Abstract
Background/Objectives: Delirium is a common and serious neurocognitive disorder among hospitalised adults, which is associated with prolonged hospital stays, increased treatment costs, and increased mortality. Nurses, as healthcare professionals in constant contact with patients, play crucial roles in the early recognition, prevention, and management of delirium. This systematic review aimed to synthesise the evidence on nursing roles and interventions in the recognition, prevention, and treatment of delirium in hospitalised adult patients. Methods: A systematic literature search was conducted in PubMed/MEDLINE, Scopus, and CINAHL/EBSCO for studies published between January 2015 and August 2025. The protocol was registered in PROSPERO. Results: Out of the 3791 records identified, 39 met the inclusion criteria. Studies included randomised controlled trials, systematic reviews, and cross-sectional studies conducted in various hospital settings. Key nursing roles included early detection of risk factors, routine use of tools (e.g., CAM, CAM-ICU, 4AT), and implementation of multicomponent nonpharmacological prevention programs for patients with delirium. The evidence regarding the effectiveness of nurse-led interventions has been mixed: several studies reported reductions in delirium incidence and duration with early mobilisation, sleep promotion, cognitive stimulation, pain control and family involvement, whereas others reported no statistically significant effects. Conclusions: Routine screening, targeted nonpharmacological interventions, and interdisciplinary collaboration are essential for improving delirium-related outcomes. However, the findings should be interpreted with caution due to differences in the study design, variability in nursing practice across countries, and language restrictions that may have limited the scope of the review. Further high-quality studies are needed to clarify the impact of specific nursing-led strategies on delirium outcomes.
1. Introduction
Delirium is an acute neuropsychiatric disorder that results in the loss of the ability to perceive, purposefully recognise stimuli from the environment, process them, and respond appropriately to the information received. Even if a person remains conscious, their cognitive functions undergo qualitative changes [,]. In medical classifications (e.g., ICD-10/ICD-11, DSM-5), delirium is defined as an acute, transient disturbance of a person’s consciousness and cognitive function [,]. It is a set of symptoms characterised by a sudden change in mental state, developing over a short period of time—from a few hours to a few days, rarely months—with a variable course and a significant impact on the patient’s prognosis [,]. The medical literature also describes “persistent delirium,” in which symptoms of cognitive impairment can persist for months or even years after discharge from the hospital. The incidence of delirium among hospitalised patients varies greatly depending on the population, type of ward, and assessment methods used. In general wards, it occurs in approximately 20–30% of patients, whereas in intensive care units, the incidence can reach as high as 70%. In patients who have undergone major surgery or have neurological diseases (e.g., after a stroke), delirium occurs in 25–50% of patients. In the population of older adults treated on an emergency basis, this percentage is usually 10–15% [,,,]. Delirium is a relatively common complication among hospitalised adults. Its prevalence is influenced by the characteristics of the population, the type of hospital ward, and the diagnostic methods employed []. It is estimated to occur in 10–80% of patients [,,,], particularly in elderly individuals, after stroke, in postoperative patients (20–50% of individuals over 60) [] and patients treated in intensive care units (ICUs) [,,,]. Mechanically ventilated patients are at particularly high risk, with delirium occurring in 50–70% of cases [,,]. Delirium is common in individuals who have survived cardiac arrest (CA) [,], and is least common among gynecological patients [].
There are three subtypes of delirium: hyperactive, hypoactive, or mixed [,]. Despite its prevalence, delirium often goes unrecognised, especially in its hypoactive form [,,,], which can resemble fatigue [], depression, or dementia []. Studies indicate that in ICUs and hospital emergency departments, symptoms of delirium remain undiagnosed in 66–84% of cases []. Delirium is secondary in nature and most often results from an underlying disease, injury, or external factor. Factors such as age, immobilisation (e.g., due to the presence of catheters or as a result of physical restraint), sleep disorders, malnutrition, the use of sedatives and analgesics, and hospitalisation in an ICU contribute to the onset of delirium []. These factors can be divided into predisposing (basic) and triggering (acute) factors [,,]. Effective treatment requires identification of the cause, which is often a combination of several coexisting factors [,].
Despite the availability of validated screening tools and international guidelines, the problem of undiagnosed delirium remains relevant. In 2025, updated international guidelines for the prevention and management of delirium were published [], and in 2023, recommendations for adult patients undergoing surgery were published []. Recent studies indicate that although screening tools are available, their use in clinical practice, even in intensive care units, is not standard [,,,]. Owing to the lack of effective pharmacological prevention methods [], nonpharmacological strategies play a key role, including nursing activities focused on early diagnosis and prevention of delirium []. Owing to their constant contact with patients, they play a key role in observing mental health, implementing preventive procedures, and supporting treatment [].
Although the clinical aspects, risk factors, and effects of delirium are well described, the contribution and importance of nursing practice in this area remain insufficiently defined. Previous reviews have focused mainly on pharmacological treatment or an interdisciplinary approach, often overlooking the specific responsibilities and activities of nurses in the care of patients with delirium. There is also a lack of synthesis of data on the effectiveness of nursing interventions aimed at early diagnosis, prevention, and treatment of delirium in various hospital settings. This gap justifies the need for a systematic review of nursing roles and interventions in the care of patients with delirium.
The aim of this review is to synthesise evidence from studies published between 2015 and 2025 and to address the role of nurses in the prevention, recognition, and management of delirium in hospitalised patients.
2. Methods
This systematic review was conducted in accordance with the PRISMA 2020 guidelines, which provide standardised criteria for conducting and reporting systematic reviews, ensuring transparency and reproducibility. The protocol was registered in the PROSPERO database (registration number: CRD420251143918).
2.1. Search Strategies
A systematic literature search was conducted in three databases: PubMed/MEDLINE, Scopus, and CINAHL/EBSCO. The search covered publications from the last 10 years (from 1 January 2015 to August 2025). The search strategy included combinations of the following keywords: (delirium OR confusion OR agitation OR (neurocognitive AND disorder*) OR (cognitive AND impairment) OR (acute AND confusional AND state) OR (acute AND confusion) OR inattention OR (consciousness AND disorder*) OR (cognitive AND disorder*) OR (neuropsychological AND disorder*) OR disorientation) AND ((intensive AND care AND unit*) OR ICU OR Non-ICU OR (critical AND care) OR (acute AND critical) OR (care AND unit) OR hospital* OR “general ward” OR “medical ward” OR “geriatric ward” OR “internal medicine” OR “neurology ward” (perioperative AND care))) AND (((nonpharmacolog* OR environmental OR multicomponent OR package) AND (care OR intervention* OR management OR prevent* OR treat* OR therap* OR assessment OR monitoring OR diagnosis OR role)) AND (nurse* OR nursing OR nurses)). The keywords have been tailored to the specific characteristics of each database. All databases (PubMed/MEDLINE, Scopus, and CINAHL/EBSCO) were last searched in October 2025. No additional sources, registers, or organisational websites were searched beyond these databases.
2.2. Inclusion and Exclusion Criteria
The review included studies published between 2015 and 2025 that focused on hospitalised adult patients (≥18 years). Eligible articles assessed nurses’ knowledge of delirium and described nursing activities, the role of nurses, or nursing interventions related to delirium in the care of adult patients in hospitals. Only full-text publications available online or as PDF files on scientific platforms and written in Polish or English were considered.
The review excluded studies focusing solely on pharmacotherapy without the involvement of nursing staff or pediatric populations. Works not available in full text, including conference abstracts, letters to the editor, and comments, were also omitted. In addition, studies concerning patients at home after hospital discharge and records that did not constitute original studies were excluded.
The selection of scientific articles was carried out by verifying titles, abstracts, and full texts via relevant keywords (Table 1). The number of excluded articles was 2460. The most common reasons for exclusion were studies that did not involve nursing staff, studies focusing exclusively on pharmacological treatment, studies without results related to delirium, conference abstracts, and articles not available in full text.

Table 1.
The selection of articles included in the analysis.
2.3. Information on the Included Literature
The scientific literature search was conducted in the following databases: PubMed/MEDLINE, Scopus, and CINAHL/EBSCO. To increase the precision of the search, database filters were applied, including full-text availability and publication date between 2015 and 2025. Two independent authors reviewed the titles and abstracts of the articles. In cases of discrepancies, the decision was made jointly or with the participation of a third reviewer. The selection process is presented in the PRISMA diagram (Figure 1). The completed PRISMA checklist is provided in the Supplementary Material. All included papers met the predefined inclusion criterion of being available in full text at the time of the review process–either as open-access publications or through institutional access enabling full-text download in PDF format. Therefore, the selection process remained consistent with the eligibility criteria, which focused on full-text accessibility, rather than strictly on open-access licensing status.
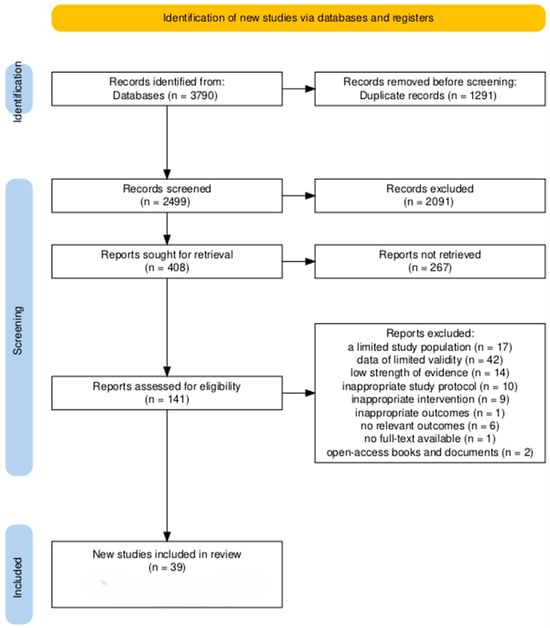
Figure 1.
The PRISMA flowchart was created via the tool [].
2.4. Data Extraction
The data were extracted via a standardised form. The following information was extracted from each study: the author and year of publication, the country and setting of the study, the study design, and the characteristics of the population. The data also included a description of the nursing interventions; results related to the recognition, prevention, or treatment of delirium; and the delirium assessment tools applied (e.g., Confusion Assessment Method–CAM; Confusion Assessment Method for the Intensive Care Unit-CAM-ICU; Intensive Care Delirium Screening Checklist-ICDSC). Data extraction was performed independently by two reviewers via a standardised form. Any discrepancies were resolved through discussion or consultation with a third reviewer. The primary outcomes that were analysed included nurses’ knowledge of delirium, their professional role, and nonpharmacological interventions related to the recognition, prevention, and treatment of delirium. All available results within these thematic areas were obtained from each study.
2.5. Data Synthesis
Owing to the diversity of study designs, populations, and outcome measures, a narrative synthesis was conducted in four stages: (I) summarising the results of each study in Table 1; (II) analysing the associations on the basis of the type of intervention and clinical context; (III) organising the results into thematic categories; and (IV) assessing the quality of the studies, methodological limitations, and consistency of the results across different settings. This approach allowed the identification of common themes in nursing practice related to the care of patients with delirium. No statistical effect measures (e.g., risk ratios, mean differences) were calculated, as the heterogeneity of study designs and outcomes precluded quantitative synthesis. Studies were assigned to one of the three synthesis categories (diagnosis, prevention, or therapeutic interventions) on the basis of the primary focus and type of nursing activity described. This categorisation was guided by tabulated study characteristics, including intervention type, setting, and outcome domain. The overall selection process is illustrated in a PRISMA 2020 flow diagram (Figure 1).
2.6. Study Risk of Bias Assessment
The assessment of the bias risk of each study was performed independently by two reviewers using predetermined methodological criteria, following the PRISMA guidelines, and contributed to the overall interpretation of the evidence. Factors such as clarity of the study’s purpose, appropriateness of the research design to the questions posed, method of sampling, clarity of results presentation, and presence of potential conflicts of interest were considered. In the case of discrepancies between assessments, decisions were made through discussion or with a third reviewer. We applied the Checklist for Qualitative Research (JBI Critical Appraisal Tools) [] and the AMSTAR-2 tool [] to assess the methodological quality of the included studies. The bias risk assessment served as one of the criteria in the final interpretation of the quality and reliability of the collected data.
The potential risk of reporting bias (bias due to missing or selectively reported results) was assessed qualitatively. The reviewers compared the outcomes reported in the included studies with those specified in the study objectives and methods sections. No formal statistical assessment was performed, as the synthesis was descriptive.
3. Results
The review yielded a total of 3790 relevant studies. After the titles and abstracts were reviewed, 408 papers were included. After analysis, a total of 39 literature items that met the selection criteria were obtained. The largest groups consisted of systematic reviews and meta-analyses (n = 13), and original papers (n = 13), followed by systematic reviews (n = 6). Other types of articles included meta-analyses (n = 2), and individual publications: secondary analyses of survey data, scoping reviews, umbrella reviews, narrative reviews and Cochrane reviews (each n = 1).
In our work, certain articles, such as [], were excluded. The main focus is on patient experiences rather than specific nursing activities or nursing interventions in relation to the assessment, prevention, or treatment of delirium []. Articles concerning nursing home residents were excluded []. We considered the conditions of patients in hospitals.
3.1. Characteristics of the Included Studies
The review included studies that met the inclusion criteria. The studies were conducted in Europe, Asia, North America, and Australia, among other places, which increases their external validity. Table 2 contains the detailed characteristics of the included studies.

Table 2.
Detailed characteristics of included studies.
On the basis of the numerical summary, most studies focused on patients in ICUs and critically ill patients, with nine articles in each of these groups. Studies on patients hospitalised outside intensive care units or from various hospital wards were equally well represented (n = 23). A slightly smaller percentage of studies concerned postoperative and surgical patients (n = 6), whereas individual studies covered specific populations, such as perioperative patients (n = 1), elderly people (n = 4), patients’ families (n = 1), and emergency department patients (n = 1) (Table 2). In addition, three articles concerned nursing staff, including nurses working in intensive care units, which indicates an interest in the subject of knowledge, attitudes, and professional practices in the care of patients with delirium. The studies analysed focused primarily on critically ill patients hospitalised in ICUs, whereas studies involving other clinical groups were of lesser importance.
In the present review of works, the most numerous group consisted of publications on nonpharmacological interventions (n = 17). The review also included articles on multicomponent interventions (n = 3), interventions targeting sleep and circadian rhythm (n = 3), cognitive function/anxiety/education/staff stress (n = 3), and pharmacological and mixed interventions (n = 2). A slightly smaller percentage of studies concerned sensory interventions, family participatory interventions, cognitive aspects/staff stress and factor analysis.
Some studies have focused on ICUs, where patient monitoring is continuous and covers critical conditions [,,]. Others focus on general hospital wards, where nursing interventions must be more targeted and adapted to less intensive care settings []. Some publications describe comprehensive multicomponent interventions covering assessment, prevention, and treatment [,,]. Others focus mainly on the diagnosis and early detection of delirium symptoms, without discussing therapeutic interventions in detail []. Some articles are primary research studies, including RCTs and nurse-led studies [,]. Others are systematic reviews or meta-analyses covering multiple studies, which allow for the generalisation of results but limit the detailed description of nursing practices [,,,,] (Table 2).
3.2. The Role of Nurses in Delirium Diagnosis
An analysis of selected publications indicated that nurses play a key role in the early recognition of delirium, patient monitoring (observation, documentation) and communication with the medical teams. Among the analysed studies, 10 articles referred to the diagnosis of delirium. These studies concerned patients [,,,,,,] and nursing staff [,,]. The goal of nurses is to recognise and identify delirium early via appropriate tools. Among the publications analysed, particular emphasis on the diagnosis of delirium was placed on work [,,,,,,,,,]. Goettel and Wueest focused directly on diagnostic methods for delirium []. However, it should be noted that most of the studies covered a much broader range of topics and were not devoted exclusively to the diagnosis of delirium (Table 3). For example, Wang and colleagues studied psychological stress in nurses caring for patients with delirium, and this stress affected their ability to assess and recognise the disorder []. In turn, Koirala et al. and McCoy et al. provided epidemiological data that serve as background information justifying the need for effective delirium diagnostics [,]. Other studies have focused on nurses’ knowledge, attitudes, practices, stress and factors associated with caregiving that affect their ability to correctly diagnose this disorder [,].

Table 3.
Assigning publications to specific subject areas.
Despite the common goal of improving the quality of care for patients with delirium, studies differ in terms of the clinical setting [,,,,] scope of intervention, and assessment methods used. Most papers emphasise that nurses are the first link in identifying symptoms of delirium, because of to their daily contact with patients [,,,,,,,,,]. In most studies, nurses use standardised tools such as the CAM-ICU, 4AT, or ICDSC, which allow for systematic monitoring of patients in different hospital wards [,,]. Notably, however, the 4AT and ICDSC are primarily screening tools, whereas the CAM is used for the diagnostic confirmation of delirium. Early identification of delirium symptoms by nurses is emphasised in all analysed studies as crucial for reducing the severity and duration of delirium [,,,].
Despite differences in clinical settings, methodologies, and scopes of intervention, all studies emphasise the key role of nurses in diagnosing and monitoring delirium. The common conclusion is the need for systematic assessment of patients and the use of standardised diagnostic tools, which enables early intervention and improved clinical outcomes. Differences between studies, however, indicate the need to adapt nursing strategies to the specific characteristics of the ward and the individual needs of patients. The literature shows a lack of interventional studies evaluating the effectiveness of training programs aimed at improving nurses’ diagnostic skills in recognising delirium. Existing studies focus mainly on describing the level of knowledge and attitudes. The impact of occupational stress and workload on the accuracy of delirium diagnosis also remains poorly understood—there are mainly cross-sectional studies, without analyses of cause-and-effect relationships. In addition, research on the diagnosis of delirium in nursing mainly covers intensive care and surgical wards, whereas other clinical contexts, such as emergency, geriatric, and neurological wards, are underrepresented, limiting the possibility of generalising the results to a wider patient population.
3.3. Preventive Interventions Undertaken by Nurses
Most publications (n = 24) concerned prevention, preventive measures, nonpharmacological interventions, and care programs [,,,,,,,,,,,,,,,,,,,,,,] (Table 3). In the studies included (Table 1), the effectiveness of multicomponent nonpharmacological interventions conducted by nurses for preventing delirium varied considerably depending on the clinical setting and study design. While several meta-analyses and original studies have shown beneficial effects, particularly in reducing the incidence of delirium, others have shown no statistically significant improvement in primary outcomes such as duration, severity, or mortality. The positive effects of interventions carried out by nurses have been noted in systematic reviews and original studies focusing on multicomponent strategies combining orientation, sleep hygiene, sensory optimisation, and family involvement [,,,,,,,,,,]. These interventions, often implemented by multidisciplinary teams, are associated with a reduction in the duration of delirium, improved patient orientation, or a shorter stay in the intensive care unit. For example, the Dy-Del program effectively reduced both the incidence and duration of delirium [], whereas multicomponent protocols based on sleep and circadian rhythms showed similar benefits in intensive care unit patients and perioperative patients [,,]. Several studies emphasise that effective delirium prevention is primarily based on nonpharmacological interventions, which are an integral part of a nurse’s work [,,,]. Publications emphasise the role of nurses in implementing nonpharmacological strategies, such as reorientation, cognitive stimulation, early mobilisation, and family support, which aid in the prevention and treatment of delirium [,,,,]. The most commonly reported nonpharmacological strategies include orienting the patient in time and space. Other important measures include ensuring adequate pain control while limiting medications with depressant effects on the nervous system, as well as promoting early mobilisation and cognitive activation []. Special emphasis is placed on the implementation of multicomponent prevention programs that integrate several of these interventions simultaneously []. Some studies conducted in specific clinical contexts reported no significant reduction in delirium incidence following nurse-led or multicomponent preventive programs, especially in surgical, cardiac-surgery, and geriatric settings [,,,,,].
Nurses play a key role in preventing delirium in hospitalised patients, both in general wards and ICUs. Daily contact with patients enables early detection of the first signs of cognitive impairment and the implementation of preventive measures that minimise the risk of delirium [,,,,,,,,,]. Delirium prevention is a key element of nursing care in various hospital wards, especially in intensive care and geriatric care. The most commonly used preventive measures include eight main strategies that complement each other and aim to reduce the risk of cognitive impairment. The most commonly used preventive nursing interventions include: (I) systematic monitoring and assessment of patients [,,,,,,,,,]; (II) cognitive reorientation and stimulation, which include reminding patients of the date, location, and purpose of hospitalisation, as well as brief mental exercises and conversations that support their cognitive function [,,,,,,]; (III) early mobilisation and physical activity. Early mobilisation, bedside exercises, and mobilising patients as much as possible are important elements of delirium prevention, reducing the risk of complications and improving patients’ overall functional status [,,,]; (IV) patients’ sense of comfort. Nurses ensure adequate lighting, noise reduction, a bed ensuring patient comfort and proper patient positioning. Activities also include pain control, hydration and nutrition, and elimination of stressors [,,,,,,]; (V) family support and communication, which has a positive effect on reducing the risk of delirium [,,,,,]; (VI) adapting to the patient’s circadian rhythm. Organising sleep and rest in accordance with the natural circadian rhythm and limiting nighttime disturbances promotes cognitive stability and reduces the risk of delirium [,,]; (VII) patient and healthcare team education. Nurses play an educational role, informing patients and team members about the risk factors for delirium and methods of prevention [,,,,]; and (VIII) multicomponent interventions [,,,,,,,,,,]. Combining the above measures into comprehensive prevention programs allows for more effective delirium prevention. Examples include the integration of early mobilisation, environmental control, cognitive stimulation, family support, and regular monitoring of the patient’s condition [,,].
However, many high-quality studies and reviews have not confirmed the positive effects of interventions carried out by nurses. Studies [,,,,] have shown that despite the active involvement of nursing staff, preventive programs do not lead to a significant reduction in the incidence or duration of delirium. For example, stepped-wedge RCT studies conducted in intensive care and neurology wards [,] and systematic reviews conducted by [,] did not show statistically significant differences between the intervention and control groups. Furthermore, a review [] revealed that although multicomponent interventions may help prevent delirium, their effect on duration or severity remains limited. These inconsistent results may reflect differences in interventions, patient populations, and methodological limitations. Many studies have reported small sample sizes, heterogeneous outcome measures, and inconsistent delirium assessment tools [,,,,,].
The management of modifiable risk factors remains a key component of effective delirium prevention. Further multicenter studies, particularly in the areas of intensive care and neurology, are needed to develop effective, integrated strategies for the treatment and prevention of delirium. Despite the growing number of studies, the literature indicates certain gaps. There is a lack of uniform protocols in general wards, data on the long-term effects of prevention in specific populations are limited, and the heterogeneity of studies makes comparisons between different settings difficult [,,]. Taken together, current evidence suggests that nurse-led multicomponent interventions are promising but not universally effective. Their success likely depends on adequate staff training, the patient population, and adherence to standardised protocols.
3.4. Therapeutic Interventions Undertaken by Nurses and Delirium Management
Nurses play an important role not only in the prevention of delirium but also in its treatment and management. Their activities include monitoring symptoms, implementing nonpharmacological interventions, supporting pharmacological treatment, and coordinating activities within a multidisciplinary team [,,,,,,,]. Nurses take an active part not only in diagnosis and prevention, but also in supportive treatment of patients diagnosed with delirium (Table 3). Their therapeutic interventions include both direct actions and cooperation with an interdisciplinary team []. The most commonly used therapeutic interventions include the following: (I) monitoring and early response to symptoms of delirium, enabling rapid implementation of therapeutic measures [,,]; (II) nonpharmacological interventions-cognitive reorientation and stimulation, assisting in maintaining orientation, and conversations supporting cognitive functions; environmental control and patient comfort, adequate lighting, and noise reduction, ensuring a comfortable position, and eliminating stressors; mobilisation and physical activity, bedside exercises or getting up as much as the patient is able; emotional and family support, the involvement of family in care and the provision of a sense of security and emotional support [,,,]; and (III) supporting pharmacological treatment. Nurses monitor the administration of drugs to treat delirium, including controlling doses, observing adverse effects, and working with physicians to adjust treatment [,]; (IV) coordination of a multidisciplinary team. Delirium management requires collaboration among nurses, physicians, physical therapists, psychologists, and patients’ families to implement a comprehensive therapeutic approach and monitor the effectiveness of interventions [,,]; (V) tailoring interventions to individual patient needs. Nurses modify therapeutic measures depending on the patient’s clinical condition, risk of complications, and comorbidities, which increases the effectiveness of treatment and patient safety [,].
Research indicates that measures such as early mobilisation [], effective pain management, proper nutrition, and hydration can lead to up to a 40% reduction in incidence in older adults []. A study by Sist and colleagues involving nurses revealed that nursing staff give the highest priority to activities that ensure patient safety, followed by interventions that support communication and continuous supervision []. Lower priority was given to activities related to family involvement and modification of the physical environment [].
Differences between publications on therapeutic nursing interventions can be observed in several aspects. First, they differ in the clinical setting in which the studies were conducted. Some focus on ICUs, where patients are in critical condition and delirium monitoring is continuous and requires a rapid response [,,]. Others concern general hospital wards, where nursing interventions are less intensive and activities are tailored to patients with a lower risk of delirium [,]. There are also differences in the scope of interventions. Publications Jang and Lee [] and Tovar and Castano [] concern active therapeutic measures taken by nurses aimed at reducing the symptoms of delirium in patients already affected by this disorder, rather than merely its prevention. The authors demonstrated that reducing anxiety levels through nonpharmacological measures (including emotional support, relaxation techniques, and therapeutic communication) translates into improved cognitive function and reduced severity of delirium []. They emphasise the importance of the therapeutic aspect of nursing care, which goes beyond traditional nursing activities and includes elements of supportive psychotherapy and behaviour modification []. In turn, a previous publication [] described a complex nursing-led intervention program for critically ill patients. This intervention includes continuous assessment of delirium symptoms, care, emotional support, cognitive orientation, and maintenance of circadian rhythm, which, in a clinical trial, resulted in a significant reduction in the frequency and duration of delirium []. Both articles focused on therapeutic measures taken after the onset of delirium. However, they differ in scope [] and focus on the psychological dimension of therapy, whereas [] describes a comprehensive, practical model of nursing therapeutic intervention in intensive care.
Some publications describe multicomponent interventions that combine patient monitoring, cognitive stimulation, mobilisation, environmental control, family support, and cooperation with the therapeutic team [,,]. Other articles focus mainly on selected nonpharmacological measures, such as reorientation or emotional support, without considering pharmacotherapy or team collaboration [,]. Another aspect is the inclusion of pharmacotherapy. Some articles describe the role of nurses in monitoring and supporting pharmacological treatment, including controlling drug doses and observing adverse effects [,]. Others focus exclusively on nonpharmacological interventions and do not analyse aspects of pharmacotherapy in detail [,,]. Differences are also evident in the research methodology. Some works are primary studies, including randomised controlled trials and nurse-led studies, allowing for the assessment of the direct impact of nursing interventions [,]. Others are systematic reviews or meta-analyses that synthesise the results of multiple studies, allowing for general conclusions but limiting the description of specific nursing actions in practice [,,,,]. The last difference concerns the degree to which interventions are tailored to individual patient needs. Some publications emphasise the importance of individualising interventions, taking into account age, comorbidities, and delirium risk level [,]. Others focus mainly on standard protocols and procedures, with less emphasis on personalising interventions [,]. All these differences highlight that although nurses play a central role in delirium management, the scope, intensity, and nature of interventions may vary depending on the clinical context, study methodology, and individual patient needs.
Nurses are key participants in delirium management, performing both therapeutic activities and coordinating the care team. Nonpharmacological interventions, early identification of symptoms, and monitoring of pharmacological treatment can reduce the severity of delirium, shorten its duration, and improve patients’ quality of life. Although several studies have confirmed the effectiveness of multicomponent, nurse-led interventions in preventing delirium [,,], several high-quality studies have not reported significant effects [,,,]. This mixed body of evidence indicates that the impact of such interventions may depend on the clinical context, patient characteristics, and implementation fidelity. Therefore, conclusions about the universal effectiveness of nurse-led interventions should be interpreted with caution.
4. Discussion
The role of nurses in caring for adults with delirium in hospitals is multifaceted. It focuses on identifying risk factors, preventive measures, recognising symptoms, and participating in the treatment of patients with delirium.
An analysis of the literature revealed that the role of nurses in caring for patients with delirium varies depending on the type of hospital ward, but all studies emphasised common elements of nursing care, primarily the importance of early recognition of delirium symptoms and systematic monitoring of risk factors [,,,,,,]. Studies have identified many factors that trigger delirium, including acute clinical conditions (e.g., sepsis, stroke, severe liver failure, advanced heart failure, and infections); injuries (including head injuries, fractures, and multiple organ injuries); dehydration, constipation, uncontrolled diabetes, and immobilisation; the effects of certain medications (benzodiazepines, dihydropyridines, antihistamines, anticholinergics, and opioids); and surgical interventions, especially in patients with comorbidities [,]. In the context of postoperative delirium, the authors emphasise that its occurrence results from the interaction of factors related to the patient, the course of the surgical procedure, and the anaesthesia used []. Symptoms usually appear within the first five days after surgery, with the most severe symptoms occurring between the first and third days [,]. Risk factors for delirium can be categorised as non-modifiable or modifiable. Non-modifiable factors include advanced age, visual and hearing impairments, a history of stroke, dementia, and previous episodes of mental disorders. Modifiable factors include hypertension, dehydration, metabolic disorders, anaemia, and inadequate pain management [,,,].
The results of the review confirm that the assessment of the risk of delirium should consider the patient’s clinical condition, procedural factors (e.g., type of surgery, method of anaesthesia), and environmental factors (e.g., isolation, confusion about time and place) [,]. Notably, delirium has a significant negative effect on the health of patients, especially in the elderly population. The most common consequences include prolonged artificial ventilation, increased risk of complications and adverse events (e.g., falls), cognitive impairment (e.g., memory loss, development of dementia), prolonged hospitalisation, increased treatment costs and mortality [,,,,,,,,]. For this reason, preventive and observational measures taken by nurses, consisting of systematic monitoring of patients and early recognition of risk factors and symptoms of delirium, play a key role [,]. The effective methods for preventing delirium vary depending on various factors []. The differences in the effectiveness of interventions across individual studies may be partly due to organisational factors. Differences in nursing staff workload, employment rates, and level of training in delirium may have a significant effect on the effectiveness and success of prevention programs. Several studies have identified limited staff availability and inadequate training as barriers to the consistent implementation of nonpharmacological interventions [,,]. These findings suggest that the success of delirium prevention strategies depends not only on the intervention design itself, but also on the work environment and institutional support. Nurses, as individuals who are in close and constant contact with patients, should be knowledgeable about the main risk factors for delirium and skilled in identifying it in their daily clinical practice. Scientific evidence confirms that effective monitoring of delirium contributes to reduced mortality and a shorter duration of mechanical ventilation, especially in surgical patients requiring intensive care [,]. The diagnostic process should involve conducting an interview, reviewing the medical history, and assessing the patient’s current clinical condition []. It is particularly important to compare the patient’s current mental state with their baseline state, as this allows for the identification of subtle changes in behaviour that may indicate the development of delirium [,]. The observations of family members and caregivers can also be valuable sources of information, allowing sudden cognitive changes and their fluctuations to be identified []. Particular attention should be given to attention disorders (e.g., difficulty concentrating) and changes in consciousness (e.g., agitation or apathy). The results are equally inconclusive with respect to the impact on the duration of delirium []. The most commonly described measures in the literature focus on continuous documentation of symptoms and their variability, as well as individualising care according to the type of delirium [].
One of the significant clinical challenges remains distinguishing delirium from dementia, especially in older people [,]. Delirium is characterised by sudden disturbances in attention and changes in consciousness (confusion, difficulty perceiving the environment) and impairments in cognitive functions such as memory, speech, and thinking. In dementia, however, symptoms develop gradually, and consciousness and attention remain normal []. In qualitative studies, nurses reported difficulties in distinguishing delirium from dementia, as well as uncertainty in the use of available diagnostic tools [,]. Standardised screening tools such as the CAM, CAM-ICU, 4AT, ICDSC, and Nu-DESC are essential for the rapid identification of patients at risk of delirium [,,]. Research has shown that the use of screening tools varies depending on the country and type of department []. The ICU-CAM and ICDSC dominate in ICUs, and the 4ATs in rehabilitation units, whereas clinical assessment without tools is often used in emergency departments and nursing homes. Unfortunately, many studies indicate the low use of screening tools in clinical practice, resulting, among other things, from a lack of training, work overload, and insufficient systemic support [,,,]. According to current international guidelines (updated in 2025 and published by the Society of Critical Care Medicine in 2018), all hospitalised patients should be routinely assessed for the risk of delirium (National Institute for Health and Care Excellence-NICE recommendations) [,,]. A correlation was observed between nursing staff participation in training and the frequency of use of standard diagnostic tools []. Studies have shown that as nurses’ knowledge and awareness of delirium increases, their ability to assess and manage delirium improves significantly [].
Depending on the level of psychomotor activity, delirium can be divided into three subtypes: hypoactive, hyperactive, and mixed [,,]. In hospital settings, the hypoactive subtype is most commonly observed, and is characterised by reduced reactivity [,]. Patients are often apathetic, drowsy, and withdrawn, with a limited attention span []. In addition to those in the ICU, reduced mobility, slowed reactions, impaired concentration, and decreased appetite are also observed []. The hypoactive subtype of delirium is more persistent than the hyperactive subtype [] and is often associated with poorer long-term cognitive functioning [,,]. The patient is overly alert, highly agitated, restless, uncooperative, emotionally unstable, and exhibits hyperactive delirium. Hyperactive delirium is easier for medical personnel to recognise [,]. Common features are found in the mixed subtype. It is estimated that the hypoactive subtype accounts for 11–17% of people treated in the ICU, the mixed form accounts for 7–10%, and the hyperactive form accounts for 4% [,]. However, evidence suggests that nurses have low knowledge about delirium and difficulty recognising the hypoactive subtype in particular [,]. It is generally more difficult to diagnose, as evidenced by the limited number of studies in the scientific databases searched. Nurses do not routinely use validated tools to diagnose delirium in their work. This may be due to workload, reluctance, or ignorance [,]. Nurses’ attitudes towards patients with delirium are influenced by their experience, seniority, age, and education, and participation in training correlated with knowledge and practice in the care of patients with delirium. Therefore, it is essential for all nurses, regardless of their age and experience, to deepen and update their knowledge. Nurses find it difficult to identify modifiable risk factors that should be targeted by nonpharmacological interventions, especially in the prevention of delirium. Current recommendations based on the guidelines of the Society of Critical Care Medicine suggest multicomponent nonpharmacological strategies for the prevention or treatment of delirium []. Nurses should implement nonpharmacological interventions, but evidence suggests that this is not the case, and that the incidence of delirium remains unacceptably high []. Numerous interventions are available in everyday clinical practice, but only a few have a high or moderate level of reliability [,]. For example, cognitive function can be stimulated by recalling personal memories, whereas patient orientation is maintained through regular communication [], conversation, and the involvement of a familiar family voice. Ensuring adequate hydration and nutrition is essential [], whether by encouraging oral fluid and food intake or, when necessary, administering intravenous therapy. Providing sensory aids such as glasses and hearing aids, fitting dentures, and educating family members about delirium symptoms and supportive strategies are equally important []. Additional interventions involve assessing and optimising oxygenation [,], early identification and treatment of infections, prevention of postoperative complications through monitoring and adherence to infection control guidelines, and prevention of falls and pressure ulcers. Creating a supportive hospital environment that is well lit during the day and quiet and darkened at night and incorporating music interventions as a form of supportive therapy have also been reported as effective strategies []. Reported strategies also include the use of music therapy as a form of supportive care and the avoidance of unnecessary catheterisation [,,]. Mobilisation is encouraged, including early postoperative ambulation, with appropriate walking aids provided if needed, as well as active range of motion exercises even for immobile patients [,,]. Pain assessment is emphasised, particularly in patients with communication difficulties, such as those with tracheostomy, ventilator support, or dementia. Light sedation is preferred over deep anaesthesia, which may help reduce the incidence of postoperative delirium []. Effective delirium management also relies on collaboration within the therapeutic team [], involving participation in clinical decision-making and monitoring of treatment effects [,,]. Family members are actively involved in care and decision-making processes, and they are educated about delirium symptoms and methods to support their loved ones [,,,,,,,,,]. While nonpharmacological interventions have been shown to be effective in populations hospitalised outside the ICUs, they have not shown a consistent effect on treatment in the critical care setting []. Research does not clearly show that the use of nonpharmacological preventive strategies implemented by nurses in ICUs to reduce the frequency and duration of delirium is effective [,,,,,].
Examples of comprehensive intervention packages include (I) the SP-CS-EM-PC-AS program (Sleep Promotion–Cognitive Stimulation–Early Mobilisation–Pain Control–Assessment Strategy). This intervention package, proposed by Matsuura and colleagues [], among others, has been shown to be effective in reducing the incidence of delirium. The greatest benefits were observed with the simultaneous use of cognitive stimulation and sleep promotion; (II) The ABCDEF package, recommended by the Society of Critical Care Medicine as part of the ICU PADIS guidelines [], encompasses several key components: assessment and treatment of pain (A), spontaneous breaks in ventilation and sedation (B), selection of appropriate sedatives (C), daily assessment of delirium (D), early mobilisation and exercise (E), and family involvement (F). The implementation of this bundle has been shown to effectively reduce the incidence of delirium, the duration of mechanical ventilation, and the length of hospitalisation, although practical challenges may limit its application; (III) the Hospital Elder Life Program (HELP), designed for nonintensive care units, focuses on six key strategies: improving sleep, providing sensory support, promoting mobilisation, ensuring nutritional support, maintaining reality orientation, and encouraging social-emotional engagement []. This program is widely implemented in the USA and Europe and has been shown to effectively reduce the incidence of delirium in patients aged 65 years and older who are hospitalised for surgical or medical reasons []. Protocols aimed at preventing delirium should prioritise the optimisation of modifiable risk factors []. According to NICE recommendations, patients identified as being at risk of developing delirium should receive care from familiar healthcare personnel, while all preventive interventions should be implemented by an interdisciplinary team specifically trained in delirium prevention and management [].
Despite the availability of effective protocols for preventing delirium, their implementation in clinical practice often fails due to various factors, including heavy workloads for nursing staff, insufficient training, lack of standard procedures, poor communication within the interdisciplinary team, limited institutional support, insufficient knowledge of diagnostic tools (CAM, 4AT, etc.) or their improper use, and lack of regular training. Overcoming these barriers is crucial for translating evidence-based strategies into real improvements in patient outcomes.
In summary, current evidence does not provide a clear answer for the selection of optimal nonpharmacological interventions, so it is very difficult to create uniform procedures to standardise the approach for the prevention and treatment of delirium. Moreover, no studies to date have identified interventions in relation to different types of delirium, which remains an important research gap. The focus on delirium in hospitals is justified because the impact of delirium is not limited to the patient alone, but also affects their environment, including their family. It is, therefore, the task of nurses to educate caregivers about what delirium is and how to provide care when delirium occurs.
5. Limitations
Although the literature review provides valuable information, it is not without certain limitations regarding the scope of the analysed works, the availability of the latest data, and the risk of publication bias, which may affect the completeness and generalisability of the conclusions. The most important of these are as follows: (I) most of the included works are review articles; (II) despite the consistency of the analysed publications the nurses’ working conditions vary significantly across countries; and (III) although the review was prepared in a systematic manner, there is a risk that some relevant material may have been omitted owing to limited access. An additional difficulty was the limitation of the analysis to publications in English and Polish only, which may have resulted in other valuable studies not being taken into account.
6. Implications for Practice
The evidence from multiple studies highlights the central and multifaceted role of nurses in preventing and managing delirium in hospitalised patients, particularly in intensive care and postoperative settings. Nurses are uniquely positioned to implement both nonpharmacological and pharmacological interventions because of their continuous patient contact and holistic understanding of patient needs. They are responsible for early detection, risk assessment, and timely initiation of interventions aimed at minimising the incidence, duration, and severity of delirium. A key implication for practice is the need for the systematic use of standardised screening and diagnostic tools, such as the CAM-ICU and 4AT, by nursing staff. Early recognition of delirium allows prompt intervention, reducing complications such as long-term cognitive impairment or prolonged hospital stays. Nurses’ daily engagement with patients places them at the forefront of monitoring subtle behavioural changes, ensuring early identification and management of delirium. Multicomponent, nonpharmacological interventions, such as reorientation, cognitive stimulation, sleep hygiene optimisation, sensory interventions, and mobilisation, require active nursing involvement for effective implementation. Nurses not only deliver these interventions but also coordinate family engagement, enhance environmental conditions, and support individualised patient care. Evidence shows that programs such as M.O.R.E. and Dy-Del, led by nursing teams, can significantly reduce delirium incidence and improve patient quality of life [,]. However, translating this evidence into routine clinical practice remains challenging. Nursing workload, staff shortages, and variations in knowledge or experience can limit the consistent application of delirium prevention protocols. The implementation of multicomponent interventions may also be constrained by limited time, inadequate staffing levels, and the absence of institutional policies that prioritise delirium prevention. Therefore, while the role of nurses is central, the feasibility of sustaining these interventions depends on organisational support, including adequate nurse-to-patient ratios, access to training programs, and interdisciplinary collaboration. Targeted education and training, including skills in hypoactive delirium recognition, sensory interventions, and circadian rhythm-based care, are vital to enhancing nurses’ competence and confidence. Moreover, psychological support and resilience-building initiatives for nurses are also important, as caring for patients with delirium can be stressful and emotionally demanding. Ultimately, the success of nursing-led delirium prevention strategies requires not only individual skills but also a systemic commitment to creating work environments that enable consistent, high-quality care.
7. Conclusions
Multicomponent, nurse-led interventions show promise in preventing and managing delirium, particularly in surgical and geriatric settings; however, evidence from ICU populations remains inconclusive. Early and systematic identification of delirium not only enables timely clinical intervention but also facilitates the tailoring of care to the individual patient’s needs, such as cognitive stimulation, orientation strategies, environmental modifications, and optimisation of hydration and nutrition. Interdisciplinary collaboration ensures that all members of the healthcare team contribute their expertise to a coordinated care plan. Furthermore, structured training programs and standardised care protocols for healthcare staff are essential for maintaining consistency in delirium management across hospital settings. Such initiatives enhance staff knowledge and competence, promote adherence to evidence-based practices, and foster an organisational culture that prioritises early recognition, prevention, and comprehensive management of delirium.
In summary, future research should aim to clarify which components are most effective in specific clinical contexts and how implementation fidelity influences outcomes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm14228113/s1, Table S1: The PRISMA checklist [].
Author Contributions
Conceptualization, A.S. and D.S.; methodology, A.S. and S.Z.; formal analysis, A.S., D.S. and S.Z.; data curation, A.S., J.K. and S.Z.; writing—original draft preparation, A.S., S.Z., J.C.-M. and J.K.; writing—review and editing, A.S., D.S. and S.Z.; visualization, A.S.; supervision, D.S. and S.Z.; funding acquisition, J.C.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Polish Ministry of Science and Higher Education, grant No. SUPB.RN.21.234.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ABCDEF bundle | Assess, prevent, and manage pain, Both spontaneous awakening and breathing trials, Choice of analgesia and sedation, Delirium: assess, prevent, and manage, Early mobility and exercise, Family engagement and empowerment |
| AS | Assessment strategy |
| 4AT | Alertness, Abbreviated Mental Test-4, Attention, Acute change or fluctuating course Test |
| CA | Cardiac arrest |
| CAM | Confusion Assessment Method |
| CAM-ICU | Confusion Assessment Method for the Intensive Care Unit |
| CHI | Cerebral hemodynamics improvement |
| CS | Cognitive stimulation |
| DSM-5 | Diagnostic and Statistical Manual of Mental Disorders, 5th Edition |
| Dy-Del intervention | Dynamic Delirium intervention |
| EM | Early mobilization |
| EP | Exercise program |
| FP | Family participation |
| HELP | Hospital Elder Life Program |
| ICD-10/ICD-11 | International Classification of Diseases, 10th/11th revision |
| ICDSC | Intensive Care Delirium Screening Checklist |
| ICUs | Intensive care units |
| KAP | Knowledge, Attitudes, Practices |
| M.O.R.E. | Music, Opening of blinds, Reorientation, Eye/Ear protocols |
| MLT | Multicomponent training |
| NICE | National Institute for Health and Care Excellence |
| Nu-DESC | Nursing Delirium Screening Scale |
| PADIS guidelines | Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Guidelines |
| PC | Pain control |
| PEI | Physical environment intervention |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCTs | Randomized controlled trials |
| SP | Sleep promotion |
| SR | Sedation reduction |
| UC | Usual care |
References
- Wójtowicz-Dacka, M.; Zając-Lamparska, L. O Świadomości. Wybrane zagadnienia. Wprow; Wydaw. UKW: Bydgoszcz, Poland, 2007; p. 200. ISBN 978-83-7096-620-1. [Google Scholar]
- Cortés-Beringola, A.; Vicent, L.; Martín-Asenjo, R.; Puerto, E.; Domínguez-Pérez, L.; Maruri, R.; Moreno, G.; Vidán, M.T.; Arribas, F.; Bueno, H. Diagnosis, Prevention, and Management of Delirium in the Intensive Cardiac Care Unit. Am. Heart J. 2021, 232, 164–176. [Google Scholar] [CrossRef]
- Prew, T.; Tahir, T.A. Delirium. Medicine 2024, 52, 552–556. [Google Scholar] [CrossRef]
- Association, E.D.; Society, A.D. The DSM-5 Criteria, Level of Arousal and Delirium Diagnosis: Inclusiveness Is Safer. BMC Med. 2014, 12, 141. [Google Scholar] [CrossRef]
- El Sheikh, W.G.; Sleem, B.; Kobeissy, F.; Bizri, M. Biomarkers of Delirium and Relation to Dementia among the Elderly in the Intensive Care Unit: A Narrative Review. Biomark. Neuropsychiatry 2023, 8, 100064. [Google Scholar] [CrossRef]
- Wilson, J.E.; Mart, M.F.; Cunningham, C.; Shehabi, Y.; Girard, T.D.; MacLullich, A.M.J.; Slooter, A.J.C.; Ely, E.W. Delirium. Nat. Rev. Dis. Prim. 2020, 6, 90. [Google Scholar] [CrossRef] [PubMed]
- Marcantonio, E.R. Delirium in Hospitalized Older Adults. N. Engl. J. Med. 2017, 377, 1456–1466. [Google Scholar] [CrossRef]
- Tieges, Z.; Quinn, T.; MacKenzie, L.; Davis, D.; Muniz-Terrera, G.; MacLullich, A.M.J.; Shenkin, S.D. Association between Components of the Delirium Syndrome and Outcomes in Hospitalised Adults: A Systematic Review and Meta-Analysis. BMC Geriatr. 2021, 21, 162. [Google Scholar] [CrossRef]
- Mei, X.; Liu, Y.-H.; Han, Y.-Q.; Zheng, C.-Y. Risk Factors, Preventive Interventions, Overlapping Symptoms, and Clinical Measures of Delirium in Elderly Patients. World J. Psychiatry 2023, 13, 973–984. [Google Scholar] [CrossRef]
- Zaher-Sánchez, S.; Satústegui-Dordá, P.J.; Ramón-Arbués, E.; Santos-Sánchez, J.A.; Aguilón-Leiva, J.J.; Pérez-Calahorra, S.; Juárez-Vela, R.; Sufrate-Sorzano, T.; Angulo-Nalda, B.; Garrote-Cámara, M.E.; et al. The Management and Prevention of Delirium in Elderly Patients Hospitalised in Intensive Care Units: A Systematic Review. Nurs. Rep. 2024, 14, 3007–3022. [Google Scholar] [CrossRef]
- Koirala, B.; Hansen, B.R.; Hosie, A.; Budhathoki, C.; Seal, S.; Beaman, A.; Davidson, P.M. Delirium Point Prevalence Studies in Inpatient Settings: A Systematic Review and Meta-analysis. J. Clin. Nurs. 2020, 29, 2083–2092. [Google Scholar] [CrossRef]
- Goettel, N.; Wueest, A.S. Diagnosing Delirium in Perioperative and Intensive Care Medicine. Curr. Opin. Anesthesiol. 2023, 36, 491–499. [Google Scholar] [CrossRef]
- Veronese, N.; Solimando, L.; Bolzetta, F.; Maggi, S.; Fiedorowicz, J.G.; Gupta, A.; Fabiano, N.; Wong, S.; Boyer, L.; Fond, G.; et al. Interventions to Prevent and Treat Delirium: An Umbrella Review of Randomized Controlled Trials. Ageing Res. Rev. 2024, 97, 102313. [Google Scholar] [CrossRef]
- Deeken, F.; Sánchez, A.; Rapp, M.A.; Denkinger, M.; Brefka, S.; Spank, J.; Bruns, C.; von Arnim, C.A.F.; Küster, O.C.; Conzelmann, L.O.; et al. Outcomes of a Delirium Prevention Program in Older Persons After Elective Surgery: A Stepped-Wedge Cluster Randomized Clinical Trial. JAMA Surg. 2022, 157, e216370. [Google Scholar] [CrossRef]
- Zipser, C.M.; Seiler, A.; Deuel, J.; Ernst, J.; Hildenbrand, F.; von Känel, R.; Boettger, S. Hospital-Wide Evaluation of Delirium Incidence in Adults under 65 Years of Age. Psychiatry Clin. Neurosci. 2020, 74, 669–670. [Google Scholar] [CrossRef] [PubMed]
- Prendergast, N.T.; Tiberio, P.J.; Girard, T.D. Treatment of Delirium During Critical Illness. Annu. Rev. Med. 2022, 73, 407–421. [Google Scholar] [CrossRef]
- Mędrzycka-Dąbrowska, W.; Lange, S.; Religa, D.; Dąbrowski, S.; Friganović, A.; Oomen, B.; Krupa, S. Delirium in ICU Patients after Cardiac Arrest: A Scoping Review. J. Pers. Med. 2022, 12, 1047. [Google Scholar] [CrossRef] [PubMed]
- McCoy, T.H.; Hart, K.L.; Perlis, R.H. Characterizing and Predicting Rates of Delirium across General Hospital Settings. Gen. Hosp. Psychiatry 2017, 46, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, Y.; Huang, Y.; Yang, F. Comparative Effectiveness of Delirium Recognition with and without a Clinical Decision Assessment System on Outcomes of Hospitalized Older Adults: Cluster Randomized Controlled Trial. Int. J. Nurs. Stud. 2025, 162, 104979. [Google Scholar] [CrossRef]
- Ramírez Echeverría, M.d.L.; Schoo, C.; Paul, M. Delirium; StatPearls Publishing: Treasure Island, FL, USA, 2017. [Google Scholar]
- Yu, M.; Mi, J.; Zhang, C.; Chen, H.; Luo, X. Knowledge, Attitude and Practice Regarding Hypoactive Delirium among ICU Nurses: A Nationwide Cross-Sectional Study. Nurse Educ. Pract. 2023, 72, 103749. [Google Scholar] [CrossRef]
- Kristensen, A.H.; Nymark, C.; Stenman, M.; Falk, A. Registered Nurses’ Experiences of Caring for Patients with Hypoactive Delirium after Cardiac Surgery—A Qualitative Study. Intensive Crit. Care Nurs. 2024, 84, 103757. [Google Scholar] [CrossRef]
- Fernandes, F.; Santos, M.; Anacleto, A.M.; Jerónimo, C.; Ferreira, Ó.; Baixinho, C.L. Nursing Intervention to Prevent and Manage Delirium in Critically Ill Patients: A Scoping Review. Healthcare 2024, 12, 1134. [Google Scholar] [CrossRef] [PubMed]
- Lewis, K.; Balas, M.C.; Stollings, J.L.; McNett, M.; Girard, T.D.; Chanques, G.; Kho, M.E.; Pandharipande, P.P.; Weinhouse, G.L.; Brummel, N.E.; et al. A Focused Update to the Clinical Practice Guidelines for the Prevention and Management of Pain, Anxiety, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit. Care Med. 2025, 53, e711–e727. [Google Scholar] [CrossRef]
- Aldecoa, C.; Bettelli, G.; Bilotta, F.; Sanders, R.D.; Aceto, P.; Audisio, R.; Cherubini, A.; Cunningham, C.; Dabrowski, W.; Forookhi, A.; et al. Update of the European Society of Anaesthesiology and Intensive Care Medicine Evidence-Based and Consensus-Based Guideline on Postoperative Delirium in Adult Patients. Eur. J. Anaesthesiol. EJA 2024, 41, 81–108. [Google Scholar] [CrossRef]
- Lange, S.; Mȩdrzycka-Dąbrowska, W.; Tomaszek, L.; Wujtewicz, M.; Krupa, S. Nurses’ Knowledge, Barriers and Practice in the Care of Patients with Delirium in the Intensive Care Unit in Poland—A Cross-Sectional Study. Front. Public Health 2023, 11, 1119526. [Google Scholar] [CrossRef]
- Kotfis, K.; Zegan-Barańska, M.; Żukowski, M.; Kusza, K.; Kaczmarczyk, M.; Ely, E.W. Multicenter Assessment of Sedation and Delirium Practices in the Intensive Care Units in Poland—Is This Common Practice in Eastern Europe? BMC Anesthesiol. 2017, 17, 120. [Google Scholar] [CrossRef]
- Liang, S.; Chau, J.P.C.; Lo, S.H.S.; Zhao, J.; Liu, W. Non-Pharmacological Delirium Prevention Practices among Critical Care Nurses: A Qualitative Study. BMC Nurs. 2022, 21, 235. [Google Scholar] [CrossRef] [PubMed]
- Morandi, A.; Piva, S.; Ely, E.W.; Myatra, S.N.; Salluh, J.I.F.; Amare, D.; Azoulay, E.; Bellelli, G.; Csomos, A.; Fan, E.; et al. Worldwide Survey of the “Assessing Pain, Both Spontaneous Awakening and Breathing Trials, Choice of Drugs, Delirium Monitoring/Management, Early Exercise/Mobility, and Family Empowerment” (ABCDEF) Bundle. Crit. Care Med. 2017, 45, e1111–e1122. [Google Scholar] [CrossRef]
- Oliveira, C.; Garnacho Martins Nobre, C.F.; Dourado Marques, R.M.; Madureira Lebre Mendes, M.M.; Pontífice Sousa, P.C. The nurse’s role in preventing delirium in critically ill adult/elderly patients. Rev. Cuid. 2022, 13, e3. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R Package and Shiny App for Producing PRISMA 2020-Compliant Flow Diagrams, with Interactivity for Optimised Digital Transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Lockwood, C.; Munn, Z.; Porritt, K. Qualitative Research Synthesis: Methodological Guidance for Systematic Reviewers Utilizing Meta-Aggregation. JBI Evid. Implement. 2015, 13, 179–187. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A Critical Appraisal Tool for Systematic Reviews That Include Randomised or Non-Randomised Studies of Healthcare Interventions, or Both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Kuusisto-Gussmann, E.; Höckelmann, C.; von der Lühe, V.; Schmädig, R.; Baltes, M.; Stephan, A. Patients’ Experiences of Delirium: A Systematic Review and Meta-Summary of Qualitative Research. J. Adv. Nurs. 2021, 77, 3692–3706. [Google Scholar] [CrossRef]
- Molitor, V.; Busse, T.S.; Giehl, C.; Lauer, R.; Otte, I.C.; Vollmar, H.C.; Thürmann, P.; Holle, B.; Palm, R. Educational Interventions Aimed at Improving Knowledge of Delirium among Nursing Home Staff—A Realist Review. BMC Geriatr. 2024, 24, 633. [Google Scholar] [CrossRef] [PubMed]
- Burton, J.K.; Craig, L.E.; Yong, S.Q.; Siddiqi, N.; Teale, E.A.; Woodhouse, R.; Barugh, A.J.; Shepherd, A.M.; Brunton, A.; Freeman, S.C.; et al. Non-Pharmacological Interventions for Preventing Delirium in Hospitalised Non-ICU Patients. Cochrane Database Syst. Rev. 2021, 7, CD013307. [Google Scholar] [CrossRef] [PubMed]
- Brennan, K.; Sanchez, D.; Hedges, S.; Lynch, J.; Hou, Y.C.; Al Sayfe, M.; Shunker, S.-A.; Bogdanoski, T.; Hunt, L.; Alexandrou, E.; et al. A Nurse-Led Intervention to Reduce the Incidence and Duration of Delirium among Adults Admitted to Intensive Care: A Stepped-Wedge Cluster Randomised Trial. Aust. Crit. Care 2023, 36, 441–448. [Google Scholar] [CrossRef]
- Siddiqi, N.; Harrison, J.K.; Clegg, A.; A Teale, E.; Young, J.; Taylor, J.; Simpkins, S.A. Interventions for Preventing Delirium in Hospitalised Non-ICU Patients. Cochrane Database Syst. Rev. 2016, 2016, CD005563. [Google Scholar] [CrossRef]
- Sist, L.; Pezzolati, M.; Ugenti, N.V.; Cedioli, S.; Messina, R.; Chiappinotto, S.; Rucci, P.; Palese, A. Prioritization Patterns of Nurses in the Management of a Patient With Delirium: Results of a Q-Methodology Study. Res. Nurs. Health 2025, 48, 257–270. [Google Scholar] [CrossRef]
- Burry, L.D.; Cheng, W.; Williamson, D.R.; Adhikari, N.K.; Egerod, I.; Kanji, S.; Martin, C.M.; Hutton, B.; Rose, L. Pharmacological and Non-Pharmacological Interventions to Prevent Delirium in Critically Ill Patients: A Systematic Review and Network Meta-Analysis. Intensive Care Med. 2021, 47, 943–960. [Google Scholar] [CrossRef] [PubMed]
- Naeem, F.; Penfold, R.S.; Soiza, R.L.; Von Haken, R.; Lindroth, H.; Liu, K.; Nydhal, P.; Quinn, T.J. Delirium Assessment, Management and Barriers to Effective Care across Scotland: A Secondary Analysis of Survey Data from World Delirium Awareness Day 2023. J. R. Coll. Physicians Edinb. 2025, 55, 6–13. [Google Scholar] [CrossRef]
- Kim, Y.H.; Kim, N.Y.; Ryu, S. Effects of Non-Pharmacological Interventions for Preventing Delirium in General Ward Inpatients: A Systematic Review & Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2022, 17, e0268024. [Google Scholar] [CrossRef]
- Lee, Y.; Lee, J.; Kim, J.; Jung, Y. Non-Pharmacological Nursing Interventions for Prevention and Treatment of Delirium in Hospitalized Adult Patients: Systematic Review of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2021, 18, 8853. [Google Scholar] [CrossRef]
- Lange, S.; Mędrzycka-Dąbrowska, W.; Friganovic, A.; Oomen, B.; Krupa, S. Non-Pharmacological Nursing Interventions to Prevent Delirium in ICU Patients—An Umbrella Review with Implications for Evidence-Based Practice. J. Pers. Med. 2022, 12, 760. [Google Scholar] [CrossRef]
- Bannon, L.; McGaughey, J.; Verghis, R.; Clarke, M.; McAuley, D.F.; Blackwood, B. The Effectiveness of Non-Pharmacological Interventions in Reducing the Incidence and Duration of Delirium in Critically Ill Patients: A Systematic Review and Meta-Analysis. Intensive Care Med. 2019, 45, 1–12. [Google Scholar] [CrossRef]
- Rood, P.J.T.; Ramnarain, D.; Oldenbeuving, A.W.; den Oudsten, B.L.; Pouwels, S.; van Loon, L.M.; Teerenstra, S.; Pickkers, P.; de Vries, J.; van den Boogaard, M. The Impact of Non-Pharmacological Interventions on Delirium in Neurological Intensive Care Unit Patients: A Single-Center Interrupted Time Series Trial. J. Clin. Med. 2023, 12, 5820. [Google Scholar] [CrossRef]
- Herling, S.F.; Greve, I.E.; Vasilevskis, E.E.; Egerod, I.; Mortensen, C.B.; Møller, A.M.; Svenningsen, H.; Thomsen, T. Interventions for Preventing Intensive Care Unit Delirium in Adults. Cochrane Database Syst. Rev. 2018, 11, CD009783. [Google Scholar] [CrossRef] [PubMed]
- Tehranineshat, B.; Hosseinpour, N.; Mani, A.; Rakhshan, M. The Effect of Multi-Component Interventions on the Incidence Rate, Severity, and Duration of Post Open Heart Surgery Delirium among Hospitalized Patients. J. Cardiothorac. Surg. 2021, 16, 32. [Google Scholar] [CrossRef]
- Kang, J.; Cho, Y.S.; Lee, M.; Yun, S.; Jeong, Y.J.; Won, Y.-H.; Hong, J.; Kim, S. Effects of Nonpharmacological Interventions on Sleep Improvement and Delirium Prevention in Critically Ill Patients: A Systematic Review and Meta-Analysis. Aust. Crit. Care 2023, 36, 640–649. [Google Scholar] [CrossRef]
- Li, J.; Fan, Y.; Luo, R.; Yin, N.; Wang, Y.; Jing, J.; Zhang, J. The Impact of Non-Pharmacological Sleep Interventions on Delirium Prevention and Sleep Improvement in Postoperative ICU Patients: A Systematic Review and Network Meta-Analysis. Intensive Crit. Care Nurs. 2025, 87, 103925. [Google Scholar] [CrossRef]
- Jang, S.; Lee, M. Effects of Anxiety Focused Nursing Interventions on Anxiety, Cognitive Function and Delirium in Neurocritical Patients: A Non-Randomized Controlled Design. Nurs. Crit. Care 2025, 30, e70062. [Google Scholar] [CrossRef] [PubMed]
- Gómez Tovar, L.O.; Henao Castaño, A.M. Dynamic Delirium—Nursing Intervention to Reduce Delirium in Patients Critically Ill, a Randomized Control Trial. Intensive Crit. Care Nurs. 2024, 83, 103691. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.-X.; Cao, L.; Zhang, L.-N.; Peng, X.-B.; Zhang, L. Non-Pharmacological Interventions to Reduce the Incidence and Duration of Delirium in Critically Ill Patients: A Systematic Review and Network Meta-Analysis. J. Crit. Care 2020, 60, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Rivosecchi, R.M.; Smithburger, P.L.; Svec, S.; Campbell, S.; Kane-Gill, S.L. Nonpharmacological Interventions to Prevent Delirium: An Evidence-Based Systematic Review. Crit. Care Nurse 2015, 35, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Liu, S.; Zhao, H.; Dong, L.; Zhu, X.; Liu, J. Non-Pharmacological Interventions to Prevent and Treat Delirium in Older People: An Overview of Systematic Reviews. Int. J. Nurs. Stud. 2023, 148, 104584. [Google Scholar] [CrossRef]
- Chen, T.-J.; Traynor, V.; Wang, A.-Y.; Shih, C.-Y.; Tu, M.-C.; Chuang, C.-H.; Chiu, H.-Y.; Chang, H.-C.R. Comparative Effectiveness of Non-Pharmacological Interventions for Preventing Delirium in Critically Ill Adults: A Systematic Review and Network Meta-Analysis. Int. J. Nurs. Stud. 2022, 131, 104239. [Google Scholar] [CrossRef]
- Wang, Y.; Li, L.; Tan, S.; Guan, Y.; Luo, X. Psychological Stress and Associated Factors in Caring for Patients with Delirium among Intensive Care Unit Nurses: A Cross-Sectional Study. Aust. Crit. Care 2023, 36, 793–798. [Google Scholar] [CrossRef]
- Vitorino, M.L.; Henriques, A.; Melo, G.; Henriques, H.R. The Effectiveness of Family Participation Interventions for the Prevention of Delirium in Intensive Care Units: A Systematic Review. Intensive Crit. Care Nurs. 2025, 89, 103976. [Google Scholar] [CrossRef]
- Jensen, J.; Thorhauge, K.A.L.; Petri, C.L.; Madsen, M.T.; Burcharth, J.F.H. Preventative Interventions for Postoperative Delirium after Intraabdominal Surgery—A Systematic Review and Meta-Analysis of Randomized Trials. Am. J. Surg. 2025, 243, 116245. [Google Scholar] [CrossRef]
- Wang, J.; Lu, Y.; Chen, X.; Wu, Y. Effectiveness of Nurse-led Non-pharmacological Interventions on Outcomes of Delirium in Adults: A Meta-analysis of Randomized Controlled Trials. Worldviews Evid.-Based Nurs. 2024, 21, 514–527. [Google Scholar] [CrossRef]
- Xu, C.; Zhang, Y.; Yuan, D.; Wang, C.; Wang, X.; Liang, X.; Wang, J.; Duan, J. Effects of Sensory-Based Interventions on Delirium Prevention in Critically Ill Patients: A Systematic Review and Meta-Analysis. Int. J. Nurs. Pract. 2025, 31, e13321. [Google Scholar] [CrossRef] [PubMed]
- Pelin, M.; Sert, H. The Effect of Nursing Care Provided to Coronary Intensive Care Patients According to Their Circadian Rhythms on Sleep Quality, Pain, Anxiety, and Delirium: A Randomised Controlled Trial. BMC Nurs. 2025, 24, 143. [Google Scholar] [CrossRef]
- Matsuura, Y.; Ohno, Y.; Toyoshima, M.; Ueno, T. Effects of Non-Pharmacologic Prevention on Delirium in Critically Ill Patients: A Network Meta-Analysis. Nurs. Crit. Care 2023, 28, 727–737. [Google Scholar] [CrossRef]
- Zhao, X.; Yuan, W. Perioperative Multicomponent Interdisciplinary Program Reduces Delirium Incidence in Elderly Patients With Hip Fracture. J. Am. Psychiatr. Nurses Assoc. 2022, 28, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Unal, N.; Guvenc, G.; Naharci, M. Evaluation of the Effectiveness of Delirium Prevention Care Protocol for the Patients with Hip Fracture: A Randomised Controlled Study. J. Clin. Nurs. 2022, 31, 1082–1094. [Google Scholar] [CrossRef]
- Noel, C.; Cirbus, J.; Han, J. Emergency Department Interventions and Their Effect on Delirium’s Natural Course: The Folly May Be in the Foley. J. Emergencies Trauma Shock 2019, 12, 280–285. [Google Scholar] [CrossRef]
- Rosa, R.G.; Falavigna, M.; da Silva, D.B.; Sganzerla, D.; Santos, M.M.S.; Kochhann, R.; de Moura, R.M.; Eugênio, C.S.; Haack, T.d.S.R.; Barbosa, M.G.; et al. Effect of Flexible Family Visitation on Delirium Among Patients in the Intensive Care Unit: The ICU Visits Randomized Clinical Trial. JAMA 2019, 322, 216–228. [Google Scholar] [CrossRef]
- Faustino, T.N.; Suzart, N.A.; Rabelo, R.N.D.S.; Santos, J.L.; Batista, G.S.; Freitas, Y.S.d.; Saback, D.A.; Sales, N.M.M.D.; Brandao Barreto, B.; Gusmao-Flores, D. Effectiveness of Combined Non-Pharmacological Interventions in the Prevention of Delirium in Critically Ill Patients: A Randomized Clinical Trial. J. Crit. Care 2022, 68, 114–120. [Google Scholar] [CrossRef]
- Lee, H.-J.; Jung, Y.-J.; Choi, N.-J.; Hong, S.-K. The Effects of Environmental Interventions for Delirium in Critically Ill Surgical Patients. Acute Crit. Care 2023, 38, 479–487. [Google Scholar] [CrossRef]
- Lim, Z.; Ling, N.; Ho, V.W.T.; Vidhya, N.; Chen, M.Z.; Wong, B.L.L.; Ng, S.E.; Murphy, D.; Merchant, R.A. Delirium Is Significantly Associated with Hospital Frailty Risk Score Derived from Administrative Data. Int. J. Geriatr. Psychiatry 2023, 38, e5872. [Google Scholar] [CrossRef]
- Liu, X.; Wang, Y.; Wu, J.; Ye, C.; Ma, D.; Wang, E. Emergence Delirium and Postoperative Delirium Associated with High Plasma NfL and GFAP: An Observational Study. Front. Med. 2023, 10, 1107369. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, T.E.; Chen, C.; Wang, Y.; Jung, E.; Swanson, A.; Ing, C.; Garcia, P.S.; Whittington, R.A.; Moitra, V. Association of Delirium With Long-Term Cognitive Decline: A Meta-Analysis. JAMA Neurol. 2020, 77, 1373–1381. [Google Scholar] [CrossRef] [PubMed]
- Boyd, A.; Kirwan, M.; Bannon, L. Nurses’ Usage of Validated Tools to Assess for Delirium in General Acute Care Settings: A Scoping Review Protocol. HRB Open Res. 2025, 8, 33. [Google Scholar] [CrossRef]
- Al Huraizi, A.R.; Al-Maqbali, J.S.; Al Farsi, R.S.; Al Zeedy, K.; Al-Saadi, T.; Al-Hamadani, N.; Al Alawi, A.M. Delirium and Its Association with Short- and Long-Term Health Outcomes in Medically Admitted Patients: A Prospective Study. J. Clin. Med. 2023, 12, 5346. [Google Scholar] [CrossRef]
- Luetz, A.; Weiss, B.; Boettcher, S.; Burmeister, J.; Wernecke, K.-D.; Spies, C. Routine Delirium Monitoring Is Independently Associated with a Reduction of Hospital Mortality in Critically Ill Surgical Patients: A Prospective, Observational Cohort Study. J. Crit. Care 2016, 35, 168–173. [Google Scholar] [CrossRef]
- Bates, C. Confusion and Delirium in the Acute Setting. Medicine 2017, 45, 110–114. [Google Scholar] [CrossRef]
- Stollings, J.L.; Kotfis, K.; Chanques, G.; Pun, B.T.; Pandharipande, P.P.; Ely, E.W. Delirium in Critical Illness: Clinical Manifestations, Outcomes, and Management. Intensive Care Med. 2021, 47, 1089–1103. [Google Scholar] [CrossRef] [PubMed]
- Nydahl, P.; Liu, K.; Bellelli, G.; Benbenishty, J.; van den Boogaard, M.; Caplan, G.; Chung, C.R.; Elhadi, M.; Gurjar, M.; Heras-La Calle, G.; et al. A World-Wide Study on Delirium Assessments and Presence of Protocols. Age Ageing 2024, 53, afae129. [Google Scholar] [CrossRef]
- Thomas, N.; Coleman, M.; Terry, D. Nurses’ Experience of Caring for Patients with Delirium: Systematic Review and Qualitative Evidence Synthesis. Nurs. Rep. 2021, 11, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Fordyce, C.B.; Katz, J.N.; Alviar, C.L.; Arslanian-Engoren, C.; Bohula, E.A.; Geller, B.J.; Hollenberg, S.M.; Jentzer, J.C.; Sims, D.B.; Washam, J.B.; et al. Prevention of Complications in the Cardiac Intensive Care Unit: A Scientific Statement From the American Heart Association. Circulation 2020, 142, e379–e406. [Google Scholar] [CrossRef]
- Instituto Nacional para la Excelencia en la Salud y la Atención (NICE). Delirium: Prevention, Diagnosis and Management in Hospital and Long-Term Care. NICE Guidelines; Instituto Nacional para la Excelencia en la Salud y la Atención (NICE): Ra’Anana, Israel, 2023. [Google Scholar]
- Öztürk, Z.; Kaya, M.; Aksoy, M.; Karaman Özlü, Z. Investigation of the Factors Affecting Delirium Evaluation by Intensive Care Nurses: A Cross-Sectional Descriptive Study. BMC Nurs. 2025, 24, 968. [Google Scholar] [CrossRef]
- Krewulak, K.D.; Stelfox, H.T.; Leigh, J.P.; Ely, E.W.; Fiest, K.M. Incidence and Prevalence of Delirium Subtypes in an Adult ICU: A Systematic Review and Meta-Analysis. Crit. Care Med. 2018, 46, 2029–2035. [Google Scholar] [CrossRef]
- Krewulak, K.D.; Stelfox, H.T.; Ely, E.W.; Fiest, K.M. Risk Factors and Outcomes among Delirium Subtypes in Adult ICUs: A Systematic Review. J. Crit. Care 2020, 56, 257–264. [Google Scholar] [CrossRef]
- Hayhurst, C.J.; Marra, A.; Han, J.H.; Patel, M.B.; Brummel, N.E.; Thompson, J.L.; Jackson, J.C.; Chandrasekhar, R.; Ely, E.W.; Pandharipande, P.P.; et al. Association of Hypoactive and Hyperactive Delirium With Cognitive Function After Critical Illness. Crit. Care Med. 2020, 48, e480–e488. [Google Scholar] [CrossRef]
- Ragheb, J.; Norcott, A.; Benn, L.; Shah, N.; McKinney, A.; Min, L.; Vlisides, P.E. Barriers to Delirium Screening and Management during Hospital Admission: A Qualitative Analysis of Inpatient Nursing Perspectives. BMC Health Serv. Res. 2023, 23, 712. [Google Scholar] [CrossRef]
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.C.; Pandharipande, P.P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B.; et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit. Care Med. 2018, 46, e825–e873. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.U.; Towell-Barnard, A.; McLean, C.; Ewens, B. The Development of a Family-Led Novel Intervention for Delirium Prevention and Management in the Adult Intensive Care Unit: A Co-Design Qualitative Study. Aust. Crit. Care Off. J. Confed. Aust. Crit. Care Nurses 2025, 38, 101088. [Google Scholar] [CrossRef] [PubMed]
- Rosted, E.E.; Prokofieva, T.V.; Sanders, S.C.; Schultz, M. Serious Consequences of Malnutrition and Delirium in Frail Older Patients. J. Nutr. Gerontol. Geriatr. 2018, 37, 105–116. [Google Scholar] [CrossRef]
- Morandi, A.; Inzitari, M.; Udina, C.; Gual, N.; Mota, M.; Tassistro, E.; Andreano, A.; Cherubini, A.; Gentile, S.; Mossello, E. Visual and Hearing Impairment Are Associated With Delirium in Hospitalized Patients: Results of a Multisite Prevalence Study. J. Am. Med. Dir. Assoc. 2021, 22, 1162–1167.e3. [Google Scholar] [CrossRef]
- Kim, J.; Choi, D.; Yeo, M.S.; Yoo, G.E.; Kim, S.J.; Na, S. Effects of Patient-Directed Interactive Music Therapy on Sleep Quality in Postoperative Elderly Patients: A Randomized-Controlled Trial. Nat. Sci. Sleep 2020, 12, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Slooter, A.J.C. Nonpharmacological Interventions in Delirium: The Law of the Handicap of a Head Start. Am. J. Respir. Crit. Care Med. 2021, 204, 624–626. [Google Scholar] [CrossRef]
- Rood, P.J.T.; Zegers, M.; Ramnarain, D.; Koopmans, M.; Klarenbeek, T.; Ewalds, E.; van der Steen, M.S.; Oldenbeuving, A.W.; Kuiper, M.A.; Teerenstra, S.; et al. The Impact of Nursing Delirium Preventive Interventions in the ICU: A Multicenter Cluster-Randomized Controlled Clinical Trial. Am. J. Respir. Crit. Care Med. 2021, 204, 682–691. [Google Scholar] [CrossRef]
- Hshieh, T.T.; Yue, J.; Oh, E.; Puelle, M.; Dowal, S.; Travison, T.; Inouye, S.K. Effectiveness of Multicomponent Nonpharmacological Delirium Interventions: A Meta-Analysis. JAMA Intern. Med. 2015, 175, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).