Investigating the Association of Assisted Reproduction Techniques and Adverse Perinatal Outcomes
Abstract
1. Introduction
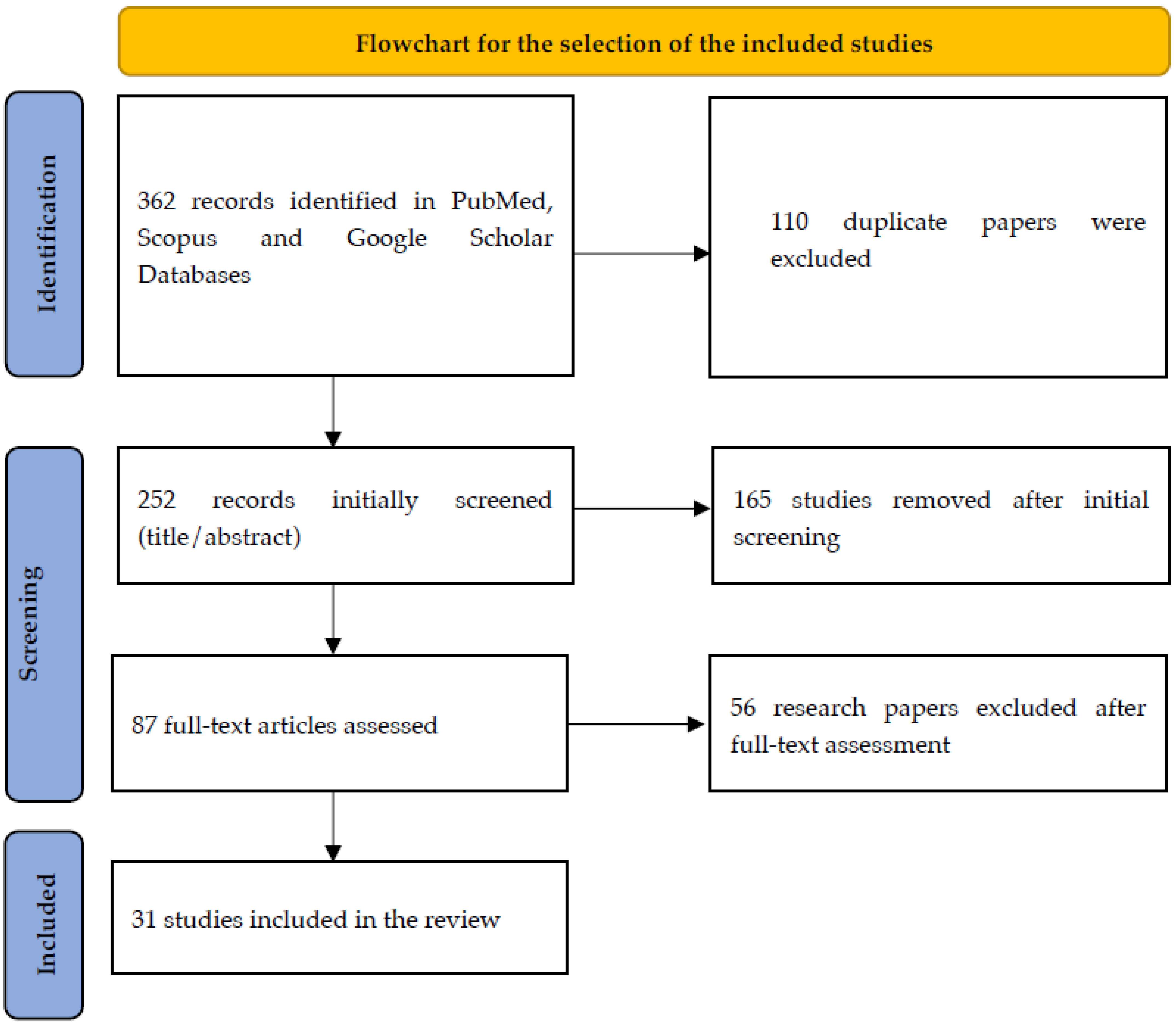
2. Materials and Methods
3. Results
3.1. Pre-Term Birth and Birthweight
3.2. Congenital and Chromosomal Defects
3.3. Hypospadias—Male Genital Anomalies
3.4. Heart and Metabolic Defects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luke, B. Pregnancy and birth outcomes in couples with infertility with and without assisted reproductive technology: With an emphasis on US population-based studies. Am. J. Obstet. Gynecol. 2017, 217, 270–281. [Google Scholar] [CrossRef] [PubMed]
- Kupka, M.S.; Ferraretti, A.P.; de Mouzon, J.; Erb, K.; D’Hooghe, T.; Castilla, J.A.; Calhaz-Jorge, C.; De Geyter, C.; Goossens, V.; Strohmer, H.; et al. Assisted reproductive technology in Europe, 2010: Results generated from European registers by ESHREdagger. Hum. Reprod. 2014, 29, 2099–2113. [Google Scholar] [CrossRef] [PubMed]
- Banker, M.; Dyer, S.; Chambers, G.M.; Ishihara, O.; Kupka, M.; de Mouzon, J.; Zegers-Hochschild, F.; Adamson, G.D. International Committee for Monitoring Assisted Reproductive Technologies (ICMART): World report on assisted reproductive technologies, 2013. Fertil. Steril. 2021, 116, 741–756. [Google Scholar] [CrossRef] [PubMed]
- Nyboe Andersen, A.; Erb, K. Register data on Assisted Reproductive Technology (ART) in Europe including a detailed description of ART in Denmark. Int. J. Androl. 2006, 29, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Pandey, S.; Shetty, A.; Hamilton, M.; Bhattacharya, S.; Maheshwari, A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: A systematic review and meta-analysis. Hum. Reprod. Update 2012, 18, 485–503. [Google Scholar] [CrossRef] [PubMed]
- Fauser, B.C.; Devroey, P.; Diedrich, K.; Balaban, B.; Bonduelle, M.; Delemarre-van de Waal, H.A.; Estella, C.; Ezcurra, D.; Geraedts, J.P.; Howles, C.M.; et al. Health outcomes of children born after IVF/ICSI: A review of current expert opinion and literature. Reprod. Biomed. Online 2014, 28, 162–182. [Google Scholar] [CrossRef] [PubMed]
- Glasser, S.; Segev-Zahav, A.; Fortinsky, P.; Gedal-Beer, D.; Schiff, E.; Lerner-Geva, L. Primiparity at very advanced maternal age (>/= 45 years). Fertil. Steril. 2011, 95, 2548–2551. [Google Scholar] [CrossRef] [PubMed]
- Chambers, G.M.; Ledger, W. The economic implications of multiple pregnancy following ART. Semin. Fetal Neonatal Med. 2014, 19, 254–261. [Google Scholar] [CrossRef]
- Senat, M.V.; Ancel, P.Y.; Bouvier-Colle, M.H.; Breart, G. How does multiple pregnancy affect maternal mortality and morbidity? Clin. Obstet. Gynecol. 1998, 41, 78–83. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Kamath, M.S. Reducing multiple births in assisted reproduction technology. Best. Pract. Res. Clin. Obstet. Gynaecol. 2014, 28, 191–199. [Google Scholar] [CrossRef]
- Pinborg, A.; Wennerholm, U.B.; Romundstad, L.B.; Loft, A.; Aittomaki, K.; Soderstrom-Anttila, V.; Nygren, K.G.; Hazekamp, J.; Bergh, C. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum. Reprod. Update 2013, 19, 87–104. [Google Scholar] [CrossRef] [PubMed]
- Di Tommaso, M.; Sisti, G.; Colombi, I.; Seravalli, V.; Magro Malosso, E.R.; Vannuccini, S.; Petraglia, F. Influence of assisted reproductive technologies on maternal and neonatal outcomes in early preterm deliveries. J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 845–848. [Google Scholar] [CrossRef] [PubMed]
- Simpson, J.L.; Lamb, D.J. Genetic effects of intracytoplasmic sperm injection. Semin. Reprod. Med. 2001, 19, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Marconi, N.; Raja, E.A.; Bhattacharya, S.; Maheshwari, A. Perinatal outcomes in singleton live births after fresh blastocyst-stage embryo transfer: A retrospective analysis of 67 147 IVF/ICSI cycles. Hum. Reprod. 2019, 34, 1716–1725. [Google Scholar] [CrossRef] [PubMed]
- Sunkara, S.K.; LaMarca, A.; Polyzos, N.P.; Seed, P.T.; Khalaf, Y. Live birth and perinatal outcomes following stimulated and unstimulated IVF: Analysis of over two decades of a nationwide data. Hum. Reprod. 2016, 31, 2261–2267. [Google Scholar] [CrossRef] [PubMed]
- Sunkara, S.K.; Antonisamy, B.; Selliah, H.Y.; Kamath, M.S. Pre-term birth and low birth weight following preimplantation genetic diagnosis: Analysis of 88 010 singleton live births following PGD and IVF cycles. Hum. Reprod. 2017, 32, 432–438. [Google Scholar] [CrossRef]
- Premru-Srsen, T.; Bokal Vrtacnik, E.; Bizjak, T.; Verdenik, I.; Korosec, S.; Ban Frangez, H. Preterm delivery risk in infertile women who conceived after reproductive surgery: Natural conception versus IVF/ICSI. Hum. Reprod. 2021, 36, 1630–1639. [Google Scholar] [CrossRef]
- Scherrer, U.; Rimoldi, S.F.; Rexhaj, E.; Stuber, T.; Duplain, H.; Garcin, S.; de Marchi, S.F.; Nicod, P.; Germond, M.; Allemann, Y.; et al. Systemic and pulmonary vascular dysfunction in children conceived by assisted reproductive technologies. Circulation 2012, 125, 1890–1896. [Google Scholar] [CrossRef]
- Szymusik, I.; Kosinska-Kaczynska, K.; Krowicka, M.; Sep, M.; Marianowski, P.; Wielgos, M. Perinatal outcome of in vitro fertilization singletons—10 years’ experience of one center. Arch. Med. Sci. 2019, 15, 666–672. [Google Scholar] [CrossRef]
- Kaveh, M.; Ghajarzadeh, M.; Davari Tanha, F.; Nayeri, F.; Keramati, Z.; Shariat, M.; Ghaheri, A. Pregnancy Complications and Neonatal Outcomes in Multiple Pregnancies: A Comparison between Assisted Reproductive Techniques and Spontaneous Conception. Int. J. Fertil. Steril. 2015, 8, 367–372. [Google Scholar] [CrossRef]
- Al-Fifi, S.; Al-Binali, A.; Al-Shahrani, M.; Shafiq, H.; Bahar, M.; Almushait, M.; Sobandi, L.; Eskandar, M. Congenital anomalies and other perinatal outcomes in ICSI vs. naturally conceived pregnancies: A comparative study. J. Assist. Reprod. Genet. 2009, 26, 377–381. [Google Scholar] [CrossRef]
- Kamath, M.S.; Antonisamy, B.; Mascarenhas, M.; Sunkara, S.K. High-risk of preterm birth and low birth weight after oocyte donation IVF: Analysis of 133,785 live births. Reprod. Biomed. Online 2017, 35, 318–324. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sunkara, S.K.; La Marca, A.; Seed, P.T.; Khalaf, Y. Increased risk of preterm birth and low birthweight with very high number of oocytes following IVF: An analysis of 65 868 singleton live birth outcomes. Hum. Reprod. 2015, 30, 1473–1480. [Google Scholar] [CrossRef]
- Yuan, S.; Guo, L.; Cheng, D.; Li, X.; Hu, H.; Hu, L.; Lu, G.; Lin, G.; Gong, F.; Tan, Y.Q. The de novo aberration rate of prenatal karyotype was comparable between 1496 fetuses conceived via IVF/ICSI and 1396 fetuses from natural conception. J. Assist. Reprod. Genet. 2022, 39, 1683–1689. [Google Scholar] [CrossRef] [PubMed]
- Olson, C.K.; Keppler-Noreuil, K.M.; Romitti, P.A.; Budelier, W.T.; Ryan, G.; Sparks, A.E.; Van Voorhis, B.J. In vitro fertilization is associated with an increase in major birth defects. Fertil. Steril. 2005, 84, 1308–1315. [Google Scholar] [CrossRef] [PubMed]
- Luke, B.; Brown, M.B.; Wantman, E.; Schymura, M.J.; Browne, M.L.; Fisher, S.C.; Forestieri, N.E.; Rao, C.; Nichols, H.B.; Yazdy, M.M.; et al. The risks of birth defects and childhood cancer with conception by assisted reproductive technology. Hum. Reprod. 2022, 37, 2672–2689. [Google Scholar] [CrossRef] [PubMed]
- Fauque, P.; De Mouzon, J.; Devaux, A.; Epelboin, S.; Gervoise-Boyer, M.J.; Levy, R.; Valentin, M.; Viot, G.; Bergere, M.; De Vienne, C.; et al. Do in vitro fertilization, intrauterine insemination or female infertility impact the risk of congenital anomalies in singletons? A longitudinal national French study. Hum. Reprod. 2021, 36, 808–816. [Google Scholar] [CrossRef] [PubMed]
- Belva, F.; Bonduelle, M.; Buysse, A.; Van den Bogaert, A.; Hes, F.; Roelants, M.; Verheyen, G.; Tournaye, H.; Keymolen, K. Chromosomal abnormalities after ICSI in relation to semen parameters: Results in 1114 fetuses and 1391 neonates from a single center. Hum. Reprod. 2020, 35, 2149–2162. [Google Scholar] [CrossRef]
- Jozwiak, E.A.; Ulug, U.; Mesut, A.; Erden, H.F.; Bahceci, M. Prenatal karyotypes of fetuses conceived by intracytoplasmic sperm injection. Fertil. Steril. 2004, 82, 628–633. [Google Scholar] [CrossRef]
- Samli, H.; Solak, M.; Imirzalioglu, N.; Beyatli, Y.; Simsek, S.; Kahraman, S. Fetal chromosomal analysis of pregnancies following intracytoplasmic sperm injection with amniotic tissue culture. Prenat. Diagn. 2003, 23, 847–850. [Google Scholar] [CrossRef]
- Akay, M.A.; Yildiz, G.E. Impact of gestational and parental factors and maternal intake of progesterone on the development of hypospadias: A retrospective case-control study. Taiwan. J. Obstet. Gynecol. 2021, 60, 894–898. [Google Scholar] [CrossRef] [PubMed]
- Silver, R.I.; Rodriguez, R.; Chang, T.S.; Gearhart, J.P. In vitro fertilization is associated with an increased risk of hypospadias. J. Urol. 1999, 161, 1954–1957. [Google Scholar] [CrossRef]
- Funke, S.; Flach, E.; Kiss, I.; Sandor, J.; Vida, G.; Bodis, J.; Ertl, T. Male reproductive tract abnormalities: More common after assisted reproduction? Early Hum. Dev. 2010, 86, 547–550. [Google Scholar] [CrossRef] [PubMed]
- Bang, J.K.; Lyu, S.W.; Choi, J.; Lee, D.R.; Yoon, T.K.; Song, S.H. Does infertility treatment increase male reproductive tract disorder? Urology 2013, 81, 644–648. [Google Scholar] [CrossRef] [PubMed]
- Aliani, F.; Haghshenas, Z.; Vosough Dizaj, A.; Arabipoor, A.; Vesali, S.; Ashrafi, M. Birth prevalence of genital anomalies among males conceived by intracytoplasmic sperm injection cycles: A cross-sectional study. Int. J. Reprod. Biomed. 2023, 21, 53–60. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, Y.; Gu, H.T.; Feng, Q.L.; Liu, J.Y.; Zhou, J.; Yan, F. Association between assisted reproductive technology and cardiac alteration at age 5 years. JAMA Pediatr. 2015, 169, 603–605. [Google Scholar] [CrossRef]
- von Arx, R.; Allemann, Y.; Sartori, C.; Rexhaj, E.; Cerny, D.; de Marchi, S.F.; Soria, R.; Germond, M.; Scherrer, U.; Rimoldi, S.F. Right ventricular dysfunction in children and adolescents conceived by assisted reproductive technologies. J. Appl. Physiol. (1985) 2015, 118, 1200–1206. [Google Scholar] [CrossRef]
- Ceelen, M.; van Weissenbruch, M.M.; Roos, J.C.; Vermeiden, J.P.; van Leeuwen, F.E.; Delemarre-van de Waal, H.A. Body composition in children and adolescents born after in vitro fertilization or spontaneous conception. J. Clin. Endocrinol. Metab. 2007, 92, 3417–3423. [Google Scholar] [CrossRef]
- Ceelen, M.; van Weissenbruch, M.M.; Vermeiden, J.P.; van Leeuwen, F.E.; Delemarre-van de Waal, H.A. Cardiometabolic differences in children born after in vitro fertilization: Follow-up study. J. Clin. Endocrinol. Metab. 2008, 93, 1682–1688. [Google Scholar] [CrossRef]
- Sakka, S.D.; Loutradis, D.; Kanaka-Gantenbein, C.; Margeli, A.; Papastamataki, M.; Papassotiriou, I.; Chrousos, G.P. Absence of insulin resistance and low-grade inflammation despite early metabolic syndrome manifestations in children born after in vitro fertilization. Fertil. Steril. 2010, 94, 1693–1699. [Google Scholar] [CrossRef]
- Qin, J.; Liu, X.; Sheng, X.; Wang, H.; Gao, S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: A meta-analysis of cohort studies. Fertil. Steril. 2016, 105, 73–85.e6. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.B.; Sheng, X.Q.; Wu, D.; Gao, S.Y.; You, Y.P.; Yang, T.B.; Wang, H. Worldwide prevalence of adverse pregnancy outcomes among singleton pregnancies after in vitro fertilization/intracytoplasmic sperm injection: A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2017, 295, 285–301. [Google Scholar] [CrossRef] [PubMed]
- Cavoretto, P.; Candiani, M.; Giorgione, V.; Inversetti, A.; Abu-Saba, M.M.; Tiberio, F.; Sigismondi, C.; Farina, A. Risk of spontaneous preterm birth in singleton pregnancies conceived after IVF/ICSI treatment: Meta-analysis of cohort studies. Ultrasound Obstet. Gynecol. 2018, 51, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Morel, F.; Douet-Guilbert, N.; Le Bris, M.J.; Amice, V.; Le Martelot, M.T.; Roche, S.; Valeri, A.; Derrien, V.; Amice, J.; De Braekeleer, M. Chromosomal abnormalities in couples undergoing intracytoplasmic sperm injection. A study of 370 couples and review of the literature. Int. J. Androl. 2004, 27, 178–182. [Google Scholar] [CrossRef]
- Schneuer, F.J.; Milne, E.; Jamieson, S.E.; Pereira, G.; Hansen, M.; Barker, A.; Holland, A.J.A.; Bower, C.; Nassar, N. Association between male genital anomalies and adult male reproductive disorders: A population-based data linkage study spanning more than 40 years. Lancet Child. Adolesc. Health 2018, 2, 736–743. [Google Scholar] [CrossRef]
- Beydoun, H.A.; Sicignano, N.; Beydoun, M.A.; Matson, D.O.; Bocca, S.; Stadtmauer, L.; Oehninger, S. A cross-sectional evaluation of the first cohort of young adults conceived by in vitro fertilization in the United States. Fertil. Steril. 2010, 94, 2043–2049. [Google Scholar] [CrossRef]
| Year | Design | Sample | Outcome | Mean ± SD | CI | ||
|---|---|---|---|---|---|---|---|
| ART | Control Group | ||||||
| Tommaso et al. [12] | 2010–2017 | Retrospective case–control study | 71 | 640 | No difference | ||
| Simpson et al. [13] | 1997 | Prospective cohort study | 6077 | General population | No difference | ||
| Marconi et al. [14] | 1991–2012 | Retrospective cohort study | 11.152 Blastocysts vs. 55.995 cleavages | General population | No difference at the risk of preterm birth | PTB: 1 (0.79–1.25) LBW: 0.92 (0.73–1.16) | 99.5% |
| Sunkara et al. [15] | 1991–2011 | Retrospective cohort study | 584,835 Stimulated IVF cycles | 6168 unstimulated | No significant difference | PTB: 1.27 (0.8–2) LBW: 1.48 (0.9–2.42) | 95% |
| Sunkara et al. [16] | 1996–2011 | Retrospective cohort study | 439 | 87.571 | No difference | PTB: 0.68 (0.46–0.99) LBW: 0.56 (0.37–0.85) | 95% |
| Premru-Srsen T. et al. [17] | 2012–2015 | Retrospective case–control study | 333 | 1186 | Increased risk but not statistically significant | PTB: 1.07 (0.63–1.81) | 95% |
| Scherrer et al. [18] | 2007–2010 | Prospective cohort study | 65 | 57 | No increase in PTB and LBW risk | ||
| Szymusik et al. [19] | 2004–2014 | Retrospective case–control study | 336 | 308 | Increased risk for PTB and LBW | PTB (OR = 2.06; 1.16–3.68) LBW: (OR = 2.27; 1.19–4.36) | 95% |
| Kaveh et al. [20] | 2004–2009 | Retrospective case–control study | 84 | 106 | Significant higher risk for preterm labor | PROM: 0.2 (0.07–0.8) LBW: 1.4 (0.6–3) | 95% |
| Al-Fifi et al. [21] | 2003–2007 | Retrospective case–control study | 327 | 354 | Shorter birth date at ICSI group. | ||
| Kamath et al. [22] | 1991–2011 | Retrospective case–control study | 5929 | 127.856 | Higher risk for PTB and LBW | PTB: 1.54 (1.34–1.80) LBW: 1.43 (1.24–1.66) | 99.5% |
| Sunkara et al. [23] | 1991–2008 | Observational study | 65.868 live births after ART | General population | Significantly higher risk of PTB and LBW in the study | PTB: 1.15 (1.03–1.28) LBW: 1.17 (1.05–1.30) | 95% |
| Year | Design | Sample | Outcome | Mean ± SD | CI | ||
|---|---|---|---|---|---|---|---|
| ART | Control Group | ||||||
| Marconi et al. [14] | 1991–2012 | Retrospective cohort study | 11.152 Blastocyst-stage vs. 55.995 cleavage-stage | General population | 16% higher risk in blastocyst stage group | 0.9–1.49 | 99.5% |
| Al-Fifi et al. [21] | 2003–2007 | Retrospective case–control Study | 327 | 354 | No difference for major defects | ||
| Yuan et al. [24] | 2004–2020 | Retrospective cohort study | 1496 | 1396 | Slight but not statistically significant increase | 1.03 (0.71–1.5) | 95% |
| Olson et al. [25] | 1989–2002 | Retrospective cohort study | 1805 | 8422 | Slightly higher rate of major birth defects | 1.30 (1–1.67) | 95% |
| Luke et al. [26] | 2004–2017 | Population-based cohort study | 165.125 ART, 12.451 OI/IUI | 1.353.440 | Higher risk | 1.22–1.85 | 95% |
| Fauque et al. [27] | 2013–2017 | Retrospective cohort study | 20.218 IUI, 45.303 fresh-ET 18.885 FET | 3.417.089 from NC | Increased risk in fresh-ET and FET group. | Fresh-ΕΤ: 1.15 (1.1–1.2) FET: 1.13 (1.05–1.21) | 95% |
| Belva et al. [28] | 2004–2012 | Prospective clinical follow-up study | 1114 | General population | Abnormal fetal karyotype was found 41/1114 | 3.7% (2.7–4.9%) | 95% |
| Jozwiak et al. [29] | 1997–2002 | Retrospective case–control study | 1136 | General population | No difference between ICSI group due to male factor and other subfertility issues | ||
| Samli et al. [30] | 1996–2000 | Prospective cohort Study | 142 | General population | Increased rate of genetic defects in ICSI pregnancies | ||
| Year | Design | Sample | Outcome | Mean ± SD | CI | ||
|---|---|---|---|---|---|---|---|
| ART | Control Group | ||||||
| Simpson et al. [13] | 1997 | Prospective cohort Study | 6077 | General population | Increased risk for hypospadias | 2.9 (1.4–5.4) | 95% |
| Silver et al. [32] | 1988–1994 | Retrospective case–control study | 14 | 14 | 5x higher risk in IVF group versus the control group | 1.46% IVF 0.27% control | |
| Funke et al. [33] | 1999–2008 | Retrospective case–control study | 890 | 14316 | Increased risk for hypospadias; not cryptorchidism | 3.19 (1.266–8.042) | 95% |
| Bang et al. [34] | 2008–2011 | Prospective cohort study | 7752 | General population | Increased risk in the ART group | 99 (1.3%) cryptorchidism 8 (0.1%) hypospadias 4(0.05%) both | |
| Aliani et al. [35] | 2013–2015 | Prospective cross-sectional study | 5608 | General population | No relationship with infertility factor | 0.34% cryptorchidism 0.038% hypospadias | |
| Year | Design | Sample | Outcome | Mean ± SD | CI | ||
|---|---|---|---|---|---|---|---|
| ART | Control Group | ||||||
| Scherrer et al. [18] | 2007–2010 | Prospective cohort study | 65 | 57 | ART group: 25% smaller brachial artery, 30% higher pulmonary artery pressure. | ||
| Liu et al. [36] | 2015 | Prospective observational study | 100 | 100 | Higher rates in systolic and diastolic heart disorders | ||
| Arx et al. [37] | 2015 | Prospective clinical trial | 54 | 54 | RV end-diastolic area significantly larger in study group; no difference in pulmonary artery pressure | ||
| Ceelen et al. [38] | 1986–1995 | Retrospective cohort study | 233 | 233 | Higher body fat percentage in study group | ||
| Ceelen et al. [39] | 1986–1995 | Retrospective cohort study | 1313 | 131 | Elevated rates of BP and blood glucose in ART group | Systolic BP: 2.1 (1.4–3.3) Diastolic: 1.9 (1.2–3) | 95% |
| Sakka et al. [40] | 2010 | Prospective case–control study | 106 | 68 | Higher systolic and diastolic BP and TRG. | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Potiris, A.; Perros, P.; Drakaki, E.; Mavrogianni, D.; Machairiotis, N.; Sfakianakis, A.; Karampitsakos, T.; Vrachnis, D.; Antonakopoulos, N.; Panagopoulos, P.; et al. Investigating the Association of Assisted Reproduction Techniques and Adverse Perinatal Outcomes. J. Clin. Med. 2024, 13, 328. https://doi.org/10.3390/jcm13020328
Potiris A, Perros P, Drakaki E, Mavrogianni D, Machairiotis N, Sfakianakis A, Karampitsakos T, Vrachnis D, Antonakopoulos N, Panagopoulos P, et al. Investigating the Association of Assisted Reproduction Techniques and Adverse Perinatal Outcomes. Journal of Clinical Medicine. 2024; 13(2):328. https://doi.org/10.3390/jcm13020328
Chicago/Turabian StylePotiris, Anastasios, Paraskevas Perros, Eirini Drakaki, Despoina Mavrogianni, Nikolaos Machairiotis, Antonios Sfakianakis, Theodoros Karampitsakos, Dionysios Vrachnis, Nikolaos Antonakopoulos, Periklis Panagopoulos, and et al. 2024. "Investigating the Association of Assisted Reproduction Techniques and Adverse Perinatal Outcomes" Journal of Clinical Medicine 13, no. 2: 328. https://doi.org/10.3390/jcm13020328
APA StylePotiris, A., Perros, P., Drakaki, E., Mavrogianni, D., Machairiotis, N., Sfakianakis, A., Karampitsakos, T., Vrachnis, D., Antonakopoulos, N., Panagopoulos, P., Drakakis, P., & Stavros, S. (2024). Investigating the Association of Assisted Reproduction Techniques and Adverse Perinatal Outcomes. Journal of Clinical Medicine, 13(2), 328. https://doi.org/10.3390/jcm13020328








