Mechanical Behavior of Five Different Morse Taper Implants and Abutments with Different Conical Internal Connections and Angles: An In Vitro Experimental Study
Abstract
1. Introduction
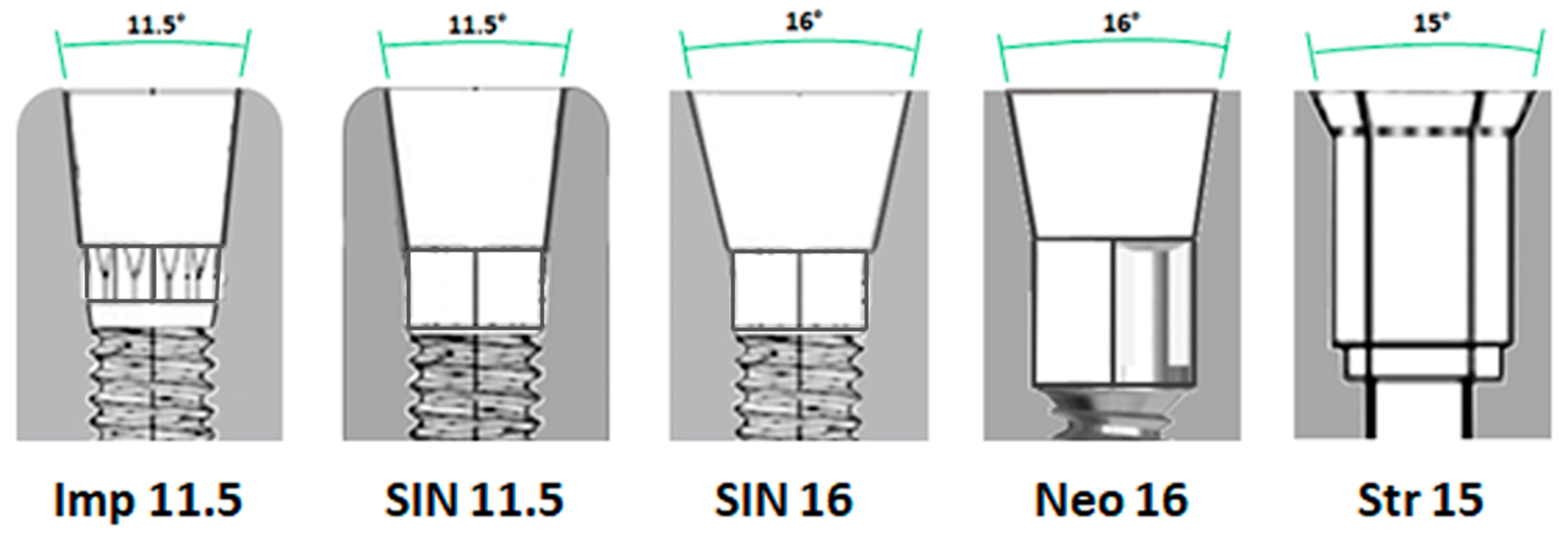
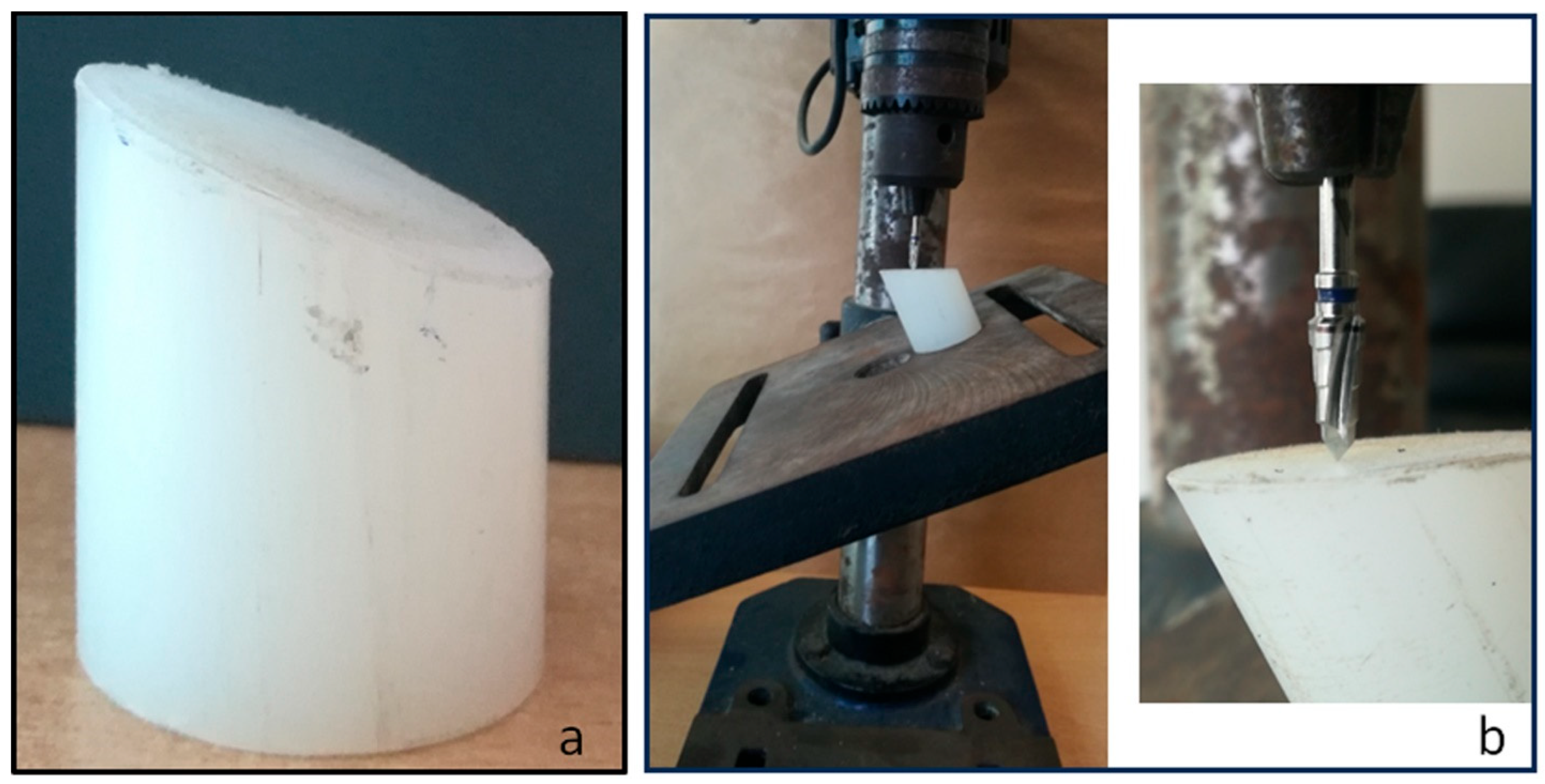
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sartoretto, S.C.; Shibli, J.A.; Javid, K.; Cotrim, K.; Canabarro, A.; Louro, R.S.; Lowenstein, A.; Mourão, C.F.; Moraschini, V. Comparing the Long-Term Success Rates of Tooth Preservation and Dental Implants: A Critical Review. J. Funct. Biomater. 2023, 14, 142. [Google Scholar] [CrossRef]
- Elani, H.W.; Starr, J.R.; Da Silva, J.D.; Gallucci, G.O. Trends in Dental Implant Use in the U.S., 1999–2016, and Projections to 2026. J. Dent. Res. 2018, 97, 1424–1430. [Google Scholar] [CrossRef]
- Staedt, H.; Rossa, M.; Lehmann, K.M.; Al-Nawas, B.; Kämmerer, P.W.; Heimes, D. Potential risk factors for early and late dental implant failure: A retrospective clinical study on 9080 implants. Int. J. Implant. Dent. 2020, 6, 81. [Google Scholar] [CrossRef]
- Kochar, S.P.; Reche, A.; Paul, P. The Etiology and Management of Dental Implant Failure: A Review. Cureus 2022, 14, e30455. [Google Scholar] [CrossRef]
- Sadowsky, S.J. Occlusal overload with dental implants: A review. Int. J. Implant. Dent. 2019, 5, 29. [Google Scholar] [CrossRef]
- Albrektsson, T.; Tengvall, P.; Amengual-Peñafiel, L.; Coli, P.; Kotsakis, G.; Cochran, D.L. Implications of considering peri-implant bone loss a disease, a narrative review. Clin. Implant Dent. Relat. Res. 2022, 24, 532–543. [Google Scholar] [CrossRef]
- Hanif, A.; Qureshi, S.; Sheikh, Z.; Rashid, H. Complications in implant dentistry. Eur. J. Dent. 2017, 11, 135–140. [Google Scholar] [CrossRef]
- Gupta, S.; Gupta, H.; Tandan, A. Technical complications of implant-causes and management: A comprehensive review. Natl. J. Maxillofac. Surg. 2015, 6, 3–8. [Google Scholar] [CrossRef]
- Cervino, G.; Germanà, A.; Fiorillo, L.; D’amico, C.; Abbate, F.; Cicciù, M. Passant Connection Screw of Dental Implants: An In Vitro SEM Preliminary Study. BioMed Res. Int. 2022, 2022, 9720488. [Google Scholar] [CrossRef]
- Mattheos, N.; Li, X.; Zampelis, A.; Ma, L.; Janda, M. Investigating the micromorphological differences of the implant–abutment junction and their clinical implications: A pilot study. Clin. Oral Implant. Res. 2015, 27, e134–e143. [Google Scholar] [CrossRef]
- Jorge, J.R.; Barao, V.A.; Delben, J.A.; Assuncao, W.G. The role of implant/abutment system on torque maintenance of retention screws and vertical misfit of implant-supported crowns before and after mechanical cycling. Int. J. Oral Maxillofac. Implant. 2013, 28, 415–422. [Google Scholar] [CrossRef]
- Jo, J.-Y.; Yang, D.-S.; Huh, J.-B.; Heo, J.-C.; Yun, M.-J.; Jeong, C.-M. Influence of abutment materials on the implant-abutment joint stability in internal conical connection type implant systems. J. Adv. Prosthodont. 2014, 6, 491–497. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, J. Mechanism of and factors associated with the loosening of the implant abutment screw: A review. J. Esthet. Restor. Dent. 2019, 31, 338–345. [Google Scholar] [CrossRef]
- Klongbunjit, D.; Aunmeungtong, W.; Khongkhunthian, P. Implant-abutment screw removal torque values between customized titanium abutment, straight titanium abutment, and hybrid zirconia abutment after a million cyclic loading: An in vitro comparative study. Int. J. Implant. Dent. 2021, 7, 98. [Google Scholar] [CrossRef]
- Gehrke, S.; Delgado-Ruiz, R.; Frutos, J.; Prados-Privado, M.; Dedavid, B.; Marín, J.; Guirado, J. Misfit of Three Different Implant-Abutment Connections Before and After Cyclic Load Application: An In Vitro Study. Int. J. Oral Maxillofac. Implant. 2017, 32, 822–829. [Google Scholar] [CrossRef]
- Schmitt, C.M.; Nogueira-Filho, G.; Tenenbaum, H.C.; Lai, J.Y.; Brito, C.; Doering, H.; Nonhoff, J. Performance of conical abutment (Morse Taper) connection implants: A systematic review. J. Biomed. Mater. Res. A 2014, 102, 552–574. [Google Scholar] [CrossRef]
- Goyeneche, V.P.; Cortellari, G.C.; Rodriguez, F.; De Aza, P.N.; da Costa, E.M.; Scarano, A.; Júnior, N.D.B.; Gehrke, S.A. Does the index in Morse taper connection affect the abutment stability? An in vitro experimental study. PLoS ONE 2024, 19, e0298462. [Google Scholar] [CrossRef]
- Delben, J.A.; Barão, V.A.; Ferreira, M.B.; da Silva, N.R.; Thompson, V.P.; Assunção, W.G. Influence of abutment-to-fixture design on reliability and failure mode of all-ceramic crown systems. Dent. Mater. 2014, 30, 408–416. [Google Scholar] [CrossRef]
- Steinebrunner, L.; Wolfart, S.; Ludwig, K.; Kern, M. Implant–abutment interface design affects fatigue and fracture strength of implants. Clin. Oral Implant. Res. 2008, 19, 1276–1284. [Google Scholar] [CrossRef]
- Raoofi, S.; Khademi, M.; Amid, R.; Kadkhodazadeh, M.; Movahhedi, M.R. Comparison of the Effect of Three Abutment-implant Connections on Stress Distribution at the Internal Surface of Dental Implants: A Finite Element Analysis. J. Dent. Res. Dent. Clin. Dent. Prospect. 2013, 7, 132–139. [Google Scholar] [CrossRef]
- Gehrke, S.; Pereira, F. Changes in the abutment-implant interface in morse taper implant connections after mechanical cycling: A pilot study. Int. J. Oral Maxillofac. Implant. 2014, 29, 791–797. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Serra, R.D.C. Load fatigue performance of conical implant-abutment connection: Effect of torque level and interface junction. Minerva Stomatol. 2015, 64, 1–7. [Google Scholar]
- Nie, H.; Tang, Y.; Yang, Y.; Wu, W.; Zhou, W.; Liu, Z. Influence of a new abutment design concept on the biomechanics of peri-implant bone, implant components, and microgap formation: A finite element analysis. BMC Oral Health 2023, 23, 277. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Dedavid, B.A.; Marín, J.M.G.; Canullo, L. Behavior of implant and abutment sets of three different connections during the non-axial load application: An in vitro experimental study using a radiographic method. Bio-Medical Mater. Eng. 2022, 33, 101–112. [Google Scholar] [CrossRef]
- ISO 14801:2007; Dentistry—Implants—Dynamic Fatigue Test for Endosseous Dental Implants. The International Organization for Standardization: Geneva, Switzerland, 2015.
- Oskarsson, M.; Otsuki, M.; Welander, M.; Abrahamsson, I. Peri-implant tissue healing at implants with different designs and placement protocols: An experimental study in dogs. Clin. Oral Implant. Res. 2018, 29, 873–880. [Google Scholar] [CrossRef]
- Stiesch, M.; Pott, P.-C.; Eisenburger, M. Implantat-Abutment-Verbund. Zahnmed. up2date 2011, 5, 445–464. [Google Scholar] [CrossRef]
- Guarnieri, R.; Miccoli, G.; Reda, R.; Mazzoni, A.; Di Nardo, D.; Testarelli, L. Laser microgrooved vs. machined healing abutment disconnection/reconnection: A comparative clinical, radiographical and biochemical study with split-mouth design. Int. J. Implant. Dent. 2021, 7, 19. [Google Scholar] [CrossRef]
- Cozzolino, F.; Apicella, D.; Wang, G.; Apicella, A.; Sorrentino, R. Implant-to-bone force transmission: A pilot study for in vivo strain gauge measurement technique. J. Mech. Behav. Biomed. Mater. 2018, 90, 173–181. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Zarauz, C.; Strasding, M.; Sailer, I.; Zwahlen, M.; Zembic, A. A systematic review of the influence of the implant-abutment connection on the clinical outcomes of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin. Oral Implant. Res. 2018, 29, 160–183. [Google Scholar] [CrossRef]
- Hotinski, E.; Dudley, J. Abutment screw loosening in angulation-correcting implants: An in vitro study. J. Prosthet. Dent. 2019, 121, 151–155. [Google Scholar] [CrossRef]
- Assunção, W.G.; Barão, V.A.R.; Delben, J.A.; Gomes, A.; Garcia, I.R. Effect of unilateral misfit on preload of retention screws of implant-supported prostheses submitted to mechanical cycling. J. Prosthodont. Res. 2011, 55, 12–18. [Google Scholar] [CrossRef]
- Breeding, L.C.; Dixon, D.L.; Nelson, E.W.; Tietge, J.D. Torque required to loosen single-tooth implant abutment screws before and after simulated function. Int. J. Prosthodont. 1993, 6, 435–439. [Google Scholar]
- Coppedê, A.R.; De Mattos, M.D.G.C.; Rodrigues, R.C.S.; Ribeiro, R.F. Effect of repeated torque/mechanical loading cycles on two different abutment types in implants with internal tapered connections: An in vitro study. Clin. Oral Implant. Res. 2009, 20, 624–632. [Google Scholar] [CrossRef]
- Nissan, J.; Ghelfan, O.; Gross, O.; Priel, I.; Gross, M.; Chaushu, G. The Effect of Crown/Implant Ratio and Crown Height Space on Stress Distribution in Unsplinted Implant Supporting Restorations. J. Oral Maxillofac. Surg. 2011, 69, 1934–1939. [Google Scholar] [CrossRef]
- Piermatti, J.; Yousef, H.; Luke, A.; Mahevich, R.; Weiner, S. An In Vitro analysis of implant screw torque loss with external hex and internal connection implant systems. Implant. Dent. 2006, 15, 427–435. [Google Scholar] [CrossRef]
- El-Sheikh, M.A.Y.; Mostafa, T.M.N.; El-Sheikh, M.M. Effect of different angulations and collar lengths of conical hybrid implant abutment on screw loosening after dynamic cyclic loading. Int. J. Implant. Dent. 2018, 4, 39. [Google Scholar] [CrossRef]
- Zeno, H.A.; Buitrago, R.L.; Sternberger, S.S.; Patt, M.E.; Tovar, N.; Coelho, P.; Kurtz, K.S.; Tuminelli, F.J. The effect of tissue entrapment on screw loosening at the implant/abutment interface of external- and internal-connection implants: An In Vitro study. J. Prosthodont. 2015, 25, 216–223. [Google Scholar] [CrossRef]
- Diez, J.S.V.; Brigagão, V.C.; Cunha, L.G.; Neves, A.C.C.; Concilio, L.S. Influence of diamondlike carbon-coated screws on the implant-abutment interface. Int. J. Oral Maxillofac. Implant. 2012, 27, 1055–1060. [Google Scholar]
- Lee, J.-H.; Cha, H.-S. Screw loosening and changes in removal torque relative to abutment screw length in a dental implant with external abutment connection after oblique cyclic loading. J. Adv. Prosthodont. 2018, 10, 415–421. [Google Scholar] [CrossRef]
- Cho, W.-R.; Huh, Y.-H.; Park, C.-J.; Cho, L.-R. Effect of cyclic loading and retightening on reverse torque value in external and internal implants. J. Adv. Prosthodont. 2015, 7, 288–293. [Google Scholar] [CrossRef]
- Bagegni, A.; Weihrauch, V.; Vach, K.; Kohal, R. The Mechanical Behavior of a Screwless Morse Taper Implant–Abutment Connection: An In Vitro Study. Materials 2022, 15, 3381. [Google Scholar] [CrossRef] [PubMed]
- Ugurel, C.S.; Steiner, M.; Isik-Ozkol, G.; Kutay, O.; Kern, M. Mechanical resistance of screwless morse taper and screw-retained implant-abutment connections. Clin. Oral Implant. Res. 2013, 26, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Ebadian, B.; Fathi, A.; Khodadad, S. Comparison of the effect of four different abutment screw torques on screw loosening in single implant-supported prosthesis after the application of mechanical loading. Int. J. Dent. 2021, 2021, 3595064. [Google Scholar] [CrossRef]


| Without Load | With Load | ||||
|---|---|---|---|---|---|
| Groups | RT | DT | Perc. diff. | DT | Perc. diff. |
| G1 | 20 Ncm | 14.9 ± 1.44 Ncm | −25.7% | 11.2 ± 1.44 Ncm | −44.0% |
| G2 | 10 Ncm | 7.0 ± 0.87 Ncm | −30.4% | 5.7 ± 0.81 Ncm | −43.5% |
| G3 | 20 Ncm | 12.7 ± 1.28 Ncm | −36.8% | 10.3 ± 1.15 Ncm | −48.5% |
| G4 | 20 Ncm | 14.1 ± 1.32 Ncm | −29.6% | 10.6 ± 1.08 Ncm | −47.2% |
| G5 | 35 Ncm | 25.9 ± 1.42 Ncm | −25.7% | 17.6 ± 1.49 Ncm | −49.8% |
| Groups | Without Load TSv | With Load TSv |
|---|---|---|
| G1 | 56.3 ± 2.21 N | 63.5 ± 3.06 N |
| G2 | 30.7 ± 2.00 N | 34.2 ± 2.45 N |
| G3 | 0 N | 0 N |
| G4 | 0 N | 0 N |
| G5 | 26.0 ± 2.52 N | 23.1 ± 1.29 N |
| Without Load | With Load | |||||
|---|---|---|---|---|---|---|
| Comparisons | Mean Diff. | p-Value | 95% CI of diff | Mean Diff. | p-Value | 95% CI of diff |
| G1 vs. G2 | 25.56 | <0.0001 | 22.98 to 28.14 | 29.32 | 0.0002 | 26.60 to 32.04 |
| G1 vs. G5 | 30.28 | <0.0001 | 27.70 to 32.86 | 40.42 | 0.0002 | 37.70 to 43.14 |
| G2 vs. G5 | 4.720 | 0.0009 | 2.144 to 7.296 | 11.10 | 0.0002 | 8.382 to 13.82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caballero, C.; Rodriguez, F.; Cortellari, G.C.; Scarano, A.; Prados-Frutos, J.C.; De Aza, P.N.; Fernandes, G.V.O.; Gehrke, S.A. Mechanical Behavior of Five Different Morse Taper Implants and Abutments with Different Conical Internal Connections and Angles: An In Vitro Experimental Study. J. Funct. Biomater. 2024, 15, 177. https://doi.org/10.3390/jfb15070177
Caballero C, Rodriguez F, Cortellari GC, Scarano A, Prados-Frutos JC, De Aza PN, Fernandes GVO, Gehrke SA. Mechanical Behavior of Five Different Morse Taper Implants and Abutments with Different Conical Internal Connections and Angles: An In Vitro Experimental Study. Journal of Functional Biomaterials. 2024; 15(7):177. https://doi.org/10.3390/jfb15070177
Chicago/Turabian StyleCaballero, Claudia, Fernando Rodriguez, Guillermo Castro Cortellari, Antonio Scarano, Juan Carlos Prados-Frutos, Piedad N. De Aza, Gustavo Vicentis Oliveira Fernandes, and Sergio Alexandre Gehrke. 2024. "Mechanical Behavior of Five Different Morse Taper Implants and Abutments with Different Conical Internal Connections and Angles: An In Vitro Experimental Study" Journal of Functional Biomaterials 15, no. 7: 177. https://doi.org/10.3390/jfb15070177
APA StyleCaballero, C., Rodriguez, F., Cortellari, G. C., Scarano, A., Prados-Frutos, J. C., De Aza, P. N., Fernandes, G. V. O., & Gehrke, S. A. (2024). Mechanical Behavior of Five Different Morse Taper Implants and Abutments with Different Conical Internal Connections and Angles: An In Vitro Experimental Study. Journal of Functional Biomaterials, 15(7), 177. https://doi.org/10.3390/jfb15070177











