract. 2018, 21, 1476–1483. [Google Scholar] [CrossRef]
- Bello, S.I.; Aliyu, F.O.; Yusuf, H.; Aliyu, B.J. Evaluation of knowledge, attitudes and practices of human healthcare students about antimicrobial drug use and resistance: A cross-sectional study in University of Maiduguri, Nigeria. J. Pharm. Bioresour. 2021, 18, 182–191. [Google Scholar] [CrossRef]
- Oyebanji, B.O.; Oyebisi, M.O. Use of Antibiotics and Knowledge of Antibiotics Resistance by Selected Farmers in Oyo Town, Nigeria. Uganda J. Agric. Sci. 2018, 8, 43–56. [Google Scholar] [CrossRef]
- Salihu Dadari, H.I. Antibiotics use, knowledge and practices on antibiotic resistance among breastfeeding mothers in Kaduna state (Nigeria). J. Infect. Public Health 2020, 13, 2072–2079. [Google Scholar] [CrossRef]
- Odetokun, I.A.; Akpabio, U.; Alhaji, N.B.; Biobaku, K.T.; Oloso, N.O.; Ghali-Mohammed, I.; Biobaku, A.J.; Adetunji, V.O.; Fasina, F.O. Knowledge of Antimicrobial Resistance among Veterinary Students and Their Personal Antibiotic Use Practices: A National Cross-Sectional Survey. Antibiotics 2019, 8, 243. [Google Scholar] [CrossRef]
- Oloso, N.O.; Odetokun, I.A.; Ghali-Mohammed, I.; Fasina, F.O.; Olatoye, I.O.; Adetunji, V.O. Knowledge, Attitudes, and Risk Perception of Broiler Grow-Out Farmers on Antimicrobial Use and Resistance in Oyo State, Nigeria. Antibiotics 2022, 11, 567. [Google Scholar] [CrossRef]
- Huang, S.; Eze, U.A. Awareness and Knowledge of Antimicrobial Resistance, Antimicrobial Stewardship and Barriers to Implementing Antimicrobial Susceptibility Testing among Medical Laboratory Scientists in Nigeria: A Cross-Sectional Study. Antibiotics 2023, 12, 815. [Google Scholar] [CrossRef] [PubMed]
- Babatola, A.O.; Fadare, J.O.; Olatunya, O.S.; Obiako, R.; Enwere, O.; Kalungia, A.; Ojo, T.O.; Sunmon, T.A.; Desalu, O.; Godman, B. Addressing antimicrobial resistance in Nigerian hospitals: Exploring physicians prescribing behavior, knowledge, and perception of antimicrobial resistance and stewardship programs. Expert. Rev. Anti. Infect. Ther. 2021, 19, 537–546. [Google Scholar] [CrossRef]
- Anyanwu, M.U.; Okorie-Kanu, O.J.; Anyaoha, C.O.; Kolade, O.A. Veterinary Medical Students’ Perceptions, Attitude and Knowledge about Antibiotic Resistance and Stewardship: How Prepared Are Our Future Prescribers? Not. Sci. Biol. 2018, 10, 156–174. [Google Scholar] [CrossRef]
- Ajibola, O.; Omisakin, O.A.; Eze, A.A.; Omoleke, S.A. Self-Medication with Antibiotics, Attitude and Knowledge of Antibiotic Resistance among Community Residents and Undergraduate Students in Northwest Nigeria. Diseases 2018, 6, 32. [Google Scholar] [CrossRef]
- Abdu-Aguye, S.N.; Barde, K.G.; Yusuf, H.; Lawal, B.K.; Shehu, A.; Mohammed, E. Investigating Knowledge of Antibiotics, Antimicrobial Resistance and Antimicrobial Stewardship Concepts Among Final Year Undergraduate Pharmacy Students in Northern Nigeria. Integr. Pharm. Res. Pract. 2022, 11, 187–195. [Google Scholar] [CrossRef]
- Ahmad, J.L.; Aminu, B.; Arkillamagaji, B. Knowledge, belief and practice of interventions to contain antimicrobial resistance among physicians in Sokoto, North-West Nigeria. Orient J. Med. 2015, 27, 71–78. [Google Scholar]
- Augie, B.M.; van Zyl, R.L.; McInerney, P.A.; Miot, J. Knowledge and perceptions about antibiotic resistance and prudent antibiotic prescribing among final year medical students in two African countries. Int. J. Pharm. Pract. 2021, 29, 508–514. [Google Scholar] [CrossRef]
- Chukwu, E.E.; Oladele, D.A.; Enwuru, C.A.; Gogwan, P.L.; Abuh, D.; Audu, R.A.; Ogunsola, F.T. Antimicrobial resistance awareness and antibiotic prescribing behavior among healthcare workers in Nigeria: A national survey. BMC Infect. Dis. 2021, 21, 22. [Google Scholar] [CrossRef] [PubMed]
- Akande-Sholabi, W.; Ajamu, A.T. Antimicrobial stewardship: Assessment of knowledge, awareness of antimicrobial resistance and appropriate antibiotic use among healthcare students in a Nigerian University. BMC Med. Educ. 2021, 21, 488. [Google Scholar] [CrossRef]
- Chukwu, E.E.; Oladele, D.A.; Awoderu, O.B.; Afocha, E.E.; Lawal, R.G.; Abdus-Salam, I.; Ogunsola, F.T.; Audu, R.A. A national survey of public awareness of antimicrobial resistance in Nigeria. Antimicrob. Resist. Infect. Control 2020, 9, 72. [Google Scholar] [CrossRef] [PubMed]
- Nwafia, I.; Ohanu, M.; Ebede, S.; Okoil, C.; Nwachukwu, P.; Umenzekwe, C.; Ndubueze, C.; Aroh, A.; Oraebueze, I.; Ezomike, C.; et al. Antibiotic use and resistance: Assessment of healthcare workers’ knowledge, attitude, and practice. Int. J. Med. Health Dev. 2022, 27, 31–37. [Google Scholar]
- Nisabwe, L.; Brice, H.; Umuhire, M.C.; Gwira, O.; Harelimana, J.D.; Nzeyimana, Z.; Sebatunzi, O.R.; Rusingiza, E.K.; Hahirwa, I.; Muvunyi, C.M. Knowledge and attitudes towards antibiotic use and resistance among undergraduate healthcare students at University of Rwanda. J. Pharm. Policy Pract. 2020, 13, 7. [Google Scholar] [CrossRef]
- Bassoum, O.; Sougou, N.M.; Ndiaye, O.D.; Camara, M.; Fall, D. Knowledge and practice of graduating students of pharmacy at the Cheikh Anta Diop University relating to antibiotic use and bacterial resistance in 2019 (Senegal). Pan. Afr. Med. J. 2023, 44, 127. [Google Scholar] [CrossRef] [PubMed]
- Bassoum, O.; Sougou, N.M.; Diongue, M.; Lèye, M.M.; Mbodji, M.; Fall, D.; Seck, I.; Faye, A.; Tal-Dia, A. Assessment of General Public’s Knowledge and Opinions towards Antibiotic Use and Bacterial Resistance: A Cross-Sectional Study in an Urban Setting, Rufisque, Senegal. Pharmacy 2018, 6, 103. [Google Scholar] [CrossRef]
- Balliram, R.; Sibanda, W.; Essack, S.Y. The knowledge, attitudes and practices of doctors, pharmacists and nurses on antimicrobials, antimicrobial resistance and antimicrobial stewardship in South Africa. S. Afr. J. Infect. Dis. 2021, 36, 262. [Google Scholar] [CrossRef]
- WHO. WHO Multi-Country Survey Reveals Widespread Public Misunderstanding about Antibiotic Resistance: Geneva, 2015. Available online: https://www.who.int/news/item/16-11-2015-who-multi-country-survey-reveals-widespread-public-misunderstanding-about-antibiotic-resistance (accessed on 1 October 2019).
- Farley, E.; Stewart, A.; Davies, M.A.; Govind, M.; Van den Bergh, D.; Boyles, T.H. Antibiotic use and resistance: Knowledge, attitudes and perceptions among primary care prescribers in South Africa. S. Afr. Med. J. 2018, 108, 763–771. [Google Scholar] [CrossRef]
- Wasserman, S.; Potgieter, S.; Shoul, E.; Constant, D.; Stewart, A.; Mendelson, M.; Boyles, T.H. South African medical students’ perceptions and knowledge about antibiotic resistance and appropriate prescribing: Are we providing adequate training to future prescribers? S. Afr. Med. J. 2017, 107, 405–410. [Google Scholar] [CrossRef]
- Farley, E.; van den Bergh, D.; Coetzee, R.; Stewart, A.; Boyles, T. Knowledge, attitudes and perceptions of antibiotic use and resistance among patients in South Africa: A cross-sectional study. S. Afr. J. Infect. Dis. 2019, 34, 118. [Google Scholar] [CrossRef]
- Smith, P.W.; Agbaje, M.; LeRoux-Pullen, L.; Van Dyk, D.; Debusho, L.K.; Shittu, A.; Sirdar, M.M.; Fasanmi, O.G.; Adebowale, O.; Fasina, F.O. Implication of the knowledge and perceptions of veterinary students of antimicrobial resistance for future prescription of antimicrobials in animal health, South Africa. J. S. Afr. Vet. Assoc. 2019, 90, e1–e8. [Google Scholar] [CrossRef]
- Emgård, M.; Mwangi, R.; Mayo, C.; Mshana, E.; Nkini, G.; Andersson, R.; Msuya, S.E.; Lepp, M.; Muro, F.; Skovbjerg, S. Tanzanian primary healthcare workers’ experiences of antibiotic prescription and understanding of antibiotic resistance in common childhood infections: A qualitative phenomenographic study. Antimicrob. Resist. Infect. Control 2021, 10, 94. [Google Scholar] [CrossRef]
- Mangesho, P.E.; Caudell, M.A.; Mwakapeje, E.R.; Ole-Neselle, M.; Kimani, T.; Dorado-García, A.; Kabali, E.; Fasina, F.O. Knowing Is Not Enough: A Mixed-Methods Study of Antimicrobial Resistance Knowledge, Attitudes, and Practises Among Maasai Pastoralists. Front. Vet. Sci. 2021, 8, 645851. [Google Scholar] [CrossRef] [PubMed]
- Simba, D.; Kakoko, D.; Semali, I.; Kessy, A.; Embrey, M. Household Knowledge of Antimicrobials and Antimicrobial Resistance in the Wake of an Accredited Drug Dispensing Outlet (ADDO) Program Rollout in Tanzania. PLoS ONE 2016, 11, e0163246. [Google Scholar] [CrossRef] [PubMed]
- Katakweba, A.A.S.; Mtambo, M.M.A.; Olsen, J.E.; Muhairwa, A.P. Awareness of human health risks associated with the use of antibiotics among livestock keepers and factors that contribute to selection of antibiotic resistance bacteria within livestock in Tanzania. Livest. Res. Rural Dev. 2012, 24, 170. [Google Scholar]
- Frumence, G.; Mboera, L.E.G.; Sindato, C.; Durrance-Bagale, A.; Jung, A.-S.; Mshana, S.E.; Clark, T.G.; Legido-Quigley, H.; Matee, M.I. Practices and Challenges of Veterinary Paraprofessionals in Regards to Antimicrobial Use and Resistance in Animals in Dar Es Salaam, Tanzania. Antibiotics 2021, 10, 733. [Google Scholar] [CrossRef]
- Sindato, C.; Mboera, L.E.G.; Katale, B.Z.; Frumence, G.; Kimera, S.; Clark, T.G.; Legido-Quigley, H.; Mshana, S.E.; Rweyemamu, M.M.; Matee, M. Knowledge, attitudes and practices regarding antimicrobial use and resistance among communities of Ilala, Kilosa and Kibaha districts of Tanzania. Antimicrob. Resist. Infect. Control 2020, 9, 194. [Google Scholar] [CrossRef]
- Bedekelabou, A.P.; Talaki, E.; Dzogbema, K.F.; Dolou, M.; Savadogo, M.; Orou Seko, M.; Bada Alambedji, R. Assessing farm biosecurity and farmers’ knowledge and practices concerning antibiotics and antibiotic resistance in poultry and pig farms in Southern Togo. Vet. World 2022, 15, 1727–1737. [Google Scholar] [CrossRef]
- Gulleen, E.A.; Lubwama, M.; Komakech, A.; Krantz, E.M.; Liu, C.; Phipps, W. Knowledge and perceptions of antimicrobial resistance and antimicrobial stewardship among staff at a national cancer referral center in Uganda. Antimicrob. Steward. Healthc. Epidemiol. 2022, 2, e54. [Google Scholar] [CrossRef]
- Kanyike, A.M.; Olum, R.; Kajjimu, J.; Owembabazi, S.; Ojilong, D.; Nassozi, D.R.; Amongin, J.F.; Atulinda, L.; Agaba, K.; Agira, D.; et al. Antimicrobial resistance and rational use of medicine: Knowledge, perceptions, and training of clinical health professions students in Uganda. Antimicrob. Resist. Infect. Control 2022, 11, 145. [Google Scholar] [CrossRef]
- Muleme, J.; Ssempebwa, J.C.; Musoke, D.; Kankya, C.; Wafula, S.T.; Okello, J.; Ninsiima, L.R.; Wambi, R.; Baguma, J.N.; Lubega, G.; et al. Antimicrobial resistance among farming communities in Wakiso District, Central Uganda: A knowledge, awareness and practice study. PLoS ONE 2023, 18, e0284822. [Google Scholar] [CrossRef]
- Amelia, A.; Walter, A.; Emmanuel, A.; Timothy, M.; Aminah, N.; Phillip, O.; Nekaka, R.; Stanley, I.J. Awareness of Antimicrobial Resistance among Primary Health Care Workers in Buyende District, Rural Eastern Uganda. Microbiol. Res. J. Int. 2017, 22, 1–11. [Google Scholar] [CrossRef]
- Zulu, A.; Matafwali, S.K.; Banda, M.; Mudenda, S. Assessment of knowledge, attitude and practices on antibiotic resistance among undergraduate medical students in the school of medicine at the University of Zambia. Int. J. Basic Clin. Pharmacol. 2022, 9, 263–270. [Google Scholar] [CrossRef]
- Tembo, N.; Mudenda, S.; Banda, M.; Chileshe, M.; Matafwali, S. Knowledge, attitudes and practices on antimicrobial resistance among pharmacy personnel and nurses at a tertiary hospital in Ndola, Zambia: Implications for antimicrobial stewardship programmes. JAC Antimicrob. Resist. 2022, 4, dlac107. [Google Scholar] [CrossRef] [PubMed]
- Nowbuth, A.A.; Monteiro, F.J.; Sheets, L.R.; Asombang, A.W. Assessment of the knowledge, attitudes and perceived quality of education about antimicrobial use and resistance of medical students in Zambia, Southern Africa. JAC Antimicrob. Resist. 2023, 5, dlad073. [Google Scholar] [CrossRef]
- Mufwambi, W.; Stingl, J.; Masimirembwa, C.; Manasa, J.; Nhachi, C.; Stadler, N.; Mwila, C.; Kalungia, A.C.; Mukosha, M.; Mutiti, C.S.; et al. Healthcare Professionals’ Knowledge of Pharmacogenetics and Attitudes Towards Antimicrobial Utilization in Zambia: Implications for a Precision Medicine Approach to Reducing Antimicrobial Resistance. Front. Pharmacol. 2021, 11, 551522. [Google Scholar] [CrossRef] [PubMed]
- Mudenda, S.; Mukela, M.; Matafwali, S.; Banda, M.; Mutati, R.K.; Muungo, L.T.; Daka, V.; Saad, S.A.M.; Bumbangi, F.N.; Chabalenge, B. Knowledge, Attitudes, and Practices towards Antibiotic Use and Antimicrobial Resistance among Pharmacy Students at the University of Zambia: Implications for Antimicrobial Stewardship Programmes. Sch. Acad. J. Pharm. 2022, 11, 117–124. [Google Scholar] [CrossRef]
- Mudenda, S.; Mukosha, M.; Godman, B.; Fadare, J.; Malama, S.; Munyeme, M.; Hikaambo, C.N.; Kalungia, A.C.; Hamachila, A.; Kainga, H. Knowledge, Attitudes, and Practices of Community Pharmacy Professionals on Poultry Antibiotic Dispensing, Use, and Bacterial Antimicrobial Resistance in Zambia: Implications on Antibiotic Stewardship and WHO AWaRe Classification of Antibiotics. Antibiotics 2022, 11, 1210. [Google Scholar] [CrossRef]
- Chilawa, S.; Mudenda, S.; Daka, V.; Chileshe, M.; Matafwali, S.; Chabalenge, B.; Mpundu, P.; Mufwambi, W.; Mohamed, S.; Mfune, R.L. Knowledge, Attitudes, and Practices of Poultry Farmers on Antimicrobial Use and Resistance in Kitwe, Zambia: Implications on Antimicrobial Stewardship. Open J. Anim. Sci. 2023, 13, 60–81. [Google Scholar] [CrossRef]
- Olaru, I.D.; Ferrand, R.A.; Yeung, S.; Chingono, R.; Chonzi, P.; Masunda, K.P.E.; Dixon, J.; Kranzer, K. Knowledge, attitudes and practices relating to antibiotic use and resistance among prescribers from public primary healthcare facilities in Harare, Zimbabwe. Wellcome Open Res. 2022, 6, 72. [Google Scholar] [CrossRef]
- Fuller, W.L.; Aboderin, A.O.; Yahaya, A.; Adeyemo, A.T.; Gahimbare, L.; Kapona, O.; Hamzat, O.T.; Bassoum, O. Gaps in the implementation of national core elements for sustainable antimicrobial use in the WHO-African region. Front. Antibiot. 2022, 1, 1047565. [Google Scholar] [CrossRef]
- Gahamanyi, N.; Umuhoza, T.; Saeed, S.I.; Mayigane, L.N.; Hakizimana, J.N. A Review of the Important Weapons against Antimicrobial Resistance in Sub-Saharan Africa. Appl. Biosci. 2023, 2, 136–156. [Google Scholar] [CrossRef]
- Mitchell, J.; Cooke, P.; Ahorlu, C.; Arjyal, A.; Baral, S.; Carter, L.; Dasgupta, R.; Fieroze, F.; Fonseca-Braga, M.; Huque, R.; et al. Community engagement: The key to tackling Antimicrobial Resistance (AMR) across a One Health context? Glob. Public Health 2022, 17, 2647–2664. [Google Scholar] [CrossRef] [PubMed]
- Hamers, R.L.; Dobreva, Z.; Cassini, A.; Tamara, A.; Lazarus, G.; Asadinia, K.S.; Burzo, S.; Olaru, I.D.; Dona, D.; Emdin, F.; et al. Global knowledge gaps on antimicrobial resistance in the human health sector: A scoping review. Int. J. Infect. Dis. 2023, 134, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.; Harant, A.; Fernandes, G.; Mwamelo, A.J.; Hein, W.; Dekker, D.; Sridhar, D. Measuring the global response to antimicrobial resistance, 2020–2021: A systematic governance analysis of 114 countries. Lancet Infect. Dis. 2023, 23, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Health Workers’ Education and Training on Antimicrobial Resistance: Curricula Guide; World Health Organization: Geneva, Switzerland, 2019.
- Calvo-Villamañán, A.; San Millán, Á.; Carrilero, L. Tackling AMR from a multidisciplinary perspective: A primer from education and psychology. Int. Microbiol. 2023, 26, 1–9. [Google Scholar] [CrossRef]
- Wow Wow Wow: A Club Way to Teach Young People about Drug Resistance. Available online: https://www.afro.who.int/news/wow-wow-wow-club-way-teach-young-people-about-drug-resistance (accessed on 12 September 2023).
- Acharya, K.P.; Subedi, D. Use of Social Media as a Tool to Reduce Antibiotic Usage: A Neglected Approach to Combat Antimicrobial Resistance in Low and Middle Income Countries. Front. Public Health 2020, 8, 558576. [Google Scholar] [CrossRef]
- Semambo, H. Social media as; an agent for behavioral change among young people: Case of Facebook usage among mass communication students of Uganda Martyrs University. Int. J. Res. Anal. Rev. 2020, 7, 212–229. Available online: www.ijrar.org/IJRAR2AA1032.pdf (accessed on 14 September 2023). [CrossRef]
- Al Sattar, A.; Chisty, N.N.; Irin, N.; Uddin, M.H.; Hasib, F.M.Y.; Hoque, M.A. Knowledge and practice of antimicrobial usage and resistance among poultry farmers: A systematic review, meta-analysis, and meta-regression. Vet. Res. Commun. 2023, 47, 1047–1066. [Google Scholar] [CrossRef]
- McKernan, C.; Benson, T.; Farrell, S.; Dean, M. Antimicrobial use in agriculture: Critical review of the factors influencing behaviour. JAC-Antimicrob. Resist. 2021, 3, dlab178. [Google Scholar] [CrossRef]
- Caudell, M.A.; Kiambi, S.; Afakye, K.; Koka, E.; Kabali, E.; Kimani, T.; Dorado-Garcia, A. Social-technical interventions to reduce antimicrobial resistance in agriculture: Evidence from poultry Farmer Field Schools in Ghana and Kenya. JAC Antimicrob. Resist. 2022, 4, dlab193. [Google Scholar] [CrossRef]
- Allerton, F.; Russell, J. Antimicrobial stewardship in veterinary medicine: A review of online resources. JAC Antimicrob. Resist. 2023, 5, dlad058. [Google Scholar] [CrossRef] [PubMed]
- Fortifying Veterinary Training in Fighting Antimicrobial Resistance. Available online: https://www.fao.org/europe/news/detail/fortifying-veterinary-training-in-fighting-antimicrobial-resistance/en (accessed on 15 September 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).