Current Practices and Opportunities for Outpatient Parenteral Antimicrobial Therapy in Hospitals: A National Cross-Sectional Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Participants
2.2. Survey Development and Administration
2.3. Data Analysis
2.4. Ethical Considerations
3. Results
3.1. Response and Hospital Characteristics
3.2. OPAT Performance and OPAT Program
3.3. Current OPAT Practices in The Netherlands
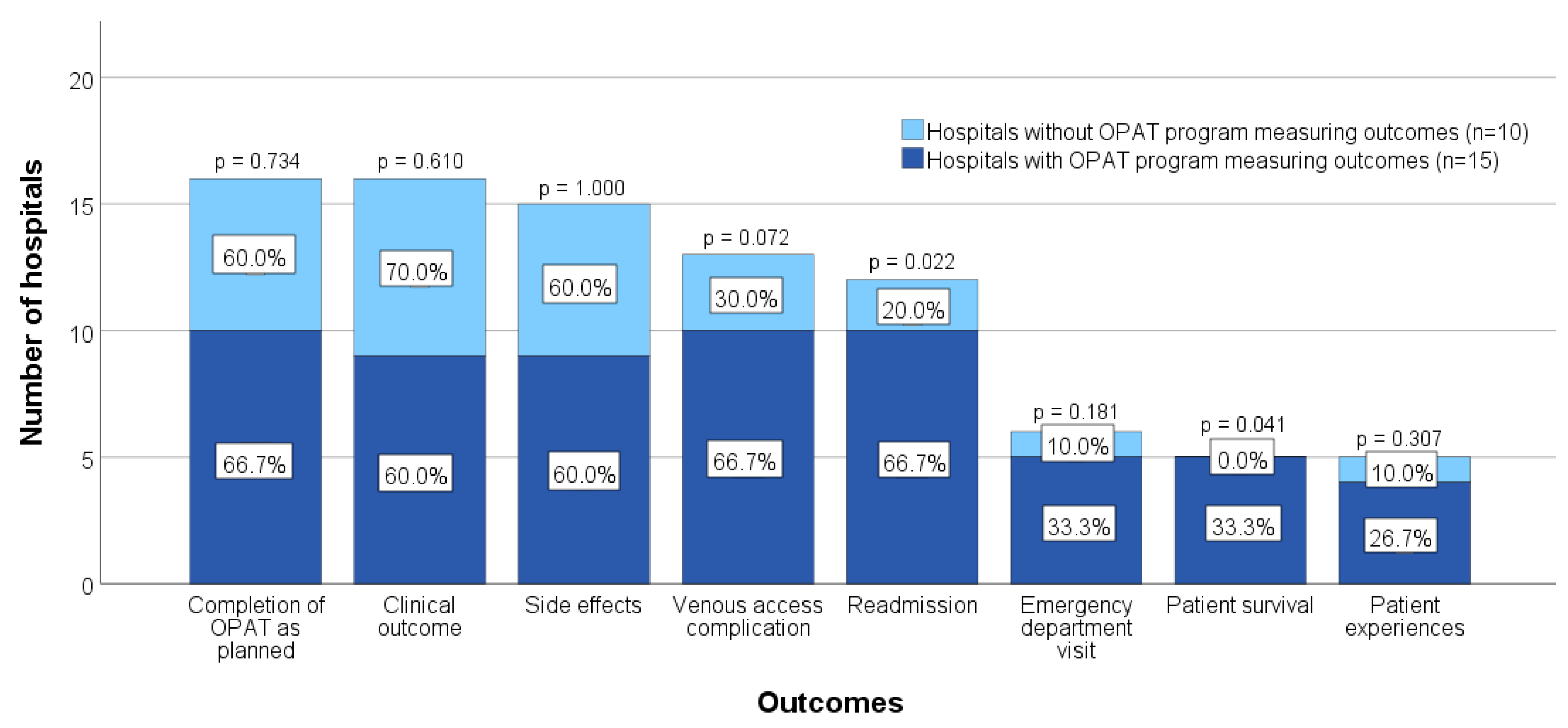
3.4. Monitoring of OPAT-Related Outcome Measures
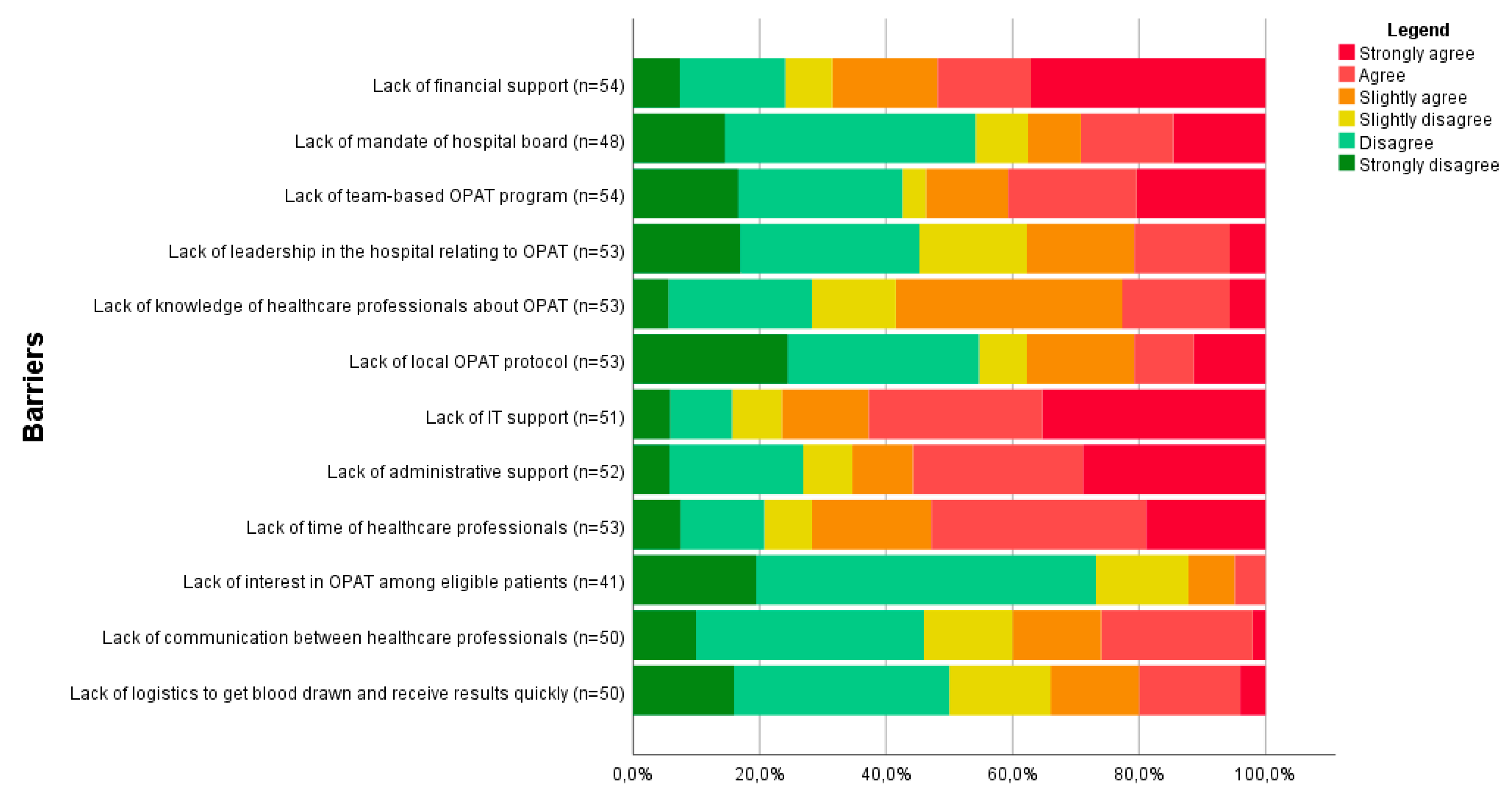
3.5. Experienced Barriers to OPAT Care
4. Discussion
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gilchrist, M.; Barr, D.; Drummond, F.; Muir, A.; Williams, J.; Scriven, J.; Snape, S.; Hemsley, C.; Durojaiye, C.O.; Patel, S.; et al. Outpatient parenteral antimicrobial therapy (OPAT) in the UK: Findings from the BSAC National Outcomes Registry (2015–19). J. Antimicrob. Chemother. 2022, 77, 1481–1490. [Google Scholar] [CrossRef] [PubMed]
- Chapman, A.L.N.; Dixon, S.; Andrews, D.; Lillie, P.; Bazaz, R.; Patchett, J.D. Clinical efficacy and cost-effectiveness of outpatient parenteral antibiotic therapy (OPAT): A UK perspective. J. Antimicrob. Chemother. 2009, 64, 1316–1324. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, R.L.; Latorraca, C.D.O.C.; dos Santos, A.P.P.; Martimbianco, A.L.C.; Moreira, R.D.F.C.; Logullo, P.; Riera, R. Efficacy and safety of home-based intravenous antibiotic therapy among adults: A systematic review. Int. J. Antimicrob. Agents 2022, 59, 106555. [Google Scholar] [CrossRef]
- Berrevoets, M.A.H.; Oerlemans, A.J.M.; Tromp, M.; Kullberg, B.J.; Oever, J.T.; Schouten, J.A.; Hulscher, M.E. Quality of outpatient parenteral antimicrobial therapy (OPAT) care from the patient’s perspective: A qualitative study. BMJ Open 2018, 8, e024564. [Google Scholar] [CrossRef] [PubMed]
- Seaton, R.; Barr, D. Outpatient parenteral antibiotic therapy: Principles and practice. Eur. J. Intern. Med. 2013, 24, 617–623. [Google Scholar] [CrossRef]
- Saillen, L.; Arensdorff, L.; Moulin, E.; Voumard, R.; Cochet, C.; Boillat-Blanco, N.; Gardiol, C.; De Vallière, S. Patient satisfaction in an outpatient parenteral antimicrobial therapy (OPAT) unit practising predominantly self-administration of antibiotics with elastomeric pumps. Eur. J. Clin. Microbiol. Infect. Dis. 2017, 36, 1387–1392. [Google Scholar] [CrossRef]
- Mitchell, E.D.; Murray, C.C.; Meads, D.; Minton, J.; Wright, J.; Twiddy, M. Clinical and cost-effectiveness, safety and acceptability of community intravenous antibiotic service models: CIVAS systematic review. BMJ Open 2017, 7, e013560. [Google Scholar] [CrossRef]
- Steffens, E.; Quintens, C.; Derdelinckx, I.; Peetermans, W.E.; Van Eldere, J.; Spriet, I.; Schuermans, A. Outpatient parenteral antimicrobial therapy and antibiotic stewardship: Opponents or teammates? Infection 2019, 47, 169–181. [Google Scholar] [CrossRef]
- Chapman, A.L.N.; Patel, S.; Horner, C.; Green, H.; Guleri, A.; Hedderwick, S.; Snape, S.; Statham, J.; Wilson, E.; Gilchrist, M.; et al. Updated good practice recommendations for outpatient parenteral antimicrobial therapy (OPAT) in adults and children in the UK. JAC-Antimicrob. Resist. 2019, 1, dlz026. [Google Scholar] [CrossRef]
- Madaline, T.; Nori, P.; Mowrey, W.; Zukowski, E.; Gohil, S.; Sarwar, U.; Weston, G.; Urrely, R.; Palombelli, M.; Pierino, V.F.; et al. Bundle in the Bronx: Impact of a Transition-of-Care Outpatient Parenteral Antibiotic Therapy Bundle on All-Cause 30-Day Hospital Readmissions. Open Forum Infect. Dis. 2017, 4, ofx097. [Google Scholar] [CrossRef]
- Huck, D.; Ginsberg, J.; Gordon, S.M.; Nowacki, A.S.; Rehm, S.J.; Shrestha, N.K. Association of laboratory test result availability and rehospitalizations in an outpatient parenteral antimicrobial therapy programme. J. Antimicrob. Chemother. 2014, 69, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Norris, A.H.; Shrestha, N.K.; Allison, G.M.; Keller, S.C.; Bhavan, K.P.; Zurlo, J.J.; Hersh, A.L.; Gorski, L.A.; Bosso, J.A.; Rathore, M.H.; et al. 2018 Infectious Diseases Society of America Clinical Practice Guideline for the Management of Outpatient Parenteral Antimicrobial Therapya. Clin. Infect. Dis. 2018, 68, e1–e35. [Google Scholar] [CrossRef] [PubMed]
- Berrevoets, M.A.H.; Oever, J.T.; Oerlemans, A.J.M.; Kullberg, B.J.; Hulscher, M.E.; Schouten, J.A. Quality Indicators for Appropriate Outpatient Parenteral Antimicrobial Therapy in Adults: A Systematic Review and RAND-modified Delphi Procedure. Clin. Infect. Dis. 2020, 70, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Grimshaw, J.M.; Eccles, M.P.; Lavis, J.N.; Hill, S.J.; Squires, J.E.; Grimshaw, J.M.; Eccles, M.P.; Lavis, J.N.; Hill, S.J.; Squires, J.E. Knowledge translation of research findings. Implement. Sci. 2012, 7, 50. [Google Scholar] [CrossRef] [PubMed]
- Hulscher, M.; Prins, J. Antibiotic stewardship: Does it work in hospital practice? A review of the evidence base. Clin. Microbiol. Infect. 2017, 23, 799–805. [Google Scholar] [CrossRef] [PubMed]
- Hamad, Y.; Lane, M.A.; Beekmann, S.E.; Polgreen, P.M.; Keller, S.C. Perspectives of United States–Based Infectious Diseases Physicians on Outpatient Parenteral Antimicrobial Therapy Practice. Open Forum Infect. Dis. 2019, 6, ofz363. [Google Scholar] [CrossRef]
- Flottorp, S.A.; Oxman, A.D.; Krause, J.; Musila, N.R.; Wensing, M.; Godycki-Cwirko, M.; Baker, R.; Eccles, M.P. A checklist for identifying determinants of practice: A systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement. Sci. 2013, 8, 35. [Google Scholar] [CrossRef]
- Ten Oever, J.; Harmsen, M.; Schouten, J.; Ouwens, M.; van der Linden, P.; Verduin, C.; Kullberg, B.; Prins, J.; Hulscher, M. Human resources required for antimicrobial stewardship teams: A Dutch consensus report. Clin. Microbiol. Infect. 2018, 24, 1273–1279. [Google Scholar] [CrossRef]
- Dutch Working Party on Antibiotic Policy (SWAB). NethMap 2021: Consumption of Antimicrobial Agents and Antimicrobial Aesistance among Medically Important Bacteria in The Netherlands, Report 2021-0062. Available online: https://rivm.openrepository.com/handle/10029/625006 (accessed on 1 June 2022).
- Dutch Working Party on Antibiotic Policy (SWAB). Praktijkgids: Implementatie Van Een OPAT-Programma in Het Ziekenhuis. Available online: https://swab.nl/en/opat-practice-guide (accessed on 1 June 2022).
- Banerjee, R.; Beekmann, S.E.; Doby, E.H.; Polgreen, P.M.; Rathore, M.H.; Hersh, A.L. Outpatient Parenteral Antimicrobial Therapy Practices among Pediatric Infectious Diseases Consultants: Results of an Emerging Infections Network Survey. J. Pediatric Infect. Dis. Soc. 2014, 3, 85–88. [Google Scholar] [CrossRef][Green Version]
- Chary, A.; Tice, A.D.; Martinelli, L.P.; Liedtke, L.A.; Plantenga, M.S.; Strausbaugh, L.J. Experience of infectious diseases consultants with outpatient parenteral antimicrobial therapy: Results of an emerging infections network survey. Clin. Infect. Dis. 2006, 43, 1290–1295. [Google Scholar] [CrossRef]
- Durojaiye, O.C.; Cartwright, K.; Ntziora, F. Outpatient parenteral antimicrobial therapy (OPAT) in the UK: A cross-sectional survey of acute hospital trusts and health boards. Diagn. Microbiol. Infect. Dis. 2019, 93, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Fisher, D.; Michaels, J.; Hase, R.; Zhang, J.; Kataria, S.; Sim, B.; Tsang, J.K.-Y.; Pollard, J.; Chan, M.; Swaminathan, S. Outpatient parenteral antibiotic therapy (OPAT) in Asia: Missing an opportunity. J. Antimicrob. Chemother. 2017, 72, 1221–1226. [Google Scholar] [CrossRef] [PubMed]
- Lane, M.A.; Marschall, J.; Beekmann, S.E.; Polgreen, P.M.; Banerjee, R.; Hersh, A.L.; Babcock, H.M. Outpatient parenteral antimicrobial therapy practices among adult infectious disease physicians. Infect. Control Hosp. Epidemiol. 2014, 35, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, E.G.; Allison, G.M.; Gallagher, D.; Snydman, D.R.; Bergin, C. Outpatient parenteral antimicrobial therapy (OPAT) in the Republic of Ireland: Results of a national survey. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 1465–1470. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, E.G.; Switkowski, K.; Tice, A.; Snydman, D.R.; Allison, G.M. A national survey of infectious disease practitioners on their use of outpatient parenteral antimicrobial therapy (OPAT). Infect. Dis. 2015, 47, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Seaton, R.A.; Nathwani, D. Outpatient and home parenteral antibiotic therapy (OHPAT) in the UK: Survey of infection specialists’ experience and views. Clin. Microbiol. Infect. 2000, 6, 387–390. [Google Scholar] [CrossRef][Green Version]
- Vaz, L.E.; Felder, K.K.; Newland, J.G.; Hersh, A.L.; Rajapakse, N.S.; Willis, Z.I.; Banerjee, R.; Gerber, J.S.; Schwenk, H.T.; Wang, M.E. A National Survey of Outpatient Parenteral Antibiotic Therapy Practices. J. Pediatric Infect. Dis. Soc. 2022, 11, 115–118. [Google Scholar] [CrossRef]
- Maraqa, N.F.; Rathore, M.H. Pediatric outpatient parenteral antimicrobial therapy: An update. Adv. Pediatr. 2010, 57, 219–245. [Google Scholar] [CrossRef]
- Yadav, K.; Suh, K.N.; Eagles, D.; Thiruganasambandamoorthy, V.; Wells, G.A.; Stiell, I.G. Evaluation of an emergency department to outpatient parenteral antibiotic therapy program for cellulitis. Am. J. Emerg. Med. 2019, 37, 2008–2014. [Google Scholar] [CrossRef]
- Browning, S.; Loewenthal, M.R.; Freelander, I.; Dobson, P.M.; Schneider, K.; Davis, J.S. Safety of prolonged outpatient courses of intravenous antibiotics: A prospective cohort study. Clin. Microbiol. Infect. 2022, 28, 832–837. [Google Scholar] [CrossRef]
- Palms, D.L.; Jacob, J.T. Close Patient Follow-up among Patients Receiving Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2020, 70, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Petrak, R.; Fliegelman, R.; Shrestha, N.; Allison, G.; Zurlo, J.; Parker, S.; Poretz, D.; McKinsey, D.; Dougherty, M.; et al. Infectious Diseases Specialty Intervention Is Associated with Better Outcomes among Privately Insured Individuals Receiving Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2019, 68, 1160–1165. [Google Scholar] [CrossRef] [PubMed]
- Rivera, C.G.; Mara, K.C.; Mahoney, M.V.; Ryan, K.L. Survey of pharmacists on their roles and perceptions of outpatient parenteral antimicrobial therapy in the United States. Antimicrob. Steward. Health Epidemiol. 2022, 2, e69. [Google Scholar] [CrossRef]
| Characteristic | With OPAT Program a (n = 22) |
|---|---|
| Composition of OPAT b team | |
| Pharmacist | 20 (90.9%) |
| Infectious disease physician | 18 (81.8%) |
| Transfer of care nurse/employee c | 17 (77.3%) |
| Nurse specialist | 11 (50.0%) |
| Clinical microbiologist | 10 (45.5%) |
| Pharmacist assistant d | 5 (22.7%) |
| Nurse | 5 (22.7%) |
| Home care nurse/employee | 2 (9.1%) |
| Internal medicine specialist | 1 (4.5%) |
| OPAT physician | 1 (4.5%) |
| Paediatric oncologist | 1 (4.5%) |
| Administrative assistant | 1 (4.5%) |
| IT specialist e | 1 (4.5%) |
| Paediatrician | 0 (0%) |
| OPAT program falling under the responsibility of the AMS f team | 17 (77.3%) |
| Annual frequency for policy meetings g of OPAT team, median (IQR h) | 4.0 (1.8–6.0) |
| Percentage of patients where the OPAT team takes on medical responsibility, median (IQR) | 7.5% (0.0–42.5) |
| Characteristic | Total a (n = 55) | With OPAT Program a (n = 22) | Without OPAT Program a (n = 33) | p-Value b |
|---|---|---|---|---|
| Location of first dose of antimicrobials c | ||||
| At home for outpatients | 8 (14.5%) | 3 (13.6%) | 5 (15.2%) | 0.876 |
| At the day care facility for outpatients | 19 (34.5%) | 13 (59.1%) | 6 (18.2%) | 0.002 |
| At the emergency department when hospital admission is unnecessary | 0 (0%) | 0 (0%) | 0 (0%) | n.a. |
| In the patient ward before discharge | 55 (100.0%) | 22 (100.0%) | 33 (100.0%) | n.a. |
| Intravenous access device (<7 days) most frequently used | 0.794 | |||
| Peripherally inserted central catheter (PICC) | 26 (47.3%) | 11 (50.0%) | 15 (45.5%) | |
| Peripheral intravenous catheter | 23 (41.8%) | 8 (36.4%) | 15 (45.5%) | |
| Central vascular access device (other than PICC) | 2 (3.6%) | 1 (4.5%) | 1 (3.0%) | |
| Midline | 1 (1.8%) | 0 (0%) | 1 (3.0%) | |
| Not applicable d | 3 (5.5%) | 2 (9.1%) | 1 (3.0%) | |
| Intravenous access device (>7 days) most frequently used | 0.329 | |||
| Peripherally inserted central catheter (PICC) | 48 (87.3%) | 18 (81.8%) | 30 (90.9%) | |
| Peripheral intravenous catheter | 0 (0%) | 0 (0%) | 0 (0%) | |
| Central vascular access device (other than PICC) | 3 (5.5%) | 1 (4.5%) | 2 (6.1%) | |
| Midline | 4 (7.3%) | 3 (13.6%) | 1 (3.0%) | |
| Infusion administration method most frequently used | 0.246 | |||
| Electronic infusion pump | 31 (56.4%) | 10 (45.5%) | 21 (63.6%) | |
| Elastomeric device | 24 (43.6%) | 12 (54.5%) | 12 (36.4%) | |
| Presence of in- and exclusion criteria for OPAT | 31 (56.4%) | 19 (86.4%) | 12 (36.4%) | <0.001 |
| Presence of a protocol for laboratory follow-up | 34 (61.8%) | 19 (86.4%) | 15 (45.5%) | 0.002 |
| Consultation with infectious disease physician mandatory before start OPAT | 12 (21.8%) | 7 (31.8%) | 5 (15.2%) | 0.143 |
| Start of OPAT reported to general physician or geriatrist | 37 (67.3%) | 15 (68.2%) | 22 (66.7%) | 0.907 |
| Possibility of self-administered OPAT by patient or carer | 16 (29.1%) | 8 (36.4%) | 8 (24.2%) | 0.332 |
| Presence of in- and exclusion criteria for S-OPAT e | 4 (25.0%) | 2 (25.0%) | 2 (25.0%) | 1.000 |
| Presence of a training program for S-OPAT | 3 (18.8%) | 0 (0%) | 3 (37.5%) | 0.055 |
| Percentage of patients performing S-OPAT, median (IQR) | 5.0% (2.3–10.0) | 5.0% (4.0–17.8) | 3.5% (1.0–10.0) | 0.442 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stoorvogel, H.H.; Hulscher, M.E.J.L.; Wertheim, H.F.L.; Yzerman, E.P.F.; Scholing, M.; Schouten, J.A.; ten Oever, J. Current Practices and Opportunities for Outpatient Parenteral Antimicrobial Therapy in Hospitals: A National Cross-Sectional Survey. Antibiotics 2022, 11, 1343. https://doi.org/10.3390/antibiotics11101343
Stoorvogel HH, Hulscher MEJL, Wertheim HFL, Yzerman EPF, Scholing M, Schouten JA, ten Oever J. Current Practices and Opportunities for Outpatient Parenteral Antimicrobial Therapy in Hospitals: A National Cross-Sectional Survey. Antibiotics. 2022; 11(10):1343. https://doi.org/10.3390/antibiotics11101343
Chicago/Turabian StyleStoorvogel, Hester H., Marlies E. J. L. Hulscher, Heiman F. L. Wertheim, Ed P. F. Yzerman, Maarten Scholing, Jeroen A. Schouten, and Jaap ten Oever. 2022. "Current Practices and Opportunities for Outpatient Parenteral Antimicrobial Therapy in Hospitals: A National Cross-Sectional Survey" Antibiotics 11, no. 10: 1343. https://doi.org/10.3390/antibiotics11101343
APA StyleStoorvogel, H. H., Hulscher, M. E. J. L., Wertheim, H. F. L., Yzerman, E. P. F., Scholing, M., Schouten, J. A., & ten Oever, J. (2022). Current Practices and Opportunities for Outpatient Parenteral Antimicrobial Therapy in Hospitals: A National Cross-Sectional Survey. Antibiotics, 11(10), 1343. https://doi.org/10.3390/antibiotics11101343






