Abstract
Background/Objectives: Endovascular therapy (EVT) is the treatment of choice for femoropopliteal artery (FPA) disease manifesting as critical limb-threatening ischemia (CLTI) or intermittent claudication (IC). This study aimed to compare the clinical outcomes of patients with CLTI with those of patients with IC after EVT in a real-world setting. Methods: In total, 1924 patients with FPA disease (CLTI: n = 812, IC: n = 1112) from the K-VIS ELLA (Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases) registry who underwent EVT between 2006 and 2021 were analyzed. The primary endpoint was defined as target limb amputation or clinically driven (CD) target extremity revascularization (TER) 2 years after the procedure. Results: The incidence of the primary endpoint after inverse probability of treatment weighting (IPTW) was significantly higher in the CLTI group (hazard ratio [HR], 1.314; 95% confidence interval [CI], 1.105–1.561; p = 0.002). The incidences of loss of clinical patency, major adverse limb events (MALEs), and all-cause mortality were also higher in the CLTI group (hazard ratio [HR], 1.312; 95% confidence interval [CI], 1.157–1.488; p < 0.001). However, the risk of repeat percutaneous transluminal angioplasty (PTA) was similar between the groups (HR, 1.014; 95% CI, 0.833–1.234; p = 0.920). The use of drug-coated balloons (DCBs) was associated with favorable primary outcomes in both groups, particularly in patients with IC (HR: 0.429, 95% CI: 0.25–0.734; p = 0.002). Conclusions: Patients with CLTI undergoing EVT for FPA disease experienced worse clinical outcomes than those with IC, although the repeat PTA rates were similar. The use of DCBs showed promising results in both groups.
1. Introduction
Peripheral artery disease (PAD), a common manifestation of advanced systemic atherosclerosis, is the third leading cause of atherosclerotic morbidity after coronary heart disease and stroke [1,2]; it affects over 200 million adults globally. Atherosclerotic changes in the femoropopliteal artery (FPA) often result in the formation of long occlusive calcified lesions [3]. FPA disease may remain asymptomatic or present with symptoms ranging from intermittent claudication (IC) to severe ischemic conditions such as tissue loss or gangrene [2]. Critical limb-threatening ischemia (CLTI), a severe form of PAD, is characterized by resting pain, non-healing wounds, and tissue damage [4]. Endovascular therapy (EVT) is widely accepted as the preferred revascularization strategy for femoropopliteal artery disease, particularly in high-risk surgical risk [5]. Rapid advancements have been made in EVT for the management of FPA disease in recent years, and a significant improvement in post-treatment clinical outcomes has been observed since the introduction of newer treatment devices such as drug-coated balloons (DCBs) and drug-eluting stents (DESs) for the management of FPA disease [6,7,8,9,10].
The comorbidities observed in patients with CLTI are typically worse than those observed in patients with claudication. Moreover, patients with CLTI are at a higher risk of adverse events such as major amputations and periprocedural complications. Notably, a higher risk of cardiovascular events, including increased mortality [4,11], has been observed in patients with CLTI. Thus, it is imperative to develop an optimal treatment strategy to improve outcomes in this high-risk population is imperative [4,12,13]. However, few studies have directly compared the outcomes of EVT in patients with CLTI and those with IC. Therefore, this study aimed to compare the clinical outcomes of EVT in patients with native FPA disease according to the presence of CLTI or IC, using data from a real-world multicenter cohort with a 2-year follow-up period.
2. Materials and Methods
2.1. Data Sources
The Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) is a multicenter registry that includes data from patients diagnosed with lower extremity PAD who underwent EVT at 19 cardiovascular centers in South Korea between 2006 and 2021 (ClinicalTrials.gov: NCT02748226).
2.2. Population
The study design and inclusion/exclusion criteria are detailed in a previous publication [3]. Figure 1 presents a flowchart of the study. Among the 2951 patients included in the registry, 2564 who had undergone EVT for FPA disease were eligible for inclusion in the present study. Patients who underwent bypass surgery, those with in-stent restenosis, and those with no data available regarding the EVT devices used, follow-up duration, Rutherford class, or TASC classification were excluded from the present study. Thus, the final sample comprised 1924 patients. The Institutional Review Board of each participating center approved the study protocol. This study was conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained from all patients, except for those whose data were retrospectively collected. All the patients underwent a comprehensive clinical assessment at baseline. The clinical and imaging data of the patients, along with their demographic characteristics and comorbidities, were collected prospectively and analyzed retrospectively. Follow-up examinations were scheduled 6, 12, and 24 months after the initial procedure. The median follow-up duration was 1.9 ± 0.4 years. All patients were followed up for up to 2 years after EVT.
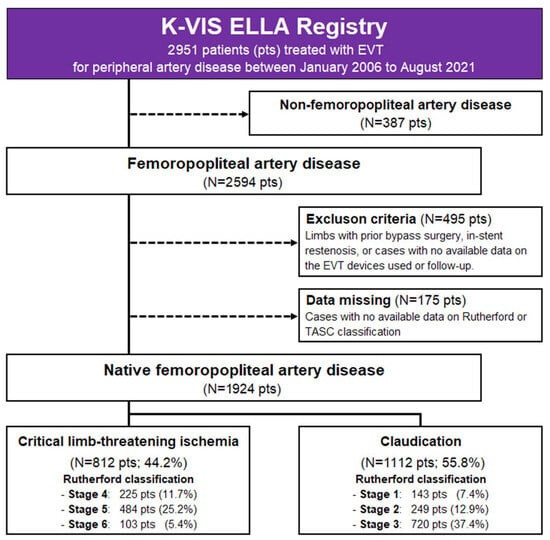
Figure 1.
Study flowchart. EVT, endovascular therapy; K-VIS ELLA, Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases.
2.3. Procedures
Experienced interventional cardiologists performed all EVT procedures using the device of their choice. Intraluminal wiring was performed using 0.018- or 0.035-inch guidewires. A subintimal approach with re-entry into the distal true lumen or a retrograde approach was used in cases where wire passage could not be achieved. Pre-dilatation was performed using a plain balloon unless an atherectomy was initially performed. Pretreatment with atherectomy devices was favored in selected cases of calcified or long-segment lesions after intraluminal wire passage. The dilatation pressure of the DCB was determined by the surgeon and maintained above the nominal pressure. This pressure was maintained for at least 180 s after successful vessel preparation. Provisional stenting with bare metal stents (BMS) was performed if flow-limiting dissection or residual stenosis of ≥30% was angiographically confirmed after DCB, and these cases were included in the DCB group. Post-dilatation with a non-compliant balloon was performed after stenting with the BMS and DES to achieve a residual stenosis of <30%. Periprocedural complications such as vascular rupture, distal embolization, or access-site bleeding were managed at the operator’s discretion, typically with prolonged balloon inflation, additional stent implantation (including bailout stenting), thrombus aspiration or distal protection, and adjunctive pharmacologic therapy. Unless contraindicated, dual antiplatelet therapy with aspirin and P2Y12 inhibitors such as clopidogrel was initiated and continued for at least 6 months after the procedure. Cilostazol, a third antiplatelet agent, was administered at the physician’s discretion.
2.4. Definitions and Study Endpoints
The primary outcome was the target limb amputation or clinically driven (CD) target extremity revascularization (TER). CD-TER was defined as any subsequent intervention on the target extremity performed for stenosis > 50% of the angiographic diameter at a site within 5 mm proximal or distal to the original treatment segment, accompanied by symptom worsening and a decrease in ankle-brachial index (ABI) > 0.15 compared to the immediate postprocedural ABI. Loss of clinical patency, major adverse limb events (MALEs), and all-cause mortality were the secondary outcomes. Clinical patency was defined as the absence of worsening of symptoms by ≥1 Rutherford category change accompanied by a decrease of >0.15 in the ABI or a ≥50% absence of restenosis on imaging studies such as duplex ultrasound, computed tomographic angiography, or intra-arterial angiography. Above-ankle amputation or repeat revascularization of the index limb was defined as MALE. Revascularization of the target vessel with <30% residual stenosis and the absence of flow-limiting dissection was defined as technical success. Major amputation was defined as amputation of the index limb occurring above the ankle level, whereas minor amputation was defined as any amputation below the ankle, including toe or forefoot amputation. All patients were followed up for up to 2 years from the date of the procedure until the occurrence of an outcome event. The principal investigators at the participating centers identified and adjudicated all the clinical events.
2.5. Statistical Analysis
Continuous variables are presented as mean ± standard deviation, whereas discrete variables are presented as counts and percentages. The unpaired t-test or Mann–Whitney rank test was used to assess the differences between continuous variables. The χ2 test or Fisher’s exact test was used to assess the differences between discrete variables. Inverse probability weighting (IPTW) analysis was conducted using a logistic regression model to adjust for confounding factors. Table 1 and Table 2 present the covariates used to calculate the propensity for CLTI. Cox proportional regression analysis adjusted for IPTW was performed to determine the impact of various types of EVT on the primary and secondary endpoints over a 2-year follow-up period. All statistical analyses were performed using SPSS software (version 24.0; SPSS-PC Inc., Chicago, IL, USA). Statistical significance was defined as a two-sided p-value of <0.05.

Table 1.
Baseline characteristics and laboratory findings.

Table 2.
Angiographic and procedural characteristics.
3. Results
3.1. Baseline Characteristics
Of the 1924 patients included in the final analysis, 812 (42.2%) were classified as having CLTI, and 1112 (57.8%) as having IC. Table 1 presents the baseline demographics, comorbidities, risk factors, prior surgical or intervention procedures, and laboratory findings of the patients with CLTI and IC before and after IPTW. The median age of the patients was 69.7 years (CLTI, 70.3; IC, 69.0), and 81.6% were male (CLTI, 81.7%; IC, 81.6%). Regarding severity, 37.4% of the IC group were categorized as Rutherford class 3, whereas 25.2% of the CLTI group were categorized as Rutherford class 5 (Figure 2). The sex distribution, age, BMI, and comorbidities, such as hypertension, diabetes, dyslipidemia, presence of coronary artery disease, and history of myocardial infarction (MI), were adequately balanced after IPTW.
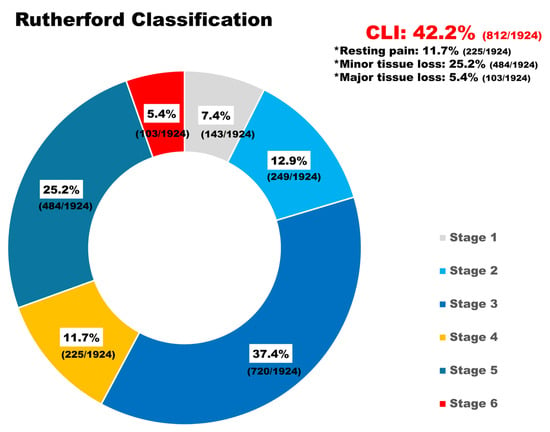
Figure 2.
Distribution of Rutherford classifications in the study population. The donut chart illustrates the proportion of Rutherford classifications among 1924 patients who underwent femoropopliteal endovascular therapy. Critical limb-threatening ischemia (CLTI; stages 4–6) occurred in 44.2% of the study population.
Table 2 shows the angiographic and procedural characteristics, and the list of devices is shown in Supplementary Table S1. Among patients treated with DCB, the IN.PACT balloon (paclitaxel 3.5 µg/mm2 with urea excipient, Medtronic, Minneapolis, MN, USA) was most frequently used, accounting for more than 70% of all cases, followed by Lutonix (paclitaxel 2.0 µg/mm2 with polysorbate/sorbitol excipient, Bard Peripheral Vascular, Tempe, AZ, USA) and Ranger (paclitaxel 2.0 µg/mm2 with acetyl tributyl citrate excipient, Boston Scientific, Marlborough, MA, USA). Among DES cases, Eluvia (paclitaxel with a poly[glycolide-co-lactide] fluoropolymer, 120-µm strut thickness, Boston Scientific) was used in more than 60% of all cases. The temporal patterns of devices used during enrollment are illustrated in Supplemental Figure S1. A higher proportion of patients with infrapopliteal artery disease was observed in the CLTI group (CLTI: 48.6%; IC: 18.4%), more frequently involving the anterior tibial artery (ATA). The prevalence of calcified lesions was higher in the CLTI group (60.7%) than in the IC group (52.5%). However, the prevalence of total occlusion was similar in both groups (CLTI, 48.5%; IC, 48.6%). The patients in the CLTI group underwent subintimal tracking more frequently than those in the IC group (CLTI, 19.4%; IC, 14.3%). Patients in the IC group underwent plaque modification strategies, such as atherectomy (CLTI, 10.5%; IC, 11.6%), directional atherectomy, and anti-restenotic therapy (DAART; CLTI, 8.7%; IC, 10.7%). Plaque modification strategies, including atherectomy (CLTI, 10.5%; IC, 11.6%), directional atherectomy, and anti-restenotic therapy (DAART; CLTI, 8.7%; IC, 10.7%), were more frequently performed in the IC group.
Table 3 summarizes the procedural outcomes and medications administered at discharge. The initial procedural success rate, defined as residual stenosis of ≤30%, was identical in both groups (CLTI: 96.6%, IC: 96.6%). However, procedural complications, including bleeding and vascular rupture, occurred more frequently in the CLTI group (6.2%) than in the IC group (2.7%).

Table 3.
Procedural outcomes and medications at discharge.
3.2. Clinical Outcomes
Crude analysis (Table 4) revealed that CLTI was associated with a higher risk of adverse outcomes than IC. Patients with CLTI were at a greater risk of undergoing target limb amputation or clinically driven TER (hazard ratio [HR], 1.762; 95% confidence interval [CI], 1.385–2.242; p < 0.001). Additionally, CLTI was associated with an increased risk of loss of clinical patency, MALEs, and all-cause mortality (HR, 1.715; 95% CI, 1.428–2.059; p < 0.001). The risk of all-cause mortality was substantially higher in patients with CLTI (HR, 4.067; 95% CI, 2.794–5.920; p < 0.001). The risk of symptom aggravation was also higher in the CLTI group (HR 1.679, 95% CI [1.399–2.016], p < 0.001). Among patients who experienced symptom aggravation, only 11.8% in the CLTI group and 15.0% in the IC group subsequently underwent CD-TER. Furthermore, CLTI was associated with an increased risk of minor (HR, 15.12; 95% CI, 6.919–33.06; p < 0.001) and major (HR, 14.01; 95% CI, 3.266–60.13; p < 0.001) lower limb amputations. However, the risk of repeat procedures was similar in both groups (HR, 1.177; 95% CI, 0.894–1.549; p = 0.259). After IPTW adjustment, the higher incidence of adverse events in the CLTI group remained significant, whereas the risk of repeat procedures did not differ between the groups (HR, 1.014; 95% CI, 0.833–1.234; p = 0.920). These findings remained consistent in the time-stratified sensitivity analysis (2006–2014 and 2014–2021), indicating that the association between CLTI and adverse outcomes was stable across different treatment eras. Amputation-free survival curves stratified by clinical presentation and Rutherford classification are presented in Supplementary Figure S2.

Table 4.
Clinical outcomes and hazard ratio of critical limb ischemia up to 2 years.
3.3. Subgroup Analysis: Treatment Strategy and Clinical Outcomes
DCB was associated with a lower risk of target limb amputation or clinically driven TER (hazard ratio [HR], 0.455; 95% confidence interval [CI] 0.325–0.638; p < 0.001) in the crude population. The HR of the DCB-only group was 0.443 (95% CI, 0.317–0.621), whereas that of the combination of DCB with a BMS bail-out strategy was 0.518 (95% CI, 0.284–0.946). These findings show that provisional BMS implantation following DCB slightly attenuates the effect size of DCB; however, it does not account for the overall benefit observed in the total DCB group. EVT with DES showed a lower risk of target limb amputation or clinically driven TER than POBA (HR, 0.604; 95% CI, 0.358–0.946; p = 0.028), although the benefit was less pronounced than that of DCB. (Figure 3). Baseline characteristics of each treatment strategy subgroup are shown in Supplementary Tables S3 and S4.
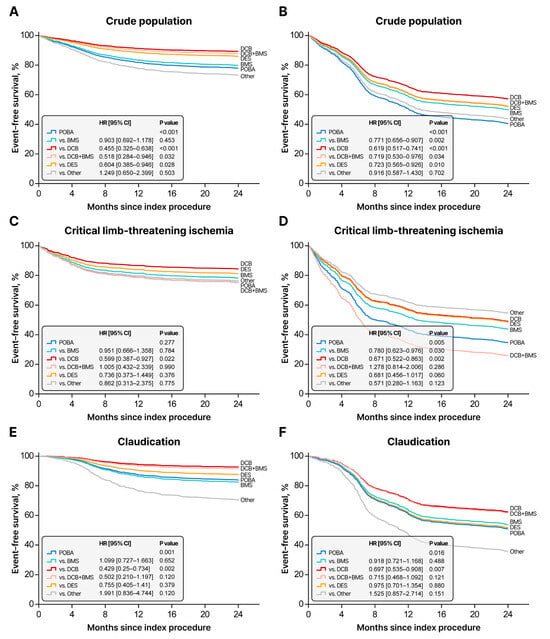
Figure 3.
Two-year clinical outcomes according to the treatment strategy; Kaplan–Meier curves for event-free survival based on treatment strategy using the Cox proportional hazards model with inverse probability of treatment weighting: (A,C,E) represent the primary endpoint: target limb amputation or clinically driven target extremity revascularization in the crude population (A), critical limb ischemia (C), and claudication (E) groups. (B,D,F) depict the secondary endpoint: loss of clinical patency, major adverse limb events (MALEs), or all-cause mortality in the crude population (B), critical limb ischemia (D), and claudication (F) groups. Treatment strategies include POBA, BMS, DES, DCB, and DCB + BMS. POBA, plain old balloon angioplasty; BMS, bare-metal stent; DCB, drug-coated balloon; DES, drug-eluting stent.
4. Discussion
The major findings of the present study are as follows: (1) The risk of target limb amputation or CD-TER was approximately 1.3-fold higher in the CLTI group compared to the IC group; (2) the risks of all-cause mortality, target limb amputation, MALEs, and loss of clinical patency in the CLTI group were 2.4, 7.8, 1.5, and 1.3 times higher, respectively, compared to the IC group at the 2-year follow-up; (3) no significant difference were observed between the CLTI and IC groups in terms of the rates of repeat PTA; and (4) a potential benefit of DCB in reducing the primary and secondary outcomes was observed in both groups.
The Global Burden of Disease, Injuries, and Risk Factors Study 2017 (GBD 2017) revealed that peripheral vascular disease accounted for 25.6% of the global burden of cardiovascular diseases and 1.7% of the overall global disease burden [14]. A retrospective analysis of the U.S. healthcare database (2003–2008) reported PAD prevalence and incidence rates of 10.7% and 2.4%, respectively [15]. A diagnosis of PAD poses a substantial economic burden on communities [16]. Despite the increasing prevalence of PAD in Korea due to the aging population, Asian populations remain underrepresented in PAD studies, leaving the current prevalence unclear. In recent Korean national health insurance data, a 20–25% annual increase in procedures was observed between 2008 and 2012, with EVT accounting for 80–95% of lower extremity arterial procedures [17,18]. Thus, PAD and its complications pose a growing burden on global morbidity and the economy.
Patients with CLTI typically present with more severe comorbidities than those with IC [2,19]. CLTI, often accompanied by diabetes mellitus and multiple comorbidities, such as metabolic disorders, renal failure, and prior cardiac disease, is characterized by severe inflammation and tissue necrosis, which limit treatment options [20]. In contrast, although claudication causes pain and reduced mobility due to decreased blood flow, it does not result in tissue loss and can be managed conservatively. The differences in the natural course and outcomes between CLTI and claudication following EVT have not been studied in real-world clinical settings, despite the poorer prognosis of CLTI.
The strengths of the K-VIS ELLA study lie in its large-scale real-world registry data, prospective enrollment, and long-term follow-up. Unlike previous studies that excluded Rutherford class 6 patients, this study included all patients, encompassing Rutherford class 6. Notably, most patients in the other studies were classified as Rutherford class 4. In the IN.PACT post hoc analysis, all-cause mortality (37.4% vs. 17.4%) and major limb amputation rates (6.8% vs. 1.1%) were higher in the CLTI group, whereas the 5-year freedom from CD-TER rate was lower (60.7% vs. 70.5%) [19]. However, the limited number of patients with CLTI (n = 156) compared with IC patients (n = 1246) prevented us from drawing definite conclusions. Another single-center study reported that the overall risk of reintervention at 3.7 years was similar between the groups (CLTI: 53.8%, IC: 60.2%), consistent with our findings [12]. However, this was a retrospective study, and the Rutherford classification was not available. In the present study, the rates of repeat procedures among patients with CLTI and IC were 13.1% and 11.4% (HR: 1.177, 95% CI: 0.894–1.549), respectively. Thus, existing evidence, including our findings, suggests that despite worse clinical outcomes in patients with CLTI, the need for repeat revascularization may not significantly differ from that in patients with IC.
These paradoxical findings of similar repeat revascularization rates despite markedly poorer outcomes in patients with CLTI raise important questions regarding the current treatment patterns. These findings may indicate that patients with CLTI do not receive sufficiently aggressive and timely interventions despite a higher risk of adverse events. Although various treatment options and dedicated guidelines are available for CLTI, late presentation and delayed management frequently increase the risk of amputation. Current guidelines emphasize the importance of diagnostic imaging in revascularization strategies in patients with CLTI [5]. However, the timing and aggressiveness of the treatment approaches in real-world practice are heterogeneous. Patients often undergo major amputations without proper angiographic evaluation [21]. As shown in Supplementary Table S5, the proportion of patients undergoing repeat PTA following symptom aggravation was similar between CLTI and IC, yet 11.7% of CLTI patients proceeded directly to amputation without any repeat EVT. This gap suggests that, despite having a substantially higher disease burden, a subset of patients with CLTI may not receive sufficiently timely reintervention. Below-the-knee procedures are technically challenging, time-consuming, and associated with poorer-than-usual long-term patency rates in this population. Thus, systematic evaluation of the vascular status and prompt revascularization are key elements affecting the management of CLTI. Our findings suggest that more intensive monitoring and structured follow-up protocols are essential for patients with CLTI, as similar rates of repeat revascularization, despite a higher amputation risk, may indicate suboptimal surveillance.
The ‘leave nothing behind’ strategy, using a drug-eluting device, is preferred for the management of extensive FPA disease. The findings of the present study indicated that compared with other treatment strategies, EVT with DCB was associated with a lower risk of target limb amputation or CD-TER, loss of clinical patency, MALEs, and all-cause mortality. Randomized clinical trials have confirmed the superiority of DCB over POBA in terms of its ability to reduce the incidence of binary restenosis and target lesion revascularization (TLR) in patients with relatively short FPA lesions. Moreover, prospective registry studies have indicated the efficacy of DCB in the management of more complex FPA lesions, including diffuse lesions and in-stent restenosis [22,23,24,25,26,27]. Compared with POBA, EVT with DCB significantly improves primary patency [6,7]. A previous study comparing EVT with DCB and DES revealed that patency rates were similar in both groups [8,9]. In contrast, the TLR rate associated with EVT with BMS was higher than that associated with POBA, possibly because of the increased risk of restenosis from the metallic scaffold without antiproliferative drug effects. The findings of the present study further support these observations, demonstrating that EVT with DCB is associated with a lower risk of adverse events than the other treatment strategies.
In this cohort, we observed that DCB and DES have gradually become the forefront devices in the management of FPA disease, with their use increasingly marked since the mid-2010s. Consistent with this shift in real-world practice, there was a progressive decline in POBA and BMS during the study period. Although EVT technology has evolved substantially over the 15-year study period, our sensitivity analysis stratified by enrollment era (2006–2014 and 2014–2021) showed that comparative clinical outcomes between patients with CLTI and IC remained consistent across periods. This suggests that advancements in device technology did not modify the fundamental differences in prognosis between CLTI and IC, indicating that disease biology rather than EVT remains the primary driver of outcomes. Comprehensive management, including optimal medical therapy, aggressive risk-factor control, and rehabilitation, may have an additional role in improving the prognosis of patients with CLTI in addition to EVT.
The findings of this study should be interpreted within the context of certain limitations. First, given the retrospective nature of this multicenter registry study, the potential for selection and information biases could not be entirely excluded. Although the IPTW analysis was conducted to mitigate these biases, unmeasured confounding factors may have influenced the outcomes. Second, the absence of the wound, ischemia, and foot infection classification limits the detailed evaluation of severity. Third, variability in device selection and procedural strategies may exist due to reliance on individual physician discretion. Fourth, routine imaging and functional assessments used to evaluate vessel patency after the procedure were not uniform. Fifth, in the subgroup analyses of treatment strategies and clinical outcomes, the choice of device was left to the operator’s discretion. Therefore, these findings should be interpreted with caution, as differences in lesion characteristics, along with indication bias, may have influenced the selection of devices and consequently the observed outcomes. Sixth, in cases of technical failure or peri-procedural complications after EVT, such as flow-limiting dissection, vascular rupture, or access-site events, detailed information on subsequent management strategies was not systematically captured in the registry, and post-complication treatments may have varied among operators. Our dataset does not provide information on whether these cases required surgical conversion or other adjunctive procedures. Thus, detailed therapeutic approaches to failed EVT cannot be fully assessed. Finally, variations in postoperative medical management, including antiplatelet therapy duration and medication adherence across participating centers, might represent additional unaccounted confounders. Especially, longitudinal information on drug adherence was not available. Although dual antiplatelet therapy was recommended for more than 6 months following EVT, actual post-discharge medical treatment was at the discretion of the physicians.
5. Conclusions
This real-world registry study of patients undergoing EVT for FPA disease demonstrated that the clinical outcomes of patients with CLTI were worse than those of patients with IC. However, this difference in outcomes did not extend to the risk of repeat PTA, which was similar in both groups at the 2-year follow-up. The present study revealed that compared to POBA, the use of DCB was associated with superior outcomes in both groups.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm14248919/s1, Figure S1: Temporal trend of the device used (2006–2021); Figure S2: Two-year amputation-free survival according to clinical presentation and Rutherford classification; Table S1: List of devices; Table S2: Clinical outcomes after EVT stratified by treatment era (2006–2014 and 2014–2021); Table S3: Baseline characteristics and laboratory findings stratified by treatment strategy; Table S4: Angiographic and procedural characteristics stratified by treatment strategy; Table S5: Patients who experienced worsening symptom after EVT.
Author Contributions
Conceptualization: S.P., C.U.C., S.-W.R. and C.G.P.; Data curation: M.R.M.P.S., S.Y.C. and B.G.C.; Formal analysis: S.P. and B.G.C.; Investigation: S.-W.R., Y.-G.K., D.C., J.-H.L., C.-H.Y., I.-H.C., C.W.Y., S.W.L., S.H.C. and P.-K.M.; Methodology: S.P. and S.-W.R.; Supervision: S.-W.R., Y.-G.K., D.C., J.-H.L., C.-H.Y., I.-H.C., C.W.Y., S.W.L., S.H.C. and P.-K.M.; Visualization: S.P. and B.G.C.; Writing—original draft: M.R.M.P.S. and S.P.; Writing—review and editing: S.P. and S.-W.R. The K-VIS (Korean Vascular Intervention Society) Investigators contributed to data collection and provided overall support for the conduct of this multicenter registry. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Korea University Guro Hospital (IRB No. 2019GR0378; protocol code K2019-1335-002, approved on 14 October 2019, and extended through June 2022). All participating institutions obtained approval from their local IRB review boards before data collection.
Informed Consent Statement
Written informed consent was obtained from all the prospectively enrolled patients. For retrospectively collected cases, the requirement for informed consent was waived by the Institutional Review Boards of the participating centers.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding author upon request.
Acknowledgments
The authors would like to express their sincere gratitude to all participating patients as well as to the K-VIS investigators and clinical staff at each center for their dedication, cooperation, and valuable contributions to this registry.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CLTI | critical limb-threatening ischemia |
| DCB | drug-coated balloon |
| DES | drug-eluting stent |
| FPA | femoropopliteal artery |
| IC | intermittent claudication |
| IPTW | inverse probability weighting |
| POBA | plain old balloon angioplasty |
| PTA | percutaneous transluminal angioplasty |
References
- Shu, J.; Santulli, G. Update on peripheral artery disease: Epidemiology and evidence-based facts. Atherosclerosis 2018, 275, 379–381. [Google Scholar] [CrossRef]
- Ko, Y.-G.; Ahn, C.-M.; Min, P.-K.; Lee, J.-H.; Yoon, C.-H.; Yu, C.W.; Lee, S.W.; Lee, S.-R.; Choi, S.H.; Koh, Y.S.; et al. Baseline Characteristics of a Retrospective Patient Cohort in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry. Korean Circ. J. 2017, 47, 469–476. [Google Scholar] [CrossRef]
- Lee, S.J.; Lee, H.H.; Ko, Y.G.; Ahn, C.M.; Lee, Y.J.; Kim, J.S.; Kim, B.K.; Hong, M.K.; Chang Kim, H.; Yu, C.W.; et al. Device Effectiveness for Femoropopliteal Artery Disease Treatment: An Analysis of K-VIS ELLA Registry. JACC Cardiovasc. Interv. 2023, 16, 1640–1650. [Google Scholar] [CrossRef]
- Varu, V.N.; Hogg, M.E.; Kibbe, M.R. Critical limb ischemia. J. Vasc. Surg. 2010, 51, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Mazzolai, L.; Teixido-Tura, G.; Lanzi, S.; Boc, V.; Bossone, E.; Brodmann, M.; Bura-Riviere, A.; De Backer, J.; Deglise, S.; Della Corte, A.; et al. 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. Eur. Heart J. 2024, 45, 3538–3700. [Google Scholar] [CrossRef] [PubMed]
- Tepe, G.; Laird, J.; Schneider, P.; Brodmann, M.; Krishnan, P.; Micari, A.; Metzger, C.; Scheinert, D.; Zeller, T.; Cohen, D.J.; et al. Drug-coated balloon versus standard percutaneous transluminal angioplasty for the treatment of superficial femoral and popliteal peripheral artery disease: 12-month results from the IN.PACT SFA randomized trial. Circulation 2015, 131, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, K.; Jaff, M.R.; White, C.J.; Rocha-Singh, K.; Mena-Hurtado, C.; Metzger, D.C.; Brodmann, M.; Pilger, E.; Zeller, T.; Krishnan, P.; et al. Trial of a Paclitaxel-Coated Balloon for Femoropopliteal Artery Disease. N. Engl. J. Med. 2015, 373, 145–153. [Google Scholar] [CrossRef]
- Liistro, F.; Angioli, P.; Porto, I.; Ducci, K.; Falsini, G.; Ventoruzzo, G.; Ricci, L.; Scatena, A.; Grotti, S.; Bolognese, L. Drug-Eluting Balloon Versus Drug-Eluting Stent for Complex Femoropopliteal Arterial Lesions: The DRASTICO Study. J. Am. Coll. Cardiol. 2019, 74, 205–215. [Google Scholar] [CrossRef]
- Bausback, Y.; Wittig, T.; Schmidt, A.; Zeller, T.; Bosiers, M.; Peeters, P.; Brucks, S.; Lottes, A.; Scheinert, D.; Steiner, S. Drug-Eluting Stent Versus Drug-Coated Balloon Revascularization in Patients with Femoropopliteal Arterial Disease. J. Am. Coll. Cardiol. 2019, 73, 667–679. [Google Scholar] [CrossRef]
- Gouëffic, Y.; Torsello, G.; Zeller, T.; Esposito, G.; Vermassen, F.; Hausegger, K.A.; Tepe, G.; Thieme, M.; Gschwandtner, M.; Kahlberg, A.; et al. Efficacy of a Drug-Eluting Stent Versus Bare Metal Stents for Symptomatic Femoropopliteal Peripheral Artery Disease: Primary Results of the EMINENT Randomized Trial. Circulation 2022, 146, 1564–1576. [Google Scholar] [CrossRef]
- Rabellino, M.; Zander, T.; Baldi, S.; Nielsen, L.G.; Aragon-Sanchez, F.J.; Zerolo, I.; Llorens, R.; Maynar, M. Clinical follow-up in endovascular treatment for TASC C-D lesions in femoro-popliteal segment. Catheter. Cardiovasc. Interv. 2009, 73, 701–705. [Google Scholar] [CrossRef]
- Mohamedali, A.; Kiwan, G.; Kim, T.; Zhang, Y.; Zhuo, H.; Tonnessen, B.; Dardik, A.; Chaar, C.I.O. Reinterventions in Patients with Claudication and Chronic Limb Threatening Ischemia. Ann. Vasc. Surg. 2022, 79, 56–64. [Google Scholar] [CrossRef]
- Chen, S.L.; Whealon, M.D.; Kabutey, N.K.; Kuo, I.J.; Sgroi, M.D.; Fujitani, R.M. Outcomes of open and endovascular lower extremity revascularization in active smokers with advanced peripheral arterial disease. J. Vasc. Surg. 2017, 65, 1680–1689. [Google Scholar] [CrossRef]
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [PubMed]
- Nehler, M.R.; Duval, S.; Diao, L.; Annex, B.H.; Hiatt, W.R.; Rogers, K.; Zakharyan, A.; Hirsch, A.T. Epidemiology of peripheral arterial disease and critical limb ischemia in an insured national population. J. Vasc. Surg. 2014, 60, 686–695.e2. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, A.T.; Allison, M.A.; Gomes, A.S.; Corriere, M.A.; Duval, S.; Ershow, A.G.; Hiatt, W.R.; Karas, R.H.; Lovell, M.B.; McDermott, M.M.; et al. A call to action: Women and peripheral artery disease: A scientific statement from the American Heart Association. Circulation 2012, 125, 1449–1472. [Google Scholar] [CrossRef] [PubMed]
- Ryu, G.W.; Park, Y.S.; Kim, J.; Yang, Y.S.; Ko, Y.G.; Choi, M. Incidence and Prevalence of Peripheral Arterial Disease in South Korea: Retrospective Analysis of National Claims Data. JMIR Public Health Surveill. 2022, 8, e34908. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Park, Y.J.; Min, S.-I.; Kim, S.Y.; Ha, J.; Kim, S.J.; Kim, H.-S.; Yoon, B.-W.; Min, S.-K. High Prevalence of Peripheral Arterial Disease in Korean Patients with Coronary or Cerebrovascular Disease. J. Korean Med. Sci. 2012, 27, 625–629. [Google Scholar] [CrossRef]
- Reijnen, M.M.P.J.; van Wijck, I.; Brodmann, M.; Micari, A.; Torsello, G.; Rha, S.-W.; Menk, J.; Zeller, T.; On behalf of the IN.PACT Global Study Investigators. Five-Year Outcomes after Paclitaxel Drug-Coated Balloon Treatment of Femoropopliteal Lesions in Diabetic and Chronic Limb-Threatening Ischemia Cohorts: IN.PACT Global Study Post Hoc Analysis. Cardiovasc. Interv. Radiol. 2023, 46, 1329–1345. [Google Scholar] [CrossRef]
- Kawarada, O.; Zen, K.; Hozawa, K.; Obara, H.; Matsubara, K.; Yamamoto, Y.; Doijiri, T.; Tamai, N.; Ito, S.; Higashimori, A.; et al. Characteristics, Antithrombotic Patterns, and Prognostic Outcomes in Claudication and Critical Limb-Threatening Ischemia Undergoing Endovascular Therapy. J. Endovasc. Ther. 2022, 31, 622–633. [Google Scholar] [CrossRef]
- Goodney, P.P.; Holman, K.; Henke, P.K.; Travis, L.L.; Dimick, J.B.; Stukel, T.A.; Fisher, E.S.; Birkmeyer, J.D. Regional intensity of vascular care and lower extremity amputation rates. J. Vasc. Surg. 2013, 57, 1471–1480.e3, discussion 1479–1480. [Google Scholar] [CrossRef]
- Dake, M.D.; Ansel, G.M.; Jaff, M.R.; Ohki, T.; Saxon, R.R.; Smouse, H.B.; Snyder, S.A.; O’Leary, E.E.; Tepe, G.; Scheinert, D.; et al. Sustained safety and effectiveness of paclitaxel-eluting stents for femoropopliteal lesions: 2-year follow-up from the Zilver PTX randomized and single-arm clinical studies. J. Am. Coll. Cardiol. 2013, 61, 2417–2427. [Google Scholar] [CrossRef]
- Thieme, M.; Von Bilderling, P.; Paetzel, C.; Karnabatidis, D.; Perez Delgado, J.; Lichtenberg, M. The 24-Month Results of the Lutonix Global SFA Registry: Worldwide Experience with Lutonix Drug-Coated Balloon. JACC Cardiovasc. Interv. 2017, 10, 1682–1690. [Google Scholar] [CrossRef]
- Schmidt, A.; Piorkowski, M.; Görner, H.; Steiner, S.; Bausback, Y.; Scheinert, S.; Banning-Eichenseer, U.; Staab, H.; Branzan, D.; Varcoe, R.L.; et al. Drug-Coated Balloons for Complex Femoropopliteal Lesions: 2-Year Results of a Real-World Registry. JACC Cardiovasc. Interv. 2016, 9, 715–724. [Google Scholar] [CrossRef]
- Brodmann, M.; Keirse, K.; Scheinert, D.; Spak, L.; Jaff, M.R.; Schmahl, R.; Li, P.; Zeller, T. Drug-Coated Balloon Treatment for Femoropopliteal Artery Disease: The IN.PACT Global Study De Novo In-Stent Restenosis Imaging Cohort. JACC Cardiovasc. Interv. 2017, 10, 2113–2123. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.; Ullery, B.W.; Kret, M.R.; Lee, J.T. Real-World Performance of Paclitaxel Drug-Eluting Bare Metal Stenting (Zilver PTX) for the Treatment of Femoropopliteal Occlusive Disease. Ann. Vasc. Surg. 2017, 38, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Gray, W.A.; Keirse, K.; Soga, Y.; Benko, A.; Babaev, A.; Yokoi, Y.; Schroeder, H.; Prem, J.T.; Holden, A.; Popma, J.; et al. A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): A randomised, non-inferiority trial. Lancet 2018, 392, 1541–1551. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).