Adhesive Property of 3D-Printed PEEK Abutments: Effects of Surface Treatment and Temporary Crown Material on Shear Bond Strength
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
2.2. Surface Treatment
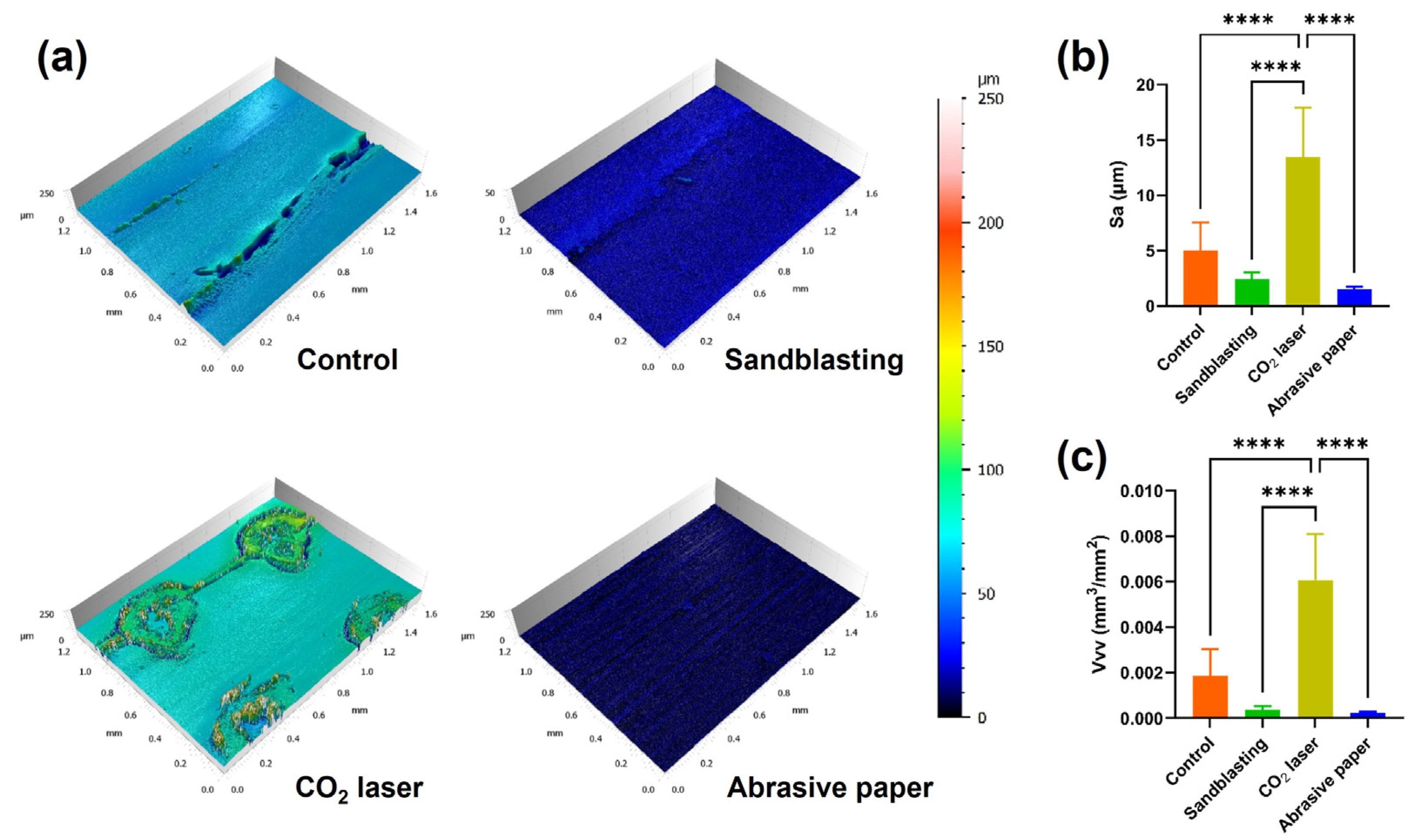
2.3. Surface Characterization
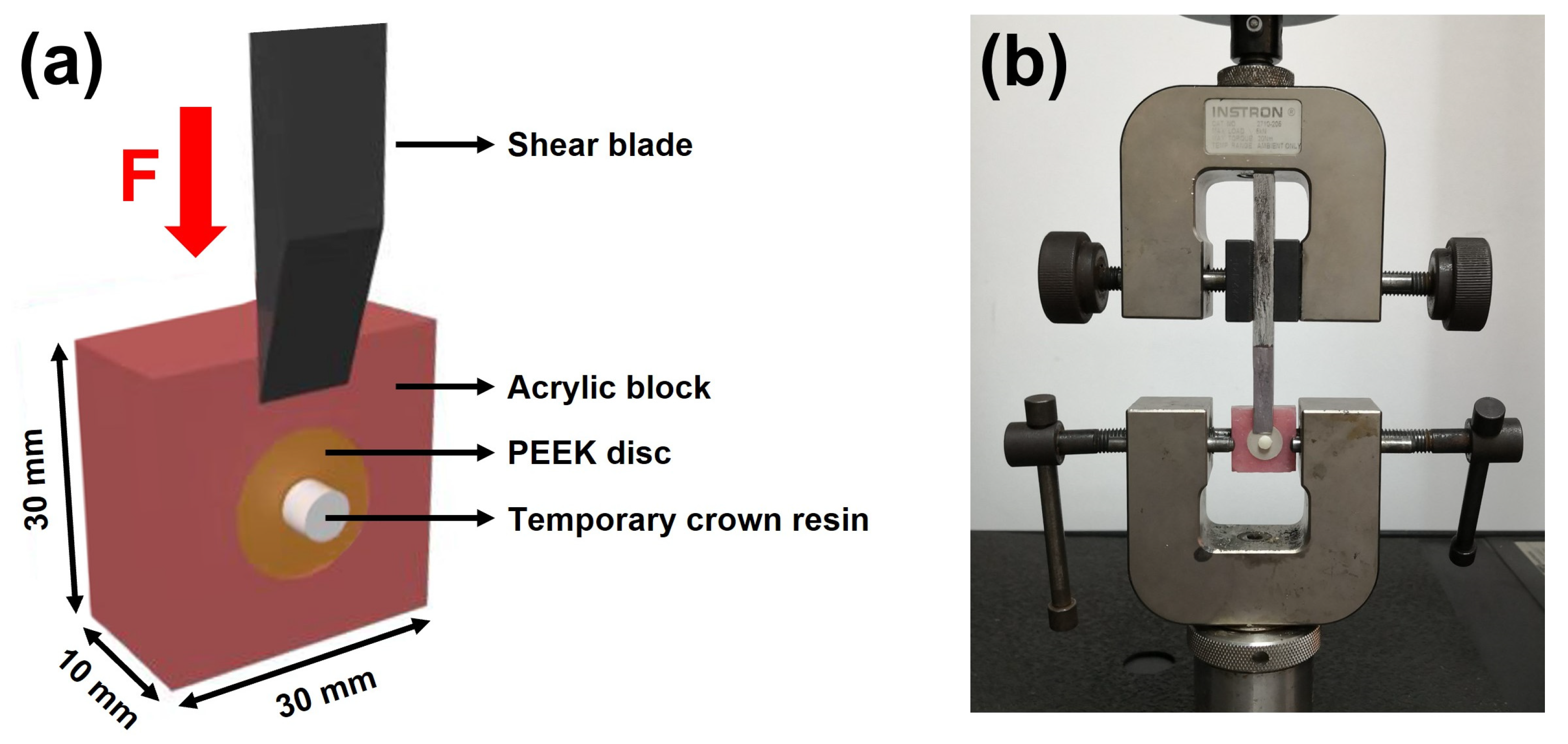
2.4. Shear Bond Strength Test
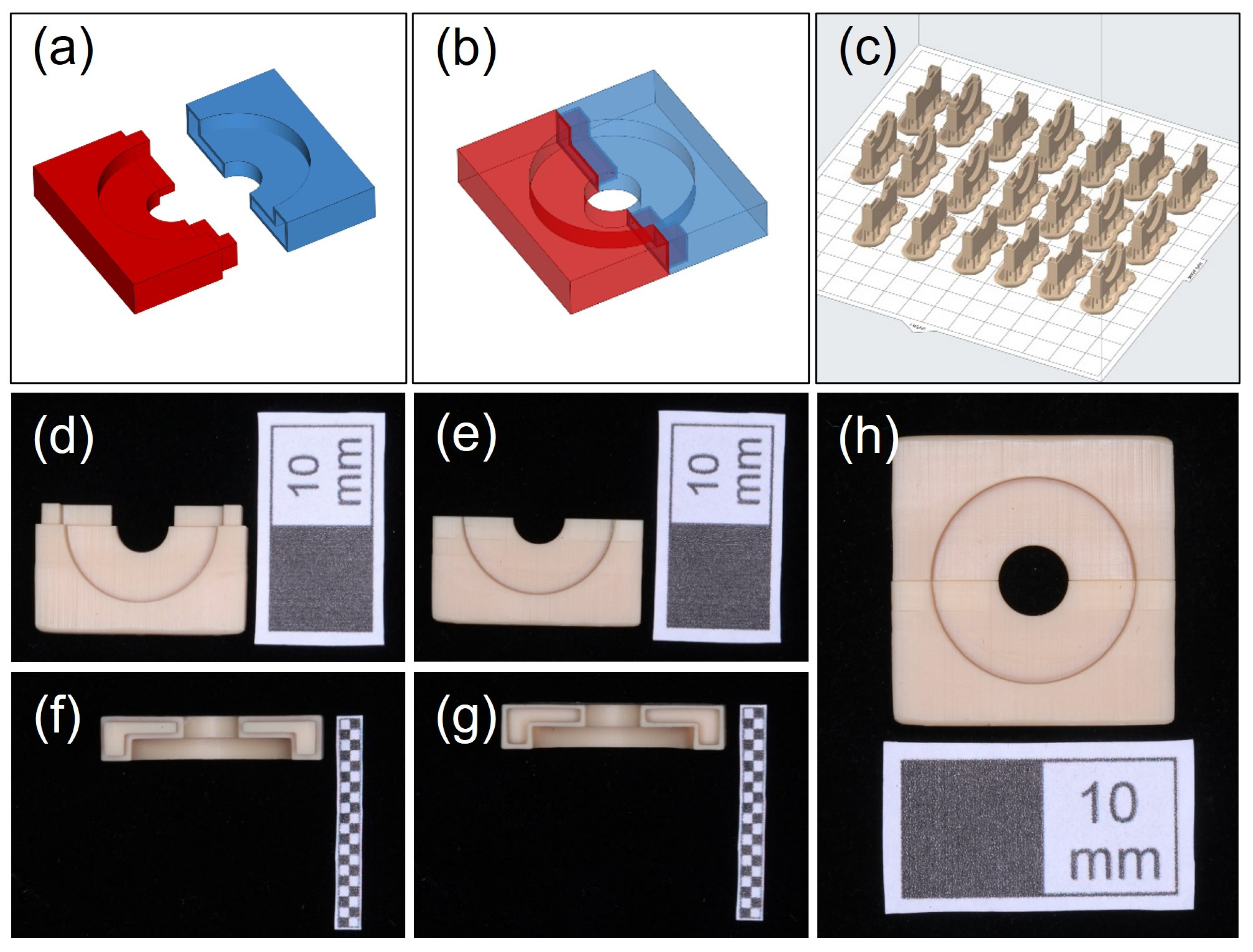
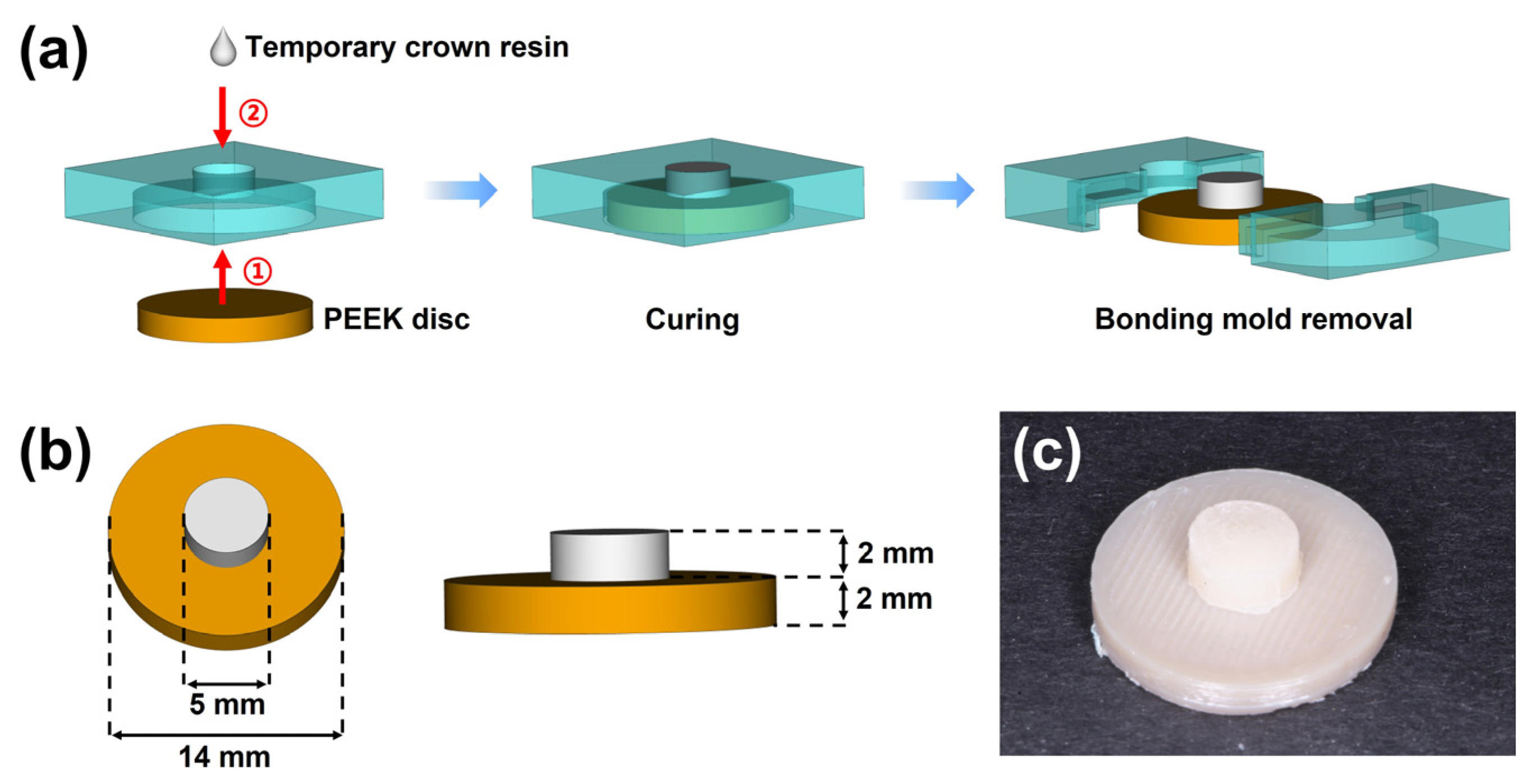
2.4.1. Fabrication of Bonding Mold
2.4.2. Preparation of the Bonding Specimen
2.4.3. Shear Bond Strength Measurement
2.5. Statistical Analysis
3. Results
3.1. Surface Morphology
3.2. Roughness Measurement
3.3. Shear Bond Strength
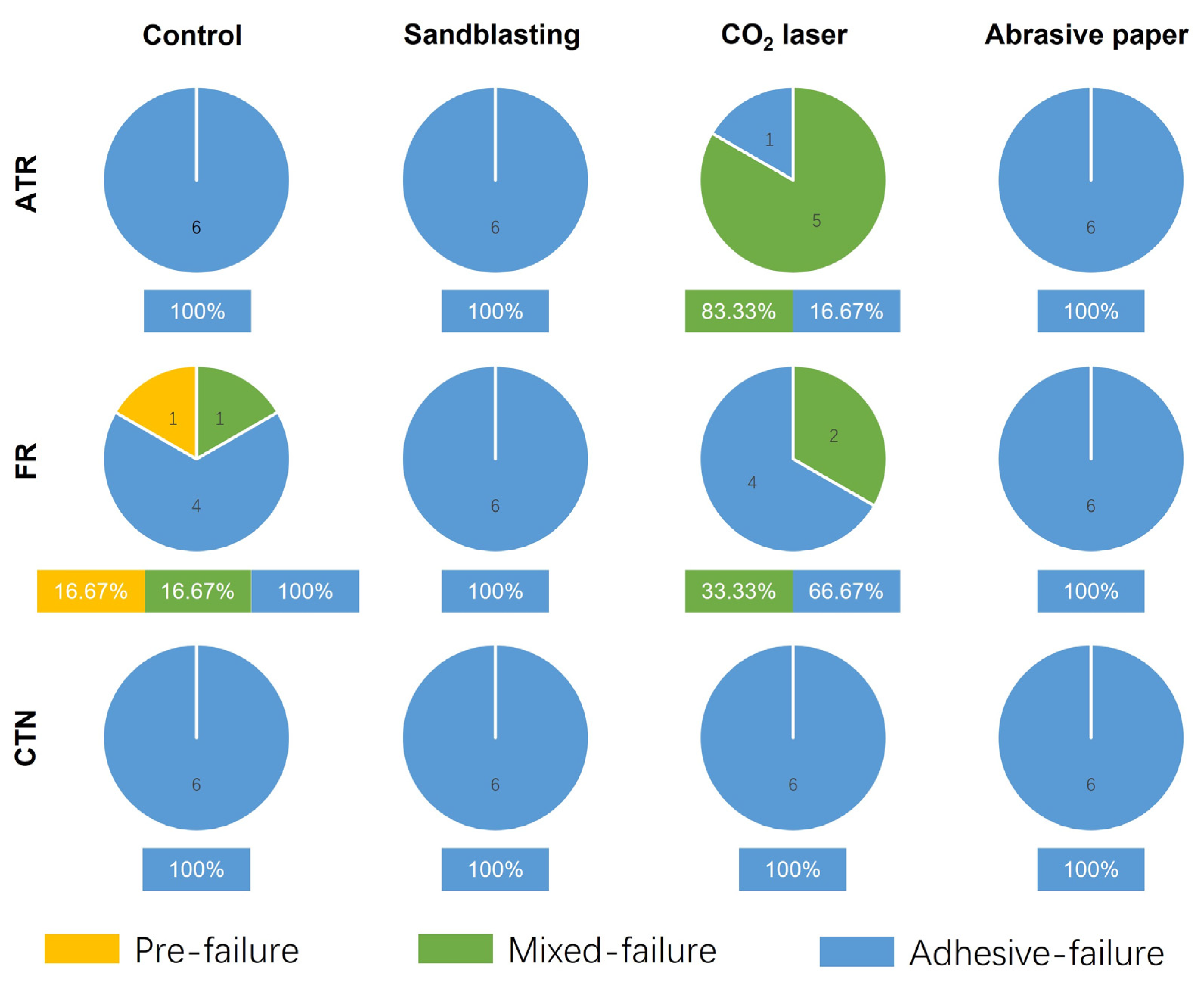
3.4. Failure Mode Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cosyn, J.; Eghbali, A.; De Bruyn, H.; Collys, K.; Cleymaet, R.; De Rouck, T. Immediate Single-Tooth Implants in the Anterior Maxilla: 3-Year Results of a Case Series on Hard and Soft Tissue Response and Aesthetics: Immediate Single-Tooth Implants. J. Clin. Periodontol. 2011, 38, 746–753. [Google Scholar] [CrossRef] [PubMed]
- den Hartog, L.; Huddleston Slater, J.J.R.; Vissink, A.; Meijer, H.J.A.; Raghoebar, G.M. Treatment Outcome of Immediate, Early and Conventional Single-Tooth Implants in the Aesthetic Zone: A Systematic Review to Survival, Bone Level, Soft-Tissue, Aesthetics and Patient Satisfaction. J. Clin. Periodontol. 2008, 35, 1073–1086. [Google Scholar] [CrossRef] [PubMed]
- Chee, W.W.L. Provisional Restorations in Soft Tissue Management around Dental Implants: Chee. Periodontology 2000 2001, 27, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Abichandani, S.; Nadiger, R.; Kavlekar, A. Abutment Selection, Designing, and Its Influence on the Emergence Profile: A Comprehensive Review. Eur. J. Prosthodont. 2013, 1, 1. [Google Scholar] [CrossRef]
- Mirza, J.; Robertson, G. Vital Guide to Dental Implants. Vital 2008, 6, 19–22. [Google Scholar] [CrossRef]
- Hartlev, J.; Kohberg, P.; Ahlmann, S.; Andersen, N.T.; Schou, S.; Isidor, F. Patient Satisfaction and Esthetic Outcome after Immediate Placement and Provisionalization of Single-Tooth Implants Involving a Definitive Individual Abutment. Clin. Oral Implant. Res. 2014, 25, 1245–1250. [Google Scholar] [CrossRef]
- Xu, Y.; Huang, H.; Wu, M.; Tian, Y.; Wan, Q.; Shi, B.; Hu, T.; Spintzyk, S. Rapid Additive Manufacturing of a Superlight Obturator for Large Oronasal Fistula in Pediatric Patient. Laryngoscope 2022, lary.30352. [Google Scholar] [CrossRef]
- Li, P.; Krämer-Fernandez, P.; Klink, A.; Xu, Y.; Spintzyk, S. Repairability of a 3D Printed Denture Base Polymer: Effects of Surface Treatment and Artificial Aging on the Shear Bond Strength. J. Mech. Behav. Biomed. Mater. 2021, 114, 104227. [Google Scholar] [CrossRef]
- Rosentritt, M.; Raab, P.; Hahnel, S.; Stöckle, M.; Preis, V. In-Vitro Performance of CAD/CAM-Fabricated Implant-Supported Temporary Crowns. Clin. Oral Invest. 2017, 21, 2581–2587. [Google Scholar] [CrossRef]
- Rayyan, M.M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparison of Interim Restorations Fabricated by CAD/CAM with Those Fabricated Manually. J. Prosthet. Dent. 2015, 114, 414–419. [Google Scholar] [CrossRef]
- Xu, Y.; Unkovskiy, A.; Klaue, F.; Rupp, F.; Geis-Gerstorfer, J.; Spintzyk, S. Compatibility of a Silicone Impression/Adhesive System to FDM-Printed Tray Materials—A Laboratory Peel-off Study. Materials 2018, 11, 1905. [Google Scholar] [CrossRef] [PubMed]
- van Noort, R. The Future of Dental Devices Is Digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Devine, J.N. PEEK Biomaterials in Trauma, Orthopedic, and Spinal Implants. Biomaterials 2007, 28, 4845–4869. [Google Scholar] [CrossRef] [PubMed]
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. PEEK Polymer’s Properties and Its Use in Prosthodontics. A Review. Stomatologija 2018, 20, 54–58. [Google Scholar]
- Katzer, A.; Marquardt, H.; Westendorf, J.; Wening, J.V.; von Foerster, G. Polyetheretherketone--Cytotoxicity and Mutagenicity in Vitro. Biomaterials 2002, 23, 1749–1759. [Google Scholar] [CrossRef]
- Escobar, M.; Henriques, B.; Fredel, M.C.; Silva, F.S.; Özcan, M.; Souza, J.C.M. Adhesion of PEEK to Resin-Matrix Composites Used in Dentistry: A Short Review on Surface Modification and Bond Strength. J. Adhes. Sci. Technol. 2019, 34, 1241–1252. [Google Scholar] [CrossRef]
- Zhou, L.; Qian, Y.; Zhu, Y.; Liu, H.; Gan, K.; Guo, J. The Effect of Different Surface Treatments on the Bond Strength of PEEK Composite Materials. Dent. Mater. 2014, 30, e209–e215. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Jordan, P.; Schmidlin, P.R.; Roos, M.; Eichberger, M.; Gernet, W.; Keul, C. PEEK Surface Treatment Effects on Tensile Bond Strength to Veneering Resins. J. Prosthet. Dent. 2014, 112, 1278–1288. [Google Scholar] [CrossRef]
- Gama, L.T.; Duque, T.M.; Özcan, M.; Philippi, A.G.; Mezzomo, L.A.M.; Gonçalves, T.M.S.V. Adhesion to High-Performance Polymers Applied in Dentistry: A Systematic Review. Dent. Mater. 2020, 36, e93–e108. [Google Scholar] [CrossRef]
- Han, X.; Sharma, N.; Spintzyk, S.; Zhou, Y.; Xu, Z.; Thieringer, F.M.; Rupp, F. Tailoring the Biologic Responses of 3D Printed PEEK Medical Implants by Plasma Functionalization. Dent. Mater. 2022, 38, 1083–1098. [Google Scholar] [CrossRef]
- Spintzyk, S.; Yamaguchi, K.; Sawada, T.; Schille, C.; Schweizer, E.; Ozeki, M.; Geis-Gerstorfer, J. Influence of the Conditioning Method for Pre-Sintered Zirconia on the Shear Bond Strength of Bilayered Porcelain/Zirconia. Materials 2016, 9, 765. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Runzi, M.; Gilchrist, M.; Gong, H. Mechanical Properties of High-Performance Plastic Polyether-Ether-Ketone (PEEK) Printed by Fused Deposition Modeling; University of Texas at Austin: Austin, TX, USA, 2021. [Google Scholar] [CrossRef]
- Xu, Y.; Xu, Y.; Zhang, W.; Li, M.; Wendel, H.-P.; Geis-Gerstorfer, J.; Li, P.; Wan, G.; Xu, S.; Hu, T. Biodegradable Zn-Cu-Fe Alloy as a Promising Material for Craniomaxillofacial Implants: An in Vitro Investigation into Degradation Behavior, Cytotoxicity, and Hemocompatibility. Front. Chem. 2022, 10, 860040. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Yang, R.; Shi, B.; Xu, Y.; Huang, H. Obturator Manufacturing for Oronasal Fistula after Cleft Palate Repair: A Review from Handicraft to the Application of Digital Techniques. JFB 2022, 13, 251. [Google Scholar] [CrossRef] [PubMed]
- Stansbury, J.W.; Idacavage, M.J. 3D Printing with Polymers: Challenges among Expanding Options and Opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Hohenstein, S.; Bergweiler, G.; Lukas, G.; Krömer, V.; Otten, T. Decision Basis for Multi-Directional Path Planning for Post-Processing Reduction in Material Extrusion. Prod. Eng. 2021, 15, 457–466. [Google Scholar] [CrossRef]
- Witteman, W.J. The CO2 Laser; Softcover Reprint of the Original 1st ed. 1987; Springer: Berlin, Germany, 2013; ISBN 978-3-662-13617-1. [Google Scholar]
- Omi, T.; Numano, K. The Role of the CO2 Laser and Fractional CO2 Laser in Dermatology. Laser Ther. 2014, 23, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Świderska, J.; Czech, Z.; Kowalczyk, A. Polymerization Shrinkage by Investigation of Uv Curable Dental Restorative Composites Containing Multifunctional Methacrylates. Pol. J. Chem. Technol. 2013, 15, 81–85. [Google Scholar] [CrossRef]
- Wenzel, R.N. Resistance of solid surfaces to wetting by water. Ind. Eng. Chem. 1936, 28, 988–994. [Google Scholar] [CrossRef]
- Çulhaoğlu, A.K.; Özkır, S.E.; Şahin, V.; Yılmaz, B.; Kılıçarslan, M.A. Effect of Various Treatment Modalities on Surface Characteristics and Shear Bond Strengths of Polyetheretherketone-Based Core Materials. J. Prosthodont. 2020, 29, 136–141. [Google Scholar] [CrossRef]
- Akkan, C.K.; Hammadeh, M.; Brück, S.; Park, H.W.; Veith, M.; Abdul-Khaliq, H.; Aktas, C. Plasma and Short Pulse Laser Treatment of Medical Grade PEEK Surfaces for Controlled Wetting. Mater. Lett. 2013, 109, 261–264. [Google Scholar] [CrossRef]
- Gheisarifar, M.; Thompson, G.A.; Drago, C.; Tabatabaei, F.; Rasoulianboroujeni, M. In Vitro Study of Surface Alterations to Polyetheretherketone and Titanium and Their Effect upon Human Gingival Fibroblasts. J. Prosthet. Dent. 2021, 125, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Riveiro, A.; Soto, R.; Comesaña, R.; Boutinguiza, M.; del Val, J.; Quintero, F.; Lusquiños, F.; Pou, J. Laser Surface Modification of PEEK. Appl. Surf. Sci. 2012, 258, 9437–9442. [Google Scholar] [CrossRef]
- Dupuis, A.; Ho, T.H.; Fahs, A.; Lafabrier, A.; Louarn, G.; Bacharouche, J.; Airoudj, A.; Aragon, E.; Chailan, J.-F. Improving Adhesion of Powder Coating on PEEK Composite: Influence of Atmospheric Plasma Parameters. Appl. Surf. Sci. 2015, 357, 1196–1204. [Google Scholar] [CrossRef]
- Kuscu, E.; Klink, A.; Spintzyk, S.; Kraemer Fernandez, P.; Huettig, F. Bonding Interface and Repairability of 3D-Printed Intraoral Splints: Shear Bond Strength to Current Polymers, with and without Ageing. Materials 2021, 14, 3935. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Keul, C.; Beuer, F.; Roos, M.; Schmidlin, P.R. Tensile Bond Strength of Veneering Resins to PEEK: Impact of Different Adhesives. Dent. Mater. J. 2013, 32, 441–448. [Google Scholar] [CrossRef]
- Mair, L.; Padipatvuthikul, P. Variables Related to Materials and Preparing for Bond Strength Testing Irrespective of the Test Protocol. Dent. Mater. 2010, 26, e17–e23. [Google Scholar] [CrossRef]





| Product Name | Manufacturer, City, Country | Lot No. | Main Component |
|---|---|---|---|
| Artificial teeth resin | Xin Shi Ji, Shanghai, China | 20211118 | Methyl methacrylate |
| 3M™ Filtek™ Supreme Flowable Restorative | 3M, St. Paul, MN, USA | NF20341 | Dimethacrylates |
| Cool Temp NATURAL | Coltène/Whaledent AG, Altstätten, Switzerland | L25817 | Trimethylolpropane trimethacrylate, dimethacrylates |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, D.; Han, X.; Luo, F.; Thieringer, F.M.; Xu, Y.; Ou, G.; Spintzyk, S. Adhesive Property of 3D-Printed PEEK Abutments: Effects of Surface Treatment and Temporary Crown Material on Shear Bond Strength. J. Funct. Biomater. 2022, 13, 288. https://doi.org/10.3390/jfb13040288
Wang D, Han X, Luo F, Thieringer FM, Xu Y, Ou G, Spintzyk S. Adhesive Property of 3D-Printed PEEK Abutments: Effects of Surface Treatment and Temporary Crown Material on Shear Bond Strength. Journal of Functional Biomaterials. 2022; 13(4):288. https://doi.org/10.3390/jfb13040288
Chicago/Turabian StyleWang, Dingjie, Xingting Han, Feng Luo, Florian M. Thieringer, Yichen Xu, Guomin Ou, and Sebastian Spintzyk. 2022. "Adhesive Property of 3D-Printed PEEK Abutments: Effects of Surface Treatment and Temporary Crown Material on Shear Bond Strength" Journal of Functional Biomaterials 13, no. 4: 288. https://doi.org/10.3390/jfb13040288
APA StyleWang, D., Han, X., Luo, F., Thieringer, F. M., Xu, Y., Ou, G., & Spintzyk, S. (2022). Adhesive Property of 3D-Printed PEEK Abutments: Effects of Surface Treatment and Temporary Crown Material on Shear Bond Strength. Journal of Functional Biomaterials, 13(4), 288. https://doi.org/10.3390/jfb13040288







