Abstract
Background: Diet and lifestyle play important roles in preventing and improving chronic diseases, and evaluating behavioral risk factors in these pathologies allows for efficient management. Methods: A clinical study by screening biochemical parameters and pulmonary function was carried out to evaluate behavioral risk factors in obstructive pulmonary disease associated with metabolic syndrome. Results: Of the total of 70 patients included in the clinical study, 46 were men and 24 were women (χ2 = 3.9, p = 0.168). Forty-eight patients presented at least three met risk criteria associated with the metabolic syndrome (19 women and 29 men). Regarding the assessment of lung function, only 7 of the patients presented normal spirometry values (χ2 = 75.28, p < 0.001), and the other 63 patients presented with ventilatory dysfunction; most (over 80%) declared that they were smokers or had smoked in the past (χ2 = 5.185, p = 0.075). In terms of body weight, 45 of the patients are overweight or obese, most of them declaring that they do not consume enough vegetable products, they consume large amounts of foods of animal origin (meat, milk, eggs) but also super processed foods (food products type of junk food), do not hydrate properly, and are predominantly sedentary people (54 of the patients do no physical activity at all; χ2 = 2.12, p = 0.713). Conclusion: From the statistical processing of the data, it is noted that insufficient hydration, low consumption of vegetables, increased consumption of hyper-caloric food products rich in additives, sedentary lifestyle, and smoking are the main disruptive behavioral factors that worsen the health status in lung disease associated with the metabolic syndrome. An important conclusion emerging from the study is that the imbalances that aggravate obstructive lung diseases are generated by unhealthy food and an unbalanced lifestyle.
1. Introduction
Despite their distinct pathophysiology, Chronic Obstructive Pulmonary Disease (COPD) and Asthma exert a profound impact on respiratory health. Characterized by chronic inflammation, airway obstruction, and debilitating symptomatology, they not only pose a physical and emotional burden on millions of people, with a direct impact on lowering life quality, but they also represent a substantial economic challenge for healthcare systems, thereby affecting society worldwide [1].
Considering its multiple environmental and genetic risk factors, one still stands out, holding the leading position for COPD: tobacco smoking. With recent data suggesting that over 200 million individuals are living with this diagnosis, the major concern is that this staggering number is expected to rise. Globally, this condition has been assigned third place among the most prevalent causes of death, intensifying the emotional distress of patients facing this condition [2,3,4].
Although over the years the primary concern regarding COPD was focused on the high rates of morbidity observed among the elderly, current guidelines are also directing our attention towards the concept of ‘young COPD’, emphasizing the importance and the benefits of early disease diagnosis for patients within the age range of 20 to 50 years [4,5].
Another public health challenge, Asthma exerts substantial influence across all age groups, with a significant impact during childhood. Viral or bacterial respiratory infections, environmental allergens, and certain air pollutants represent a small part of the triggers involved in exacerbations [6,7].
Both asthma and COPD are responsible for high mortality rates, particularly in low- and middle-income areas. To improve disease control and overall survival, it is mandatory to adopt a comprehensive approach to the cases and consider and treat comorbidities in direct correlation with associated risk factors [4,8].
Multimorbidity, the coexistence of multiple chronic conditions in an individual, is a widespread issue significantly impacting patients with obstructive lung diseases. Therefore, clinicians encounter cases with more severe symptoms, a higher risk of drug interactions, and an increased probability of undesired therapeutical outcomes [9,10].
Recent treatment guidelines emphasize the importance of addressing and managing comorbidities in both asthma and COPD. While the specific conditions may vary, cardiovascular diseases, diabetes, metabolic syndrome, gastroesophageal reflux, and depression are among the most frequently encountered [4,11].
Assessing all these, metabolic syndrome (MetS) notably sets itself apart due to its alarmingly increasing incidence and complex pathogenesis. With rapid urbanization, changing lifestyles, and dietary habits, it is estimated that this multifaceted syndrome has reached a global prevalence of about 20 to 25% of the adult population [12].
MetS represents a cluster of conditions, including high blood pressure, central obesity, insulin resistance, and atherogenic dyslipidemia, that can occur together and thus significantly increase the patient’s risk of cardiovascular disease by approximately twofold and amplify the probability of developing type 2 diabetes by fivefold [13].
The link between MetS and obstructive lung diseases has gained attention in recent medical research. While some studies emphasized the idea that obesity, a key characteristic of MetS, represents a risk factor for both the onset and the severity of asthma, others delve deeper into the issue, suggesting that changes in hormones originating from adipose tissue, such as leptin and adiponectin, influenced by obesity, might negatively impact the asthmatic profile. Furthermore, hyperinsulinemia in correlation with insulin resistance, another core feature of MetS, might impact the pathogenesis of this condition considering its possible effects of growing airway smooth muscle mass and enhancing contractile function, as observed in the experimental analysis [14,15,16].
In addition, it was found that MetS could influence the progression and outcomes of COPD, highlighting the possibility of shared inflammatory pathways [17,18,19].
Considering all this invaluable data, there is still a recurring emphasis on the imperative need for more comprehensive approaches to facilitate the management of patients dealing with these conditions.
This study aims to determine and evaluate anthropometric and biological parameters utilized to diagnose MetS among patients admitted for obstructive pulmonary diseases. Additionally, a comprehensive analysis of potentially modifiable lifestyle factors was conducted to assess their associated risk regarding the occurrence of metabolic syndrome among patients with COPD or Asthma.
2. Materials and Methods
2.1. Study Design
To establish an appropriate management strategy for patients who present both obstructive bronchial pathology and metabolic syndrome, we conducted a comprehensive cross-sectional, non-interventional clinical study involving patients with chronic obstructive pathology selected from the pneumology clinics of two hospitals.
Hence, we included a total of 70 consecutive patients hospitalized in the pneumology departments of Leamna Clinical Pneumophthisiology Hospital and, respectively, from The Clinical Hospital of Infectious Diseases and Pneumophthisiology “Victor Babeș” from Craiova, between 1 March 2023, and 3 July 2023, in the Oltenia region. The number of participants in the study was calculated using G*Power version 3.1.9.4 [20]. Based on a previous study which indicates a prevalence of metabolic syndrome among the Romanian population of 38.5% [21] and taking into account the Romanian population reported at the last census [22], 66 participants were required, with an effect size of 0.38 at a significance level of 0.05, and a power of 0.90.
Subject participation in the study was voluntary, following the presentation and signing of the informed consent. The present research adhered to the ethical principles outlined in the updated Declaration of Helsinki and received approval from the Ethics Committee of the University of Medicine and Pharmacy in Craiova (No.143/04.07.2023). The patients participated in the study after giving their informed consent voluntarily, without any political, social, or religious discrimination, and in compliance with data protection laws.
The inclusion criteria aimed to enroll patients aged 18 and above, with informed consent for study inclusion, hospitalized for the diagnosis of Chronic Obstructive Pulmonary Disease (COPD) or asthma. Patients were assessed based on specific criteria, with details regarding pulmonary function, and were required to be out of infectious exacerbations and suitable for study participation. The participants enrolled in the study had previously been hospitalized for routine clinical assessments. We included subjects during stable clinical conditions to accurately assess their clinical, paraclinical, and respiratory functional status, avoiding the potential negative impact of infectious exacerbations on lung volumes.
Subjects were allocated into two distinct cohorts based on the presence or absence of meeting the criteria for metabolic syndrome as follows:
Cohort 1: Patients with COPD or asthma who had associated metabolic syndrome.
Cohort 2: Patients with COPD or asthma who did not meet the conditions for the diagnosis of metabolic syndrome.
The updated version of the guideline established by the National Cholesterol Education Program—Adult Treatment Panel III (NCEP-ATP III) was used to define the presence of metabolic syndrome. All measurements were conducted following the specified recommendations. According to this definition, metabolic syndrome is defined by the presence of at least three of the following criteria [23]:
- Abdominal obesity defined by waist circumference:≥102 cm for men;≥88 cm for women.
- Hypertriglyceridemia defined by triglyceride levels:≥150 mg/dL or hypotriglyceridemic medication.
- Low HDL cholesterol:<40 mg/dL for men or medication for reduced HDL cholesterol;<50 mg/dL for women or medication for reduced HDL cholesterol.
- Increased blood pressure (BP):
- -
- systolic BP (SBP) ≥130 mmHg and/or diastolic BP (DBP) ≥85 mmHg or antihypertensive medication.
- Hyperglycemia:
- -
- fasting glucose ≥100 mg/dL or antidiabetic medication.
Exclusion criteria for both cohorts of patients were represented by situations in which the progressive stages of associated conditions did not permit the proposed evaluation. The presence of additional comorbidities that would significantly impact the overall health status of the patients was considered, leading to the exclusion from the study of any patient with severely compromised general health. Considering that all patients underwent respiratory functional assessment, subjects with symptoms or pathologies overlapping absolute or relative contraindications of spirometry were not included. The study prioritized the well-being of the participants, and we made a deliberate decision to exclude individuals with significantly compromised health status resulting from concurrent comorbidities. This exclusion aimed to ensure the robustness of our designated study cohort’s clinical, biological, and respiratory functional data. The rationale behind this decision was rooted in the anticipation that patients with markedly altered clinical statuses might present biological markers strongly influenced by the severity of other severe health conditions. Recognizing spirometry as a demanding test that necessitates respiratory effort, we acknowledged the potential of aggravating underlying conditions or even encountering contraindications for the test in specific cases. Additionally, clinical questionnaires thoroughly assessed all participants’ lifestyle and dietary habits. Thus, inclusion criteria emphasized patient cooperation and the absence of severe neurological impairment. Moreover, anthropometric measurements required a clinical state facilitating unassisted orthostasis—a condition unattainable for those with severely altered statuses.
During the enrollment, participants underwent a comprehensive medical history review, particularly emphasizing cardiovascular, metabolic, and pulmonary elements of interest. Subsequently, anthropometric measurements, including height and weight, were taken. The same personnel consistently conducted these measurements using standardized medical equipment: OMRON Body Composition Monitor BF511 HBF-511T-E/HBF-511B-E (OMRON HEALTHCARE Company; Kyoto, Japan). Blood pressure was determined using a calibrated automatic sphygmomanometer (OMRON X3 Comfort HEM-7155-EO; Omron Company; Kyoto, Japan). The evaluations were conducted following the guidelines provided by the American Heart Association (AHA).
Within the research, venous blood samples of 6 milliliters per patient were collected to assess various essential biological parameters needed for evaluating elements regarding metabolic syndrome. These parameters included fasting blood glucose, triglycerides (TGL), high-density lipoprotein (HDL) cholesterol, and low-density lipoprotein (LDL) cholesterol. The analysis was performed using the BioSystems A15 automatic analyzer (BioSystems Company, Barcelona, Spain).
All enrolled patients underwent respiratory functional assessment through spirometry using Spirolab IV (Medical International Research Company; Roma, Italy). We recorded both the absolute values and the percentage of predicted values for forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) and calculated the FEV1/FVC ratio for each patient.
All patients were asked to respond to three standardized questionnaires (used in evaluation studies of behavioral risk actors and studies published in specialized journals). The first two surveys aimed to evaluate various aspects of lifestyle and eating habits, specifically focusing on the consumption of non-alcoholic beverages and unhealthy food products [24,25,26]. To assess the behavioral risk factors in correlation with the patient’s biochemical parameters, they measured the frequency of consumption of junk food, alcoholic beverages, sweetened beverages, sweets, vegetables, fruits, dairy products, pasta, fish, meat, and eggs, along with physical activity and smoking. The third one included queries designed to assess the impact and severity of symptoms related to pulmonary obstructive diseases, employing the COPD Assessment Test (CAT) and the Modified Medical Research Council (MMrc) Dyspnea Scale [27]. The obstructive ventilatory dysfunction (DVO), the restrictive ventilatory dysfunction (DVR), and the mixed ventilatory dysfunction (DVM) were evaluated.
The Body Mass Index (BMI) was calculated using the formula [body mass (kg)/height (m2)], involving the processing of the anthropometric data [28,29].
The chosen approach for survey registration was an online platform using Google Forms. To ensure the correct recording of responses in accordance with the patient’s order number within the study, a physician was trained to read each question to the included individuals, enumerate response options, repeat them if necessary, and finally, mark the corresponding checkbox with every single answer received.
The initial assessment of patients involved studying them in correlation to a set of general characteristics. Therefore, for each patient group, the distribution of cases based on gender and age distribution was specified.
2.2. Statistical Analysis
The background attributes of the subjects included in the study were outlined using descriptive statistics. For categorical variables, absolute frequencies (n) and relative frequencies (%) were employed for presentation. To discern conceivable relationships between behavioral risk factors (diet, physical activity, tobacco use) and anthropometric data (gender and BMI), a simple correspondence analysis was employed.
The Kolmogorov–Smirnov test was used to assess the normality of the distribution of variables. Spearman’s correlation test was used for variables that did not present normal distribution. In the comparison between two independent groups for variables with n < 30 or without normal distribution, the Mann–Whitney’s test was performed.
To examine the hypothesis of dependence between categorical variables, a Chi-square test was conducted. A receiver operating characteristics (ROC) curve analysis, quantified by the area under the ROC curve (AUC), was used to assess the values of the indicators (age, fasting blood glucose, abdominal circumference, BMI, TGL, and FEV) for predicting MetS. Youden’s index (sensitivity + specificity − 1) was used to determine the optimal cut-off point of each index.
The statistical outcomes regarding the consumption frequency of soft drinks are derived from two-sided tests. During the conclusive phase of the analysis, we investigated the relationship between the variable “Quantity of junk food” and independent variables, including gender and BMI groups. The statistical analysis employed XLSTAT (version 2020, Addinsoft, New York, NY, USA) for Correspondence and the Statistical Package for the Social Sciences, version 23 (SPSS Inc., Chicago, IL, USA). A significance threshold of p < 0.05 was considered for statistical significance [30,31,32].
To ensure the homogeneity and integrity of the clinical database used in the statistical analysis, patients who had contraindications to some clinical evaluations due to severe health conditions were not included in the study. Thus, patients with severe metabolic syndrome and health-altered conditions were excluded from the evaluation group.
3. Results
The average age of the patients in the study was 62.42 ± 10.93. Regarding the abdominal circumference in the persons included in the studied group, an average value of 103.38 ± 15.89 cm was observed. The average abdominal circumference in men was 105.39 ± 15.56, and in women, 99.54 ± 16.12. The statistical analysis showed that out of the total of 70 people included in the study group, 48 of them (68.57%) had at least three metabolic syndrome factors.
At the time of lung function evaluation by spirometry, 63 patients presented ventilatory dysfunction (χ2 = 75.28, p < 0.001). The majority of the patients (80.95%) declared that they were smokers or ex-smokers (χ2 = 5.185, p = 0.075). Most of the patients (Table 1), according to the processing of the anthropometric data, are overweight (22 patients) or obese (23 patients), and in the group of patients with detected metabolic syndrome, patients were predominantly obese and overweight; 23 patients were normal weight from the study group and there were 2 underweight patients (χ2= 16.59, p = 0.006). Most of the patients, i.e., 54 of them, declared that they do not engage in any physical activity at all, and 75% of them presented metabolic syndrome according to the evaluations (χ2 = 2.12, p = 0.713). Among the patients with metabolic syndrome, 45.8% declared that they work in dangerous conditions (χ2 = 6.266, p = 0.394), and 89.6% consider that they eat a balanced diet (χ2 = 4.76, p = 0.092) without excesses, which means that either they do not realize that they are eating excessively or the sedentary lifestyle is the leading cause of excess weight and the consumption of hyper-caloric junk food.

Table 1.
Demographic, anthropometric characteristics, and behavioral factors in correlation with the risk of metabolic syndrome and obstructive pulmonary disease.
A negative correlation between FEV1 and BMI was found (r = 0.310, p = 0.009). FEV1 correlates negatively with SBP (r = −0.234, p = 0.049). Also, in addition to BMI and age, it is a factor that influences the occurrence of metabolic syndrome (r = 0.304, p = 0.017).
The data presented in Table 2 indicate a negative correlation between the consumption of packs of cigarettes per year and lung function: patients with an increased tendency to smoke cigarettes show a greater reduction in FEV1. However, both age and the severity of the metabolic syndrome might accentuate the degradation of lung function. Thus, in the case of patients with a higher number of metabolic syndrome factors, tobacco consumption might affect lung function more compared to those with fewer factors of metabolic syndrome, even if, in some situations, tobacco consumption is higher among those in the latter category.

Table 2.
Cigarette consumption in smokers and the percentage of predicted values for forced expiratory volume in one second (FEV1).
3.1. Metabolic Syndrome Risk Assessment
The correlation between the risk of metabolic syndrome and the results of the evaluation by spirometry, as well as the FEV, are shown in Figure 1:
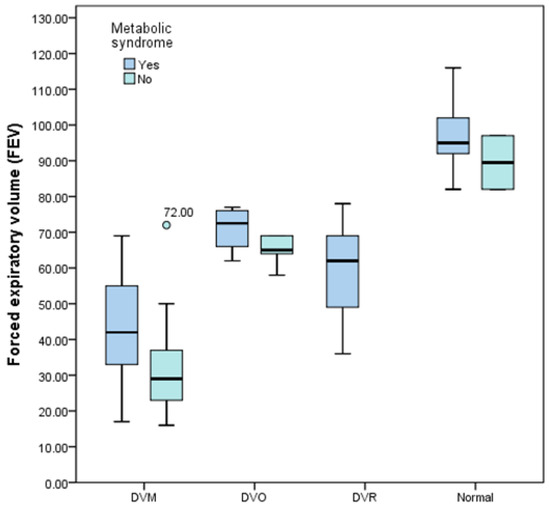
Figure 1.
Box-and-whisker graph of the risk of metabolic syndrome associated with the degree of severity of obstructive pulmonary disease.
- -
- For risk score 0: a total of two patients, a female patient aged 48 and a male patient aged 63. Both patients are of normal weight.
- -
- Spirometry results for SCOR 0 (0 risk criteria fulfilled): moderate DVO for both patients.
- -
- For risk score 1: a total number of five patients, all male, average age 57 years, four normal weight patients, one slightly overweight.
- -
- SCOR 1 spirometry results (1 risk criterion fulfilled): DVO—moderate one patient, moderate-severe DVM one patient, and very severe DVM three patients (60%).
- -
- For risk score 2: a total number of 15 patients, 4 women and 11 men, average age of 57.26 years, 1 underweight patient, 8 normal weight patients, 6 overweight or obese patients.
- -
- Spirometry results for SCOR 2 (2 risk criteria met): normal two patients, DVO—moderate one patient, moderate-severe DVO one patient, mild DVM one patient, severe DVM three patients, and very severe DVM three patients; DVM type (mixed ventilatory dysfunction) predominates in 11 patients, i.e., 73.33%.
- -
- For risk score 3: a total number of 12 patients, 6 women and 6 men, average age of 63.25 years, 1 underweight patient, 7 normal weight patients, 4 obese patients.
- -
- Spirometry results for SCOR 3 (3 risk criteria fulfilled): normal two patients, DVO—moderate one patient, moderate DVM one patient, moderate-severe DVM one patient, severe DVM three patients, very severe DVM three patients, mild DVR one patient; DVM type (mixed ventilatory dysfunction) predominates in eight patients, i.e., 66.66%.
- -
- For risk score 4: a total number of 12 patients, 3 women and 9 men, average age of 63.25 years, 2 normal weight patients, 6 overweight patients and 4 obese patients.
- -
- Spirometry results for SCOR 4 (4 risk criteria fulfilled): normal one patient, DVO—mild one patient, moderate-severe DVM two patients, severe DVM three patients, very severe DVM three patients, moderate DVR one patient, severe DVR one patient; DVM type (mixed ventilatory dysfunction) predominates in eight patients, i.e., 66.66%.
- -
- For risk score 5: a total number of 24 patients, 10 women and 14 men, average age of 66.54 years, 11 overweight patients and 13 obese patients.
- -
- Spirometry results for SCOR 5 (5 risk criteria fulfilled): normal two patients, DVO—mild two patients, DVM moderate two patients, DVM moderate-severe three patients, DVM severe five patients, DVM very severe three patients, DVR mild one patient, DVR moderate three patients, DVR moderate-severe two patients, DVR severe one patient; DVM type (mixed ventilatory dysfunction) predominates in 13 patients, i.e., 54.16%.
3.2. Analysis of Behavioral Risk Factors
Table 3 shows the correlations between the different parameters involved in the onset of the metabolic syndrome. A positive correlation is observed between metabolic syndrome, pulmonary respiratory dysfunction, blood pressure, and the serum level of triglycerides, and a negative correlation between the serum level of HDL-cholesterol, metabolic syndrome, pulmonary respiratory dysfunction, and blood pressure.

Table 3.
Correlation matrix (Spearman’s rank correlation coefficient) between the parameters that influence the risk of metabolic syndrome.
The ROC curve highlighted that age, with a probability of 68.8%, has an important role in the occurrence of metabolic syndrome (Figure 2). The optimal cut-off value of age to detect the metabolic syndrome with maximum sensitivity and specificity was 57 years old, with a positive predictive value (PPV) of 79.5% and a negative predictive value (NPV) of 57.1%. For fasting blood glucose, the optimal cut-off value was 98 (mg/dL), positive predictive value (PPV) 84.3%, and negative predictive value (NPV) 73.6%. For abdominal circumference, the optimal cut-off value was 89 cm, positive predictive value (PPV) 88.8%, and negative predictive value (NPV) 68.0%. For TGL, cut-off value was 105 mg/dL, the positive predictive value (PPV) was 91.8%, and the negative predictive value (NPV) was 57.5%.
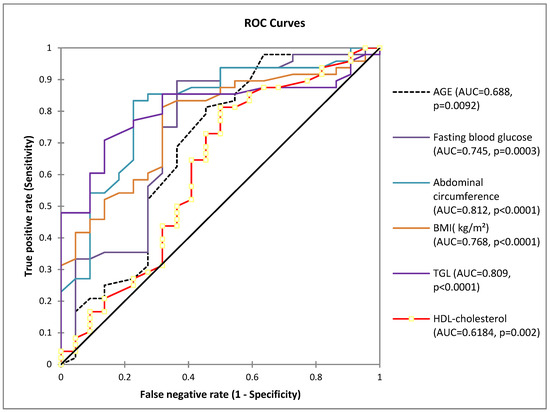
Figure 2.
Receiver operating characteristic curves (ROC) for the parameters involved in the risk of metabolic syndrome (AUC = area under the curve). The diagonal represents the no-effect line (AUC = 0.50).
A strong negative correlation was found between the habit of smoking (smokers or ex-smokers = Former) and the FEV1 value (F = 3.494, p = 0.040), smoking being an important risk factor for obstructive pulmonary disease (Figure 3).
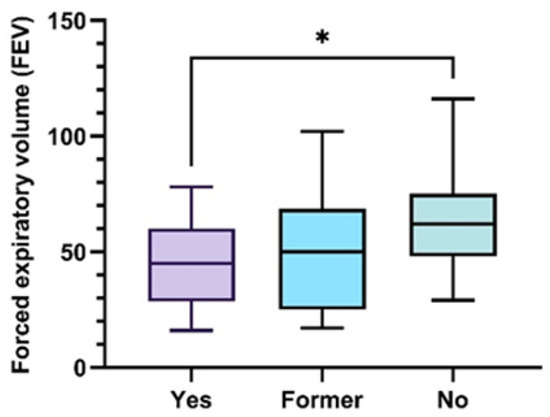
Figure 3.
Box-and-whisker graph of FEV as a function of tobacco consumption 25th and 75th percentiles with median in between (ANOVA, with post hoc Tukey test), * p ˂ 0.05.
The evaluation of the consumption of junk food consumption (sweets, fast food products, fried potatoes, pastries, candies, chewing gum, sweetened carbonated and non-carbonated drinks, and coffee) was carried out by quantifying the number of various products consumed, but also by quantification of consumption frequency (Figure 4). There is a greater tendency to consume hypercaloric processed foods among patients with metabolic syndrome.
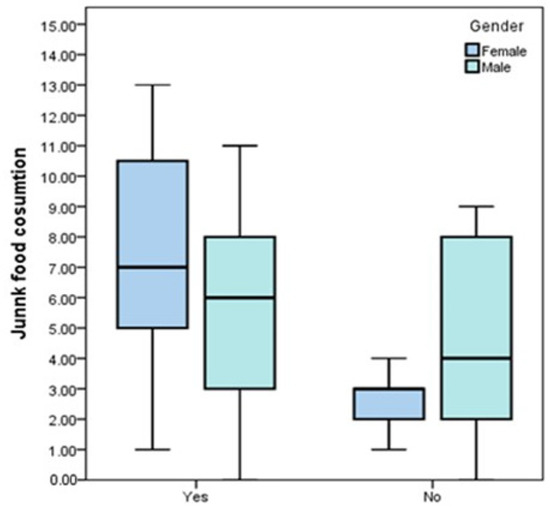
Figure 4.
Box-and-whisker graph of FEV according to the average number of various junk food type products consumed, gender, and the presence of metabolic syndrome.
Exploratory factor analysis was performed to identify underlying dietary patterns using the average portions consumed. Bartlett’s test of sphericity (p = 0.010) supported the appropriateness of factor analysis. D1 (Metabolic syndrome-YES) had high positive loadings on alcohol and carbonated drinks, and negative loading on dairy products. D2 (Metabolic syndrome-NO) was characterized by high positive loadings on fish, eggs, and pasta (Figure 5).
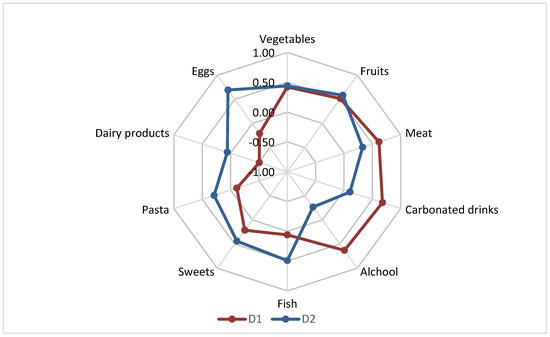
Figure 5.
Factor loadings after varimax rotation on identified dietary patterns. % variance explained: Metabolic syndrome-YES D1: 19.30%; Metabolic syndrome-NO: 16.88. Total variance explained: 36.18%.
Correspondence analysis (CA) was conducted for variables of BMI, gender, spirometry, and the number of met metabolic syndrome conditions.
The bi-plot indicates that 83.78% of the variability observed can be attributed to the two main components for F1 (59.30%) and F2 (24.48%).
Those presenting 5 and 4 criteria are mostly male, generally having a body mass index > 25.00. The higher the number of fulfilled conditions, the lower the mean FEV1 values (Figure 6). As patients meet a greater number of metabolic syndrome conditions, there is a tendency for an increase in BMI and a decrease in FEV1, but also an increase in pulmonary dysfunctions (DVO, DVR, DVM). Patients with a low metabolic syndrome score (0 and 1) have increased FEV1 values, and those with a high metabolic syndrome score (4 and 5) tend to have a more pronounced pulmonary function impairment.
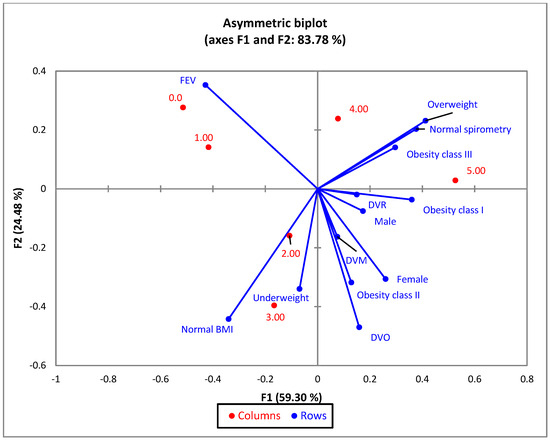
Figure 6.
The first two dimensions of the correspondence analysis (CA) symmetric plot using BMI groups and the results of the spirometry tests as rows, and all 5 metabolic syndrome risk criteria as columns.
The forced expiratory volume in one second (FEV1) decreases as more metabolic syndrome risk criteria are met; the decrease is more pronounced in female patients (Figure 7).
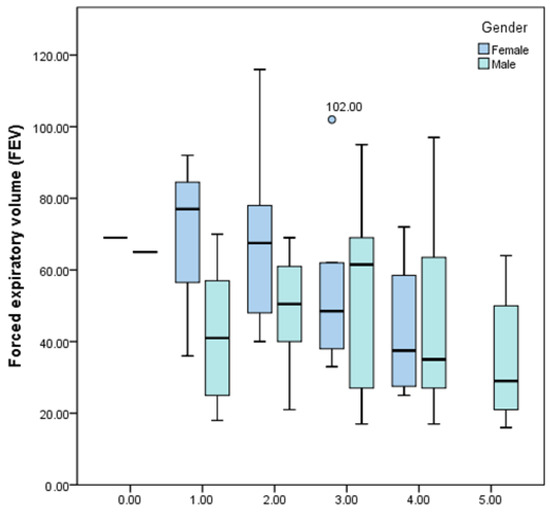
Figure 7.
Box-and-whisker graph of FEV1 depending on the number of met metabolic syndrome risk criteria and gender.
4. Discussion
Among the 70 patients included in the clinical study, 46 are men (65.71%) and 24 are women (34.29%). According to the analysis of metabolic syndrome association criteria, 48 patients meet at least 3 risk criteria, 19 women and 29 men, so a higher prevalence of metabolic syndrome is seen among female patients (79.16%) compared to male patients, where the percentage is 63.04% (Table 1). Men tend to consume a more diverse range of junk food products compared to women; as regards the average number of junk food products consumed, patients with metabolic syndrome consume a narrower range of products compared to those without metabolic syndrome (Figure 4). Regarding the frequency of consumption, men and especially people with metabolic syndrome tend to more frequently consume junk food and ultra-processed and high-calorie products.
People with metabolic syndrome are used to consuming small amounts of vegetable products (maximum 1 or 2 portions of 100 g per day or every 2-3 days) and even dairy products, over 50% consume water up to one liter per day, and they very rarely consume fish; instead, they consume large amounts of meat, carbonated drinks, and alcohol (Figure 5). People without metabolic syndrome consume larger quantities of vegetable products and hydrate better.
According to the statistical correlations in Figure 6, a worsening of obstructive pulmonary disease (accentuation of ventilatory dysfunction) is observed as the severity of the metabolic syndrome increases, and men present a higher risk compared to the women included in the study. There are studies in specialized literature that indicate that obstructive pulmonary disease associated with metabolic syndrome, especially in conditions of increased insulin resistance and obesity, elevated the associated risk of morbidity and mortality, especially due to cardiovascular complications [33,34,35]. A meta-analysis encompassing eleven studies concluded that, excluding the effects of hypolipidemic interventions on the serum lipid profile, patients with COPD had higher triglyceride levels than subjects without this condition [36]. Increased levels of serum triglycerides were also linked to the occurrence of asthma in individuals with obesity, suggesting that elevated triglycerides could represent a potential characteristic contributing to the onset of asthma [37,38].
Smoking, genetic factors, physical inactivity, and unhealthy diet are also incriminated as aggravating factors [39,40].
Pulmonary function is affected by the severity of the associated metabolic syndrome, and also by behavioral risk factors, as shown in this clinical study. Some studies indicate an alteration of the spirometry parameters with the severity of the metabolic syndrome, especially when the patients also have significant cardiovascular diseases [41,42,43,44]. Several epidemiological investigations revealed an association between low levels of serum high-density lipoprotein cholesterol (HDL-C) and the occurrence of wheezing [45,46]. Multiple studies observed that abdominal obesity had a notable negative impact on respiratory functions [47,48]. Additional findings show that an increase in abdominal obesity markedly lowers the asthma control score [49,50]. Specialists draw attention to the need to balance patients with comorbidities through diet and adequate rest [47,48]. Similar negative correlations have been observed in patients with COPD. Several studies indicated that abdominal obesity is associated with increased comorbidities and poorer therapeutical outcomes [51,52]. Along with the hyper-caloric diet rich in saturated fats, the specialized literature indicates two more important behavioral risk factors involved in the deterioration of lung function: sedentary lifestyle and smoking [53,54,55,56,57].
The limitations of the study are determined by the advanced age of the patients, the lower presence of female patients, and the uneven distribution of the patients on different degrees of risk in relation to the metabolic syndrome. Also, accurate quantification of cigarette packs smoked by patients was difficult to achieve. Through extensive discussions with the participants, especially active smokers, we observed difficulties in accurately quantifying the number of cigarettes smoked daily and providing precise data on the years of smoking. Many participants recounted various attempts of cessation, undergoing multiple stages in their smoking habits throughout the course of the disease. Factors such as worsening clinical status during exacerbations, financial constraints, motivation derived from participation in educational programs, or fear of developing bronchopulmonary neoplasms following the diagnosis of similar cases in acquaintances contribute to periods of tobacco cessation. On the other hand, many patients reported that during certain periods of emotional stress, or conversely, during leisure and relaxation, when they had the opportunity to spend more time with friends, there was a discernible escalation in their smoking habits. Another notable limitation of this study is excluding patients with severely compromised clinical status. This decision was made to preserve the integrity of the evaluation process at each stage of the study. The practical aspects of patient participation, including the need for ortho-stasis during anthropometric measurements, patient cooperation in answering lifestyle assessment questionnaires, and the demanding nature of spirometry with multiple contraindications, influenced this exclusion. The study’s cross-sectional design inherently limits our ability to infer causality, as it disallows establishing temporal precedence and determining a clear cause-and-effect relationship between metabolic syndrome and chronic obstructive airway diseases. While associations are discerned, the direction of influence remains uncertain. Future longitudinal investigations are needed to unravel the nuanced dynamics between the pathological entities mentioned before offering a more comprehensive understanding of their interrelationship. The observations can only be indicative and important to formulating a series of recommendations related to nutrition and lifestyle in order to improve the patient’s quality of life.
The importance of the study lies in the significant correlations highlighted between certain behavioral risk factors and the severity of metabolic syndrome as well as pulmonary dysfunctions. Thus, increased consumption of hyper-caloric ultra-processed foods, reduced consumption of vegetable products, smoking, and a sedentary lifestyle are the main factors that can aggravate obstructive pulmonary diseases associated with metabolic syndrome. Also, the severity of the metabolic syndrome, especially the increase in excess weight and serum lipids, significantly affects lung function.
5. Conclusions
Obstructive pulmonary disease is a condition that can endanger the patient’s life if risk factors with an aggravating effect are not effectively monitored. The clinical study carried out on patients with pulmonary function impairment highlighted that metabolic syndrome is an aggravating factor, which, as it becomes more intense, progressively affects pulmonary function in a negative sense. Behavioral risk factors can also play an important role in the deterioration of lung function; smoking, alcohol consumption, and consumption of ultra-processed and hyper-caloric foods increase the risk of metabolic syndrome and worsening respiratory dysfunction.
An unhealthy lifestyle and an unbalanced diet produce, in the long term, a series of imbalances in the body that worsen over time and trigger a series of pathologies with a risk of premature death. One of the most frequent consequences is represented by metabolic syndrome, which, as it worsens, generates a series of associated pathologies that significantly affect the quality of life and even its duration.
Author Contributions
Conceptualization, A.M., E.C.L. and L.S.; methodology, R.C., C.C. and C.T.S.; software, I.M.V., M.L.I. and Ș.S.B.; validation, R.C., C.C. and C.T.S.; formal analysis, M.M. (Magdalena Mititelu) and M.M. (Marius Matei); investigation, A.M., E.C.L. and L.S.; resources, I.M.V.; data curation, M.M. (Magdalena Mititelu) and M.M. (Marius Matei); writing—original draft preparation, M.M. (Magdalena Mititelu) and M.M. (Marius Matei); writing—review and editing, M.M. (Magdalena Mititelu) and M.M. (Marius Matei); visualization, Ș.S.B.; supervision, C.T.S.; project administration, A.M., E.C.L. and L.S.; funding acquisition, M.L.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University of Medicine and Pharmacy in Craiova (No.143/04.07.2023) for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Acknowledgments
This research received technical support from the grant no. 3126/2022, University of Medicine and Pharmacy of Craiova (“Prediction model for the management of patients with pulmonary disease and metabolic syndrome”).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Cukic, V.; Lovre, V.; Dragisic, D.; Ustamujic, A. Asthma and Chronic Obstructive Pulmonary Disease (COPD)—Differences and Similarities. Mater. Sociomed. 2012, 24, 100–105. [Google Scholar] [CrossRef] [PubMed]
- May, S.M.; Li, J.T. Burden of chronic obstructive pulmonary disease: Healthcare costs and beyond. Allergy Asthma Proc. 2015, 36, 4–10. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Chronic Obstructive Pulmonary Disease (COPD). 16 March 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd) (accessed on 7 December 2023).
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for Prevention, Diagnosis and Management of COPD: 2023 Report. Available online: https://goldcopd.org/2023-gold-report-2/ (accessed on 7 December 2023).
- Wang, Z.; Li, Y.; Lin, J.; Huang, J.; Zhang, Q.; Wang, F.; Tan, L.; Liu, S.; Gao, Y.; Peng, S.; et al. Prevalence, risk factors, and mortality of COPD in young people in the USA: Results from a population-based retrospective cohort. BMJ Open Respir. Res. 2023, 10, e001550. [Google Scholar] [CrossRef]
- World Health Organization. Asthma. 4 May 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/asthma (accessed on 7 December 2023).
- Castillo, J.R.; Peters, S.P.; Busse, W.W. Asthma Exacerbations: Pathogenesis, Prevention, and Treatment. J. Allergy Clin. Immunol. Pract. 2017, 5, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Mortimer, K.; Reddel, H.K.; Pitrez, P.M.; Bateman, E.D. Asthma management in low and middle income countries: Case for change. Eur. Respir. J. 2022, 60, 2103179. [Google Scholar] [CrossRef] [PubMed]
- Cazzola, M.; Rogliani, P.; Ora, J.; Calzetta, L.; Matera, M.G. Asthma and comorbidities: Recent advances. Pol. Arch. Intern. Med. 2022, 132, 16250. [Google Scholar] [CrossRef]
- Burke, H.; Wilkinson, T.M.A. Unravelling the mechanisms driving multimorbidity in COPD to develop holistic approaches to patient-centred care. Eur. Respir. Rev. 2021, 30, 210041. [Google Scholar] [CrossRef]
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2023 GINA Main Report. Available online: https://ginasthma.org/2023-gina-main-report/ (accessed on 7 December 2023).
- Ranasinghe, P.; Mathangasinghe, Y.; Jayawardena, R.; Hills, A.P.; Misra, A. Prevalence and trends of metabolic syndrome among adults in the asia-pacific region: A systematic review. BMC Public Health 2017, 17, 101. [Google Scholar] [CrossRef]
- Cornier, M.A.; Dabelea, D.; Hernandez, T.L.; Lindstrom, R.C.; Steig, A.J.; Stob, N.R.; Van Pelt, R.E.; Wang, H.; Eckel, R.H. The metabolic syndrome. Endocr. Rev. 2008, 29, 777–822. [Google Scholar] [CrossRef]
- Peters, U.; Dixon, A.E.; Forno, E. Obesity and asthma. J. Allergy Clin. Immunol. 2018, 141, 1169–1179. [Google Scholar] [CrossRef]
- Shore, S.A. Obesity and asthma: Possible mechanisms. J. Allergy Clin. Immunol. 2008, 121, 1087–1093. [Google Scholar] [CrossRef]
- Wu, T.D. Diabetes, insulin resistance, and asthma: A review of potential links. Curr. Opin. Pulm. Med. 2021, 27, 29–36. [Google Scholar] [CrossRef]
- Naik, D.; Joshi, A.; Paul, T.V.; Thomas, N. Chronic obstructive pulmonary disease and the metabolic syndrome: Consequences of a dual threat. Indian J. Endocrinol. Metab. 2014, 18, 608–616. [Google Scholar]
- Ioniță-Mîndrican, C.-B.; Mititelu, M.; Musuc, A.M.; Oprea, E.; Ziani, K.; Neacșu, S.M.; Grigore, N.D.; Negrei, C.; Dumitrescu, D.-E.; Mireșan, H.; et al. Honey and Other Beekeeping Products Intake among the Romanian Population and Their Thera-peutic Use. Appl. Sci. 2022, 12, 9649. [Google Scholar] [CrossRef]
- Matran, I.M.; Martin-Hadmaș, R.M.; Niculaș, C.; Muntean, D.L.; Tarcea, M. Dietary and pharmaco-therapy in skin diseases. Farmacia 2022, 70, 177–183. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Popa, S.; Moţa, M.; Popa, A.; Moţa, E.; Serafinceanu, C.; Guja, C.; Catrinoiu, D.; Hâncu, N.; Lichiardopol, R.; Bala, C.; et al. Prevalence of overweight/obesity, abdominal obesity and metabolic syndrome and atypical cardiometabolic phenotypes in the adult Romanian population: PREDATORR study. J. Endocrinol. Investig. 2016, 39, 1045–1053. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.recensamantromania.ro/rezultate-rpl-2021/rezultate-definitive/ (accessed on 11 November 2023).
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; SmithJr, S.C.; et al. Diagnosis and Management of the Metabolic Syndrome, An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement: Executive Summary. Circulation 2005, 112, e285–e290. [Google Scholar]
- Mititelu, M.; Oancea, C.-N.; Neacșu, S.M.; Musuc, A.M.; Gheonea, T.C.; Stanciu, T.I.; Rogoveanu, I.; Hashemi, F.; Stanciu, G.; Ioniță-Mîndrican, C.-B.; et al. Evaluation of Junk Food Consumption and the Risk Related to Consumer Health among the Romanian Population. Nutrients 2023, 15, 3591. [Google Scholar] [CrossRef] [PubMed]
- Mititelu, M.; Oancea, C.-N.; Neacșu, S.M.; Olteanu, G.; Cîrțu, A.-T.; Hîncu, L.; Gheonea, T.C.; Stanciu, T.I.; Rogoveanu, I.; Hashemi, F.; et al. Evaluation of Non-Alcoholic Beverages and the Risk Related to Consumer Health among the Romanian Population. Nutrients 2023, 15, 3841. [Google Scholar] [CrossRef] [PubMed]
- Năstăsescu, V.; Mititelu, M.; Stanciu, T.I.; Drăgănescu, D.; Grigore, N.D.; Udeanu, D.I.; Stanciu, G.; Neacșu, S.M.; Dinu-Pîrvu, C.E.; Oprea, E. Food Habits and Lifestyle of Romanians in the Context of the COVID-19 Pandemic. Nutrients 2022, 14, 504. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.catestonline.org/hcp-homepage.html (accessed on 7 December 2023).
- Branca, F.; Nikogosian, H.; Lobstein, T.; World Health Organization; Regional Office for Europe. The Challenge of Obesity in the WHO European Region and the Strategies for Response; WHO Regional Office for Europe: Copenhagen, Denmark, 2007. [Google Scholar]
- Ashwell, M.; Gibson, S. Waist-to-height ratio as an indicator of early health risk: Simpler and more predictive than using a matrix based on BMI and waist circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef] [PubMed]
- Ionus, E.; Bucur, L.A.; Lupu, C.E.; Gird, C.E. Evaluation of the chemical composition of Ajuga chamaepitys (L.) schreb. From the spontaneous flora of Romania. Farmacia 2021, 69, 461–466. [Google Scholar] [CrossRef]
- Leahu, A.; Lupu, E.C. Statistical simulation and prediction in software reliability. Analele Univ. Ovidius Constanta Ser. Mat. 2008, 16, 81–90. [Google Scholar]
- Mititelu, M.; Neacsu, S.M.; Oprea, E.; Dumitrescu, D.-E.; Nedelescu, M.; Drăgănescu, D.; Nicolescu, T.O.; Rosca, A.C.; Ghica, M. Black Sea Mussels Qualitative and Quantitative Chemical Analysis: Nutritional Benefits and Possible Risks through Consumption. Nutrients 2022, 14, 964. [Google Scholar] [CrossRef]
- Katsiki, N.; Stoian, A.P.; Steiropoulos, P.; Papanas, N.; Suceveanu, A.-I.; Mikhailidis, D.P. Metabolic Syndrome and Abnormal Peri-Organ or Intra-Organ Fat (APIFat) Deposition in Chronic Obstructive Pulmonary Disease: An Overview. Metabolites 2020, 10, 465. [Google Scholar] [CrossRef]
- Cebron Lipovec, N.; Beijers, R.J.; van den Borst, B.; Doehner, W.; Lainscak, M.; Schols, A.M. The prevalence of metabolic syndrome in chronic obstructive pulmonary disease: A systematic review. COPD 2016, 13, 399–406. [Google Scholar] [CrossRef]
- Dave, L.; Garde, S.; Ansari, O.A.; Shrivastava, N.; Sharma, V.K. A study of association between metabolic syndrome and COPD. J. Evol. Med. Dent. Sci. 2014, 3, 6183–6188. [Google Scholar] [CrossRef]
- Xuan, L.; Han, F.; Gong, L.; Lv, Y.; Wan, Z.; Liu, H.; Zhang, D.; Jia, Y.; Yang, S.; Ren, L.; et al. Association between chronic obstructive pulmonary disease and serum lipid levels: A meta-analysis. Lipids Health Dis. 2018, 17, 263. [Google Scholar] [CrossRef] [PubMed]
- van Zelst, C.M.; de Boer, G.M.; Türk, Y.; van Huisstede, A.; In’t Veen, J.C.C.M.; Birnie, E.; Boxma-de Klerk, B.M.; Tramper-Stranders, G.A.; Braunstahl, G.J. Association between elevated serum triglycerides and asthma in patients with obesity: An explorative study. Allergy Asthma Proc. 2021, 42, e71–e76. [Google Scholar] [CrossRef] [PubMed]
- van Zelst, C.; De Boer, G.; Tramper, G.; Braunstahl, G.-J. Relations between serum lipid levels and inflammatory markers in obese asthma. Eur. Respir. J. 2018, 52, PA663. [Google Scholar] [CrossRef]
- Koul, P.A. Metabolic syndrome and chronic obstructive pulmonary disease. Lung India 2016, 33, 359–361. [Google Scholar] [CrossRef]
- Mannino, D.M.; Thorn, D.; Swensen, A.; Holguin, F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur. Respir. J. 2008, 32, 962–969. [Google Scholar] [CrossRef] [PubMed]
- Molina-Luque, R.; Molina-Recio, G.; de-Pedro-Jiménez, D.; Álvarez Fernández, C.; García-Rodríguez, M.; Romero-Saldaña, M. The Impact of Metabolic Syndrome Risk Factors on Lung Function Impairment: Cross-Sectional Study. JMIR Public Health Surveill. 2023, 9, e43737. [Google Scholar] [CrossRef]
- Ramalho, S.H.; Shah, A.M. Lung function and cardiovascular disease: A link. Trends Cardiovasc. Med. 2021, 31, 93–98. [Google Scholar] [CrossRef] [PubMed]
- McNeill, J.N.; Lau, E.S.; Zern, E.K.; Nayor, M.; Malhotra, R.; Liu, E.E.; Bhat, R.R.; Brooks, L.C.; Farrell, R.; Sbarbaro, J.A.; et al. Association of obesity-related inflammatory pathways with lung function and exercise capacity. Respir Med. 2021, 183, 106434. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.Y.; Tsao, Y.C.; Yang, C.K.; Chuang, C.H.; Yu, W.; Chen, J.C.; Li, W.C. Association between risk factors of metabolic syndrome with lung function. Eur. J. Clin. Nutr. 2020, 74, 811–817. [Google Scholar] [CrossRef]
- Fenger, R.V.; Gonzalez-Quintela, A.; Linneberg, A.; Husemoen, L.L.; Thuesen, B.H.; Aadahl, M.; Vidal, C.; Skaaby, T.; Sainz, J.C.; Calvo, E. The relationship of serum triglycerides, serum HDL, and obesity to the risk of wheezing in 85,555 adults. Respir. Med. 2013, 107, 816–824. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, H.; Park, Y.; Chung, S.J.; Yeo, Y.; Park, T.S.; Park, D.W.; Kim, S.H.; Kim, T.H.; Sohn, J.W.; et al. Additive Effect of Obesity and Dyslipidemia on Wheezing in Korean Adults: A Nationwide Representative Survey Study. Allergy Asthma Immunol. Res. 2021, 13, 808–816. [Google Scholar] [CrossRef]
- Capelo, A.V.; de Fonseca, V.M.; Peixoto, M.V.M.; de Carvalho, S.R.; Guerino, L.G. Central obesity and other factors associated with uncontrolled asthma in women. Allergy Asthma Clin. Immunol. 2015, 11, 12. [Google Scholar] [CrossRef]
- Choe, E.K.; Kang, H.Y.; Lee, Y.; Choi, S.H.; Kim, H.J.; Kim, J.S. The longitudinal association between changes in lung function and changes in abdominal visceral obesity in Korean non-smokers. PLoS ONE 2018, 13, e0193516. [Google Scholar] [CrossRef] [PubMed]
- Lv, N.; Xiao, L.; Camargo, C.A.; Wilson, S.R.; Buist, A.S.; Strub, P.; Nadeau, K.C.; Ma, J. Abdominal and general adiposity and level of asthma control in adults with uncontrolled asthma. Ann. Am. Thorac. Soc. 2014, 11, 1218–1224. [Google Scholar] [CrossRef] [PubMed]
- Yücel, Ü.Ö.; Çalış, A.G. The relationship between general and abdominal obesity, nutrition and respiratory functions in adult asthmatics. J. Asthma 2023, 60, 1183–1190. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.; Almeras, N.; Després, J.P.; Coxson, H.O.; Washko, G.R.; Vivodtzev, I.; Wouters, E.F.; Rutten, E.; Williams, M.C.; Murchison, J.T.; et al. Ectopic fat accumulation in patients with COPD: An ECLIPSE substudy. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 451–460. [Google Scholar] [CrossRef] [PubMed]
- Inomoto, A.; Fukuda, R.; Deguchi, J.; Kato, G.; Kanzaki, R.; Hiroshige, K.; Nakamura, K.; Nakano, K.; Toyonaga, T. The association between the body composition and lifestyle affecting pulmonary function in Japanese workers. J. Phys. Ther. Sci. 2016, 28, 2883–2889. [Google Scholar] [CrossRef][Green Version]
- Ford, E.S.; Cunningham, T.J.; Mercado, C.I. Lung function and metabolic syndrome: Findings of national health and nutrition examination survey 2007–2010. J. Diabetes 2014, 6, 603–613. [Google Scholar] [CrossRef]
- Campbell Jenkins, B.W.; Sarpong, D.F.; Addison, C.; White, M.S.; Hickson, D.A.; White, W.; Burchfiel, C. Joint effects of smoking and sedentary lifestyle on lung function in African Americans: The Jackson Heart Study cohort. Int. J. Environ. Res. Public Health 2014, 11, 1500–1519. [Google Scholar] [CrossRef]
- Lim, S.Y.; Zhao, D.; Guallar, E.; Chang, Y.; Ryu, S.; Cho, J.; Shim, J.Y. Risk of chronic obstructive pulmonary disease in healthy individuals with high C-reactive protein levels by smoking status: A population-based cohort study in Korea. Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 2037–2046. [Google Scholar] [CrossRef]
- Lei, Y.; Zou, K.; Xin, J.; Wang, Z.; Liang, K.; Zhao, L.; Ma, X. Sedentary behavior is associated with chronic obstructive pulmonary disease: A generalized propensity score-weighted analysis. Medicine 2021, 100, e25336. [Google Scholar] [CrossRef]
- Mesquita, R.; Meijer, K.; Pitta, F.; Azcuna, H.; Goërtz, Y.M.J.; Essers, J.M.N.; Wouters, E.F.M.; Spruit, M.A. Changes in physical activity and sedentary behaviour following pulmonary rehabilitation in patients with COPD. Respir. Med. 2017, 126, 122–129. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).