Abstract
Background: The aim was to explore independent wheeled mobility in children with CP, and identify predictors of early independent wheeled mobility and changes over time across birth cohorts. Methods: We included data from the Norwegian Quality and Surveillance Registry for Cerebral Palsy (NorCP) comprising 11,565 assessments of 1780 children born in 2002–2019. Variables included demographic data, Gross Motor Function Classification System (GMFCS) and Manual Ability Classification System (MACS) levels, wheelchair use, and independent wheeled mobility. Cox proportional hazard regression was used to identify predictors for early independent wheeled mobility. Kaplan–Meier survival curves were used to compare birth cohorts. Results: Of 769 (43%) children who used a wheelchair, 511 (67%) had independent wheeled mobility. Two thirds of the children (n = 337) achieved independent wheeled mobility before age 7. Most children with independent wheeled mobility used powered wheelchairs. Children at GMFCS levels III and IV were more likely to reach independent wheeled mobility at an early age. Children at MACS levels III–V had a lower probability of early independent wheeled mobility. The average age of achieving independent mobility decreased from 9.5 to 4.0 years between birth years 2002 and 2019. Conclusions: Two in three children were independent wheelchair users before 7 years of age, and the age of obtaining independent wheeled mobility has decreased over the last 20 years. Children with better hand function were more likely to obtain early independent wheeled mobility. Early intervention programs to promote mobility, development and participation should include powered mobility, adapted steering options, and interventions for hand function.
1. Introduction
Independent mobility is a major developmental milestone with important implications for children’s socio-emotional development and parent–child interaction [1]. Adolescents with physical disabilities have identified being present where things happen as the single most important factor for participation [2]. This requires the ability to move around actively in different settings.
Independent mobility provides new opportunities to explore and engage in the environment, enables new experiences, and affords children the opportunity to exert some degree of control [3,4,5]. Children with mobility limitations, such as cerebral palsy (CP), require different mobility options to explore and navigate in their environment and to take advantage of opportunities for social interaction and participation [6,7,8]. Despite growing evidence of the impact of self-mobility on overall development [9,10], a gap still exists between current knowledge and clinical practice, especially when prescribing powered mobility devices to young children [11,12]. Despite reports that independent mobility is more often reached in powered versus manual wheelchairs, younger children with CP still have access mainly to manual wheelchairs [13]. Powered wheelchairs, ride-on toy cars, and other mobility devices allow children to initiate mobility, which is crucial to enable play, the development of psychosocial skills, interpersonal relationships, and general participation [8,11,14,15,16].
In recent years, the early detection and diagnosis of CP has improved. An accurate and timely diagnosis of CP facilitates the implementation of tailored early intervention programs, which can optimize a child’s brain plasticity, support their development, and improve caregiver well-being [17]. The complexity of motor, cognitive and visual challenges experienced by young children with CP can limit their functional mobility options. Consequently, a multidisciplinary approach has been recommended in the international clinical practice guideline for early intervention in children with CP [18]. Although the guideline does not specifically include recommendations for wheeled mobility, the authors emphasized the importance of the frequent practice of activities that facilitate skilled movement and functional independence. A recent randomized controlled trial investigating early powered mobility in young children with CP has provided evidence supporting the inclusion of early powered mobility as a strategy to enhance functional skills and promote independence [19]. This has also been supported by qualitative data wherein parents described how powered mobility enhanced their children’s independence and self-efficacy, providing the child with more opportunities to make independent choices and to object to choices made by parents [20]. To our knowledge, the extent to which wheeled mobility is introduced at early ages has not been previously examined in large population-based cohorts.
Only two population-based studies have previously described wheelchair use and independent wheeled mobility in children with CP [13,21]. Data from the Swedish national follow-up program for CP showed that children were less likely to self-propel manual wheelchairs compared to powered wheelchairs, regardless of age, gross motor function, or hand function, suggesting that powered mobility should be introduced at earlier ages to promote independent mobility [13]. In a mixed-methods review of the effectiveness of powered mobility for children, Bray et al. (2020) concluded that powered mobility for children under 5 years of age seems to have multiple benefits [22].
The purpose of this study was to explore independent wheeled mobility in children with CP according to age, motor function levels, and CP subtypes. Additionally, we aimed to identify factors associated with early independent wheeled mobility and changes in the age of independent wheeled mobility across birth cohorts from 2002 to 2019, using data from the Norwegian Quality and Surveillance Registry for Cerebral Palsy (NorCP). Our research questions were: (1) What are the proportions and characteristics of children who reach independent wheeled mobility, particularly below 7 years of age? (2) To what extent do CP subtype, gross motor function, manual ability and birth year predict early independent wheeled mobility? (3) Has the age for independent wheeled mobility decreased over the last 20 years?
2. Materials and Methods
2.1. Study Design
The study included longitudinal data registered in NorCP from January 2006 to October 2021. Data for birth years 2002–2006 included one health region (Helse Sør-Øst, covering approximately half of the country’s population), while data for children born 2007–2019 included approximately 90% of all Norwegian children with CP in these birth years [23]. The NorCP registry includes the classification of CP subtypes, levels of the Gross Motor Function Classification System (GMFCS) and the Manual Ability Classification System (MACS), mobility and use of wheelchairs, clinical assessments, and interventions [23]. Children are followed systematically and registered in NorCP annually or every other year by regional physiotherapists (PT) and occupational therapists (OT) from specialized healthcare sectors in close collaboration with their local therapists in the communities.
2.2. Participants
Data from 11,565 assessments of 1780 children registered in NorCP from January 2006 to October 2021 (birth years 2002–2019) were used to identify the total number of wheelchair users, independent wheelchair users, and age for independent wheeled mobility.
2.3. Variables and Data Collection
Data from NorCP assessments include information on use of manual or powered wheelchair for mobility and the ability to self-propel, obtained through the following questions posed to the child or caregiver: “Does the child use a wheelchair? (1) Manual wheelchair for mobility indoors? (2) Powered wheelchair for mobility indoors? (3) Manual wheelchair for mobility outdoors? (4) Powered wheelchair for mobility outdoors?” The response options were (a) yes, self-propels; (b) yes, is pushed/transported; (c) no wheelchair. Two new collapsed variables were created based on these questions, as follows: wheelchair use, including all who used wheelchairs in any setting; independent wheeled mobility, including those who self-propelled either a manual or a powered wheelchair.
CP subtypes were classified according to ICD-10 into hemiplegic, diplegic, quadriplegic, dyskinetic, ataxic, or unspecified. The GMFCS [24] level I to V was used to classify gross motor function. GMFCS is an age-related five-level classification system in which level I describes the most independent and level V the least independent levels of gross motor function. Manual ability was classified according to the five ordinal levels of MACS, ranging from level I, indicating ability to handle age-appropriate objects easily and successfully, to level V, indicating severely limited ability to handle even simple objects [25]. Age was grouped into four categories based on the age of first being registered as using a wheelchair or having independent wheeled mobility, as follows: 0–3 years, 4–6 years, 7–12 years, and 13–18 years. Four cohorts were created based on birth years—2002–2005, 2006–2010, 2011–2014, and 2015–2019.
2.4. Statistical Analyses
Descriptive statistics for age were presented with mean, standard deviation (SD), median, and min/max. Categorical data were presented as frequencies and percentages.
Cox proportional hazard regression analysis was used to identify predictors for earlier independent wheeled mobility. We use the term “independent wheelchair ratio” to reflect hazard ratio in this context. When this ratio is over (under) 1 for a given covariate, then the likelihood of earlier independent wheeled mobility increases (decreases) with this covariate. The following covariates were included one at a time (unadjusted), prior to including all covariates simultaneously (adjusted): sex, birth year cohort (4 categories), CP subtype (5 categories), GMFCS (5 categories), and MACS (5 categories). All children were included in the primary analyses, but children who were not wheelchair users were excluded from a secondary analysis. Kaplan–Meier survival plots [26] were used to show differences in time from birth to event (i.e., age of independent wheeled mobility) between the four birth cohorts (Figure 1). For some participants, the time from birth to the first report of independent wheeled mobility (i.e., age at the event) was not observed, and was censored at their last assessment. Table 1 shows the number of participants with different reasons for censoring. Children who were wheelchair users but dead (n = 17) or emigrated (n = 2) without reaching independent wheeled mobility were censored at the age of their last assessment. Children who were wheelchair users but with no report on independence status (n = 13) were excluded from the analysis. In the primary analysis, all children with valid data were included, yet children who were non-wheelchair users (n = 999) were censored at their last assessment. In the secondary analysis, all non-wheelchair users were excluded. Children with no registered data on wheelchair use (n = 12) were excluded from all analyses.

Table 1.
Different sequences in the data set (N = 1780).
We report 95% confidence intervals (CI) where relevant and regard p-values under 0.05 to represent statistical significance. SPSS version 27.0 was used for the statistical analyses.
3. Results
3.1. Background Characteristics
Among the 1780 included children, there were more boys (58%) than girls (42%) (Table 2). Most children (87%) had spastic CP (including hemiplegia 44%, diplegia 30%, and quadriplegia 13%), whereas 7% had dyskinetic CP, 4% ataxic CP, and 2% unspecified CP. Approximately two thirds were classified at GMFCS levels I and II (69%) or MACS I and II (67%), while less than one third were classified at GMFCS levels III to V (30%) or MACS III to V (29%) (Table 2). The mean age at the first assessment was 45.4 (SD 33.5) months; median age was 36.0 (range 6–208) months. The mean age at the final assessment was 119.7 (SD 53.0) months, and median age was 123.0 (range 8–229) months.

Table 2.
The descriptive statistics for all 1780 children with cerebral palsy (birth years 2002–2019), children who used wheelchairs (assisted or independent), children with independent wheeled mobility (any type), and children with independent wheeled mobility in a manual or powered wheelchair.
3.2. Wheelchair Users
In total, 769 (43%) children used wheelchairs (Table 2), with 597 (78%) getting their first wheelchair before 7 years of age. Wheelchair users were distributed across all CP subtypes, GMFCS levels, and MACS levels. Most children with quadriplegic (86%) and dyskinetic (79%) CP subtypes used wheelchairs, compared with only 18% of children with hemiplegic CP (Table 2). The largest proportion of wheelchair users was classified at GMFCS level III (96%) and the smallest proportion at GMFCS level I (12%). For hand function, the largest proportion of wheelchair users was at MACS level V (90%) and the smallest at MACS level I (19%).
3.3. Independent Wheeled Mobility
Independent wheeled mobility was achieved by 511 children (67% of all of the wheelchair users) (Table 2). The largest proportions of children with independent wheeled mobility were found within the ataxic (88%) and diplegic (81%) CP subtypes, and almost half of the children with quadriplegic CP had independent wheeled mobility (48%). For gross motor function, the largest proportion of children with independent wheeled mobility was in GMFCS level III (86%), and the smallest proportion was at GMFCS level V (38%). For hand function, the largest proportion with independent wheeled mobility was at MACS level II (82%) and the smallest was at level V (37%).
Almost half of the children (46%) with independent wheeled mobility reached independence at between 4 and 6 years of age, and by the age of 7 years, two thirds of the children (n = 337, 66%) had achieved independent wheeled mobility (Table 3).

Table 3.
Distribution of children with independent wheeled mobility in manual or powered wheelchair, according to the age when first registered with independent wheeled mobility.
For all age groups except 0–3 years, most of the children with independent wheeled mobility used powered wheelchairs (Table 3). Among children under 7 years of age, 42% (n = 140) were independent in manual wheelchairs, while 45% (n = 151) were independent in powered wheelchairs. Some of the children in all age groups were independent users of both manual and powered wheelchairs (n = 53, 10%); data were missing on type of wheelchair for 27% (n = 137).
3.4. Predictors of Early Independent Wheeled Mobility
In the primary Cox regression analysis with all children included (n = 1766, missing data n = 14, Table 4), there was a significant (p < 0.001) increase in the likelihood of reaching earlier independent wheeled mobility for each consecutive birth cohort after 2002–2005. In the multiadjusted analysis, children born in 2015–2019 were more than four times more likely to be independent wheelchair users at an early age compared to children born in 2002–2005 (ratio 4.38, 95% CI 2.92–6.57, p < 0.001). Compared to children with hemiplegic CP, children with diplegic (ratio 1.45, 95% CI 1.08–1.95, p = 0.013) and ataxic (ratio 1.59, 95% CI 1.02–2.47, p = 0.039) CP were more likely to reach independent wheeled mobility at an early age. Children classified at GMFCS levels II–V were more likely to reach independent wheeled mobility at an early age compared to GMFCS level I, yet for the MACS levels, children classified at level IV (ratio 0.65, 95% CI 0.43–1.00, p = 0.052) and V (ratio 0.37, 95% CI 0.22–0.63, p < 0.001) were less likely to reach independent wheeled mobility at an early age compared to MACS level I.

Table 4.
Cox proportional hazard regression analysis with age at independent wheeled mobility as the dependent variable, calculated for (A) primary analysis with all included children, and (B) secondary analysis with only children using a wheelchair. Unadjusted—with one covariate at a time; Adjusted—with all the listed covariates included.
In the secondary Cox regression analysis, including only wheelchair users (n = 769, Table 4), children born in 2015–2019 were almost six times as likely to reach early independent wheeled mobility as children born in 2002–2005 (ratio 5.74, 95% CI 3.83–8.59, p < 0.001); this difference was significant for all cohorts after 2002–2005. In the multiadjusted analysis, CP subtype was not a significant predictor of early independent wheeled mobility. Children classified at GMFCS levels III and IV were over two (ratio 2.69, 95% CI 1.86–3.90, p < 0.001) and three (ratio 3.62, 95% CI 2.36–5.57, p < 0.001) times as likely to reach independent wheeled mobility at an early age compared to level I, in contrast to children classified at GMFCS levels II (ratio 1.16, 95% CI 0.85–1.57, p = 0.36) and V (ratio 1.30, 95% CI 0.73–2.29, p = 0.38). Children classified at MACS levels III to V were less likely to reach independent wheeled mobility at an early age compared to MACS levels I, yet the difference was significant only for level IV (ratio 0.44, 95% CI 0.29–0.66, p < 0.001) and V (ratio 0.27, 95% CI 0.29 to 0.66, p < 0.001).
In accordance with the Cox regression analyses, the Kaplan–Meier survival curves (Figure 1) show the changes over time for age of independent wheeled mobility between the four birth cohorts. Estimated medians and quartiles for the age for each birth cohort are presented in Table 5. In both the primary and secondary analyses, independent wheeled mobility was reached at significantly younger ages for the most recent birth cohorts. The median age at independent wheeled mobility decreased significantly over time, from 9.5 years for children born 20 years ago (birth cohort 2002–2005) to 4 years for the most recent birth cohort.

Table 5.
Estimated medians and quartiles for age (years) when reaching independent wheeled mobility among children in four birth cohorts, based on Kaplan–Meier survival analysis. Calculated for all the included children (primary analysis) and for children registered as wheelchair users (secondary analysis).
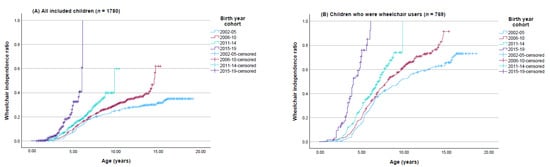
Figure 1.
Kaplan–Meier survival curves for age of reaching independent wheeled mobility, according to four birth cohorts from 2002–2019. Estimated for (A) all included children, and (B) only children who were wheelchair users.
4. Discussion
In this population-based registry study with data from 11,565 assessments for 1780 children with CP born from 2002 to 2019, two thirds of the wheelchair users had independent wheeled mobility. Two thirds of the children reached this independence before the age of 7 years, with the largest proportion between 4–6 years. For all age groups except 0–3 years, the majority of children with independent wheeled mobility used powered wheelchairs. The likelihood of reaching early independent wheeled mobility was positively associated with GMFCS levels III and IV and negatively associated with more limited hand function (MACS IV–V). Children born in the most recent birth years reached independent wheeled mobility at a significantly younger age compared to children born in the earlier birth years.
The strengths of this study include the use of registry data from NorCP with a large sample size. The NorCP covers >90% of the Norwegian population of children with CP [23]. For the earliest cohort, participants were included only from the health region of southeastern Norway. This region represents half of the country’s population, and the distribution of CP subtypes and functional levels is representative of the national CP population [27]. The NorCP webpage contains the NorCP protocols and corresponding manuals with definitions and descriptions; there is a network of local professionals (i.e., OTs, PTs, pediatricians, and psychologists) who participate in learning activities and discussions to ensure a common understanding of the included variables in the registry [28]. A limitation of the study is the relatively large number of missing data for independence in manual or powered wheelchairs, likely due to the non-mandatory nature of these variables in the registry. The study is population-based, and the results may be generalizable to other high-income countries with similar healthcare systems as in Scandinavia.
For 2016, national data on more than 2300 children registered in the Swedish CP follow-up program and quality registry (CPUP) show that, despite a small number of children using powered wheeled mobility, the proportion of children with independent mobility was much higher for those with powered wheelchairs compared to manual wheelchairs [13]. In our study, we have not reported on the proportion of manual versus powered wheelchair users, yet two thirds of the children who used a wheelchair reached independent wheeled mobility, and the largest proportion used powered wheelchairs.
Our results show that two thirds of the children with independent wheeled mobility became independent before 7 years of age, with the largest proportion (46%) learning to self-propel between 4 and 6 years of age. Among children both below and above 7 years of age, the largest proportion were independent in powered wheelchairs. More than half of the children aged 4–6, and one third of the children aged 0–3, were independent in powered wheelchairs. These results contrast with those from a study by Rodby-Bousquet and Hägglund (2010), wherein no children below 3 years of age were reported in the CPUP to use powered mobility [21]. Sweden and Norway are comparable Scandinavian countries, with similar healthcare systems based on a welfare model wherein all citizens have access to the same services, which are free of charge for children. The NorCP follow-up program is based on the Swedish CPUP [29]. A factor likely contributing to the difference in powered wheelchair use among the youngest children is the emergence of a wider selection of powered mobility devices suitable for small children during the 15 years since the data collection performed for the study by Rodby-Bousquet and Hägglund [21]. It may also reflect a significant gap between evidence-based recommendations and clinical practice in providing power mobility to young children, as previously reported from several countries [10,11,12].
In the primary Cox regression analysis, CP subtype was a highly significant predictor for early independent wheeled mobility for all CP subtypes compared to hemiplegia. In the secondary analysis, wherein only users of a wheelchair were included, children with diplegia and ataxia were more likely, and children with quadriplegia were less likely, to be early independent wheelchair users, compared to those with hemiplegia. In the adjusted model, only ataxia was a nearly significant predictor. To understand the clinical relevance of these findings, we need to look at the functional profiles of the CP subtypes as described by Patel et al. [30], Arner et al. [31], and Andersen et al. [32]. Whereas children with hemiplegic CP most often walk independently (GMFCS I–III) and handle objects in daily life independently (MACS I–II), children with diplegic CP are found within all GMFCS levels, yet most often in MACS levels I–II. Children with ataxic CP most frequently are classified at GMFCS levels I–II, and despite hand function classified within the whole functional range (MACS I–V), they most often handle objects independently (MACS I–II) and do not have the asymmetry that makes the self-propelling of manual wheelchair particularly difficult for those with hemiplegic CP.
In addition to predicting independent wheeled mobility, as shown in previous research [13], this study shows that GMFCS and MACS levels also predict the likelihood of independent wheeled mobility at an early age. Children classified at GMFCS III–IV were most likely to be early independent users of a wheelchair compared to GMFCS level I. Moreover, children classified at GMFCS level V were almost equally likely to reach early independent wheeled mobility as children at GMFCS level I, a finding that needs some reflection. The included wheelchair variables represent whether the person uses a wheelchair and whether it self-propels (performance), not whether it is able to self-propel (capacity). By definition, a child classified at GMFCS level I “walks without limitations” [33], and does not need a wheelchair for mobility per se. Nevertheless, even ambulant children with CP experience more fatigue than the typically developing population [34,35]; hence those classified at GMFCS level I may use their wheelchairs merely to save energy despite the capacity to use the wheelchair independently. On the other hand, GMFCS level V represents a group of children with complex disability, defined as “transported in manual wheelchair” [33], and often classified at MACS levels IV or V [36,37], which reduces the probability of independent wheeled mobility.
The finding that MACS levels III–V reduce the likelihood of early independent wheeled mobility has important clinical implications. There is a close association between MACS level V and GMFCS level V [36]. In line with our results, and as per the extended definition, children classified at GMFCS level V “can achieve self-mobility only if they learn how to operate a powered wheelchair” [24]. Increasing the opportunities for independent wheeled mobility among these children requires the thorough assessment of the individual child’s most precise and goal-directed movements, and of possibilities to adapt the operating system (joystick) accordingly, such as control by eye-gaze or head array [38].
For all age cohorts except 0–3 years, the use of powered wheelchairs increased the probability of independent wheeled mobility. More than half of the children with independent wheeled mobility at 4–6 years of age used a powered wheelchair, while 39% were independent in manual wheelchairs. Even children below 4 years of age reached independence in powered wheelchairs. This finding challenges the clinical tradition of introducing manual wheelchairs first and transitioning to powered wheelchairs later. Although many therapists may hesitate to introduce a powered wheelchair to a young child who may have the potential to achieve some walking ability, our results indicate a promising tendency toward earlier introduction to powered mobility. The results show an almost six times higher likelihood of early wheeled mobility for birth years 2015–2019 compared to 2002–2005; compared to children born earlier, a higher proportion of children in the most recent birth years become independent users of powered mobility.
Being able to move independently around home, in kindergarten, or in the community represents an important milestone for all young children, and is an important concern for parents [39]. Numerous studies support the importance of early mobility for psychosocial development and play [5,40], for spatial perception [41], and for participation in everyday life [42]. It is encouraging to find that the proportion of young children who self-propel their wheelchairs has increased over the last 20 years. This trend probably results from better access to powered mobility devices for young children and improved technologies for alternate operation modes to compensate for limited hand function, and also from a shift in the therapeutic view of independent wheeled mobility being not just for transportation, but also a facilitator for overall development and general participation. Although the international clinical practice guidelines for early intervention in children with CP does not include specific recommendations for early wheeled mobility [18], several studies have reported on the multiple benefits of such interventions [7,8,14,19,22]. More research is still needed to strengthen the knowledge base so as to support early wheeled mobility as a standard practice in early intervention programs. Meanwhile, policy arrangements should reflect our findings together with the current knowledge, and wheeled mobility devices should be accepted as useful tools to stimulate overall development not only for children with the most limited walking ability.
5. Conclusions
In this large population-based registry study, two out of three children with CP who used wheelchairs moved around independently, and a majority with independent wheeled mobility used powered wheelchairs. Children classified at GMFCS levels III–IV were most likely to be independent wheelchair users at an early age. Children with more limited hand function were less likely to be early independent wheelchair users. Advances in technology over the last 20 years, and a shift in the therapeutic views of wheeled mobility as a facilitator of development, have likely contributed to the significant decrease in the age of independent wheeled mobility. To promote early mobility, general development, and participation, early intervention programs for young children with CP should include powered mobility, adapted steering options, and interventions to promote hand function.
Author Contributions
A.K. designed the study, collected and analyzed the data, provided tables and figures, and drafted the manuscript. K.A.I.E. designed the study, supervized analyses, and actively improved and revised the manuscript. N.K. designed the study and contributed to writing the manuscript. E.R.-B. interpreted the findings and actively improved and revised the manuscript. S.L. supervized the statistical analyses and interpreting of results, and contributed to writing the manuscript. G.L.K. designed the study, supervized the analyses, interpreted the findings, and actively improved and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Regional Committee for Medical and Health Research Ethics of South East Norway (reg. number 280350) in September 2021. Informed consent for registry data to be used in research was provided by the legal caregivers of all participants upon registration to the NorCP. All methods were carried out in accordance with relevant guidelines and regulations.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets analyzed during the current study are part of the NorCP registry and are not publicly available due to data protection regulations. The data are available from the corresponding author (G.L.K.) upon reasonable request.
Acknowledgments
We would like to express our sincere gratitude to all families who participate in NorCP and to the therapists who perform the assessments and enter data into the registry.
Conflicts of Interest
The authors declare that they have no competing interests.
Abbreviations
| CI | Confidence intervals |
| CP | Cerebral Palsy |
| GMFCS | Gross Motor Function Classification System |
| MACS | Manual Ability Classification System |
| OT | Occupational therapist |
| PT | Physiotherapist |
| NorCP | Norwegian Quality and Surveillance Registry for Cerebral Palsy |
References
- Hendrix, R.R.; Thompson, R.A. Development of self-produced locomotion in the first year: Changes in parent perceptions and infant behaviour. Infant Child Dev. 2011, 20, 288–300. [Google Scholar] [CrossRef]
- Asbjørnslett, M.; Hemmingsson, H. Participation at school as experienced by teenagers with physical disabilities. Scand. J. Occup. Ther. 2008, 15, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Lobo, M.A.; Harbourne, R.T.; Dusing, S.C.; McCoy, S.W. Grounding early intervention: Physical therapy cannot just be about motor skills anymore. Phys. Ther. 2013, 93, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Adolph, K.E.; Franchak, J.M. The development of motor behavior. Wiley Interdiscip. Rev. Cogn. Sci. 2017, 8, e1430. [Google Scholar] [CrossRef]
- Anderson, D.I.; Campos, J.J.; Witherington, D.C.; Dahl, A.; Rivera, M.; He, M.; Uchiyama, I.; Barbu-Roth, M. The role of locomotion in psychological development. Front. Psychol. 2013, 4, 440. [Google Scholar] [CrossRef]
- Livingstone, R.; Paleg, G. Practice considerations for the introduction and use of power mobility for children. Dev. Med. Child. Neurol. 2014, 56, 210–221. [Google Scholar] [CrossRef]
- Kenyon, L.K.; Mortenson, W.B.; Miller, W.C. ‘Power in Mobility’: Parent and therapist perspectives of the experiences of children learning to use powered mobility. Dev. Med. Child. Neurol. 2018, 60, 1012–1017. [Google Scholar] [CrossRef]
- Huang, H.H.; Chen, Y.M.; Huang, H.W. Ride-On Car Training for Behavioral Changes in Mobility and Socialization Among Young Children with Disabilities. Pediatr. Phys. Ther. 2017, 29, 207–213. [Google Scholar] [CrossRef]
- Evensen, K.A.I. Does movement matter? Consequences of motor problems for everyday life in children born preterm. Dev. Med. Child. Neurol. 2023, 65, 1546–1547. [Google Scholar] [CrossRef]
- Rodby-Bousquet, E. The power of mobility. Dev. Med. Child. Neurol. 2018, 60, 968–969. [Google Scholar] [CrossRef]
- Kenyon, L.K.; Jones, M.; Livingstone, R.; Breaux, B.; Tsotsoros, J.; Williams, K.M. Power mobility for children: A survey study of American and Canadian therapists’ perspectives and practices. Dev. Med. Child. Neurol. 2018, 60, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- Rodby-Bousquet, E. The gap between current knowledge and clinical practice in childhood disability. Dev. Med. Child. Neurol. 2018, 60, 969–970. [Google Scholar] [CrossRef] [PubMed]
- Rodby-Bousquet, E.; Paleg, G.; Casey, J.; Wizert, A.; Livingstone, R. Physical risk factors influencing wheeled mobility in children with cerebral palsy: A cross-sectional study. BMC Pediatr. 2016, 16, 165. [Google Scholar] [CrossRef] [PubMed]
- Guerette, P.; Furumasu, J.; Tefft, D. The positive effects of early powered mobility on children’s psychosocial and play skills. Assist. Technol. 2013, 25, 39–48, quiz 9–50. [Google Scholar] [CrossRef]
- Hospodar, C.M.; Feldner, H.A.; Logan, S.W. Active mobility, active participation: A systematic review of modified ride-on car use by children with disabilities. Disabil. Rehabil. Assist. Technol. 2023, 18, 974–988. [Google Scholar] [CrossRef]
- Livingstone, R.; Field, D. Systematic review of power mobility outcomes for infants, children and adolescents with mobility limitations. Clin. Rehabil. 2014, 28, 954–964. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.-C.; et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef]
- Morgan, C.; Fetters, L.; Adde, L.; Badawi, N.; Bancale, A.; Boyd, R.N.; Chorna, O.; Cioni, G.; Damiano, D.L.; Darrah, J.; et al. Early Intervention for Children Aged 0 to 2 Years with or at High Risk of Cerebral Palsy International Clinical Practice Guideline Based on Systematic Reviews. JAMA Pediatr. 2021, 175, 846–858. [Google Scholar] [CrossRef]
- Feldner, H.A.; Logan, S.W.; Otieno, S.; Fragomeni, A.; Kono, C.; Riordan, K.; Sloane, B.; Kenyon, L.K. Short-Term Powered Mobility Intervention is Associated with Improvements in Development and Participation for Young Children with Cerebral Palsy: A Randomized Clinical Trial. Phys. Ther. 2024, pzae152. [Google Scholar] [CrossRef]
- Currier, B.A.; Jones, M.A.; DeGrace, B.W. Experiences of Families with Young Power Wheelchair Users. J. Early Interv. 2019, 41, 125–140. [Google Scholar] [CrossRef]
- Rodby-Bousquet, E.; Hägglund, G. Use of manual and powered wheelchair in children with cerebral palsy: A cross-sectional study. BMC Pediatr. 2010, 10, 59. [Google Scholar] [CrossRef] [PubMed]
- Bray, N.; Kolehmainen, N.; McAnuff, J.; Tanner, L.; Tuersley, L.; Beyer, F.; Grayston, A.; Wilson, D.; Edwards, R.T.; Noyes, J.; et al. Powered mobility interventions for very young children with mobility limitations to aid participation and positive development: The EMPoWER evidence synthesis. Health Technol. Assess. 2020, 24, 1–194. [Google Scholar] [CrossRef] [PubMed]
- Hollung, S.J.; Jahnsen, R.; Klevberg, G.L.; Kløve, N.; Andersen, G.L. The impact of longitudinal surveillance of individuals with cerebral palsy in Norway; a 20-year quality registry and follow-up program perspective. Norsk Epidemiol. 2023, 31, 15–23. [Google Scholar] [CrossRef]
- Palisano, R.J.; Rosenbaum, P.; Bartlett, D.; Livingston, M.H. Content validity of the expanded and revised Gross Motor Function Classification System. Dev. Med. Child. Neurol. 2008, 50, 744–750. [Google Scholar] [CrossRef]
- Eliasson, A.-C.; Krumlinde-Sundholm, L.; Rösblad, B.; Beckung, E.; Arner, M.; Öhrvall, A.-M.; Rosenbaum, P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child. Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef]
- Rich, J.T.; Neely, J.G.; Paniello, R.C.; Voelker, C.C.; Nussenbaum, B.; Wang, E.W. A practical guide to understanding Kaplan-Meier curves. Otolaryngol. Head Neck Surg. 2010, 143, 331–336. [Google Scholar] [CrossRef]
- NorCP. Norsk Kvalitet- og Oppfølgingsregister for Cerebral Parese (NorCP): Årsrapport for 2023; Sykehuset i Vestfold: Tønsberg, Norway, 2024. [Google Scholar]
- NorCP. Norwegian Quality and Surveillance Registry (NorCP) Webpage. Available online: https://www.oslo-universitetssykehus.no/avdelinger/barne-og-ungdomsklinikken/barneavdeling-for-nevrofag/norsk-kvalitets-og-oppfolgingsregister-for-cerebral-parese (accessed on 1 December 2024).
- Alriksson-Schmidt, A.I.; Arner, M.; Westbom, L.; Krumlinde-Sundholm, L.; Nordmark, E.; Rodby-Bousquet, E.; Hägglund, G. A combined surveillance program and quality register improves management of childhood disability. Disabil. Rehabil. 2016, 39, 830–836. [Google Scholar] [CrossRef]
- Patel, D.R.; Neelakantan, M.; Pandher, K.; Merrick, J. Cerebral palsy in children: A clinical overview. Transl. Pediatr. 2020, 9 (Suppl. S1), S125–S135. [Google Scholar] [CrossRef]
- Arner, M.; Eliasson, A.C.; Nicklasson, S.; Sommerstein, K.; Hagglund, G. Hand function in cerebral palsy. Report of 367 children in a population-based longitudinal health care program. J. Hand Surg. Am. 2008, 33, 1337–1347. [Google Scholar] [CrossRef]
- Andersen, G.L.; Irgens, L.M.; Haagaas, I.; Skranes, J.S.; Meberg, A.E.; Vik, T. Cerebral palsy in Norway: Prevalence, subtypes and severity. Eur. J. Paediatr. Neurol. 2008, 12, 4–13. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Bartlett, D.; Livingston, M.H. Gross Motor Function Classification System, Expanded and Revised (GMFCS E&R ©); CanChild Centre for Childhood Disability Research, McMaster University: Hamilton, ON, Canada, 2007; Available online: https://www.canchild.ca/system/tenon/assets/attachments/000/000/058/original/GMFCS-ER_English.pdf (accessed on 1 December 2024).
- Eken, M.M.; Houdijk, H.; Doorenbosch, C.A.M.; Kiezebrink, F.E.M.; Bennekom, C.A.M.v.; Harlaar, J.; Dallmeijer, A.J. Relations between muscle endurance and subjectively reported fatigue, walking capacity, and participation in mildly affected adolescents with cerebral palsy. Dev. Med. Child. Neurol. 2016, 58, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Brunton, L.K. Descriptive Report of the Impact of Fatigue and Current Management Strategies in Cerebral Palsy. Pediatr. Phys. Ther. 2018, 30, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Compagnone, E.; Maniglio, J.; Camposeo, S.; Vespino, T.; Losito, L.; De Rinaldis, M.; Gennaro, L.; Trabacca, A. Functional classifications for cerebral palsy: Correlations between the gross motor function classification system (GMFCS), the manual ability classification system (MACS) and the communication function classification system (CFCS). Res. Dev. Disabil. 2014, 35, 2651–2657. [Google Scholar] [CrossRef] [PubMed]
- Carnahan, K.D.; Arner, M.; Hagglund, G. Association between gross motor function (GMFCS) and manual ability (MACS) in children with cerebral palsy. A population-based study of 359 children. BMC Musculoskelet. Disord. 2007, 8, 50. [Google Scholar] [CrossRef] [PubMed]
- Dicianno, B.E.; Cooper, R.A.; Coltellaro, J. Joystick Control for Powered Mobility: Current State of Technology and Future Directions. Phys. Med. Rehabil. Clin. N. Am. 2010, 21, 79–86. [Google Scholar] [CrossRef]
- Novak, I.; Hines, M.; Goldsmith, S.; Barclay, R. Clinical prognostic messages from a systematic review on cerebral palsy. Pediatrics 2012, 130, e1285–e1312. [Google Scholar] [CrossRef]
- Campos, J.J.; Anderson, D.I.; Barbu-Roth, M.A.; Hubbard, E.M.; Hertenstein, M.J.; Witherington, D. Travel Broadens the Mind. Infancy 2000, 1, 149–219. [Google Scholar] [CrossRef]
- Foreman, N.; Orencas, C.; Nicholas, E.; Morton, P.; Gell, M. Spatial awareness in seven to 11-year-old physically handicapped children in mainstream schools. Eur. J. Spec. Needs Educ. 1989, 4, 171–179. [Google Scholar] [CrossRef]
- Kerem Günel, M.; Arslan, U.; Bıyık, K.; Özal, C.; Numanoğlu, A.; Unes, S.; Tunçdemir, M.; Çankaya, Ö.; Özcebe, H.; Green, D. Evaluation of daily and social participation of children with Cerebral Palsy across different age groups with a focus on the ‘F’-words: Function, family, fitness, fun, friends and future. Res. Dev. Disabil. 2023, 140, 104588. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).