Abstract
Background: The most recommended treatment for a Helicobacter pylori infection is high doses of combined antibiotics. The objective of this article is to perform a systematic review of the economic evaluation studies applied to assess the efficiency of diagnostic testing for H. pylori infections, so that their main characteristics can be identified and to learn from the literature how the antimicrobial resistance (AMR) issue is incorporated into these economic evaluations. Methods: We conducted a systematic review to compare the costs and clinical effectiveness of diagnostic strategies for H. pylori infections. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and extracted the items from the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist. Results: We found thirteen articles that were of good quality according to CHEERS: six studies focused on diagnostics of Helicobacter pylori infections associated with dyspepsia and four on duodenal ulcers. Testing was found to be the most cost-effective strategy in eight articles. Four studies considered AMR. Conclusions: Testing was more cost-effective than empirical treatment, except in cases of high prevalence (as with developing countries) or when patients could be stratified according to their comorbidities. The introduction of AMR into the model may change the efficiency of the testing strategy.
1. Introduction
Helicobacter pylori (hence forth referred to as H. pylori) infection affects over half the world’s population [1]. As described by Warren and Marshall in 1983 [2], this infection has been associated with disorders such as peptic ulcers, chronic gastritis, dyspepsia, lymphomas of lymphoid tissue of the gastric mucosa and gastric cancer [3,4,5]. H. pylori has been reported to cause 90% of duodenal ulcers and 80% of gastric ulcers [6].
The frequency of H. pylori infection and its consequences has influenced the definition of treatment standards. The V Maastricht Consensus for the Treatment of H. pylori Infections (2015) [7] recognizes the implications that antimicrobial resistance has had on the effectiveness of treatments. The Consensus notes the increasing rates of resistance in high and middle-income countries. Levels of resistance to clarithromycin reach 30% in Italy and Japan, 40% in Turkey and 50% in China, among others [8,9,10,11,12,13]. Therefore, the Consensus recommends that standard triple therapy (the combination of PPI (proton pump inhibitor)-clarithromycin and amoxicillin or metronidazole) without prior susceptibility testing should not be used when resistance to clarithromycin exceeds 15%. Furthermore, another cause of reduction in the eradication rate is the presence of biofilms on the surface of gastric mucosa, which may cause antibiotic treatment to fail. As noted in the literature, H. pylori biofilm formation increases the threat of antimicrobial resistance (AMR) development [14].
At present, the adequate treatment of H. pylori infections requires progress in two areas: improving the quality of existing or new diagnostic tests so that infections are identified more quickly and accurately [15,16,17] and widening the diagnostic options to detect better AMR before treatment is prescribed.
Non-invasive and invasive methods are currently available for diagnosing H. pylori [1,18]. Most frequently included among the former are the urea breath test (UBT) and the stool antigen test. The invasive diagnostic option is the upper endoscopy, including histological testing, polymerase chain reaction (PCR), culture and rapid urease testing (RUT). PCR tests have been proposed as one of the diagnostic alternatives to avoid endoscopies and to evaluate bacterial resistance. It has been reported that the Amplidiag H. pylory+ClariR Mobidiag essay has a high sensitivity and specificity for the detection of both H. pylori and CLA resistance [19].
Evidence of the role of antimicrobial resistance in reducing the rate of eradication influences the use of other therapeutic options, such as bismuth quadruple therapy, quadruple sequential therapy, quadruple concomitant therapy (QCT) and hybrid therapy [20]. It has been reported that QCT may overcome the declining H. pylori eradication rate [20]. Although quadruple-regimen therapy (bismuth or non-bismuth) has been reported to be useful when resistance to clarithromycin or metronidazole is present, it also increases resistance if treatment is prolonged with multiple antibiotics [21].
The worrying evolution of the increase in AMR, including primary resistance, has generated a growing international consensus on the importance of tailored therapy through analysis of susceptibility prior to the initiation of treatment for H. pylori infection [6,21,22]. However, susceptibility testing is not commonly performed [22]. The high frequency of this infection results in the use of primary care services, causing indications of antibiotics and increasing the chances of antimicrobial resistance. That is why it is particularly important to analyze the economic evaluation of diagnostic alternatives in these diseases that will facilitate the adoption of evidence-based decision strategies regarding antibiotic treatments and, consequently, the potential reduction of AMR. We are particularly interested in the studies that examine the existence of AMR and its effects on the efficiency of antibiotic treatment.
The objective of this article is twofold. First, we perform a systematic review of the economic evaluation studies applied to assess the efficiency of diagnostic testing for the H. pylori infection. We intend to summarize the methods applied to these economic evaluations and to highlight the main characteristics of these studies. The second objective is to learn from the literature review how the AMR issue is incorporated in economic evaluation of diagnostic testing.
2. Materials and Methods
2.1. Types of Studies
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed in this study [23]. Articles included in this review compare both the costs and the clinical effectiveness outcomes of at least two different diagnostic strategies for H. pylori infection. We assess the efficiency a strategy that reduces the uncertainty of the physician when a patient with symptoms common to several diseases must be diagnosed in clinical practice. Accordingly, screening and genotype studies were excluded. The main difference between diagnostics and screening is the population: in the former it concerns patients presenting with symptoms and in the latter it concerns the general population which is to be healthy [24,25]. Protocols and review articles were also excluded.
2.2. Search Strategy and Selection Criteria
The syntax used in the search was created to retrieve economic evaluations of diagnostic strategies for the management of H. pylori infection (Appendix A). Articles included in this systematic review were obtained from three databases of peer-reviewed literature: Scopus, PubMed and Web of Science. Geographical limitations were not established but in order to provide updates on clinical practice, only articles published between January 2000 and October 2020 were included. The first round consisted of title and abstract screening performed by P.R.G., M.G., R.R.I., C.A.J.C. and S.v.d.P. Duplicates were removed and articles were selected according to the aforementioned inclusion criteria. In the second step, full-text reports were evaluated for eligibility. In case of any discrepancy among the reviewers, another reviewer was asked (A.D.I.v.A.).
2.3. Data Extraction and Analysis
In order to obtain the data from the included articles, authors followed the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist, performing consistency checks as recommended [26]. Furthermore, new items not considered in the CHEERS checklist were added: AMR included in the model, specific limitation found relating to the diagnostic strategy and the pros and cons of the modelling technique identified by the authors. Microsoft Excel was used to manage data extraction and categorize articles by the management of infection. This software was also used to transform data and create tables. The references manager Zotero was used to store the bibliography.
3. Results
A total of thirteen articles were retrieved through the systematic review. Figure 1 shows a PRISMA flow diagram of inclusion and exclusion number of articles. According to the abstract of these articles, we have classified the studies into three groups: diagnostics of H. pylori infection associated with dyspepsia, diagnostics associated with duodenal ulcers and diagnostics associated with other symptoms.
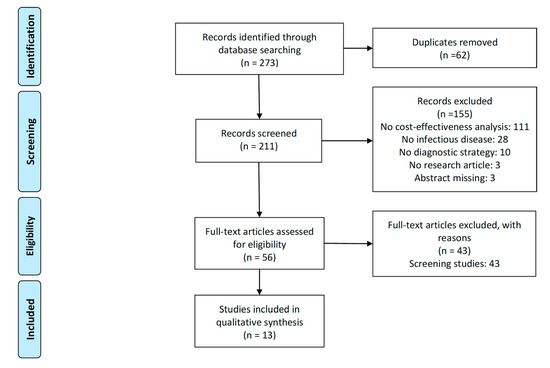
Figure 1.
PRISMA flow diagram.
Table 1 shows the quality of the articles, in terms of the items reported and recommended in the CHEERS checklist. Most items were found in the articles. Most of the articles had a time horizon of less than one year, so it was not necessary to report discount rates.

Table 1.
CHEERS checklist results (percentage of articles that included the item).
3.1. Diagnostics of H. pylori Infection Associated with Dyspepsia
Six articles [27,28,29,30,31,32] examined the cost-effectiveness of a range of test and treat strategies to manage patients attending primary care with dyspepsia as the predominant symptom. Table 2 shows the models’ main characteristics. Two models [30,32] introduced AMR into the analysis: reducing the eradication rate for triple therapy (ranitidine, metronidazole and tetracycline) from 80–100% to 50–100%, arguing that as in China over-the-counter antibiotics are occasionally available, AMR may cause a higher failure rate [30] and reducing the eradication rate, as the prevalence of clarithromycin resistance increases [32]. All articles assess the use of a H. pylori test and in four of them this was found to be the most cost-effective strategy. In one of the other two cases, the most cost-effective strategy was to stratify patients using a score system (using a previously validated predictive model) then referring those at higher risk of organic dyspepsia to endoscopy [29]. In the other one, treating them with empiric PPI even when the prevalence of H. pylori infection varied from 5% to 40% [31]. This last result was reached after authors modelled how the test is actually used in U.S. practice, assuming that clinicians would perform a biopsy in the case of a lack of symptomatic relief, thus reducing the benefits of testing.

Table 2.
Articles related to diagnosing H. pylori infection associated with dyspepsia.
3.2. Diagnostics of H. pylori Infection Associated with Duodenal Ulcers
Four articles [33,34,35,36] studied the cost-effectiveness of alternative strategies of diagnosing H. pylori infection in patients with duodenal ulcers. Table 3 shows the main characteristics of the models. In two articles [34,35] empirical triple therapy was the most cost-effective approach, considering that the analysis was performed in a country with high prevalence of the infection and first-line therapy was more cost-effective than treatment for recurrent ulcers or long-term maintenance treatment. One model [36] introduced AMR into the analysis, taking into consideration that diagnostic testing can provide rapid and reliable results regarding the presence of clarithromycin resistance. The dual priming oligonucleotide (DPO) PCR test, which gives information regarding clarithromycin resistance, reduced secondary prescriptions, thus making this strategy more cost-effective than other diagnostic approaches, such as rapid urease tests.

Table 3.
Articles related to diagnosing H. pylori infection associated with duodenal ulcers.
3.3. Diagnostics of. H. pylori Infection
Three articles [37,38,39] studied the cost-effectiveness of alternative initial strategies of diagnosing H. pylori infection in patients attending primary care with any predominant symptom. Table 4 shows the models’ main characteristics. Two studies [37,39] found that the initial test for H. pylori was the most cost-effective strategy, although this result depended on the prevalence of the H. pylori infection. The other article [38] introduced AMR into its analysis, considering that, if the first antibiotic treatment failed due to clarithromycin-resistance, the patient was treated with metronidazole. In this case, testing for H. pylori was not cost effective in the given modest prevalence of clarithromycin resistance. When the model considered a high prevalence of clarithromycin resistance (>45%), testing was the most cost-effective alternative.

Table 4.
Articles related to diagnosing H. pylori infection with other symptoms.
4. Discussion
In the present literature review, thirteen articles related to the efficiency of diagnostic testing for H. pylori infection were retrieved following the PRISMA guidelines. All of them are of a good quality in terms of the items reported and recommended in the CHEERS checklist. A preferable strategy should reflect a long-term time horizon (as H. pylori infections can lead to other health conditions), include AMR in the analysis (which could be as simple as reducing the disease eradication rate based on the prevalence of resistant infections in the population) and report time or costs until correct diagnosis or appropriate treatment prescribed (due to the high antibiotic doses that the treatment of H. pylori demands). As new and faster diagnostic tests become available, economic evaluations should be used to assess their cost-effectiveness.
This review represents a small number of studies. In the 1990s, the diagnosis of H. pylori infection was based on invasive approaches such as endoscopy [40]. Eight articles were published between 2000 and 2010, highlighting the rise of the breath test, which led to a proliferation of these studies. The current literature focuses on the increasing demand for rapid non-invasive tests that can inform prescriptions. The standard treatment for H. pylori infection is based on high doses of combined antibiotics and second-line antibiotics with more risk of AMR [15]. The most recently published articles consider AMR in their analysis, decreasing the eradication figures [30,32,38]. In these articles, the study is performed in a country where antibiotics can be occasionally obtained over the counter (year 2006, China) or in high-resistance areas (Greece and Japan), leading to AMR causing a higher failure rate. Even in other countries where antibiotics are only given with a prescription, the rate of patients that present resistance to antibiotics is increasing, worsening this public health threat [41]. The inclusion of AMR into the analysis has been done by reducing the rate of antibiotic efficacy but other alternatives such as increasing treatment costs have not been found in any article. Interestingly, AMR can change the results of the most cost-effective strategy to diagnose H. pylori infections [38]. Furthermore, the CHEERS checklist focused on methodological issues, thus the inclusion of AMR is not considered as an important item to be reported.
The lack, or even delay, of diagnostic tests for the H. pylori infection increases the risk of developing not only AMR but also significant complications [17,42]. In this review, nine articles reported a time horizon of one year or shorter. Only three articles used a longer time horizon in order to capture the medical consequences of developing gastric cancer [31], acute treatment failure [43] or childhood acute lymphoblastic leukemia [44]. The reviewed articles did not consider either the relapses or biofilm formation, perhaps due to the short time horizon reported in the majority of the studies. Future studies could be extended using other forms of modeling. In this review, most of the articles (78%) used a decision tree to determine the cost-effectiveness of different diagnostic techniques. Only three articles performed a Markov model and two of them [31,44] considered an extended time horizon. The most frequent clinical outcome reported was cost or length of time until correct diagnosis [32,33,37,38,39,45], cost per appropriate treatment prescribed [27,30,34,45] and second-line antibiotics treatment safely avoided [36], which highlights the importance of a correct diagnosis to reduce unnecessary antibiotic treatment. Also, quality adjusted life year (QALYs) [35,44] and days free from disease [28,29,31] were used.
As a limitation, this review specifically excludes screening studies, which are carried out in some regions due to the higher prevalence of H. pylori infections in older patients, as an effect of a generation exposed to poor sanitation [46]; the number of articles finally selected was therefore substantially reduced. However, we wanted to assess the cost-effectiveness of a testing strategy when the patient has at least one related symptom of infection. Screening studies do not take any previous symptoms into consideration. Setting was not reported particularly in articles of H. pylori infection associated with dyspepsia or duodenal ulcers, discerning between screening and diagnostics strategies was not straightforward. In all cases, the reviewers agreed on inclusion, if the article assessed a diagnostic test or exclusion, if the article considered a screening strategy. The number of studies found was geographically limited and, apart from Spain and Greece, there were no studies from other European countries. It would be interesting to know the efficiency of this diagnostic approach in regions other than the USA and Asia, in order to select the most appropriate for H. pylori infection. Finally, although we limited the published year to include last two decades studies, we believe that this period is wide enough to capture the time when the economic evaluation of this issue has been performed.
At this point, it is interesting to know how economic evaluation has been applied to the H. pylori infection so that the results on the efficiency of the different options can guide the adoption of decisions related to testing strategy. As with any other diagnostic technology, its efficiency is subject to the assumptions made on subsequent treatments; furthermore, given that these treatments are based on antibiotics, the considerations about the potential generation of resistances and its costs may drastically change the indication of the technology’s ultimate efficiency. How all these aspects can be accounted for in different studies is an interesting issue to be analyzed and included in future research.
Author Contributions
Conceptualization, P.R.G., M.G., F.A., R.R.-I., C.A.J.-C.; methodology, P.R.G., M.G., S.v.d.P., A.D.I.v.A.; software, P.R.G., S.v.d.P.; validation, P.R.G., M.G., F.A., R.R.-I., C.A.J.-C., S.v.d.P., A.D.I.v.A., M.P.; formal analysis, P.R.G., M.G.; investigation, P.R.G., M.G., R.R.-I., C.A.J.-C.; re-sources, P.R.G., M.G., F.A., R.R.-I., C.A.J.-C., S.v.d.P., A.D.I.v.A., M.P.; data curation, P.R.G., S.v.d.P.; writing—original draft preparation, P.R.G., M.G.; writing—review and editing, P.R.G., M.G., F.A., R.R.-I., C.A.J.-C., S.v.d.P., A.D.I.v.A., M.P.; visualization, P.R.G., S.v.d.P.; supervision, F.A.; project administration, P.R.G., S.v.d.P.; funding acquisition, F.A., M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No. 820755. This Joint Undertaking receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA and bioMérieux SA, Janssen Pharmaceutica NV, Accelerate Diagnostics S.L., Abbott, Bio-Rad Laboratories, BD Switzerland Sàrl and The Wellcome Trust Limited.
Data Availability Statement
Data is contained within the article.
Acknowledgments
The authors thank Gabriela Bittencourt Gonzalez Mosegui, Carmen Torres and David Soldevilla for their contribution and collaboration in this study.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Syntax used in the search to retrieve economic evaluation of diagnostic strategies for the management of H. pylori infections.
| SCOPUS |
| (TITLE-ABS-KEY(pharmacoeconomic *) |
| OR TITLE-ABS-KEY(cost-effectiveness) |
| OR TITLE-ABS-KEY(“economic evaluation”) |
| OR TITLE-ABS-KEY(“health technology assessment”)) |
| AND (TITLE-ABS-KEY(antibiotic*) |
| OR TITLE-ABS-KEY(infectious) |
| OR TITLE-ABS-KEY(“bacterial infection”) |
| OR TITLE-ABS-KEY(“viral infection”)) |
| AND (TITLE-ABS-KEY(“diagnostic”) |
| OR TITLE-ABS-KEY(“diagnostics”) |
| OR TITLE-ABS-KEY(“test”) |
| OR TITLE-ABS-KEY(“tests”) |
| OR TITLE-ABS-KEY(“testing”)) |
| AND (TITLE-ABS-KEY(“pylori”)) |
| AND PUBYEAR > 1999 |
| AND PUBYEAR < 2020 |
| PUBMED |
| (infectious |
| OR “bacterial infection” |
| OR “viral infection” |
| OR antibiotic * |
| OR antimicrobial) |
| AND (“diagnostic” |
| OR “diagnostics” |
| OR “test” |
| OR “tests” |
| OR “testing”) |
| AND (“1 Januray 2000”[Date—Publication]: “31 December 2020”[Date—Publication]) |
| AND (pharmacoeconomic * |
| OR “cost-effectiveness” |
| OR “economic evaluation” |
| OR “health technology assessment”) |
| AND (“pylori”) |
| WEB OF SCIENCE |
| TS = (((“bacterial infection” |
| OR “viral infection” |
| OR antibiotic * |
| OR antimicrobial |
| OR infectious) |
| AND (“diagnostics” |
| OR “diagnostic” |
| OR “test” |
| OR “tests” |
| OR “testing”) |
| AND |
| (pharmacoeconomic* |
| OR cost-effectiveness |
| OR “economic evaluation” |
| OR “health technology assessment”) |
| AND (“pylori”))) |
| Period of time: 2000–2020 |
References
- Guevara, B.; Cogdill, A.G. Helicobacter pylori: A Review of Current Diagnostic and Management Strategies. Dig. Dis Sci. 2020, 65, 1917–1931. [Google Scholar] [CrossRef]
- Warren, J.R.; Marshall, B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet 1983, 1, 1273–1275. [Google Scholar]
- Hu, Y.; Wan, J.-H.; Li, X.-Y.; Zhu, Y.; Graham, D.Y.; Lu, N.-H. Systematic review with meta-analysis: The global recurrence rate of Helicobacter pylori. Aliment. Pharmacol Ther. 2017, 46, 773–779. [Google Scholar] [CrossRef]
- Plummer, M.; Franceschi, S.; Vignat, J.; Forman, D.; de Martel, C. Global burden of gastric cancer attributable to Helicobacter pylori. Int. J. Cancer 2015, 136, 487–490. [Google Scholar] [CrossRef]
- Chey, W.D.; Leontiadis, G.I.; Howden, C.W.; Moss, S.F. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am. J. Gastroenterol. 2017, 112, 212–239. [Google Scholar] [CrossRef]
- Kasahun, G.G.; Demoz, G.T.; Desta, D.M. Primary Resistance Pattern of Helicobacter pylori to Antibiotics in Adult Population: A Systematic Review. Infect. Drug Resist. 2020, 13, 1567–1573. [Google Scholar] [CrossRef]
- Malfertheiner, P.; Megraud, F.; O’morain, C.A.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.T.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut 2017, 66, 6–30. [Google Scholar] [CrossRef]
- Boyanova, L.; Gergova, G.; Evstatiev, I.; Spassova, Z.; Kandilarov, N.; Yaneva, P.; Markovska, R.; Mitov, I. Helicobacter pylori resistance to six antibiotics by two breakpoint systems and resistance evolution in Bulgaria. Infect. Dis. 2016, 48, 56–62. [Google Scholar] [CrossRef]
- Megraud, F.; Coenen, S.; Versporten, A.; Kist, M.; Lopez-Brea, M.; Hirschl, A.M.; Andersen, L.P.; Goossens, H.; Glupczynski, Y. Helicobacter pylori resistance to antibiotics in Europe and its relationship to antibiotic consumption. Gut 2013, 62, 34–42. [Google Scholar] [CrossRef]
- Saracino, I.M.; Zullo, A.; Holton, J.; Castelli, V.; Fiorini, G.; Zaccaro, C.; Ridola, L.; Ricci, C.; Gatta, L.; Vaira, D. High prevalence of primary antibiotic resistance in Helicobacter pylori isolates in Italy. J. Gastrointestin. Liver Dis. 2012, 21, 363–365. [Google Scholar]
- Kobayashi, I.; Murakami, K.; Kato, M.; Kato, S.; Azuma, T.; Takahashi, S.I.; Uemura, N.; Katsuyama, T.; Fukuda, Y.; Haruma, K.; et al. Changing antimicrobial susceptibility epidemiology of Helicobacter pylori strains in Japan between 2002 and 2005. J. Clin. Microbiol. 2007, 45, 4006–4010. [Google Scholar] [CrossRef] [PubMed]
- Toros, A.B.; Ince, A.T.; Kesici, B.; Saglam, M.; Polat, Z.; Uygun, A. A new modified concomitant therapy for Helicobacter pylori eradication in Turkey. Helicobacter 2011, 16, 225–228. [Google Scholar] [CrossRef]
- Lu, H.; Zhang, W.; Graham, D.Y. Bismuth-containing quadruple therapy for Helicobacter pylori: Lessons from China. Eur. J. Gastroenterol. Hepatol. 2013, 25, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Yonezawa, H.; Osaki, T.; Kamiya, S. Biofilm Formation by Helicobacter pylori and Its Involvement for Antibiotic Resistance; Manfredi, M., Ed.; BioMed Research International Hindawi Publishing Corporation: London, UK, 2015. [Google Scholar]
- O’Morain, N.R.; Dore, M.P.; O’Connor, A.J.P.; Gisbert, J.P.; O’Morain, C.A. Treatment of Helicobacter pylori infection in 2018. Helicobacter 2018, 23 (Suppl. S1), e12519. [Google Scholar]
- Delgado, J.S.; García-Iglesias, P.; Titó, L.; Puig, I.; Planella, M.; Gené, E.; Saló, J.; Martínez-Cerezo, F.; Molina-Infante, J.; Gisbert, J.P.; et al. Update on the management of Helicobacter pylori infection. Position paper from the Catalan Society of Digestology. Gastroenterol. Hepatol. 2018, 41, 272–280. [Google Scholar]
- González-Carbajal Pascual, M.; Martínez Leyva, L. MAASTRICHT III and dyspepsia. Reasons for a discrepancy. Rev. Cubana Med. 2008, 47, 4. [Google Scholar]
- Saleem, N.; Howden, C.W. Update on the Management of Helicobacter pylori Infection. Curr. Treat. Options Gastroenterol. 2020, 18, 476–487. [Google Scholar] [CrossRef]
- Pichon, M.; Pichard, B.; Barrioz, T.; Plouzeau, C.; Croquet, V.; Fotsing, G.; Chéron, A.; Vuillemin, É.; Wangermez, M.; Haineaux, P.A.; et al. Diagnostic Accuracy of a Noninvasive Test for Detection of Helicobacter pylori and Resistance to Clarithromycin in Stool by the Amplidiag H. pylori+ClariR Real-Time PCR Assay. J. Clin. Microbiol. 2020, 58, e01787-19. [Google Scholar] [CrossRef]
- Zou, Y.; Qian, X.; Liu, X.; Song, Y.; Song, C.; Wu, S.; An, Y.; Yuan, R.; Wang, Y.; Xie, Y. The effect of antibiotic resistance on Helicobacter pylori eradication efficacy: A systematic review and meta-analysis. Helicobacter 2020, 25, e12714. [Google Scholar] [CrossRef]
- Kim, S.Y.; Chung, J.-W. Best Helicobacter pylori Eradication Strategy in the Era of Antibiotic Resistance. Antibiotics 2020, 9, 436. [Google Scholar] [CrossRef]
- Savoldi, A.; Carrara, E.; Graham, D.Y.; Conti, M.; Tacconelli, E. Prevalence of Antibiotic Resistance in Helicobacter pylori: A Systematic Review and Meta-analysis in World Health Organization Regions. Gastroenterology 2018, 155, 1372–1382.e17. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Pulia, M.S.; O’Brien, T.P.; Hou, P.C.; Schuman, A.; Sambursky, R. Multi-Tiered Screening and Diagnosis Strategy for COVID-19: A Model. for Sustainable Testing Capacity in Response to Pandemic. Ann. Med. 2020, 52, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Bhise, V.; Rajan, S.S.; Sittig, D.F.; Morgan, R.O.; Chaudhary, P.; Singh, H. Defining and Measuring Diagnostic Uncertainty in Medicine: A Systematic Review. J. Gen. Intern. Med. 2018, 33, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Husereau, D. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013, 346, 1049. [Google Scholar] [CrossRef]
- Chey, W.D.; Fendrick, A.M. Noninvasive Helicobacter pylori testing for the “test-and-treat” strategy: A decision analysis to assess the effect of past infection on test choice. Arch. Intern. Med. 2001, 161, 2129–2132. [Google Scholar] [CrossRef][Green Version]
- Makris, N.; Barkun, A.; Crott, R.; Fallone, C.A. Cost-effectiveness of alternative approaches in the management of dyspepsia. Int. J. Technol. Assess. Health Care 2003, 19, 446–464. [Google Scholar] [CrossRef]
- García-Altés, A.; Rota, R.; Barenys, M.; Abad, Á.; Moreno, V.; Pons, J.M.; Piqué, J. Cost-effectiveness of a “score and scope” strategy for the management of dyspepsia. Eur. J. Gastroenterol. Hepatol. 2005, 17, 709–719. [Google Scholar]
- You, J.H.S.; Wong, P.-L.; Wu, J.C.Y. Cost-effectiveness of Helicobacter pylori “test and treat” for patients with typical reflux symptoms in a population with a high prevalence of H. pylori infection: A Markov model analysis. Scand. J. Gastroenterol. 2006, 41, 21–29. [Google Scholar] [CrossRef]
- Holmes, K.P.; Fang, J.C.; Jackson, B.R. Cost-effectiveness of six strategies for Helicobacter pyloridiagnosis and management in uninvestigated dyspepsia assuming a high resource intensity practice pattern. BMC Health Serv. Res. 2010, 10, 344. [Google Scholar] [CrossRef]
- Papaefthymiou, A.; Liatsos, C.; Georgopoulos, S.D.; Apostolopoulos, P.; Doulberis, M.; Kyriakos, N.; Giakoumis, M.; Papadomichelakis, M.; Galanopoulos, M.; Katsinelos, P.; et al. Helicobacter pylori eradication regimens in an antibiotic high-resistance European area: A cost-effectiveness analysis. Helicobacter 2020, 25, e12666. [Google Scholar] [CrossRef] [PubMed]
- Rich, M.; Scheiman, J.M.; Tierney, W.; Fendrick, A.M. Is upper gastrointestinal radiography a cost-effective alternative to a Helicobacter pylori “test and treat” strategy for patients with suspected peptic ulcer disease? Am. J. Gastroenterol. 2000, 95, 651–658. [Google Scholar] [PubMed]
- Ghoshal, U.C.; Das, A. Management strategies for duodenal ulcer in India in the Helicobacter pylori era: An economic analysis. Natl. Med J. India 2002, 15, 140–144. [Google Scholar] [PubMed]
- Ghoshal, U.C.; Aggarwal, R.; Sreenivasa Baba, C. Recurrent duodenal ulcer haemorrhage: A pharmacoeconomic comparison of various management strategies. Expert Opin. Pharmacother. 2003, 4, 1593–1603. [Google Scholar] [CrossRef]
- Cho, J.-H.; Jeon, S.R.; Kim, H.G.; Jin, S.-Y.; Park, S. Cost-effectiveness of a tailored Helicobacter pylori eradication strategy based on the presence of a 23S ribosomal RNA point mutation that causes clarithromycin resistance in Korean patients. J. Gastroenterol. Hepatol. 2019, 34, 700–706. [Google Scholar] [CrossRef]
- Vakil, N.; Rhew, D.; Soll, A.; Ofman, J.J. The cost-effectiveness of diagnostic testing strategies for Helicobacter pylori. Am. J. Gastroenterol. 2000, 95, 1691–1698. [Google Scholar] [CrossRef]
- Omata, F.; Shimbo, T.; Ohde, S.; Deshpande, G.A. Cost-Effectiveness Analysis of Helicobacter Pylori Diagnostic Methods in the Patients with Atrophic Gastritis. Gastroenterology 2017, 152, S448. [Google Scholar] [CrossRef][Green Version]
- Beresniak, A.; Malfertheiner, P.; Franceschi, F.; Liebaert, F.; Salhi, H.; Gisbert, J.P. Helicobacter pylori “Test-and-Treat” strategy with urea breath test: A cost-effective strategy for the management of dyspepsia and the prevention of ulcer and gastric cancer in Spain—Results of the Hp-Breath initiative. Helicobacter 2020, 25, e12693. [Google Scholar] [CrossRef]
- Shirin, H.; Kenet, G.; Shevah, O.; Wardi, Y.; Birkenfeld, S.; Shahmurov, M.; Bruck, R.; Niv, Y.; Moss, S.F.; Avni, Y. Evaluation of a novel continuous real time 13C urea breath analyser for Helicobacter pylori. Aliment. Pharmacol. Ther. 2001, 15, 389–394. [Google Scholar] [CrossRef]
- Hirayama, Y.; Kawai, T.; Otaki, J.; Kawakami, K.; Harada, Y. Prevalence of Helicobacter pylori infection with healthy subjects in Japan. J. Gastroenterol. Hepatol. 2014, 29, 16–19. [Google Scholar] [CrossRef]
- Castañeda Guillot, C. Sobrecrecimiento bacteriano intestinal. Rev. Médica Chile 2006, 8, 4–7. [Google Scholar]
- Xuan, S.; Zangwill, K.M.; Ni, W.; Ma, J.; Hay, J.W. Cost-Effectiveness Analysis of Four Common Diagnostic Methods for Clostridioides difficile Infection. J. Gen. Intern. Med. 2020, 35, 1102–1110. [Google Scholar] [CrossRef] [PubMed]
- Kastenberg, Z.J.; Hurley, M.P.; Luan, A.; Vasu-Devan, V.; Spain, D.A.; Owens, D.K.; Goldhaber-Fiebert, J.D. Cost-effectiveness of preoperative imaging for appendicitis after indeterminate ultrasonography in the second or third trimester of pregnancy. Obstet. Gynecol. 2013, 122, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Shen, B. Diagnosis and treatment of patients with pouchitis. Drugs 2003, 63, 453–461. [Google Scholar] [CrossRef]
- Pilotto, A.; Franceschi, M. Helicobacter pylori infection in older people. World J. Gastroenterol. 2014, 20, 6364–6373. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).