Abstract
Background: The management of infections involving the distal tibia and ankle is a significant challenge in orthopedic surgery due to complex anatomy and the high risk of complications. The study aims to present our clinical experience in managing these infections and focusing on surgical strategies, infection control, and functional outcomes over a minimum 24-month follow-up period. Methods: This is an observational, retrospective case series of 17 patients treated for osteoarticular infections of the distal tibia and/or ankle between January 2020 and May 2023, in a second-level referral trauma center. A staged surgical approach was employed, including radical debridement, temporary stabilization with external fixation, and, in most cases, implantation of a cement spacer loaded with antibiotics. Functional outcomes were assessed using scores such as EQ-5D-5L. Results: The cohort was predominantly male (76.5%), with a high prevalence of elevated BMI and comorbidities. Infection onset was most frequently associated with open fractures (64.7%). Staphylococcus aureus was the most common isolated pathogen (41.2%), and infections caused by Gram-negative or multidrug-resistant bacteria were associated with more reoperations. Overall, complications occurred in 10 patients (58.8%), requiring reintervention in 9 patients (52.9%). Limb salvage was achieved in 16 of 17 patients (94.1%). Conclusions: Our study highlights the critical role of a tailored, multidisciplinary approach in managing these complex infections. Meticulous surgical planning and proactive management of complications are essential for optimizing patient outcomes.
1. Introduction
Distal tibia and ankle fractures are among the most common injuries in emergency settings due to their complex anatomy and critical role in functional movements [1].
Even more, distal tibial and ankle infections represent a significant challenge in orthopedic surgery and management, particularly in patients with open fractures, impaired soft tissue integrity, or previous unsuccessful treatments [2,3]. The incidence of these infections has increased in recent years, especially in cases involving complex fractures and in patients with multiple comorbidities, such as diabetes and peripheral vascular disease [4,5,6]. Inadequate early management, delayed diagnosis, and insufficient debridement can exacerbate these infections, leading to non-union, chronic osteomyelitis, and potential limb amputation [7,8].
Effective management requires a multidisciplinary approach that integrates accurate skin and cutaneous exposure irrigation and debridement, fracture stabilization, adequate antibiotic therapy, and soft tissue reconstruction [9,10]. The appropriate fixation method option, whether external or internal one, is determined by several factors such as bone loss extension, infection severity, and soft tissue conditions [11,12]. Recent data underscore the benefits of external fixation in managing complex fractures with severe soft tissue damage, although this method is associated with complications like pin site infections and delayed union [10].
Recent studies emphasize the importance of timely surgical intervention, as delayed treatment is often associated with higher infection recurrence and the need for multiple re-interventions [13,14].
Advanced reconstructive techniques, including the Masquelet technique and distraction osteogenesis, as well as custom-made implants and other innovative approaches, have demonstrated good and effective results in managing segmental bone defects in infections [14,15,16].
However, the optimal timing for conversion from external to internal fixation remains debated, with some studies suggesting that early conversion may reduce infection rates, while others recommend prolonged external fixation to ensure infection control [17,18].
Furthermore, antibiotic management is critical in controlling infection, particularly in the context of multidrug-resistant organisms. Empiric broad-spectrum antibiotics are typically initiated, followed by targeted therapy based on microbiological culture results [19]. The emergence of resistant pathogens has underscored the need for tailored antibiotic regimens and adjunctive treatments, such as local antibiotic delivery systems [20].
Therefore, the aim of this study is to present our clinical experience in the management of distal tibia and ankle infections, focusing on surgical strategies, infection control, and functional outcomes over a minimum 24-month follow-up period.
2. Materials and Methods
2.1. Study Design
This is an observational, retrospective case series about patients treated for distal tibia and/or ankle infections who underwent several surgical treatments at IRCCS Fondazione Policlinico Universitario A. Gemelli (Rome, Italy), a second-level referral trauma center. Data were analysed from September 2024 to May 2025. The recruitment period extended from January 2020 to May 2023, ensuring that all patients included had completed at least 24 months of follow-up by the time of data analysis. At hospital admission, all patients signed a written informant consent concerning demographic and clinical data for scientific purposes according to institutional protocols. The study respects national ethical standards and the Helsinki Declaration.
2.2. Inclusion and Exclusion Criteria
Inclusion criteria were (i) patients aged ≥ 18 years; (ii) diagnosis of distal tibial or ankle osteomyelitis, (iii) treated surgically at our institution. Exclusion criteria were (i) previous amputation or non-functional limb; (ii) incomplete data or loss to follow-up.
Inclusion criteria were defined broadly to collect all established osteoarticular infections of the distal tibia and ankle requiring surgical management at our department, including both Fracture-Related Infection (FRI) and primary chronic osteomyelitis without trauma. Patients were categorized according to the FRI Consensus Group definitions [21].
For cases of chronic osteomyelitis unrelated to fractures, diagnostic principles from the Musculoskeletal Infection Society (MSIS) were additionally considered.
2.3. Data Collection and Patients Setting
Relevant clinical, demographic, and perioperative data were retrospectively collected from the institutional electronic medical records and operative reports of all patients meeting the inclusion criteria. Data sources included hospital discharge summaries, surgical charts, microbiology and pathology reports, and outpatient follow-up documentation.
Recorded variables included age, sex, Body Mass Index (BMI), smoking status, comorbidities, infection aetiology and localization, microbiological isolate, surgical procedures (both initial and staged), soft tissue reconstruction techniques, complications, and duration of follow-up. Diagnostic imaging data were reviewed to assess bone involvement and infection extension, including X-ray, Computed Tomography (CT) scan, and, when available, Magnetic Resonance Imaging (MRI).
Patients were clinically followed at regular intervals post-operatively. Functional outcome data were collected during in-person evaluations or via telephonic interviews, performed by trained clinical personnel, using the European Quality of Life 5 Dimensions 5 Level Version (EQ-5D-5L). Data consistency was ensured through double entry verification and cross-referencing between medical records and surgical logs. Missing data were minimized and addressed through direct patient contact or review of archived documentation.
Although the American Orthopaedic Foot and Ankle Society (AOFAS) score, Foot Function Index (FFI), and Short Form-36 (SF-36) questionnaires were initially planned for functional assessment, only the EQ-5D-5L was consistently completed by all patients at final follow-up. Therefore, functional outcome analysis was limited to this score.
All patient information was anonymized prior to statistical processing.
Infection control was defined as the absence of clinical signs or symptoms of infection (such as persistent drainage, erythema, or local pain), normalization of inflammatory markers (C-reactive protein < 10 mg/L and erythrocyte sedimentation rate < 30 mm/h), and radiographic or CT evidence of progressive bone healing or stable consolidation without lytic progression at final follow-up. Patients meeting all three criteria at their last evaluation were considered infection-free.
2.4. Outcome Measures
Patients were stratified into two groups based on the time period between the initial injury/osteosynthesis and the definitive staged surgical debridement: acute/subacute infection (treatment initiate days ≤ 90 days post-injury) and chronic post-traumatic osteomyelitis (treatment initiated ≥ 90 days post-injury). The reintervention was defined as any unplanned surgical procedure, excluding minor debridement or pin-site care, performed at the infection site following the definitive first stage of the orthoplastic protocol.
Complications were categorized as either minor or major. Minor complications included local issues that were resolved with conservative or outpatient treatment (e.g., pin tract infections, superficial wound dehiscence). Major complications included recurrence of deep infection, new fractures, failure of reconstruction requiring a completely different treatment strategy, or the need for a major unplanned procedure (e.g., amputation).
2.5. Statistical Analysis
Descriptive statistical analysis was conducted using Microsoft Excel 2019 (Microsoft Corporation, Redmond, WA, USA) and Python 3.10.12 (Python Software Foundation, https://www.python.org/, accessed on 16 October 2025) with standard scientific libraries: Pandas 2.1.1, NumPy 1.26.2, Matplotlib 3.8.1, and Seaborn 0.12.2. Continuous variables were expressed as means ± standard deviations (SD) or medians with interquartile ranges (IQR), depending on data distribution. Categorical variables were summarized as absolute frequencies and percentages.
No inferential statistical tests were performed, as the study was designed as a retrospective descriptive case series without a control group. However, to descriptively support specific observations of clinical interest regarding complication risk, focused exploratory comparative analyses (e.g., using Fisher’s exact test for categorical outcomes) were conducted post hoc to investigate the association between the extent of bone resection and complications, as well as surgical duration and complication rates. All other continuous and categorical variables were summarized descriptively, and subgroup comparisons were explored descriptively, particularly regarding reintervention rates, infection aetiology, and surgical procedures.
Functional outcomes based on EQ-5D-5L were analysed by computing mean scores for each domain (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), and results were reported both individually and in aggregate. Graphical representations, including bar charts, pie charts, histograms, and radar plots, were used to highlight relevant trends in demographics, comorbidity impact on outcomes, microbiology, systemic and local antibiotic regimens, soft tissue reconstruction techniques and success rates, and outcome distribution [22].
3. Results
3.1. Patient Presentation and Baseline Data
The study cohort consisted of 17 patients diagnosed with chronicsubacute or chronic osteoarticular infections involving the distal tibia and/or ankle, surgically treated between January 2020 and May 2023. All patients met strict inclusion criteria, including a confirmed diagnosis of infection based on clinical, radiological, and microbiological findings, and a minimum follow-up duration of 24 months. 13 patients met the diagnostic criteria for FRI, while four presented with chronic osteomyelitis unrelated to previous fracture or internal fixation. The cohort was predominantly male (13 of 17, 76.5%), reflecting a gender distribution consistent with the higher incidence of post-traumatic and post-surgical musculoskeletal infections in males reported in the literature.The mean age at presentation was 55.3 years (range 32–82; SD ± 13.4), with a bimodal distribution and a peak in the fourth and seventh decades. This reflects the two typical epidemiological profiles most commonly affected: younger patients with high-energy trauma and older patients with multiple comorbidities or previous surgeries.
Anthropometric evaluation showed a BMI of 29.4 (range 18.9–37.5). Eight patients (47%) met the World Health Organization (WHO) criteria for obesity (BMI ≥ 30), and two were morbidly obese (BMI ≥ 35). Given the known association between obesity and increased risk of surgical site complications, impaired vascular supply, and delayed bone healing, the high prevalence of elevated BMI values in this cohort is notable.
Comorbidities were common and clinically relevant. Ten patients (58.8%) had systemic arterial hypertension, while other conditions included chronic obstructive pulmonary disease 4 patients), ischemic heart disease (3 patients), and insulin-dependent diabetes mellitus (3 patients). The clinical significance of these comorbidities was demonstrated by the finding that all diabetic patients developed complications during follow-up, including delayed soft tissue healing and persistent infection, requiring further procedures. Three patients (17.6%) had multiple major comorbidities. Smoking was reported by only two patients, and none were on immunosuppressive therapies or had active malignancies.
Infection occurred following open fracture in 11 patients (64.7%), with fracture patterns corresponding to Gustilo-Anderson grade II or III. Four patients developed infection following previous internal fixation of closed fractures, and two had chronic osteomyelitis without associated trauma. The time between injury and definitive surgical treatment averaged 85 days (range 20–430 days), with three patients presenting after more than one year. Infections treated beyond 90 days from trauma had a significantly higher rate of surgical reintervention (67%) than those treated earlier (37%), showing a strong association with chronicity and treatment complexity (Table 1).

Table 1.
Demographic and clinical characteristics of the study cohort, including age, sex distribution, BMI, comorbidities, etiology of infection, and baseline clinical status. These variables provide an overview of the patient population treated for distal tibia and ankle infections in our institution.
All patients underwent standard imaging protocols, including X-rays and CT scans. MRI was selectively performed in ten patients (58.8%) to evaluate the extension of intramedullary involvement, cortical necrosis, and soft tissue edema.
3.2. Treatment Strategies and Outcomes Analysis
All patients were treated with a staged surgical approach based on contemporary principles of infection control and reconstruction. The first stage included radical bone and soft tissue debridement and temporary stabilization using external fixation. Uniplanar Hoffmann III devices were used in less complex cases, while circular or hexapod fixators were applied in patients with unstable fracture patterns, bone loss, or expected length restoration procedures.
The cohort was divided into 10 patients with acute/subacute infection (≤90 days) and 7 patients with chronic post-traumatic osteomyelitis (≥90 days). The reintervention rate was significantly higher in the chronic group: 57.1% (4 of 7) of chronic cases required a subsequent reintervention compared to 37% (3 of 10) in the acute/subacute group (Table 2). The comparison of reintervention rates between the two groups was assessed using Fisher’s Exact Test due to the small sample size; although the chronic osteomyelitis group exhibited a numerically higher reintervention rate (57.1% vs. 30.0%), this difference did not reach statistical significance (p = 0.3395).

Table 2.
Comparison of the rate of reintervation betweens patients treated early (≤90 days) and those with chronic post-traumatic osteomyelitis (≥90 days). The comparison of reintervention rates between the two groups was assessed using Fisher’S Exact Test due to the small sample size (p = 0.3395).
In 13 patients (76.4%), a polymethylmethacrylate (PMMA) spacer loaded with antibiotics was implanted. These spacers allowed for temporary defect filling, maintenance of soft tissue tension, and creation of a biologically active membrane consistent with the induced membrane technique, also known as the Masquelet technique. Six patients (35.3%) underwent bone resection exceeding 5 cm, with one patient requiring removal of a 15 cm segment of the tibial diaphysis. In all these cases, the Masquelet technique was applied to promote membrane formation prior to delayed reconstruction. One patient with massive segmental loss underwent reconstruction using a vascularized fibular graft in combination with circular external fixation, demonstrating the utility of advanced orthoplastic techniques in high-demand cases (Figure 1).

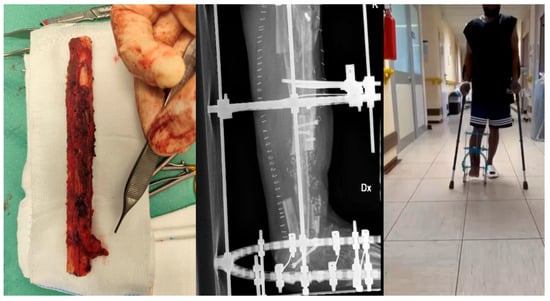
Figure 1.
30-year-old male with chronic osteomyelitis of the mid-distal tibia following an undiagnosed and untreated closed trauma for nearly two years. Management included a staged orthoplastic approach: (i) first stage—tibial resection (15 cm) with talar resection, Masquelet technique, and external fixation; (ii) second stage—removal of cement and external fixator with initiation of bone transport; (iii) third stage—fistulectomy, debridement, and reconstruction with a free vascularized fibular flap combined with circular external fixation. Radiographic and clinical signs of healing were achieved, with satisfactory pain control.
Antibiotics were mixed with cement spacers based on microbiological data and included vancomycin, gentamicin, and tobramycin. In five cases, local therapy was enhanced by bioabsorbable carriers such as calcium sulphate beads.
Soft tissue reconstruction was required in 15 patients (88.2%). Sural fasciocutaneous flaps were used in 9 cases, while 3 patients underwent perforator-based flap reconstruction. Two patients received musculocutaneous gastrocnemius flaps, and 1 patient received a vascularized fibular bone and soft tissue flap, reflecting the need for individualized treatment strategies in extensive defects. Overall, the majority of soft tissue reconstruction attempts were successful, with flap-related complications occurring in only 3 patients (20% of reconstructed cases), including minor necrosis and delayed healing, all of which were managed successfully without requiring a complete flap failure reintervention.
Microbiological cultures were positive in all cases. The most frequently isolated organism was Staphylococcus aureus (seven patients, 41.2%), including MRSA and MSSA strains. Pseudomonas aeruginosa was cultured in 3 patients, each requiring at least one reintervention. Other organisms included Cutibacterium acnes, Acinetobacter pittii, Enterococcus faecalis, Klebsiella pneumoniae, and Corynebacterium striatum. Polymicrobial infections occurred in 7 cases. One patient had a rare pathogen, Wohlfahrtiimonas chitiniclastica, complicating diagnosis and therapy. Infections caused by Gram-negative or multidrug-resistant bacteria were associated with longer treatment durations and more reoperations.
Systemic antibiotic regimens were selected in collaboration with infectious disease specialists and were tailored to the organism identified. A key component of our protocol was the use of Daptomycin, which was the most frequently used agent (11 patients), often in combination with rifampicin, cefepime, or meropenem. Overall, the majority of the cohort (12 patients, 70.6%) received combined systemic and local antimicrobial treatment, with therapy continued for more than 12 weeks in 10 patients (58.8%). This combined approach underscores the aggressive nature of treatment for these resistant pathogens.
Complications were reported in 10 patients (58.8%), the most common being persistent draining fistulas (5 patients), non-union (4 patients), and implant failure (1patient). Reintervention was necessary in 9 patients (52.9%), primarily among those with infections due to Pseudomonas aeruginosa or MRSA, and among those undergoing arthrodesis or bone transport. Patients with polymicrobial or resistant infections had the highest risk of failure. Limb salvage was achieved in 16 patients (94.1%). Therefore, minor complications accounted for 47.1% (8 of 17) of the cohort and including 6 cases of pin tract infection and 2 cases of superficial wound dehiscence, all managed conservatively. Major complications accounted for 11.7% (2 of 17) of the cohort, comprising one case of deep re-infection requiring repeat debridement and the single case resulting in below-knee amputation.
Second-stage surgical procedures were performed in 10 patients. Autologous iliac crest bone grafts were used in four patients, while two received cadaveric grafts. The remaining cases used synthetic or composite substitutes. Seven patients underwent tibiotalar or tibiocalcaneal arthrodesis using either retrograde nails or plates. Two patients underwent bone transport with corticotomy and distraction through circular frames. One patient ultimately required transtibial amputation due to combined failure of soft tissue coverage, infection control, and fixation (Table 3).

Table 3.
Laboratory and type of treatment of the study cohort, including isolated pathogen microorganism, antibiotic therapy, bone and soft tissues reconstruction techniques, following by all complications registered in almost 24 months of follow-up.
Functional recovery and health-related quality of life were assessed at final follow-up using the self-reported EQ-5D-5L questionnaire. It is a standardized, non-disease-specific Patient-Reported Outcome Measures (PROMs) used internationally to assess an individual’s Health-Related Quality of Life (HRQoL). It is frequently employed in clinical trials, economic evaluations, and health policy decisions due to its simplicity and robust psychometric properties [23]. The most impaired domains were “usual activities” (mean 3.4), “mobility” (3.1), and “pain/discomfort” (2.9). “Self-care” and “anxiety/depression” were less severely impacted. Patients who required multiple surgeries, especially for infection recurrence, reported lower functional scores overall. These findings are consistent with published data on the long-term morbidity of chronic post-traumatic osteomyelitis (Table 4).

Table 4.
Functional outcomes were evaluated using the EQ-5D-5L index at final follow-up.
4. Discussion
The management of infections involving the distal tibia and ankle remains a significant challenge in orthopedic surgery. These complex cases require a multidisciplinary approach that integrates orthopedic and plastic surgery principles to optimize outcomes. Key components of successful treatment include meticulous debridement, stable skeletal fixation, and effective soft tissue coverage [2,3].
Within our cohort, several highly complex cases were managed through coordinated collaboration between orthopedic surgeons, infectious disease specialists, plastic surgeons, and interventional radiologists (Figure 2). Our findings underscore the critical impact of chronicity on the treatment complexity, demonstrating that infections treated beyond 90 days from the initial trauma were associated with a notably higher surgical reintervention rate (67% vs. 37%). This observation aligns closely with established literature. Similarly, Niebuhr et al., in their systematic review, identified chronic infection as a major risk factor for subsequent treatment failure [24].

Figure 2.
39-year-old male with a history of distal tibial metaphyseal fracture treated with ORIF, complicated by chronic osteomyelitis. He underwent one single stage surgical procedure including fistulectomy, partial tibial resection with 3 × 5 cm cortical window, debridement, and antibiotic cement placement, covered with a peroneal perforator flap.
In our cohort, external fixation was as the most frequently employed surgical technique, particularly in cases characterized by severe bone loss and multi-fragmentary fractures. This approach is supported by previous studies demonstrating the efficacy of external fixation in managing of complex distal tibial fractures while minimizing disruption of soft tissues [25]. However, our findings showed higher incidence of complications associated with external fixation, notably fistulas and hardware exposure, in line with complication rates reported in the literature ranging from 7% to 32% [7].
Our overall complication rate (58.8%) aligns with the study of Brauns et al., who observed a 55% reoperation rate in infected pilon non-unions [26]. However, our limb salvage rate (94.1%) was higher than the 85–90% typically reported in similar series, possibly reflecting early multidisciplinary management [27,28]. This case involved a patient presenting with an extremely chronic, polymicrobial infection (including resistant Pseudomonas), coupled with severe, uncontrolled diabetes mellitus and extensive vascular compromise precluding successful revascularization and reliable free flap coverage. Despite aggressive debridement and multiple attempts at infection control, the combination of a persistently non-healing soft tissue envelope, progressive bony necrosis, and significant patient-reported pain led to the final decision for below-knee amputation, prioritizing patient function and definitive infection clearance.
A recent study by Sambri et al. evaluated 13 patients with infection-related distal tibial fractures managed through an orthoplastic approach, including antibiotic-loaded spacers and vascularized flaps. At a follow-up of 25 months, no recurrences of infection were observed, suggesting the efficacy of a comprehensive orthoplastic protocol in infection control [27]. Compared with this study, our results confirm that combined orthoplastic management achieves infection control rates exceeding 90%, despite variable reconstructive techniques.
Conversely, the utilization of plates and bone transport techniques demonstrated lower complication rates. The strategic application of these methods in less complex fracture patterns or as part of a staged reconstruction protocol may account for the favourable outcomes observed [8]. A case report involving the use of the Masquelet technique combined with a PRECICE nail for segmental bone defects further underscores the utility of staged reconstructive procedures in managing post-traumatic infections [4].
Our exploratory analysis revealed a statistically significant correlation between the extent of bone resection and the occurrence of complications (p = 0.0043), highlighting a strong association within this cohort. Larger resections pose challenges in achieving stable fixation and adequate soft tissue coverage, thereby increasing the risk of postoperative complications [24]. Additionally, prolonged orthoplastic procedures were significantly associated with higher complication rates (p = 0.0017), suggesting that extended surgical time reflects the level of procedural complexity and potential morbidity in these challenging cases [25].
A study on the implementation of an orthoplastic treatment protocol for open tibial fractures demonstrated a marked reduction in infection rates from 20.6% to 1.6%, further reinforcing the importance of a structured, multidisciplinary approach in managing complex tibial infections [28].
The demographic profile of our patient population, characterized by a mean age of 47.2 years and a male predominance (68%), reflects the epidemiological trends observed in distal tibial and ankle infections [29]. While our study did not find a statistically significant association between sex and fracture frequency (p = 0.3856), the higher prevalence in males warrants further investigation into potential occupational or behavioural risk factors.
The retrospective nature of our study and the relatively small sample size limit the generalizability of our findings. Moreover, given the retrospective and descriptive nature of our study, all associations should be interpreted as correlations rather than causal relationships. In fact, while our analysis identified strong associations between factors such as the timing of surgery (beyond 90 days), the extent of bone resection, and the presence of complications, these findings represent correlations within our cohort and do not establish a causal relationship. Future prospective studies are necessary to validate these observations and confirm the prognostic value of these factors.
One other limitation of this study is that incomplete data for AOFAS, FFI, and SF-36 scores prevented their inclusion in the analysis. Moreover, the integration of advanced imaging modalities and biomarker analyses may enhance the early detection of complications and inform personalized treatment strategies.
5. Conclusions
Our study underscores the critical role of a tailored, multidisciplinary approach in managing distal tibial and ankle infections. The selection of surgical techniques should be guided by the complexity of the fracture, the extent of bone and soft tissue involvement, and patient-specific factors. External fixation was the most frequently employed technique in this cohort, primarily due to the complexity of the cases rather than superior efficacy. Given the observed rate of complications, its role should be considered within a staged, multidisciplinary treatment algorithm rather than as a standalone solution. Careful patient selection, appropriate timing of conversion to internal fixation, and coordinated orthoplastic management remain key to optimizing outcomes and minimizing recurrent infection.
Author Contributions
Conceptualization, A.M. and C.C.; methodology, T.G.; software, F.M.; validation, A.D.F. and G.G.M.; formal analysis, V.C.; investigation, C.B.; resources, C.P.; data curation, C.C.; writing—original draft preparation, A.M.; writing—review and editing, C.C.; visualization, C.B.; supervision, G.M.; project administration, C.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Orthopedic and Traumatology Institute of Università Cattolica del Sacro Cuore—Roma. As this is an approval from the Review Board of Orthopedic and Traumatology Institute, there is no code.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AOFAS | Orthopaedic Foot & Ankle Society |
| BMI | Body Mass Index |
| CT | Computed Tomography |
| EQ-5D-5L | European Quality of Life 5 Dimensions 5 Level Version |
| FFI | Foot Function Index |
| FRI | Fracture-Related Infection |
| IQR | Interquartile Range |
| MRI | Magnetic Resonance Imaging |
| MRSA | methicillin-resistant Staphylococcus aureus |
| MSSA | methicillin-susceptible Staphylococcus aureus |
| PMMA | Polymethylmethacrylate |
| SD | Standard Deviation |
| SF | Short Form |
| WHO | World Health Organization |
References
- Court-Brown, C.M.; Caesar, B. Epidemiology of Adult Fractures: A Review. Injury 2006, 37, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Tausendfreund, J.; Halm, J.; Tanis, E.; Swords, M.; Schepers, T. Post-Operative Infection Following Ankle Fracture Surgery: A Current Concepts Review. Eur. J. Trauma Emerg. Surg. 2025, 51, 157. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Yang, D.; Li, W. Assessment and Management Strategies for Postoperative Infection Risk in Tibial Plateau Fractures. Curr. Probl. Surg. 2025, 68, 101763. [Google Scholar] [CrossRef] [PubMed]
- Zuluaga, M.; Cadavid, S.; Reina, F.; Reyes-Arceo, A.; Benedetti, F. Orthoplastic Management of Distal Tibia Bone Infection Using Masquelet Technique and PRECICE Nail: A Case Report. Trauma Case Rep. 2023, 45, 100834. [Google Scholar] [CrossRef]
- Kotsarinis, G.; Santolini, E.; Kanakaris, N.; Giannoudis, P.V. The Outcomes of the Management of Complex Distal Tibia and Ankle Fractures in Elderly with Tibiotalocalcaneal Nail in a Minimum 12-Month Follow-up Period. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 2723–2728. [Google Scholar] [CrossRef]
- Lindbloom, B.J.; James, E.R.; McGarvey, W.C. Osteomyelitis of the Foot and Ankle: Diagnosis, Epidemiology, and Treatment. Foot Ankle Clin. 2014, 19, 569–588. [Google Scholar] [CrossRef]
- Tausendfreund, J.; Penning, D.; Naryapragi, M.A.; Reisinger, K.W.; Tanis, E.; Joosse, P.; Schepers, T. Predicting Surgical Site Infections after Open Reduction and Internal Fixation for Ankle Fractures. Arch. Orthop. Trauma Surg. 2025, 145, 135. [Google Scholar] [CrossRef]
- Sharma, B.; Kapoor, R.; Mittal, V.; Sharma, Y.; Anand, V.S.; Gupta, P.; Vimal, Y. Evaluating Fixation Strategies in Distal Tibial Fractures: Nailing versus Plating. J. Orthop. Traumatol. Rehabil. 2025, 17, 24–27. [Google Scholar] [CrossRef]
- Trimaille, A.; Kerfant, N.; Henry, A.-S.; Ta, P.; Rouanet, M.; Le Nen, D.; Stindel, E.; Ansart, S.; Hu, W. Multidisciplinary Management of the Bone and Joint Infection Complicating Treatment of an Open Fracture of the Lower Limb. Ann. Chir. Plast. Esthet. 2020, 65, 380–393. [Google Scholar] [CrossRef]
- Lim, J.A.; Thahir, A.; Zhou, A.K.; Girish, M.; Krkovic, M. Definitive Management of Open Pilon Fractures with Fine Wire Fixation. Injury 2020, 51, 2717–2722. [Google Scholar] [CrossRef]
- Mathieu, L.; Bilichtin, E.; Durand, M.; de l’Escalopier, N.; Murison, J.C.; Collombet, J.-M.; Rigal, S. Masquelet Technique for Open Tibia Fractures in a Military Setting. Eur. J. Trauma Emerg. Surg. 2020, 46, 1099–1105. [Google Scholar] [CrossRef]
- Halawi, M.J.; Morwood, M.P. Acute Management of Open Fractures: An Evidence-Based Review. Orthopedics 2015, 38, e1025–e1033. [Google Scholar] [CrossRef] [PubMed]
- Aljuhani, W.S.; Alshabi, Y.A.; Alanazi, A.M.; Alothri, M.A.; Almutairi, S.A.; Aljaafri, Z.A.; Alzahrani, A.M. Risk of Infection and Conversion Time from External to Definitive Fixation in Open Tibial Fracture. J. Orthop. Surg. Res. 2024, 19, 867. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, S.M.; Papakostidis, C.; Giannoudis, V.P.; Mandía-Martínez, A.; Giannoudis, P.V. Distraction Osteogenesis versus Induced Membrane Technique for Infected Tibial Non-Unions with Segmental Bone Loss: A Systematic Review of the Literature and Meta-Analysis of Available Studies. Eur. J. Trauma Emerg. Surg. 2024, 50, 705–721. [Google Scholar] [CrossRef]
- Comisi, C.; Greco, T.; Inverso, M.; Mascio, A.; Polichetti, C.; Barbaliscia, M.; La Vergata, V.; Mosca, M.; Caravelli, S.; Mondanelli, N.; et al. Tibiotalocalcaneal Arthrodesis in a Rare Case of Tuberculosis of the Talus. Med. Glas. 2024, 21, 222–228. [Google Scholar] [CrossRef]
- Caravelli, S.; Ambrosino, G.; Vocale, E.; Di Ponte, M.; Puccetti, G.; Perisano, C.; Greco, T.; Rinaldi, V.G.; Marcheggiani Muccioli, G.M.; Zaffagnini, S.; et al. Custom-made implants in ankle bone loss: A retrospective assessment of reconstruction/arthrodesis in sequelae of septic non-union of the tibial pilon. Medicina 2022, 58, 1641. [Google Scholar] [CrossRef]
- Ye, Z.; Zhao, S.; Zeng, C.; Luo, Z.; Yuan, S.; Li, R. Study on the Relationship between the Timing of Conversion from External Fixation to Internal Fixation and Infection in the Treatment of Open Fractures of Extremities. J. Orthop. Surg. Res. 2021, 16, 662. [Google Scholar] [CrossRef] [PubMed]
- Perisano, C.; Cannella, A.; Polichetti, C.; Mascio, A.; Comisi, C.; De Santis, V.; Caravelli, S.; Mosca, M.; Spedicato, G.A.; Maccauro, G.; et al. Tibiotalar and Tibiotalocalcaneal Arthrodesis with Paragon28 SilverbackTM Plating System in Patients with Severe Ankle and Hindfoot Deformity. Medicina 2023, 59, 344. [Google Scholar] [CrossRef]
- Momodu, I.I.; Savaliya, V. Osteomyelitis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Mills, H.; Donnelly, L.; Platt, S. Locally Delivered Antibiotics in Fracture-Related Infection. Cureus 2024, 16, e73210. [Google Scholar] [CrossRef]
- Metsemakers, W.J.; Morgenstern, M.; McNally, M.A.; Moriarty, T.F.; McFadyen, I.; Scarborough, M.; Athanasou, N.A.; Ochsner, P.E.; Kuehl, R.; Raschke, M.; et al. Fracture-Related Infection: A Consensus on Definition from an International Expert Group. Injury 2018, 49, 505–510. [Google Scholar] [CrossRef]
- Feng, Y.-S.; Kohlmann, T.; Janssen, M.F.; Buchholz, I. Psychometric Properties of the EQ-5D-5L: A Systematic Review of the Literature. Qual. Life Res. 2021, 30, 647–673. [Google Scholar] [CrossRef] [PubMed]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and Preliminary Testing of the New Five-Level Version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Niebuhr, D.; Mattson, T.; Jensen, N.M.; Viberg, B.; Steenstrup Jensen, S. Risk Factors for Tibial Infections Following Osteosynthesis—A Systematic Review and Meta-Analysis. J. Clin. Orthop. Trauma 2024, 50, 102376. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chen, K.; Xue, H.; Cheng, J.; Yu, X. Efficacy Comparison between Intramedullary Nail Fixation and Plate Fixation in Distal Tibia Fractures: A Meta-Analysis of Randomized Controlled Trials. J. Orthop. Surg. Res. 2024, 19, 403. [Google Scholar] [CrossRef] [PubMed]
- Brauns, A.; Lammens, J. The Challenge of the Infected Pilon Tibial Non-Union: Treatment with Radical Resection, Bone Transport and Ankle Arthrodesis. Acta Orthop. Belg. 2020, 86, 335–341. [Google Scholar]
- Sambri, A.; Pignatti, M.; Tedeschi, S.; Lozano Miralles, M.E.; Giannini, C.; Fiore, M.; Filippini, M.; Cipriani, R.; Viale, P.; De Paolis, M. Combined Orthoplastic Approach in Fracture-Related Infections of the Distal Tibia. Microorganisms 2022, 10, 1640. [Google Scholar] [CrossRef]
- Ylitalo, A.A.J.; Hurskainen, H.; Repo, J.P.; Kiiski, J.; Suomalainen, P.; Kaartinen, I. Implementing an Orthoplastic Treatment Protocol for Open Tibia Fractures Reduces Complication Rates in Tertiary Trauma Unit. Injury 2023, 54, 110890. [Google Scholar] [CrossRef]
- Wang, B.; Xiao, X.; Zhang, J.; Han, W.; Hersi, S.A.; Tang, X. Epidemiology and Microbiology of Fracture-Related Infection: A Multicenter Study in Northeast China. J. Orthop. Surg. Res. 2021, 16, 490. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).