Abstract
Background: Emerging parameters, such as the spino-pelvic unit and the combined sagittal index (CSI), are gaining importance in evaluating and optimizing implant positioning in total hip arthroplasty (THA). Our institution adopts the “femur first” technique to achieve the desired combined anteversion (CA). The purpose of this study is to evaluate the role of the ‘femur first’ technique and spinopelvic characteristics in achieving the CSIstanding ‘safe zone’ in primary THA. Methods: Consecutive patients undergoing primary THA were included in the present retrospective study. All patients underwent radiographic assessments in the standing position with the EOS 2D/3D radiography system. Results: Forty patients (40 hips) were enrolled. Of these, 34 patients fell inside the CSIstanding “safe zone” (205–245°). When considering the restricted CSIstanding “safe zone” for patients at high risk for adverse spinopelvic characteristics (215–245°), only 16 patients fell inside the range. We demonstrated a positive linear correlation between CSIstanding and CA (p < 0.0001). Pelvic tilt (PT) showed a positive correlation both in standing and relaxed sitting positions, (p < 0.001). Sacral slope (SS) showed a significant positive correlation in the relaxed sitting (p = 0.003) position but not in the standing position (p = 0.34). The correlation analysis between CSIrelaxed-sitting and ΔSS showed a positive correlation (p = 0.003). Conclusions: The “femur first” technique is able to achieve the CSI “safe zone” in most patients; however, it seems insufficient in those with adverse spinopelvic characteristics, who are at higher risk of dislocation. Moreover, the CA, the position of the pelvis in space (PT), and its mobility (ΔSS) greatly influence the CSI “safe zone” in patients undergoing primary THA.
1. Introduction
Deserving the title of ‘operation of the century’, total hip arthroplasty (THA) has revolutionized the life of patients suffering from hip osteoarthritis (OA), and it is expected that the total number of procedures performed will grow up to 635,000 by 2030 [,,]. As a direct consequence, the number of revision procedures is in constant increase, reaching 50.000 yearly only in the US with related costs up to $1 billion [,,,]. When evaluating causes of revisions, recurrent dislocation appears to be the most represented; thus, new parameters are emerging to evaluate and properly perform the implant position [,,]. Among these, the spino-pelvic unit and the resulting hip–spine relationship are becoming particularly relevant in preoperative planning [,,,,]. Heckman et al. introduced a new parameter to assess the sagittal plane of movement, the combined sagittal index (CSI), which is the sum of Pelvic Femoral Angle (PFA) and Anteinclination (AI) (CSI = PFA + AI). This parameter can be calculated in both the standing and relaxed-seated position and is a predictor of impingement and dislocation risk []. Heckman et al. introduced a CSIrelaxed-sitting “safe zone” of CSIrelaxed-sitting > 158.5° for risk for anterior impingement and posterior dislocation []. Grammatopoulos et al. introduced a “safe zone” for this parameter. A CSIstanding under 215° could expose the patients to posterior instability and a CSIstanding over 245° could expose the patients to anterior instability. Hence, the suggested window of security is 205° < CSIstanding < 245° for patients without spinopelvic pathology and 215° < CSIstanding < 235° in case of unbalanced or rigid spine. Values beyond these ranges have been considered to be at increased risk of dislocation [].
Our institution has so far adopted a ‘Femur First’ Technique to obtain the desired combined anteversion (CA), translating in a proper orientation of both acetabular and femoral components. It represents a smart method able to achieve a satisfactory implant positioning in a non-navigated and non-robotic way, through a simple though reproducible surgical technique []. However, no studies were conducted to evaluate the eventual relation between this surgical technique and the emerging spinopelvic characteristics. Hence, the purpose of the present study is to evaluate the role of the ‘Femur First’ Technique, CA, and spinopelvic characteristics in achieving the CSI ‘safe zone’ in primary THA.
Our primary endpoint was to evaluate if patients undergoing THA with the “femur first” technique would fall inside the CSI “safe zone”.
Our secondary endpoints were correlation between the CSIstanding value and the CA value; correlation between the CSIstanding value and the femoral torsion (FT) value; correlation between the CSIstanding value and the pelvic tilt (PT) or the sacral slope (SS) in the standing position; correlation between the CSIrelaxed-sitting value and the PT or SS in the sitting position; and correlation between the CSIrelaxed-sitting value and spine mobility.
2. Materials and Methods
2.1. Study Population
All individual participants signed written informed consents for undergoing the surgery and for inclusion in the registry of orthopaedic surgical procedures, within the scope of research and improvement of clinical practice. The study was conducted in accordance with the Declaration of Helsinki and good clinical practice guidelines. The study protocol was approved by the Ethics Committee of IRCCS Humanitas Research Hospital (protocol code 618/17). Consecutive patients undergoing primary THA were included in the present study. Inclusion criteria included patients >18 years old eligible for primary THA with diagnosis of primary OA or secondary OA due to mild development dysplasia, Perthes disease, slipped capital femoral epiphysis, and post-trauma osteoarthritis. Exclusion criteria were patients eligible for partial or total THA revision, THA associated with other procedures (i.e., femoral osteotomy), previous pelvic and/or femoral osteotomy, severe hip dysplasia (Crowe III or IV), primitive or metastatic tumors of hip joint, previous spine and/or sacroiliac joint instrumentation, previous or current hip joint infection, and previous hip surgery of any type. All patients underwent the same surgical technique. Briefly, in lateral decubitus, after the neck osteotomy femoral rasps were inserted up to the desired size, which is left in situ. After the exposure of the acetabulum and a sequential reaming, the femur was then reduced with the proper sized rasp in situ by using a 44 mm trial plastic head with a long neck. After reduction, with the hip in neutral position at 0° of flexion and abduction, the femur was internally rotated to reach an angle of 35°, the value of the mean combined anteversion suggested by most authors, between the longitudinal axis of the tibia and the operating table []. Only cementless short-stem femoral components were used across all cases. Since the CA is the degree of internal rotation to produce a coplanar head and cup, the definitive cup was placed parallel to the horizontal line on the trial head in both the axial and coronal planes [].
2.2. Radiographic Assessment
All patients underwent a radiographic assessment in a standing position with the EOS 2D/3D radiography system (Biospace Med, Paris, France), performed preoperatively and at 3 months follow-up, as per department usual practice. The EOS system allows one to achieve an antero-posterior (AP) and lateral radiographic view of the whole skeletal system [,,]. The 2D images were used to perform a 3D reconstruction of the skeletal system and prosthetic components with dedicated software (sterEOS 3D, version 1.5.3.7947, Biospace Med, Paris, France). In addition, 3D images were used to preoperatively measure the caput-collum-diaphyseal (CCD) angle and femoral antetorsion [], postoperative acetabular abduction (AAb) and anteversion (AA), and postoperative FT []. The combined anteversion was determined by the following formula: cup anteversion + (0.7 × stem antetorsion) []. The AAb and AA were measured in the patient frame based on a vertical plane passing through the center of the acetabular cup, which avoids the effect of a potential axial rotation of the pelvis during acquisition. On the other hand, the FT was measured relative to posterior bi-condylar plane. The CSI is the algebraic sum of PFA and AI (CSI = PFA + AI). This parameter can be calculated both in the standing and relaxed sitting position. The PT was measured on a lateral X-ray of the pelvis as the angle between a line drawn from the midpoint of the bicoxofemoral axis to the midpoint of the sacral plate and the vertical []. The SS were measured on a lateral X-ray of the pelvis as the angle between the superior plate of S1 and a horizontal line to the floor []. Spine mobility was defined by the difference in SS from the standing and relaxed sitting position (ΔSS). Spinopelvic mobility was classified based on ΔSS as previously described [,]: stiff (<10°), normal (10–30°), and hypermobile (>30°). A ΔSS < 5° was considered suggestive of a biologically or surgically fused spine []. The AI was measured on a lateral X-ray of the pelvis as the angle between a line tangent to the anterior and posterior edges of the cup and a horizontal line parallel to the margin of the radiograph []. The PFA was measured on a lateral X-ray as the angle subtended by a line connecting the midpoint of the S1 end plate and the center of the bicoxofemoral axis and a line from the center of the bicoxofemoral axis projected distally toward the center of the knee, typically along the anterior shaft of the proximal femur [] (Figure 1 and Figure 2).
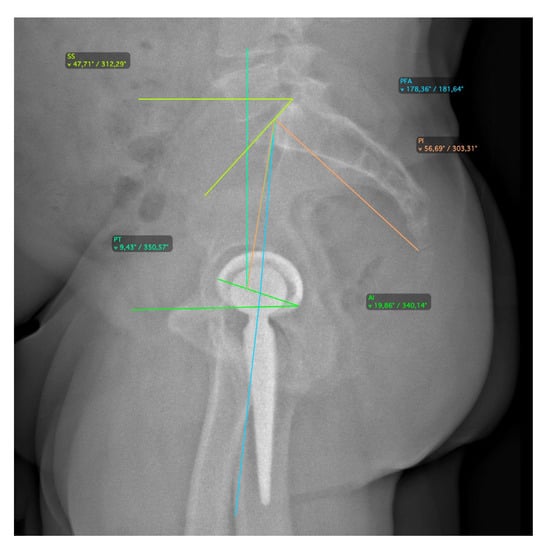
Figure 1.
Radiographic measurements for spinopelvic parameters in standing position.
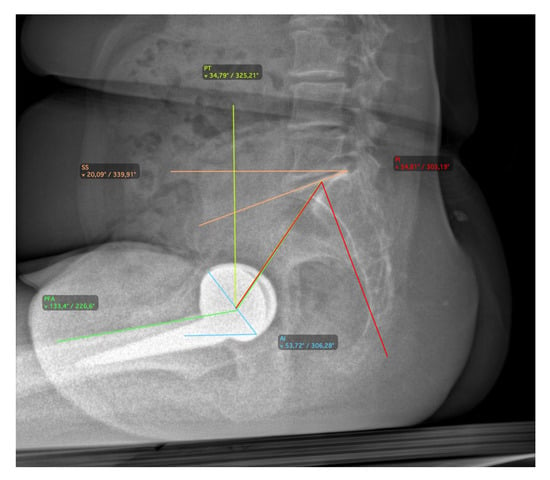
Figure 2.
Radiographic measurements for spinopelvic parameters in relaxed-sitting position.
2.3. Data Analyses
All the analyses were performed using Stata for Windows (version 18.0, StataCorp LCC, College Station, TX, USA). Descriptive statistics were calculated. The categorical variables were expressed as a frequency with percentage. Continuous variable data were expressed as a mean with standard deviation and range as minimum and maximum values. Correlation analysis was performed among the considered radiological indices. The p was considered significant for values <0.05.
3. Results
Forty patients (40 hips) undergoing primary THA were enrolled. Seventeen patients were men. The mean age was 61 years (36–84) at the time of the index procedure. Mean BMI at the surgery was 27 (18–39). The preoperative diagnosis was primary osteoarthritis in 33 patients, osteoarthritis secondary to mild development dysplasia of the hip in 6 patients, and post-trauma osteoarthritis in one patient. ΔSS was calculated for all patients and spinopelvic mobility was categorized accordingly (Table 1).

Table 1.
The table shows the distribution of the ΔSS across the patients.
All patients underwent THA through the “femur first” technique to reach the optimal intraoperative combined anteversion. Of these, 34 patients (85%) fell inside the CSIstanding “safe zone” (205–245°) (Figure 3).
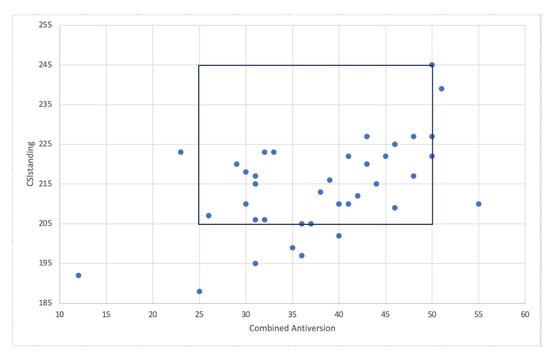
Figure 3.
The graph shows the patients inside both combined anteversion “safe zone” and CSIstanding “safe zone”.
When considering the restricted CSIstanding “safe zone” for patients at high risk for adverse spinopelvic characteristics (215–245°), only 16 (40%) patients fell inside the range (Figure 4).
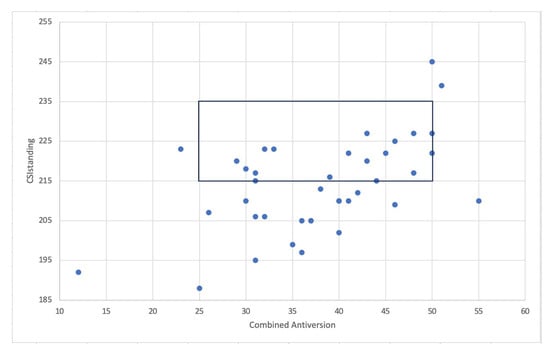
Figure 4.
The graph shows the patients inside both combined anteversion “safe zone” and CSIstanding “safe zone” for patients with adverse spinopelvic characteristics.
A further correlation analysis was performed, and it demonstrated a linear regression between combined anteversion value and the CSIstanding value. The correlation coefficient was r = 0.54, and the regression analysis showed a statistically significant correlation (r = 0.54, coefficient 0.71, 95%CI0.35; 107, p < 0.0001) (Figure 5).
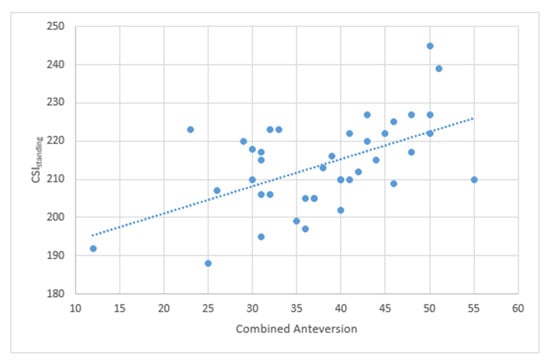
Figure 5.
The graph shows the positive linear correlation between CA and CSIstanding.
The subgroup analysis showed no statistically significant difference when adjusting the correlation for sex (p = 0.37) and age (p = 0.51).
The correlation analysis between CSIstanding and FT showed a positive correlation r = 0.18, though not statistically significant (Figure 6).
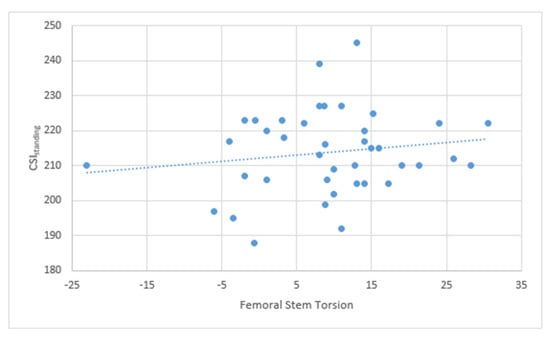
Figure 6.
The graph shows the positive linear correlation between FT and CSIstanding.
The study on the positional parameters of the pelvis and the CSIstanding or CSIrelaxed-sitting showed a statistically significant positive correlation for most of the parameter in either position. PT showed a significant positive correlation both in a standing (r = 0.6548, coefficient 1.07, 95%CI 0.67; 1.47, p < 0.001) and in a relaxed sitting position (r = 0.6360, coefficient 1.27, 95%CI 0.76; 1.78, p < 0.001). SS showed a significant positive correlation in a relaxed sitting (r = −0.4572, coefficient −0.75, 95%CI −1.23; −0.27, p = 0.003) position but not in a standing position (r= 0.25, 95%CI −0.27, 0.78, p = 0.34).
The correlation analysis between CSIrelaxed-sitting and ΔSS showed a statistically significant positive correlation with a correlation coefficient of 0.82 (p = 0.003) (Figure 7).
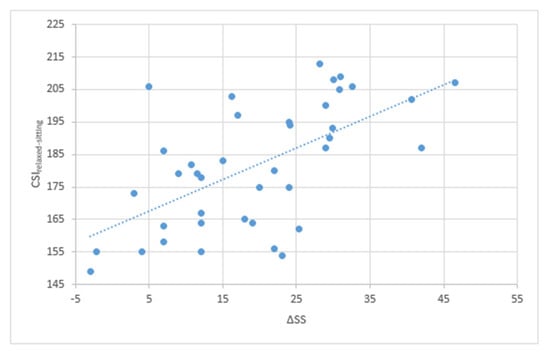
Figure 7.
The graph shows the positive linear correlation between ΔSS and CSIrelaxed-sitting.
4. Discussion
The main finding of the present retrospective clinical study is that the “femur first” technique is able to achieve the CSI “safe zone” in most patients; however, it seems insufficient in those with adverse spinopelvic characteristics, who are at higher risk of dislocation. Moreover, the CA, the position of the pelvis in the space (PT), and its mobility (ΔSS) greatly influence the CSI “safe zone” in patients undergoing primary THA.
The continuous effort in terms of dislocation prevention is given by the current trends in hip arthroplasty surgery. In fact, despite these efforts, the revision rate for dislocation in the last 8 years has not diminished significantly. This is demonstrated by the annual report from the British NHS, which shows a slight decrease in the overall revision rate from 1 per 1000 THA to 0.76 per 1000 THA. However, the revision rate in the first year after surgery has actually increased, from 2.33 per 1000 THA to 2.46 per 1000 THA []. Hence, the last few years have witnessed the rise of the functional and personalized positioning of the acetabular and femoral component to reduce the postoperative dislocation rate []. The supporters of this new approach claim that placing the cup and the femoral stem with functional or personalized technique should prevent impingement, whether it be implant on implant, implant on bone, or bone on bone, in each position that the patient is able to achieve []. The advent and spread of navigation systems and robot-assisted surgery, enabling surgeons to position the components with minimal error, have paved a new era in the field of THA. These innovations allow the operator to aim for very precise target zones, usually required in functional or personalized implant positioning []. However, to date there is not unanimous agreement on what is the “correct positioning” of the implants, and which is the correct “safe zone” that should be aimed for. CSIStanding “safe zone” is a promising target that considers the sagittal component positioning and the sagittal balance of the patient. In 2021, Grammatopoulos et al. defined two CSIstanding “safe zones”: one for patients without adverse spinopelvic characteristics (205° < CSIstanding < 245°) and one for patients with adverse spinopelvic characteristics (215° < CSIstanding < 235°), defined by the authors as unbalanced (PI-LL > 10°) and/or rigid (ΔSS < 10°) lumbar spine []. In the present study, it was demonstrated that performing a THA with a “femur first” technique can result in having 85% of patients (34 patients out of 40) falling inside the CSIstanding safe zone of 205–245. It is known that having an implant outside this “safe zone” increases your risk of dislocation (odds ratio [OR]: 4.2; 95% confidence interval [CI]: 2.2 to 8.2; p < 0.001). When considering the “safe zone” for patients at high risk for their spinopelvic characteristics, only 40% (16 patients out of 40) fell inside the CSIstanding safe zone (215–245°). Being outside the “safe zone” exposes these patients to an even greater risk of dislocation (OR: 5.1; 95% CI: 1.8 to 14.9; p = 0.001) [].
Falling inside the CSIstanding 205–245° “safe zone” four out of five times is an interesting result, considering that this specific “safe zone” was not aimed for. It is possible that these results were retrieved thanks to this specific surgical technique, which aims at achieving a perfect coplanarity between the implants, not only regarding the CA value but also the abduction angle of the cup. Furthermore, extreme anatomical abnormalities were corrected, such as high-grade ante- or retroversion of the femur or the acetabulum.
This hypothesis is further strengthened by the statistically significant linear positive correlation between the CA value and the CSIstanding with an increase of 0.71° of CSI every 1° of CA value. This could be interpreted as a significant finding that advances our understanding of how different parameters and “safe zones” are interconnected.
When evaluating the restricted CSIstanding 215–235° “safe zone”, only 40% (16 out of 40) of the patients fell inside the target. These results could be considered unsatisfactory, as patients who need to achieve this restricted “safe zone” are those at higher risk of dislocation. Therefore, it is obvious that the current “femur first” technique needs to be improved to better target both the CA and the CSIstanding “safe zone”. To achieve such a narrow target, the use of a navigation system or robot-assisted surgery might be required. Moreover, it is predictable that, once these new technologies prove their efficacy and reliability, they could be adopted for all patients, regardless of their risk factors.
Moreover, a positive correlation between the FT and the CSIstanding value was found, with a coefficient of 0.18 (for every degree of anteversion of the femoral stem the CSI increase of 0.18°), but it was not statistically significant. This is possibly related to the small sample of this study, and it should be tested on a larger sample size. The low value of the coefficient is probably a consequence of acetabular anteversion being one of the three parameters forming the AI (acetabular anteversion, angle of abduction of the cup, and pelvic tilt) []. These findings support the idea that correcting extreme abnormalities in femoral version helps to achieve the CSIstanding “safe zone”. A similar conclusion was drawn by Loppini et al., advising against positioning the acetabular cup in severe anteversion or retroversion, to compensate for femoral abnormalities []. In this study it was demonstrated that positional parameter of the pelvis, such as PT and SS, and mobility of the pelvis, such as ΔSS, influence greatly the CSIstanding and CSIrelaxed-sitting. PT has a statistically significant linear positive correlation with CSIstanding and CSIrelaxed-sitting. SS has a statistical correlation with CSIrelaxed-sitting but not with CSIstanding. The authors believe this could be attributed to the limited sample size of the study. This is because the positional parameters of the pelvis are governed by a mathematical formula (Pl = PT + SS) and exhibit an inverse relationship []. Therefore, it is necessary to conduct further testing with a larger sample size. Furthermore, it was observed that these correlations are analogous to the femoral anteversion value, as Al is also influenced by PT and SS. Additionally, a statistically significant positive linear correlation between CSlrelaxed-siting and ∆SS was established, from the standing to the sitting position, with a correlation coefficient of 0.82. ΔSS represents the mobility of the spine necessary for the acetabulum to open up when transitioning from the standing to the sitting position []. Patients with low ΔSS have the tendency of having a low CSIrelaxed-sitting value, exposing them to the risk of anterior impingement and posterior dislocation when transitioning to the sitting position. While this relationship was previously recognized in the literature, to our knowledge, this is the first time it was demonstrated in clinical practice [].
Nonetheless, the present study is not free from limitations. A formal power calculation was not performed due to the retrospective nature and limited patient sample, hence limiting the generalizability of our findings. In fact, while several statistically significant associations were identified, suggesting an adequate statistical signal, these findings should be interpreted with caution and validated in future prospective studies with predefined sample size estimation. Additionally, although a consistent surgical approach and implant system were used, unmeasured variables such as lumbar degenerative disease, spinopelvic stiffness, or patient-reported outcome scores may have influenced implant positioning or outcomes and should be investigated in future studies. Moreover, the retrospective nature of the study, the absence of a control group, and the impossibility to categorize the patients for their spinal characteristics due to the lack of the lumbar spine in the available X-rays, further reduce the strength of the retrieved results. Additionally, although a consistent surgical approach and implant system were used for all patients, we acknowledge that not measured variables, such as undiagnosed lumbar spine stiffness or other spinal disease, may influence pelvic dynamics and implant orientation. These potential confounders should be explored in future prospective studies that include dedicated lumbar imaging and spinal mobility assessments. These limitations highlight the need for further investigations to eventually confirm our hypothesis.
5. Conclusions
The “femur first” technique is able to achieve the CSI “safe zone” in most patients; however, it seems insufficient in those with adverse spinopelvic characteristics, who are at higher risk of dislocation. Moreover, the CA, the position of the pelvis in space (PT), and its mobility (ΔSS) greatly influence the CSI “safe zone” in patients undergoing primary THA.
Author Contributions
Conceptualization, E.G., M.L. and G.G.; methodology, M.L. and E.G.; software, E.G.; validation, E.G., G.A., and M.L.; formal analysis, E.M.; investigation, E.G. and M.L.; resources, E.G. and G.A.; data curation, E.G., G.A., and E.M.; writing—original draft preparation, E.G.; writing—review and editing, G.A. and M.L.; visualization, G.G. and F.L.C.; supervision, G.G., F.L.C., and M.L.; project administration, M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study protocol for the development of this registry was approved on 18 December 2017 by the Ethics Committee of IRCCS Humanitas Research Hospital (protocol code 618/17).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data supporting the reported results can be found in a repository (Zenodo).
Acknowledgments
The authors would like to thank the Livio Sciutto Foundation for Medical Research. This is a non-profit social organization that recorded in its database the data of the patients included in the study with the previous consent of the patients and respecting the current law on privacy.
Conflicts of Interest
The authors declare the following financial interests/personal relationships, which may be considered as potential competing interests: G.G. declares royalties and licenses from Zimmer Biomet, Innomed, and Adler Ortho, and financial support for attending symposia and educational programs from Zimmer Biomet. M.L. declares research grants as Principal Investigator for a post-market study for medical devices from Zimmer Biomet and a research grant as principal investigator (2022YME9N3) from the Italian Ministry of University. E.G., G.A., F.L.C., and E.M. declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PFA | pelvic femoral angle (PFA) |
| OA | osteoarthritis |
| AI | anteinclination |
| CSI | combined sagittal index |
| THA | total hip arthroplasty |
| CA | combined anteversion |
| CCD | caput-collum-diaphyseal |
| AA | anteversion |
| FT | femoral torsion |
| AP | antero-posterior |
| AAb | acetabular abduction |
| PT | pelvic tilt |
| SS | sacral slope |
References
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J. Bone Jt. Surg. Am. 2018, 100, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The Operation of the Century: Total Hip Replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Maradit Kremers, H.; Larson, D.R.; Crowson, C.S.; Kremers, W.K.; Washington, R.E.; Steiner, C.A.; Jiranek, W.A.; Berry, D.J. Prevalence of Total Hip and Knee Replacement in the United States. JBJS 2015, 97, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Prokopetz, J.J.; Losina, E.; Bliss, R.L.; Wright, J.; Baron, J.A.; Katz, J.N. Risk Factors for Revision of Primary Total Hip Arthroplasty: A Systematic Review. BMC Musculoskelet. Disord. 2012, 13, 251. [Google Scholar] [CrossRef]
- Heo, K.; Karzon, A.; Shah, J.; Ayeni, A.; Rodoni, B.; Erens, G.A.; Guild, G.N.; Premkumar, A. Trends in Costs and Professional Reimbursements for Revision Total Hip and Knee Arthroplasty. J. Arthroplast. 2024, 39, 612–618.e1. [Google Scholar] [CrossRef]
- Loppini, M.; Gambaro, F.M.; Nelissen, R.G.H.H.; Grappiolo, G. Large Variation in Timing of Follow-up Visits after Hip Replacement: A Review of the Literature. EFORT Open Rev. 2022, 7, 200–205. [Google Scholar] [CrossRef]
- Loppini, M.; Pisano, A.; Gandolfi, C.E.; Morenghi, E.; Grappiolo, G. Complications, Readmission and Reoperation Rates in One-Stage Bilateral versus Unilateral Total Hip Arthroplasty: A High-Volume Single Center Case-Control Study. Sci. Rep. 2021, 11, 6299. [Google Scholar] [CrossRef]
- Bozic, K.J.; Kurtz, S.M.; Lau, E.; Ong, K.; Vail, T.P.; Berry, D.J. The Epidemiology of Revision Total Hip Arthroplasty in the United States. J. Bone. Jt. Surg. Am. 2009, 91, 128–133. [Google Scholar] [CrossRef]
- Gwam, C.U.; Mistry, J.B.; Mohamed, N.S.; Thomas, M.; Bigart, K.C.; Mont, M.A.; Delanois, R.E. Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J. Arthroplast. 2017, 32, 2088–2092. [Google Scholar] [CrossRef]
- Loppini, M.; Temporiti, F.; Furone, R.; Galli, M.; Grappiolo, G.; Gatti, R. Static and Dynamic Pelvic Kinematics after One-Stage Bilateral or Unilateral Total Hip Arthroplasty. Hip Int. 2021, 31, 729–734. [Google Scholar] [CrossRef]
- Dorr, L.D.; Callaghan, J.J. Death of the Lewinnek “Safe Zone”. J. Arthroplast. 2019, 34, 1–2. [Google Scholar] [CrossRef]
- Loppini, M.; Pisano, A.; Ruggeri, R.; Della Rocca, A.; Grappiolo, G. Pelvic Tilt and Functional Acetabular Position after Total Hip Arthroplasty: An EOS 2D/3D Radiographic Study. Hip Int. 2023, 33, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Loppini, M.; Longo, U.G.; Ragucci, P.; Trenti, N.; Balzarini, L.; Grappiolo, G. Analysis of the Pelvic Functional Orientation in the Sagittal Plane: A Radiographic Study with EOS 2D/3D Technology. J. Arthroplast. 2017, 32, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
- Grammatopoulos, G.; Innmann, M.; Phan, P.; Bodner, R.; Meermans, G. Spinopelvic Challenges in Primary Total Hip Arthroplasty. EFORT Open Rev. 2023, 8, 298–312. [Google Scholar] [CrossRef] [PubMed]
- van der Gronde, B.A.T.D.; Schlösser, T.P.C.; van Erp, J.H.J.; Snijders, T.E.; Castelein, R.M.; Weinans, H.; de Gast, A. Current Evidence for Spinopelvic Characteristics Influencing Total Hip Arthroplasty Dislocation Risk. JBJS Rev. 2022, 10, e22. [Google Scholar] [CrossRef]
- Heckmann, N.; McKnight, B.; Stefl, M.; Trasolini, N.A.; Ike, H.; Dorr, L.D. Late Dislocation Following Total Hip Arthroplasty: Spinopelvic Imbalance as a Causative Factor. J. Bone Jt. Surg. Am. 2018, 100, 1845–1853. [Google Scholar] [CrossRef]
- Grammatopoulos, G.; Oxon, D.; Tr, F.; Falsetto, A.; Sanders, E. Integrating the Combined Sagittal Index Reduces. JBJS 2022, 104, 397–411. [Google Scholar] [CrossRef]
- Loppini, M.; Longo, U.G.; Caldarella, E.; Rocca, A.; Della; Denaro, V.; Grappiolo, G. Femur First Surgical Technique: A Smart Non-Computer-Based Procedure to Achieve the Combined Anteversion in Primary Total Hip Arthroplasty. BMC Musculoskelet. Disord. 2017, 18, 331. [Google Scholar] [CrossRef]
- Widmer, K.-H.; Zurfluh, B. Compliant Positioning of Total Hip Components for Optimal Range of Motion. J. Orthop. Res. 2004, 22, 815–821. [Google Scholar] [CrossRef]
- Rivière, C.; Hardijzer, A.; Lazennec, J.Y.; Beaulé, P.; Muirhead-Allwood, S.; Cobb, J. Spine-Hip Relations Add Understandings to the Pathophysiology of Femoro-Acetabular Impingement: A Systematic Review. Orthop. Traumatol. Surg. Res. 2017, 103, 549–557. [Google Scholar] [CrossRef]
- Lazennec, J.Y.; Brusson, A.; Dominique, F.; Rousseau, M.A.; Pour, A.E. Offset and Anteversion Reconstruction after Cemented and Uncemented Total Hip Arthroplasty: An Evaluation with the Low-Dose EOS System Comparing Two- and Three-Dimensional Imaging. Int. Orthop. 2015, 39, 1259–1267. [Google Scholar] [CrossRef]
- Lazennec, J.Y.; Rousseau, M.A.; Rangel, A.; Gorin, M.; Belicourt, C.; Brusson, A.; Catonné, Y. Pelvis and Total Hip Arthroplasty Acetabular Component Orientations in Sitting and Standing Positions: Measurements Reproductibility with EOS Imaging System versus Conventional Radiographies. Orthop. Traumatol. Surg. Res. 2011, 97, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Than, P.; Szuper, K.; Somoskeöy, S.; Warta, V.; Illés, T. Geometrical Values of the Normal and Arthritic Hip and Knee Detected with the EOS Imaging System. Int. Orthop. 2012, 36, 1291–1297. [Google Scholar] [CrossRef] [PubMed]
- Lazennec, J.-Y.; Rousseau, M.-A.; Brusson, A.; Folinais, D.; Amel, M.; Clarke, I.; Pour, A.E. Total Hip Prostheses in Standing, Sitting and Squatting Positions: An Overview of Our 8 Years Practice Using the EOS Imaging Technology. Open Orthop. J. 2015, 9, 26–44. [Google Scholar] [CrossRef] [PubMed]
- Yoshimine, F. The Safe-Zones for Combined Cup and Neck Anteversions That Fulfill the Essential Range of Motion and Their Optimum Combination in Total Hip Replacements. J. Biomech. 2006, 39, 1315–1323. [Google Scholar] [CrossRef]
- Buckland, A.; DelSole, E.; George, S.; Vira, S.; Lafage, V.; Errico, T.; Vigdorchik, J. Sagittal Pelvic Orientation A Comparison of Two Methods of Measurement. Bull. Hosp. Jt. Dis. 2017, 75, 234–240. [Google Scholar]
- Legaye, J.; Duval-Beaupère, G.; Hecquet, J.; Marty, C. Pelvic Incidence: A Fundamental Pelvic Parameter for Three-Dimensional Regulation of Spinal Sagittal Curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef]
- Stefl, M.; Lundergan, W.; Heckmann, N.; McKnight, B.; Ike, H.; Murgai, R.; Dorr, L.D. Spinopelvic Mobility and Acetabular Component Position for Total Hip Arthroplasty. Bone Jt. J. 2017, 99-B, 37–45. [Google Scholar] [CrossRef]
- Kanawade, V.; Dorr, L.D.; Wan, Z. Predictability of Acetabular Component Angular Change with Postural Shift from Standing to Sitting Position. JBJS 2014, 96, 978–986. [Google Scholar] [CrossRef]
- The National Joint Registry 11th Annual Report 2014. National Joint Registry for England, Wales and Northern Ireland. Available online: https://www.hqip.org.uk/wp-content/uploads/2018/02/national-joint-registry-11th-annual-report-2014.pdf (accessed on 14 August 2023).
- Wang, R.; Zheng, X.; Xu, T.; Gong, S.; Liu, S.; Han, L.; Yang, S.; Xu, W. Personalized Cup Positioning Guides Improved Cup Positioning and Hip Ranges of Motion in Robotic Assisted Total Hip Arthroplasty. Front. Bioeng. Biotechnol. 2020, 8, 988. [Google Scholar] [CrossRef]
- Fontalis, A.; Raj, R.D.; Kim, W.J.; Gabr, A.; Glod, F.; Foissey, C.; Kayani, B.; Putzeys, P.; Haddad, F.S. Functional Implant Positioning in Total Hip Arthroplasty and the Role of Robotic-Arm Assistance. Int. Orthop. 2023, 47, 573–584. [Google Scholar] [CrossRef]
- Le Huec, J.C.; Aunoble, S.; Philippe, L.; Nicolas, P. Pelvic Parameters: Origin and Significance. Eur. Spine J. 2011, 20, 564–571. [Google Scholar] [CrossRef]
- Heckmann, N.; Tezuka, T.; Bodner, R.J.; Dorr, L.D. Functional Anatomy of the Hip Joint. J. Arthroplast. 2021, 36, 374–378. [Google Scholar] [CrossRef]
- Louette, S.; Wignall, A.; Pandit, H. Spinopelvic Relationship and Its Impact on Total Hip Arthroplasty. Arthroplast. Today 2022, 17, 87–93. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).