Abstract
Among scaffolds used in tissue engineering, natural biomaterials such as plant-based materials show a crucial role in cellular function due to their biocompatibility and chemical indicators. Because of environmentally friendly behavior and safety, green methods are so important in designing scaffolds. A key bioactive flavonoid of the Epimedium plant, Icariin (ICRN), has a broad range of applications in improving scaffolds as a constant and non-immunogenic material, and in stimulating the cell growth, differentiation of chondrocytes as well as differentiation of embryonic stem cells towards cardiomyocytes. Moreover, fusion of ICRN into the hydrogel scaffolds or chemical crosslinking can enhance the secretion of the collagen matrix and proteoglycan in bone and cartilage tissue engineering. To scrutinize, in various types of cancer cells, ICRN plays a decisive role through increasing cytochrome c secretion, Bax/Bcl2 ratio, poly (ADP-ribose) polymerase as well as caspase stimulations. Surprisingly, ICRN can induce apoptosis, reduce viability and inhibit proliferation of cancer cells, and repress tumorigenesis as well as metastasis. Moreover, cancer cells no longer grow by halting the cell cycle at two checkpoints, G0/G1 and G2/M, through the inhibition of NF-κB by ICRN. Besides, improving nephrotoxicity occurring due to cisplatin and inhibiting multidrug resistance are the other applications of this biomaterial.
Keywords:
Icariin (ICRN); natural product; cancer therapy; tissue engineering; cell cycle; apoptosis 1. Introduction
Nowadays, an international movement has engaged targeting the development of natural products for biomedical uses in order to decrease or remove the side effects of non-biological materials [1,2]. A wide-range of naturally occurring materials derived from plants has been tested for their applications in cell toxicity and medicine [3,4,5]. The application of natural materials has been documented in the earliest cultures such as China and Iran, where they relied on plant-derived compounds for health and medical aims and healing purposes [6]. The employment of biomolecules for use in various industries has become an effectual manner in several applications comprising, biocompatible polymers, nano-structural materials, drug delivery, foods and the pharmacological industries [7,8,9].
The growing subject of tissue engineering is very multifaceted and links specialists from varied arenas of materials engineering, mechanical, medicine, and other subjects of bio-sciences [10]. A number of scaffolds prepared by diverse materials have been employed in tissue engineering [9]. Without considering the kind of tissue, several key features such as biocompatibility, mechanical belongings, and used methodology of synthesis are important in scaffold designing [11,12]. Normally, classified groups of materials, such as ceramics and polymers are employed in scaffolds research. Natural biopolymers for instance plant-based materials can show a chief role in cell behavior formation, mostly in regard to chemical indicators and bio-compatibility [13,14,15,16]. However, some factors for example poor mechanical properties and fast biodegradability reduce their efficacy. However, these weaknesses could be bypassed using a crosslinking technique with suitable cross linkers or by a combination of natural polymers. Plants and plant-derived materials are regularly explored for various biomedical uses [17,18,19,20]. Green methods are of special importance in the design of scaffolds due to their high safety and environmental friendliness [21,22]. The uses of nontoxic production technologies and the usage of natural resources can stop pollution and really decrease the uses of unsafe things for the assembly of scaffolds [23,24]. Tissue engineering includes a set of biologically active molecules, engineering and biochemical processes, and the production of materials to make, modify, or treat damaged tissues [25,26,27,28].
ICRN is a kind of flavonoid considered as the key bioactive of the Epimedium herb, which has long been utilized in common Chinese medical research. In primary works, the studies on ICRN were generally focused on increasing anti-aging and reproductive activities [29,30]. In current years, with the deepening of medical investigations, positive development on bio-properties of ICRN has been made in immune, cancer, and protective systems [31,32]. So far, various effects of ICRN were proven in osteoporotic bone regeneration [33], attenuates pulmonary fibrosis [34], improvement in chronic kidney issues [35], and many more. Given the beneficial properties of Epimedium, this plant has been included into Chinese pharmacopeia [36,37]. Therefore, in this review, the most important biomedical and biomaterials activities of ICRN are taken in to consideration. The following search strategy was conducted. Several relevant literature databases (PubMed, Scopus and Web of Science) were searched. The relevant works were selected using the following keywords in various combinations: Icariin, cell cycle, cancer, apoptosis, and angiogenesis.
2. Botanical Origins and Distribution
The genus Epimedium L. from Berberidaceae with chief remedial species, comprises a total of 71 species universally [38]. Various species of Epimedium have long been recruited in Chinese medication. Among them, the most popular and commercially important are Epimedium koreanum Nakai, Epimedium pubescens Maxim., Epimedium brevicornu Maxim., Epimedium sagittatum (Siebold & Zucc.) Maxim. and Epimedium wushanense T.S.Ying which is distributed broadly from Japan to Algeria [39,40]. Epimedium taxa grows mostly on cliffs under high humidity, and wet lands at height above sea level ranging from 200–3700 m [39]. Epimedium is a slow-growing herb with leathery leaves and its stems extend beneath the ground. The leaves are different, lengthy-petiolate, ternately divided twice. The pendant-shaped flowers have lengthy spurs and show a discrepancy in color with colorful flowers including four sepals and four petaloides. It has been shown that a lot of species of this plant (Figure 1) have aphrodisiac assets.

Figure 1.
Various species of Epimedium.
3. Traditional Applications and Ethnopharmacology of Epimedium Species
Several species of Epimedium was used in traditional Asian medicine. In China and Japan, Epimedium sagittatum (Sieb. & Zucc.) Maxim. and Epimedium grandiflorum have been used to treat impotence, prospermia, hyperdiuresis, osteoporosis, menopause syndrome, rheumatic arthritis, hypertension, and chronic tracheitis [41]. In Korea, Sam-ji-goo-yeop-cho, the herb Epimedium koreanum, was traditionally used for impotence, spermatorrhoea and forgetfulness. Now, the major five Epimedium species, Epimedium brevicornum Maxim, Epimedium sagittatum (Sieb. and Zucc.) Maxim., Epimedium pubescens Maxim. Epimedium wushanense T.S. Ying and Epimedium koreanum Nakai are designated as the official sources of Herba Epimedii in the Chinese Pharmacopoeia (The State Committee of Pharmacopeia, 2005) [42]. Herba Epimedii has a long history as a medicinal plant to treat a wide range of complaints. As far as we know, the earliest record was in Shen Nong Materia Medica which was written in the Eastern Han Dynasty. In this famous medical classic, it was stated that the root and leaves can all be used for treatment, but the details are not very clear. Annotation of Materia Medica is one of the pharmacopoeias published by the government of the Tang Dyansty, but the record is also very simple. The characteristics of Herba Epimedii were exactly stated in the Compendium of Materia Medica that was completed by Li Shi-Zhen in the Ming Dyansty. It was stated that Herba Epimedii can strengthen bones and muscles, tonify pneuma, reinforce the liver and kidney, enhance psychic energy. The PRC codex also records that Herba Epimedii has all these effects and can be used for therapy for some related diseases. Modern pharmacological research displayed that Herba Epimedii and its extracts have many kinds of bioactivities that include stimulation of osteoblastogenesis and suppression of the activity of osteoclasts. It inhibits the invasion and migration of cancer cells, improves sexual function, enhances memory, increases the activity of phytoestrogens, promotes the immunological ability and has antiinflammatory properties. So Herba Epimedii is always used for the treatment of osteoporosis, tumors, erectile dysfunction, Alzheimer disease and menopausal syndrome in clinical practice [43].
4. Physicochemical Properties
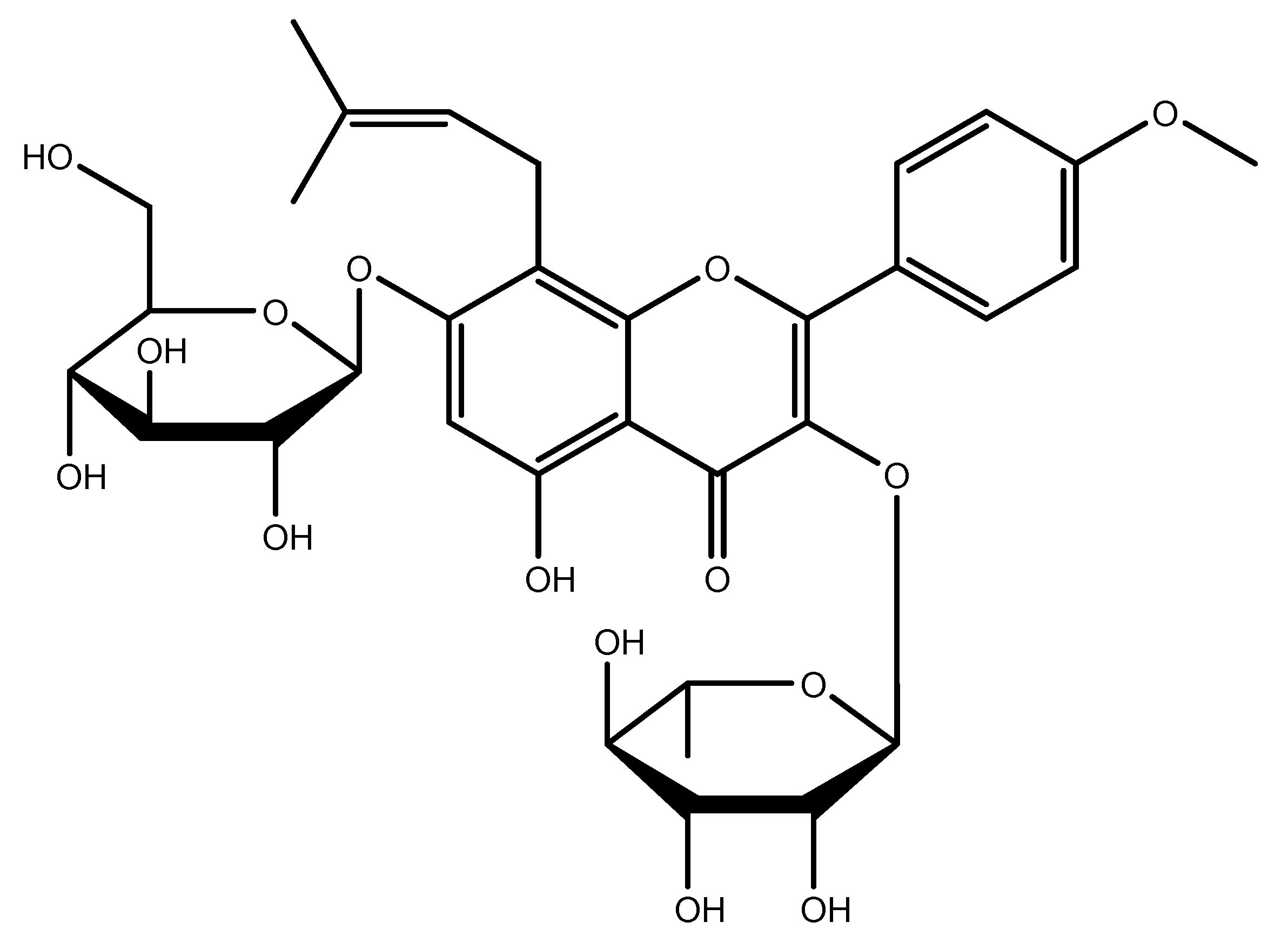
ICRN (C33H40O15, Mw = 676.67) is a type of prenylated flavonoid, showing extensive bioactivities such as antioxidant [44,45,46,47], neuroprotective [48,49,50,51,52], and antitumor [53,54,55,56,57,58,59,60,61] behavior as well as anti-inflammatory responses [62,63,64,65,66,67,68], and can be used to treat erectile dysfunction [69,70,71,72]. It appears it can improve the function of organs including bones and the heart [73,74,75,76,77,78,79,80,81,82,83,84,85,86]. It is crystalline and stable at a low temperature (−20 °C) for approximately two years [87,88,89,90]. The chemical structure is depicted in Figure 2. The stock solutions of ICRN were usually made in DMF or DMSO (20 mg/mL). The solubility of ICRN in organic solvent increases as the temperature increases. To prevent degradation, purging inert gases could be useful. Due to low solubility and stability considerations in water, freshly prepared solutions in the buffer can be used. Usually, a stock solution in DMSO was diluted to increase the solubility in a buffer (the ratio of DMSO to PBS can be 1:10 at pH 7.2) a [87,88,90].
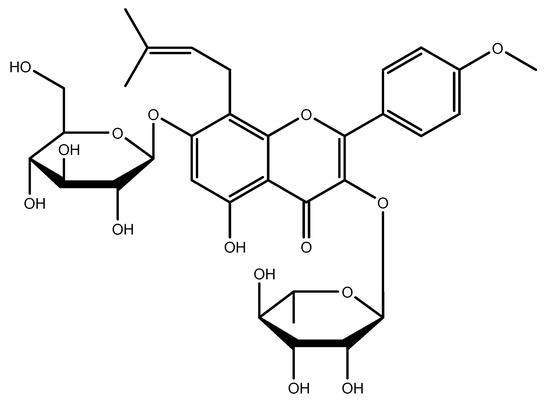
Figure 2.
Chemical structure of ICRN.
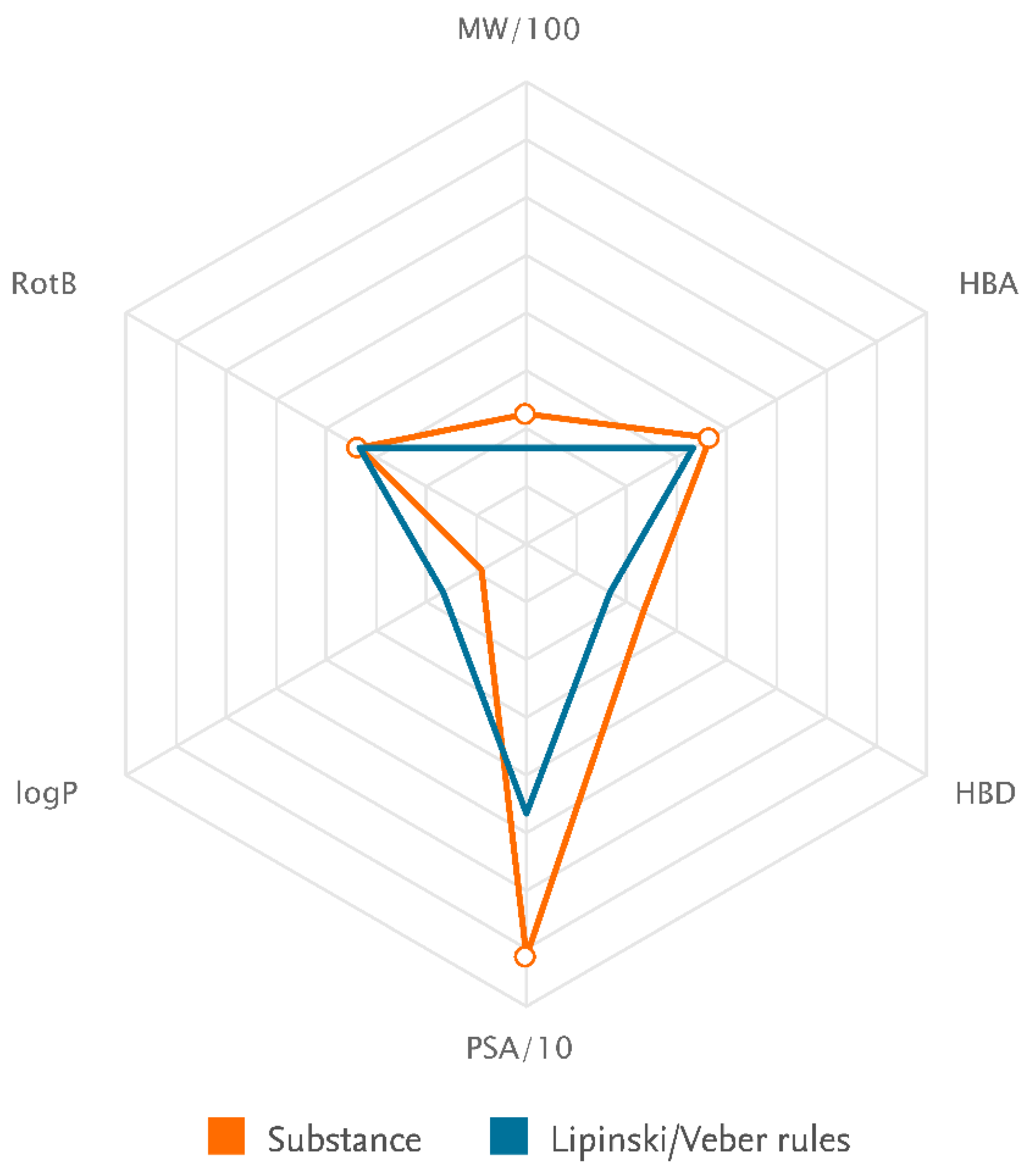
ICRN is a light yellow-to-yellow powder. It is a flammable solid with a predicted flash point of 300.9 °C and a predicted boiling point of 948.5 °C (at 760 mmHg). It can be stored at temperature. It is partly miscible with water and soluble in pyridine. In a DMSO: PBS (PH = 7.2) ratio of 1:10, the solubility is approximately 0.1 mg/mL. The solubility in DMSO, DMF, and ethanol is 50 mg/mL, ≈20 mg/mL, and <1 mg/mL at 25 °C. In solution, it has no turbidity and the color could be in clear from colorless to dark yellow (Sigma-Aldrich and Santa Cruz safety data sheets). The IUPAC name is 2-(4-methoxyphenyl)-8-(3-methylbut-2-enyl)-7-[(2S,3R,4S,5S,6R)-3,4,5-trihydroxy-6-(hydroxymethyl)oxan-2-yl]oxy-3-[[(2S,3R,4R,5R,6S)-3,4,5-trihydroxy-6-methyloxan-2-yl]methoxy]chromen-4-one, which was computed by LexiChem 2.6.6. To the best of our knowledge, the chemical, physical, and toxicological properties have not been thoroughly explored. The known calculated data for the drug likeness of icariin were shown by Lipinski, the rules and Veber rules components, which revealed only one matched criterion in both cases (Table 1, Figure 3). According to the rules of Lipinski, the hydrogen bond donor (HBD), hydrogen bond acceptors (HBA) and octanol-water partition coefficient (log P) should be less than or equal to 5, 10, and 5, respectively. The molecular weight must be less the 500 [91]. Therefore, logP is only acceptable according to the Lipinski rules component. According to Veber’s rule, bioavailability is acceptable only when less than ten rotatable bonds (RB) exist in the molecular structure and the polar surface area (PSA) was less than 140 [92]. Icariin can be metabolized into nearly 10 constituents. The icaritin and icariside II are the metabolized forms of icariin in the small intestine, showing lipid-lowering and lipid-regulating effects. Icariside II can be absorbed in the bloodstream [93]. In many physiological complex systems, icariin could also improve bioactivity and biocompatibility [94,95,96].

Table 1.
Identification and drug likeness of icariin.
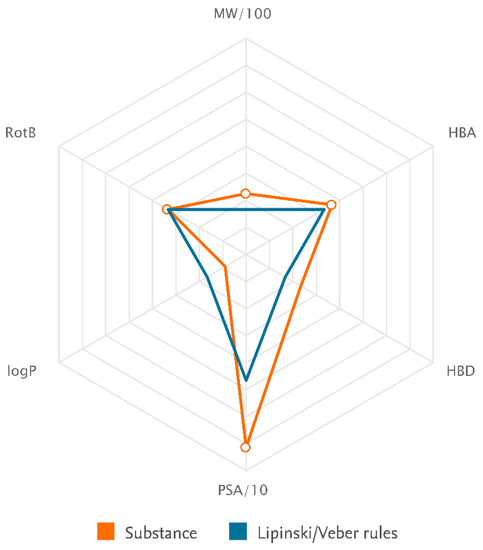
Figure 3.
The illustration of the compatibility of substance physicochemical properties with Lipinski/Veber rules component (National Center for Biotechnology Information (2022). PubChem Compound Summary for CID 72302. Retrieved from https://pubchem.ncbi.nlm.nih.gov/compound/72302) (accessed on 1 January 2023).
In UV-visible spectroscopy, the absorption peak of 268 nm can be seen in the curve. In the FTIR spectrogram, the characteristic peaks at ≈1650, 1600, 1510, 1070, and 1260 cm−1 can be assigned to free icariin. In differential scanning calorimetry, the endothermic peak at ≈250 °C is related to icariin [97].
5. Bioengineering Application of ICRN
5.1. Bone Tissue Engineering
Bone disorders are becoming usual frequently as the aging community grows, and bone breaks often moreover happen. The treatment of major bone defects remains a main challenge [98]. The necessity for osteogenic bone alternatives causes the advancement of approaches in bone material engineering. A usual material engineering plan typically contains cells, biomaterials, and bioactive scaffolds [99]. Autologous multipotent cells have been broadly employed for bone renewal [100]. Though a perfect bone tissue engineering scaffold must be both osteoconductive and osteoinductive [101], most polymers and metal scaffolds are only osteoconductive [102,103]. To increase the beneficial properties, biological factors are generally used by viral gene or protein delivery [104,105]. Even though an employment of bone morphogenetic proteins (BMPs) has been widely considered for bone renewal, huge volumes of BMPs are essential and BMP-comprising plans tend to fail in a certain proportion of cases, thus raising worries over expenses and safety [106,107]. The high cost and quick ruin of BMPs and other protein drugs [108] bound their experimental usage, too. Hence, there is a critical need for alternative agents with higher usefulness and cost-effectiveness. There is a limited amount of information on low molecular weight agents that effectually enhance bone construction, for instance statins [109] and isoflavone products [110]. With the advances in separation procedures, it has become more facile to acquire purified molecules such as ICRN from natural sources instead of using unsafe materials, which is even expensive.
In a study, ICRN encapsulated with PLGA was implanted in 3-dimensional printed polycaprolactone/nano-hydroxyapatite scaffolds to simplify in-situ regeneration of bones. Such a scaffold displayed outstanding mechanical efficiency due to the nano-hydroxyapatite and revealed sustainable diffusion of ICRN as the polycaprolactone degraded [111]. Another study represented that ICRN can activate both ERα (non-genomic estrogen receptor) and Akt (serine/threonine-specific protein kinase) by increasing rapid induction of insulin-like growth factor I (IGF-1) signaling in osteoblastic cells for osteogenesis [112]. It is demonstrated that ICRN promotes and inhibits, respectively, humanoid osteogenic and adipogenic differentiation of bone marrow mesenchymal stem (BM-MS) cells via activating of the Wnt/β-catenin pathway mediated by microRNA 23a [113]. In a work, the released drug from thiolated ICRN/biphasic calcium phosphate scaffolds could increase the migration, proliferation and osteogenesis of ovariectomized rat BM-MS cells, and upregulate the angiogenic gene expression in humanoid umbilical vein endothelial cells in vitro [33]. ICRN in combination with other substances can be even more effective. A study by Don et al. showed that fetal bovine serum exosomes-ICRN more efficiently increased the osteoblasts’ proliferation than the time ICRN was used alone [114]. It was shown that ICRN is considered a factor for knee osteoarthritis by involving four pain-related genes as well [115].
5.2. Cartilage Tissue Engineering
Osteoarthritis is the most public chronic joint sickness and is related with signs for instance, cartilage damage and deprivation. Cartilage displays too low affinity to self-repair because of the little regenerative ability of resident chondrocytes and the privation of vascular, nervous, and lymphatic structures [116]. Existing clinically presented cartilage treatments consist of autologous chondrocyte implantation, matrix induced autologous chondrocyte implantation, microfracture, and abrasion arthroplasty. On the other hand, these plans are only responsible for sub-optimal clinical results and are frequently not enough for keeping the durable function of articular cartilage [117]. Because of these problems, studies in recent years were intensive on cartilage engineering which cells, functional molecules, and scaffolds to lead cartilage creation. Chondrocytes are the best cell resources for cartilage tissue treatment. Nevertheless, chondrocytes have a tendency to miss their phenotype and go through hypertrophy upon in vitro growth, that could be described by reduced fabrication of proteoglycan and type II collagen, and enhanced secretion of type I and type X collagens [118]. Hence, existing approaches for applied material engineering scaffolds for preserving the differentiated state of chondrocytes, endorsing cartilage creation, and the latest works revealed that a suitable scaffold with organized release biomolecules may perhaps be more in effect [119,120]. Numerous works also revealed that ICRN is able to enable the chondrogenesis of mesenchymal stem (MS) cells in an accustomed medium, provide propagation of chondrocytes, keep the phenotype of chondrocytes, stimulate the secretion of proteoglycan and the collagen matrix and prevent the deprivation of collagen and proteoglycan [121,122]. Furthermore, in cooperation with exogenous growth regulators, ICRN is low-cost, constant and non-immunogenic [123]. As a result, ICRN has been widely employed in scaffolds to increase speed tissue regeneration [124]. Some works proposed that an upper concentration of ICRN can motivate chondrocytes to secrete a further cartilage matrix within the in effect harmless concentration variety [125]. It was indicated that ICRN could prevent cell propagation at concentrations above 10 mM [126].
With the aim of enhancing the ICRN loading to retain the enduring biological property of the scaffolds, ICRN was fused into the hydrogel scaffolds or chemical crosslinking. The achieved hydrogel scaffolds continued an elongated smooth release of drugs and permitted the encapsulated chondrocytes to secrete more proteoglycan and the collagen matrix, but its poisonousness to the encapsulated cells is not adopted for clinical uses [123,127].Some bioengineering applications of ICRN are listed in Table 2.

Table 2.
Bioengineering application of ICRN.
6. Cancer Therapy by ICRN
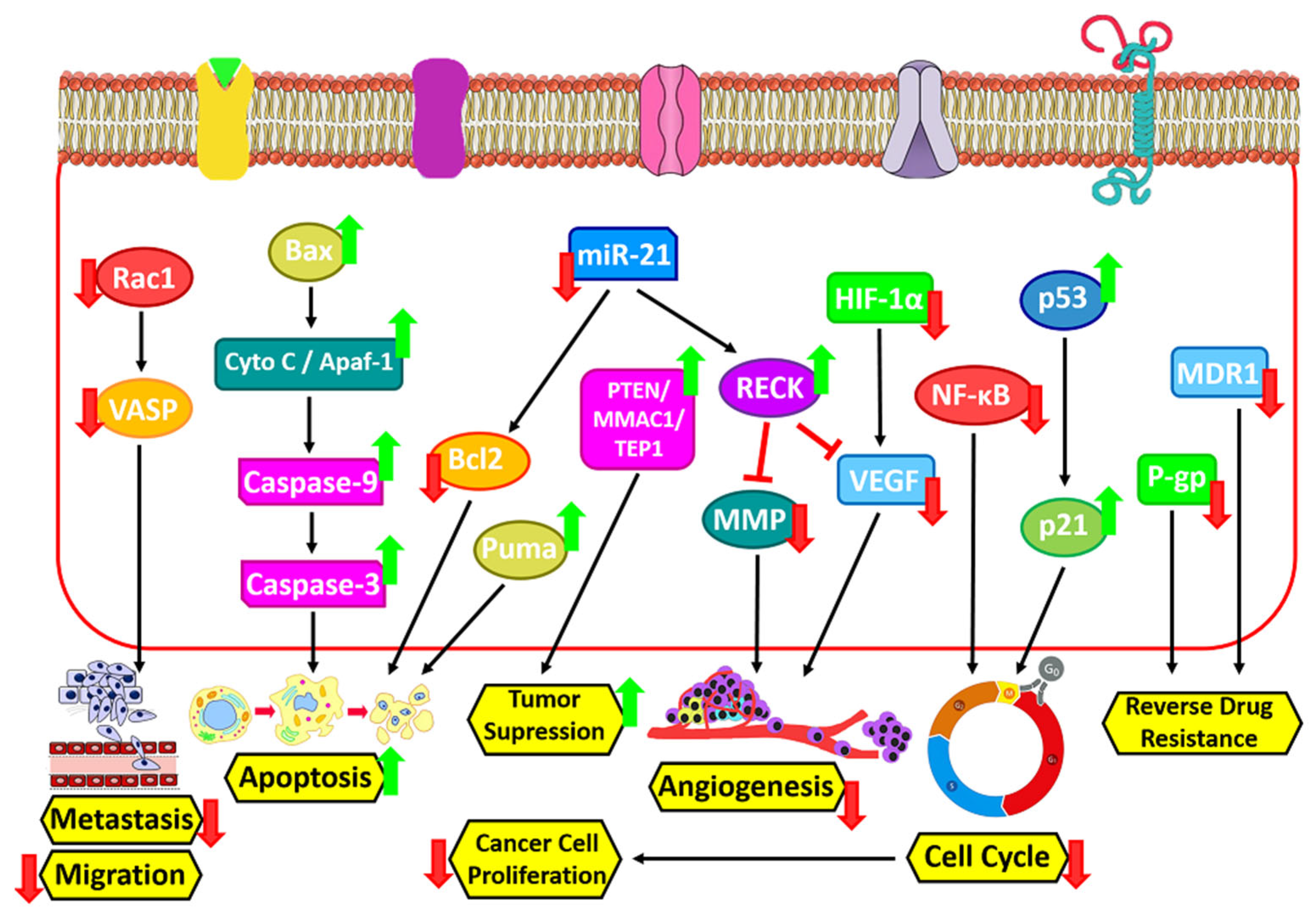
6.1. Apoptosis Induction
The planned cell death that occurs in the organs of the body is called apoptosis. Biochemical changes including mixing, nuclear disintegration, chromatin density, DNA cleavage, mRNA decay, and eventually cell shrinkage alter cell morphology and other characteristics and cause cell death [131]. ICRN and its derivatives exert their apoptotic effect by activating the innate pathway of apoptosis. ICRN and icaritin increase cytochrome c secretion, Bax/Bcl2 ratio, poly (ADP-ribose) polymerase and caspase stimulation in various types of cancer cells (Figure 4) [132]. MiR-21 is extremely expressed in numerous human tumors and can cause cell proliferation, differentiation and apoptosis, and also play a key role in the formation of metastases in tumors. In a study by Li et al., they showed that ICRN can stimulate caspase-3 activity, block the expression of miR-21, and induce cellular apoptosis in ovarian cancerous cells. Wang et al. represented that ICRN inhibits Bcl-2 protein expression and induces apoptosis in MLTC-1 cells by regulating Bcl-2/Bax expression (Figure 4) [133]. In cancer cells, ICRN significantly reduces the expression of microRNA 21 and the Bcl-2 protein, and increases the expression of PTEN and RECK protein (Figure 3) [134]. According to Sharma et al., however, ICRN treatment noticeably leads to CDK2, CDK4, Cyclin D1, Bcl-2, and Beclin-1 downregulation, it up-regulates the expression ranks of caspase 3 (Figure 4), PARP and p62 [135].
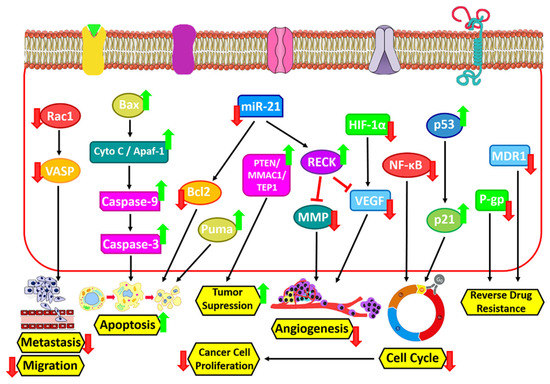
Figure 4.
Cancer therapy by ICRN.
The results of Western blot tests by Fan et al. to evaluate the anti-cancer action of ICRN in esophageal squamous cells carcinoma (ESCC) showed that ICRN upregulated the expression of GRP78 ATF4 and CHOP. It also upregulated p-PERK and p-eIF2α amounts in EC109 and TE1 cells in an amount-dependent way as well as increased Puma expression and decreased Bcl2 expression. In this study, the apoptotic index of ESCC was evaluated after concentrations of 20, 40 and 80 μM ICRN for 24 h. The results showed an enhancement in the stimulation of apoptosis with an increasing ICRN dose [136]. Moreover, ICRN induces the apoptosis process through the upregulation of Bax/Bcl-2 and induce ROS in a mitochondria mediated way. Notably, the blockage of breast cancer cells invasion through the abating of NF-κB/EMT activation by ICRN as shown [137]. In another study it was reported that ICRN inhibits the proliferation and migration of ovarian cancer cells in vitro and stimulates apoptosis via stopping the PI3K/AKT signaling [138].
6.2. Inhibition of Cancer Cell Proliferation
ICRN stops the cell cycle at the G0/G1 and G2/M phases by inhibiting NF-κB activity and thus blocks the growth of cancer cells (Figure 4) [132]. Song et al. reported that in vitro, ICRN induces dose/time dependent cell toxicity to MDA-MB-231, MDA-MB-453, and 4T1 cell lines, and inhibits breast cancer cell proliferation [137]. They also used colony formation methods to confirm the anti-proliferative effect of ICRN. The ability to form colonies of cells concentrated with 10 or 20 μM ICRN was considerably repressed and the size of colonies uncovered to ICRN was reduced in comparison to the control group. ICRN can inhibit the tumor growing in vivo. To see if the anti-tumor activity of ICRN in vivo is similar to its effects in vitro, tumor-bearing mice MDA-MB-231 and 4T1 were treated with doses of 20 and 40 mg/kg of ICRN. A therapeutic dosage of 20 mg/kg (p < 0.01) and therapeutic quantity of 40 mg/kg (p < 0.005) significantly inhibited the growth of the MDA-MB-231 tumor in a dose-dependent way compared to the control group. The mice did not show any abnormal alterations in body weight during treatment. Immunohistochemical results of tumors showed that ICRN inhibits the proliferation of Ki-67-positive cells, increases caspase-3 expression, induces cell apoptosis, and regulates NF-κB expression. Moreover, Western blot results of tumors indicated that ICRN increases the SIRT6 expression level, inhibits NF-κB p65 nuclear expression, and decreases PD-L1 expression. ICRN was similar in the model of 4T1 tumor-bearing mice, and was able to reduce tumor cell proliferation and NF-κB expression levels and stop tumor growth (Figure 4) [137]. A latest work by Wang et al. on the therapeutic properties of ICRN at concentrations of 25 μM, 50 μM, and 100 μM for 48 h in relation to cancer showed that this biomaterial could be significantly dose-dependent and inhibit SKOV3 cell proliferation [138].
6.3. Angiogenesis Inhibition
ICRN stops the proliferation, migration and formation of cancer cells. Moreover, it has anti-angiogenic action in vivo in various tumor models. CD31 is a pan-endothelial indicator and is expressed on the surface of endothelial cells. ICRN treatment significantly reduced CD31-positive regions in tumor mice. As is clear, the vascular endothelial growth factor (VEGF) is an important growing agent that acts as a major controller of angiogenesis. The consequences of both in vitro and in vivo investigation show that the decrease in VEGF levels by down regulation of this factor in both ICRN treated groups showed the anti-angiogenic effect of this biomaterial (Figure 4).
Hypoxia-inducible factor-1α (HIF-1α) is a substantial goal in solid tumors therapy and is induced by hypoxia in a dose-dependent way in cancer cells. It is assumed that Icariside II (one of the ICRN-derivatives) increases the interaction between HIF-1α and von Hippel-Lindau (VHL) whereby a decrease in the protein level of HIF-1α occurs (Figure 4) [139]. Additionally, Icariside-II blocks the migration rate in human osteosarcoma cells and the tube creation rate in humanoid umbilical vein endothelial cells.
RECK is a recently explored tumor-inhibitor gene and is known as a matrix metalloproteinase inhibitor, in turn, decreasing the tumor invasion and angiogenesis [140]. The influence of ICRN on the expression of the RECK protein in A2780 ovarian cancer cells was tested. The consequences displayed that treatment with ICRN for 2 days at dose of 25 and 50 μM significantly enhanced the expression level of the RECK protein compared to the control group (Figure 4) [134].
6.4. Metastasis and Migration Inhibition
Metastasis is the movement of a pathogen from a primary site to a secondary site in the host body. That is very common in the later stages of cancer and occurs through the blood, lymph, or both. The most common sites of metastasis are the lungs, liver, brain, and bones. The anti-metastatic activity of ICRN has also been investigated. A study of very metastatic human lung cancerous cells after treatment with ICRN displayed a reduction in the capability of these cells to attack and migrate (Figure 4) [141]. Another study on ICRN indicated that it could suppress the adhesion of lung adenocarcinoma by acting on vasodilator phosphoprotein (VASP), which is important in cell migration along with tumor metastasis. This study also showed that this biomaterial inhibits gastric cancerous cell invasion and cell migration and is the main process for suppressing the expression of genes associated with Rac1 and VASP cell motility (Figure 4) [142]. The results of these works showed that ICRN and its derivatives prevent cancer cell metastasis by regulating proteins that are critical for cancer metastasis [143,144]. A study by Song et al. found that ICRN could inhibit the pulmonary metastasis pattern of 4T1 cells in BALB/c mice. Moreover, lung tissues were examined using H&E staining to estimate the anti-metastatic efficiency of ICRN. In these tissue sections, H&E staining showed that there were fewer tumor nodules in the ICRN group compared to the control group [137].
6.5. Regulation of Immune System
Immunomodulation is thought to revolutionize the treatment of inflammation-related diseases such as autoimmune diseases, and cancer. [145]. The immune system in these situations could be either motivated or inhibited by biomaterials. ICRN has been shown to reduce tumor progress and the ratio of Myeloid-derived suppressor cells (MDSCs) [132]. Liu et al. reported the sex hormone-like properties of ICRN on T-cells immune modulation in spontaneously hypertensive rats. Their results proved that ICRN can regulate T-cells differentiation related to blood pressure reduction in SHR rats [146]. According to these studies, the effect of modulating the immune system of ICRN causes anti-tumor immunity in killing tumor cells and stunting tumor cells.
In another study, due to the effective inhibitory result of ICRN on the NF-kB signaling way, the ability of ICRN to suppress the microenvironment of the tumor environment was investigated. MDSCs, which typically accumulate in tumors, are responsible for suppressing the immune system’s microenvironment. In the study of the effect of ICRN on CD4+ and CD8+ T-cells, the results represented that the ratio of tumor infiltration to CD4+ and CD8+ cells was meaningfully enhanced. In addition, it significantly regulated the proportion of MDSCs in the tumor compared to the control group. In general, ICRN can improve the microenvironment of the tumor suppressor immune system, thus increasing the anti-tumor effect [137].
7. Effects of ICRN on Drugs Used in Cancer Therapy
7.1. Multidrug Resistance (MDR) Inhibition
Multidrug Multidrug resistance is a principal concern in community health. It defines a complex phenotype whose principal feature is resistance to a wide-ranging of structurally unrelated cell toxicity complexes, many of which are anticancer factors [147]. Moreover, MDR could be caused by a species of micro-organism to at least one antimicrobial drug in three or more antimicrobial classes [22,24,148]. Some studies were performed to overcome drug resistance induced by tumor cells with ICRN and its derivatives. A study on the adriamycin-resistant ADR-resistant human hepatocellular cell line found that ICRN-derived icarithin can reduce ADR cytotoxicity by decreasing MDR1 gene expression, decreasing P-gp levels, and increasing intracellular accumulation ADR [149]. PTEN gene deficiency is present in malignant tumors and tumor cell lines (Figure 4) [150]. Lee et al. showed that ICRN enhances PTEN protein expression in ovarian cancer cells [134].
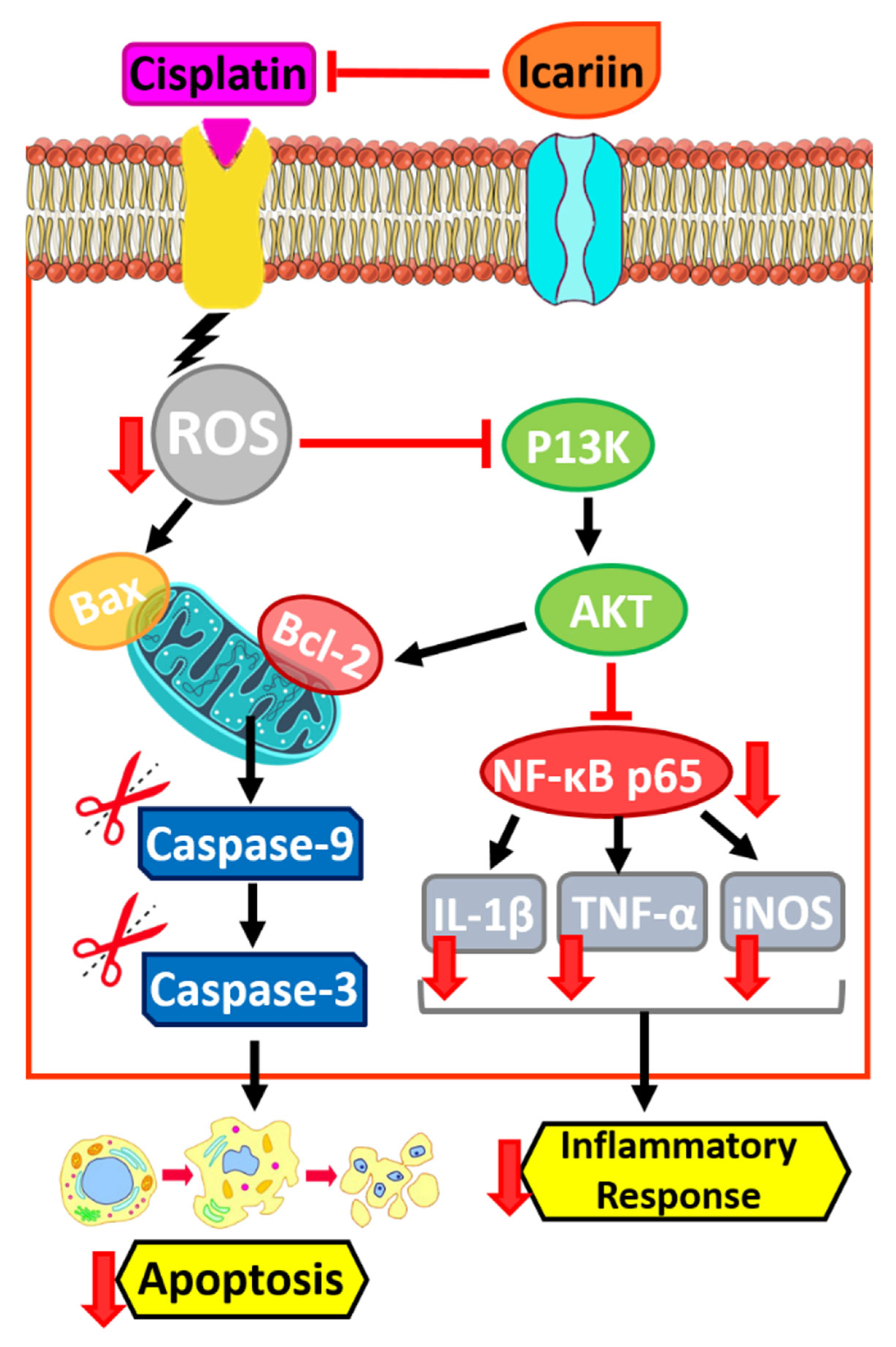
7.2. Effects of ICRN on Cisplatin
ICRN, as a major and remarkable flavonoid is utilized in cancer therapy. Cisplatin, as an efficient chemo-remedial factor, is usually employed to treat several kinds of cancers [151,152]. Nephrotoxicity stimulated by cisplatin extremely limits its clinical uses [153,154,155].
The mechanism principal for the decrease in cisplatin-induced renal damage using ICRN was investigated. Treatment of mice with cisplatin cause renal injury, displaying enhancement in blood urea nitrogen, tubular damage, and apoptosis. These renal alterations could be meaningfully improved by ICRN. The results show that ICRN decreased the expression of TNF-α and NF-κB, cleaved caspase-3, and Bax, as well as enhanced the expression of BCL-2 [156]. It is reported that ICRN increases the chemosensitivity of cisplatin-resistant ovarian cancerous cells by inhibiting autophagy using activation of the AKT/mTOR/ATG5 way (Figure 5) [157].
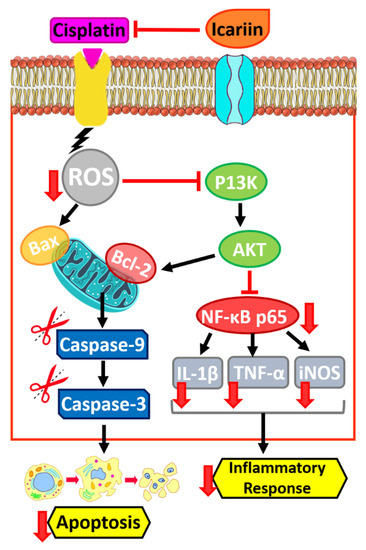
Figure 5.
Effects of ICRN on Cisplatin in cancer therapy.
8. Other pharmacological Effects of ICRN
Natural products have contributed to the improvement of numerous drugs for various signs. It is becoming clear that many natural products are able to influence receptor positions on or inside cells, just as a drug must do [158]. Natural-product frameworks are labelled as privileged constructions. Several in vivo works verified the useful result of ICRN on reproductive utilities. Treatment of ICRN meaningfully enhances epididymal sperm counts and testosterone ranks of male rats [71]. ICRN as well effectively enhanced the erectile action in gelded wistar rats using an enhancing proportion of smooth muscle and inducible NO-synthase in the corpus cavernosum [159]. ICRN is a main biological pharmaceutical material with strong cardiovascular protecting roles [160]. Emerging data in the previous reports revealed that it has numerous atheroprotective roles, by several mechanisms, comprising decreasing DNA destruction [161], modifying endothelial dysfunction [162], preventing the propagation and migration of smooth muscle cells [163], inhibiting macrophage derived foam cell creation and inflammatory responses. [164,165].
Two main hallmarks are regarded as Alzheimer’s disease (AD): extracellular gathering of amyloid b peptide (Ab) and intraneuronal accumulation of the tau protein as well-known as neurofibrillary tangles (NFTs) [166]. Guo et al. proposed that ICRN can progress spatial learning and memory capabilities in rats with brain dysfunction prompted by lipopolysaccharide (LPS), a result which could be caused by reduced expressions of TNFα, IL-1β and COX2 in the hippocampus (Table 3) [167].

Table 3.
Other pharmacological effects of ICRN.
9. Conclusions
Use of bio-scaffolds in tissue engineering is an inevitable application, but biodegradability and biocompatibility are the main properties of scaffolds that should be considered. Animal or plant derived proteins that are recognized as natural biopolymers have critical impacts on cell behaviors. Interestingly, safer and eco-friendly greener technologies resulting from plant-based polymers can make promising effects on regenerative medicine and tissue engineering. ICRN as a reliable plant biomaterial shows many effects in medical treatment such as increasing osteogenesis by induction of IGF-1, also by activating the Wnt/β-catenin pathway and inhibiting adipogenesis. Preventing cell propagation at concentrations above 10 mM, inducing the apoptosis process through the upregulation of Bax/Bcl-2, inducing cell apoptosis due to increasing caspase-3 expression, suppressing the adhesion of lung adenocarcinoma by acting on VASP thereby influencing cell migration as well as tumor metastasis are the other applications of ICRN. Besides, the elongated smooth release of drugs giving permission to the encapsulated chondrocytes to secrete more collagen matrix exemplifies the role of ICRN in bio- and tissue engineering when it is combined with hydrogel scaffolds. Tumor progression is often linked with a phenotypic switch from M1 to M2 in tumor associated macrophages (TAMs) in the tumor microenvironment. Seyedi and her colleagues showed that downregulation of STAT3 resulted in the switching of M2 to M1 in the tumor microenvironment, in turn causing inhibition of tumor progression [183]. Moreover, other studies demonstrate the activation of cancer stem cells by increasing IL6 and MFG-E8 secretion stemming from overexpression of STAT3 in the tumor microenvironment [184,185]. Hence, the evaluation of ICRN on STAT3 downregulation in order to switch M2 to M1 in the tumor microenvironment as well as in cancer stemming cell inactivation can be a promising study in the future. Above all, an emphasis is placed on the mechanism of ICRN and its future perspective, aiming at providing a relative theoretical base for the application of ICA in the future biomedical treatment plans.
Author Contributions
Conceptualization, M.E.T.Y., M.R.H., V.M. and M.S.A.; methodology, M.E.T.Y. and M.R.H.; validation, Z.S., M.S.A., A.H., M.R.H., J.S.-G. and M.E.T.Y.; investigation, Z.S., M.S.A., V.M., A.H., A.H.-M., M.M., M.Q., M.R.H., J.S-G. and M.E.T.Y.; resources, M.S.A., V.M., A.H., M.R.H., J.S.-G. and M.E.T.Y.; writing—original draft preparation, Z.S., V.M., A.H., A.H.-M., M.M. and M.Q.; writing—review and editing, M.S.A., M.R.H., J.S.-G. and M.E.T.Y.; project administration, M.S.A., M.R.H., J.S.-G. and M.E.T.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public or commercial.
Data Availability Statement
The data availability statement is not applicable to this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Mobaraki, F.; Momeni, M.; Yazdi, M.E.T.; Meshkat, Z.; Toosi, M.S.; Hosseini, S.M. Plant-derived synthesis and characterization of gold nanoparticles: Investigation of its antioxidant and anticancer activity against human testicular embryonic carcinoma stem cells. Process. Biochem. 2021, 111, 167–177. [Google Scholar] [CrossRef]
- Yazdi, M.E.; Amiri, M.S.; Darroudi, M. Biopolymers in the Synthesis of Different Nanostructures. In Reference Module in Materials Science and Materials Engineering; Elsevier: Amsterdam, The Netherlands, 2019; pp. 29–43. [Google Scholar] [CrossRef]
- Darroudi, M.; Yazdi, M.E.T.; Amiri, M.S. Plant-Mediated Biosynthesis of Nanoparticles. In 21st Century Nanoscience—A Handbook; CRC Press: Boca Raton, FL, USA, 2020. [Google Scholar] [CrossRef]
- Yazdi, M.E.T.; Amiri, M.S.; Nourbakhsh, F.; Rahnama, M.; Forouzanfar, F.; Mousavi, S.H. Bio-indicators in cadmium toxicity: Role of HSP27 and HSP70. Environ. Sci. Pollut. Res. 2021, 28, 26359–26379. [Google Scholar] [CrossRef] [PubMed]
- Es-haghi, A.; Javadi, F.; Yazdi, M.E.T.; Amiri, M.S. The Expression of Antioxidant Genes and Cytotoxicity of Biosynthesized Cerium Oxide Nanoparticles Against Hepatic Carcinoma Cell Line. Avicenna J. Med. Biochem. 2019, 7, 16–20. [Google Scholar] [CrossRef]
- Amiri, M.S.; Taghavizadeh Yazdi, M.E.; Rahnama, M. Medicinal plants and phytotherapy in Iran: Glorious his-tory, current status and future prospects. Plant Sci. Today 2021, 8, 95–111. [Google Scholar] [CrossRef]
- Alabyadh, T.; Albadri, R.; Es-Haghi, A.; Yazdi, M.E.T.; Ajalli, N.; Rahdar, A.; Thakur, V.K. ZnO/CeO2 Nanocomposites: Metal-Organic Framework-Mediated Synthesis, Characterization, and Estimation of Cellular Toxicity toward Liver Cancer Cells. J. Funct. Biomater. 2022, 13, 139. [Google Scholar] [CrossRef] [PubMed]
- Nadaf, M.; Abad, M.H.K.; Gholami, A.; Yazdi, M.E.T.; Iriti, M.; Mottaghipisheh, J. Phenolic content and antioxidant activity of different Iranian populations of Anabasis aphylla L. Nat. Prod. Res. 2022. [Google Scholar] [CrossRef] [PubMed]
- Ghorani-Azam, A.; Mottaghipisheh, J.; Amiri, M.S.; Mashreghi, M.; Hashemzadeh, A.; Haddad-Mashadrizeh, A.; Nourbakhsh, F.; Nadaf, M.; Qayoomian, M.; Yazdi, M.E.T. Resveratrol-Mediated Gold-Nanoceria Synthesis as Green Nanomedicine for Phytotherapy of Hepatocellular Carcinoma. Front. Biosci. 2022, 27, 227. [Google Scholar] [CrossRef] [PubMed]
- Farhangi, M.J.; Es-Haghi, A.; Yazdi, M.E.T.; Rahdar, A.; Baino, F. MOF-Mediated Synthesis of CuO/CeO2 Composite Nanoparticles: Characterization and Estimation of the Cellular Toxicity against Breast Cancer Cell Line (MCF-7). J. Funct. Biomater. 2021, 12, 53. [Google Scholar] [CrossRef]
- Gershlak, J.R.; Hernandez, S.; Fontana, G.; Perreault, L.R.; Hansen, K.J.; Larson, S.A.; Binder, B.Y.; Dolivo, D.M.; Yang, T.; Dominko, T.; et al. Crossing kingdoms: Using decellularized plants as perfusable tissue engineering scaffolds. Biomaterials 2017, 125, 13–22. [Google Scholar] [CrossRef]
- Es-Haghi, A.; Yazdi, M.T.; Sharifalhoseini, M.; Baghani, M.; Yousefi, E.; Rahdar, A.; Baino, F. Application of Response Surface Methodology for Optimizing the Therapeutic Activity of ZnO Nanoparticles Biosynthesized from Aspergillus niger. Biomimetics 2021, 6, 34. [Google Scholar] [CrossRef]
- Hashemzadeh, M.R.; Yazdi, M.E.T.; Amiri, M.S.; Mousavi, S.H. Stem cell therapy in the heart: Biomaterials as a key route. Tissue Cell 2021, 71, 101504. [Google Scholar] [CrossRef]
- Mousavi-Kouhi, S.M.; Beyk-Khormizi, A.; Mohammadzadeh, V.; Ashna, M.; Es-haghi, A.; Mashreghi, M.; Hashemzadeh, V.; Mozafarri, H.; Nadaf, M.; Taghavizadeh Yazdi, M.E. Biological synthesis and characterization of gold nanoparticles using Verbascum speciosum Schrad. and cytotoxicity properties toward HepG2 cancer cell line. Res. Chem. Intermed. 2021, 48, 167–178. [Google Scholar] [CrossRef]
- Yazdi, M.E.T.; Khara, J.; Housaindokht, M.R.; Sadeghnia, H.R.; Bahabadid, S.E.; Amiri, M.S.; Darroudi, M. Biocomponents and Antioxidant Activity of Ribes khorasanicum. Int. J. Basic Sci. Med. 2018, 3, 99–103. [Google Scholar] [CrossRef]
- Taghavizadeh Yazdi, M.E.; Khara, J.; Housaindokht, M.R.; Sadeghnia, H.R.; Esmaeilzadeh Bahabadi, S.; Amiri, M.S.; Darroudi, M. Assessment of phytochemical components and antioxidant activity of Rheum turkestanicum Janisch. Stud. Med. Sci. 2020, 31, 75–81. [Google Scholar]
- Yazdi, M.E.T.; Amiri, M.S.; Hosseini, H.A.; Oskuee, R.K.; Mosawee, H.; Pakravanan, K.; Darroudi, M. Plant-based synthesis of silver nanoparticles in Handelia trichophylla and their biological activi-ties. Bull. Mater. Sci. 2019, 42, 155. [Google Scholar] [CrossRef]
- Yazdi, M.E.T.; Darroudi, M.; Amiri, M.S.; Hosseini, H.A.; Nourbakhsh, F.; Mashreghi, M.; Farjadi, M.; Kouhi, S.M.M.; Mousavi, S.H. Anticancer, antimicrobial, and dye degradation activity of biosynthesised silver nanoparticle using Artemisia kopetdaghensis. Micro Nano Lett. 2020, 15, 1046–1050. [Google Scholar] [CrossRef]
- Nourbakhsh, F.; Lotfalizadeh, M.; Badpeyma, M.; Shakeri, A.; Soheili, V. From plants to antimicrobials: Natural products against bacterial membranes. Phytother. Res. 2021, 36, 33–52. [Google Scholar] [CrossRef]
- Modarres, M.; Yazdi, M.E.T. Elicitation Improves Phenolic Acid Content and Antioxidant Enzymes Activity in Salvia leriifolia Cell Cultures. Iran. J. Sci. Technol. Trans. A Sci. 2021, 45, 849–855. [Google Scholar] [CrossRef]
- Ashna, M.; Es-Haghi, A.; Noghondar, M.K.; Al Amara, D.; Yazdi, M.E.T. Greener synthesis of cerium oxide nanoemulsion using pollen grains of Brassica napus and evaluation of its antitumour and cytotoxicity properties. Mater. Technol. 2020, 37, 525–532. [Google Scholar] [CrossRef]
- Taghavizadeh Yazdi, M.E.; Darroudi, M.; Amiri, M.S.; Zarrinfar, H.; Hosseini, H.A.; Mashreghi, M.; Mozafarri, H.; Ghorbani, A.; Mousavi, S.H. Antimycobacterial, Anticancer, Antioxidant and Photocatalytic Activity of Bio-synthesized Silver Nanoparticles Using Berberis Integerrima. Iran. J. Sci. Technol. Trans. A Sci. 2021, 46, 1–11. [Google Scholar]
- Mohammadzadeh, V.; Barani, M.; Amiri, M.S.; Yazdi, M.E.T.; Hassanisaadi, M.; Rahdar, A.; Varma, R.S. Applications of plant-based nanoparticles in nanomedicine: A review. Sustain. Chem. Pharm. 2022, 25, 100606. [Google Scholar] [CrossRef]
- Yazdi, M.E.T.; Nourbakhsh, F.; Mashreghi, M.; Mousavi, S.H. Ultrasound-based synthesis of ZnO·Ag2O3 nanocomposite: Characterization and evaluation of its antimicrobial and anticancer properties. Res. Chem. Intermed. 2021, 47, 1285–1296. [Google Scholar] [CrossRef]
- Mousavi-Kouhi, S.M.; Beyk-Khormizi, A.; Amiri, M.S.; Mashreghi, M.; Yazdi, M.E.T. Silver-zinc oxide nanocomposite: From synthesis to antimicrobial and anticancer properties. Ceram. Int. 2021, 47, 21490–21497. [Google Scholar] [CrossRef]
- Pomeroy, J.E.; Helfer, A.; Bursac, N. Biomaterializing the promise of cardiac tissue engineering. Biotechnol. Adv. 2019, 42, 107353. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Zhang, J.; Liao, Y.; Alakpa, E.V.; Bunpetch, V.; Zhang, J.; Ouyang, H. Current advances in microsphere based cell culture and tissue engineering. Biotechnol. Adv. 2019, 39, 107459. [Google Scholar] [CrossRef]
- Hashemzadeh, M.R.; Mahdavi-Shahri, N.; Bahrami, A.R.; Kheirabadi, M.; Naseri, F.; Atighi, M. Use of an in vitro model in tissue engineering to study wound repair and differentiation of blastema tissue from rabbit pinna. Vitr. Cell. Dev. Biol. - Anim. 2015, 51, 680–689. [Google Scholar] [CrossRef]
- Sun, J.; Xu, W.; Zheng, S.; Lv, C.; Lin, J.; Chen, S.; Qiu, Y.; Jiang, X.; Draz, E.; Wang, S. Icariin promotes mouse Leydig cell testosterone synthesis via the Esr1/Src/Akt/Creb/Sf-1 pathway. Toxicol. Appl. Pharmacol. 2022, 441, 115969. [Google Scholar] [CrossRef]
- Zheng, J.; Hu, S.; Wang, J.; Zhang, X.; Yuan, D.; Zhang, C.; Liu, C.; Wang, T.; Zhou, Z. Icariin improves brain function decline in aging rats by enhancing neuronal autophagy through the AMPK/mTOR/ULK1 pathway. Pharm. Biol. 2021, 59, 181–189. [Google Scholar] [CrossRef]
- Li, C.; Li, Q.; Mei, Q.; Lu, T. Pharmacological effects and pharmacokinetic properties of icariin, the major bioactive component in Herba Epimedii. Life Sci. 2015, 126, 57–68. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, H.; Xiong, J.; Zhao, J.; Guo, M.; Chen, J.; Zhao, X.; Chen, C.; He, Z.; Zhou, Y.; et al. Icariin as an emerging candidate drug for anticancer treatment: Current status and perspective. Biomed. Pharmacother. 2023, 157. [Google Scholar] [CrossRef]
- Luo, Z.; Chen, X.; Liu, M.; Wang, Y.; Li, D.; Li, X.; Xiao, Y.; Wang, Y.; Zhang, X. The controlled release of a novel thiolated icariin for enhanced osteoporotic bone regeneration. Mater. Des. 2021, 200, 109468. [Google Scholar] [CrossRef]
- Du, W.; Tang, Z.; Yang, F.; Liu, X.; Dong, J. Icariin attenuates bleomycin-induced pulmonary fibrosis by targeting Hippo/YAP pathway. Biomed. Pharmacother. 2021, 143, 112152. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wang, M.; Wang, L.; Zhou, L.; Feng, X.; Ye, C.; Wang, C. Icariin attenuates renal fibrosis in chronic kidney disease by inhibiting interleukin-1β/transforming growth factor-β-mediated activation of renal fibroblasts. Phytother. Res. 2021, 35, 6204–6215. [Google Scholar] [CrossRef] [PubMed]
- Angeloni, C.; Barbalace, M.C.; Hrelia, S. Icariin and Its Metabolites as Potential Protective Phytochemicals Against Alzheimer’s Disease. Front. Pharmacol. 2019, 10, 00271. [Google Scholar] [CrossRef]
- Pharmacopoeia, C. Chinese Pharmacopoeia Commission Chinese Pharmacopoeia; Chinese Medical Science and Technology Press: Beijing, China, 2020. [Google Scholar]
- The Plant List, 2013. Version 1.1. Published on the Internet. Available online: http://www.theplantlist.org/ (accessed on 1 January 2023).
- Shen, P.; Guo, B.; Gong, Y.; Hong, D.Y.; Hong, Y.; Yong, E. Taxonomic, genetic, chemical and estrogenic characteristics of Epimedium species. Phytochemistry 2007, 68, 1448–1458. [Google Scholar] [CrossRef] [PubMed]
- Yan-Jun, Z.; Jian-Qiang, L. A New Species of Epimedium (Berberidaceae) from Hubei, China. Novon 2009, 19, 567–569. [Google Scholar] [CrossRef]
- Liu, C.; Xu, L. Analysis of active ingredients of traditional Chinese herbal drug. Assay of icariin in Epimedium. Chin J Pharm Anal 1984, 4, 81–84. [Google Scholar]
- Ma, H.; He, X.; Yang, Y.; Li, M.; Hao, D.; Jia, Z. The genus Epimedium: An ethnopharmacological and phytochemical review. J. Ethnopharmacol. 2011, 134, 519–541. [Google Scholar] [CrossRef]
- Zhai, Y.-K.; Guo, X.; Pan, Y.-L.; Niu, Y.-B.; Li, C.-R.; Wu, X.-L.; Mel, Q.-B. A systematic review of the efficacy and pharmacological profile of Herba Epimedii in osteoporosis therapy. Die Pharm. 2013, 68, 713–722. [Google Scholar]
- Aljehani, A.A.; Albadr, N.A.; Nasrullah, M.Z.; Neamatallah, T.; Eid, B.G.; Abdel-Naim, A.B. Icariin ameliorates metabolic syndrome-induced benign prostatic hyperplasia in rats. Environ. Sci. Pollut. Res. 2021, 29, 20370–20378. [Google Scholar] [CrossRef]
- Hou, L.; Lin, Z.; Xu, A.; Le, G.; Ge, L.; Liu, S.; Muhmood, A.; Gan, F.; Huang, K. Combined protective effects of icariin and selenomethionine on novel chronic tubulointerstitial nephropathy models in vivo and in vitro. Br. J. Nutr. 2021, 127, 12–22. [Google Scholar] [CrossRef]
- Kou, Z.; Wang, C.; Gao, L.; Chu, G.; Yang, G.; Pang, W. Icariin improves pig sperm quality through antioxidant and antibacterial effects during liquid storage at 17 °C. Livest. Sci. 2022, 256, 104827. [Google Scholar] [CrossRef]
- Yuan, J.-Y.; Yuan, J.-Y.; Tong, Z.-Y.; Dong, Y.-C.; Zhao, J.-Y.; Shang, Y. Research progress on icariin, a traditional Chinese medicine extract, in the treatment of asthma. Allergologia Immunopathol. 2022, 50, 9–16. [Google Scholar] [CrossRef]
- Liu, Y.; Lin, L.; Xiao, W.; Ji, Q.; Liu, Y. Effects of icariin on NRG1-ErbB signaling pathways in hippocampus of schizophrenia rats. Chin. J. Tissue Eng. Res. 2023, 27, 3236–3241. [Google Scholar]
- Lu, C.; Zou, K.; Guo, B.; Li, Q.; Wang, Z.; Xiao, W.; Zhao, L. Linker-peptide-mediated one-step purification and immobilization of alpha-L-rhamnosidase from Bacteroides thetaiotaomicron for direct biotransformation from epimedin C to icariin. Enzym. Microb. Technol. 2023, 162, 110131. [Google Scholar] [CrossRef]
- Mei, J.; He, Q.; Sun, X.; Yin, H.; Qian, W.Q. Icariin promotes osteoblast proliferation and differentiation through a non-nuclear signaling pathway. Chinese J. Tissue Eng. Res. 2023, 27, 3129–3135. [Google Scholar]
- Xue, P.; Du, B.; Liu, X.; Sun, G.; Cheng, T.; Chen, H.; He, S. Characterization and osteogenic ability of Mg-F membrane/icariin membrane/beta-tricalcium phosphate scaffolds fabricated by coating process combined with 3D printing. Chin. J. Tissue Eng. Res. 2023, 27, 2480–2487. [Google Scholar]
- Yan, F.; Liu, J.; Chen, M.-X.; Zhang, Y.; Wei, S.-J.; Jin, H.; Nie, J.; Fu, X.-L.; Shi, J.-S.; Zhou, S.-Y.; et al. Icariin ameliorates memory deficits through regulating brain insulin signaling and glucose transporters in 3?Tg-AD mice. Neural Regen. Res. 2023, 18, 183–188. [Google Scholar]
- Chen, M.; Wu, J.; Luo, Q.; Mo, S.; Lyu, Y.; Wei, Y.; Dong, J. The Anticancer Properties of Herba Epimedii and Its Main Bioactive Componentsicariin and Icariside II. Nutrients 2016, 8, 563. [Google Scholar] [CrossRef]
- Iqubal, M.K.; Chaudhuri, A.; Iqubal, A.; Saleem, S.; Gupta, M.M.; Ahuja, A.; Ali, J.; Baboota, S. Targeted Delivery of Natural Bioactives and Lipid-nanocargos against Signaling Pathways Involved in Skin Cancer. Curr. Med. Chem. 2021, 28, 8003–8035. [Google Scholar] [CrossRef]
- Aboulthana, W.M.; Mehta, D.K. Phyto-Phospholipid Complexation as a Novel Drug Delivery System for Management of Cancer with Better Bioavailability: Current Perspectives and Future Prospects. Anti-Cancer Agents Med. Chem. 2021, 21, 1403–1412. [Google Scholar] [CrossRef]
- He, Q.; Dong, H.; Gong, M.; Guo, Y.; Xia, Q.; Gong, J.; Lu, F. New Therapeutic Horizon of Graves’ Hyperthyroidism: Treatment Regimens Based on Immunology and Ingredients from Traditional Chinese Medicine. Front. Pharmacol. 2022, 13. [Google Scholar] [CrossRef]
- Liu, J.-P. Novel strategies for molecular targeting to cancer. Clin. Experim. Pharmacol. Physiol. 2016, 43, 287–289. [Google Scholar] [CrossRef]
- Abbas, M.N.; Kausar, S.; Cui, H. Therapeutic potential of natural products in glioblastoma treatment: Targeting key glioblas-toma signaling pathways and epigenetic alterations. Clin. Transl. Oncol. 2020, 22, 963–977. [Google Scholar] [CrossRef]
- Alhakamy, N.A.; Badr-Eldin, S.M.; Alharbi, W.S.; Alfaleh, M.A.; Al-Hejaili, O.D.; Aldawsari, H.M.; Eid, B.G.; Bakhaidar, R.; Drago, F.; Caraci, F.; et al. Development of an Icariin-Loaded Bilosome-Melittin Formulation with Improved Anticancer Activity against Cancerous Pancreatic Cells. Pharmaceuticals 2021, 14, 1309. [Google Scholar] [CrossRef]
- Agarwal, S.; Sau, S.; Iyer, A.K.; Dixit, A.; Kashaw, S.K. Multiple strategies for the treatment of invasive breast carcinoma: A comprehensive prospective. Drug Discov. Today 2022, 27, 585–611. [Google Scholar] [CrossRef]
- Almoshari, Y. Development, Therapeutic Evaluation and Theranostic Applications of Cubosomes on Cancers: An Up-dated Review. Pharmaceutics 2022, 14, 600. [Google Scholar] [CrossRef]
- Wu, J.-F.; Dong, J.-C.; Xu, C.-Q. Effects of icariin on inflammation model stimulated by lipopolysaccharide in vitro and in vivo. Chin. J. Integr. Tradit. West. Med. 2009, 29, 330–334. [Google Scholar]
- Yasukawa, K.; Ko, S.-K.; Whang, W.-K. Inhibitory effects of the aerial parts of Epimedium koreanum on TPA-induced inflammation and tumour promotion in two-stage carcinogenesis in mouse skin. J. Pharm. Nutr. Sci. 2016, 6, 38–42. [Google Scholar] [CrossRef]
- Hua, W.; Zhang, Y.; Wu, X.; Kang, L.; Tu, J.; Zhao, K.; Li, S.; Wang, K.; Song, Y.; Luo, R.; et al. Icariin attenuates interleukin-1beta-induced inflammatory response in human nucleus pulposus cells. Curr. Pharm. Des. 2017, 23, 6071–6078. [Google Scholar] [CrossRef]
- Zhong, S.; Ge, J.; Yu, J.-Y. Icariin prevents cytokine-induced beta-cell death by inhibiting NF-kappaB signaling. Exp. Ther. Med. 2018, 16, 2752–2762. [Google Scholar]
- Li, X.; Zhu, T.; Wang, M.; Zhang, F.; Zhang, G.; Zhao, J.; Zhang, Y.; Wu, E.; Li, X. Icariin Attenuates M1 Activation of Microglia and Abeta Plaque Accumulation in the Hippocampus and Prefrontal Cortex by Up-Regulating PPARgamma in Restraint/Isolation-Stressed APP/PS1 Mice. Front. Neurosci. 2019, 13, 291. [Google Scholar]
- Ma, A.; Ma, A.; You, Y.; Chen, B.; Wang, W.; Liu, J.; Qi, H.; Liang, Y.; Li, Y.; Li, C. Icariin/aspirin composite coating on TiO2 nanotubes surface induce immunomodulatory effect of macro-phage and improve osteoblast activity. Coatings 2020, 10, 427. [Google Scholar] [CrossRef]
- Desai, T.D.; Wen, Y.-T.; Daddam, J.R.; Cheng, F.; Chen, C.-C.; Pan, C.-L.; Lin, K.-L.; Tsai, R.-K. Long term therapeutic effects of icariin-loaded PLGA microspheres in an experimental model of optic nerve ischemia via modulation of CEBP-beta/G-CSF/noncanonical NF-kappaB axis. Bioeng. Transl. Med 2022, 7, e10289. [Google Scholar] [CrossRef]
- Liu, T.; Xin, H.; Li, W.; Zhou, F.; Li, G.; Gong, Y.; Gao, Z.; Qin, X.; Cui, W.; Shindel, A.W.; et al. Effects of Icariin on Improving Erectile Function in Streptozotocin-Induced Diabetic Rats. J. Sex. Med. 2011, 8, 2761–2772. [Google Scholar] [CrossRef]
- Niu, Y.; Lin, G.; Pan, J.; Liu, J.; Xu, Y.; Cai, Q.; Wang, T.; Luan, Y.; Chen, Y.; Feng, Y.; et al. Deciphering the myth of icariin and synthetic derivatives in improving erectile function from a molecular biology perspective: A narrative review. Transl. Androl. Urol. 2021. [Google Scholar] [CrossRef]
- Chen, M.; Hao, J.; Yang, Q.; Li, G. Effects of Icariin on Reproductive Functions in Male Rats. Molecules 2014, 19, 9502–9514. [Google Scholar] [CrossRef]
- Xu, Y.; Xin, H.; Wu, Y.; Guan, R.; Lei, H.; Fu, X.; Xin, Z.; Yang, Y. Effect of icariin in combination with daily sildenafil on penile atrophy and erectile dysfunction in a rat model of bilateral cavernous nerves injury. Andrology 2017, 5, 598–605. [Google Scholar] [CrossRef]
- Yang, A.; Yu, C.; Lu, Q.; Li, H.; Li, Z.; He, C. Mechanism of Action of Icariin in Bone Marrow Mesenchymal Stem Cells. Stem Cells Int. 2019, 2019, 1–12. [Google Scholar] [CrossRef]
- Liu, J.; Cheng, Q.; Wu, X.; Zhu, H.; Deng, X.; Wang, M.; Yang, S.; Xu, J.; Chen, Q.; Li, M. Icariin Treatment Rescues Diabetes Induced Bone Loss via Scavenging ROS and Activating Primary Cilia/Gli2/Osteocalcin Signaling Pathway. Cells 2022, 11, 4091. [Google Scholar] [CrossRef]
- Xu, H.; Zhou, S.; Qu, R.; Yang, Y.; Gong, X.; Hong, Y.; Jin, A.; Huang, X.; Dai, Q.; Jiang, L. Icariin prevents oestrogen deficiency–induced alveolar bone loss through promoting osteogenesis via STAT3. Cell Prolif. 2020, 53, e12743. [Google Scholar] [CrossRef]
- Wei, Q.; He, M.; Chen, M.; Chen, Z.; Yang, F.; Wang, H.; Zhang, J.; He, W. Icariin stimulates osteogenic differentiation of rat bone marrow stromal stem cells by increasing TAZ expression. Biomed. Pharmacother. 2017, 91, 581–589. [Google Scholar] [CrossRef]
- Bi, Z.; Zhang, W.; Yan, X. Anti-inflammatory and immunoregulatory effects of icariin and icaritin. Biomed. Pharmacother. 2022, 151. [Google Scholar] [CrossRef]
- Zhang, Z.; Qin, F.; Feng, Y.; Zhang, S.; Xie, C.; Huang, H.; Sang, C.; Hu, S.; Jiao, F.; Jiang, J. Icariin regulates stem cell migration for endogenous repair of intervertebral disc degeneration by in-creasing the expression of chemotactic cytokines. BMC Complem. Med. Ther. 2022, 22, 1–11. [Google Scholar] [CrossRef]
- Bian, Q.; Liu, S.; Zhao, Y.; Huang, J.; Shen, Z. Icariin promotes osteoblastic differentiation in OVX mice via MAPK signaling pathway revealed by profiling. Tradit. Med. Mod. Med. 2018, 1, 33–41. [Google Scholar] [CrossRef]
- Xin, G.; Yuedong, Y.; Xuemei, S.; Chenhan, M.; Meng, Z.; Chenbo, Z.; Ning, G.; Xindong, W. The mechanism of Epimedium in the treatment of coronary atherosclerotic heart disease based on network pharmacology, molecular docking, and in vitro studies. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 2478–2488. [Google Scholar]
- Sharma, S.; Khan, V.; Dhyani, N.; Najmi, A.; Haque, S. Icariin attenuates isoproterenol-induced cardiac toxicity in Wistar rats via modulating cGMP level and NF-κB signaling cascade. Human Exper. Toxicol. 2020, 39, 117–126. [Google Scholar] [CrossRef]
- Zhai, M.; Minghe, Z.; Ju, X.; Shao, L.; Ling, S.; Zhang, Y.; Liu, Y.; Zhao, H. Icariin Acts as a Potential Agent for Preventing Cardiac Ischemia/Reperfusion Injury. Cell Biochem. Biophys. 2015, 72, 589–597. [Google Scholar] [CrossRef]
- Zeng, Y.; Xiong, Y.; Yang, T.; Wang, Y.; Zeng, J.; Zhou, S.; Luo, Y.; Li, L. Icariin and its metabolites as potential protective phytochemicals against cardiovascular disease: From effects to molecular mechanisms. Biomed. Pharmacother. 2022, 147, 112642. [Google Scholar] [CrossRef]
- Ni, T.; Lin, N.; Huang, X.; Lu, W.; Sun, Z.; Zhang, J.; Lin, H.; Chi, J.; Guo, H. Icariin Ameliorates Diabetic Cardiomyopathy Through Apelin/Sirt3 Signalling to Improve Mitochondrial Dysfunction. Front. Pharmacol. 2020, 11. [Google Scholar] [CrossRef]
- Shi, Y.; Yan, W.; Lin, Q.; Wang, W. Icariin influences cardiac remodeling following myocardial infarction by regulating the CD147/MMP-9 pathway. J. Int. Med. Res. 2018, 46, 2371–2385. [Google Scholar] [CrossRef] [PubMed]
- Ke, Z.; Liu, J.; Xu, P.; Gao, A.; Wang, L.; Ji, L. The Cardioprotective Effect of Icariin on Ischemia–Reperfusion Injury in Isolated Rat Heart: Potential Involvement of the PI 3 K-A kt Signaling Pathway. Cardiovasc. Ther. 2015, 33, 134–140. [Google Scholar] [CrossRef]
- Dell’Agli, M.; Galli, G.V.; Cero, E.D.; Belluti, F.; Matera, R.; Zironi, E.; Pagliuca, G.; Bosisio, E. Potent Inhibition of Human Phosphodiesterase-5 by Icariin Derivatives. J. Nat. Prod. 2008, 71, 1513–1517. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhao, Y.H.; Bin Jia, X.; Hu, M. Intestinal Absorption Mechanisms of Prenylated Flavonoids Present in the Heat-Processed Epimedium koreanum Nakai (Yin Yanghuo). Pharm. Res. 2008, 25, 2190–2199. [Google Scholar] [CrossRef]
- Ding, L.; Liang, X.; Zhu, D.; Lou, Y. Icariin promotes expression of PGC-1α, PPARα, and NRF-1 during cardiomyocyte differentiation of murine embryonic stem cells in vitro 1. Acta Pharm. Sin. 2007, 28, 1541–1549. [Google Scholar] [CrossRef]
- Yin, X.X.; Chen, Z.Q.; Liu, Z.J.; Dang, G.T. Icariine stimulates proliferation and differentiation of human osteoblasts by increasing production of bone morphogenetic protein 2. Chin. Med. J. 2007, 120, 204–210. [Google Scholar] [CrossRef]
- Hsiung, S.C.; Adlersberg, M.; Arango, V.; Mann, J.J.; Tamir, H.; Liu, K.P. Attenuated 5-HT1A receptor signaling in brains of suicide victims: Involvement of adenylyl cyclase, phosphatidylinositol 3-kinase, Akt and mitogen-activated protein kinase. J. Neurochem. 2003, 87, 182–194. [Google Scholar] [CrossRef]
- Wen, H.; Jung, H.; Li, X. Drug delivery approaches in addressing clinical pharmacology-related issues: Opportunities and challenges. AAPS J. 2015, 17, 1327–1340. [Google Scholar] [CrossRef]
- Wang, M.; Gao, H.; Li, W.; Wu, B. Icariin and its metabolites regulate lipid metabolism: From effects to molecular mechanisms. Biomed. Pharmacother. 2020, 131, 110675. [Google Scholar] [CrossRef]
- Zhang, X.D.; Guo, Y.; Li, D.X.; Wang, R.; Fan, H.S.; Xiao, Y.M.; Zhang, L.; Zhang, X.D. The effect of loading icariin on biocompatibility and bioactivity of porous β-TCP ceramic. J. Mater. Sci. Mater. Med. 2011, 22, 371–379. [Google Scholar] [CrossRef]
- Choi, S.; Noh, S.; Lim, C.; Kim, H.-J.; Jo, H.-S.; Min, J.; Park, K.; Kim, S. Icariin-Functionalized Nanodiamonds to Enhance Osteogenic Capacity In Vitro. Nanomaterials 2020, 10, 2071. [Google Scholar] [CrossRef]
- Oprita, E.I.; Iosageanu, A.; Craciunescu, O. Progress in Composite Hydrogels and Scaffolds Enriched with Icariin for Osteochondral Defect Healing. Gels 2022, 8, 648. [Google Scholar] [CrossRef]
- Cui, Y.-L.; Zhang, Y.; Meng, F.-C.; Lin, K.-M.; Wang, Q.-S. Changes in the intestinal absorption mechanism of icariin in the nanocavities of cyclodextrins. Int. J. Nanomed. 2012, 7, 4239–4249. [Google Scholar] [CrossRef]
- Otto, W.; Rao, J. Tomorrow’s skeleton staff: Mesenchymal stem cells and the repair of bone and cartilage. Cell Prolif. 2004, 37, 97–110. [Google Scholar] [CrossRef]
- Li, W.-J.; Tuli, R.; Huang, X.; Laquerriere, P.; Tuan, R.S. Multilineage differentiation of human mesenchymal stem cells in a three-dimensional nanofibrous scaffold. Biomaterials 2005, 26, 5158–5166. [Google Scholar] [CrossRef]
- Cowan, C.M.; Shi, Y.-Y.; Aalami, O.; Chou, Y.-F.; Mari, C.; Thomas, R.; Quarto, N.; Contag, C.; Wu, B.; Longaker, M.T. Adipose-derived adult stromal cells heal critical-size mouse calvarial defects. Nat. Biotechnol. 2004, 22, 560–567. [Google Scholar] [CrossRef]
- Datta, N.; Pham, Q.P.; Sharma, U.; Sikavitsas, V.I.; Jansen, J.A.; Mikos, A.G. In vitro generated extracellular matrix and fluid shear stress synergistically enhance 3D osteoblastic differentiation. Proc. Natl. Acad. Sci. USA 2006, 103, 2488–2493. [Google Scholar] [CrossRef]
- Liu, X.; Ma, P.X. Polymeric Scaffolds for Bone Tissue Engineering. Ann. Biomed. Eng. 2004, 32, 477–486. [Google Scholar] [CrossRef]
- Vehof, J.; van den Dolder, J.; de Ruijter, J.E.; Spauwen, P.H.M.; Jansen, J.A. Bone formation in CaP-coated and noncoated titanium fiber mesh. J. Biomed. Mater. Res. Part A Off. J. Soc. Biomater. 2003, 64, 417–426. [Google Scholar] [CrossRef]
- Franceschi, R.T.; Yang, S.; Rutherford, R.B.; Krebsbach, P.H.; Zhao, M.; Wang, D. Gene Therapy Approaches for Bone Regeneration. Cells Tissues Organs 2004, 176, 95–108. [Google Scholar] [CrossRef]
- Byers, B.A.; Guldberg, R.E.; García, A.J. Synergy between Genetic and Tissue Engineering: Runx2 Overexpression and in vitro Construct Development Enhance In Vivo Mineralization. Tissue Eng. 2004, 10, 1757–1766. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J.R.; Daluiski, A.; Einhorn, T. The role of growth factors in the repair of bone: Biology and clinical applications. JBJS 2002, 84, 1032–1044. [Google Scholar] [CrossRef] [PubMed]
- Bridwell, K.; Anderson, P.; Boden, S.; Vaccaro, A.; Wang, J. What’s New in Spine Surgery. Spine Surg. 2009, 99–111. [Google Scholar] [CrossRef]
- Zhao, B.; Katagiri, T.; Toyoda, H.; Takada, T.; Yanai, T.; Fukuda, T.; Chung, U.-I.; Koike, T.; Takaoka, K.; Kamijo, R. Heparin Potentiates the in Vivo Ectopic Bone Formation Induced by Bone Morphogenetic Protein-2. J. Biol. Chem. 2006, 281, 23246–23253. [Google Scholar] [CrossRef] [PubMed]
- Mundy, G.; Garrett, R.; Harris, S.; Chan, J.; Chen, D.; Rossini, G.; Boyce, B.; Zhao, M.; Gutierrez, G. Stimulation of Bone Formation in Vitro and in Rodents by Statins. Science 1999, 286, 1946–1949. [Google Scholar] [CrossRef] [PubMed]
- Civitelli, R. In Vitro and In Vivo effects of ipriflavone on bone formation and bone biomechanics. Calcif. Tissue Int. 1997, 61, S12–S14. [Google Scholar] [CrossRef]
- Zou, L.; Hu, L.; Pan, P.; Tarafder, S.; Du, M.; Geng, Y.; Xu, G.; Chen, L.; Chen, J.; Lee, C.H. Icariin-releasing 3D printed scaffold for bone regeneration. Compos. Part B Eng. 2022, 232, 109625. [Google Scholar] [CrossRef]
- Zhou, L.; Poon, C.C.-W.; Wong, K.-Y.; Cao, S.; Dong, X.; Zhang, Y.; Wong, M.-S. Icariin ameliorates estrogen-deficiency induced bone loss by enhancing IGF-I signaling via its crosstalk with non-genomic ERα signaling. Phytomedicine 2021, 82, 153413. [Google Scholar] [CrossRef]
- Xu, Y.; Jiang, Y.; Jia, B.; Wang, Y.; Li, T. Icariin stimulates osteogenesis and suppresses adipogenesis of human bone mesenchymal stem cells via miR-23a-mediated activation of the Wnt/β-catenin signaling pathway. Phytomedicine 2021, 85, 153485. [Google Scholar] [CrossRef]
- Dong, M.; Wu, S.; Xu, H.; Yu, X.; Wang, L.; Bai, H.; Niu, W. FBS-Derived Exosomes as a Natural Nano-Scale Carrier for Icariin Promote Osteoblast Proliferation. Front. Bioeng. Biotechnol. 2021, 9, 615920. [Google Scholar] [CrossRef]
- Li, X.; Xu, Y.; Li, H.; Jia, L.; Wang, J.; Liang, S.; Cai, A.; Tan, X.; Wang, L.; Wang, X.; et al. Verification of pain-related neuromodulation mechanisms of icariin in knee osteoarthritis. Biomed. Pharmacother. 2021, 144, 112259. [Google Scholar] [CrossRef] [PubMed]
- Makris, E.A.; Gomoll, A.H.; Malizos, K.N.; Hu, J.C.; Athanasiou, K.A. Repair and tissue engineering techniques for articular cartilage. Nat. Rev. Rheumatol. 2014, 11, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Singh, Y.P.; Bhardwaj, N.; Mandal, B.B. Potential of Agarose/Silk Fibroin Blended Hydrogel for in Vitro Cartilage Tissue Engineering. ACS Appl. Mater. Interfaces 2016, 8, 21236–21249. [Google Scholar] [CrossRef] [PubMed]
- Bian, L.; Hou, C.; Tous, E.; Rai, R.; Mauck, R.L.; Burdick, J.A. The influence of hyaluronic acid hydrogel crosslinking density and macromolecular diffusivity on human MSC chondrogenesis and hypertrophy. Biomaterials 2013, 34, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; Lin, S.; Zhang, K.; Dong, C.; Wu, T.; Huang, H.; Yan, X.; Zhang, L.; Li, G.; Bian, L. Sulfated hyaluronic acid hydrogels with retarded degradation and enhanced growth factor retention promote hMSC chondrogenesis and articular cartilage integrity with reduced hypertrophy. Acta Biomater. 2017, 53, 329–342. [Google Scholar] [CrossRef] [PubMed]
- Rey-Rico, A.; Madry, H.; Cucchiarini, M. Hydrogel-based controlled delivery systems for articular cartilage repair. BioMed Res. Int. 2016, 2016, 1215263. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Liu, Y.; He, L.; Wang, Q.; Wang, L.; Yuan, T.; Xiao, Y.; Fan, Y.; Zhang, X. Icariin conjugated hyaluronic acid/collagen hydrogel for osteochondral interface restoration. Acta Biomater. 2018, 74, 156–167. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, J.; Luo, Z.; Li, D.; Lu, J.; Wang, Q.; Xiao, Y.; Zhang, X. Development of an injectable thiolated icariin functionalized collagen/hyaluronic hydrogel to promote cartilage formation in vitro and in vivo. J. Mater. Chem. B 2019, 7, 2845–2854. [Google Scholar] [CrossRef]
- Yuan, T.; He, L.; Yang, J.; Zhang, L.; Xiao, Y.; Fan, Y.; Zhang, X. Conjugated icariin promotes tissue-engineered cartilage formation in hyaluronic acid/collagen hydrogel. Process. Biochem. 2015, 50, 2242–2250. [Google Scholar] [CrossRef]
- Lai, Y.; Cao, H.; Wang, X.; Chen, S.; Zhang, M.; Wang, N.; Yao, Z.; Dai, Y.; Xie, X.; Zhang, P. Porous composite scaffold incorporating osteogenic phytomolecule icariin for promoting skeletal regen-eration in challenging osteonecrotic bone in rabbits. Biomaterials 2018, 153, 1–13. [Google Scholar] [CrossRef]
- Kankala, R.K.; Lu, F.-J.; Liu, C.-G.; Zhang, S.-S.; Chen, A.-Z.; Wang, S.-B. Effect of Icariin on Engineered 3D-Printed Porous Scaffolds for Cartilage Repair. Materials 2018, 11, 1390. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.-J.; Cao, L.-G.; Wu, T.; Wang, D.-X.; Jin, D.; Jiang, S.; Zhang, Z.-Y.; Bi, L.; Pei, G.-X. The Dose-Effect of Icariin on the Proliferation and Osteogenic Differentiation of Human Bone Mesenchymal Stem Cells. Molecules 2011, 16, 10123–10133. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Yang, J.; Lu, J.; Xiao, Y.; Fan, Y.; Zhang, X. Preparation and characterization of a novel hyaluronic acid–icariin conjugate hydrogel. Mater. Lett. 2014, 136, 41–44. [Google Scholar] [CrossRef]
- Wu, Y.; Cao, L.; Xia, L.; Wu, Q.; Wang, J.; Wang, X.; Xu, L.; Zhou, Y.; Xu, Y.; Jiang, X. Evaluation of Osteogenesis and Angiogenesis of Icariin in Local Controlled Release and Systemic Delivery for Calvarial Defect in Ovariectomized Rats. Sci. Rep. 2017, 7, 1–14. [Google Scholar] [CrossRef]
- Wang, Z.; Li, K.; Sun, H.; Wang, J.; Fu, Z.; Liu, M. Icariin promotes stable chondrogenic differentiation of bone marrow mesenchymal stem cells in self-assembling peptide nanofiber hydrogel scaffolds. Mol. Med. Rep. 2018, 17, 8237–8243. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Ye, L.; Cai, X.; Li, Z.; Fan, Y.; Yang, F. Icariin-Loaded Hydrogel Regulates Bone Marrow Mesenchymal Stem Cell Chondrogenic Differentiation and Promotes Cartilage Repair in Osteoarthritis. Front. Bioeng. Biotechnol. 2022, 10. [Google Scholar] [CrossRef]
- Green, D.R. Means to an End: Apoptosis and Other Cell Death Mechanisms; Cold Spring Harbor Laboratory Press: New York, NY, USA, 2011. [Google Scholar]
- Tan, H.-L.; Chan, K.-G.; Pusparajah, P.; Saokaew, S.; Duangjai, A.; Lee, L.-H.; Goh, B.-H. Anti-Cancer Properties of the Naturally Occurring Aphrodisiacs: Icariin and Its Derivatives. Front. Pharmacol. 2016, 7, 191. [Google Scholar] [CrossRef]
- Wang, Q.; Hao, J.; Pu, J.; Zhao, L.; Lü, Z.; Hu, J.; Yu, Q.; Wang, Y.; Xie, Y.; Li, G. Icariin induces apoptosis in mouse MLTC-10 Leydig tumor cells through activation of the mitochon-drial pathway and down-regulation of the expression of piwil4. Int. J. Oncol. 2011, 39, 973–980. [Google Scholar]
- Li, J.; Jiang, K.; Zhao, F. Icariin regulates the proliferation and apoptosis of human ovarian cancer cells through microRNA-21 by targeting PTEN, RECK and Bcl-2. Oncol. Rep. 2015, 33, 2829–2836. [Google Scholar] [CrossRef]
- Sharma, B.; Fermanian, S.; Gibson, M.; Unterman, S.; Herzka, D.A.; Cascio, B.; Coburn, J.; Hui, A.Y.; Marcus, N.; Gold, G.E.; et al. Human Cartilage Repair with a Photoreactive Adhesive-Hydrogel Composite. Sci. Transl. Med. 2013, 5, 167ra6. [Google Scholar] [CrossRef]
- Fan, C.; Yang, Y.; Liu, Y.; Jiang, S.; Di, S.; Hu, W.; Ma, Z.; Li, T.; Zhu, Y.; Xin, Z.; et al. Icariin displays anticancer activity against human esophageal cancer cells via regulating endoplasmic reticulum stress-mediated apoptotic signaling. Sci. Rep. 2016, 6, 21145. [Google Scholar] [CrossRef] [PubMed]
- Song, L.; Chen, X.; Mi, L.; Liu, C.; Zhu, S.; Yang, T.; Luo, X.; Zhang, Q.; Lu, H.; Liang, X. Icariin-induced inhibition of SIRT6/NF-κB triggers redox mediated apoptosis and enhances anti-tumor immunity in triple-negative breast cancer. Cancer Sci. 2020, 111, 4242. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Gao, J.; Li, Q.; Ming, W.; Fu, Y.; Song, L.; Qin, J. Study on the regulatory mechanism and experimental verification of icariin for the treatment of ovarian cancer based on network pharmacology. J. Ethnopharmacol. 2020, 262, 113189. [Google Scholar] [CrossRef]
- Zhang, X.; He, C.; Xiang, G. Engineering nanomedicines to inhibit hypoxia-inducible Factor-1 for cancer therapy. Cancer Lett. 2022, 530, 110–127. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Huang, S.; Jiang, L.; Zhang, S.; Li, W.; Chen, Z.; Zhang, D. Expression of RECK and MMP-2 in salivary adenoid cystic carcinoma: Correlation with tumor progression and patient prognosis. Oncol. Lett. 2014, 7, 1549–1555. [Google Scholar] [CrossRef]
- Mao, H.; Zhang, L.; Wang, Y.; Li, X. Experimental studies of icariin on anticancer mechanism. J. Chin. Med. Mater. 2000, 23, 554–556. [Google Scholar]
- Wang, Y.; Dong, H.; Zhu, M.; Ou, Y.; Zhang, J.; Luo, H.; Luo, R.; Wu, J.; Mao, M.; Liu, X. Icariin exterts negative effects on human gastric cancer cell invasion and migration by vasodilator-stimulated phosphoprotein via Rac1 pathway. Eur. J. Pharmacol. 2010, 635, 40–48. [Google Scholar] [CrossRef]
- Liu, Z.-B.; Zhang, T.; Ye, X.; Sun, X.; Zhang, L.-L.; Wu, C.-J. Natural substances derived from herbs or plants are promising sources of anticancer agents against colorectal cancer via triggering apoptosis. J. Pharm. Pharmacol. 2021, 74, 162–178. [Google Scholar] [CrossRef]
- Zou, J.; Xu, M.; Li, F.; Wang, Y.; Li, X.; Yu, D.; Ma, Y.; Zhang, Y.; Sun, X. Icaritin alleviates docetaxel-induced skin injury by suppressing reactive oxygen species via estrogen receptors. Thorac. Cancer 2021, 13, 190–201. [Google Scholar] [CrossRef]
- Deng, J.; Wang, J.; Shi, J.; Li, H.; Lu, M.; Fan, Z.; Gu, Z.; Cheng, H. Tailoring the physicochemical properties of nanomaterials for immunomodulation. Adv. Drug Deliv. Rev. 2021, 180, 114039. [Google Scholar] [CrossRef]
- Liu, X.; Liu, Z.; Miao, Y.; Wang, L.; Yin, H. Sex hormone-like Effects of Icariin on T-cells immune modulation in spontaneously hypertensive rats. J. Ethnopharmacol. 2020, 269, 113717. [Google Scholar] [CrossRef] [PubMed]
- Catalano, A.; Iacopetta, D.; Ceramella, J.; Scumaci, D.; Giuzio, F.; Saturnino, C.; Aquaro, S.; Rosano, C.; Sinicropi, M.S. Multidrug Resistance (MDR): A Widespread Phenomenon in Pharmacological Therapies. Molecules 2022, 27, 616. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.T.; Carmeli, Y.; Falagas, M.T.; Giske, C.T.; Harbarth, S.; Hindler, J.T.; Kahlmeter, G.; Olsson-Liljequist, B. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Chen, W.; Qu, L.; Wu, J.; Si, J. Icaritin reverses multidrug resistance of HepG2/ADR human hepatoma cells via downregulation of MDR1 and P-glycoprotein expression. Mol. Med. Rep. 2013, 8, 1883–1887. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Wang, Y.; Ribeiro, C.F.; Manokaran, C.; Chang, H.; Von, T.; Rodrigues, S.; Cizmecioglu, O.; Jia, S.; Korpal, M.; et al. Blocking PI3K p110β Attenuates Development of PTEN-Deficient Castration-Resistant Prostate Cancer. Mol. Cancer Res. 2022, 20, 673–685. [Google Scholar] [CrossRef]
- Oberoi, H.S.; Nukolova, N.; Laquer, F.C.; Poluektova, L.; Alnouti, Y.; Yokohira, M.; Arnold, L.L.; Kabanov, A.; Cohen, S.M.; Bronich, T.K.; et al. Cisplatin-loaded core cross-linked micelles: Comparative pharmacokinetics, antitumor activity, and toxicity in mice. Int. J. Nanomed. 2012, 7, 2557–2571. [Google Scholar] [CrossRef]
- Launay-Vacher, V.; Rey, J.-B.; Isnard-Bagnis, C.; Deray, G.; Daouphars, M. Prevention of cisplatin nephrotoxicity: State of the art and recommendations from the Eu-ropean Society of Clinical Pharmacy Special Interest Group on Cancer Care. Cancer Chemother. Pharmacol. 2008, 61, 903–909. [Google Scholar] [CrossRef]
- Ma, Z.-n.; Liu, Z.; Wang, Z.; Ren, S.; Tang, S.; Wang, Y.-p.; Xiao, S.-y.; Chen, C.; Li, W. Supplementation of American ginseng berry extract mitigated cisplatin-evoked nephrotoxicity by suppressing ROS-mediated activation of MAPK and NF-κB signaling pathways. Food Chem. Toxicol. 2017, 110, 62–73. [Google Scholar] [CrossRef]
- Arivarasu, N.; Priyamvada, S.; Mahmood, R. Oral administration of caffeic acid ameliorates the effect of cisplatin on brush border membrane enzymes and antioxidant system in rat intestine. Exp. Toxicol. Pathol. 2013, 65, 21–25. [Google Scholar] [CrossRef]
- Van Angelen, A.A.; Glaudemans, B.; van der Kemp, A.W.; Hoenderop, J.G.; Bindels, R.J. Cisplatin-induced injury of the renal distal convoluted tubule is associated with hypomagnesaemia in mice. Nephrol. Dial. Transplant. 2012, 28, 879–889. [Google Scholar] [CrossRef]
- Ma, P.; Zhang, S.; Su, X.; Qiu, G.; Wu, Z. Protective effects of icariin on cisplatin-induced acute renal injury in mice. Am. J. Transl. Res. 2015, 7, 2105–2114. [Google Scholar] [PubMed]
- Jiang, S.; Chang, H.; Deng, S.; Fan, D. Icariin enhances the chemosensitivity of cisplatin-resistant ovarian cancer cells by suppressing au-tophagy via activation of the AKT/mTOR/ATG5 pathway. Int. J. Oncol. 2019, 54, 1933–1942. [Google Scholar] [PubMed]
- Beutler, J.A. Natural Products as a Foundation for Drug Discovery. Curr. Protoc. Pharmacol. 2019, 86, e67. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.-J.; Xin, Z.-C.; Xin, H.; Yuan, Y.-M.; Tian, L.; Guo, Y.-L. Effects of icariin on erectile function and expression of nitric oxide synthase isoforms in castrated rats. Asian J. Androl. 2005, 7, 381–388. [Google Scholar] [CrossRef]
- Fang, J.; Zhang, Y. Icariin, an Anti-atherosclerotic Drug from Chinese Medicinal Herb Horny Goat Weed. Front. Pharmacol. 2017, 8, 734. [Google Scholar] [CrossRef]
- Shen, C.-Y.; Jiang, J.-G.; Yang, L.; Wang, D.-W.; Zhu, W. Anti-ageing active ingredients from herbs and nutraceuticals used in traditional Chinese medicine: Pharmacological mechanisms and implications for drug discovery. Br. J. Pharmacol. 2016, 174, 1395–1425. [Google Scholar] [CrossRef]
- Chen, Y.; Sun, T.; Wu, J.; Kalionis, B.; Zhang, C.; Yuan, D.; Huang, J.; Cai, W.; Fang, H.; Xia, S. Icariin intervenes in cardiac inflammaging through upregulation of SIRT6 enzyme activity and inhibition of the NF-kappa B pathway. BioMed Res. Int. 2015, 2015, 895976. [Google Scholar] [CrossRef]
- Shen, X.; He, H. Effects of icariin on expression of glucose regulated protein 78 in vascular smooth muscle cell in-duced by homocysteine. China J. Chin. Mater. Med. 2009, 34, 1964–1967. [Google Scholar]
- Yang, H.; Yan, L.; Qian, P.; Duan, H.; Wu, J.; Li, B.; Wang, S. Icariin Inhibits Foam Cell Formation by Down-Regulating the Expression of CD36 and Up-Regulating the Expression of SR-BI. J. Cell. Biochem. 2014, 116, 580–588. [Google Scholar] [CrossRef]
- Xu, C.-Q.; Liu, B.-J.; Wu, J.-F.; Xu, Y.-C.; Duan, X.-H.; Cao, Y.-X.; Dong, J.-C. Icariin attenuates LPS-induced acute inflammatory responses: Involvement of PI3K/Akt and NF-κB signaling pathway. Eur. J. Pharmacol. 2010, 642, 146–153. [Google Scholar] [CrossRef]
- Calderon-Garcidueñas, A.L.; Duyckaerts, C. Alzheimer disease. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2018; pp. 325–337. [Google Scholar]
- Guo, J.; Li, F.; Wu, Q.; Gong, Q.; Lu, Y.; Shi, J. Protective effects of icariin on brain dysfunction induced by lipopolysaccharide in rats. Phytomedicine 2010, 17, 950–955. [Google Scholar] [CrossRef] [PubMed]
- Dai, M.; Chen, B.; Wang, X.; Gao, C.; Yu, H. Icariin enhance mild hypothermia-induced neuroprotection via inhibiting the activation of NF-κB in experimental ischemic stroke. Metab. Brain Dis. 2021, 36, 1179–1790. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Rong, Y.; Luo, L. Neuroprotective effects of icariin in neonatal hypoxia-ischemic brain damage via its anti-apoptotic property. Child’s Nerv. Syst. 2020, 37, 39–46. [Google Scholar] [CrossRef]
- Zou, X.; Feng, X.; Fu, Y.; Zheng, Y.; Ma, M.; Wang, C.; Zhang, Y. Icariin Attenuates Amyloid-β (Aβ)-Induced Neuronal Insulin Resistance Through PTEN Downregulation. Front. Pharmacol. 2020, 11, 880. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, Y.; Shi, P.; Liu, Y.; Li, T.; Liu, S.; Wang, C.; Wang, L.; Cao, Y. Icariin treatment reduces blood glucose levels in type 2 diabetic rats and protects pancreatic function. Exp. Ther. Med. 2020, 19, 2690–2696. [Google Scholar] [CrossRef]
- Qiao, C.; Wang, H.; Song, Z.; Ding, Y.; Tao, J.; Aa, J.; Ding, X. Icariin Attenuates Diabetic Cardiomyopathy and Downregulates Extracellular Matrix Proteins in Heart Tissue of Type 2 Diabetic Rats. Pharmacology 2020, 105, 576–585. [Google Scholar] [CrossRef]
- Qi, C.; Shao, Y.; Liu, X.; Wang, D.; Li, X. The cardioprotective effects of icariin on the isoprenaline-induced takotsubo-like rat model: Involvement of reactive oxygen species and the TLR4/NF-κB signaling pathway. Int. Immunopharmacol. 2019, 74, 105733. [Google Scholar] [CrossRef]
- Li, N.; Wang, J.; Wang, X.; Sun, J.; Li, Z. Icariin exerts a protective effect against d-galactose induced premature ovarian failure via promoting DNA damage repair. Biomed. Pharmacother. 2019, 118, 109218. [Google Scholar] [CrossRef]
- Ni, G.; Zhang, X.; Afedo, S.Y.; Rui, R. Evaluation of the protective effects of icariin on nicotine-induced reproductive toxicity in male mouse—A pilot study. Reprod. Biol. Endocrinol. 2020, 18, 1–8. [Google Scholar] [CrossRef]
- Wang, J.-L.; Liu, B.; Zhang, C.; Wang, X.-M.; Zhen, D.; Huang, X.-M.; Chen, W.; Gao, J.-M. Effects of icariin on ovarian function in d-galactose-induced aging mice. Theriogenology 2018, 125, 157–167. [Google Scholar] [CrossRef]
- Song, L.; Liu, C.; Zhu, S.; Chen, H.; Zhang, Q. Icariin Suppresses Proliferation and Metastasis and Enhances Antitumor Immunity in Triple-Negative Breast Cancer via SIRT6/NF-κB Signaling Pathway. Authorea Preprints. 2020. Available online: https://www.authorea.com/users/314916/articles/445270-icariin-suppresses-proliferation-and-metastasis-and-enhances-antitumor-immunity-in-triple-negative-breast-cancer-via-sirt6-nf-%CE%BAb-signaling-pathway (accessed on 1 January 2023).
- Wu, X.; Kong, W.; Qi, X.; Wang, S.; Chen, Y.; Zhao, Z.; Wang, W.; Lin, X.; Lai, J.; Yu, Z.; et al. Icariin induces apoptosis of human lung adenocarcinoma cells by activating the mitochondrial apoptotic pathway. Life Sci. 2019, 239, 116879. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Seo, J.H.; Lee, K.Y.; Park, B. Icariin sensitizes human colon cancer cells to TRAIL-induced apoptosis via ERK-mediated upregulation of death receptors. Int. J. Oncol. 2020, 56, 821–834. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Wu, P.-Y.; Zhang, Z.-F.; Qin, F.-W.; Tang, W.; Liu, D.-H. Icariin interferes with TDP43-induced inflammatory factor secretion and inhibits the JNK and p38 MAPK signaling pathway in vitro. Arch. Med Sci. 2021. [Google Scholar] [CrossRef]
- Wang, P.; Meng, Q.; Wang, W.; Zhang, S.; Xiong, X.; Qin, S.; Zhang, J.; Li, A.; Liu, Z. Icariin inhibits the inflammation through down-regulating NF-κB/HIF-2α signal pathways in chondrocytes. Biosci. Rep. 2020, 40, BSR20203107. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.A.; Chen, C.-M.; Guan, S.-S.; Chiang, C.-K.; Wu, C.-T.; Liu, S.-H. The antifibrotic and anti-inflammatory effects of icariin on the kidney in a unilateral ureteral obstruction mouse model. Phytomedicine 2019, 59, 152917. [Google Scholar] [CrossRef] [PubMed]
- Seyedi, Z.; Hashemzadeh, M.R.; Colagar, A.H.; Jaafari, M.R. Signal transducer and activator of transcription 3 downregulation in J774A.1 cell line as a model of M2 macrophages in tumor microenvironment. J. Cancer Res. Ther. 2018, 14, 1121–1125. [Google Scholar] [CrossRef] [PubMed]
- Jinushi, M.; Baghdadi, M.; Chiba, S.; Yoshiyama, H. Regulation of cancer stem cell activities by tumor-associated macrophages. Am. J. Cancer Res. 2012, 2, 529–539. [Google Scholar]
- Aramini, B.; Masciale, V.; Grisendi, G.; Banchelli, F.; D’Amico, R.; Maiorana, A.; Morandi, U.; Dominici, M.; Haider, K.H. Cancer stem cells and macrophages: Molecular connections and future perspectives against cancer. Oncotarget 2021, 12, 230–250. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).