Abstract
Introduction: 3D-printing is an emerging technology in the field of prosthetics, offering advantages such as cost-effectiveness, ease of customization, and improved accessibility. While previous reviews have focused on limited aspects, the aim of this systematic review is to provide a comprehensive evaluation of the clinical outcomes of 3D-printed prostheses for both upper and lower limbs. Methods: A search was conducted following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines across six databases (PubMed, Web of Science, EBSCO, Scopus, Cochrane Library, and Sage). Studies on 3D-printed prostheses in human rehabilitation that focused on the clinical outcomes of the device were included, while studies lacking clinical data, 3D printing details, or focusing on traditional manufacturing methods were excluded. Finally, the risk of bias was assessed using the modified Downs & Black Checklist. Results: A total of 1420 studies were identified, with 11 meeting the inclusion criteria. The included studies assessed different 3D-printed prosthetic types and upper and lower limb prostheses. The main clinical outcomes analyzed were functional performance, design and material integrity, and overall effectiveness of 3D-printed prostheses. Studies on upper limb prostheses reported improved dexterity, range of motion (ROM), and user satisfaction, despite some durability limitations. Lower limb prostheses showed enhancements in comfort, gait parameters, and customization, particularly in amphibious and partial foot designs. Conclusions: 3D-printed prostheses show potential to improve functional performance, patient satisfaction, fit, and implementation feasibility compared to conventional methods. However, limitations such as small sample sizes, variability in assessment tools, and limited high-quality evidence highlight the need for further research to support broader clinical adoption.
1. Introduction
3D printing and scanning have emerged as promising technologies with the potential to transform the field of prosthetics [1,2]. These technologies offer a competitive alternative to conventional prosthetic manufacturing by providing advantages such as cost-effectiveness [3], customization [2], rapid reprinting [4,5], improved comfort [6], enhanced user satisfaction [7], better functional performance [8], higher acceptance among users [9], reduced fitting errors [10], and the possibility of remote fitting [11,12].
While previous systematic reviews have explored aspects of 3D-printed prostheses, they have been limited in scope. For example, Kim et al. [13] focused on the structural integrity of 3D-printed prosthetic sockets, Diment et al. [14] evaluated the clinical viability of upper-limb prostheses, and Abbady et al. [15] considered prosthetic applications in low- and lower–middle-income countries. However, to the best of the authors’ knowledge, no comprehensive review has systematically assessed the clinical outcomes of both upper and lower limb 3D-printed prostheses. Evaluating both types is important because upper and lower limb prostheses serve distinct functional roles—upper limb devices primarily support fine and gross motor activities, while lower limb devices are critical for mobility, gait, and weight-bearing function—yet both significantly impact patient quality of life, satisfaction, and independence.
This systematic review therefore aims to fill this gap by synthesizing the evidence on clinical outcomes, which are essential indicators of prosthetic effectiveness. The outcomes considered include functional performance (gait, strength, ROM, dexterity, physiological changes, Electromyography (EMG)), patient-reported outcomes (satisfaction, comfort, pain, quality of life, ease of use), design and material integrity, usage patterns and implementation feasibility, fit, and the overall effectiveness of 3D-printed prostheses. By providing a comprehensive evaluation, this review contributes new knowledge on how 3D-printed prosthetic devices impact patient function, experience, and clinical applicability, highlighting both opportunities and limitations for future clinical adoption.
2. Materials and Methods
2.1. Study Team
To ensure clinically robust and meaningful findings, the study was conducted by an inter-professional team comprising experts in evidence synthesis, quantitative research methods, prosthetics and orthotics, occupational therapy, and rehabilitation medicine.
2.2. Search Strategy and Data Sources
A systematic search was completed in April 2025 in compliance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and the study protocol was registered in PROSPERO (no. CRD420250611965). Data collection was carried out using six electronic databases: PubMed, Web of Science, EBSCO, Scopus, Cochrane Library, and Sage. To maximize coverage, reference lists of the included studies were also manually screened, and supplementary searches were performed in Google Scholar to capture any additional relevant publications. According to the Patient, Intervention, Comparison/control, Outcomes (PICO) framework, we used the following keywords (customized for each database): “3D Printing”, “3D Printed”, “Additive Manufacturing”, “Three-Dimensional Printing”, “Prostheses”, “Prosthetic”, “Prosthesis”, “Upper Limb”, “Upper Extremity”, “Lower Limb”, “Lower Extremity”. No language filters were used for the search strategy. The keywords applied in the search strategy are presented in Table S1.
We included papers assessing the clinical outcomes of both upper and lower limb 3D-printed prostheses, written in English language. Case reports, meta-analyses, systematic reviews, meeting abstracts, posters, and thesis papers were excluded.
2.3. Study Selection and Eligibility Criteria
Following the removal of duplicates, the retrieved titles and abstracts were organized in an Excel sheet for screening. Study selection was conducted in two phases. In the first phase, titles and abstracts were independently reviewed for eligibility, with any differences in judgment resolved through discussion. Assistance with data collection and literature review was also provided during this stage. In the second phase, the full texts of potentially eligible studies were assessed against the inclusion criteria outlined in Table 1, and any disagreements were settled through independent arbitration to maintain consistency in the selection process.
2.4. Data Extraction, Synthesis and Analysis
The following data items were extracted: first author and year of publication, country/setting, study design, sample size and population characteristics (e.g., age, amputation level), type of intervention (prosthetic design, material, or fabrication approach), comparison groups (if applicable), outcome measures (functional performance, patient-reported outcomes, design/material integrity, and feasibility), results, and authors’ main conclusions. Studies were included only when clinical outcomes showed sufficient consistency, with particular emphasis placed on functional performance (gait, strength, range of motion (ROM), dexterity, physiological changes, and Electromyography (EMG)), patient-reported outcomes (satisfaction, comfort, pain, quality of life (QoL), and ease of use), design and material integrity, usage patterns and implementation feasibility, fit, and overall effectiveness of 3D-printed prostheses. Clinical outcomes were grouped by prosthetic type, including upper limb prostheses and lower limb prostheses. Data extraction and cross-checking procedures were performed independently, and discrepancies were resolved through discussion to ensure accuracy. Data interpretation, synthesis, and quality review were conducted collaboratively. Data management was carried out using Excel and Word.
2.5. Methodological Quality Assessment
The quality of the selected articles was evaluated using the modified Downs & Black Checklist [16]. This tool was selected for its established validity in assessing the methodological rigor of both randomized and non-randomized controlled trials and is widely recognized as a robust instrument for quality appraisal in systematic reviews. In cases where consensus was not initially achieved, a final decision was reached through further review. The checklist consists of 27 items divided into five categories: study quality, external validity, internal validity bias, confounding selection bias, and study power, with a maximum score of 28 points. Each checklist item was allocated a score of one, with the exception of item 27, which carried two points. Based on the total scores, studies were classified into quality categories using established thresholds: poor (<14), fair (15–19), good (20–25), and excellent (26–28).
3. Results
A PRISMA flowchart of the study identification process is presented in Figure 1. Of the 1420 potential records, 731 studies underwent title/abstract screening, 188 were reviewed in full, and 11 studies were ultimately included for appraisal. Across the studies included, 7 reported improvements in dexterity, 5 noted increased comfort and satisfaction, 3 described enhanced range of motion, and 4 highlighted durability issues such as component breakage. Two lower-limb studies reported improved swimming performance and higher comfort with digitally designed sockets.
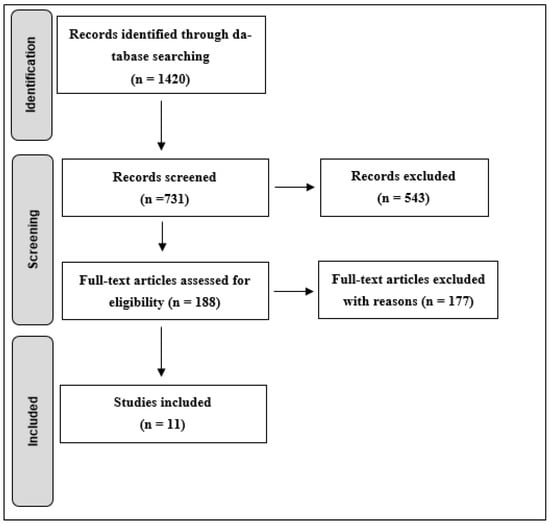
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.
The search resulted in 1 cross-sectional study, 3 prospective cohort studies, and 7 studies employing other designs (such as comparative, qualitative, prospective observational, general prospective, descriptive, pilot, and feasibility studies). Complete details of the study characteristics are summarized in Table S2. Studies represented data from 177 participants across several countries, including the USA, Nepal, India, Korea, and Canada. Upper limb studies primarily focused on body-powered and myoelectric prostheses (Table 1). Improvements in gross manual dexterity and daily functional use were frequently reported, although fine motor tasks and device durability remained common limitations [3,8,9,11,17,18,19,20,21]. Lower limb studies demonstrated benefits in comfort, socket fit, and amphibious use (Table 2), though evidence remains limited to feasibility and pilot studies [6,22] (Table S3).

Table 1.
3D-printed upper limb prostheses.
Table 1.
3D-printed upper limb prostheses.
| Author | Year | Aim | Methods | Results | Conclusion |
|---|---|---|---|---|---|
| Shrestha and Gautam [9] | 2023 | To explore the functionality of 3D-printed prosthetic hands with respect to performance, usability, and user satisfaction. |
|
| Participants were able to complete certain tasks using the 3D-printed prosthetic hands. |
| Belter et al. [8] | 2016 | To evaluate the effectiveness of a low-cost, 3D-printed body-powered prosthetic hand. |
|
| The multigrasp 3D-printed prosthetic hand demonstrated comparable performance to existing terminal devices among inexperienced users. However, participants with trans-radial amputations scored lower with the 3D-printed hand compared to the mechanical hook. The availability of multiple grasp types, despite experiencing challenges with grip regulation. Overall, the 3D-printed hand shows promise in enhancing prosthetic functionality. |
| Zuniga et al. [17] | 2016 | Identify the effects of using a wrist-driven 3D-printed prosthetic hand over six months in children with upper-limb deficiencies. |
|
| Despite limitations in durability, environmental impact, and regulatory standards, 3D-printed prosthetic hands—such as the Cyborg Beast—offer an affordable and practical solution to enhance mobility for individuals with upper-limb deficiencies, particularly in developing countries. |
| Zuniga et al. [11] | 2019 | To describe the remote fitting process for 3D-printed upper-limb prostheses and evaluate patient satisfaction and comfort. |
|
| The remote fitting method for 3D-printed upper-limb prostheses shows promise for rapidly delivering functional devices in developing countries, leveraging widespread access to digital technologies even in rural areas. |
| Zuniga et al. [18] | 2019 | Identify the functional and strength changes associated with the use of 3D-printed body-powered upper-limb prostheses |
|
| Use of a 3D-printed body-powered upper-limb prosthesis improves gross manual dexterity in children with upper-limb differences after several weeks of use. Despite some durability issues, the device remains a functional and practical body-powered option. |
| Bhat et al. [19] | 2021 | To assess the utility of 3D-printed upper-limb prostheses in children with congenital hand amputations, and to evaluate their functionality and cost-effectiveness. |
|
| 3D-printed upper-limb prostheses improve gross grasping in children with congenital hand amputations but lack fine motor functions such as lateral and tripod pinch. Despite these limitations, they are affordable, easily replaceable, and serve effectively as transitional devices for growing children. |
| Ku et al. [20] | 2019 | Evaluate the clinical impact of a low-cost, 3D-printed myoelectric prosthetic hand with a user interface on patients’ daily lives |
| After using the 3D-printed, single-channel myoelectric prosthesis for 3 months:
| The low-cost, 3D-printed prosthetic hand with a single-channel myoelectric interface shows potential to improve the quality of life of amputees through daily use. |
| Zuniga et al. [3] | 2015 | Describe a low-cost, 3D-printed prosthetic hand for children, and propose a remote fitting method to improve access to affordable prosthetic care |
|
| The low-cost, 3D-printed hand, combined with the proposed distance-fitting method, presents a promising and affordable prosthetic solution for underserved children. |
| Zuniga et al. [21] | 2018 | Assess using a wrist-driven, 3D-printed partial hand prosthesis for 6 months affects muscle coordination (co-activation index) in children with one-sided upper-limb reduction. |
|
| The wrist-driven, 3D-printed hand prosthesis significantly reduced the co-activation index in children with congenital upper-limb reduction deficiencies, potentially enhancing motor control strategies and improving outcomes in prosthetic rehabilitation. |

Table 2.
3D-printed lower limb prostheses.
Table 2.
3D-printed lower limb prostheses.
| Author | Year | Aim | Methods | Results | Conclusion |
|---|---|---|---|---|---|
| Goldstein et al. [6] | 2020 | Assess the usability and acceptance of a 3D-printed amphibious prosthesis and compare its performance to that of a standard Swim Ankle. |
|
| The novel 3D-printed amphibious lower-limb prosthesis was well-received and demonstrated good user-friendliness among a small group of participants in a recreational setting. These positive findings suggest potential benefits of the device for future use. |
| Eshraghi et al. [22] | 2024 | To explore the feasibility of a protocol for analyzing geometric and clinical differences between manually designed and digitally designed 3D-printed prosthetic sockets for individuals with trans-tibial amputations, with the aim of informing a future larger trial. |
|
| 3D scanning and digital design enhance socket production and patient engagement but face challenges such as limited tactile feedback, post-processing requirements, and variability among 3D printers. Overcoming regulatory and practical barriers, along with advances in materials and technology, will facilitate wider adoption in prosthetics and orthotics. |
The Modified Downs & Black checklist ratings of included studies are summarized in Table S4. One of the 11 studies included in this systematic review was classified as poor quality, 9 were classified as fair, and one was classified as Good. Given that the majority of studies were rated as fair quality, with only one study classified as good, findings should be interpreted cautiously. The limited methodological rigor reduces the strength and generalizability of the evidence.
4. Discussion
This review examines the clinical outcomes of 3D-printed prostheses, including both upper and lower limb designs, with a focus on functional performance (gait, strength, ROM, dexterity, physiological changes, EMG), patient-reported outcomes (satisfaction, comfort, pain, QoL, ease of use), design and material integrity, usage patterns, implementation feasibility, fit, and overall effectiveness. Across studies, 3D printing has demonstrated the potential to improve accessibility, personalization, and patient satisfaction, though limitations in device durability and fine-motor performance remain common.
Previous systematic reviews have addressed certain aspects of 3D-printed prostheses. Kim et al. [13] focused on the structural integrity of transtibial sockets, Diment et al. [14] examined upper-limb prostheses but highlighted a lack of randomized controlled trials, and Abbady et al. [15] reviewed applications in low- and lower–middle-income countries. However, none of these reviews comprehensively evaluated clinical outcomes across both upper and lower limb devices, nor did they integrate functional, patient-reported, and implementation-related outcomes. By synthesizing evidence from multiple prosthetic types, our review provides a broader understanding of real-world effectiveness and user experience.
4.1. 3D-Printed Upper Limb Prostheses
Across the reviewed literature, 3D-printed upper limb prostheses consistently improved gross grasp, manual dexterity, and user satisfaction. Limitations in fine-motor tasks and device durability were frequently reported, particularly for body-powered designs. Myoelectric devices showed promise in enhancing functional performance, though evidence remains limited [20]. Our review expands upon Diment et al.’s work [14] by including more recent studies, reporting additional patient-centered outcomes such as ease of use, comfort, daily usage, and neuromuscular adaptations [3,8,9,11,17,18,19,20,21]. Studies also indicate that remote fitting and digital sizing techniques, including photographic measurements, can improve accessibility and user comfort without compromising fit [3,11,17,18]. Overall, the pattern suggests that 3D-printed upper limb prostheses enhance gross motor function and engagement in daily activities, but durability and fine-motor precision remain barriers to widespread clinical adoption.
4.2. 3D-Printed Lower Limb Prostheses
3D-printed lower limb prostheses demonstrate clear advantages in comfort, fit, and specialized functionality, including amphibious designs for recreational use [6]. Digital socket workflows generally improved efficiency and user experience, though technical and regulatory barriers remain [22]. While Kim et al. [13] focused solely on socket integrity, our review evaluates clinical outcomes such as gait, comfort, satisfaction, and implementation feasibility, offering a more comprehensive assessment. Across studies, improvements in gait biomechanics, patient satisfaction, and device usability were consistently observed. This suggests that additive manufacturing can provide versatile solutions for lower limb prostheses, though broader clinical adoption will require continued refinement of digital design workflows and material durability.
Overall, while the findings of this review highlight the potential of 3D-printed prostheses, it is important to emphasize the limited quality and scope of the current evidence. Most available studies are small in scale, lack rigorous designs such as randomized controlled trials, and employ heterogeneous outcome measures. As such, caution is warranted when interpreting these results. At present, there is insufficient high-quality scientific evidence to support broad conclusions regarding the efficacy, accessibility, or equity of 3D-printed prostheses. Further well-designed clinical studies are required before these technologies can be considered established alternatives to conventional prosthetic manufacturing.
4.3. Study Limitation and Future Recommendation
This review has several limitations. Many included studies were case series with small sample sizes, limiting generalizability. Heterogeneity in assessment methods, including variable questionnaires for patient satisfaction, made comparisons across studies difficult. No studies were identified on 3D printing for other common prosthetic types, such as above-knee devices. Finally, only one study met criteria for high methodological quality. Future research should focus on standardized evaluation protocols, long-term durability, and broader applications across diverse prosthetic types to strengthen the evidence base and facilitate clinical adoption. By addressing these gaps, future studies can build on our findings and expand the practical clinical impact of 3D-printed prosthetic technologies.
5. Conclusions
The reviewed evidence suggests that 3D printing holds promise for the development of both upper and lower limb prostheses, particularly with respect to personalization, accessibility, patient satisfaction, and certain aspects of functional performance. However, the findings should be interpreted with caution, as most included studies were of limited methodological quality, small in scale, and heterogeneous in outcome measures, with only one study rated as “Good.” Current evidence does not yet provide sufficient scientific support to draw firm conclusions about the overall efficacy, accessibility, or equity of 3D-printed prostheses compared to conventional approaches. Future research should prioritize well-designed clinical trials with larger sample sizes, standardized outcome measures, and long-term follow-up to more rigorously evaluate both the benefits and limitations of 3D-printed prosthetic technologies and to guide their safe and effective integration into clinical practice.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jfb16100370/s1, Table S1: Database Search Strategy and Keywords; Table S2: Characteristics of included studies; Table S3: Clinical outcomes; Table S4: Bias Assessment Scores and Levels.
Author Contributions
Conceptualization, H.A. and R.N.; methodology, H.R.B. and T.Q.; software, R.N.; validation, D.V., E.D. and T.Q.; formal analysis, G.F.; investigation, H.A.; resources, B.M.; data curation, H.A. and T.Q.; writing—original draft preparation, T.Q., D.V., E.D. and R.N.; writing—review and editing, H.A., H.R.B., G.F. and B.M.; visualization, H.R.B. and G.F.; supervision, H.A. and B.M.; project administration, H.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
The authors would like to acknowledge the support of The University of Jordan, Princess Nourah bint Abdulrahman University, University of Insubria, and the University of Pécs.
Conflicts of Interest
Author Rabee Naeem was employed by the company Digital Fabrication Division, Revolutionary Technologies for Medical Solutions. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| ROM | Range of Motion |
| EMG | Electromyography |
| QoL | Quality of Life |
References
- Vujaklija, I.; Farina, D. 3D printed upper limb prosthetics. Expert Rev. Med. Devices 2018, 15, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Ten Kate, J.; Smit, G.; Breedveld, P. 3D-printed upper limb prostheses: A review. Disabil. Rehabil. Assist. Technol. 2017, 12, 300–314. [Google Scholar] [CrossRef] [PubMed]
- Zuniga, J.; Katsavelis, D.; Peck, J.; Stollberg, J.; Petrykowski, M.; Carson, A.; Fernandez, C. Cyborg beast: A low-cost 3d-printed prosthetic hand for children with upper-limb differences. BMC Res. Notes 2015, 8, 1–9. [Google Scholar] [CrossRef]
- Gao, W.; Zhang, Y.; Ramanujan, D.; Ramani, K.; Chen, Y.; Williams, C.B.; Wang, C.C.L.; Shin, Y.C.; Zhang, S.; Zavattieri, P.D. The status, challenges, and future of additive manufacturing in engineering. Comput. Aided Des. 2015, 69, 65–89. [Google Scholar] [CrossRef]
- Ngo, T.D.; Kashani, A.; Imbalzano, G.; Nguyen, K.T.; Hui, D. Additive manufacturing (3D printing): A review of materials, methods, applications and challenges. Compos. Part. B Eng. 2018, 143, 172–196. [Google Scholar] [CrossRef]
- Goldstein, T.; Oreste, A.; Hutnick, G.; Chory, A.; Chehata, V.; Seldin, J.; Gallo, M.D.; Bloom, O. A pilot study testing a novel 3D printed amphibious lower limb prosthesis in a recreational pool setting. PMR 2020, 12, 783–793. [Google Scholar] [CrossRef]
- Abdelaal, O.; Darwish, S.; Abd Elmougoud, K.; Aldahash, S. A new methodology for design and manufacturing of a customized silicone partial foot prosthesis using indirect additive manufacturing. Int. J. Artif. Organs 2019, 42, 645–657. [Google Scholar] [CrossRef]
- Belter, J.T.; Leddy, M.T.; Gemmell, K.D.; Dollar, A.M. (Eds.) Comparative clinical evaluation of the Yale Multigrasp Hand. In Proceedings of the 2016 6th IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob), Singapore, 26–29 June 2016; IEEE: New York, NY, USA, 2016. [Google Scholar]
- Shrestha, S.; Gautam, S. Outcome of Three Dimensional Printed Functional Prostheses for Children with Upper Limb Deficiency in Nepal. Kathmandu Univ. Med. J. 2023, 81, 52–57. [Google Scholar] [CrossRef]
- Barrios-Muriel, J.; Romero-Sánchez, F.; Alonso-Sánchez, F.J.; Salgado, D.R. Advances in orthotic and prosthetic manufacturing: A technology review. Materials 2020, 13, 295. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Young, K.J.; Peck, J.L.; Srivastava, R.; Pierce, J.E.; Dudley, D.R.; Salazar, D.A.; Bergmann, J. Remote fitting procedures for upper limb 3d printed prostheses. Expert Rev. Med. Devices 2019, 16, 257–266. [Google Scholar] [CrossRef]
- Sterkenburg, A.; Van der Stelt, M.; Koroma, A.R.; Van Gaalen, M.; Van der Pols, M.; Grobusch, M.P.; Slump, C.; Maal, T.; Brouwers, L. Quality of life of patients with 3D-printed arm prostheses in a rural area of Sierra Leone. Heliyon 2021, 7, e07447. [Google Scholar] [CrossRef]
- Kim, S.; Yalla, S.; Shetty, S.; Rosenblatt, N.J. 3D printed transtibial prosthetic sockets: A systematic review. PLoS ONE 2022, 17, e0275161. [Google Scholar] [CrossRef]
- Diment, L.E.; Thompson, M.S.; Bergmann, J.H. Three-dimensional printed upper-limb prostheses lack randomised controlled trials: A systematic review. Prosthet. Orthot. Int. 2018, 42, 7–13. [Google Scholar] [CrossRef]
- Abbady, H.E.; Klinkenberg, E.T.; de Moel, L.; Nicolai, N.; van der Stelt, M.; Verhulst, A.C.; Maal, T.J.; Brouwers, L. 3D-printed prostheses in developing countries: A systematic review. Prosthet. Orthot. Int. 2022, 46, 19–30. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Peck, J.; Srivastava, R.; Katsavelis, D.; Carson, A. An open source 3D-printed transitional hand prosthesis for children. JPO J. Prosthet. Orthot. 2016, 28, 103–108. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Peck, J.L.; Srivastava, R.; Pierce, J.E.; Dudley, D.R.; Than, N.A.; Stergiou, N. Functional changes through the usage of 3D-printed transitional prostheses in children. Disabil. Rehabil. Assist. Technol. 2019, 14, 68–74. [Google Scholar] [CrossRef]
- Bhat, A.K.; Acharya, A.M. Functional assessment of 3D printed prosthesis in children with congenital hand differences-a prospective observational study. J. Hand Surg. (Asian-Pac. Vol.) 2021, 26, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Ku, I.; Lee, G.K.; Park, C.Y.; Lee, J.; Jeong, E. Clinical outcomes of a low-cost single-channel myoelectric-interface three-dimensional hand prosthesis. Arch. Plast. Surg. 2019, 46, 303–310. [Google Scholar] [PubMed]
- Zuniga, J.M.; Dimitrios, K.; Peck, J.L.; Srivastava, R.; Pierce, J.E.; Dudley, D.R.; Salazar, D.A.; Young, K.J.; Knarr, B.A. Coactivation index of children with congenital upper limb reduction deficiencies before and after using a wrist-driven 3D printed partial hand prosthesis. J. Neuroeng. Rehabil. 2018, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Eshraghi, A.; Phillips, C.; MacKay, C.; Dilkas, S.; Riondato, Z.; Lehkyj, S.; Heim, W. Comparison of Socket Geometry, Socket Comfort, and Patient Experience between Manually-and Digitally-Designed Prosthetic Sockets for Lower-Limb Amputees: A Feasibility Study. Prosthesis 2024, 6, 672–682. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).