Abstract
To date, risk factors for temporomandibular joint (TMJ) sounds are still not completely understood, and anatomical factors are suspected to influence their occurrence. This study aimed to evaluate the impact of body constitution on temporomandibular joint sounds of adolescents. 10- to 18-year-old participants of the LIFE Child Study were examined for TMJ sounds, and physical parameters such as body height, body weight, and general laxity of joints were measured. Odds ratios (OR) for associations of TMJ sounds and standard deviation scores (SDS) of body height and body weight were calculated by using binary logistic regression, including cofactors such as age and number of hypermobile joints. The OR for TMJ sounds and SDS of body height was 1.28 (95% confidence interval (CI) 1.06; 1.56) in females when the age-adjusted height value was above 0. SDS of body weight indicated significant ORs for TMJ sounds in males with values of 0.81 (95% CI 0.70; 0.94). No correlation was detected for SDS values and TMJ crepitus. Tall female adolescents seem to be more prone to TMJ clicking sounds, while their occurrence seems less likely in male adolescents with higher body weight.
Keywords:
body constitution; body height; body weight; children; gender; temporomandibular disorders 1. Introduction
Temporomandibular joint (TMJ) sounds are categorized as cardinal symptoms of temporomandibular disorders (TMD) [1]. According to a systematic review, 14.0% of the children or adolescents had clinical TMJ sounds [2], while a current investigation detected an even higher percentage—up to 31.9%—for German adolescents [3]. The gap between prevalence values might be due to the ethnicity of the participants, as previous investigations revealed that anatomical structures, e.g., the angulation of the articular eminence, varies between different ethnical groups [4]. In general, differences in the growth of the maxilla and the mandible in adolescents might lead to an incongruence of the condyle and the articular eminence, and consequently foster TMJ sounds that were, for example, caused by disc displacements (DD) [5,6]. Therefore, the age of young patients seems to be an influencing factor for joint sounds [6]. Moreover, sex [7,8,9] and psychosocial characteristics [10] might be risk factors for TMJ sounds, yet their influence is controversially discussed. A recent investigation observed that psychosocial factors barely influence DD, and it described that some habits like pen biting can act as a risk factor for DD in adolescents [6]. Another reason for TMJ sounds might be the hypermobility of the TMJ. The latter can be induced by a general joint laxity, which is very common in younger patients, and was observed as generalized hypermobility (≥4 joints) in 21.3% of the 10- to 18-year-olds. This mobility usually decreases during pubertal development, however less in girls than in boys, which can be explained by hormonal effects [11]. In most cases, TMJ sounds affect adolescents only minimally, but if painful, the TMJ should be treated, since an impaired oral health-related quality of life and limitations of the jaw movements can occur [12,13]. All in all, the risk factors for TMJ sounds are still not fully understood, and anatomical causes seem to affect changes in the TMJ, which could lead to TMJ sounds. Thus, an influence of the body growth on the onset of TMJ sounds might be possible, and age-dependent tall adolescents might be prone to disc displacement due to rapid growth, whereas a shorter body height might be protective. However, the influence of the body constitution has never been thoroughly investigated.
The present study aims to evaluate the influence of the age-dependent body height and body weight on temporomandibular joint sounds in adolescents. The working hypothesis of this investigation was that the occurrence of TMJ sounds do not depend on the individual body constitutions.
2. Material and Methods
A cross-sectional sample of the LIFE Child Study, aged 10 to 18 years, was recruited to investigate physical parameters as well as characteristics of the masticatory and dental system of the participants, the procedure has already been described in detail elsewhere [3,14,15]. Temporomandibular joint sounds were examined by trained dentists who used the examination form of the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) [16]. This part of the study was approved by the local Ethical Committee (354-10-13122010). For statistical purposes, all reproducible TMJ sounds during vertical and excursive jaw movements were summarized as clinical TMJ sounds [11]. Moreover, the TMJ sounds were separately analyzed, for clicking sounds on the one hand and for crepitus on the other. Physical parameters were examined by calibrated investigators that measured body height, body weight, and general laxity of joints (GJL). According to the reference values for German adolescents, published by Kromeyer-Hauschild et al., standard deviation scores (SDS) were calculated that comprised age- and sex-adapted values for body height and weight [17]. A positive value is comparable to a relatively tall or heavy, and a negative value to a short or thin adolescent, respectively [17]. The Beighton classification was utilized to identify GJL, and it included the examination of nine joints [11,18]. For statistical analysis (SPSS 24, IBM, Armonk, NY, USA), a normal distribution was observed for SDS height values (Shapiro–Wilk test: p = 0.132), while age, SDS weight values, and the number of hypermobile joints were not normally distributed (Shapiro–Wilk tests: p ≤ 0.001). Consequently, unpaired t-tests (normal distribution) and Mann–Whitney U tests (no normal distribution) were utilized, as well as binary logistic regression, to reveal odds ratios (OR) assuming a level of significance of p < 0.050. By using binary regression, the odds ratios for TMJ sounds, TMJ clicking, and TMJ clicking in comparison to the age-adjusted height (SDS height) and age-adjusted weight (SDS weight) values were determined, and the potentially confounding effects of hypermobile joints (GJL) were included. The latter were not age-adjusted; thus, age was included as a confounding factor for GJL as well.
3. Results
In total, 1116 adolescents (10 to 18 years, 12.9 ± 2.3 years, 51.4% female) were enrolled in the study. For 104 participants, no DC/TMD examination could be performed. For seven participants, no body height was measured, and nine measurements of body weight were not performed.
The comparison of SDS values for body height or body weight of the participants did not yield statistically significant differences for adolescents with or without TMJ sounds (Table 1). A TMJ clicking was observed in 309, and a crepitus in 20 adolescents. Sex-dependent pyramid histograms revealed that TMJ sounds might be correlated to SDS height values in females (Figure 1) and to SDS weight in males (Figure 2).

Table 1.
Means and standard deviation (SD) of physical variables in relation to temporomandibular joint (TMJ) sounds (both sexes); SDS: standard deviation scores, CI: confidence interval, n.s.: not significant.
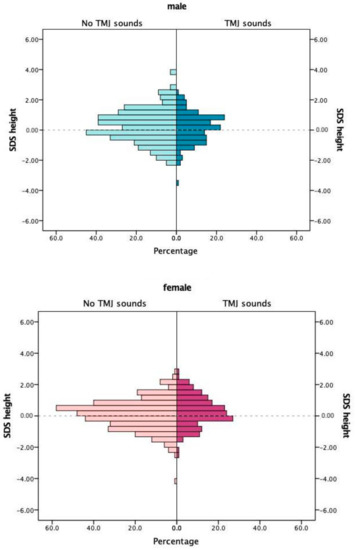
Figure 1.
Standard deviation scores (SDS) of body height in relation to temporomandibular joint sounds.
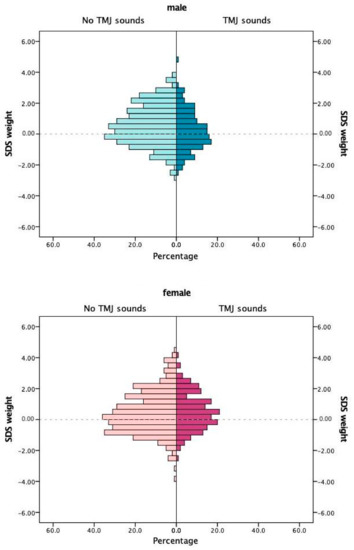
Figure 2.
Standard deviation scores (SDS) of body weight in relation to temporomandibular joint sounds.
These results were corroborated by statistical comparisons of SDS height in females that differed significantly (p = 0.011) with a mean SDS height of 0.10 without TMJ sounds, and a mean of 0.33 for females with TMJ sounds (Table 2). Moreover, SDS values for body weight in males (0.59/0.24; p = 0.006), and the number of hypermobile joints (females), as well as age (females), showed statistically significant differences. Based on these results, four models were created (Table 3) to calculate sex-dependent ORs. When adjusting for cofactors, ORs for SDS height (1.30–1.40, females) and SDS weight (0.75, males) reached significance. Afterwards, TMJ sounds were separately analyzed as click or as crepitus according to the same four models (Table 4 and Table 5). ORs in females revealed values of 1.27–1.38 for clicking sounds and body height, while for body weight of males, ORs of 0.72–0.79 were calculated. For crepitus in both sexes, no statistically significant ORs for SDS height nor SDS weight were detected.

Table 2.
Sex-dependent means and standard deviation (SD) of physical variables in relation to TMJ sounds; SDS: standard deviation scores, CI: confidence interval, n.s.: not significant.

Table 3.
Multivariable analyses of TMJ sounds (N = 322) in relation to physical variables; SDS: standard deviation scores, OR: odds ratio, CI: confidence interval, n.s.: not significant.

Table 4.
Multivariable analyses of TMJ clicking (N = 309) in relation to physical variables; SDS: standard deviation scores, OR: odds ratio, CI: confidence interval, n.s.: not significant.

Table 5.
Multivariable analyses of TMJ crepitus (N = 20) in relation to physical variables; SDS: standard deviation scores, OR: odds ratio, CI: confidence interval, n.s.: not significant.
4. Discussion
The present investigation aimed to examine the relationship between age- and sex-dependent body constitution and TMJ sounds in adolescents. It was observed that rapid growth in females is a risk factor for TMJ sounds (OR 1.28), which does not apply for crepitus but to clicking sounds revealing an OR of 1.27. TMJ sounds in males do not seem to be affected by being relatively tall but by having age-dependent body weight. Thus, the working hypothesis of this investigation could be partially rejected. Moreover, the results of this study corroborate that age, sex, and general joint laxity influence joint sounds in adolescents.
In most patients, a clicking sound can be explained by the movement of the articular disc onto and off the condyle during jaw movements. This pathologic movement is caused by a displacement of the articular disc (DD) with reduction [19]. The latter is a condition that implicates little or no discomfort for the patient, yet it can induce pain or limitations in jaw movements especially while chewing [6,20]. Previous investigations assumed that a TMJ clicking examined in adolescents can be explained by differences in the growth of the maxilla or the mandible and can be interpreted as a sign of adaption [8]. Even if a treatment is not needed, a careful follow-up is necessary, and patients, as well as their parents, should be informed about the etiology and prognosis of DD [19]. Moreover, it is important to avoid an overtreatment of these adolescents [21]. If necessary, a treatment with reversible/conservative measures, such as manual therapy or splints, can be indicated [22], as it might be useful for adolescents with painful TMJ sounds or DD without reduction with limited opening.
The results of this investigation corroborate the hypothesis that anatomical variations can influence the onset of TMJ clicking sounds in adolescents [6,19]. The authors assume that taller girls can be featured by a low muscle tonus and weakness of the ligaments due to the rapid body growth. Consequently, an abrupt growth spurt in the maxilla or mandible might not be compensated by the anatomical structures. This theory is supported by investigations focusing on body height and other health-related issues in adolescents, as it was observed that body height is associated with knee injuries, especially meniscal injuries, in females [23]. Even lower back pain is positively associated and was determined with an OR of 1.22 [24].
To the surprise of the authors, the results of the present study revealed that body weight seems to be a protective factor to avoid TMJ sounds in male adolescents. The authors assume that higher body weight could be related to more muscular mass or soft tissue, which might obviate potential disc displacements in adolescents.
In the present study, some data could not be collected, which can be explained by the fact that some participants/parents rejected parts of the examination. This might be due to the high number of questionnaires and examinations, which could have been exhausting for the adolescents and could have led to a lower adherence. Moreover, organizational reasons are possible, since dental and physical examinations were not performed on the same day. This investigation only included the examination of German adolescents, yet it is reported that ethnical anatomical variances are possible in adolescents [4]. Therefore, the measured values for height and weight were transformed to SDS values with the help of normative data from the German adolescent population. Thus, the SDS values can be easily compared to SDS values observed in other countries. Another limiting factor is that joint sounds were only clinically examined. However, with regard to the costs and estimated time of methods to verify the results like ultrasonography or magnetic resonance [19], the clinical examination was preferred. Moreover, results for TMJ crepitus should be interpreted with caution, since it occurred only in a few adolescents.
The strengths of this study are the large sample size of approximately 1000 participants, which reduces the risk for confounding and bias. Moreover, standardized examination methods were used by trained investigators. The results of the current study provide additional information on the etiology of TMJ sounds in adolescents and describe their relationship to the body constitution of adolescents for the first time. To corroborate results of this investigation, future longitudinal research projects should be created to verify if rapid growth over a distinct period of time influences TMJ sounds in a multinational approach.
The results of this investigation can help to improve healthcare and management of TMD in adolescents, since dentists, orthodontists, and pediatricians should be aware that taller girls seem to be more prone to DD with reduction. Further research on the etiology of disc displacements in adolescents will help to fully understand the influencing factors of TMJ sounds.
5. Conclusions
TMJ sounds in adolescents are influenced by sex, body constitution, and general joint laxity. Tall female adolescents are more prone to TMJ clicking sounds. Increased age-dependent body weight seems to be a protective factor to prevent the onset of TMJ clicking sounds in male adolescents.
Author Contributions
A.K., W.K., and C.H. substantially contributed to the development of the LIFE Child Study, were involved in analysis of data, and proofread the manuscript. A.R. and O.S. had the idea for the investigation and were involved in the extraction and analysis of data. A.R. wrote the manuscript and O.S. critically revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This investigation was supported by the LIFE-Leipzig Research Center for Civilization Diseases at the University of Leipzig and the German Research Foundation (DFG: HI 707/3-1). LIFE is funded by the European Union, the European Regional Development Fund (ERDF), and by the Free State of Saxony within the framework of the excellence initiative.
Acknowledgments
The authors thank all participants of the LIFE Child study for their support of this investigation, all members of the LIFE Child Team for their assistance, and Annett Schrock for data preparation. The authors acknowledge support from Leipzig University for Open Access Publishing.
Conflicts of Interest
The authors declare no conflict of interest.
Data Availability Statement
Data available on request from the corresponding author due to restrictions, e.g., privacy or ethical reasons.
References
- LeResche, L. Epidemiology of Temporomandibular Disorders: Implications for the Investigation of Etiologic Factors. Crit. Rev. Oral Biol. Med. 1997, 8, 291–305. [Google Scholar] [CrossRef]
- Da Silva, C.G.; Pachêco-Pereira, C.; Porporatti, A.L.; Savi, M.G.; Peres, M.A.; Flores-Mir, C.; Canto, G.D.L. Prevalence of clinical signs of intra-articular temporomandibular disorders in children and adolescents: A systematic review and meta-analysis. J. Am. Dent. Assoc. 2016, 147, 10–18. [Google Scholar] [CrossRef]
- Rauch, A.; Schierz, O.; Körner, A.; Kiess, W.; Hirsch, C. Prevalence of anamnestic symptoms and clinical signs of temporomandibular disorders in adolescents—Results of the epidemiologic LIFE Child Study. J. Oral Rehabil. 2019, 47, 425–431. [Google Scholar] [CrossRef]
- Jasinevicius, T.R.; Pyle, M.A.; Lalumandier, J.A.; Nelson, S.; Kohrs, K.J.; Sawyer, D.R. The Angle of the Articular Eminence in Modern Dentate African-Americans and European-Americans. CRANIO® 2005, 23, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Nahhas, R.W.; Valiathan, M.; Sherwood, R.J. Variation in Timing, Duration, Intensity, and Direction of Adolescent Growth in the Mandible, Maxilla, and Cranial Base: The Fels Longitudinal Study. Anat. Rec. Adv. Integr. Anat. Evol. Biol. 2014, 297, 1195–1207. [Google Scholar] [CrossRef] [PubMed]
- Marpaung, C.; Van Selms, M.K.; Lobbezoo, F. Temporomandibular joint anterior disc displacement with reduction in a young population: Prevalence and risk indicators. Int. J. Paediatr. Dent. 2018, 29, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Keeling, S.D.; McGorray, S.; Wheeler, T.T.; King, G.J. Risk factors associated with temporomandibular joint sounds in children 6 to 12 years of age. Am. J. Orthod. Dentofac. Orthop. 1994, 105, 279–287. [Google Scholar] [CrossRef]
- Torii, K. Longitudinal course of temporomandibular joint sounds in Japanese children and adolescents. Head Face Med. 2011, 7, 17. [Google Scholar] [CrossRef]
- Bertoli, F.M.D.P.; Bruzamolin, C.D.; Pizzatto, E.; Losso, E.M.; Brancher, J.A.; De Souza, J.F. Prevalence of diagnosed temporomandibular disorders: A cross-sectional study in Brazilian adolescents. PLoS ONE 2018, 13, e0192254. [Google Scholar] [CrossRef]
- Spruijt, R.; Wabeke, K. Psychological factors related to the prevalence of temporomandibular joint sounds. J. Oral Rehabil. 1995, 22, 803–808. [Google Scholar] [CrossRef]
- Graf, C.; Schierz, O.; Steinke, H.; Körner, A.; Kiess, W.; Kratzsch, J.; Hirsch, C.; LIFE Child study team. Sex hormones in association with general joint laxity and hypermobility in the temporomandibular joint in adolescents—Results of the epidemiologic LIFE child study. J. Oral Rehabil. 2019, 46, 1023–1030. [Google Scholar] [CrossRef] [PubMed]
- John, M.T.; Reissmann, D.R.; Schierz, O.; Wassell, R.W. Oral health-related quality of life in patients with temporomandibular disorders. J. Orofac. Pain 2007, 21, 46–54. [Google Scholar] [PubMed]
- Natu, V.P.; Yap, A.U.; Su, M.H.; Ali, N.M.I.; Ansari, A. Temporomandibular disorder symptoms and their association with quality of life, emotional states and sleep quality in South-East Asian youths. J. Oral Rehabil. 2018, 45, 756–763. [Google Scholar] [CrossRef] [PubMed]
- Poulain, T.; the LIFE Child study team; Baber, R.; Vogel, M.; Pietzner, D.; Kirsten, T.; Jurkutat, A.; Hiemisch, A.; Hilbert, A.; Kratzsch, J.; et al. The LIFE Child study: A population-based perinatal and pediatric cohort in Germany. Eur. J. Epidemiol. 2017, 32, 145–158. [Google Scholar] [CrossRef]
- Quante, M.; for the LIFE Child Study Investigators; Hesse, M.; Döhnert, M.; Fuchs, M.; Hirsch, C.; Sergeyev, E.; Casprzig, N.; Geserick, M.; Naumann, S.; et al. The LIFE child study: A life course approach to disease and health. BMC Public Health 2012, 12, 1021. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Kromeyer-Hauschild, K.; Wabitsch, M.; Kunze, D.; Geller, F.; Geisz, H.C.; Hesse, V.; Von Hippel, A.; Jaeger, U.; Johnsen, D.; Korte, W.; et al. Percentiles of body mass index in children and adolescents evaluated from different German studies. Mon. Kinderheilkd. 2001, 149, 807–818. [Google Scholar] [CrossRef]
- Beighton, P.; Solomon, L.; Soskolne, C.L. Articular mobility in an African population. Ann. Rheum. Dis. 1973, 32, 413–418. [Google Scholar] [CrossRef]
- Poluha, R.L.; Canales, G.D.L.T.; Costa, Y.M.; Grossmann, E.; Bonjardim, L.R.; Conti, P.C.R. Temporomandibular joint disc displacement with reduction: A review of mechanisms and clinical presentation. J. Appl. Oral Sci. 2019, 27. [Google Scholar] [CrossRef]
- Kalaykova, S.; Lobbezoo, F.; Naeije, M. Effect of chewing upon disc reduction in the temporomandibular joint. J. Orofac. Pain 2011, 25, 49–55. [Google Scholar]
- Magnusson, T.; Carlsson, G.E.; Egermark, I. Changes in clinical signs of craniomandibular disorders from the age of 15 to 25 years. J. Orofac. Pain 1994, 8, 207–215. [Google Scholar] [PubMed]
- Wänman, A.; Agerberg, G. Temporomandibular joint sounds in adolescents: A longitudinal study. Oral Surg. Oral Med. Oral Pathol. 1990, 69, 2–9. [Google Scholar] [CrossRef]
- Thein, R.; Gordon, B.; Burstein, G.; Tenenbaum, S.; Derazne, E.; Tzur, D.; Shamis, A.; Afek, A.; Kreiss, Y.; Hershkovich, O. The Prevalence of Cruciate Ligament and Meniscus Knee Injury in Young Adults and Associations with Gender, Body Mass Index, and Height a Large Cross-Sectional Study. J. Knee Surg. 2016, 30, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Hershkovich, O.; Friedlander, A.; Gordon, B.; Arzi, H.; Derazne, E.; Tzur, D.; Shamis, A.; Afek, A. Associations of Body Mass Index and Body Height With Low Back Pain in 829,791 Adolescents. Am. J. Epidemiol. 2013, 178, 603–609. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).